Abstract
Background
Fluoride varnish with therapeutic tricalcium phosphate formulas such as Clinpro™ varnish has shown greater tendency in treating white spot lesions (WSLs) by inhibiting the progression of initial enamel lesions through the mineral exchange. The self-assembling peptide SAP11-4 (Curodont Repair, CDR) works on a different scale in treating WSLs by mimicking the enamel matrix and aiming to guided enamel regeneration.
Aim
To quantitatively and qualitatively compare the effectiveness of the SAP11-4 vs tricalcium posphate fluoride (TCPF) in remineralization of WSLs in young permanent teeth.
Materials and methods
Nine healthy patients were enrolled in this study. The trial was performed on 40 young permanent teeth in the initial demineralization stage. Teeth were randomly assigned to receive either TCPF (group I) or SAP11-4 (group II). Lesions were assessed at pretreatment, 3, and 6 months posttreatment quantitatively per laser fluorescence DIAGNOdent pen and qualitatively through the International Caries Detection and Assessment System (ICDAS) II.
Results
The result of the current study revealed a significant quantitative and qualitative increase in remineralization of WSLs in both groups and over time intervals. However, the WSL recovery was significantly better in the self-assembling peptide group, reflecting an excellent remineralization potential of the WSLs by the SAP11-4 compared to TCPF varnish.
Conclusion
Both TCPF and SAP11-4 were effective in treating WSLs. However, the success of guided enamel regeneration by the SAP11-4 through the biomineralization has proven superiority of this material compared to TCPF.
Clinical significance
Early detection of WSLs and minimal intervention through remineralizing agents can limit unnecessary tissue loss, further caries progression, and consequently prevent further harm to the patients.
How to cite this article
Kobeissi R, Badr SBY, Osman E. Effectiveness of Self-assembling Peptide P11-4 Compared to Tricalcium Phosphate Fluoride Varnish in remineralization of White Spot Lesions: A Clinical Randomized Trial. Int J Clin Pediatr Dent 2020;13(5):451–456.
Keywords: Enamel regeneration, Remineralization, Self-assembling peptide, Tricalcium phosphate fluoride varnish, White spot lesion, Young permanent teeth
Introduction
White spot lesions (WSLs), the earliest evidence of enamel demineralization, are facing an alarming trend based on remineralization with a single goal of healing the precious enamel. In fact, there is a paradigm shift in caries management toward the minimally invasive approach.1 This approach is based on the development of methodologies for early caries detection, noninvasive treatment of these lesions, and preventing their progression with important consequence on esthetic and function regression.2 At earlier stages, these WSLs are amenable to remineralization or arrest. Eventually, if the demineralization process continues, the intact enamel surface will collapse and cavitate. Although saliva can remineralize WSLs to some extent, this natural mechanism is slow and rarely heals the lesions completely, which is why external factors are a prerequisite for the remineralization process.3
Accurate diagnosis and early detection of WSLs is of paramount importance and is the cornerstone of the remineralization process success, as it allows proper preventive measure implementation and control on the lesion progression. Among these devices, DIAGNOdent pen can provide an objective and reliable method to assess the presence of WSLs. Considering the reported sensitivity and specificity in different studies, it has been proved that it is relevant for early caries detection.4
Fluoride-based strategies are the gold standard for prevention and management of WSLs.5 Fluoride can interact with saliva on the enamel surface and subsurface and combine with phosphate and calcium ions to form new and large crystals that contain more fluoride (Fluor-hydroxyapatite) that enhance remineralization.6 Novel fluoride varnish with therapeutic tricalcium phosphate formulas such as Clinpro™ varnish (5%) has shown the greater tendency in treating WSLs by inhibiting the progression of primary enamel lesions.7
Recently, a new material had been introduced to promote the enamel remineralization SAP11-4 (Curodont Repair, CDR) through guided enamel regeneration to mimic the natural enamel matrix formation by biomineralization at a nanometer scale.
In vitro studies concerning the effect of SAP11-4 on artificially induced lesions on smooth enamel surfaces has advantaged the remineralizing potency of this product.8 However, there is a deficiency of research conducted on this product in vivo, especially on young permanent teeth. Therefore, this in vivo study was conducted to quantitatively and qualitatively compare the effectiveness of the SAP11-4 vs tricalcium phosphate fluoride varnish in remineralization of WSLs in young permanent teeth. It is hypothesized that none of the tested materials has more potential in remineralizing WSLs than the other.
Materials and Methods
This study is a randomized controlled clinical trial with allocation ratio of 1 to 1 with no changes in the methods after trial commencement. Ethical approval for the study was obtained before performing the study from the scientific and ethical review committee and institutional review board IRB at Beirut Arab University (BAU IRB code: 2016H-0041-D-M-0156). This study was conducted at Beirut Arab University dental clinics.
