Graphical abstract

Keywords: Severe pulmonary regurgitation, Bilateral pulmonary valves, Right ventricular dysfunction, Cardiac MRI
Highlights
-
•
Severe PR is a common long-term complication after valvotomy.
-
•
There are no current endovascular valves for severe dilation of the main PA.
-
•
Implantation of transcatheter valves in the main PA branches is an alternative.
Introduction
Pulmonary regurgitation (PR) is a known long-term complication after surgical repair of congenital pulmonary stenosis (PS). It is most commonly seen two to three decades after correction of congenital tetralogy of Fallot.1 According to the 2014 American Heart Association/American College of Cardiology valvular heart disease guidelines, interventions for PR should be considered only if there are signs or symptoms of right ventricular (RV) dysfunction in the setting of severe PR.2 Although surgical pulmonary valve replacement remains the gold standard treatment for PR, transcatheter pulmonary valve implantation has evolved as a safe alternative to minimize the need for repeat surgical interventions in these patients. Available transcatheter valves, approved for implantation in the RV outflow tract (RVOT), have been shown to result in good short- and long-term outcomes.3 However, there are limited data regarding outcomes among patients in whom deployment of the valve in the outflow tract is contraindicated. Only a few case reports and small case series have been reported. In this case report, we present the unusual management of a patient with severe PR after valvotomy in whom a primary intervention was contraindicated because of severe RVOT dilation.
Case Presentation
A 32-year-old man with a medical history of congenital ventricular septal defect and PS status post patch repair and surgical valvotomy, respectively, was diagnosed with heart failure. Transthoracic echocardiography (TTE) showed a left ventricular ejection fraction of 20%. New York Heart Association functional class could not be determined, because of limited communication skills. His medical history was also significant for end-stage renal disease on hemodialysis secondary to autosomal dominant polycystic kidney disease, autism spectrum disorder, and intellectual disability.
Subsequent TTE, 5 months after initial TTE, showed severe PR without evidence of any obvious pulmonary valve leaflets in the RVOT. The pulmonary annulus was dilated (approximately 25 mm in diameter). The right ventricle was severely dilated with signs of dysfunction: tricuspid annular plane systolic excursion of 1.7 cm and a shortening fraction of 25% (Video 1). Cardiac magnetic resonance imaging performed 2 months later showed a 45% regurgitant fraction. The measured RV size confirmed severe dilation, with an RV end-diastolic volume of 379 mL (indexed value 223 mL/m2) and an RV end-systolic volume of 246 mL (indexed value 145 mL/m2)and an RV ejection fraction of 35% (Videos 2 and 3).
At 4-month follow-up, TTE showed worsening RV dysfunction (tricuspid annular plane systolic excursion of 1.0 cm; Figure 1), at which point it was decided to proceed with an intervention. Initial catheterization showed a severely dilated pulmonary valve annulus of 32.39 × 34.25 mm. The diameters of the right and left pulmonary arteries (PAs) were 15 and 14 mm, respectively. Given the size of the pulmonary valve annulus and the patient's multiple comorbidities, he was deemed a high-risk surgical candidate, and as such a transcatheter approach with Melody valves (Medtronic, Minneapolis, MN) was planned. Bilateral stents 2 cm in length were placed initially in the main PAs, with final diameters of 19.6 mm on the left and 17.9 mm on the right. Valve deployment at the time was delayed, allowing stent epithelization for a more secure landing zone (Videos 4 and 5).
Figure 1.

TTE demonstrating tricuspid annular plane systolic excursion of 1.0 cm.
Five months after the stents were placed, hemodynamics were notable for ventricularization of PA pressures secondary to severe PR (PA diastolic pressure = RV end-diastolic pressure). There was no gradient from the right or left PA to the main PA, and there was no gradient across the pulmonary valve. At that time, 22-mm Melody valves were deployed, overlapping the prior PA stents. No regurgitation of the valves was noted on angiography (Video 6). RV end-diastolic pressure remained at about 6 to 8 mm Hg. Detailed pressures are outline in Table 1. The patient tolerated the procedure without complications and was safely discharged home days later. Postoperative TTE with direct view of the RVOT demonstrated no PR on continuous-wave Doppler (Video 7, Figure 2).
Table 1.
Hemodynamics before and after implantation of valves
| Pressure measurement | Before | After |
|---|---|---|
| Mean PA pressure, mm Hg | 28/6 (14) | 37/21 (28) |
| PCWP, mm Hg | 6 | 6 |
| TPG | 8 | 20 |
| PVR, WU | 4.5 | 8 |
PCWP, Pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; TPG, transpulmonary gradient; WU, Wood units.
Figure 2.
