Abstract
Background:
Dopaminergic medications administered to remedy motor symptoms in Parkinson’s disease are associated with an enhanced risk for impulse control disorders (ICD) and related compulsive behaviors (ICD-RB). Thus, the present study focuses on investigating the gender difference in the prevalence of ICD-RBs in Indian PD patients on dopamine replacement therapy (DRT), its impact on quality of life and to identify ICDs relevant in Indian scenario apart from the criteria set in QUIP-RS.
Method:
This was a hospital-based observational cross-sectional study in which Parkinson’s disease patients attending neurology clinic were included. Complete details of anti-parkinsonian therapy along with demographic and clinical variables were recorded on a predesigned Performa. Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s disease (QUIP), which is a validated quick screening tool, was used to detect ICD-RBs. The relative frequency and comparative impact of ICD on health-related quality of life (QOL) was studied using validated PDQ-39 Questionnaire.
Results:
Out of 102 patients, at least one ICD or ICD-RB was present in 41.19% and ≥2 ICD-RBs were present in 15.59%. At least one ICD was present in 16.67%, any ICD-related compulsive behaviors was present in 34.31% patients. The most common was punding and compulsive medication use (12.75% each), followed by hobbyism (7.84%), compulsive eating (6.86%), pathological gambling (3.92%), and hypersexuality, walkabout, and compulsive shopping (2.94% each). ICDs not classified elsewhere such as trichotillomania were found 3 patients (2.94%). ICD-RBs showed a trend to be more frequent in women (44.82% women vs. 39.39% men). As compared with patients without ICD-RBs, those with ICD-RBs were found to have higher dose of LD and DA and higher Hoehn and Yahr stage. ICD-RBs have a negative impact on the quality of life of Parkinson’s disease patients.
Conclusion:
ICDs and ICD-RBs have been included in the behavioral spectrum of nonmotor symptoms in PD. PD patients are at increased risk of developing ICD-RBs which interfere with important activities and have obligation in ordinary life, leading to legal and psychological consequences with a great impact on QOL.
Keywords: Compulsive behaviors, impulse control disorders and related compulsive behaviors, impulsive-compulsive disorders in Parkinson’s disease, impulse control disorders not classified elsewhere, quality of life
INTRODUCTION
The term impulse control disorder and related behaviors (ICD-RBs) defines a heterogeneous group of complex behavioral disorders characterized by failure to resist the temptation to perform a pleasurable act. The common features of all these are a) impulsiveness (lack of forethought of consequences); b) compulsiveness (performed repetitively and excessively); and c) performed despite the knowledge that they can lead to adverse consequences on oneself or others.[1] Throughout the past decade, it has been well recognized that dopaminergic medications administered to remedy motor symptoms in Parkinson’s disease are associated with an enhanced risk for impulse control disorders and related compulsive behaviors.[2] The spectrum of ICDs reported in Parkinson’s disease includes pathological gambling, compulsive buying, compulsive sexual behavior, binge or compulsive eating, hobbyism, punding, dopamine dysregulation syndrome (DDS), and other unclassified behavioral disorders, with varying prevalence according to regional and cultural differences.[3]
These complications are relatively frequent, affecting 6%–15.5% of patients.[4] Besides a high dose of dopamine (DA) agonists, additional risk factors associated with ICD-RBs in PD include young age at PD onset, male gender, depression, personal or family history of addictive behaviors, and genetic factors.[5] In the context of the potential genetic and environmental factor affecting the expression of ICD-RBs, there is limited data on the prevalence of ICDs in PD from Asian countries. No previous studies have examined the impact of ICDs on Quality of life (QoL) of PD patients in north Indian population. Thus, the present study aimed to investigate the gender difference in the prevalence of ICD-RBs in Indian PD patients on dopamine replacement therapy (DRT) and identify the additional ICDs relevant in the Indian scenario apart from the criteria set in QUIP-RS and the possible risk factors associated with it and its impact on quality of life.
