Abstract
Objective:
Our aim was to evaluate High Frequency Ultrasonography as a tool for diagnosis in patients withcarpal tunnel syndrome in comparison with electrophysiological study.
Methods:
Thirty- one patients [56 hands] with CTS and twenty-five asymptomatic controls [50 hands] were assessed and underwent ultrasonography of the wrists and electrophysiological testing. Data from the patient and the control groups was compared for both the investigations to determine the CTS and the grade of severity.
Results:
There was a high degree of correlation between the conduction abnormalities of the median nerve as detected by electrodiagnostic tests, historic and objective scale [Hi-Ob] and the measurement of the cross-sectional area of the nerve by US (P < 0.05). A cut-off point of 0.88 mm2 for the mean cross-sectional area of the median nerve was found to be the upper limit for normal values. Compared to Ultrasonography which found one hand negative, six hands (10%) were negative on the electrophysiological tests. Using critical CSA value of 1.0 mm2 in these CTS cases by US with sensitivity and specificity of 100% and 88%. Based on the results of this study, ultrasonography of wrist is another useful tool along with nerve conduction studies as per sensitivity and specificity patterns found in our study in diagnosis of carpal tunnel syndrome.
Conclusion:
High-frequency US examination of the median nerve and measurement of its cross-sectional area can be strongly considered as useful diagnostic diagnostic modality for the evaluation of CTS along with nerve conduction studies. In addition to its high diagnostic accuracy it is able to define the cause of nerve compression, aids treatment planning and provides a reliable method to follow response to therapy.
Keywords: Carpal tunnel syndrome (CTS), nerve conduction study, ultrasonography (USG)
INTRODUCTION
Carpal tunnel syndrome, the entrapment neuropathy of median nerve at wrist is one of the most come focal compressive mono neuropathies.[1,2,3,4] Carpal tunnel is located at base of the palm, just distal to the distal wrist crease. The tunnel is bounded superficially by the transverse carpal ligament (the flexor retinaculum) and laterally and inferiorly by carpal bones with their fibrous coverings and interosseous ligament. In the tunnel, median nerve is predisposed to damage by compression by local trauma, overuse of hand and wrist, improper position of hand and local constriction, leading to recognized cause of work disability. CTS is more prevalent amongst women (about 3%) compared to men (2%) with peak prevalence in women older than 55 years of age. Various conditions associated with CTS include pregnancy, amyloidosis, inflammatory arthritis, hypothyroidism, diabetes mellitus, acromegaly etc., Various activities and postures precipitate CTS symptoms like driving, typing on computer, writing for long hours, making dough, milking of cows especially in Indian population, wringing of clothes etc., Common symptoms of CTS include pain, paraesthesias, with nocturnal exacerbations, sometimes associated with sensory loss in the distribution of median nerve i.e. thumb and lateral two and half fingers and wasting of thenar muscles in advanced cases. Therefore it’s important to diagnose and treat this condition early to prevent irreversible median nerve damage. Besides clinical diagnosis, nerve conduction studies are very useful in diagnosis of CTS and highly specific,[5] but have substantial false negative rate of 10-20% and false positive in some cases.[6,7] Though nerve conduction studies often indicate the level of the lesion, but do not give the spatial information about the nerve or its surroundings. Recently MRI imaging[8] and ultra-sonography[9,10,11,12] have shown to be of value in diagnosis of CTS. Both have an advantage over nerve conduction study in that they provide information about the possible causes of CTS, such as rheumatoid arthritis, tenosynovitis or synovitis of the wrist[13] Imaging criteria for MRI and sonography for carpal tunnel syndrome appeared to be the same in most studies.[1,14,15] Compared to MR imaging, sonography has the advantages as it has lower cost, takes shorter time, possibility of sonography guided intervention and treatment. Although few studies have been done to assess the value of quantitative sonography in CTS diagnosis,[3,16] these studies were mainly concerned with investigating the sonographic features of median nerve as well as carpal tunnel. Therefore we performed this study to evaluate the application of ultrasonography (US) in Asian patients with CTS using B mode US as a tool for diagnosis in comparison with nerve conduction studies.
