Abstract
Purpose
To evaluate the time cost of intraoperative aberrometry (IA), to compare IA prediction error to the prediction error associated with conventional formulas using preoperative calculations (PC) and evaluate when IA provides clinically relevant benefit.
Methods
This is a retrospective study of eyes that underwent cataract phacoemulsification surgery with IA at an academic eye center. IA versus PC prediction error were compared amongst various preoperative and intraoperative characteristics. Additionally, a dichotomous variable indicating clinically relevant benefit of IA, where IA absolute prediction error was less than 0.5D and PC absolute prediction error greater than 0.5D, was associated with clinical factors.
Results
Five hundred eyes of 341 patients were included in the analysis. The quantitative difference between mean absolute prediction errors for IA versus PC was between 0.0D and 0.03D in most subgroups. For the 11.0% of eyes that had clinically relevant benefit to IA, the multivariable model identified the following strongest predictors: prior myopic corneal refractive surgery (Odds ratio (OR) 3.9, p<0.01 for myopic LASIK/PRK, OR 5.5, p=0.01 for radial keratotomy), toric or multifocal/EDOF lens implantation (OR 2.7, p=0.03 for toric monofocal lenses, OR 3.1, p=0.01 for EDOF/multifocal lenses), and short and long axial lengths (p<0.01). On average, IA implementation added 3.0 minutes to surgery (p<0.01).
Conclusion
For greatest likelihood of a clinically meaningful improvement in outcomes despite increased surgical time, surgeons and patients should consider using IA for eyes with extremes in axial length, eyes with prior myopic corneal refractive surgery, or when implanting lenses with toric or extended-depth-of-focus/multifocal properties.
Keywords: intraoperative aberrometry, IOL calculations, cataract refractive outcomes
Introduction
Cataract surgery has increasingly become a precise refractive procedure. Success is no longer marked merely by removal of the cataractous lens, but also by achieving the refractive target defined preoperatively. Several generations of intraocular lens (IOL) formulas have been developed to enhance refractive outcomes. Recent studies with large numbers of non-post refractive eyes have endorsed the Barrett Universal II Formula1 and the Kane formula2 as the most accurate formulas using preoperative measurements to calculate prediction error.
Intraoperative aberrometry (IA) is the most common supplement to IOL predictions based on formulas and preoperative measurements. Talbot-Moiré interferometry measurements can be captured by the Optiwave Refractive Analysis (ORA) System (Alcon Laboratories Inc, Fort Worth, TX) intraoperatively to assist in IOL selection using a modified vergence formula.3 A multicenter study found that in eyes without history of refractive surgery, use of IA improved the percentage of eyes with a postoperative absolute refractive error of 0.5 diopters (D) or less from 75.9% using conventional IOL formulas to 81.9% using IA (p<0.0001).4 As over 3 million cataract surgeries occur per year in the United States, this represents a significant improvement in patients who would be left with nominal refractive error after surgery with IA.
Surveys from the American Society of Cataract and Refractive Surgery report that the number of surgeons using IA grew from 15% in 2016 to 28% in 2017 and has since remained relatively stable.5,6 Despite this growth in use, there is a paucity of data on the time utilization and clinical benefit of IA.
We present data on prediction error of all cases using IA at an academic medical center, including high-risk subgroups such as prior refractive surgery or very long or short eyes. We also address the added time of performing IA, as well as model predictors for those cases in which IA is most beneficial.
Methods
The study was conducted in compliance with the Declaration of Helsinki and was reviewed and approved by the Colorado Multiple Institutional Review Board with a waiver of consent due to the retrospective nature of the study. Patient confidentiality was maintained with anonymization following data abstraction.
Data Extraction
Data from eyes that underwent cataract surgery with IA by two surgeons at our institution (MT and RD) between January 1, 2015 and December 31, 2018 were collected retrospectively. Data collected included biometry measurements by IOLMaster 500 (software version V.7.7, Carl Zeiss Meditech, Jena, Germany), IOL formula used, lens type implanted (ZCB00, ZCTxxx, ZXR00, ZXTxxx (Johnson & Johnson, Santa Ana, California), MX60 (Bausch and Lomb, Bridgewater, NJ), or SN60WF, SA6ATx, SV25Tx, SN6ADx (Alcon, Fort Worth, Texas)), femtosecond laser use, surgery length, and postoperative refraction collected by an experienced ophthalmic technician at the last visit available between 3 and 26 weeks following cataract surgery.
Preoperative IOL calculations (PC) were performed using the surgeon’s best choice of formulas (SRK/T, Hoffer Q, Holladay 1, Holladay 2, and Barrett Universal II) prior to surgery. The online Barrett True K calculator was used to determine predicted refraction retrospectively for post-refractive surgery eyes.7
Cataract phacoemulsification was performed in the standard fashion, with or without femtosecond laser based on surgeon preference. Intraoperative aphakic lens measurements were collected using the ORA device following instillation of a cohesive viscoelastic and use of a Barraquer tonometer to achieve pressure around 21mm Hg. The intraocular lens selected for implantation was based on the surgeon’s best prediction using information from both PC and IA. In cases where IA and PC both predicted the same lens, that mutually predicted lens was typically chosen. In cases where IA and PC differed in their lens prediction, the surgeons most often would choose the lens predicted by IA or one between the IA and PC prediction.