Sample Size and Participants Enrolment
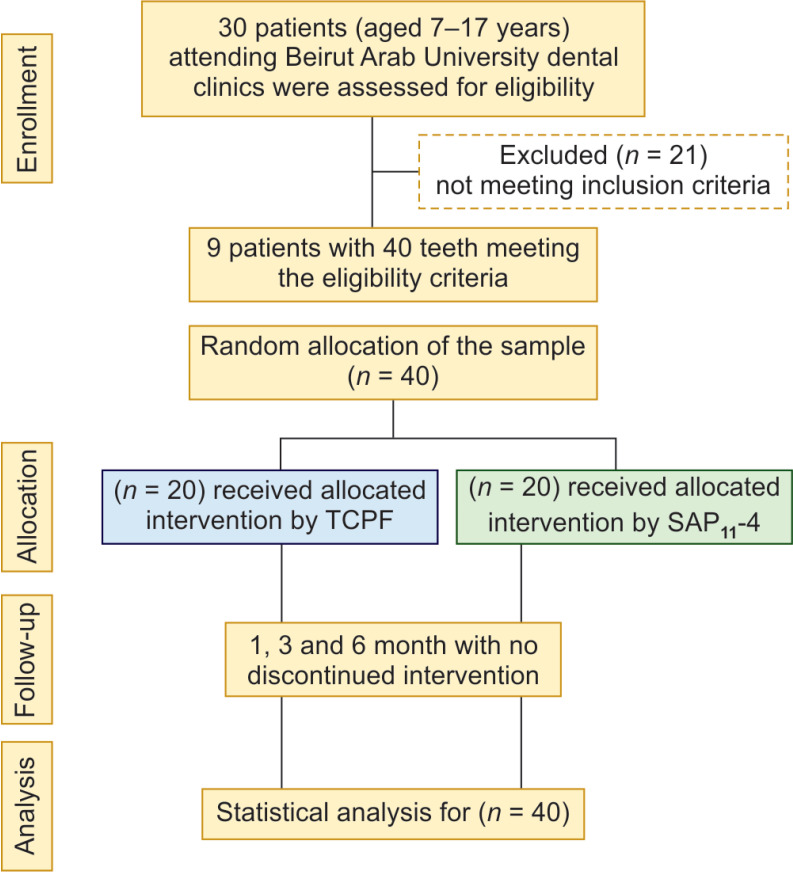
The sample size was calculated through a free online calculator (www.sample-size.net), where a sample size of 40 young permanent teeth was determined to establish a true level of significance of 5% with 95% level of confidence and was estimated as adequate to produce statistically significant results at less than 0.05. Moreover, this sample size was similar to other previously published studies.8–10 Nine healthy patients (5 girls and 4 boys), aged 7 to 17 years, were enrolled in this study. The eligibility criteria were based on accessible WSL on the buccal or labial surfaces of their young permanent teeth with a DIAGNOdent pen reading <24 and International Caries Detection and Assessment System (ICDAS) II code ranging between 1 and 3, denoting initial demineralization in addition to the absence of caries, restoration, and cavitation on the surfaces to be treated. Patient allocation through the trial is presented in the consort flow diagram (Flowchart 1). Written consent was obtained from all patients or their legal guardian after a detailed explanation of the procedure, its benefits, and any possible discomfort. Contralateral teeth in patients fulfilling the inclusion criteria were assigned randomly to either the TCPF (Clinpro™ White Varnish) or the SAP11-4 containing product (CURODONT REPAIR) using simple randomization by a flip of a coin which is the most straightforward method for the patient's allocation.11 This simple random allocation was done by a third-party, the assignment of the patient teeth to either group I or group II was determined though sequentially numbered opaque sealed envelopes. The study was single blinded such that the patient was blind to what material was used.
Flowchart 1.
Flowchart showing patient allocation
Procedures
Group I consisted of 20 WSLs on young permanent teeth treated with TCPF (Clinpro™ White Varnish), whereas group II consisted of 20 WSLS on young permanent teeth treated with SAP11-4 (curodont repair). For all patients, oral prophylaxis was performed followed by isolation of tooth or teeth in concern with a conventional or light-cured rubber dam followed by drying with an air–water syringe, since any moisture contamination can cause light deflection during lesions assessment. Furthermore, oral hygiene instructions and diet counseling were given at the first visit and routinely checked during the follow-up.
In the group I, the TCPF was prepared by dispensing the entire content of 1-unit dose package of the varnish onto the dosage guide followed by thorough mixing with the brush provided. The varnish was then applied by even distribution by the applicator brush.
