Abstract
Background
Treatment of lower limb post-traumatic osteomyelitis used to be a staged process, with radical debridement of bone and soft tissues at first stage, followed by a second-stage limb reconstruction operation to restore the limb integrity. Some studies recently reported that achieving infection eradication and limb reconstruction at single-stage seems to be an effective method for lower limb infection, but a comparative study remains lacking. This study aims to compare the results of radical debridement combined with a first/second-staged osteotomy and bone transport, for the management of lower limb post-traumatic osteomyelitis.
Methods
From January 2013 to June 2018, a total of 102 patients with lower limb post-traumatic osteomyelitis met the criteria were included for analysis, in which 70 patients received one-stage debridement, antibiotic-loaded implantation, metaphysis osteotomy and bone transport were named as one-stage group, while 32 patients with first-stage debridement and antibiotic-loaded calcium sulfate implantation, second-stage osteotomy and bone transport were devised as two-stage group. The outcomes of hospitalization (hospital stay, costs of treatment, surgical time, antibiotic usage) and follow-up (infection-free, treatment failure, infection recurrence, external fixation index (EFI) and docking site union) between the two groups were retrospectively compared.
Results
For outcomes of hospitalization, patients in the one-stage group had batter results on hospital stay (18.2 days versus 28.9 days, P < 0.05), surgical time (164.8 min versus 257.4 min, P < 0.05), cost of treatment (¥101726.1 versus ¥126718.8, P < 0.05) and the course of antibiotic usage (10.3 days versus 12.0 days, P < 0.05). During the follow-up, 87.1% (61/70) patients in the one-stage group compared to 93.8% (30/32) patients in the two-stage group achieved infection-free (P > 0.05) without any additional debridement operation. 94.3% (66/70) patients in the one-stage group earned wound healing after the operation, comparing to 96.9% (31/32) patients healed in the two-stage group (P > 0.05). Uncontrolled infection was observed on 4 (5.7%) patients in the one-stage group and 1 (3.1%) patients in the two-stage group (P > 0.05), with a result of three achieved infection free in the one-stage group and one patient suffered from amputation in each group respectively. 5 (7.2%) patients in the one-stage group and 1 (3.2%) patient in the two-stage group encountered with infection recurrence (P > 0.05) and were well-managed with re-debridement and antibiotics usage. Significance was not found between two groups on EFI (74.8 days/cm versus 69.0 days/cm, P > 0.05) and docking site nonunion rate (14.5% versus 18.9%, P > 0.05), indicating that bone transport in different stages played a less essential role on bone generation process. The other complications, such as prolonged aseptic drainage [24.3% (17/70) versus 21.9% (7/32)], re-fracture [5.8% (4/69) versus 3.2% (1/31)], pin-tract infection [23.2% (16/69) versus 19.4% (6/31)], joint stiffness and deformity [26.1% (18/69) versus 32.3% (10/31)], also showed less significance when comparing between two groups (P > 0.05), suggesting that different transport stages play little role on complications formation.
Conclusions
One-stage radical debridement and bone transport was proven to be a safe and effective method for treating static (or near static) lower limb osteomyelitis.
Translational potential statement
Translational potential statement One-stage debridement and bone transport is sample, effective and time-saving, with similar complications compared to conventional two-stage protocol. This treatment protocol might provide an alternative for the treatment of static (or near static) lower limb osteomyelitis.
Keywords: Osteomylitis, Segmental bone defect, Bone transport, Distraction osteogenesis, External fixation
1. Introduction
Post-traumatic osteomyelitis on the lower extremity is a kind of refractory disease for orthopedic surgeons and usually caused by an open fracture or inappropriate open reduction and internal fixation (ORIF). Once established, patients are prone to suffer from a variety of disastrous complications, which can significantly reduce the quality of life [1]. To date, the treatment of those types of infection remains challenging, as orthopedic surgeons need to take various factors into consideration, which at least include persistent and stubborn infection, poor soft tissue coverage, subsequent segmental bone defects, and potential limbs deformity [[2], [3], [4]]. Therefore, although there has been progressing in surgical techniques and related equipment, treatment of post-traumatic osteomyelitis on lower extremity still represents a relatively complicated and time-consuming process.
Currently, the mainstay protocol of lower-limb post-traumatic osteomyelitis is staged progress containing two essential phases, namely, infection elimination and secondary limb reconstruction [5,6]. As the first and basic stage of treatment process, infection elimination mainly includes segmental bone resection, extensive soft tissue debridement, and postoperative antibiotics application, aiming to remove infected focus radically and provide a satisfying environment for secondary reconstruction. Conventionally the second-stage reconstruction is carried out 6–8 weeks or months later, after the symptoms of infection have completely disappeared and the inflammatory markers have reduced to normal levels [6], by means of Masquelet technique [7,8], vascularized fibular grafts [9], cancellous bone grafting [10] or Ilizarov segmental bone transport [[11], [12], [13]]. In total, the entire hospital stay for post-traumatic osteomyelitis treatment usually takes several weeks or even months, during which patients have to endure two episodes of invasive operations, regardless of the failure of therapy and sharply increased financial costs. Therefore, a simplified treatment method is imperative.