MATERIALS AND METHODS
Patients
This was a prospective cross-sectional, blinded case–control study. The study population was of two types, one was of patients with symptoms suggestive of CTS, who were enrolled prospectively from the neurology outpatient department of Postgraduate Institute of Medical Education and Research, Chandigarh, from July 2005 to December 2006. Second population was of controls, consisting of asymptomatic people. Total 45 patients were screened, after excluding 9 patients as they did not meet the inclusion criteria, 36 patients were planned to enroll in the study. During enrollment process, five out of 36 patients were excluded as two patients were found to have Diabetes mellitus and three had hypothyroidism. Total 31 patients (56 hands) were included in the study, two patients had amputation of index finger and one had amputation of ring finger of one hand. Two had trauma over the wrist of one hand each and one was uncooperative and didn’t allow to examine the other hand, therefore six hands were excluded and 56 hands were taken for the study. Ethical clearance was taken from the Institutional Ethics Committee.
Definition of cases and data collection at initial evaluation
Diagnosis of CTS was based on the American Academy of Neurology clinical diagnostic criteria (1993)[17] summarized here: paraesthesia; pain; swelling, weakness or clumsiness of the hand provoked or worsened by sleep; sustained hand or arm position; repetitive action of the hand or wrist that is mitigated by changing posture or by shaking of the hand; sensory deficit or hypotrophy of the median innervated thenar muscle; symptoms elicited by the Phalen test (1 min passive forced flexion of the wrist), performed on each patient.
A detailed clinical history, a careful examination and extended neurophysiological evaluation was performed in all patients. Laboratory investigations to diagnose any secondary cause for CTS were done. Patients with only idiopathic CTS (with no aetiological factors) were included in the study. Patients with trauma to wrist and or deformity, clinical examination suggestive of generalized neuropathy or radiculopathy, patients treated previously for CTS using steroid injection or surgical therapy, pregnant patients with carpal tunnel syndrome and patients with systemic disease like hypothyroidism and rheumatoid arthritis etc., were excluded from the study.
Control group
Twenty-five (50 hands) healthy subjects were enrolled in the study with no sign and symptoms of CTS with normal neurological and medical examination. The control subjects were either from the healthy subjects accompanying the patients during their visit to the hospital or from hospital staff. They were subjected to full neurological and medical examination to verify their normality. In addition, they were subjected to the same investigative protocol as for patients after informed consent.
Patient-oriented data
Historic and objective scale (Hi-Ob)
Historic and objective scale (Hi-Ob) of CTS was used to determine the severity of clinical CTS.[18] It included the two measures, the first measure was a score (Hi-Ob) determined by clinical history and objective findings: 1) nocturnal paraethesias only, 2) nocturnal and diurnal paraethesias, 3) sensory deficit, 4) hypotrophy and motor deficit of the median innervated thenar muscles and 5) wasting of median innervated thenar muscles. The second measure of the scale was evaluated by patient oriented measurements. The presence or absence of pain was taken as dichotomous categoric score obtained from the patients with the forced choice answer (yes or no). Therefore, the Hi-Ob score was compared with or without pain variable. All clinical diagnosed CTS patients were subjected to both nerve conduction studies and wrist sonography. Both studies were done within seven days of period by different two examiners. The sonographer was blinded to the electrophysiological findings as well as the clinical history and symptoms of the patients. He was not supposed to ask the history from patients as well as controls.
Electrodiagnostic evaluation
We followed American Association of Electrodiagnostic Medicine recommendations and electrodiagnostic studies were performed for all subjects included in this study according to the protocol[17] by the using a Medtronic Keypoint Machine. All testing was done in the same room and in similar temperature conditions. We performed standard tests i.e., median sensory nerve conduction velocity in two-digit/wrist segments and median distal motor latency from the wrist to the thenar eminence, along with comparative median/ulnar sensory studies. Nerve stimulation was done from equivalent distance for both ulnar and median nerves and recording electrode was placed on 4th digit for ulnar and 2nd digit for median sensory conduction studies respectively.[19] Measurements performed and cut-off points or normal values used in our study were as follows- (1) Median nerve distal sensory latency, upper limit of normal 3.6 ms, (2) Difference between the median and ulnar nerve distal sensory latencies, upper limit of normal 0.4 ms, (3) Distal motor latency over the thenar, upper limit of normal 4.3 ms,(4) Median motor nerve conduction velocity, lower limit of normal 49 m/s, (5) Median sensory nerve conduction velocity, lower limit of normal 49 m/s.[19] The second lumbrical- interosseus distal motor latency difference was not measured in our study. Patients who were found to have CTS on nerve conductions studies, underwent nerve conductions of peroneal, tibial and sural nerves. All patients who had DM, hypothyroidism or connective tissue disorder were excluded. Patients with symptoms suggestive of cervical myelopathy, with history of neck pain and radiating pain were not enrolled for the study. In some selected cases, cerival spine X ray and MRI cervical spine was performed and were not considered for the study. The severity of electrophysiological CTS impairment was assessed according to the classification reported by Padua.[20] CTS hands were divided into six groups on the basis of neurophysiological findings on all tests:
Negative: normal findings on all tests.