In group II, the SAP 11-4 was carefully prepared by adding 0.05 mL of distilled water to the Curodont vial by a syringe. The next step was the aspiration of the material from the vial. Before the application of the material, tooth Pellicle was removed by conditioning of the surface to be treated by 5% sodium hypochlorite for 20 seconds followed by rinsing and drying the tooth. The tooth was then etched with 37% phosphoric acid for 20 seconds to remove the inorganic materials and open the microspores into the subsurface cavity to achieve successful treatment with Curodont. After thorough rinsing with water for 20 seconds and air drying of the lesion, one drop of the material was placed on the surface of the tooth using a special syringe. Moisture control was maintained for approximately 5 minutes until the SAP11-4 solution is no longer visible.
WSLs were first assessed by using ICDAS II codes to determine the severity of the lesion at pretreatment, 1 month, 3 months, and 6 months, respectively. The scoring criteria of the ICDAS-II system for Coronal Smooth Surface Caries are coded from 0 to 6 according to the following table (Table 1).12
Table 1.
The scoring criteria of the ICDAS-II system for coronal smooth surface caries
| 0 | Sound tooth surface |
| 1 | Enamel first visual change |
| 2 | Enamel distinct visual change |
| 3 | Enamel initial breakdown |
| 4 | Underlying dark shadow from dentin |
| 5 | Distinct cavity with visible dentin |
| 6 | Extensive distinct cavity |
Lesions were then assessed with the DIAGNOdent pen that was calibrated against its ceramic disk before each reading. It was also mandatory to individually adjust the 0 point of the DIAGNOdent pen to each patient to overcome the difference in the level of fluorescence of the teeth among patients. The change in codes qualitatively determined the effect of the remineralizing material (TCP fluoride varnish and self-assembling peptide P11-4) on the WSLs at the different time interval, whereas the change of DIAGNOdent pen readings quantitatively determined this effect. There were no allergic reactions, medical complications, or adverse events related to the treatments during treatment and follow-up.
Outcomes
The primary outcome was remineralization of WSLs as reflected by the decrease in DIAGNOdent pen readings and the decrease in ICDASII codes of these lesions with its effect on the esthetic appearance and patient compliance. The secondary outcome was the correlation between ICDASII score and DIAGNOdent pen readings.
Statistical Analysis
The data were statistically analyzed on a computer using the SPSS for Windows (Chicago, IL, USA, version 22.0). The level of significance was set at p value ≤ 0.05. Descriptive statistics were used. Data were explored for normality using Kolmogorov–Smirnov tests. The results of this test indicated that most of the data were not normally distributed, so non-parametric tests were therefore accomplished for the qualitative and quantitative assessments. For the qualitative assessment Friedman test was performed to assess the change in ICDAS II code over time for each remineralization material. For the quantitative assessment, Friedman test followed by Wilcoxon signed rank tests were performed to compare DIAGNOdent pen readings within groups for each remineralization material. A percentage variation for DIAGNOdent pen readings according to pretreatment period was calculated for each tooth in each group according to the formula: [(reading at pre-treatment − reading at follow-up)/reading at pretreatment] × 100 Student t tests were then performed to compare DIAGNOdent pen readings variations between groups. The correlation between ICDAS II Codes and DIAGNOdent pen readings was investigated by Spearman correlation test.
Results
Study Subjects
Nine children (5 girls 55.55%, four boys 45.45%) with a mean age of 11.11 ± 3.8.years, were enrolled with no patient withdrawal.
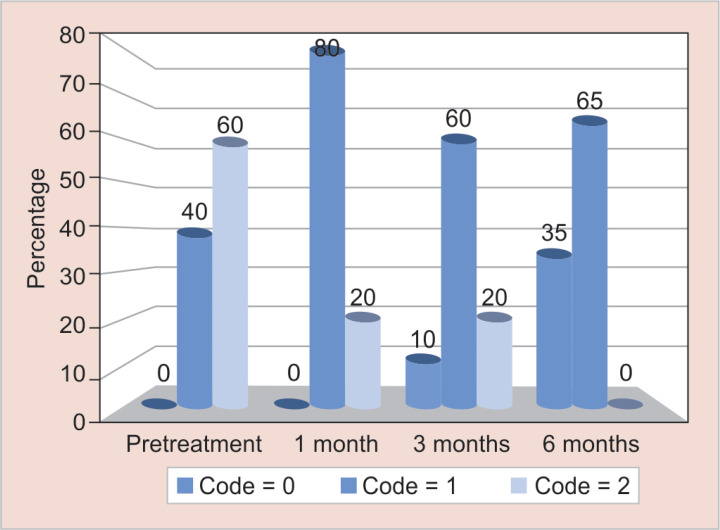
Qualitative Assessment Using International Caries Detection and Assessment System II Codes for WSLs Treated with TCPF
The results of the current study showed that the ICDAS II codes for teeth treated with TCPF varnish decreased significantly over time (p value < 0.001; Friedman test).The overall percentages of codes of WSLs at pretreatment, 1, 3, and 6 months post-treatment are presented in Figure 1.
Fig. 1.
