Abstract
Dissatisfaction with the sound of one’s own voice is common among hearing-aid users. Little is known regarding how hearing impairment and hearing aids separately affect own-voice perception. This study examined own-voice perception and associated issues before and after a hearing-aid fitting for new hearing-aid users and refitting for experienced users to investigate whether it was possible to differentiate between the effect of (unaided) hearing impairment and hearing aids. Further aims were to investigate whether First-Time and Experienced users as well as users with dome and mold inserts differed in the severity of own-voice problems. The study had a cohort design with three groups: First-Time hearing-aid users going from unaided to aided hearing (n = 70), Experienced hearing-aid users replacing their old hearing aids (n = 70), and an unaided control group (n = 70). The control group was surveyed once and the hearing-aid users twice; once before hearing-aid fitting/refitting and once after. The results demonstrated that own-voice problems are common among both First-Time and Experienced hearing-aid users with either dome- or mold-type fittings, while people with near-normal hearing and not using hearing aids report few problems. Hearing aids increased ratings of own-voice problems among First-Time users, particularly those with mold inserts. The results suggest that altered auditory feedback through unaided hearing impairment or through hearing aids is likely both to change own-voice perception and complicate regulation of vocal intensity, but hearing aids are the primary reason for poor perceived sound quality of one’s own voice.
Keywords: hearing aids, voice, hearing impairment, voice quality, auditory perception
Dislike of the sound of one’s own voice has for a long time been a common factor affecting hearing-aid satisfaction (Kochkin, 2002, 2005, 2010). Historically, this has been attributed to the occlusion effect, which manifests itself as a low-frequency increase of self-produced sounds (such as vocalization, chewing, and swallowing) due to the hearing-aid mold occluding the ear canal (Kiessling et al., 2005; Stenfelt & Reinfeldt, 2007). However, occlusion effect-related issues are now recognized as providing only a partial explanation for user complaints regarding the sound quality of one’s own voice (Laugesen et al., 2011). Several other explanations and suggestions for potential solutions exist (Dillon, 2012b), but the phenomenon has not been studied in great detail. As pointed out by Laugesen et al. (2011), most of the standard outcome measurements in audiological rehabilitation contain no mention of the sound of one’s own voice.
Understanding the mechanisms that affect the experience of own voice of hearing-aid users requires consideration of several aspects. The sound of one’s own voice is a complex function of vibrations transmitted through air as well as through the various structures of the throat and head. The latter pathways are referred to as bone conduction (BC; Stenfelt, 2016; Stenfelt & Goode, 2005). The acoustic properties of the human skull have been studied in the past (Fry & Barger, 1978), as has the relative contribution of air-conducted (AC) and BC sounds for own-voice perception (Reinfeldt et al., 2010). The results from these studies show that while AC and BC sounds are of approximately equal importance, their contributions are frequency dependent and vary widely for different speech sounds (Békésy, 1949; Pörschmann, 2000; Reinfeldt et al., 2010).
The acoustic properties of bone have been of practical importance for the development of BC hearing aids. These properties have also been explored in relation to the aforementioned occlusion effect. During natural sound transmission through BC, the low-frequency sound pressure in the ear canal is low, due to the low acoustic impedance of the open ear canal (Stenfelt et al., 2003). However, closed ear molds, which block the ear canal, cause an increase in the low-frequency BC sound pressure in the ear canal due to an increase in the acoustic impedance (Dillon, 2012a; Stenfelt & Reinfeldt, 2007). Perceptually, the effect has been described as making the sound of one’s own voice unnatural, specifically boomy, hollow, or like talking in a barrel (Winkler et al., 2016, p.3).