At present, the Ilizarov bone transport technique seems to be a more convenient and effective method in the reconstruction of an infected defect, as it permits not only gradually restoring the integrity of lower extremity, but correcting the limb deformity, joint contractures and allowing early weight bearing [11]. Additionally, the distinction of Ilizarov bone transport technique from other reconstruction techniques is that its bone regeneration process occurs at the aseptic distraction zone outside the infection focus [11], thus avoiding direct interference from the infected area. Furthermore, today’s progress of debridement guidelines and the introduction of degradable local antibiotic carriers [[14], [15], [16]] also help remove infected tissues radically and eradicate the residual pathogens more efficiently. Combining with above-mentioned reasons, simplifying the conventional multi-staged operations into a single operation seems to be a practical approach.
Although a similar sequential treatment protocol has been introduced in previous studies [11,13,17,18], unfortunately, the aims of those studies did not focus on assessing this technique. Besides, to our best knowledge, a comparative study to evaluate the difference of radical debridement combined with bone transport at different stages remains lacking in the report. The objective of this comparative study was to compare two treatment methods; a single procedure that included radical debridement, topical antibiotic-loaded spacer placement, metaphysis osteotomy and bone transport versus the first-stage debridement and topical antibiotics placement followed by a second-stage osteotomy and bone transport, for the management of static (or near static) post-traumatic osteomyelitis, and to evaluate the safety and effectiveness of such one-stage treatment method at the same time.
2. Methods and materials
2.1. Participants and preoperative management
This retrospective comparative study focused on patients with tibial or femoral post-traumatic osteomyelitis treated in our medical center from January 2013 to June 2018. The main inclusion criteria of our study were 1) patients over 16 years old, 2) femoral or tibial post-traumatic osteomyelitis without severe soft tissues defects or apparent active infection symptoms, 3) treated with radical debridement, antibiotic-loaded calcium sulfate implantation followed by one/two-stage bone transport with the help of a unilateral external fixator. The study’s exclusion criteria were 1) patients treated by the other reconstruction methods, 2) no use of antibiotic-loaded calcium sulfate as a topical antibiotic spacer, 3) associated severe liver, kidney or cardiac dysfunction, or 4) incomplete reconstruction treatment or refused to participate in the study. In accordance with the above-mentioned criteria, a total of 102 patients with 102 infected limbs (76 on tibia and 26 on femur) were qualified to be included for analysis. Based on one-stage osteotomy and bone transport or not, 70 patients received one-stage management were allocated as the one-stage group. In comparison, 32 patients received two-stage management were assigned as the two-stage group.
The medical history of patients was initially documented after presentation, followed by a complete physical examination, imaging examinations, and laboratory tests. Since a part of patients in both groups had implants from previous operations, Magnetic Resonance Imaging (MRI) was accomplished only in a position of patients to detect the extent of infection more accurately. Preoperative antibiotics usage was suspended until samples had been obtained for culture during surgery, in order to avoid interference in biopsy culture. The details of patients in the two groups were presented in Table 1. Our study has been approved by the Ethical Committee of Guangdong second provincial general hospital and Nanfang hospital. All included patients consented to participate in this study and signed a consent form.
Table 1.
Preoperative characteristics of two groups.
| Parameters | One-stage group | Two-stage group | P value |
|---|---|---|---|
| No. of patients | 70 | 32 | — |
| Mean ages (years) | 38.1 (17–63) | 38.0 (17–62) | 0.974 |
| Sex (Male) | 65/70 | 30/32 | 1.000 |
| Side (Left) | 36 | 9 | 0.048 |
| Site (Tibia) | 56 | 20 | 0.06 |
| Mean infection history (months)∗ | 53.6 (0.1–306) | 46.8 (0.2–48) | 0.282 |
| Etiology of infection | 0.853 | ||
| Infected after open fracture | 38 | 18 | |
| Infected after ORIF | 32 | 15 | |
| Alcohol/Cigarette abuse | 6 | 1 | 0.429 |
| Hypertension/Diabetes | 3 | 4 | 0.201 |
| Mean WBC count ( × 109/L) | 7.76 (3.67–12.83) | 7.72 (4.62–12.08) | 0.945 |
| Mean CRP (ng/L) | 10.39 (0.2–59.69) | 13.56 (0.98–39.40) | 0.200 |
| Mean ESR (mm/h)∗ | 28.2 (1–147) | 32.5 (1–138) | 0.109 |
Note: ∗, data failed to pass normality test and were compared using a Mann–Whitney U test
2.2. Surgical technique
Surgical procedures were carried out by experienced surgeons after spinal anesthesia. Before radical debridement, 2 to 3 Schanz screws were screwed into three positions, namely, the proximal and distal tibia or femurs, the place adjacent to the infected bone, for conveniently restoring the good alignment after segmental bone resection. Usually, an incision was made along with previous surgical scars, or an anterolateral longitudinal incision was adopted if skin was still intact. Extensive infected bone resection and soft tissue debridement were performed until the “Paprika sign” [19,20] from surrounding tissue was appreciated. Meanwhile, bone samples were collected from different areas of infection focal and sent for bacterial culture and histological examination. Following the extensive debridement, at least 9 L of saline was employed for adequate irrigation and removing the residues.