Surgery length was calculated for all IA cases using the operative record. For purposes of computing the additional time required for IA, a cohort of all non-IA cataract surgeries for the same two surgeons over the same time period with the same exclusion criteria was defined, and surgery length was computed for these cases as well.
Inclusion/Exclusion Criteria
Only eyes with complete data meaning both postoperative refraction and ORA database prediction information were included. Practice patterns at our center consist most often of recommending IA to any patient with prior corneal refractive surgery (LASIK, PRK, RK) as well as commonly to those patients electing implantation of a toric, multifocal, or extended depth-of-focus IOL or corneal astigmatism correction (limbal relaxing incisions) to be performed intraoperatively, therefore these are the eyes most predominantly represented in this study. Patients with traumatic cataracts or combined surgeries such as vitrectomy and minimally invasive glaucoma surgery were excluded from this study, as were cases which had a posterior capsule rupture or vitreous loss. Eyes for which IA was used for toric rotation or pseudophakic measurements (a minority at this institution due to practice patterns) were excluded, however, eyes for which aphakic IA measurements were captured to aid in spherical strength selection of a toric lens without attention to axis were included. Patients with final postoperative corrected distance visual acuity worse than 20/40 were excluded from the study.
Statistical Analysis
Refraction prediction error (RPE) was calculated as the difference between actual postoperative refraction and predicted refraction for both IA and PC. Since errors in either direction are clinically relevant, the absolute value of the prediction error for each method was used for analysis and summarized by mean absolute error (MAE) and median absolute error (MedAE).
Surgery length for IA cases was collected from the operating room documentation and compared to surgery length for all non-IA cases for the same two surgeons during the same time period using means and standard deviations. Linear regression modeling with generalized estimating equations was used for statistical comparisons to account for some patients having two eyes included in the study. Modeling was performed with and without adjusting for individual surgeon since the two surgeons had slightly different average surgery lengths.
Separate calculations were performed and reported for the outcomes of interest: 1) IA versus PC prediction errors as continuous variables for various subgroups, and 2) a prediction model using a dichotomous outcome indicating clinically relevant benefit of IA. For the first outcome of interest, IA versus PC prediction errors, generalized linear models were used to univariately compare the errors from both methods, stratified by each clinical factor, using a gamma distribution and generalized estimating equations (GEE) to account for inclusion of both eyes for some subjects.
For the second outcome of interest, a dichotomous variable was defined for eyes in which the IA prediction error was less than 0.5D and the PC prediction error was greater than 0.5D to indicate clinically relevant benefit of using IA. A GEE model was fit for this binary variable as the dependent variable, using a binomial distribution and a logit link. Backward variable selection was used to identify a small set of important predictors. All analyses were performed using SAS Version 9.4 software; the GEE models were fit using PROC GENMOD with repeated measures indicated using a nested eye within subject effect and unstructured working correlation matrix (SAS Institute, Inc., Care, NC, 2018).
Results
Demographic Information
There were 636 eyes from 451 patients that underwent cataract surgery with plan for IA by the two surgeons at our institution during the time period selected. Of those, eight were excluded for postoperative corrected vision worse than 20/40, 52 were missing postoperative refraction data, and 76 were missing IA data either because the surgeon decided not to use IA or because the aberrometer was unable to register accurate readings. This left 500 eyes of 341 patients for analysis. All patients were greater than 18 years of age (average 67.9 ± 8.6 years), 64.8% were female, and the vast majority (90.6%) were white (Table 1).
Table 1.
Subject Demographics and Preoperative Characteristics
| Number (%), or Mean (SD) | |
|---|---|
| Patients (N=341) | |
| Female | 221 (64.8%) |
| Race | |
| White | 309 (90.6%) |
| Black | 7 (2.1%) |
| Asian | 10 (2.9%) |
| Hispanic | 4 (1.2%) |
| Unknown/Other | 11 (3.2%) |
| BMI (kg/m2) | 25.5 (5.2) |
| Age (years) | 67.9 (8.6) |
| Eyes (N=500) | |
| Axial Length (mm) | 25.1 (1.6) |
| Flattest K (D) | 41.8 (3.0) |
| Steepest K (D) | 43.0 (3.1) |
Abbreviations: BMI, body mass index; K, keratometry; D, diopters.
Most eyes (51.4%) underwent implantation of a non-toric monofocal lens. As it is customary in these two surgeons’ practice to use IA in most cases with history of refractive surgery, 55.0% of the eyes had a history of refractive surgery (myopic or hyperopic LASIK/PRK or radial keratotomy). Forty-eight percent of included surgeries were performed with assistance of the femtosecond laser.
For preoperative measurement IOL and refractive error prediction, 42.0% of eyes were calculated using the Holladay 1 formula, 29.9% using the SRK/T formula, 21.8% using the Barrett Universal II formula, 4.9% using the Hoffer Q formula, and 1.2% using the Holladay 2 formula.