The introduction of open hearing-aid fittings greatly reduced problems related to the occlusion effect (Kiessling et al., 2005; Stenfelt & Reinfeldt, 2007). An open-fitted hearing aid has a small, cone-shaped piece of plastic called a dome that is placed in the ear canal and usually has large openings allowing excessive ventilation. A mold or closed fit refers to a hearing aid with an insert that has been custom molded for the individual users’ ear canal (Winkler et al., 2016). A mold can have vents of varying diameters allowing for ventilation and decreasing the occlusion effect. However, hearing-aid users continued to report dissatisfaction with the sound of their own voice after open fittings became more common in the clinic (Kochkin, 2010; Laugesen et al., 2011).
Open fittings are not appropriate for all types of hearing-aid users. The choice of an open or closed fit is usually based on the user’s hearing thresholds. Hearing aids with domes can typically provide adequate amplification for individuals with moderate high-frequency hearing loss. For individuals with severe hearing loss, low-frequency hearing loss, or hearing loss over all parts of the frequency spectrum, a closed fitting is often necessary to achieve sufficient amplification without feedback problems (Winkler et al., 2016). This means that some users will still experience problems related to the occlusion effect. Another issue is that even an optimally fitted hearing aid with an open fit will, to an extent, alter the sound of one’s own voice (Stenfelt, 2011), as hearing aids amplify only AC sounds. A sensorineural hearing impairment involves a deficit in the ability to hear AC and BC sounds to the same extent. A hearing aid therefore alters the relative contributions of the AC and BC components of one’s own voice (Stenfelt, 2011), which leads to a change in perception of one’s own voice (Pörschmann, 2000; Stenfelt, 2011).
The time delay in a hearing aid can also affect the perception of one’s own voice. The digital processing by the hearing aid introduces a time difference between the aided AC and BC components of one’s own voice. A speaker may perceive this as disturbing if the delay exceeds 20 ms (Stone & Moore, 1999), but this is rare in practice. Bramsløw (2010) investigated perceived own-voice sound quality for time delays between 5 and 10 ms and for high-pass filter cutoffs between 100 and 2200 Hz in open-fitting hearing aids. Neither participants with hearing impairment nor participants with normal hearing showed any preference for time delays. There was a preference for a high-frequency cutoff of 2200 Hz for the participants with normal hearing but no preference for cutoff frequency for the participants with hearing impairment (Bramsløw, 2010).
The term ampclusion has been used to describe problems with own-voice sounds that have a broader origin than occlusion of the ear canal. It includes problems that are believed to be caused by digital sound processing and hearing-aid amplification (Kuk & Ludvigsen, 2002). Some examples of plausible nonocclusion causes of own-voice complaints are described later.
The proximity of the mouth to the ear causes a higher input level to the hearing aid for one’s own voice than for other people’s voices, and this can be a possible cause of distortion (Dillon, 2012b). A hearing aid is usually set to amplify weak sounds while reducing the gain at louder sounds (dynamic range compression). The compression typically quickly reduces the gain when one’s own voice is active, followed by a slower increase of the gain once one’s own voice has stopped (Dillon, 2012a). Consequently, compression applied to one’s own voice can result in distortion of the own-voice signal. Modern sound processing, individual settings, and directional microphones can also alter how one’s own voice is perceived (Dillon, 2012b; Kuk & Ludvigsen, 2002; Stenfelt, 2011).
Dillon (2012b) also writes that, because a high-frequency hearing impairment affects the tonal quality of everything, another potential explanation for dislike of one’s own voice is that some new hearing-aid users may have forgotten what their voice should sound like. This explanation is sometimes used as a justification for counseling the patient that they will become used to the sound of their own voice, given some time. Dillon (2012b) did not consider this a likely explanation for own-voice complaints, but he concluded that no data are available on the topic.
Conventional adjustments to solve occlusion problems are to increase vent size and reduce low-frequency amplification. Suggested adjustments to solve nonocclusion related voice complaints include changing the compression settings or decreasing low-frequency amplification for high-level sounds. Each possible solution is associated with potential adverse effects (Dillon, 2012b; Groth, 2014).