MATERIALS AND METHODS
This was a hospital-based observational cross-sectional study conducted in the Department of Neurology, Dayanand Medical College and Hospital, Ludhiana (Punjab) a tertiary health care center in north India, after obtaining clearance from the Institutional Ethics Committee. All adult patients with Idiopathic Parkinson’s disease (diagnosed on the basis of United Kingdom Parkinson’s Disease Society Brain Bank Criteria) attending neurology clinic between 1st January-31st December, 2018 during their regular outpatient visits, who were on treatment with dopamine replacement therapy for more than 6 months with a documented response and whose treatment was not modified based on prior reporting of ICD-RBs were included in the study. Patient with cognitive abnormality (mini-mental state examination, MMSE < 24), or those on any psychiatric medications, secondary Parkinson disease (Multiple system atrophy, Progressive supranuclear palsy, corticobasal degeneration) and those not consenting were excluded from the study.
Data collection and analysis
The following demographic and clinical variables were recorded on a predesigned Structured Performa: age, sex, marital status, education status, socioeconomic status, age at onset, duration of disease, and Modified Hoehn and Yahr scale (H and Y) score for staging of disease. Personal history and substance-related addiction (alcohol/smoking) history was recorded according to DSM-IV criteria.
All participants were informed that the primary purpose of the study was to examine the frequency of ICD-RBs in PD and their association with PD medications. Complete details of anti-parkinsonian therapy including individual drugs were recorded. Levodopa (LD), dopamine agonist (DA), and levodopa equivalent dose (LED) were then calculated in milligrams according to the conversion factor of the individual drugs.
QUIP-RS questionnaire
The QUIP is a screening instrument with high discriminate validity for ICD-RBs in PD and covers a comprehensive range of impulsive-compulsive behaviors.[6] Two independent professionals translated the questions and response categories of QUIP-RS scale individually into Hindi and Punjabi. Another professional translated this questionnaire back into English to check for the discrepancies between Hindi/Punjabi version and the original questionnaire. After a careful review and a few changes, the provisional version of the questionnaire was finalized.
In the next phase, this questionnaire was pilot-tested by the administration to a sample of ten patients of PD and ten healthy individuals as controls (the age-gender matched family members of patients). The questionnaire in English was completed with the help of the doctor and the Hindi/Punjabi version by the patient himself/herself. The comparison of QUIP-RS in English and Hindi/Punjabi in this pilot group yielded similar results. After pilot testing, a few more changes were made and then a final version of the scale was prepared and used in the study.
After taking informed consent, patients and their informants (spouse or primary caregiver) were given the questionnaire in the language of choice (English/Punjabi/Hindi) and were instructed to answer questions based on behavior that occurred any time after the diagnosis of PD and that had lasted at least 4 consecutive weeks.
Impulse control disorders and related behaviors (ICD-RB) were categorized into three categories. 1) Impulse control disorder (ICD) that included pathological gambling, hypersexual behavior, buying, and eating behaviors. These were accessed in Section 1 of the QUIP. ICD-related compulsive behaviours (ICRB) included punding, hobbyism, walkabout, and compulsive medication use. Section 2 and 3 of QUIP were used to access these. 3) Impulse control disorders not classified elsewhere.