IA versus PC Prediction Errors for Various Subgroups
The RPE, MAE, and MedAE for the following subgroups were evaluated: lens type (monofocal, monofocal toric, multifocal/EDOF), history of refractive surgery (none, myopic LASIK/PRK, hyperopic LASIK/PRK, and RK), axial length (>26.5mm, <26.5mm), steepest keratometry > 46D, flattest keratometry < 40D, and femtosecond laser-assisted cataract surgery. For two subgroups, the difference between IA and PC predictions was statistically significant with a difference of 0.03D: the no history of refractive surgery group (MAE 0.34D for IA versus 0.37D for PC (p=0.04)), and the femtosecond laser-assisted cataract surgery group (MAE 0.37D for IA vs 0.40D for PC (p=0.01)). The absolute prediction error was not significantly different between IA and PC for any other subgroup and generally the MAE between IA and PC differed by between 0.0D and 0.03D in either direction for all subgroups (with the exception of post-hyperopic LASIK/PRK with MAE for IA 0.53D vs PC 0.45D (p=0.32)). The highest MAEs were found in the group of 37 eyes (7.4%) with a history of radial keratotomy (MAE 0.71D for IA and 0.70D for PC (p=0.98)), followed by the group of 135 eyes (27.0%) with a flattest keratometry value less than 40.0D (MAE 0.61D for IA and 0.58D for PC (p=0.51)).
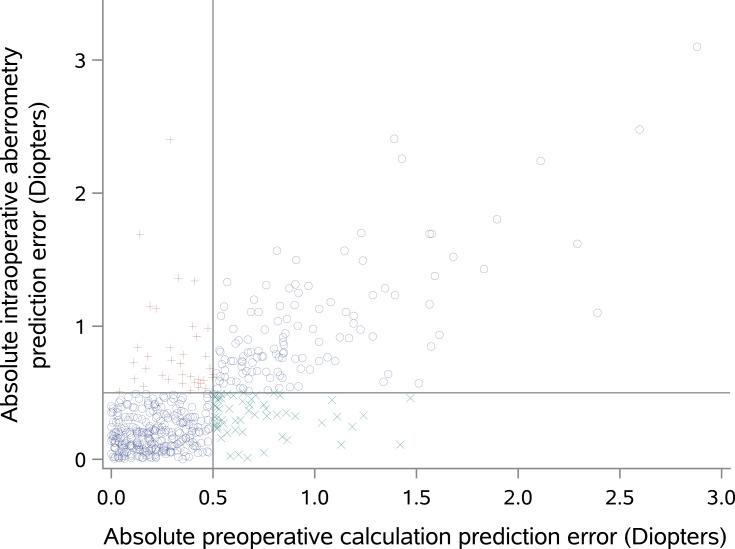
Predictors for Situations Where IA is Most Beneficial
Eyes were divided into categories using the cutoff of 0.5D prediction error to define clinically relevant accuracy of predictions by IA and PC (Table 2). Two hundred eighty-eight eyes (57.6%) had prediction errors less than 0.5D simultaneously for both IA and PC. One hundred nineteen (23.8%) had prediction errors worse than 0.5D simultaneously for both IA and PC. Of the remaining eyes, 55 (11.0%) had an error of less than 0.5D for IA and greater than 0.5D for PC, and 38 (7.6%) had an error of less than 0.5D for PC and greater than 0.5D for IA (Figure 1).
Table 2.
Distribution of Absolute Prediction Error for Intraoperative Aberrometry (IA) and Preoperative Calculation (PC) by Category (Greater Than or Less Than 0.5 Diopters)
| Variables | n | IA Error <0.5D, PC Error >0.5D (11.0% of All Eyes) | IA Error >0.5D, PC Error >0.5D (23.8% of All Eyes) | IA Error <0.5D, PC Error <0.5D (57.6% of All Eyes) | IA Error >0.5D, PC Error <0.5D (7.6% of All Eyes) |
|---|---|---|---|---|---|
| Monofocal lens | 257 | 26 (10.1%) | 77 (30%) | 134 (52.1%) | 20 (7.8%) |
| Toric monofocal lens | 105 | 11 (10.5%) | 25 (23.8%) | 61 (58.1%) | 8 (7.6%) |
| EDOF/multifocal lens | 138 | 18 (13%) | 17 (12.3%) | 93 (67.4%) | 10 (7.2%) |
| No prior refractive surgery | 225 | 20 (8.9%) | 37 (16.4%) | 154 (68.4%) | 14 (6.2%) |
| Prior myopic laser refractive surgery | 219 | 26 (11.9%) | 64 (29.2%) | 112 (51.1%) | 17 (7.8%) |
| Prior hyperopic laser refractive surgery | 19 | 4 (21.1%) | 4 (21.1%) | 9 (47.4%) | 2 (10.5%) |
| Prior radial keratotomy | 37 | 5 (13.5%) | 14 (37.8%) | 13 (35.1%) | 5 (13.5%) |
| Axial Length < 26.5mm | 91 | 12 (13.2%) | 28 (30.8%) | 39 (42.9%) | 12 (13.2%) |
| Axial length > 26.5mm | 409 | 43 (10.5%) | 91 (22.2%) | 249 (60.9%) | 26 (6.4%) |
| Axial Length > 23.0mm | 461 | 46 (10%) | 111 (24.1%) | 268 (58.1%) | 36 (7.8%) |
| Axial Length < 23.0mm | 39 | 9 (23.1%) | 8 (20.5%) | 20 (51.3%) | 2 (5.1%) |
| IA and PC predicted same lens | 135 | 12 (8.9%) | 29 (21.5%) | 89 (65.9%) | 5 (3.7%) |
| IA and PC differed, and something between PC and IA was chosen | 247 | 32 (13%) | 69 (27.9%) | 120 (48.6%) | 26 (10.5%) |