In the one-stage group, low-energy metaphyseal osteotomy was performed percutaneously followed by radical osteomyelitis debridement, with the help of an aseptic osteotome. External fixator was then completely assembled, and the antibiotic-loaded calcium sulfate (Stimulan, Biocomposites Ltd.) was prepared with a conventional ratio (vancomycin 0.5g + gentamycin 2ml + calcium sulfate 5 cc + saline 0.5ml) and embedded into the bony defect space. In the two-stage group, external fixator was directly assembled after debridement and antibiotic-loaded calcium sulfate implantation without one-staged metaphyseal osteotomy. The osteotomy was carried out in the secondary surgery weeks later, when the symptoms of infection were completely disappeared, and the infection markers had reduced to normal levels (See Fig. 1).
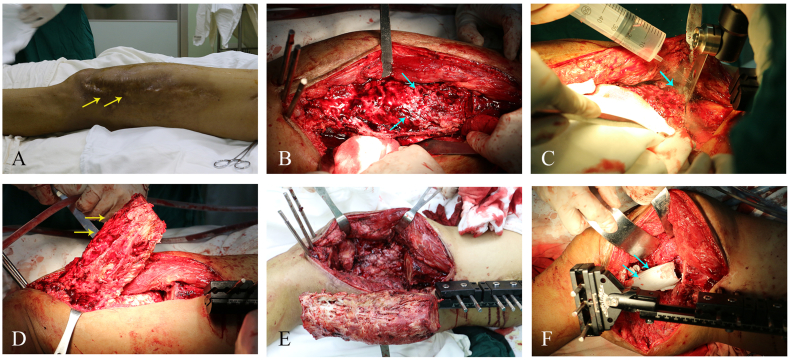
Figure 1.
Intra-operative presentation of debridement and antibiotic-loaded calcium sulfate implantation. (A) Pre-operative appearance of a patient. (B) Radical soft tissue debridement. (C–E) Segmental bone resection of the left femur. (F) Monolateral external fixator assembly and antibiotic-loaded calcium sulfate implantation.
2.3. Postoperative management
Intravenous antibiotics were prescribed to the patients in both groups, with the protocol of empirical antibiotics for the first several days and exchanged to sensitive antibiotics according to the culture results. Wound dressing and nail tract disinfection were performed every two days, unless the excessive drainage was noted in the meantime. In the one-stage group, patients were suggested to start bone transport 6–10 days after the operation, with a distraction length of 1mm/day completed by four times external fixator manipulation. Patients in the two-stage group received similar management after their first operation but started transport 6–10 days after the second-stage osteotomy operation. Patients in both groups were encouraged to begain full-wright-bearing exercise and joints motion once pain had been disappeared. After discharge, patients were followed-up in the clinic each month for physical, laboratory, and radiograph examination during the next several months, for observing the infection control, monitoring new bone mineralization, and correcting complications caused by distraction, until the limb discrepancy was completely restored and the limb length equalization was finally achieved. Then they were recommended to attend outpatient every 2–3 months. When the osteogenesis of distraction area and docking site was well-consolidated, and at least three cortices had connected on radiographs [18], dynamization was carried out for another one month, and then the external fixator was completely removed.
2.4. Data collection and evaluation
The outcomes of this comparative study mainly focused on two sections, namely the section of hospitalization and follow-up. During hospitalization, we compared the hospital stay, total costs of treatments, surgery time, and culture results of intra-operative samples between two groups. In the follow-up section, wound healing, infection remission, treatment failure (including uncontrolled infection and infection recurrence), external fixation time (EFT), length of bone transport, external fixation index (EFI), docking site nonunion, and treatment-related complications (prolonged aseptic drainage, refracture after external removal, pin-tract infection, etc.) in two groups were compared.
2.5. Statistical analysis
Data were collated using Microsoft Excel (Redmond, Washington) and analyzed using SPSS v25.0 (SSPS Inc., Chicago, Illinois). Continuous variables which were verified of normal distribution and the homogeneity of variance were compared using Independent-Samples T-Test; Continuous variables which failed to pass normality test were compared using a Mann–Whitney U test. Pearson χ2 or Fisher Exact Test were used in comparing the enumeration data. P < 0.05 was considered statistically significant.