Pathological gambling was defined according to DSM-IV as persistent and recurrent maladaptive gambling behavior indicated by features such as preoccupation with gambling; increasing amounts of money; unsuccessful attempts to control; restlessness or irritability when cutting down; lying to others about gambling; jeopardizing relationships, work, or education; and relying on others for money (at least five criteria required).[7] Compulsive eating was characterized by eating greater amounts of food than is necessary to alleviate hunger, leading to harmful weight gain.[8] Compulsive buying was defined by the presence of repetitive impulsive and excessive buying of goods that are not needed and that may lead to financial stress.[9] Hypersexuality was a behavioral disorder characterized by increased preoccupation with sexual thoughts, excessive demands for sex from partners, increased use of pornography, seeking out prostitutes, engaging in exhibitionism and paraphilia.[10] Punding is a stereotypical motor behavior in which there is an intense fascination with repetitive handling and examining of mechanical objects.[11] There is a continuum of punding behavior ranging from excessive “hobbyism” to prolonged disabling highly stereotyped ritualistic behavior. Activities include collecting or hoarding items, cleaning, repairing things, gardening, writing and categorizing information, artistic drawing or craft-making, singing or playing a musical instrument, playing cards, fishing, and excessive computer and Internet use.[12] Dopamine dysregulation syndrome (DDS) refers to the compulsive use of dopaminergic medications well beyond the dose needed to optimally control motor disability and in the face of a mounting number of harmful physical, psychiatric, and social sequel.[13]
Impulse-control disorder not elsewhere classified
Certain presentations of Impulse control disorders which can be relevant in the Indian population and have yet not been explored such as body-focused repetitive behaviors (trichotillomania, hair nibbling, skin picking, nail-biting, cheek biting), hypergraphia, and pyrophilia in patients with Parkinson’s disease were studied with the help of a Questionnaire as a part of this research [Annexure 1].[14]
Annexure l.
| Impulse control disorders not elsewhere classified | |
| 1. Body-focused repetitive behavior | |
| • Trichotillomania (hair pulling) | Yes/No |
| • Trichophagia (hair nibbling) | Yes/No |
| • Trichotemnomania (hair cutting) | Yes/No |
| • Dermatillomania (skin picking) | Yes/No |
| • Dermatophagia (skin nibbling) | Yes/No |
| • Onychotillomania (nail picking) | Yes/No |
| • Onychophagia (nail biting) | Yes/No |
| • Morsicatio labiorum (inner lip biting) | Yes/No |
| • Morsicatio buccarum (cheek biting) | Yes/No |
| • Morsicatio linguarum (tongue biting) | Yes/No |
| • Rhinotillexomania (compulsive nose picking) | Yes/No |
| 2. Hypergraphia | Yes/No |
| 3. Pyrophilia | Yes/No |
| 4. Kleptomania | Yes/No |
| 5. Utilization behavior | Yes/No |
| 6. Any other impulse control disorder (which fulfills the criteria of I CD as per definition) |
Impact of Impulse control disorders on the quality of life (QOL) of PD patients
The relative frequency and comparative impact of ICD on health-related quality of life (QOL) was studied a using validated PDQ-39 Questionnaire.[15]
Statistical analysis
At the end of study period, the data was analyzed using appropriate statistical parameters. The mean and standard deviation were used for quantitative variables. Prevalence of impulse control disorders (ICD) and related compulsive behaviors (ICRB) and together as ICD-RB was calculated as percentage. Association of various risk factors and parameters with Impulse control disorders in PD was analyzed using Chi-square and Fisher’s exact tests.
The continuous descriptors and domains of quality of life scores were tested for differences of means between different ICD-RB groups using independent sample t-test and further validated through Wilcoxon’s rank sum test. P value <0.05 was considered significant.
RESULTS
Out of the 124 patients of PD visiting the neurology OPD during the study period, 102 patients were included in the study as 18 were diagnosed as secondary Parkinson’s disease on subsequent work-up and 4 did not consent to share information about their ICD. The cohort included 64 males (62.7%) and 38 females (37.2%). The mean age of the participants in the study was 60.1 ± 9.7 years. The mean duration PD was 3.92 ± 2.9 years (range, 9 months–8 years). The mean H and Y stage was 2.2 ± 0.83. All patients were taking either levodopa (LD) or dopamine agonists (DA) or both. The mean levodopa equivalent dose (LED) was 398.27 ± 176.16 mg and DA dose was 25.78 ± 51.55 mg. In our study, 57 patients (55.8%) had urban background and the mean years of education were 10.2 years (range 4–22). In our cohort, 98.3% were married and living with their spouse.
