Abstract
The severe respiratory illness due to SARS-CoV-2, the virus responsible for coronavirus disease 2019 (COVID-19), is triggered by an intense pro-inflammatory host response. Statins, prescribed primarily for lipid reduction, are known to have anti-inflammatory and immunomodulatory properties and have been associated with a reduced mortality rate among COVID-19 patients taking statins as reported in two recent retrospective studies. However, a meta-analysis that included nine studies showed that statin use did not improve in-hospital outcomes of those with COVID-19. In addition, concerns regarding the use of statins and an increase in COVID-19 infections have been raised, as statins may increase the expression of angiotensin-converting enzyme 2 (ACE2), the primary receptor for the SARS-CoV-2 virus. Our goal was to investigate the effect of statins in COVID-19 patients in a large, diverse patient population across the United States containing nearly 120,000 patients diagnosed with COVID-19. We used propensity score matching of demographics, comorbidities, and medication indication to compare statin-treated patients (N = 2,297) with matched controls (N = 4,594). We observed a small, but statistically significant, decrease in mortality among patients prescribed statins (16.1%) when compared with matched COVID-19-positive controls (18.0 to 20.6%). These results support previous evidence that statins do not increase COVID-19-related mortality and may, in fact, have a mitigating effect on severity of the disease reflected in a slight reduction in mortality. Mixed findings on effects of statins in COVID-19 patients reported in the literature should prompt prospective randomized controlled trials in order to define better who might be advantaged with respect to clinical outcomes.
Keywords: SARS-CoV-2, COVID-19, statins, electronic health records, inflammatory response, oxidative stress, mortality rate
Introduction
In less than a year since its outbreak, the coronavirus disease 2019 (COVID-19) pandemic has taken over one million lives to date (1). The severity of COVID-19 symptoms in patients is strongly associated with being older and having pre-existing medical conditions (2). The severe respiratory illness of COVID-19 is primarily triggered by an intense pro-inflammatory host response (3). Statins—medications routinely prescribed for cholesterol and lipid lowering—are also known to have anti-inflammatory and immunomodulatory properties, capable of reducing inflammatory responses and oxidative stress (4–6). Furthermore, several observational studies have indicated that statin use may be effective in reducing mortality and hospitalization due to viral infections, such as influenza (7–9). Statins have also been shown to be beneficial for patients with various autoimmune inflammatory conditions (5) via several pathways.
The potential capability of statins to reduce the severity of COVID-10 outcomes has been investigated recently in several retrospective studies. Specifically, in a study of 13,981 COVID-19 patients in Hubei Province, China (10) and in a smaller study of 154 elderly patients in nursing home residents in Belgium (11), the use of statins was associated with a reduced mortality rate. However, a meta-analysis that included nine studies (for a total of 3,449 patients) showed that statin use did not improve in-hospital outcomes of those with COVID-19 (12). Furthermore, an increased mortality rate was observed among COVID-19 patients with Type-2 diabetes taking statins (13). In addition, concerns regarding the use of statins and an increase in COVID-19 infections have been raised, as statins can increase the expression of angiotensin-converting enzyme 2 (ACE2), the primary receptor for the SARS-CoV-2 virus (14). Electronic health records (EHR) provide an opportunity to study therapeutic effects on a population level. Our goal was to leverage data from electronic health records covering a comprehensive population of nearly 120,000 COVID-19 patients to investigate the potential effects of statin use in COVID-19 patients in a large, diverse population in the United States.