3. Results
Between January 2013 to June 2018, a total of 102 patients with tibial or femoral post-traumatic osteomyelitis were treated in our infection center, of which 68.6% (70/102) patients underwent one-stage debridement, antibiotic-loaded calcium sulfate implantation, osteotomy, and bone transport, 31.4% (32/102) patients underwent debridement and antibiotic-loaded calcium sulfate implantation at first-stage, followed by a second-staged osteotomy and bone transport. This study mainly focused on the outcomes of hospitalization and follow-up to detect the difference between two groups.
3.1. Outcomes of hospitalization
Under the hospitalization section, the data of hospital stay, surgical time, bone defects, costs of treatment, the type of fixators, bacterial results and antibiotics usage were collected and compared. As presented in Table 2, comparing to those in the two-stage group, patients in the one-stage group earned an apparently shorter hospital stay (18.2 days versus 28.9 days, P < 0.05). Concerning the surgical duration and financial costs, patients in the one-stage group omitted second anesthesia and pre-operative preparation, thus also had a short surgical time (164.8 min versue 257.4 min, P < 0.05), less cost of treatment (¥ 101726.1 versue ¥ 126718.8, P < 0.05). Additionally, attributing to one-stage operation, patients in the one-stage group also earned a shorter antibiotics administration course (10.3 days versue 12.0 days, P < 0.05). Postoperative histology results of 102 limbs confirmed the preoperative diagnosis of low limb osteomyelitis.
Table 2.
Outcomes of patients in two groups during hospitalization and follow-up.
| Outcome parameters | One-stage group N = 70 |
Two-stage group N = 32 |
P value |
|---|---|---|---|
| Mean hospital stay (days) | 18.2 (6–35) | 28.9 (14–53) | <0.0001 |
| Mean surgical time (minutes)∗ | 164.8 (72–324) | 257.4 (125–556) | <0.0001 |
| Mean cost of treatment (¥)∗ | 101726.1 (50439-176241) | 126718.8 (70224-18870) | <0.0001 |
| Positive culture results | 34 | 21 | 0.109 |
| Postoperative antibiotics usage (days)∗ | 10.3 (0–39) | 12.0 (7–23) | 0.027 |
| Mean surgery frequency during follow-up | 0.61 (42/70) | 0.72 (23/32) | 0.521 |
| Wound healing rate | 94.3% (66/70) | 96.9%(31/32) | 0.946 |
| Infection-free rate | 87.1% (61/70) | 93.8% (30/32) | 0.495 |
| Amputation rate | 1.4% (1/70) | 3.1% (1/32) | 0.531 |
| Infection recurrence rate | 7.2% (5/69) | 3.2% (1/31) | 0.663 |
| Length of distraction (cm)∗ | 8.9 (3.9–20.7) | 11.7 (3.78–25.9) | 0.004 |
| External fixation time (EFT)∗ | 599.5 (207–1821) | 685.6 (371–1070) | 0.011 |
| External fixation index (EFI)∗ | 74.8 (18.1–230.9) | 69.0 (26.1–250.3) | 0.330 |
| Docking site non-union | 14.5% (10/69) | 18.9% (7/31) | 0.319 |
Note: ∗, data failed to pass normality test and were compared using a Mann–Whitney U test
Bacterial culture of intraoperative samples showed positive results of 48.6% (34/70) samples in the one-stage group and 65.6% (21/32) positive results in the two-stage group (P > 0.05), Among which 23.5% (8/34) samples in the one-stage group and 19.0% (4/21) samples in the two-stage group were detected with polybacterial infection (P > 0.05). As presented in Fig. 2, S. aureus and P. aeruginosa were the most frequently detected bacteria of intra-operative samples’ culture, followed by E. faecalis, E.clocae, and Klebsiella pneumonia. The sensitivity test proved that all pathogens were sensitive to the topical used antibiotics.
Figure 2.
Culture results and bacterial species of two groups. Fig. 2A. Positive and negative rates of bacteria culture in two groups. Fig. 2B. Bacteria distribution of two groups. S. aureus and P. aeruginosa were the most frequent isolated bacteria of culture, followed by E. faecalis, E.clocae, Klebsiella pneumonia and the other species. Notes:S. sureus, Staphylococcus aureus. P. aeruginosa, Pseudomonas aeruginosa. E. faecalis, Enterococcus faecalis. E. cloacae, Enterobacter cloacae. KPC, Klebsiella pneunoniae. E. coli, Escherichia coli. E. faecium, Enterococcus faecium. A. baumannii, Acinetobacter baumannii. E. aerogenes, Enterobacter aerogenes. S. marcescens, Serratia marcescens. S. pasteuri, Staphylococcus pasteuri. P. mirabilis, Proteus mirabilis. P. putida, Pseudomonas putida. E. avium, Enterococcus avium. S. epidermidis, Staphylococcus epidermidis.