Out of 102 patients, at least one impulse control disorders and related behaviors i.e. either ICD or ICRB was present in 41 patients (40.19%) and ≥2 ICD RBs were present in 16 (15.68%). Among these, at least one Impulse control disorder (ICD) was present in 17 (16.67%) and any ICD-related compulsive behaviors (ICRB) was present in 35 patients (34.31%). Figure 1 shows the distribution of ICDs in cohort of patients.
Figure 1.
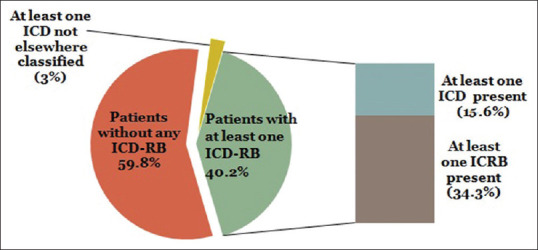
Distribution of the prevalence of Impulse control disorders and related behaviors in PD patients
ICD-related compulsive behaviors (ICRBs) were more common in PD patients than ICDs [Table 1]. ICRBs in the cohort in decreasing order of frequency were compulsive medication use and punding (12.75% each), compulsive hobbyism (7.84%), and walkabout (2.94%). Impulse control disorders present in the cohort in decreasing order of frequency were compulsive eating (6.86%), pathological gambling (3.92%), and hypersexuality and compulsive shopping (2.94% each). A new class of ICDs that have not been classified elsewhere including body-focused repetitive behavior was also studied and three patients (2.94%) were found to have trichotillomania.
Table 1.
Gender distribution of Impulse control disorders and related behaviors
| Parameter (n=41) | Male (25/68) | Female (16/34) |
|---|---|---|
| Gambling | 3 | 1 |
| Hypersexuality | 3 | 0 |
| Compulsive shopping | 1 | 2 |
| Compulsive eating | 4 | 3 |
| Punding | 7 | 6 |
| Compulsive hobbyism | 5 | 3 |
| Walkabout | 3 | 0 |
| Compulsive medication use | 8 | 5 |
| ICD not elsewhere classified | 2 | 1 |
Table 1 shows the gender distribution of ICD-RBs, with a general trend of ICD-RBs being more prevalent in females (42%) than males (39%). Punding and compulsive medication use were more common in females, whereas hypersexuality and walkabout were only seen in males.
On univariate analysis, there was a significant association of the presence of addictive behavior and substance abuse (alcohol intake, smoking) with incidence of ICD-RBs (P = 0.03). The disease factors associated with impulse control disorders in patients with PD were the severity (P = 0.001) and duration of the disease (P = 0.05). In addition, there was direct relation of occurrence of ICD to the total levodopa equivalent dose (P = 0.001) and dopamine agonist dose (P = 0.007), as shown in Table 2. There was no difference in the demographic factors (mean age, socioeconomic status, education, marital status) between the patients with or without ICD-RBs.
Table 2.
Demographic and clinical characteristics and associated risk factors in patients of PD for Impulse control disorders and related behaviors
| Demographic and clinical characteristics | All patients (n=102) | Without ICD-RB (n=61) | With ICD-RB (n=41) | P |
|---|---|---|---|---|
| Gender: Male-Female | 64 | 39 | 25 | 0.83 |
| 38 | 22 | 16 | ||
| Addiction behavior | 23 | 10 | 13 | 0.03 |
| Age at study (mean age, years) | 60.7 ± 9.7 | 57.5 | 54 | 0.06 |
| Duration of disease (years) | 3.92 | 3.47 | 4.6 | 0.05 |
| Total LED dose (mg) | 398.2 ± 176 | 343.9 | 479.1 | 0.001 |
| DA equivalent dose (mg) | 25.7 ± 51.5 | 14.71 | 42.2 | 0.007 |
| Hoehn-Yahr stage “On” | 2.2 | 2.0 | 2.4 | 0.001 |
The quality of life was much worse in patients with any ICD-RB than those without any ICD-RBs with the mean quality of life (QOL) score in patients with or without any ICD-RB being 22.40 ± 11.79 and 32.64 ± 14.14, respectively [Table 3]. This difference was statistically significant (P = 0.001). The presence of ICD-RB significantly affects all components of the scale. Domains of emotional well-being, cognitive function, communication, bodily discomfort, and mobility were worse in patients with any ICD-RB than those without any ICD-RB.