Methods
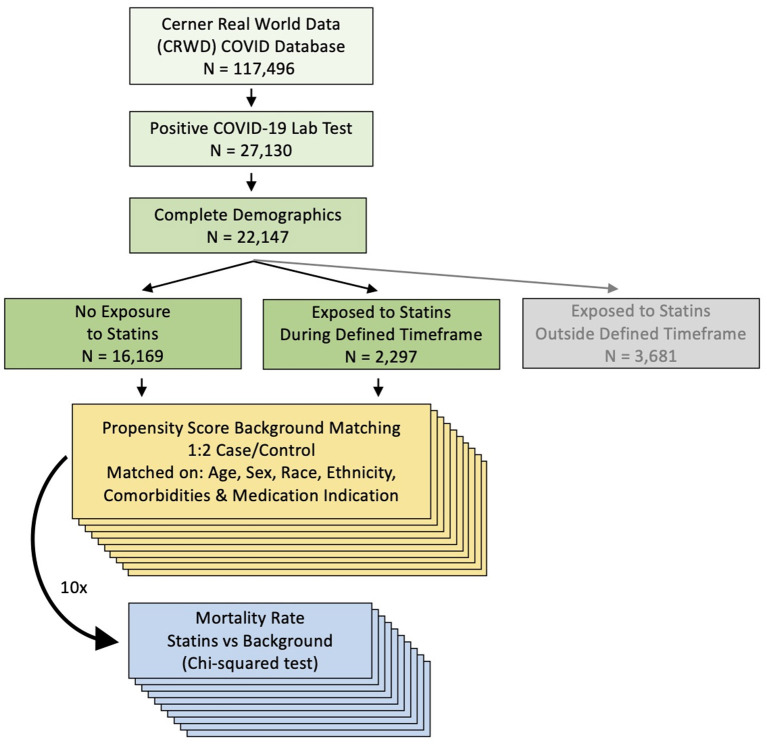
Data were obtained and analyzed from Cerner's large COVID-19 EHR database, which contains records of 117,496 COVID-19 patients across 62 healthcare centers as of July 2020. Deidentified Cerner Real-World Data is extracted from the EHR of hospitals in which Cerner has a data use agreement. Encounters include admissions, clinical and microbiology laboratory, pharmacy (medication orders and dispensing), and billing information, which are all date and time stamped, providing a temporal relationship between treatment patterns and clinical information. All patients had an emergency room visit or were hospitalized. Only patients with a COVID-19 diagnosis confirmed by a laboratory test for SARS-CoV-2 (including nucleic acid amplification tests and immunoassays) and with known values for demographics (age at encounter, sex, race and ethnicity) between February 2020 and July 2020 were included in analyses. Among 27,130 patients with a positive lab test, 22,147 had complete demographic information (Figure 1). COVID-19 patients with a medication order for a statin with an order status “active” or “completed” and without a designation of “as needed” (i.e., medication taken only when needed) at least once within a period of 10 days before and seven days after testing positive for COVID-19, were compared with COVID-19 patients who have no medication orders for statins. Individuals who were exposed to statins outside of this period of 10 days before and 7 days after testing positive for COVID-19 were excluded from our analysis (N = 3,681), resulting in total of N = 18,466 patients in the final cohort (Figure 1). If there was more than one positive laboratory test for COVID-19 for an individual, then the date of the first positive test was used. The following statins were included: atorvastatin (Lipitor), cerivastatin (Baycol), fluvastatin (Lescol), lovastatin (Mevacor), pitavastatin (Zypitamag, Livalo or Nikita), pravastatin (Pravachol), rosuvastatin (Ezallor or Crestor), simvastatin (FloLipid or Zocor). Considered comorbidities, identified by using International Classification of Diseases, 9th and 10th Revision, Clinical Modification (ICD-9/10) diagnosis codes, included hypertension (I10, I11, I12, I13, I15, I16, 401-405), diabetes (O24, E11, E10, E13, 250), COPD (J44, 491.2, 493.2, 496), obesity/high BMI (E66, 278, Z68.25, Z68.26, Z68.27, Z68.28, Z68.29, Z68.3X, Z68.4, V85.2, V85.3, V85.4), high cholesterol/hyperlipidemia (E78.0, E78.1, E78.2, E78.3, E78.4, E78.5, 272, 277), and atherosclerotic cardiovascular disease (I20, I21, I22, I23, I24, I25, 410-414, I63, I64, I65, I66, I69.3, 437.0, 437.1, G45.9, 433-435, 435.9). Body Mass Index (BMI) values were identified by Logical Observation Identifiers Names and Codes (LOINC) code 39156-5.
Figure 1.
Flow chart of the patient inclusion and the method.
Statistical Analysis
Propensity score matching (PSM) (15) with a nearest neighbor method and a 1:2 ratio was used to match statin-treated patients with controls. The R Matchit package was used for the analysis (16). Three PSMs were performed. The first matching was based on demographics (age, sex, ethnicity, race). The second matching was based on demographics and on comorbidities [hypertension, diabetes, obesity/high BMI, chronic obstructive pulmonary disease (COPD)]. The third matching included—in addition to all variables from the first two matchings—indications for a statin prescription (e.g., high cholesterol, hyperlipidemia, atherosclerotic cardiovascular disease). Welch two-sample two-sided t-test was performed to evaluate if there was a significant difference in the mean age when comparing the statin-treated group and the untreated group. Two-sample two-sided Mann–Whitney U test with continuity correction was performed to evaluate if there was a significant difference in BMI when comparing the statin-treated and untreated group. Pearson's Chi-squared test with Yates' continuity correction was performed to examine the association between statin use and the outcome of death in patients with COVID-19. For each of the three matchings, we carried out 10 iterations and evaluated mortality rate as follows. Each iteration included all statin patients and a subset of controls chosen by PSM. Due to a large number of controls, several controls could have had a same value of the propensity score value and therefore, some statin patients could be matched to more than two controls. To explore this variability and show the robustness of the results, 10 iterations were performed by varying the control patients who had a tie in their propensity scores.