Minimal: abnormal segmental or comparative tests only.
Mild: abnormal digit/wrist sensory nerve conduction velocity and normal distal motor latency.
Moderate: abnormal digit/wrist sensory nerve conduction velocity and abnormal distal motor latency.
Severe: absence of sensory response and abnormal distal motor latency.
Extreme: absence of motor and sensory responses.
Sonography
Along with detailed electrophysiology studies, all patients of suspected CTS underwent high-resolution real-time sonography of the carpal tunnel (both hands) using an ATL HDI 3500 [Philips-WA] coloured doppler ultrasound machine with a 5-12 MHz broad band linear array transducer. Sonographic examination was done either on the same day or within 7 days of the electro physiological study. The sonographer was the neurologist only as in our department nerve USG and Doppler test are performed by the neurologist only, they get training during their DM tenure in the department. The sonographic examination was performed with the patient seated in a comfortable position facing the sonographer, with the forearm resting on the table and the palm facing up in the neutral position. The volar wrist crease was used as an initial external reference point, with subsequent modifications during scanning using carpal bony landmarks and internal reference points. The full course of the median nerve in the carpal tunnel was assessed in both transverse and longitudinal planes. The median nerve is located superficial to the echogenic flexor tendons and its size, shape, echogenicity and relationship to the surrounding structures and overlying retinaculum were noted. The amount of synovial fluid and the presence or absences of masses were noted. The continuity of the median nerve and any area of constriction were assessed in both the longitudinal and transverse planes. Measurements were taken for the median nerve at the carpal tunnel inlet proximally i.e. pisiform bone and at the carpal tunnel outlet i.e. hamate bones distally. The mean cross-sectional area of the median nerve was measured by tracing with electronic calipers around the margin of the nerve at the time of sonography (direct tracing). The flattening ratio (defined as the ratio of the major axis of the median nerve to its minor axis) was also assessed at the mid portion of carpal tunnel. Measurement of the antero-posterior dimension of the carpal tunnel was also assessed at the midpoint of the carpal tunnel at the level of the distal margin of pisiform bone. Median nerve measurements were taken for both patients and control groups. Following parameters were assessed during sonography of wrist- 1. Cross section area of median nerve at carpal tunnel inlet, 2. Flattening ratio [ratio between long axis and transverse axis], 3. Antero-posterior diameter of the carpal tunnel, 4. Normal anatomy of median nerve in both long and transverse axis at wrist.
Statistical analysis
Statistical analysis was performed using the Student’s t-Test and one-way ANOVA to test differences between groups’ mean. X2 and the Fisher Exact were used for the testing the association between Qualitative variables. The cut-off point for the CSA, FR and APD were calculated taking the upper limit of the 95% confidence interval for the control. Correlation was tested using Pearson’s correlation coefficient. In all tests the P value was set at 0.05 and data manipulation and analysis were performed using the SPSS version 11.5. Tests of normality were performed beforehand.
RESULTS
Total 31 patients (56 hands) and 25 controls (50 hands) were enrolled for the study. There were 22 females and 9 males in patient group and 18 females and 7 males in control group, with mean age of 44.72 ± 13.04 and 40.68 ± 13.19 respectively. All the baseline parameters were comparable between the two groups. Fifty six hands with carpal tunnel syndrome were studied. Out of these 56 hands, positive Phalen’s sign was present in 28 hands (50%) while Tinel’s test was positive in 28 hands (50%).