| IA and PC prediction differed, and PC was chosen | 118 | 11 (9.3%) | 21 (17.8%) | 79 (66.9%) | 7 (5.9%) |
| Steepest keratometry > 46D | 419 | 42 (10%) | 100 (23.9%) | 246 (58.7%) | 31 (7.4%) |
| Steepest keratometry < 46D | 81 | 13 (16%) | 19 (23.5%) | 42 (51.9%) | 7 (8.6%) |
| Flattest keratometry > 40D | 365 | 41 (11.2%) | 72 (19.7%) | 229 (62.7%) | 23 (6.3%) |
| Flattest keratometry < 40D | 135 | 14 (10.4%) | 47 (34.8%) | 59 (43.7%) | 15 (11.1%) |
| No femtosecond laser | 211 | 24 (11.4%) | 57 (27%) | 110 (52.1%) | 20 (9.5%) |
| Used femtosecond laser (excludes 49 unknown eyes) | 240 | 28 (11.7%) | 47 (19.6%) | 150 (62.5%) | 15 (6.3%) |
| Horizontal white-to-white < 13.0mm | 488 | 54 (11.1%) | 115 (23.6%) | 283 (58%) | 36 (7.4%) |
| Horizontal white-to-white ≥ 13.0mm | 12 | 1 (8.3%) | 4 (33.3%) | 5 (41.7%) | 2 (16.7%) |
| Preoperative astigmatism < 2D | 427 | 44 (10.3%) | 100 (23.4%) | 251 (58.8%) | 32 (7.5%) |
| Preoperative astigmatism ≥ 2D | 73 | 11 (15.1%) | 19 (26%) | 37 (50.7%) | 6 (8.2%) |
Figure 1.
Absolute prediction errors for preoperative calculation versus intraoperative aberrometry. Reference lines included at 0.5D, eyes that benefited from intraoperative aberrometry in the most clinically relevant way are indicated in green, and those where the intraoperative aberrometry prediction would potentially negatively impact the preoperative calculation prediction are indicated in red.
Further evaluation was performed on the 11.0% of eyes for which IA was most beneficial (cases where prediction error less than 0.5D for IA and greater than 0.5D for PC, making it a situation where the surgeon and patient would likely be more willing to invest in IA to substantively improve results) (Table 3).
Table 3.
Variables and Their Univariate Association with Intraoperative Aberrometry Prediction Being Less Than 0.5 Diopters and Preoperative Calculation Prediction Being Greater Than 0.5 Diopters
| n/N | OR (95% CI) | p-value | |
|---|---|---|---|
| Monofocal lens | 26/257 | Reference | |
| Toric monofocal lens | 11/105 | 1.04 (0.49, 2.19) | 0.92 |
| EDOF/multifocal lens | 18/138 | 1.33 (0.70, 2.53) | 0.38 |
| No prior refractive surgery | 20/225 | Reference | |
| Prior myopic laser refractive surgery | 26/219 | 1.38 (0.75, 2.55) | 0.30 |
| Prior hyperopic laser refractive surgery | 4/19 | 2.73 (0.83, 9.03) | 0.10 |
| Prior radial keratotomy | 5/37 | 1.60 (0.56, 4.57) | 0.38 |
| Axial Length < 26.5mm | 43/409 | Reference | |
| Axial Length > 26.5mm | 12/91 | 1.29 (0.65, 1.56) | 0.46 |
| Axial Length > 23.0mm | 46/461 | Reference | |
| Axial Length < 23.0mm | 9/39 | 2.71 (1.21, 6.05) | 0.02 |
| IA and PC predicted same lens | 12/135 | Reference | |
| IA and PC differed, and something between PC and IA was chosen | 32/247 | 1.53 (0.76, 3.07) | 0.24 |
| IA and PC prediction differed, and PC was chosen | 11/118 | 1.05 (0.45, 2.49) | 0.90 |
| Steepest keratometry > 46D | 42/419 | Reference | |
| Steepest keratometry < 46D | 13/81 | 1.72 (0.88, 3.37) | 0.12 |
| Flattest keratometry > 40D | 41/365 | Reference | |
| Flattest keratometry < 40D | 14/135 | 0.91 (0.48, 1.74) | 0.78 |
| No femtosecond laser used | 24/211 | Reference | |
| Femtosecond laser used (unknown 49 eyes excluded) | 28/240 | 1.03 (0.58, 1.84) | 0.92 |
| Horizontal white-to-white <13.0mm | 54/488 | Reference | |
| Horizontal white-to-white ≥ 13.0mm | 1/12 | 0.73 (0.09, 5.77) | 0.77 |
| Preoperative astigmatism < 2D | 44/427 | Reference | |
| Preoperative astigmatism ≥ 2D | 11/73 | 1.54 (0.76, 3.15) | 0.23 |
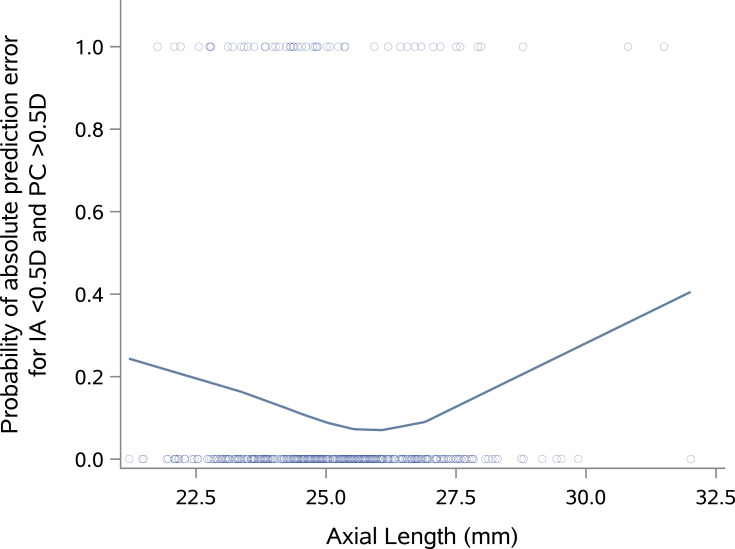