Results
A total of 18,466 patients with a laboratory-confirmed COVID-19 diagnosis and complete demographic characteristic were identified, after filtering out those who were prescribed statins outside of the defined timeframe (Figure 1). We found that 2,297 patients had an order for statins during the defined timeframe, and 16,169 patients had no orders for statins. Cohort characteristics are shown in Table 1. After matching, the mean age among statin-treated patients (68.4 years) was similar to that of controls for the three matchings (matching 1: 68.4 years, p = 0.82; matching 2: 68.6, p = 0.54; matching 3: 68.4, p = 0.93). The median BMI among statin-treated patients (29.04 kg/m2) was higher than the median BMI of controls for the three matchings (matching 1: 27.85–28.00 kg/m2, p < 1E-08; matching 2: 28.30–28.40 kg/m2, p < 1E-02; matching 3: 28.18–28.24 kg/m2, p < 1E-02); however, the calculated difference in BMI between the statin-treated and untreated groups was small (matching 1: 1.04–1.19 kg/m2; matching 2: 0.64–0.74 kg/m2; matching 3: 0.80–0.86 kg/m2) (Supplementary Table 1). Among statin-treated patients, the mortality rate was 16.1%. For the 10 iterations of PSM by demographics, we observed a higher mortality rate among controls in each iteration (18.0 to 18.4%, Chi-squared test, p < 0.05 for 9 out of 10 iterations). Exact mortality rates and p-values for each iteration are shown in Table 2. When carrying out 10 iterations of PSM by comorbidities as well as demographics, we also observed a significantly higher mortality rate in the controls (20.0 to 20.3%) in each iteration (Chi-squared test, p < 1.00E-03 for all iterations) (Table 3). When carrying out 10 iterations of PSM by medication indication as well as demographics and comorbidities, we again observed a significantly higher mortality rate in the controls (20.3 to 20.6%) in each iteration (Chi-squared test, p < 1.00E-04 for all iterations) (Table 4).
Table 1.
Cohort characteristics.
| On Statin | Overall | |||
|---|---|---|---|---|
| Characteristic | N (total = 2,297) | % | N (total = 18,466) | % |
| Age | ||||
| 18–34 | 17 | 0.7% | 4,581 | 24.8% |
| 35–49 | 166 | 7.2% | 4,104 | 22.2% |
| 50–64 | 684 | 29.8% | 4,800 | 26.0% |
| 65+ | 1,430 | 62.3% | 4,981 | 27.0% |
| Sex (%) | ||||
| Male | 1,222 | 53.2% | 8,848 | 47.9% |
| Female | 1,075 | 46.8% | 9,618 | 52.1% |
| Race | ||||
| American Indian or Alaska Native | 40 | 1.7% | 532 | 2.9% |
| Asian or Pacific islander | 91 | 4.0% | 594 | 3.2% |
| Black or African American | 742 | 32.3% | 5,378 | 29.1% |
| Mixed racial group | 232 | 10.1% | 2,985 | 16.2% |
| Other racial group | ||||
| White | 1,192 | 51.9% | 8,977 | 48.6% |
| Ethnicity | ||||
| Hispanic or Latino | 630 | 27.4% | 6,555 | 35.5% |
| Not Hispanic or Latino | 1,667 | 72.6% | 11,911 | 64.5% |
| Condition | ||||
| Hypertension | 1,833 | 79.8% | 7,481 | 40.5% |
| Diabetes | 1,254 | 54.6% | 4,365 | 23.6% |
| COPD | 321 | 14.0% | 1,171 | 6.3% |
| Obesity/High BMI | 694 | 30.2% | 4,163 | 22.5% |
| High cholesterol/Hyperlipidemia | 1,530 | 66.6% | 3,849 | 20.8% |
| ASCVD | 898 | 39.1% | 2,406 | 13.0% |
| Outcome | ||||
| Death | 369 | 16.1% | 1,619 | 8.8% |
Table 2.