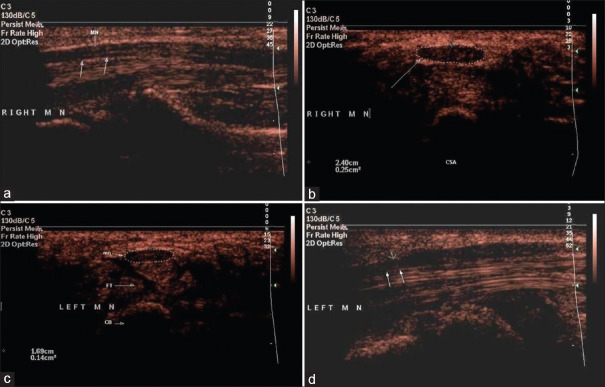
In comparison with the control group [Figure 1a], US assessment of the median nerve in the patients group showed that the swelling of the median nerve at the inlet ppears to be the most reliable criterion for diagnosing CTS [Figure 1b]. The US images also demonstrated other changes in the median nerve, such as marginal effacement from oedema and longitudinal irregularities [Figure 1c]. Longitudinal evaluation of the abnormal nerve, especially in those patients with moderate to severe abnormal NCS results, frequently revealed marked dilatation proximal to the carpal ligament with a sharp anterior calibre change [Figure 1d]. Six hands (10%) were negative on the electrophysiological tests while only one hand was found negative on the US assessment. One of control hands showed a bifid median nerve.
Figure 1.
(a). Longitudinal scan showing normal median nerve. (b). Transverse scan showing enlarged (swollen) median nerve. (c). Transverse scan showing flattening of the median nerve. FR-Flexor Retinaculum, MN-Median Nerve, FT-Flexor Tendons and CB- carpal bone. (d). Longitudinal scan showing indentation (notching) of the median nerve by the flexor retinaculum anteriorly (arrow)
Statistical analysis was done using the upper limit of 95% confidence interval to calculate the cut-off point, its specificity and sensitivity, for a pathological mean cross-sectional area of the median nerve that discriminates between cases versus the control group [Table 1]. This was revealed to be 0.88 mm2. Similarly the cut-off point for the flattening ratio was found to be 3.53 and AP diameter was 10.8 mm2. The same was done when choosing the cut-off points that discriminate between the mild and moderate groups; as well as between the moderate and severe groups. This study revealed that 1.3-1.6 mm2 were the best cut-off points to discriminate between both grades respectively. On comparison different variable means shown significant difference [P < 0.05] between two groups [Table 1]. The electrophysiological abnormality in shown in the table [Table 2].
Table 1.
Ultrasonography abnormalities in patients and comparison between two groups (n-56 hands)
| Ultrasonographic abnormalities | Number of abnormal hands | Specificity | Sensitivity |
|---|---|---|---|
| CSA mm2 [0.88] | 55 [98.21%] | 74.00 | 98.21 |
| FR [>3.53] | 18 [32.14%] | 64.00 | 32.14 |
| APD mm [>10.8] | 44 [78.57%] | 62.00 | 78.57 |
| Ultrasonographic parameter | Test group (56 hands) (Mean±SD) | Control group (50 hands) (Mean±SD) | P |
| CSA [mm2] | 1.46±0.45 | 0.079±0.018 | 0.0001 |
| FR | 3.36±0.56 | 3.31±0.78 | 0.726 |
| APD [mm] | 12.3±1.9 | 1.03±0.17 | 0.0001 |
CSA- Cross section area, FR- Flattening ratio, APD- Antero-posterior diameter
Table 2.
Electrophysiological abnormalities in Median nerve in patients and controls
| Electrophysiological Parameter [abnormal] | TEST n=56 | Control n=50 | Sn [%] | Sp [%] | NPV [%] | PPV [%] |
|---|---|---|---|---|---|---|
| MDL | 23 | 0 | 41.07 | 100 | 100 | 60.24 |
| MCV | 14 | 5 | 25.00 | 90.00 | 73.68 | 51.72 |
| MLD | 46 | 7 | 82.14 | 85.71 | 97.56 | 75.38 |
| SDL | 40 | 1 | 71.42 | 98.00 | 97.56 | 75.36 |
| SCV | 45 | 10 | 80.35 | 80.00 | 81.81 | 74.43 |
| SLD | 47 | 17 | 83.92 | 65.30 | 75.43 | 78.04 |
Sn- Sensitivity, Sp- Specificity, PPV-Positive predictive value, NPV- Negative predictive value. All value with their 95% confidence intervals MDL: Motor distal latency, MCV: Motor conduction velocity, SDL: Sensory distal latency, SCV: Sensory conduction velocity, MLD: Motor latency difference, SLD: Sensory latency difference
Statistical analysis showed a significant positive correlation between the cross-sectional area of the median nerve measured by US, as well as electrodiagnostic severity grades, with patients’ oriented measurements. Patients with abnormal NCS results demonstrated significant correlation with US grades (P < 0.01). On studying the correlation of different US and NCS measurement there were significant correlation (P < 0.05) between the cross-sectional area of the median nerve and NCS parameters except SNAP. CSA showed positive correlation with MDL and SDL, MLD and SLD but negative correlation with CMAP, MCV, SNAP and SCV and correlations were statistically significant [Table 3]. APD also showed positive correlation with MDL, SDL, MLD and SLD and negative correlation with CMAP, MCV,e SNAP and SCV. Correlations were statistically significant except with CMAP and MCV variables, however FR did not show any significant correlation with NCS parameters.