Table 3.
Summary of PDQ39 scale for Quality of life assessment in PD patients with ICD-RBs
| QOL | No- ICD-RB (n=61) | With ICD-RB (n=41) | P |
|---|---|---|---|
| PDQ39 mean score | 22.40 ± 11.79 | 32.64 ± 14.14 | 0.001 |
| Mobility | 23.4 | 37.1 | 0.005 |
| Activities of daily living | 25.8 | 38.2 | 0.001 |
| Emotional well being | 27.3 | 38.7 | 0.008 |
| Sitgma subscore | 29.9 | 40.8 | 0.05 |
| Social support | 15.1 | 20.7 | 0.05 |
| Cognitive impairment | 18.0 | 27.5 | 0.007 |
| Communication | 18.8 | 27.8 | 0.02 |
| Bodily discomfort | 21.7 | 30.6 | 0.006 |
DISCUSSION
Parkinson’s disease (PD) being a neurodegenerative disorder prominently affects motor function, but may also have multiple nonmotor manifestations. As Parkinson’s disease is largely due to a loss of dopamine-secreting neurons, pharmacologic dopamine replacement therapy (DRT) is the cornerstone of Parkinson’s disease treatment. However, over time, a proportion of patients develop complications from pharmacologic stimulation of dopamine receptors and anti-parkinsonian drugs also provoke impulse-control disorders and related behaviors which in itself lead to significant disability.
Impulse control disorders (ICDs) are defined as a failure to resist an impulse, drive or temptation to perform a harmful act. They are under-recognized and under-treated in routine clinical practice. Most patients do not spontaneously offer information about ICD-RBs, either because of shame, social stigma attached to them or because they do not understand that could be related to PD and its treatment. Early detection of ICD-RBs is crucial and all patients should be questioned directly about such behavior.
Studies of different multi-ethnic populations report varying frequencies of impulse control disorders, with prevalence numbers vary between 6.6% and 35% in studies conducted in the Western or Asian countries.[16] This may be due to the potential influence of genetic and environmental factors along with cultural and social factors that affect the expression of ICD-RBs. In addition, there are methodological differences as some studies include ICDs separately or combined (ICD-RBs, ICDs and ICRBs) as a group.
We found a higher prevalence of ICD-RBs, about 40.19% and ≥2 ICDs in 15.68%. The relatively higher frequency of ICDs in this study may not only be because of social-cultural factors but because of the use of a highly validated screening instrument (QUIP-RS); second, we combined both ICDs and ICRBs and also included some ICDs not classified elsewhere.
Many studies have estimated the prevalence of hypersexuality between 2.6% and 13% and that of pathological gambling between 1.3% and 9.3%.[17] The low prevalence of hypersexuality (2.94%) and pathological gambling (3.92%) in our study can be due to the social stigma related to these behaviors and the fact that in our country gambling is illegal, due to which the patient may not feel free to reveal it. Similarly, in an Indian study by Sharma et al. at least one ICD-RB was seen in 42.8% patients, as in our study.[18]
There is limited data that emphasizes gender disparities in the prevalence of ICD in patients with Parkinson’s disease. ICD-RBs in this study showed a trend to be more frequent in women (42% women vs. 39% men). Punding and compulsive eating showed a trend to be more frequent in women, while hypersexuality and compulsive medication use showed a trend to be higher in men. Historically, gender-related differences in addictions have been understudied. Gender differences are present in personality traits and behaviors, such as impulsivity, that have been associated with addictions (both substance and non-substance). Although hormone fluctuations in women are rarely investigated with respect to treatments, levels of estrogen and progesterone may have large impacts on the efficacies of behavioral or pharmaceutical interventions. Routine considerations of gender differences in preclinical and clinical research settings will further help advance translational efforts and improve prevention, treatment, and policy initiatives.