Propensity score matching by demographics: a mortality rate, associated X-squared and p-value in each iteration.
| Cohort | Permutation | N deceased | N total | Mortality rate | Chi-squared | P-value |
|---|---|---|---|---|---|---|
| on Statin | 1 | 369 | 2,297 | 16.06% | 4.05 | 0.0443 |
| control | 1 | 829 | 4,594 | 18.05% | ||
| on Statin | 2 | 369 | 2,297 | 16.06% | 5.36 | 0.0206 |
| control | 2 | 843 | 4,594 | 18.35% | ||
| on Statin | 3 | 369 | 2,297 | 16.06% | 4.31 | 0.0378 |
| control | 3 | 832 | 4,594 | 18.11% | ||
| on Statin | 4 | 369 | 2,297 | 16.06% | 5.56 | 0.0183 |
| control | 4 | 845 | 4,594 | 18.39% | ||
| on Statin | 5 | 369 | 2,297 | 16.06% | 4.50 | 0.0340 |
| control | 5 | 834 | 4,594 | 18.15% | ||
| on Statin | 6 | 369 | 2,297 | 16.06% | 4.13 | 0.0420 |
| control | 6 | 830 | 4,594 | 18.07% | ||
| on Statin | 7 | 369 | 2,297 | 16.06% | 4.31 | 0.0378 |
| control | 7 | 832 | 4,594 | 18.11% | ||
| on Statin | 8 | 369 | 2,297 | 16.06% | 4.22 | 0.0399 |
| control | 8 | 831 | 4,594 | 18.09% | ||
| on Statin | 9 | 369 | 2,297 | 16.06% | 3.79 | 0.0516 |
| control | 9 | 826 | 4,594 | 17.98% | ||
| on Statin | 10 | 369 | 2,297 | 16.06% | 5.56 | 0.0183 |
| control | 10 | 845 | 4,594 | 18.39% |
Bold indicates p < 0.05.
Table 3.
Propensity score matching by demographics and comorbidities: a mortality rate, associated X-squared and p-value in each iteration.
| Cohort | Permutation | N deceased | N total | Mortality rate | Chi-squared | P-value |
|---|---|---|---|---|---|---|
| on Statin | 1 | 369 | 2,297 | 16.06% | 16.71 | 4.37E-05 |
| control | 1 | 927 | 4,594 | 20.18% | ||
| on Statin | 2 | 369 | 2,297 | 16.06% | 17.38 | 3.05E-05 |
| control | 2 | 931 | 4,594 | 20.27% | ||
| on Statin | 3 | 369 | 2,297 | 16.06% | 15.06 | 1.04E-04 |
| control | 3 | 917 | 4,594 | 19.96% | ||
| on Statin | 4 | 369 | 2,297 | 16.06% | 16.20 | 5.69E-05 |
| control | 4 | 924 | 4,594 | 20.11% | ||
| on Statin | 5 | 369 | 2,297 | 16.06% | 15.71 | 7.39E-05 |
| control | 5 | 921 | 4,594 | 20.05% | ||
| on Statin | 6 | 369 | 2,297 | 16.06% | 15.71 | 7.39E-05 |
| control | 6 | 921 | 4,594 | 20.05% | ||
| on Statin | 7 | 369 | 2,297 | 16.06% | 17.38 | 3.05E-05 |
| control | 7 | 931 | 4,594 | 20.27% | ||
| on Statin | 8 | 369 | 2,297 | 16.06% | 15.87 | 6.77E-05 |
| control | 8 | 922 | 4,594 | 20.07% | ||
| on Statin | 9 | 369 | 2,297 | 16.06% | 16.54 | 4.77E-05 |
| control | 9 | 926 | 4,594 | 20.16% | ||
| on Statin | 10 | 369 | 2,297 | 16.06% | 17.21 | 3.34E-05 |
| control | 10 | 930 | 4,594 | 20.24% |
Bold indicates p < 0.05.
Table 4.