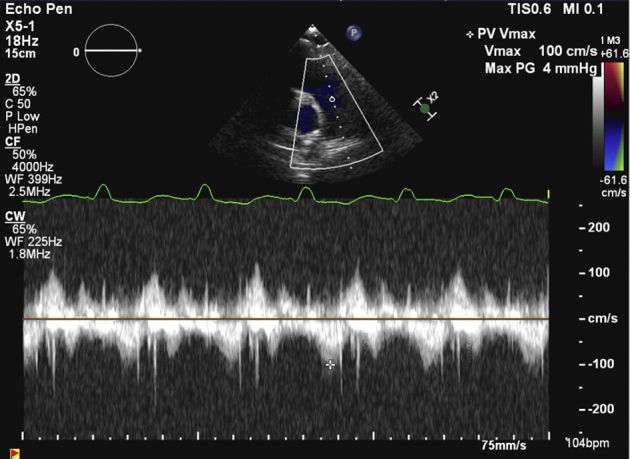
TTE after the procedure with continuous-wave Doppler demonstrating only trace PR.
Outpatient TTE 3 weeks after the procedure showed severely depressed RV function but no significant PR. The peak velocity of the proximal PA branches was normal at 1.5 m/sec (Video 8).
Discussion
Severe PR is uncommon and is mostly seen after surgery for tetralogy of Fallot or congenital lesions such as PS, as in the case of our patient. In a longitudinal study of patients who underwent surgical repair of PS before the age of 15 years, up to 21% had severe PR at a follow-up period of 33 years.4 In that study, 15% required reintervention and 9% underwent homograft implantation because of late PR. Interestingly, Nielsen et al.5 showed that freedom from reintervention decreases drastically with each decade after surgical repair of PS. Freedom from reintervention was 91% at 20 years postprocedure but decreased drastically to 26% after 50 years. This highlights the need for long-term follow-up of these patients by a cardiovascular team.
One of several challenges in the management of our patient was his late referral. By the time he was evaluated in the clinic there was already evidence of severe RV dysfunction. As mentioned before, current guidelines recommend intervention in cases of signs or symptoms of severe RV dysfunction. In the case of our patient, his intellectual disability was a barrier for communicating specific symptoms. Cardiac magnetic resonance imaging was essential for further evaluation, aiding in assessing the degree of RV dilation. At the time cardiac magnetic resonance imaging was done, the patient already exceeded the recommended thresholds for surgical intervention: RV EDV index > 150 mL/m2 or RV end-systolic volume index > 80 mL/m2. It is important to point out that severe PR, regardless of symptoms, also contributes to an increased incidence of arrhythmias and an increased risk for sudden death.6
Percutaneous pulmonary valve implantation was preferred because of high surgical risk, as previously mentioned. This approach was first introduced in the early 2000s, and since then, improvements in devices and techniques have been made. Currently there are two available valves: the Melody valve and the SAPIEN XT pulmonary valve (Edwards Lifesciences, Irvine, CA). The Melody valve can be expanded only up to 24 mm, and the largest available diameter of the SAPIEN XT valve is 29 mm, thus implantation in larger RVOTs is not feasible.
In our patient, the RVOT was severely dilatated to 34 mm in diameter, so bilateral implantation of Melody valves in the main PA branches was the only practical option.
The patient underwent bilateral implantation of Melody valves without any complications. However, it is important to point out potential complications of this approach. Stent fracture resulting from dynamic recoil of the RVOT has been reported to occur in up to 35% of implanted patients at a median follow-up of 5 years.7 Coronary compression, which should be assessed during the procedure, is seen in approximately 5% of patients.8 Last, pulmonary valve–related endocarditis can also occur. A meta-analysis by Chatterjee et al.9 showed a pooled incidence of 0.6 per 100 person-years.
Although the right ventricle was still severely dilated and tricuspid annular plane systolic excursion remained unchanged, PR was trivial on short-term follow-up TTE. Similar findings were observed in a cohort of patients who underwent Melody valve implantation for severe PR. That study, by Qureshi et al.,10 showed that 97% of patients had trivial to mild PR at a median follow-up of 2 years. More important, 50% of patients had improvement in RV size after implantation at 2-year follow-up. This highlights the need for long-term follow-up of patients undergoing percutaneous pulmonary valve implantation.
Conclusion
In this case we present the feasibility and good short-term outcomes of bilateral pulmonary valves implanted in the main PA branches. This was the only option in a patient with history of valvotomy with higher than standard surgical risk and whose anatomy was not suitable for implantation in the RVOT. Further studies are needed to evaluate long-term outcomes of patients with bilateral transcatheter implantation of Melody valves.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2020.10.005.