The most relevant finding of this study was reporting the prevalence of certain presentations of Impulse control disorders which can be relevant in the Indian population and have yet not been explored. “Impulse-control disorder not elsewhere classified” such as body-focused repetitive behavior was studied with a Questionnaire as a part of this research and trichotillomania was found in about 3% of the patients with PD.
In this study, the presence of history of addiction or substance abuse (alcohol intake and smoking), higher Hoehn and Yahr Staging, and exposure to dopamine agonists were significant of risk factors associated with the occurrence of ICDs. This warrants the screening of PD patients for ICD-RBs, especially those with severe disease and on high doses of anti-parkinsonian therapy. Compared with patients without ICD-RBs, those with ICD-RBs were found to be on higher dose of LD and DA, but it is still open for debate that does PD itself confer increased risk of developing ICD-RB as not all patients were on dopamine agonists. In addition, in our study, about 12.75% patients had compulsive medication use which may have led to intake of unprescribed and higher doses of dopaminergic drugs, thus being associated with higher incidence of ICDs.
High prevalence of ICD-RBs in PD patients is reported in the literature but there are no previous studies that have examined the effects of ICDs on Quality of life (QOL) of PD patients. ICD-RBs have a negative impact on the quality of life of Parkinson’s disease patients with the total quality of life score being worse in patients with any ICD-RB. Limitations of our study are that there may be other ICDs, yet not classified and not included in our study. Second, UPDRS score was not analyzed separately. Third, the duration of treatment that could affect the occurrence of ICD was not studied. Last, this was a small-scale single-centre study; hence, large-scale longitudinal studies are needed in future to better identify patients who are at increased risk of ICD and develop therapeutic options.
In conclusion, the findings of this study state a prudent use of dopamine agonists in populations vulnerable to have impulse disorders. In addition, periodic screening for the presence of ICDs in Parkinson’s disease patients is warranted as ICD-RBs have personal, family, psychosocial, financial, and medical consequences. Education about ICDs and modification of treatment can help to improve the quality of life and longevity. Large-scale longitudinal studies are needed in future to better identify patients at increased risk of developing ICD and therapeutic options.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Voon V, Sohr M, Lang AE, Potenza MN, Siderowf AD, Whetteckey J, et al. Impulse control disorders in Parkinson disease: A multicenter case-control study. Ann Neurol. 2011;69:986–96. doi: 10.1002/ana.22356. [DOI] [PubMed] [Google Scholar]
- 2.Driver-Dunckley E, Samanta J, Stacy M. Pathological gambling associated with dopamine agonist therapy in Parkinson’s disease. Neurology. 2003;61:422–3. doi: 10.1212/01.wnl.0000076478.45005.ec. [DOI] [PubMed] [Google Scholar]
- 3.Callesen MB, Scheel-Krüger J, Kringelbach ML, Møller A. A systematic review of impulse control disorders in Parkinson’s disease. J Parkinsons Dis. 2013;3:105–38. doi: 10.3233/JPD-120165. [DOI] [PubMed] [Google Scholar]
- 4.Antonini A, Barone P, Bonuccelli U, Annoni K, Asgharnejad M, Stanzione P. ICARUS study: Prevalence and clinical features of impulse control disorders in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2017;88:317–24. doi: 10.1136/jnnp-2016-315277. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence AJ, Blackwell AD, Barker RA. Predictors of punding in Parkinson’s disease: Results from a questionnaire survey. Mov Disord. 2007;22:2339–45. doi: 10.1002/mds.21702. [DOI] [PubMed] [Google Scholar]