Percentage of ICDAS II codes over time for WSLs treated with TCP fluoride varnish
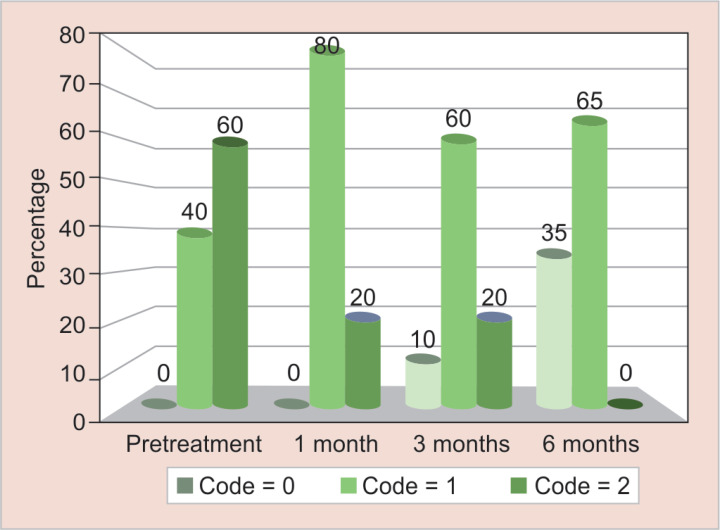
Qualitative Assessment Using ICDAS II Codes for WSLs Treated with SAP11-4
The results of the current study showed that the ICDAS II codes for teeth treated with self-assembling peptide significantly decreased over time time (p value < 0.001; Friedman test). The overall percentages of codes of WSLs at pretreatment, 1, 3, and 6 months post-treatment are presented in Figure 2.
Fig. 2.
Percentage of ICDAS II codes over time for WSLs treated with self-assembling peptide
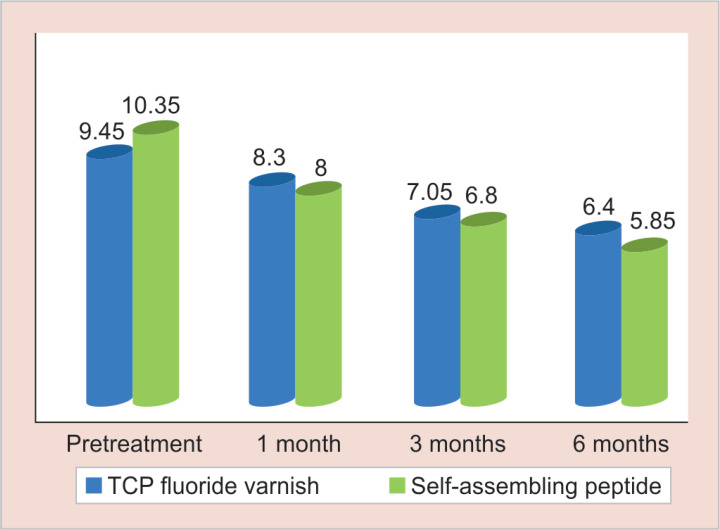
Quantitative Assessment of WSLs Using DIAGNOdent Pen
Mean and standard deviation of the DIAGNOdent pen readings for different remineralization materials showed that there was a diminution in the mean values of both groups over time (Fig. 3).
Fig. 3.
Mean DIAGNOdent pen readings in both groups over time
Statistical analysis showed a significant decrease in the DIAGNOdent pen readings over time for both TCPF and SAP11-4 groups (p value < 0.001; Friedman test). The readings decreased significantly between pretreatment and 1 month (p value < 0.001; Wilcoxon test), between 1 and 3 months (p value < 0.001; Wilcoxon test), and between 3 and 6 months (p value = 0.011; Wilcoxon test). Thus, remineralization in both groups significantly increased over time.
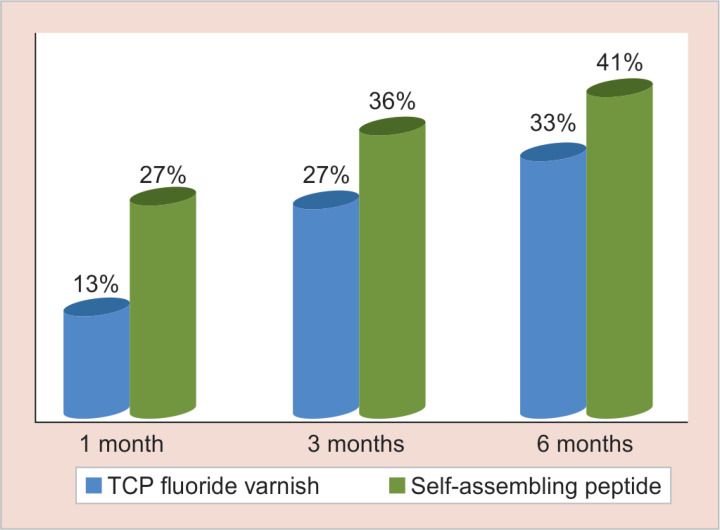
Comparison of the DIAGNOdent Pen Readings Variation Percentages in Both Groups Over Time
The mean variation in DIAGNOdent pen readings according to pretreatment was calculated for each tooth in both groups. The results showed that 1 month after application of the remineralization material, a significant difference was found in SAP11-4 group over TCPF group (p value = 0.004; Student t test), where the mean variation percentages were 12.97 ± 8.79% and 26.68 ± 12.19% for TCPF varnish and SAP11-4, respectively
Three months after material application, a significant difference was found in SAP11-4 group over TCPF group (p value = 0.014; Student t-test), where the mean variation percentages were 26.51 ± 1 0.83% and 36.11 ± 15.68% for TCPF and SAP11-4, respectively. Six months after application, a significant difference was found in SAP11-4 group over TCPF group (p value = 0.0124; Student t-test), where the mean variation percentages were 32.72 ± 7.84% and 41.39 ± 16.73% for TCPF and SAP11-4, respectively (Fig. 4).