3.2. Outcomes of follow-up
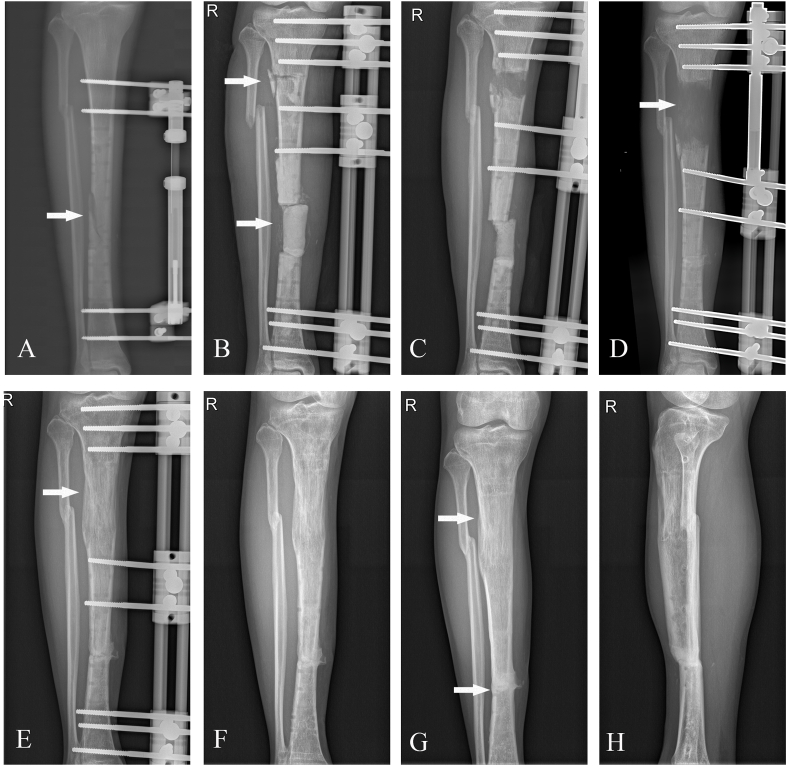
The follow-up data were presented in Table 2, and two patients with single or two-stage treatment were presented in Figure 3, Figure 4. During the entire follow-up, a total of 61 (87.1%) patients in the one-stage group achieved infection-free without any additional surgical interventions, compared to 30 (93.8%) patients in the two-stage group (P > 0.05). 66 (94.3%) patients in the one-stage group earned wound healing after the operation, comparing to 31 (96.9%) patients healing in the two-stage group (P > 0.05). 9 (12.9%) patients in the one-stage group suffered from treatment failure (4 uncontrolled infection after operation and five infection recurrence after wound healing), while 2 (6.2%) patients were recorded the same situations in the two-stage group (P > 0.05). 2 patients (1 in the one-stage group and 1 in the two-stage group respectively) suffered from a major amputation due to continuously uncontrolled infection, despite repeated re-debridement and antibiotics usage during follow-up. Infection recurrence appeared on 5 (7.2%) patients in the one-stage group and 1 (3.2%) patient in the two-stage group (P > 0.05) and was successfully managed with a repeated soft tissue debridement and segmental bone resection. Complications during treatment mainly included prolonged aseptic drainage [17 (24.3%) in one-stage group versus 7 (21.9%) in two-stage group, P > 0.05], re-fracture after fixtor removal [4 (5.8%, 4/69) versus 1 (3.2%, 1/31), P > 0.05], pin-tract infection [16 (23.2%, 16/69) versus 6 (19.4%, 6/31), P > 0.05], which were well-managed by regular dressing changing, stable re-fixation, and sensitive antibiotics application, respectively. Additionally, joint stiffness and deformity was another complication that could not be neglected, which presented at least 18 (26.1%, 18/69) cases in the one-stage group and 10 (32.3%, 19/31) cases in the two-stage group (P > 0.05).
Figure 3.
The preoperative and follow-up X-rays of a patient after one-stage debridement and bone transport. (A) White arrow showed infected non-union on the right tibia. (B) Radical debridement, antibiotic-loaded calcium sulfate placement and metaphyseal osteotomy were performed during the one-stage procedure. (C–E) Bone transport process during follow-up. (F–H) External fixator removal after new bone consolidation and docking site union.
Figure 4.
One-stage radical debridement and antibiotic-loaded calcium sulfate placement combined with a second-stage bone reconstruction operation. (A–B) Preoperative X-rays of a patient. (C) One-stage operation of radical debridement and antibiotic-loaded calcium sulfate placement. (D) Osteotomy finished at the second-stage. (E–G) Process of bone transport, mineralization and docking site union. (H) Presentation after external fixator removal.