Supplementary Data
TTE with a view of the RVOT showing severe PR.
Cardiac magnetic resonance imaging without contrast, RVOT view, demonstrating the RVOT and main PA with severe PR.
Cardiac magnetic resonance imaging without contrast, four-chamber view, demonstrating severe RV dilation with the notorious turbulence during diastole due to PR.
Angiography of the right ventricle before placement of the stents; severe PR can be appreciated.
Angiography of the right main PA after placement of the stents.
Angiography of the right main PA after placement of the Melody valves; no regurgitation can be appreciated.
TTE after the procedure, focusing on the RVOT, demonstrating only trace PR.
Pediatric echocardiography with view of PA and branches. No evidence of insufficiency of the Melody valves is noted.
References
- 1.Hirsch J. Complete repair of tetralogy of Fallot in the neonate: results in the modern era. Ann Surg. 2000;232:508–514. doi: 10.1097/00000658-200010000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishimura R.A., Otto C.M., Bonow R.O., Carabello B.A., Erwin J.P., III, Guyton R.A. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:e57–e185. doi: 10.1016/j.jacc.2014.02.536. [DOI] [PubMed] [Google Scholar]
- 3.McElhinney D.B., Hellenbrand W.E., Zahn E.M., Jones T.K., Cheatham J.P., Lock J.E. Short- and medium-term outcomes after transcatheter pulmonary valve placement in the expanded multicenter US Melody valve trial. Circulation. 2010;122:507–516. doi: 10.1161/CIRCULATIONAHA.109.921692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roos-Hesselink J.W., Meijboom F.J., Spitaels S.E., vanDomburg R.T., vanRijen E.H., Utens E.M. Long-term outcome after surgery for pulmonary stenosis (a longitudinal study of 22–33 years) Eur Heart J. 2006;27:482–488. doi: 10.1093/eurheartj/ehi685. [DOI] [PubMed] [Google Scholar]
- 5.Nielsen E.A., Hjortdal V.E. Surgically treated pulmonary stenosis: over 50 years of follow-up. Cardiol Young. 2016;26:860–866. doi: 10.1017/S1047951115001158. [DOI] [PubMed] [Google Scholar]
- 6.Konstam M.A., Kiernan M.S., Bernstein D., Bozkurt B., Jacob M., Kapur N.K. Evaluation and management of right-sided heart failure: a scientific statement from the american heart association. Circulation. 2018;137:e578–e622. doi: 10.1161/CIR.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 7.Cabalka A.K., Hellenbrand W.E., Eicken A., Kreutzer J., Gray R.G., Bergersen L. Relationships among conduit type, pre-stenting, and outcomes in patients undergoing transcatheter pulmonary valve replacement in the prospective North American and European Melody valve trials. JACC Cardiovasc Interv. 2017;10:1746–1759. doi: 10.1016/j.jcin.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 8.Morray B.H., McElhinney D.B., Cheatham J.P., Zahn E.M., Berman D.P., Sullivan P.M. Risk of coronary artery compression among patients referred for transcatheter pulmonary valve implantation: a multicenter experience. Circ Cardiovasc Interv. 2013;6:535–542. doi: 10.1161/CIRCINTERVENTIONS.113.000202. [DOI] [PubMed] [Google Scholar]
- 9.Chatterjee A., Bajaj N.S., McMahon W.S., Cribbs M.G., White J.S., Mukherjee A. Transcatheter pulmonary valve implantation: a comprehensive systematic review and meta-analyses of observational studies. J Am Heart Assoc. 2017;6:e006432. doi: 10.1161/JAHA.117.006432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qureshi A.M., Bansal N., McElhinney D.B., Boudjemline Y., Forbes T.J., Maschietto N. Branch pulmonary artery valve implantation reduces pulmonary regurgitation and improves right ventricular size/function in patients with large right ventricular outflow tracts. JACC Cardiovasc Interv. 2018;11:541–550. doi: 10.1016/j.jcin.2018.01.278. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TTE with a view of the RVOT showing severe PR.
Cardiac magnetic resonance imaging without contrast, RVOT view, demonstrating the RVOT and main PA with severe PR.
Cardiac magnetic resonance imaging without contrast, four-chamber view, demonstrating severe RV dilation with the notorious turbulence during diastole due to PR.
Angiography of the right ventricle before placement of the stents; severe PR can be appreciated.
Angiography of the right main PA after placement of the stents.
Angiography of the right main PA after placement of the Melody valves; no regurgitation can be appreciated.
TTE after the procedure, focusing on the RVOT, demonstrating only trace PR.
Pediatric echocardiography with view of PA and branches. No evidence of insufficiency of the Melody valves is noted.