After fitting a multivariable prediction model to this binary outcome, toric monofocal lenses and EDOF/multifocals were both found to be significant predictors (OR 2.7, 95% CI (1.1, 6.8), p=0.03 and OR 3.1, 95% CI (1.3, 7.1), p=0.01) as compared to monofocal lenses. Similarly, prior myopic LASIK/PRK or radial keratotomy were both associated with IA prediction error being less than 0.5D and PC prediction error being greater than 0.5D (OR 3.9, 95% CI (1.6, 9.9), p<0.01 and OR 5.5, 95% CI (1.5, 20.3), p=0.01 as compared to eyes with no prior refractive surgery). Axial length was associated with the outcome of interest in a quadratic fashion, with short and long axial lengths being more likely to simultaneously have IA prediction error less than 0.5D and PC prediction error greater than 0.5D (p<0.01) (Table 4, Figure 2).
Table 4.
Multivariable Model for Variables That Best Predict Conditions in Which Intraoperative Aberrometry Prediction Error Was Less Than 0.5D and Preoperative Calculations Prediction Error Was Greater Than 0.5D
| n/N | OR (95% CI) | p-value | |
|---|---|---|---|
| Toric Monofocal | 11/105 | 2.7 (1.1, 6.8) | 0.03 |
| EDOF/Multifocal | 18/138 | 3.1 (1.3, 7.1) | 0.01 |
| Prior Myopic LASIK/PRK | 26/219 | 3.9 (1.6, 9.9) | <0.01 |
| Prior Hyperopic LASIK/PRK | 4/19 | 2.4 (0.5, 11.0) | 0.26 |
| Prior Radial Keratotomy | 5/37 | 5.5 (1.5, 20.3) | 0.01 |
| Axial Length* | – | <0.01 | |
| Axial Length * Axial Length | – | <0.01 |
Note: *Since the association with axial length was not linear, a quadratic term was added. Odds ratios are therefore not provided for this set of parameters.
Figure 2.
Association between the probability that intraoperative aberrometry is beneficial (IA prediction error was less than 0.5D and preoperative calculation prediction error was greater than 0.5D) versus axial length. The points represent the observed data and are stacked at values of 1 (IA was beneficial) or 0 (otherwise). A scatterplot smoother illustrates the non-linear association between the probability that IA was beneficial and axial length.
Similar analysis was performed for the 38 eyes (7.6%) where PC prediction error was <0.5D and IA prediction error was >0.5D. However, no ocular or lens-choice variables emerged as significant predictors.
Case Time
The mean case time for surgeries with IA was 18.3±5.3 minutes, median 18.0 minutes, and range 9–48 minutes. For the 2241 non-IA cases performed by the same two surgeons during the same time frame the mean case time was 15.3±6.7 minutes, median 13.0 minutes, and range 5–84 minutes. Overall, the mean IA case length was 3.0 minutes slower when using IA, and the median case length was 5.0 minutes slower. This difference was statistically significant (p<0.01).
Complex surgeries (defined as use of mechanical iris expansion, trypan blue dye for capsule visualization, or capsular tension ring) were more common in the non-IA group (16.0% vs 9.8%). A sub-analysis was performed excluding complex surgeries from both groups, and the mean and median case times for IA surgeries were 17.7 ± 4.6 and 17.0 minutes compared to non-IA surgeries mean and median case times of 14.4 ± 5.5 and 13.0 minutes, with IA surgeries having a 3.3 minute slower mean case length and 4.0 minute slower median case length. This difference was highly significant (p<0.0001). After including complex surgery and surgeon in a multivariate model, there is still a significant difference in surgery times for ORA cases (p<0.0001). Rates of IA use were similar between the two surgeons (17.6% and 14.3%).