Fig. 4.
Comparison of the DIAGNOdent pen readings variation percentages
Further investigation was performed to confirm the correlation between ICDAS-II codes with the DIAGNOdent pen readings. This correlation was measured based on the chance for the DIAGNOdent pen to agree with ICDAS-II for diagnosing different scores of WSL. By normal standards, the association between the two variables was statistically significant (R = 0.8405, Spearman's correlation test) and the 2-tailed p value was 0.0001.
Discussion
The emphasis on the management of noncavitated lesions is perceived since the early 1900s.13 However, dental caries is commonly detected after cavity formation, and its management has focused mainly on operative protocols. In consequence, considerable efforts are recently undertaken to perceive a noninvasive treatment solution for dental caries from its earliest clinical sign, which is WSL on enamel surface. Decades of research has led to the advancement of technologies that can promote enamel remineralization or decrease demineralization of WSLs. These advancements have created an essential shift from monitoring lesion appearance and progress which would probably end up by placement of restoration to nonsurgical intervention in order to promote the biomineralization of the carious defect and its regeneration at the WSL stage, thus removing the wait and see concept from our daily practice.
Fluoride is the gold standard in remineralization strategies it acts by modifying the bacterial metabolism in dental plaque, thus reducing demineralization and favoring the remineralization of WSLs. However, the fluoride mechanism of action is only within reach of few μm into enamel.14 Fluoride-containing products promote the remineralization and make the enamel surface more acid resistant. Novel fluoride varnish with therapeutic tricalcium phosphate formulas such as Clinpro™ varnish (5%) has shown the greater tendency in treating WSLs by inhibiting the progression of initial primary enamel lesions. This product has an excellent resistance for the acid challenge due to the formation of a protective barrier around calcium ions during the manufacturing process, and once the varnish flows on tooth enamel and contact the saliva, this barrier is broken making fluoride phosphate and calcium ions free to enhance the remineralization potential.15 The SAP11-4 differs from fluoride by its ability to diffuse deeply into the subsurface body of WSLs, where it forms a three-dimensional matrix. The patient saliva can act as a reservoir of Ca2+ and PO43− ions that can attach to the matrix and induce de novo formation of hydroxyapatite crystals (HA)16 in contrast to fluoride who acts superficially,17 the SAP11-4 can regenerate lost crystal structures in the depth of enamel lesion.