The external fixation index (EFI) was a ratio of the number of days the frame was used to the length of regenerated bone [18], which reflects the ability of bone regeneration and consolidation. As a result of our study, the EFI between the two groups failed to show any statistical difference (74.8 days/cm versus 69.0 days/cm, P > 0.05), indicating that bone transport at different stages did not play an essential role in the process of new bone formation and consolidation. For the docking site nonunion, 14.5% (10/69) in the one-stage group compared to 18.9% (7/31) in the two-stage group without showing any statistical significance (P > 0.05), meaning that bone transport at different stages also had less influence on docking union.
4. Discussion
Conventional management of post-traumatic osteomyelitis represents a complicated and time-consuming process by means of segmental bone resection and extensive soft tissue debridement in one-stage, followed by postoperative antibiotics administration and a second-staged osteotomy and bone transport. To some extent, the advantage of such method remains apparent, with a guaranteed low failure treatment rate, especially in patients with active infection and poor topical soft tissue situations. When managing patients without noticeable infection symptoms and whose soft tissue remains in an acceptable condition, one-stage operation presents advantages in outcomes of hospitalization and could be suggested. Regrettably, to date there were still few studies compared those criteria between patients treated with such two methods. Our study firstly compared those subjects by good control of variables and proved that, if without apparent infection symptoms, patients received one-stage treatment did receive better results on hospital stay, surgery time, surgical operation, antibiotics usage, and costs for the treatment. Those outcomes were easy for understanding and explaining. Since combining the steps of infection eradication and limb reconstruction into one operation, conventional prolonged hospital stay, operation time, and additional hospitalization between two-stage surgery can be sharply shortened or even omitted, which in turn resulted in a reduced cost of hospital stay, the burden of surgery and anesthetization of patients at the same time. Therefore, patients definitely benefited from such a one-stage operation on the aspect of hospitalization.
Regarding the outcomes during follow-up, the infection-free rate and recurrence rate of the two groups were generally similar (87.1% vs. 93.8%, P > 0.05 and 7.2% vs. 3.2%, P > 0.05, respectively). Such outcomes in the one-stage group were consistent with the previous studies and proved that combining the conventional secondary osteotomy and bone transport into a single-stage operation did not sharply increase the failure of infection eradication. Hakan Kinik et al. reported all 30 patients with infected tibial nonunion achieved union and infection-free after treated with a similar method [13]. In their study of comparing clinical results of bifocal or trifocal bone transport, Maimaiaili Yushan et al. treated 37 patients with large tibial defects caused by infection debridement using such single-stage protocol, in which they reported all of the patients achieved infection eradication without further management [18]. Also, our previous study on chronic tibial and femoral osteomyelitis had received satisfying results after such one-stage infection eradication combined with osteotomy and bone transport [21]. Reasons for explaining such a high infection-free rate and low recurrence rate of this one-stage method, as far as we concerned, might contain at least three parts. Firstly, metaphyseal osteotomy and unique bone regeneration characteristic of bone transport [11] avoid direct contact of bone regeneration zone and infection zone, thus reducing the interference of infection factors on new bone formation and consolidation. Additionally, hundreds to thousands times of topical concentration antibiotics level higher than MIC [14,22,23] produced by antibiotic-loaded calcium sulfate was enough to penetrate the biofilm of bacteria and eradicate residual pathogens more efficiently. Therefore, a more aseptic environment was provided. Finally, today’s progress of debridement guidelines and techniques associated with carrying out our operation during a static period ultimately played an essential role in preventing the failure of the one-staged treatment.
External fixation index (EFI) is a widely accepted criterion to evaluate bone regeneration and consolidation. During follow-up, we recorded the external fixation time (EFT) and length of distraction to calculate the external fixation index (EFI). Our study’s results showed longer mean EFI than previous studies, which was 74.8 days/cm (2.5 months/cm) in one-stage group and 69.0 days/cm (2.3 months/cm) in two-stage group respectively, compared to mean EFI of 1.49 months/cm [14,22,23], 1.8 months/cm [11,12] and a more shorter EFI of 52 days/cm [24] in previous studies. Reasons leading to such different results were uncertain. The combined analysis of tibia and femur in our study might partially contribute to the longer EFI. Another potential reason was that some patients in our study attended outpatient without regular frequency, especially in the period of bone consolidation. Because of long-distance or poor compliance, those patients went to the outpatient clinic follow-ups every three to five months. Even after the new bone formation was complete and strong enough for weight-bearing, some patients failed to remove the external fixator in time, which inevitably prolonged the EFT and EFI.