Discussion
Intraoperative aberrometry devices are being increasingly used as a supplement to preoperative measurements in determining best intraocular lens strength. However, studies of which eyes are most likely to benefit from the technology in a clinically significant way are limited. As a continuous variable, the absolute prediction errors for both IA and PC had a statistical difference for only two subgroups analyzed; however, the magnitude of this difference for these subgroups (0.03D) as well as the others was very small. Still, we found that patients electing to receive a premium IOL (toric monofocal, multifocal, and extended depth of focus lenses), eyes with history of myopic LASIK/PRK or RK, and eyes with short or long axial lengths are more likely to benefit in a substantive way from IA measurements. This benefit, nevertheless, was associated with an average increased surgical length of 3 minutes (or 3.3 minutes when comparing only non-complex cases).
When analyzing prediction error as a continuous variable and comparing IA versus PC in different subgroups of patients, observed differences in the two prediction techniques existed for just two subgroups of eyes: those without prior corneal refractive surgery and those for which surgery was performed using femtosecond laser. However, the mean difference in prediction error was 0.03D. Overall, there were no groups with a clinically significant difference in prediction accuracy and generally, the IA and PC predictions were highly correlated.
Subsequent analysis was performed to identify predictors for which eyes IA would be most beneficial, defined as an IA prediction error of less than 0.5D accompanied by PC prediction error of greater than 0.5D (this group made up 11.0% of eyes in our study). The multivariable model elicited several variables that were predictive: toric monofocal lenses, EDOF/multifocal lenses, prior myopic LASIK/PRK, and prior RK (OR 2.7, 95% CI (1.1, 8.8), p=0.03, OR 3.1, 95% CI (1.3, 7.1), p=0.01, OR 3.9, 95% CI (1.6, 9.9), p<0.01, and OR 5.5, 95% CI (1.5, 20.3), p=0.01 respectively). Additionally, axial length was a significant predictor with short and long axial lengths being more likely to benefit from IA (p<0.01).
The increased length of time for surgeries utilizing IA can be attributed to many steps: preparing the eye for IA measurements with viscoelastic, confirming the intraocular pressure with the Barrequer tonometer, turning off the microscope light and getting the patient to fixate on the IA fixation target, taking the measurements (and repeating the measurements in some cases), making a lens selection, a surgical assistant confirming the lens choice on the aberrometry machine, the circulating nurse picking up the chosen lens (and potentially confirming the lens parameters again with the surgeon), opening of the lens and passing it onto the field, and folding the lens in the cartridge and loading it into the injector. The opening, folding, and loading steps are often done in parallel to the phacoemulsification part of the surgery for a non-IA case, but need to be done in sequence following IA measurements in cases where IA is used.
For efficient cataract surgeons, a 3.0-minute increase in case time could mean the loss of significant numbers of cases and/or revenue. Operating room time cost is difficult to calculate, but may range from $8.30 per minute8 to $11.24 per minute.9 On the other hand, if a surgery center is doing 20 cases per 10-hour day, and 3.0 minutes can be saved off of each case, two more cases could be done per day. In the United States, where the reimbursement for CPT code 66984 for a non-complicated cataract surgery is $654 in 2019,10 not operating on those extra two cases could represent a cost of approximately $1300 per operating room day for a high-volume surgeon. Some surgery centers offset a portion of this cost by charging the patient a fee for receiving IA measurements. However, for the vast majority of patients in our study (89%, ie all but 11.0%), there may not be a clinically significant benefit to the patient to electing this service. Even for the groups that are more likely to benefit from IA, such as premium lenses and prior myopic LASIK/PRK or RK, there is no assurance that the IA predictions are more accurate than the PC predictions in all cases. On the other hand, there is a cost associated with residual refractive error as well. Any improvement in accuracy of postoperative refraction could be reflected in a decreased need for future spectacle correction (a value that varies significantly, but may be estimated to be around $313 USD yearly11), lens exchange, or laser vision correction, and may certainly be worth the time cost to the surgeon and the financial cost to the patient.
Similar analysis for those eyes in which IA predictions are more likely to negatively impact the final refractive outcome (those eyes where PC prediction error is <0.5D and IA prediction error is >0.5D) would be useful for surgeons to avoid the time cost of using IA and possible inaccurate influence of its predictions. However, this group in our study was small (38 eyes, 7.6%) which made it difficult to draw any statistical conclusions. Future research on this concept is needed but does not detract from the important findings of identifying which eyes are most likely to benefit from spending the extra time and cost using IA.
Use of IA has some inherent limitations. First, eyelid squeezing, eye movement, pressure from the eyelid speculum, stromal hydration, and variations in intraocular pressure may all negatively affect the accuracy of its measurements. Despite this, there is evidence that these factors can be controlled in qualified surgeons’ hands and the surgeons in this study were experienced with the technology. Additionally, 76 eyes were excluded from this study due to missing IA data. This was either because IA was planned but the patient or surgeon changed their mind, or because the surgeon was unable to accurately register the IA device intraoperatively and so it was aborted. While it would be useful to know exactly what percentage of eyes were unable to be registered for this study, it is important for surgeons to consider this potential cost of time for eyes that may be high risk for not being able to register (patients with poor fixation, corneal scars or irregularities, etc).