Propensity score matching by demographics, comorbidities and indication for a statin prescription: a mortality rate, associated X-squared and p-value in each iteration.
| Cohort | Permutation | N deceased | N total | Mortality rate | Chi-squared | P-value |
|---|---|---|---|---|---|---|
| on Statin | 1 | 369 | 2,297 | 16.06% | 18.60 | 1.61E-05 |
| control | 1 | 938 | 4,594 | 20.42% | ||
| on Statin | 2 | 369 | 2,297 | 16.06% | 18.96 | 1.34E-05 |
| control | 2 | 940 | 4,594 | 20.46% | ||
| on Statin | 3 | 369 | 2,297 | 16.06% | 18.08 | 2.12E-05 |
| control | 3 | 935 | 4,594 | 20.35% | ||
| on Statin | 4 | 369 | 2,297 | 16.06% | 17.56 | 2.79E-05 |
| control | 4 | 932 | 4,594 | 20.29% | ||
| on Statin | 5 | 369 | 2,297 | 16.06% | 18.43 | 1.77E-05 |
| control | 5 | 937 | 4,594 | 20.40% | ||
| on Statin | 6 | 369 | 2,297 | 16.06% | 17.73 | 2.55E-05 |
| control | 6 | 933 | 4,594 | 20.31% | ||
| on Statin | 7 | 369 | 2,297 | 16.06% | 20.40 | 6.27E-06 |
| control | 7 | 948 | 4,594 | 20.64% | ||
| on Statin | 8 | 369 | 2,297 | 16.06% | 18.78 | 1.47E-05 |
| control | 8 | 939 | 4,594 | 20.44% | ||
| on Statin | 9 | 369 | 2,297 | 16.06% | 19.49 | 1.01E-05 |
| control | 9 | 943 | 4,594 | 20.53% | ||
| on Statin | 10 | 369 | 2,297 | 16.06% | 17.73 | 2.55E-05 |
| control | 10 | 933 | 4,594 | 20.31% |
Bold indicates p < 0.05.
Discussion
We observed a small, but statistically significant, decrease in mortality among COVID-19 patients prescribed statins when compared with propensity-score matched controls. Importantly, we did not find an increase in mortality associated with statin use. Our findings are in agreement with previous results indicating that statins may reduce COVID-19-related mortality (10, 11). The mean age of statin-treated patients in the current study (68.4 years) was lower than that in the Belgium study (85.6 years) and comparable to that in the Wuhan study (66.0 years). Ours is the first study performed using a large, diverse population across the United States. In contrast, an increased mortality rate was observed among COVID-19 patients with type-2 diabetes taking statins (13). One possible explanation is that this cohort focused only on high-risk patients hospitalized for COVID-19 who had Type-2 diabetes and therefore were at a higher risk for complications. Although ACE2 expression has been reported as variable in Type-2 diabetic patients independent of statin use (17), it is conceivable that high ACE2 expression in some Type-2 diabetics might have been further increased with statin use, increasing the potential for viral entry into cells (17–19).
Several mechanisms by which statins may benefit COVID-19 patients have been proposed, although not proven. A recent study suggested that statins could be efficient inhibitors of the SARS-CoV-2 main protease (Mpro), a key coronavirus enzyme (19). Inhibition of the MYD88–NF-κB pro-inflammatory pathway, blockage of the NLRP3 inflammasome, and upregulation of the stress-response protein, heme oxygenase (HO-1) (4, 11, 20–25) have also been suggested. After entering the cell through ACE2, SARS-CoV-2 can cause a downregulation of ACE2 (20) and a pro-inflammatory host response via the TLR-MYD88–NF-κB pathway, causing increased cytokine levels, inhibition of HO-1, and coagulation dysfunction (20, 26, 27). Statins have been shown to modulate the MYD88–NF-κB proinflammatory pathway, upregulate ACE2, and have anti-thrombotic properties, mainly through their effects on platelet function, all potentially important effects on patients with severe cases of COVID-19 (20, 23).
In addition, several recent studies have proposed the direct modulation of HO-1 as a potential therapeutic intervention for COVID-19 (28–30) as it can potentially prevent a “cytokine storm,” a dysfunctional anti-inflammatory response (26). Statins can upregulate HO-1 leading to the production of iron (Fe2+), carbon monoxide (CO) and biliverdin, which is rapidly reduced to bilirubin (31–34). These bioactive products have immunomodulatory, antioxidative, anti-inflammatory, vasodilatory, and anti-apoptotic properties, as well as anti-thrombotic properties, such as the inhibition of platelet aggregation and adhesion. Further support for the hypothesis that there might be therapeutic benefits of statins for COVID-19 patients is based on a known role of HO-1 in inducing type-1 interferon (IFN) expression and an established role of IFNs in inhibiting replication of various viruses including coronaviruses (28).