By comparing EFI and docking union between two groups, we aimed to detect whether bone transport at different stages influenced bone regeneration and consolidation or not. For EFI, theoretically, patients in two-stage group suffered from an additional waiting period with completely assembled external fixator but without bone transport. Thus they might have a longer external fixation time per centimetr when added with such waiting period. However, it was not well confirmed by our study. Despite having additional waiting duration, EFI in the two-stage group failed to present any prominent significance compared with the one-stage group (P > 0.05). The reasons for this result were still unclear. Perhaps patients in the two-stage group started bone transport in a more aseptic condition might lead to quicker bone regeneration and consolidation, thus resulting in a shorter EFI than estimated. Additionally, although patients in the two-stage group had an additional waiting period, such period was comparatively shorter when comparing to the whole duration of reconstruction. After divided by length of distraction, it was hard to play an essential role on EFI. Overall, our study proved that the process of bone regeneration and consolidation in the one-stage group did not differ from the same process in the two-stage group. With regard to docking union, theoretically, patients in the two-stage group would own a higher union rate with more completely controlled infection. Unfortunately, our results also failed to support such hypothesis. The rational explanation for this result was that different infection situations between two groups were a temporary factor, which was hard to play a continuous role on the relatively long bone formation process.
In this study we omitted the comparison of bone results and functional results with ASAMI and Paley’s criteria, since limb deformity, discrepancy, and joint movement limitation primarily depended on the types of external fixators, the size of defects, the position of osteotomy, and postoperative function training, instead of the different bone transport stages focused on this study. We briefly compared the complications between two groups, only aiming to confirm that different bone transport stages played little role on such complications, which could in turn support our conclusions more robustly. Not surprisingly, surgery-related complications in two groups were compared but no significance was founded, confirming our view that different bone transport stages could not influence the complications rate.
To the best of our knowledge, although some previous studies applied this one-stage treatment protocol, our study might be the first comparative study assessing the outcomes of the one-stage protocol with the conventional two-stage treatment method in treating post-traumatic osteomyelitis. The limitations of our study are mainly in two aspects. Since the study is retrospective, outcomes of two groups might not be as reliable as those from prospective randomized controlled studies. Also, we have to clarify that our study mainly focused on post-traumatic osteomyelitis in a static (or near to static) period, when the symptoms of infection were generally controlled and the inflammatory biomarkers maintained at acceptable levels. Whether one-staged protocol can be carried out safely on patients with an active infection, question remains unsolved.
5. Conclusion
Achieving radical debridement, antibiotic-loaded calcium sulfate implantation, osteotomy, and bone transport at one-stage operation have proven to be a safe and effective method for the treatment of static (or near static) lower limb post-traumatic osteomyelitis.
Funding
This study was supported by the science foundation of Guangdong Second Provincial General Hospital (NO. YY2018005). The funders had role in editing and final approval of the manuscript.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors thank all patients and staff who made this study possible.
References
- 1.Zhou C.H., Ren Y., Ali A., Meng X.Q., Zhang H.A., Fang J. Single-stage treatment of chronic localized tibial osteomyelitis with local debridement and antibiotic-loaded calcium sulfate implantation: a retrospective study of 42 patients. J Orthop Surg Res. 2020;15(1):201. doi: 10.1186/s13018-020-01721-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jain A.K., Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res. 2005;431:57–65. doi: 10.1097/01.blo.0000152868.29134.92. [DOI] [PubMed] [Google Scholar]
- 3.Bose D., Kugan R., Stubbs D., McNally M. Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint Lett J. 2015;97-B(6):814–817. doi: 10.1302/0301-620X.97B6.33276. [DOI] [PubMed] [Google Scholar]
- 4.McNally M., Ferguson J., Kugan R., Stubbs D. Ilizarov treatment protocols in the management of infected nonunion of the tibia. J Orthop Trauma. 2017;31:S47–S54. doi: 10.1097/BOT.0000000000000987. [DOI] [PubMed] [Google Scholar]
- 5.Jupiter J.B., Kour A.K., Palumbo M.D., Yaremchuk M.J. Limb reconstruction by free-tissue transfer combined with the Ilizarov method. Plast Reconstr Surg. 1991;88(6):943–951. doi: 10.1097/00006534-199112000-00001. 952-954. [DOI] [PubMed] [Google Scholar]