Table 3.
Pearson’s correlation coefficient (P)
| MDL | CMAP | MCV | SDL | SNAP | SCV | MLD | SLD | |
|---|---|---|---|---|---|---|---|---|
| CSA | 0.381 [0.004] | 0.375 [0.004] | 0.430 [0.001] | 0.33 [0.013] | 0.236 [0.08] | 295 [0.027] | 0.382 [0.004] | 0.323 [0.015] |
| FR | 0.004 [0.97] | 0.125 [0.357] | 0.135 [0.323] | 0.002 [0.988] | 0.046 [0.735] | 0.01 [0.941] | 0.026 [0.847] | 0.018 [0.897] |
| APD | 0.387 [0.004] | 0.177 [0.192] | 0.035 [0.799] | 0.406 [0.002] | 0321 [0.016] | 0.384 [0.004] | 0.332 [0.012] | 0.327 [0.014] |
MDL: Motor distal latency, MCV: Motor conduction velocity, in Median Nerve, CMAP: Compound muscle action potential. SDL: Sensory distal latency, SCV: Sensory conduction velocity, SNAP: Sensory nerve action potential. SLD: Sensory latency difference
DISCUSSION
The diagnosis of CTS is based mainly on the patient’s history and the clinical findings.[3,4] The value of provocative physical tests, such as Tinel’s or Phalen’s tests for CTS is controversial and results are often of doubtful clinical significance. Confirmation of CTS is usually based on nerve conduction studies. However, many authors have proposed that conventional electrophysiological studies are not appropriate for detecting mild median nerve compression and that the process causing symptoms of CTS might not be identical to the process causing slowing of nerve conduction.[21] Electrodiagnostic parameters are abnormal only if there is significant demyelination of axonal loss in the large myelinated fibres. In addition, symptoms may be produced by other mechanisms. Although the defined criteria of electrodiagnosis were reproduced to minimize the false negatives in diagnosis, including the 0.3 ms difference between the median and ulnar or the median and radial sensory latencies,[22] these criteria also have the potential for false positive results in diagnosing CTS. Some authors reported more than 40% false positive results using the 0.3 ms difference and proposed more generous criteria.[7]
In patients with CTS, anatomical evaluation and visualization of the carpal tunnel is a strong point in diagnosis and management. Chronic focal compression of the median nerve can lead to alteration in its morphology and cause demyelination by mechanical stress, deforming the myelin lamellae. Ischemia can account for the intermittent paraesthesias that can occur at night or with wrist flexion.[23] Imaging techniques were not under consideration in the assessment of CTS until recently. Buchberger et al.[1,11] were the first to quantify changes in carpal tunnel syndrome using sonography. Their findings confirmed those of earlier MRI studies.[24] Later on, other research was published on sonography and MRI for CTS. Current criteria for both MRI and sonography are swelling of the median nerve at the entrance to the carpal tunnel and flattening of the median nerve and palmar bowing of the flexor retinaculum at the exit from the carpal tunnel within the median nerve on T2-weighted images at the exit from the carpal tunnel in cases of CTS. Thickening of the flexor retinaculum and an increased height of the carpal tunnel, as measured from the apex of the flexor retinaculum convexity to the underlying carpal bone, are also mentioned in both MRI and sonography literature.[13,14,15,25] Thus, criteria for MRI and sonography have become similar, but are subject to discussion.[26,27]
In the present study, out of the ultrasonographic parameters, the median nerve cross sectional area appears to be useful in diagnosis of CTS. We found that the best discriminatory criterion for ultrasonographic diagnosis of CTS is a median nerve cross section area >0.88 mm2 at the carpal tunnel inlet, which also has been reported in previous studies.[9,28] The reported critical value for CSA varies mostly between 0.9 to 1.5 mm2.[1,9,28,29,30,31,32] In one of the studies, a considerably higher critical value 1.5 mm2 was found, probably because patients with mild elctrodiagnostic abnormality were excluded.[29]
Significant difference in the caliper measurements of the median nerve between CTS patients and asymptomatic controls were observed in present study as well as previous studies. There is variability in the median nerve CSA in CTS patients, although values obtained from asymptomatic are very consistent. In the present study, the median nervemean CSA was 1.46 mm2 in CTS patients and 0.079 cm2 in controls. Buchberger et al.[1] reported a mean CSA of 1.45 mm2 in CTS patients and 0.79 mm2 in the control group, Yesildag et al.[30] reported a mean CSA was 1.49 mm2 in CTS patients and 0.78 mm2 in the control group, and Duncan et al.[10] reported a mean CSA was 1,25 mm2 in CTS patients and 0.70 mm2 in the control group. In other study, mean CSA cut off value of 1.10 mm2 at the inlet showed good sensitivity and specificity and had a good correlation with all grades of CTS (33). The cause of this variability may be the differences in the study design and method as measurement.