Finally, the gene expression of HO-1 is affected by the number of glutathione thymidine (GT) dinucleotide repeats in the HO-1 promoter region (26), which greatly varies among populations. The presence of longer (GT)n repeats are associated with lower basal HO-1 expression, and a decrease response to a noxious stimulus, such as infection or any other myriad of factors that can trigger upregulation of the gene (35). Because these individuals cannot sufficiently up regulate HO-1, to regain a non-inflamed state after an inflammatory stimulus (a normal physiologic response), possibly contributing to exacerbated acute or more chronic autoimmune inflammatory syndromes. The importance of there being differences in capacity to upregulate HO-1 among people is that it is plausible that those individuals with long (GT)n repeats could be at greater risk for a “cytokine storm.” Thus, statins might be useful in boosting the expression of HO-1 in these individuals when they present with COVID-19. Interestingly, a baby born totally deficient in HO-1 died in infancy with multi-system organ failure caused by a systemic vasculitis (36). While statins vary in their intended effectiveness of lipid reduction, as a class of drugs they share the above-described mechanistic generic qualities.
One of the main limitations of our report is that it is, like others, retrospective, allowing us to only demonstrate an association between statin use and COVID-19 mortality, but not causal effects. Moreover, while records are available from 2015 and beyond for some individuals in this database, this was not the case for all individuals and as such, pertinent information including previous medication use and comorbidities for some individuals could be incomplete in this database. Statins can lower plasma LDL; however, we were unable to determine if there was a significant difference in baseline LDL levels between our statins-treated and untreated groups due to the low percentage (19 to 30%) of each group that has LDL values in the Cerner database (data not shown). Our study involved medication orders for statins with order statuses that ensured that the medications were administered to the individuals—an advantage compared to outpatient prescriptions where there can be uncertainty as to whether an individual fills the prescription or takes the medication. However, the administration of different statins and at various doses, which could have differing pleiotropic effects in lieu of their designed cholesterol-lowering effect, were not considered. Nonetheless, that any mitigating effect on COVID-19-related mortality was found is intriguing. While we considered several demographics and comorbidities known to be associated with COVID-19 outcomes, unaccounted confounding variables could alter this observed association.
Overall, our findings are reassuring in that the use of statins was not associated with an increased mortality among elderly patients with COVID-19. However, the observation that there might be some increased risk associated with statin use in individuals with Type-2 diabetes warrants some caution. Considering what has been speculated about the potential beneficial effects of statins and what retrospective findings have been reported, our results should motivate further prospective studies to elucidate the potential mechanisms by which statins might be protective in some COVID-19 patients or harmful in others. Statins are widely used, low-cost medications that, if proven an effective mitigating treatment, could be an affordable option to reduce the mortality of COVID-19 even in low-income countries.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: This was an observational study of Electronic Health Records that cannot be made publicly available. Requests to access these datasets should be directed to the Cerner Clinical Research Team, coviddatalab@cerner.com.
Author Contributions
DS proposed the hypothesis investigated in the paper and the main idea of the study, supervised the analysis, co-wrote the first draft of the manuscript with IM. MS acquired data and supervised the analysis. IM designed and performed the initial analysis for the study, co-wrote the first draft of the manuscript with DS. TO acquired data, performed the analysis, made the figure and tables, contributed to writing the manuscript. GS supervised the analysis. RW contributed to writing the manuscript. IK and BL contributed to the analysis. All authors discussed results, provided critical feedback and contributed to the final manuscript.
Conflict of Interest
MS is a scientific advisor at twoXAR. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank members of the Sirota Lab for useful discussion and Dr. Boris Oskotsky for technical support. We would also like to thank Cheryl Akridge, Gary Gasperino, Stacey Purinton, and everyone on the Cerner Clinical Research Team, for providing access to the Cerner COVID-19 de-identified data environment and for technical assistance.
Footnotes
Funding. This study was supported by the Christopher Hess Research Fund and the Roberts Foundation Research Fund, and in part by the Program for Breakthrough Biomedical Research (PBBR) Grant.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.639804/full#supplementary-material
References
- 1.Johns Hopkins University & Medicine The Johns Hopkins Coronavirus Resource Center (CRC) (2020). Available online at: https://coronavirus.jhu.edu/ [accessed October 14, 2020].