- 6.Weintraub D, Hoops S, Shea JA, Lyons KE, Pahwa R, Driver-Dunckley ED, et al. Validation of the questionnaire for impulsive-compulsive disorders in Parkinson’s disease. Mov Disord. 2009;24:1461–7. doi: 10.1002/mds.22571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giladi N, Weitzman N, Schreiber S, Shabtai H, Peretz C. New onset heightened interest or drive for gambling, shopping, eating or sexual activity in patients with Parkinson’s disease: The role of dopamine agonist treatment and age at motor symptoms onset. J Psychopharmacol. 2007;21:501–6. doi: 10.1177/0269881106073109. [DOI] [PubMed] [Google Scholar]
- 8.Nirenberg MJ, Waters C. Compulsive eating and weight gain related to dopamine agonist use. Mov Disord. 2006;21:524–9. doi: 10.1002/mds.20757. [DOI] [PubMed] [Google Scholar]
- 9.Dittmar H. Compulsive buying- a growing concern.An examination of gender, age and endorsement of materialistic values as predictors? Br J Psychol. 2005;96:467–91. doi: 10.1348/000712605X53533. [DOI] [PubMed] [Google Scholar]
- 10.Cossu G, Rinaldi R, Colosimo C. The rise and fall of impulse control behavior Disorders. Parkinsonism Relat Disord. 2018;46:S24–9. doi: 10.1016/j.parkreldis.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 11.Vela L, Martínez Castrillo JC, García Ruiz P, Gasca-Salas C, Macías Macías Y, Pérez Fernández E, et al. The high prevalence of impulse control behaviors in patients with early-onset Parkinson’s disease: A cross-sectional multicenter study. J Neurol Sci. 2016;368:150–4. doi: 10.1016/j.jns.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Garcia Ruiz PJ, Martinez Castrillo JC, Alonso-Canovas A, Herranz Barcenas A, Vela L, Sanchez Alonso P, et al. Impulse control disorder in patients with Parkinson’s disease under dopamine agonist therapy: A multicentre study. J Neurol Neurosurg Psychiatry. 2014;85:841–5. doi: 10.1136/jnnp-2013-306787. [DOI] [PubMed] [Google Scholar]
- 13.O’Sullivan SS, Evans AH, Lees AJ. Dopamine dysregulation syndrome: An overview of its epidemiology, mechanisms and management. CNS Drugs. 2009;23:157–70. doi: 10.2165/00023210-200923020-00005. [DOI] [PubMed] [Google Scholar]
- 14.Grant JE, Levine L, Kim D, Potenza MN. Impulse control disorders in adult psychiatric in patients. Am J Psychiatry. 2005;162:2184–8. doi: 10.1176/appi.ajp.162.11.2184. [DOI] [PubMed] [Google Scholar]
- 15.Weintraub D, Mamikonyan E, Papay K, Shea JA, Xie SX, Siderowf A. Questionnaire for impulsive-compulsive disorders in Parkinson’s disease—Rating scale. Mov Disord. 2012;27:242–7. doi: 10.1002/mds.24023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weintraub D, Koester J, Potenza MN, Siderowf AD, Stacy M, Voon V, et al. Impulse control disorders in Parkinson’s disease: A cross-sectional study of 3,090 patients. Arch Neurol. 2010;67:589–95. doi: 10.1001/archneurol.2010.65. [DOI] [PubMed] [Google Scholar]
- 17.Sarathchandran P, Soman S, Sarma G, Krishnan S, Kishore A. Impulse control disorders and related behaviors in Indian patients with Parkinson’s disease. Mov Disord. 2013;28:1901–2. doi: 10.1002/mds.25557. [DOI] [PubMed] [Google Scholar]
- 18.Sharma A, Goyal V, Behari M, Srivastva A, Shukla G, Vibha D. Impulse control disorders and related behaviors (ICD-RBs) in Parkinson’s disease patients: Assessment using “Questionnaire for impulsive-compulsive disorders in Parkinson’s disease” (QUIP) Ann Indian Acad Neurol. 2015;18:49–59. doi: 10.4103/0972-2327.144311. [DOI] [PMC free article] [PubMed] [Google Scholar]