The present study aims to compare the effectiveness of self-assembling peptide P11-4 based on guided enamel regeneration to fluoride varnish in remineralization of WSLs in young permanent teeth. Simple randomization has ensured comparable group's production and elimination of accidental bias. Quantitative assessment of WSLs was performed by the DIAGNOdent pen. The absence of harmful radiation is one of the crucial benefits of the DIAGNOdent pen in addition to its specificity, sensitivity, and easy manipulation. It is a portable, compact, and user-friendly device, and it delivers laser light that the tooth can absorb and reflect as infrared fluorescence that can be quantified numerically to measure the difference between the fluorescence of healthy and carious dental tissue and gives each tissue a different score thus, reducing human error.18
Qualitative assessment of WSL was done using ICDAS-II for dental caries scoring. The ICDAS-II is an easy chairside examination method listed in the FDI's Chairside Guide that can provide a robust system for ranking dental caries. The ICDAS-II encourages preventative strategies that enable remineralization of noncavitated lesions and promote tooth structure preservation. It is undoubtedly leading to a paradigm shift in the concept of recording both the cavitated and the non-cavitated lesions by eliminating the use of sharp explorer for caries detection, as it may damage the intact enamel covering the early demineralized lesion.19 The result of the current study revealed that there was a significant quantitative and qualitative increase in remineralization of WSLs in both groups and over time intervals. Clinical applicability of both treatments was regarded as satisfactory, and patients were interested in receiving noninvasive caries treatments. However, this WSL recovery was significantly better in the self-assembling peptide group, reflecting a superior remineralization potential of compared to TCPF varnish. This could be attributed to the ability of the peptide as the self-assembling peptides undergo self-assembly into three-dimensional fibrillary scaffolds in response to specific environmental triggers as was discussed by a review performed by Kyle et al. who focused on the ability of self-assembling peptide-based biomaterials to be used as 3D tissue engineering scaffolds.20
Moreover, many in vitro researches showed the efficacy of the SAP11-4.8,21–23 Jablonski-Momeni et al. evaluated the efficacy of SAP11-4 by applying it on artificially demineralized smooth surfaces of extracted human posterior teeth, the lesions evaluation was performed by DIAGNOdent and Vista proof.8 Similarly, Silvertown et al. assessed the effect of the SAP11-4 in healing WSLs through the Canary System.21 The results of those two studies have confirmed the high remineralizing potential of P11-4.8,21 Other researches compared the remineralizing potential of SAP11-4 to other available remineralizing agents. In the study performed by Saves et al., SAP11-4 (Curodont Repair) was compared to other five groups: acidulated phosphate fluoride (APF), silver diamine fluoride (SDF), ammonium hexafluorosilicate (SiF), SiF plus cetylpyridinium chloride (SiF+CPC), and a control group. After demineralization and remineralization procedures, microhardness test (VHN), energy-dispersive X-ray spectroscopy analysis, and confocal laser scanning microscopy evaluation were done.22 Besides, Soares et al. also compared SAP11-4 (Curodont Repair) with other remineralizing agents: casein phosphopeptide-amorphous calcium phosphate fluoride (CPP ACPF), bioactive glass (BAG), fluoride enhanced hydroxyapatite (HA) gel, and SAP11-4. Remineralization of artificial carious lesions in enamel was assessed in vitro after a 30-day pH cycling model using SEM and surface microhardness analysis.23 The data in those two studies proved that Curodont repair which contains SAP11-4 has a more significant remineralizing potential among all materials tested.22,23
Contrary to the results of the current study, Wierichs et al. and Golland et al. when assessing the potential of SAP11-4 for enhancing remineralization of WSLs in vitro on bovine enamel found that self-assembling peptide could neither inhibit lesion progression nor promote remineralization.24,25 The reason behind this could be attributed to the use of bovine enamel instead of human enamel. In fact, it is mentioned in the literature that for studies requiring a determination of both demineralization and remineralization, human enamel, or dentin with a softened caries-like should be the substrates of choice.26
Only a few in vivo studies on SAP11-4 have highlighted the enamel regeneration capacity of this product; moreover, there is lack of studies that has compared the effect of SAP11-4 to TCPF varnish. The first in-man clinical safety study was conducted by Brunton et al. This trial was based on applying a single treatment of P11-4 to Class V enamel lesions in healthy human volunteers followed by the recording of the adverse events and lesion appearances over 180 days. The outcomes have assured that treatment of early caries lesions with SAP11-4 was successful and that a single application can be useful in enamel recovery.27 Another one was a randomized controlled study performed by Alkilzy et al. on WSLs of erupting permanent molars. In that study, subjects were assigned to two groups: the test group (SAP11-4 + fluoride varnish) and the control group (fluoride varnish alone), and similar to our study caries assessment was at baseline and 3 and 6 months post treatment quantitatively by DIAGNOdent pen and quantitatively by a visual analog scale ICDAS. The results of that study proved a significant capacity of SAP11-4 in regenerating enamel tissue and preventing lesion progression.28
The efficacy of TCP is frequently discussed.15,29,30 Alamoudi et al. emphasized the importance of adding TCP to fluoride varnish to enhance its protective ability through his in vitro study.29 Likewise, Rirattanapong et al., in 2014, performed a clinical in vitro study which has shown that fluoride varnish containing tricalcium phosphate has a high remineralization effect and can inhibit progression of WSLs.15 Elkassas and Arafa found that new therapeutic techniques containing calcium phosphate formulas with fluoride provide can be considered a new avenue for and early carious lesions remineralization.30
Concerning the qualitative and quantitative assessment correlations, the results of the current study showed high association between them. Almosaa et al. clinically evaluated the correlation between the ICDAS-II index and the DIAGNOdent pen.31 Chalas et al. clinically evaluated the concordance of measurement obtained from ICDAS index, Carie Scan PRO, and the DIAGNOdent pen in detecting caries in the occlusal grooves of molars and premolars.31 The statistical analysis of those studies showed similar results to the current study, which is a high association between the DIAGNOdent pen device and the ICDAS index.31,32
Conclusion
Within the limitation of the current study, it is concluded that both TCPF and SAP11-4 were effective in the treatment of WSLs. SAP11-4 showed superiority due to its guided enamel regeneration potential that will undoubtedly open the doors to a new concept in enamel healing. However, when weighing advantages vs disadvantages of both products, TCPF is an excellent candidate for many reasons, especially its simplicity, cost, and its single step of application. The SAP11-4 application needed many steps, including the meticulous material preparation within the vial in addition to tooth lesion preparation through its conditioning and etching. Therefore, despite the relatively significant difference in the results of the DIAGNOdent pen readings, the characteristics of TCPF in addition to its ability to achieve significant remineralization make it a very reliable choice in our daily practice.