- 2.Garg S, Kim L, Whitaker M, O'Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019. MMWR Morb Mortal Wkly Rep. (2020) 69:458–64. 10.15585/mmwr.mm6915e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costela-Ruiz VJ, Illescas-Montes R, Puerta-Puerta JM, Ruiz C, Melguizo-Rodríguez L. SARS-CoV-2 infection: the role of cytokines in COVID-19 disease. Cytokine Growth Factor Rev. (2020) 54:62–75. 10.1016/j.cytogfr.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonopoulos AS, Margaritis M, Lee R, Channon K, Antoniades C. Statins as anti-inflammatory agents in atherogenesis: molecular mechanisms and lessons from the recent clinical trials. Curr Pharm Des. (2012) 18:1519–30. 10.2174/138161212799504803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeiser R. Immune modulatory effects of statins. Immunology. (2018) 154:69–75. 10.1111/imm.12902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan X, Deng Y, Guo X, Shang J, Zhu D, Liu H. Atorvastatin attenuates myocardial remodeling induced by chronic intermittent hypoxia in rats: partly involvement of TLR-4/MYD88 pathway. Biochem Biophys Res Commun. (2014) 446:292–7. 10.1016/j.bbrc.2014.02.091 [DOI] [PubMed] [Google Scholar]
- 7.Fedson DS. Treating influenza with statins and other immunomodulatory agents. Antiviral Res. (2013) 99:417–35. 10.1016/j.antiviral.2013.06.018 [DOI] [PubMed] [Google Scholar]
- 8.Frost FJ, Petersen H, Tollestrup K, Skipper B. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins. Chest. (2007) 131:1006–12. 10.1378/chest.06-1997 [DOI] [PubMed] [Google Scholar]
- 9.Mehrbod P, Omar AR, Hair-Bejo M, Haghani A, Ideris A. Mechanisms of action and efficacy of statins against influenza. Biomed Res Int. (2014) 2014:872370. 10.1155/2014/872370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang X-J, Qin J-J, Cheng X, Shen L, Zhao Y-C, Yuan Y, et al. In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab. (2020) 32:176–187.e4. 10.1016/j.cmet.2020.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Spiegeleer A, Bronselaer A, Teo JT, Byttebier G, De Tré G, Belmans L, et al. The effects of ARBs, ACEis, and statins on clinical outcomes of COVID-19 infection among nursing home residents. J Am Med Dir Assoc. (2020) 21:909–914.e2. 10.1016/j.jamda.2020.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hariyanto TI, Kurniawan A. Statin therapy did not improve the in-hospital outcome of coronavirus disease 2019 (COVID-19) infection. Diabetes Metab Syndr. (2020) 14:1613–5. 10.1016/j.dsx.2020.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cariou B, Goronflot T, Rimbert A, Boullu S, Le May C, Moulin P, et al. Routine use of statins and increased mortality related to COVID-19 in inpatients with type 2 diabetes: results from the CORONADO study. Diabetes Metab. (in press: ). 10.1016/j.diabet.2020.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shrestha SK. Statin drug therapy may increase COVID-19 infection. Nep Med J. (2020) 3:326–7. 10.3126/nmj.v3i1.28256 [DOI] [Google Scholar]
- 15.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. (1983) 70:41–55. 10.1093/biomet/70.1.41 [DOI] [Google Scholar]
- 16.Ho DE, Imai K, King G, Stuart EA. MatchIt : nonparametric preprocessing for parametric causal inference. J Stat Softw. (2011) 42:1–28. 10.18637/jss.v042.i08 [DOI] [Google Scholar]
- 17.Cristelo C, Azevedo C, Marques JM, Nunes R, Sarmento B. SARS-CoV-2 and diabetes: new challenges for the disease. Diabetes Res Clin Pract. (2020) 164:108228. 10.1016/j.diabres.2020.108228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. (2020) 8:e21. 10.1016/S2213-2600(20)30116-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reiner Ž, Hatamipour M, Banach M, Pirro M, Al-Rasadi K, Jamialahmadi T, et al. Statins and the COVID-19 main protease: in silico evidence on direct interaction. Arch Med Sci. (2020) 16:490–6. 10.5114/aoms.2020.94655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castiglione V, Chiriacò M, Emdin M, Taddei S, Vergaro G. Statin therapy in COVID-19 infection. Eur Heart J Cardiovasc Pharmacother. (2020) 6:258–9. 10.1093/ehjcvp/pvaa042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bifulco M, Gazzerro P. Statin therapy in COVID-19 infection: much more than a single pathway. Eur Heart J Cardiovasc Pharmacother. (2020) 6:410–1. 