We obtained the measurements of the median nerve from the inner border of echogenic perineurium surrounding the hypoechoic median nerve. Because of the echogenic perineural fat in the external border of the perineurium, the exact border may not be clearly distinguished and differences can be seen in the measurements. In some studies, the landmark used in the measurement was not mentioned and this may have led to variable results.
In our study, a non-significant difference in the flattening ratio [FR] between the two groups was observed. Duncan et al.[9] found the flattening ratio was 3.17 in patients and 2.72 in control. Buchberger et al.[1] calculated this ratio at the level of distal carpal tunnel and accepted that a FR >3 was significant for CTS. However, Yesildag et al.[30] and Wong et al.[28] did not determine significant differences in the FR between patients and controls and they suggest its diagnostic value is poor. The same results were seen in the current study.
In this study, we found significant differences in the anteroposterior [APD] of the carpal tunnel between the two groups. The anteroposterior diameter of the compression and swelling sites of the median nerve and the transverse carpal ligament thickness were measured. The mean diameter was 12.3 ± 1.9 mm in patients and 10.3 ± 1.7 mm in the control group. Lee et al.[29] reported an APD of 10.9 mm and 10.3 in asymptomatic woman and man, respectively.
Assessment of the cut-off points for moderate and severe cases on basis of to the electrodiagnostic studies, revealed that a cross-sectional area measurement greater than 13 mm2 can be considered significant and corresponds to the electrodiagnostically moderate cases, whereas a cross-sectional area of 16 mm2 corresponds to electro diagnostically severe cases. These data agree with the findings reported by Lee et al. and Miedany et al.,[16,29] they found that one can be confident of determining the degree of severity of median nerve neuropathy based on cross-sectional area on US. In their study, they reported that CSA of greater than 15 mm2 correlates with Nerve conduction studies findings of moderate to severe disease and it distinguishes severe from mild to moderate disease.
On assessing the correlation among the modalities assessed, a highly significant positive correlation was observed between ultrasound as well as electrodiagnostic measurements especially distal motor latency and distal sensory latency of median nerves; with the functional severity scales [HiOb scale]. Padua et al.[18] found that the clinical–neurophysiological relationship is very strong, with an exponential increase in functional impairment as the classification of neurophysiological severity progresses. This study showed that, similar to the electrophysiological studies, US has a strong and significant relationship to the clinical and Hi-Ob scale parameters.
On the basis of our study, we believe that a typical clinical picture of CTS with negative electrophysiological studies does not preclude a diagnosis of CTS. Six patients in our study, who had a typical clinical picture of CTS and negative electrophysiological studies, using critical CSA value of 1.0 mm2 [by present and other studies] in these cases diagnosed as of CTS by USG with sensitivity and specificity of 100% and 88%. Similarly, Padua et al.[18] reported that patients with typical CTS symptoms but negative electrophysiological studies have similar symptoms, function and examination findings to the minimally affected group, which is in agreement with our results [Table 4]. They hypothesized that negative patients are similar to minimally affected patients except that the neurophysiological findings are still within the normal range. These patients would probably become positive at a subsequent neurophysiological evaluation.
The strength of our study was that we had we clearly defined landmarks for inlet and outlet of median nerve to avoid the variability of the results. We also took patients with mild diagnostic abnormality to avoid the bias of the results, as few previously conducted studies didn’t take patients with mild diagnostic abnormalities. The limitation of our study was that our patient group was small in number. We need to perform the study on a larger population. Therefore ultrasonography is another useful tool for diagnosis of CTS as per sensitivity/specificity patterns of our study as well as other studies. The ultrasonographic quantitative measurement of the CSA of the median nerve is a particularly useful discriminatory diagnostic tool.