Recommendations
Further research can be done to test the success of enamel regeneration by SAP11-4 not only in initial caries but also in more advanced lesions. Practitioners should concentrate on early detection and early remineralization of WSls and consider guided enamel regeneration.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Swamy DF, Barretto E, Mallikarjun SB, et al. In vitro evaluation of resin infiltrant penetration into white spot lesions of deciduous molars. J Clin Diagn Res. 2017;11(9):ZC71–ZC74. doi: 10.7860/JCDR/2017/28146.10599. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta R, Nandlal B, Prashanth S. Comparative evaluation of remineralization potential of casein phosphopeptide-amorphous calcium phosphate and casein phosphopeptide-amorphous calcium phosphate fluoride on artificial enamel white spot lesion: an in vitro light fluorescence study. Indian J Dent Res. 2013;24(6):681–689. doi: 10.4103/0970-9290.127610. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Neeraj G, Inder KP, Monika G, et al. Caries infiltration of non cavitated white spot lesions: a novel approach for immediate esthetic improvement. Contemp Clin Dent. 2012;3(2):S199–S202. doi: 10.4103/0976-237X.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nokhbatolfoghahaie H, Alikhasi M, Chiniforush N, et al. Evaluation of accuracy of DIAGNOdent in diagnosis of primary and secondary caries in comparison to conventional methods. J Lasers Med Sci. 2013;4(4):159–167. [PMC free article] [PubMed] [Google Scholar]
- 5.Fontana M. Enhancing fluoride: clinical human studies of alternatives or boosters for caries management. Caries Res. 2016;50(1):22–37. doi: 10.1159/000439059. DOI: [DOI] [PubMed] [Google Scholar]
- 6.Lata S, Varghese NO, Varughese JM. Remineralization potential of fluoride and amorphous calcium phosphate-casein phosphopeptide on enamel lesions: an in vitro comparative evaluation. J Conserv Dent. 2010;13(1):42–46. doi: 10.4103/0972-0707.62634. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rirattanapong P, Vongsavan K, Saengsirinavin C, et al. Enhancing remineralization of primary enamel lesions with fluoride dentifrice containing tricalcium phosphate. Southeast Asian J Trop Med Public Health. 2017;48(2):494–500. [PubMed] [Google Scholar]
- 8.Jablonski-Momeni A, Heinzel-Gutenbrunner M. Efficacy of the self-assembling peptide P11-4 in constructing a remineralization scaffold on artificially-induced enamel lesions on smooth surfaces. Orofac Orthop. 2014;75(3):175–190. doi: 10.1007/s00056-014-0211-2. DOI: [DOI] [PubMed] [Google Scholar]
- 9.Ferrazzano GF, Amato I, Cantile T, et al. In vivo remineralizing effect of GC tooth mousse on early dental enamel lesions: SEM analysis. Int Dent J. 2011;61(4):210–216. doi: 10.1111/j.1875-595X.2011.00059.x. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metwally NI, Niazy MA, El-Malt MA. Remineralization of early carious lesions using biomimetic self-assembling peptides versus fluoride agent (in vitro and in vivo study). ADJ-for Girls. 2017;4(2):179–188. doi: 10.21608/adjg.2017.5226. DOI: [DOI] [Google Scholar]
- 11.Kao LS, Tyson JE, Blakely ML, et al. Clinical research methodology I: introduction to randomized trials. J Am Coll Surg. 2008;206(2):361–369. doi: 10.1016/j.jamcollsurg.2007.10.003. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sagarika N, Suchindran S, Loganathan SC. Velayutham Gopikrishna prevalence of white spot lesion in a section of Indian population undergoing fixed orthodontic treatment: an in vivo assessment using the visual international caries detection and assessment system II criteria. J Conserv Dent. 2012;15(2):104–108. doi: 10.4103/0972-0707.94572. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juliana. G. Detection and diagnosis of the early caries lesion. BMC Oral Health. 2015;15(1):S3. doi: 10.1186/1472-6831-15-3. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marinho VC, Higgins JP, Sheiham A, et al. Fluoride toothpaste for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;(1):CD002278. doi: 10.1002/14651858.CD002278. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rirattanapong P, Vongsavan K, Saengsirinavin C, et al. Effect of fluoride varnishes containing tri-calcium phosphate sources on remineralization of initial primary enamel lesions. Southeast Asian J Trop Med Public Health. 2014;45(2):499–504. [PubMed] [Google Scholar]