- 6.Tukiainen E., Asko-Seljavaara S. Use of the Ilizarov technique after a free microvascular muscle flap transplantation in massive trauma of the lower leg. Clin Orthop Relat Res. 1993;297:129–134. [PubMed] [Google Scholar]
- 7.Cui T., Li J., Zhen P., Gao Q., Fan X., Li C. Masquelet induced membrane technique for treatment of rat chronic osteomyelitis. Exp Ther Med. 2018;16(4):3060–3064. doi: 10.3892/etm.2018.6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akgun U., Canbek U., Aydogan N.H. Masquelet technique versus Ilizarov bone transport for reconstruction of lower extremity bone defects following posttraumatic osteomyelitis. Injury. 2018;49(3):738. doi: 10.1016/j.injury.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Schöttle P.B., Werner C.M.L., Dumont C.E. Two-stage reconstruction with free vascularized soft tissue transfer and conventional bone graft for infected nonunions of the tibia: 6 patients followed for 1.5 to 5 years. Acta Orthop. 2009;76(6):878–883. doi: 10.1080/17453670510045534. [DOI] [PubMed] [Google Scholar]
- 10.Lortat-Jacob A., Lelong P., Benoit J., Ramadier J.O. [Complimentary surgical procedures following treatment of non-union by the Papineau method (author’s transl)] Rev Chir Orthop Reparatrice Appar Mot. 1981;67(2):115–120. [PubMed] [Google Scholar]
- 11.Sigmund I.K., Ferguson J., Govaert G.A.M., Stubbs D., McNally M.A. Comparison of Ilizarov bifocal, acute shortening and relengthening with bone transport in the treatment of infected, segmental defects of the tibia. J Clin Med. 2020;9(2):279. doi: 10.3390/jcm9020279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tetsworth K., Paley D., Sen C., Jaffe M., Maar D.C., Glatt V. Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury. 2017;48(10):2276–2284. doi: 10.1016/j.injury.2017.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Kinik H., Kalem M. Ilizarov segmental bone transport of infected tibial nonunions requiring extensive debridement with an average distraction length of 9,5 centimetres. Is it safe? Injury. 2019 doi: 10.1016/j.injury.2019.12.025. 2019-12-17. [DOI] [PubMed] [Google Scholar]
- 14.Ferguson J.Y., Dudareva M., Riley N.D., Stubbs D., Atkins B.L., McNally M.A. The use of a biodegradable antibiotic-loaded calcium sulphate carrier containing tobramycin for the treatment of chronic osteomyelitis: a series of 195 cases. Bone Joint Lett J. 2014;96-B(6):829–836. doi: 10.1302/0301-620X.96B6.32756. [DOI] [PubMed] [Google Scholar]
- 15.Rod-Fleury T., Dunkel N., Assal M., Rohner P., Tahintzi P., Bernard L. Duration of post-surgical antibiotic therapy for adult chronic osteomyelitis: a single-centre experience. Int Orthop. 2011;35(11):1725–1731. doi: 10.1007/s00264-011-1221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beuerlein M.J., McKee M.D. Calcium sulfates: what is the evidence? J Orthop Trauma. 2010;24(Suppl 1):S46–S51. doi: 10.1097/BOT.0b013e3181cec48e. [DOI] [PubMed] [Google Scholar]
- 17.Yin P., Zhang L., Li T., Zhang L., Wang G., Li J. Infected nonunion of tibia and femur treated by bone transport. J Orthop Surg Res. 2015;10(1) doi: 10.1186/s13018-015-0189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yushan M., Ren P., Abula A., Alike Y., Abulaiti A., Ma C. Bifocal or trifocal (Double-Level) bone transport using unilateral rail system in the treatment of large tibial defects caused by infection: a retrospective study. Orthop Surg. 2020;12(1):184–193. doi: 10.1111/os.12604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li W., Zhu S., Hu J. Bone regeneration is promoted by orally administered bovine lactoferrin in a rabbit tibial distraction osteogenesis model. Clin Orthop Relat Res. 2015;473(7):2383–2393. doi: 10.1007/s11999-015-4270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tetsworth K., Cierny G.R. Osteomyelitis debridement techniques. Clin Orthop Relat Res. 1999;(360):87–96. doi: 10.1097/00003086-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Qin C.H., Zhang H.A., Chee Y.H., Pitarini A., Adem A.A. Comparison of the use of antibiotic-loaded calcium sulphate and wound irrigation-suction in the treatment of lower limb chronic osteomyelitis. Injury. 2019;50(2):508–514. doi: 10.1016/j.injury.2018.10.036. [DOI] [PubMed] [Google Scholar]
- 22.Gauland C. Managing lower-extremity osteomyelitis locally with surgical debridement and synthetic calcium sulfate antibiotic tablets. Adv Skin Wound Care. 2011;24(11):515–523. doi: 10.1097/01.ASW.0000407647.12832.6c. [DOI] [PubMed] [Google Scholar]
- 23.Cooper J.J., Florance H., McKinnon J.L., Laycock P.A., Aiken S.S. Elution profiles of tobramycin and vancomycin from high-purity calcium sulphate beads incubated in a range of simulated body fluids. J Biomater Appl. 2016;31(3):357–365. doi: 10.1177/0885328216663392. [DOI] [PubMed] [Google Scholar]
- 24.Aktuglu K., Gunay H., Alakbarov J. Monofocal bone transport technique for bone defects greater than 5 cm in tibia: our experience in a case series of 24 patients. Injury. 2016;47(Suppl 6):S40–S46. doi: 10.1016/S0020-1383(16)30838-5. [DOI] [PubMed] [Google Scholar]