CONCLUSION
High-frequency US examination of the median nerve and measurement of its cross-sectional area should be strongly considered as a nediagnostic modality complementing NCS and alternative diagnostic modality for the evaluation of CTS in some selected cases as it is cost effective. It offers high diagnostic accuracy, as indicated by high correlation with the present standard NCSas well as patient-oriented measures. In contrast to these two tools, US provide information about the possible causes of CTS and hence have a therapeutic impact regarding the management of the patients.[32] Moreover, US is less time consuming, pain less and easily available diagnostic and screening modality and complements the nerve conduction studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Buchberger W, Schon G, Strasser K, Jungwirth W. High-resolution ultrasonography of the carpal tunnel. J Ultrasound Med. 1991;10:531–7. doi: 10.7863/jum.1991.10.10.531. [DOI] [PubMed] [Google Scholar]
- 2.Rankin EA. Carpal tunnel syndrome issues and answers. J Natl Med Assoc. 1995;87:169–71. [PMC free article] [PubMed] [Google Scholar]
- 3.Phalen GS. The carpal tunnel syndrome: Seventeen years experience in diagnosis and treatment of six hundred fifty four hands. J Bone Joint Surg Am. 1966;48:211–28. [PubMed] [Google Scholar]
- 4.Phalen GS. The carpal tunnel syndrome: Clinical evaluation of 598 hands. Clin Orthop. 1972;8:29–40. doi: 10.1097/00003086-197203000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Nathan PA, Keniston RC, Meadows KD. Predictive value of nerve conduction measurements at the carpal tunnel. Muscle Nerve. 1993;16:1377–82. doi: 10.1002/mus.880161217. [DOI] [PubMed] [Google Scholar]
- 6.MacKinnen SE, Dellon AL. Diagnosis of nerve injury. In: MacKinned SE, Dellon AL, editors. Surgery of the Peripheral Nerve. New York: Thieme; 1988. pp. 74–9. [Google Scholar]
- 7.Redmond MD, Risner MH. False positive electrodiagnostic test in carpal tunnel syndrome. Muscle Nerve. 1988;11:511–7. doi: 10.1002/mus.880110515. [DOI] [PubMed] [Google Scholar]
- 8.Barnes GG, Curry HLF. Carpal tunnel syndrome in rheumatoid arthritis.A clinical and electrodiagnostic survey. Ann Rheum Dis. 1967;26:226–33. doi: 10.1136/ard.26.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duncan I, Sullivan P, Lomas F. Sonography in the diagnosis of carpal tunnel syndrome. Am J Roentgenol. 1999;173:681–4. doi: 10.2214/ajr.173.3.10470903. [DOI] [PubMed] [Google Scholar]
- 10.Sarria L, Cabada T, Cozcolluela R, Martinez-Berganza T, Carcia S. Carpal tunnel syndrome: Usefulness of sonography. Eur Radiol. 2000;10:1920–5. doi: 10.1007/s003300000502. [DOI] [PubMed] [Google Scholar]
- 11.Buchberger Q, Judmaier W, Birbamer G, Lener M, Schmidaner O. Carpal tunnel syndrome diagnosis with high-resolution sonography. Am J Roentgenol. 1992;159:793–8. doi: 10.2214/ajr.159.4.1529845. [DOI] [PubMed] [Google Scholar]
- 12.Kanoly LP, Schrogendorger KF, Rab M, Girsch W, Gruber N, Frey M. The precision of ultrasound imaging and its relevance for carpal tunnel syndrome. Surg Radiol Anat. 2001;23:117–21. doi: 10.1007/s00276-001-0117-8. [DOI] [PubMed] [Google Scholar]
- 13.Nakamichi K, Tachibana S. The use of ultrasonography in detection of synovitis in carpal tunnel syndrome. J Hand Surg Br. 1993;18:176–9. doi: 10.1016/0266-7681(93)90100-t. [DOI] [PubMed] [Google Scholar]
- 14.Mesgarzadch M, Schneck CD, Bonakdarpour A. Carpal tunnel: MR imaging Part 1.Normal anatomy. Radiology. 1980;171:743–8. doi: 10.1148/radiology.171.3.2717746. [DOI] [PubMed] [Google Scholar]