- 16.Aggeli A, Bell M, Carrick LM, et al. PH as a trigger of peptide beta-sheet self-assembly and reversible switching between nematic and isotropic phases. J Am Chem Soc. 2003;125(32):9619–9628. doi: 10.1021/ja021047i. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Lussi A, Hellwig E, Klimek J. Fluorides - mode of action and recommendations for use. Schweiz Monatsschr Zahnmed. 2012;122(11):1030–1042. [PubMed] [Google Scholar]
- 18.Vali Sichani A, Javadinjad S, Ghafari R. Diagnostic value of DIAGNOdent in detecting caries under composite restorations of primary molars. Dent Res J (Isfahan) 2016;13(4):327–332. doi: 10.4103/1735-3327.187874. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gugnani N, Pandit I, Srivastava N, et al. International caries detection and assessment system (ICDAS): a new concept. Int J Clin Pediat Dent. 2011;4(2):93–100. doi: 10.5005/jp-journals-10005-1089. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kyle Stuart,, Amalia A, Eileen I, et al. Production of self-assembling biomaterials for tissue engineering trends. Biotechnol. 2009;27(7):423–433. doi: 10.1016/j.tibtech.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silvertown JD, Wong BP, Sivagurunathan KS, et al. Remineralization of natural early caries lesions in vitro by P11-4 monitored with photothermal radiometry and luminescence. J Investig Clin Dent. 2017;8(4) doi: 10.1111/jicd.12257. DOI: [DOI] [PubMed] [Google Scholar]
- 22.Savas S, Kucukyilmaz E, Celik EU. Effects of remineralization agents on artificial carious lesions. Pediatr Dent. 2016;38(7):511–518. [PubMed] [Google Scholar]
- 23.Soares R, Noronha De Ataide ID, Fernandes M, et al. Assessment of enamel remineralisation after treatment with four different remineralising agents: a scanning electron microscopy (SEM) study. J Clin Diagn Res. 2017;11(4):ZC136–ZC141. doi: 10.7860/JCDR/2017/23594.9758. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wierichs RJ, Kogel J, Lausch J, et al. Effects of self-assembling peptide P11-4, fluorides, and caries infiltration on artificial enamel caries lesions in vitro. Caries Res. 2017;51(5):451–459. doi: 10.1159/000477215. DOI: [DOI] [PubMed] [Google Scholar]
- 25.Golland L, Schmidlin PR, Schätzle M. The potential of self-assembling peptides for enhancement of in vitro remineralisation of white spot lesions as measured by quantitative laser fluorescence. Oral Health Prev Dent. 2017;15(2):147–152. doi: 10.3290/j.ohpd.a37931. DOI: [DOI] [PubMed] [Google Scholar]
- 26.Milberg JR. Hard-tissue substrates for evaluation of cariogenic and anti-cariogenic activity in situ. J Dent Res. 1992;71(3_suppl):913–919. doi: 10.1177/002203459207100S25. DOI: [DOI] [PubMed] [Google Scholar]
- 27.Brunton PA, Davies RP, Burke JL, et al. Treatment of early caries lesions using biomimetic self-assembling peptides–a clinical safety trial. Br Dent J. 2013;215(4):E6. doi: 10.1038/sj.bdj.2013.741. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alkilzy M, Tarabaih A, Santamaria RM, et al. Self-assembling peptide P11-4 and fluoride for regenerating enamel. J Dent Res. 2018;97(2):148–154. doi: 10.1177/0022034517730531. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alamoudi SA, Pani SC, Alomari M. The effect of the addition of tricalcium phosphate to 5% sodium fluoride varnishes on the microhardness of enamel of primary teeth. Int J Dent. 2013;2013:486358. doi: 10.1155/2013/486358. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elkassas D, Arafa A. Remineralizing efficacy of different calcium-phosphate and fluoride based delivery vehicles on artificial caries like enamel lesions. J Dent. 2014;42(4):466–474. doi: 10.1016/j.jdent.2013.12.017. DOI: [DOI] [PubMed] [Google Scholar]
- 31.Almosaa NA, Lundgrenb T, Aldreesc AM, et al. Diagnosing the severity of buccal caries lesions in governmental and private orthodontic patients at debonding, using the ICDAS-II and the DIAGNOdent pen. Angle Orthod. 2014;84(3):430–436. doi: 10.2319/051313-371.1. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chalas R, Wojcik-Checinska I, Zubrzycka-Wrobel J, et al. Comparison of visual, impedance spectroscopy and laser fluorescence methods in detecting early carious lesions on occlusal surfaces. Curr Iss Pharm Med Sci. 2014;27(2):102–104. doi: 10.2478/cipms-2014-0023. DOI: [DOI] [Google Scholar]