There are some limitations to our study. First, multiple different lens types were used in this study (monofocal, monofocal toric, multifocal, extended depth of focus). This was to maximize the number of eyes included and is also representative of a realistic cataract surgery population. However, doing so introduces sources of variability. Our study may not have been powered to detect changes in accuracy between IA and PC for each subgroup analyzed. Also, the patients who had cataract surgery with IA at our institution may not be representative of the population as a whole. Patients with a history of corneal refractive surgery and patients electing to receive a toric, multifocal, or extended depth of focus lens are more often encouraged to undergo IA measurements during surgery at our institution. The IA group tended to have a higher proportion of white patients, female patients, patients with prior refractive surgery, and eyes with a longer axial length than our eye center as a whole. However, the IA group was biased towards eyes that are more likely to have an unexpected refractive outcome following cataract surgery, including eyes with a history of refractive surgery and those with long axial lengths, which makes it a particularly important group to study.12,13 Another weakness was the variability amongst preoperative prediction formulas used. The formula used was typically Barrett Universal II, Holladay 1, SRK/T (for long eyes), and Hoffer Q (for short eyes) using the Wang-Koch axial length correction as necessary,14 however specific subgroups that have benefit of IA versus PC may be different for different formulas. Limiting our actual postoperative refractive outcome to refractions collected in the 3–26 weeks postoperative time period with BCVA better than 20/40 increases the likelihood of a stable and reliable final postoperative refractive outcome. Refractions collected later in that period may have shifted some from early refractions secondary to capsule fibrosis and ideally would have been collected in a stricter timeframe. However, due to the retrospective nature of our study and practice patterns at our institution, a minority of our patients would have been eligible to study had a smaller timeframe been chosen.
As more modern IOL formulas improve, many of the pre-existing IA studies are becoming less informative. While IA has been shown to improve refractive accuracy for many patients,4,15,16 most comparisons that achieved statistical significance are comparisons with non-standardized aggregates of formulas or specifically comparing to “older” formulas such as Holladay 1, Holladay 2, and SRK/T. Comparison with newer formulas has shown that IA is equal or worse than the Barrett Universal II or Hill-RBF.17,18 IA has been reported to be similar to Barrett True-K for eyes with history of radial keratotomy,19 no different than Optovue, Haigis-L, or Masket regression formulas for eyes with prior laser vision correction,20 and in one study better than Haigis-L and Shammas and surgeon’s choice of formulas in eyes with prior laser vision correction.21 A similar study to ours using only newer formulas, such as the Barrett Universal II formula, Kane formula, or Hill-RBF in comparison to IA would be of interest, in particular for eyes with extremes of axial length for which these newer formulas may be an improvement over older formulas.
Conclusions
We present data on IA versus PC prediction errors for eyes undergoing cataract surgery at an academic medical center over a five-year period. This study includes eyes that are often high-risk for refractive surprises, including those with prior refractive surgery and those with extremes in axial lengths. The eyes for which IA was most beneficial in clinically relevant way (IA prediction error less than 0.5D and PC prediction error greater than 0.5D) were most common in the group with axial length further from the mean, and those with toric, EDOF/multifocal lenses, prior myopic LASIK/PRK, and prior RK. The eyes which would most benefit from IA should be considered carefully, especially considering the increased surgical time and associated costs with using IA technology.
Funding Statement
A Challenge Grant to the Department of Ophthalmology from Research to Prevent Blindness, Inc.
Data Presentation
Early data presented at the American Society of Cataract and Refractive Surgery Annual Meeting, May 4, 2019, San Diego, CA, USA.
Disclosure
None of the authors have any proprietary interests or conflicts of interest related to this submission.
References
- 1.Melles RB, Holladay JT, Chang WJ. Accuracy of intraocular lens calculation formulas. Ophthalmology. 2018;125(2):169–178. doi: 10.1016/j.ophtha.2017.08.027 [DOI] [PubMed] [Google Scholar]
- 2.Darcy K, Gunn D, Tavassoli S, Sparrow J, Kane JX. Assessment of the accuracy of new and updated intraocular lens power calculation formulas in 10 930 eyes from the UK National Health Service. J Cataract Refract Surg. 2020;46(1):2–7. doi: 10.1016/j.jcrs.2019.08.014 [DOI] [PubMed] [Google Scholar]
- 3.Cervino A, Hosking SL, Montes-Mico R, Bates K. Clinical ocular wavefront analyzers. J Refract Surg. 2007;23(6):603–616. doi: 10.3928/1081-597X-20070601-12 [DOI] [PubMed] [Google Scholar]
- 4.Cionni RJ, Dimalanta R, Breen M, Hamilton C. A large retrospective database analysis comparing outcomes of intraoperative aberrometry with conventional preoperative planning. J Cataract Refract Surg. 2018;44(10):1230–1235. doi: 10.1016/j.jcrs.2018.07.016 [DOI] [PubMed] [Google Scholar]
- 5.Sixth annual ASCRS clinical survey; 2018. Available from: https://supplements.eyeworld.org/eyeworld-supplements/december-2018-clinical-survey. Accessed September21, 2020.