- 15.Brahme SK, Holder J, Braun RM, Sebrechrs C, Jackson W, Resnick D. Dynamic MR imaging of carpal tunnel syndrome. Skeletal Radiol. 1997;26:482–7. doi: 10.1007/s002560050270. [DOI] [PubMed] [Google Scholar]
- 16.El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: Substantive or complementary tests. Rheumatol. 2004;43:887–95. doi: 10.1093/rheumatology/keh190. [DOI] [PubMed] [Google Scholar]
- 17.Practice parameter for carpal tunnel syndrome (summary statement) Report of the quality standard subcommittee of the American academy of neurology. Neurology. 1993;43:2406–9. [PubMed] [Google Scholar]
- 18.Giannini F. Quantitative assessment of historical and objective findings: A new clinical severity scale of CTS. In: Luchetti R, Amadio P, editors. Carpal Tunnel Syndrome. Berlin, Heidelberg: Springer; [Google Scholar]
- 19.Cioni R, Passero SS, Parasico C, Giannini F, Battistini N, Rushworth G. Diagnostic specificity of sensory and motor nerve conduction variables in early detection of carpal tunnel syndrome. J Neurol. 1989;236:208–13. doi: 10.1007/BF00314501. [DOI] [PubMed] [Google Scholar]
- 20.Padua L, Lo Monaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997;96:211–7. doi: 10.1111/j.1600-0404.1997.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 21.Jackson DA, Clifford JC. Electrodiagnosis of mild carpal tunnel syndrome. Arch Phys Med Rehab. 1989;70:199–204. [PubMed] [Google Scholar]
- 22.Gutmann L, Gutierrez A, Riggs JE. The contribution of median-ulnar communications in diagnosis of mild carpal tunnel syndrome. Muscle Nerve. 1986;9:319–21. doi: 10.1002/mus.880090406. [DOI] [PubMed] [Google Scholar]
- 23.Dawson DM. Entrapment neuropathies of the upper extremities. N Engl J Med. 1993;329:2013–8. doi: 10.1056/NEJM199312303292707. [DOI] [PubMed] [Google Scholar]
- 24.Mesgarzadeh M, Schneck C, Bonakdarpour A, Amitabba M, Conway D. Carpal tunnel: MR imaging. Radiology. 1989;171:749–51. doi: 10.1148/radiology.171.3.2541464. [DOI] [PubMed] [Google Scholar]
- 25.Chen P, Maklad N, Redwine M, Zelitt D. Dynamic high-resolution sonography of the carpal tunnel. Am J Roentgenol. 1997;168:533–7. doi: 10.2214/ajr.168.2.9016242. [DOI] [PubMed] [Google Scholar]
- 26.Mesgarzadch M, Triolo I, Schneck CD. Carpal tunnel syndrome: MR imaging diagnosis. MRI Clin North Am. 1995;2:249–64. [PubMed] [Google Scholar]
- 27.Radack DM, Schweitzer ME, Taras J. Carpal tunnel syndrome: Are the MR findings a result of population selection bias? Am J Roentgenol. 1997;169:1649–53. doi: 10.2214/ajr.169.6.9393185. [DOI] [PubMed] [Google Scholar]
- 28.Wong SM, Griffith JM, Hue AC, Tang A, Wong KS. Discriminatory criteria for diagnosis of the carpal tunnel syndrome arthritis rheumatology. 2002;46:1914–21. doi: 10.1002/art.10385. [DOI] [PubMed] [Google Scholar]
- 29.Lee D, Van Holsbeeck T, Janevski P, Ganos DL, Ditmars DM, Darian VB. Diagnosis of carpal tunnel syndrome. Radiol Clin North Am. 1999;37:859–72. doi: 10.1016/s0033-8389(05)70132-9. [DOI] [PubMed] [Google Scholar]
- 30.Yesildag A, Kutluhan S, Sengul N, Koyuncouglu HR, Oyar O, Guler K, et al. Role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol. 2004;59:910–5. doi: 10.1016/j.crad.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 31.Zhang L, Rehemutula A, Peng F, Yu C, Wang TB, Chen L. Does the ratio of the carpal tunnel inlet and outlet cross-sectional areas in the median nerve reflect carpal tunnel syndrome severity? Neural Regen Res. 2005;10:1172–6. doi: 10.4103/1673-5374.160117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wilder Smith EP, Seet RC, Lim EC. Diagnosing carpal tunnel syndrome- clinical criteria and ancillary tests. Nat Clin Pract Neurol. 2006;2:366–74. doi: 10.1038/ncpneuro0216. [DOI] [PubMed] [Google Scholar]