10.1093/ehjcvp/pvaa055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodrigues-Diez RR, Tejera-Muñoz A, Marquez-Exposito L, Rayego-Mateos S, Santos Sanchez L, Marchant V, et al. Statins: could an old friend help in the fight against COVID-19? Br J Pharmacol. (2020) 177:4873–86. 10.1111/bph.15166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fedson DS, Opal SM, Rordam OM. Hiding in plain sight: an approach to treating patients with severe COVID-19 infection. MBio. (2020) 11:e00398–20. 10.1128/mBio.00398-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Subir R, Jagat JM, Kalyan KG. Pros and cons for use of statins in people with coronavirus disease-19 (COVID-19). Diabetes Metab Syndr. (2020) 14:1225–9. 10.1016/j.dsx.2020.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fajgenbaum DC, Rader DJ. Teaching old drugs new tricks: statins for COVID-19? Cell Metab. (2020) 32:145–7. 10.1016/j.cmet.2020.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fakhouri EW, Peterson SJ, Kothari J, Alex R, Shapiro JI, Abraham NG. Genetic polymorphisms complicate COVID-19 therapy: pivotal role of HO-1 in cytokine storm. Antioxidants (Basel). (2020) 9:636. 10.3390/antiox9070636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazzaroni MG, Piantoni S, Masneri S, Garrafa E, Martini G, Tincani A, et al. Coagulation dysfunction in COVID-19: The interplay between inflammation, viral infection and the coagulation system. Blood Rev. (2020). 10.1016/j.blre.2020.100745. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Singh D, Wasan H, Reeta KH. Heme oxygenase-1 modulation: a potential therapeutic target for COVID-19 and associated complications. Free Radic Biol Med. (2020) 161:263–71. 10.1016/j.freeradbiomed.2020.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kwong KK, Chan S-T. The role of carbon monoxide and heme oxygenase-1 in COVID-19. Toxicol Rep. (2020) 7:1170–1. 10.1016/j.toxrep.2020.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagener FADTG, Pickkers P, Peterson SJ, Immenschuh S, Abraham NG. Targeting the heme-heme oxygenase system to prevent severe complications following COVID-19 infections. Antioxidants (Basel). (2020) 9:540. 10.3390/antiox9060540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsu M, Muchova L, Morioka I, Wong RJ, Schröder H, Stevenson DK. Tissue-specific effects of statins on the expression of heme oxygenase-1 in vivo. Biochem Biophys Res Commun. (2006) 343:738–44. 10.1016/j.bbrc.2006.03.036 [DOI] [PubMed] [Google Scholar]
- 32.Muchova L, Wong RJ, Hsu M, Morioka I, Vitek L, Zelenka J, et al. Statin treatment increases formation of carbon monoxide and bilirubin in mice: a novel mechanism of in vivo antioxidant protection. Can J Physiol Pharmacol. (2007) 85:800–10. 10.1139/Y07-077 [DOI] [PubMed] [Google Scholar]
- 33.Azuma J, Wong RJ, Morisawa T, Hsu M, Maegdefessel L, Zhao H, et al. Heme oxygenase-1 expression affects murine abdominal aortic aneurysm progression. PLoS ONE. (2016) 11:e0149288. 10.1371/journal.pone.0149288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsur A, Kalish F, Burgess J, Nayak NR, Zhao H, Casey KM, et al. Pravastatin improves fetal survival in mice with a partial deficiency of heme oxygenase-1. Placenta. (2019) 75:1–8. 10.1016/j.placenta.2018.11.001 [DOI] [PubMed] [Google Scholar]
- 35.Pechlaner R, Willeit P, Summerer M, Santer P, Egger G, Kronenberg F, et al. Heme oxygenase-1 gene promoter microsatellite polymorphism is associated with progressive atherosclerosis and incident cardiovascular disease. Arterioscler Thromb Vasc Biol. (2015) 35:229–36. 10.1161/ATVBAHA.114.304729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yachie A, Niida Y, Wada T, Igarashi N, Kaneda H, Toma T, et al. Oxidative stress causes enhanced endothelial cell injury in human heme oxygenase-1 deficiency. J Clin Invest. (1999) 103:129–35. 10.1172/JCI4165 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: This was an observational study of Electronic Health Records that cannot be made publicly available. Requests to access these datasets should be directed to the Cerner Clinical Research Team, coviddatalab@cerner.com.