- 6.Bethke W. Surgeons make do with the tried and true; 2017. Available from: https://www.reviewofophthalmology.com/article/surgeons-make-do-with-the-tried-and-true. Accessed September21, 2020.
- 7.Barrett True K Formula - for prior myopic or hyperopic lasik/prk/rk. Available from: http://calc.apacrs.org/Barrett_True_K_Universal_2105/. Accessed January20, 2021 Accessed May 1, 2020–July 30, 2020.
- 8.Hosler MR, Scott IU, Kunselman AR, Wolford KR, Oltra EZ, Murray WB. Impact of resident participation in cataract surgery on operative time and cost. Ophthalmology. 2012;119(1):95–98. doi: 10.1016/j.ophtha.2011.06.026 [DOI] [PubMed] [Google Scholar]
- 9.Taravella MJ, Davidson R, Erlanger M, Guiton G, Gregory D. Time and cost of teaching cataract surgery. J Cataract Refract Surg. 2014;40(2):212–216. doi: 10.1016/j.jcrs.2013.07.045 [DOI] [PubMed] [Google Scholar]
- 10.Physician Fee Schedule. Centers for medicare and medicaid services; April 3, 2020. Available from: https://www.cms.gov/apps/physician-fee-schedule/overview.aspx. Accessed April20, 2020.
- 11.Pineda R, Denevich S, Lee WC, Waycaster C, Pashos CL. Economic evaluation of toric intraocular lens: a short- and long-term decision analytic model. Arch Ophthalmol. 2010;128(7):834–840. doi: 10.1001/archophthalmol.2010.127 [DOI] [PubMed] [Google Scholar]
- 12.Lundstrom M, Dickman M, Henry Y, et al. Risk factors for refractive error after cataract surgery: analysis of 282 811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J Cataract Refract Surg. 2018;44(4):447–452. doi: 10.1016/j.jcrs.2018.01.031 [DOI] [PubMed] [Google Scholar]
- 13.Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. Formula choice: Hoffer Q, Holladay 1, or SRK/T and refractive outcomes in 8108 eyes after cataract surgery with biometry by partial coherence interferometry. J Cataract Refract Surg. 2011;37(1):63–71. doi: 10.1016/j.jcrs.2010.07.032 [DOI] [PubMed] [Google Scholar]
- 14.Wang L, Shirayama M, Ma XJ, Kohnen T, Koch DD. Optimizing intraocular lens power calculations in eyes with axial lengths above 25.0 mm. J Cataract Refract Surg. 2011;37(11):2018–2027. doi: 10.1016/j.jcrs.2011.05.042 [DOI] [PubMed] [Google Scholar]
- 15.Cionni RJ, Breen M, Hamilton C, Williams R. Retrospective analysis of an intraoperative aberrometry database: a study investigating absolute prediction in eyes implanted with low cylinder power toric intraocular lenses. Clin Ophthalmol. 2019;13:1485–1492. doi: 10.2147/OPTH.S191887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hill DC, Sudhakar S, Hill CS, et al. Intraoperative aberrometry versus preoperative biometry for intraocular lens power selection in axial myopia. J Cataract Refract Surg. 2017;43(4):505–510. doi: 10.1016/j.jcrs.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 17.Solomon KD, Sandoval HP, Potvin R. Evaluating the relative value of intraoperative aberrometry versus current formulas for toric IOL sphere, cylinder, and orientation planning. J Cataract Refract Surg. 2019;45(10):1430–1435. doi: 10.1016/j.jcrs.2019.05.023 [DOI] [PubMed] [Google Scholar]
- 18.Sudhakar S, Hill DC, King TS, et al. Intraoperative aberrometry versus preoperative biometry for intraocular lens power selection in short eyes. J Cataract Refract Surg. 2019;45(6):719–724. doi: 10.1016/j.jcrs.2018.12.016 [DOI] [PubMed] [Google Scholar]
- 19.Curado SX, Hida WT, Vilar CMC, Ordones VL, Chaves MAP, Tzelikis PF. Intraoperative aberrometry versus preoperative biometry for IOL power selection after radial keratotomy: a prospective study. J Refract Surg. 2019;35(10):656–661. doi: 10.3928/1081597X-20190913-01 [DOI] [PubMed] [Google Scholar]
- 20.Fram NR, Masket S, Wang L. Comparison of intraoperative aberrometry, OCT-based IOL formula, Haigis-L, and Masket formulae for IOL power calculation after laser vision correction. Ophthalmology. 2015;122(6):1096–1101. doi: 10.1016/j.ophtha.2015.01.027 [DOI] [PubMed] [Google Scholar]
- 21.Ianchulev T, Hoffer KJ, Yoo SH, et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology. 2014;121(1):56–60. doi: 10.1016/j.ophtha.2013.08.041 [DOI] [PubMed] [Google Scholar]