A general problem when studying the perception of sound quality is that perception, by definition, is a subjective experience. Some hearing-aid users have trouble finding the words to describe different sounds, and no common terminology exists for various sound qualities. The words harsh, shrill, hissy, sharp, metallic, or tinny may be used to describe excessive high-frequency amplification (or insufficient low-frequency amplification), whereas muffled, unclear, boomy, or dull may describe excessive low-frequency amplification (or insufficient high-frequency amplification; Dillon, 2012b). Typically, hearing-aid users seem more prone to notice a negative effect on sound quality due to excessive high-frequency gain than to excessive low-frequency gain (Keidser & Dillon, 2006).
The only questionnaire to date that assesses own-voice problems for hearing-aid users is Own Voice Qualities (OVQs), developed by Laugesen et al. (2011). The OVQ divides the problems into several domains: perceiving the sound quality of the voice to be poor, uncertainty in achieving correct vocal strength due to altered auditory feedback of one’s own voice, and problems relating to own-voice sounds masking the voices of other speakers or otherwise limiting participation in communication. The results of the study of Laugesen et al. (2011) showed that hearing-aid users reported most problems with the ability to alter voice intensity confidently and being able to speak and hear at the same time, compared with a group of participants with normal hearing.
While the study of Laugesen et al. (2011) resulted in a new tool for assessing the own-voice experience for hearing-aid users, the implications were somewhat limited, as the authors surveyed only the hearing-aid users at one point in time. Previous studies have suggested that hearing impairment complicates vocal regulation and is a potential risk factor for physiological voice problems (Coelho et al., 2015), which adds another layer of complexity.
In a previous study by the current authors, 110 hearing-aid users were compared with a group of 110 subjects with hearing impairment but without hearing aids and no previous experience with hearing aids, as well as to a control group with age-appropriate hearing (n = 70; Hengen et al., 2018). The results revealed that the hearing-aid users rated themselves as having significantly greater subjective voice problems (based on the standardized Voice Handicap Index [VHI] form of Jacobson et al., 1997, translated into Swedish by Ohlsson & Dotevall, 2009) than the two other groups. The group with hearing impairment but no hearing aid had a significantly higher average score (worse voice problems) than the control group. Twenty-two percent of the variance in subjective voice problems was explained by a model with gender, age, and subjectively rated hearing problems (based on the score from the Hearing Handicap Inventory for the Elderly [HHIE]) as predictors. A descriptive analysis also showed that a larger proportion of participants in the group of hearing-aid users regarded their voice as sounding hollow, sharp, metallic, dull, or distorted than for the other two groups (Hengen et al., 2018).
The effects of hearing aids on own-voice perception could be better understood by examining the own-voice experience before and after hearing-aid fitting/refitting for both naive and experienced hearing-aid users. Such a design can help to tease out own-voice problems related to the hearing aids themselves and to the underlying hearing impairment, as well as problems related to the perceived own-voice sound quality, feedback for altering voice intensity, and participation in conversations relating to the ability to speak and hear simultaneously. The aim of the current study was therefore to investigate own-voice related issues for participants with hearing impairment who were undergoing a hearing-aid fitting/refitting. The specific hypotheses were that a greater difference in own-voice perception would be observed for first-time users than for experienced users and that users with mold inserts would experience more own-voice problems than users with open fittings.
Materials and Methods
Design
The study was approved by the Regional Ethical Review Board in Linköping, Sweden (No. 2014/335-31). There were three groups. The first group had hearing impairment with no previous experience of using hearing aids (referred to as soon-to-be first-time [STB FT] users prefitting and first-time [FT] users postfitting). The second group consisted of experienced hearing-aid users (referred to as Experienced users), and the third was a control group with participants who did not have hearing impairment or hearing aids. The participants with hearing impairment were recruited from consecutive patients on the waiting list to either get their current hearing aid replaced during a refitting process (Experienced users) or to get fitted with their first hearing aid (STB FT users). The participants were drawn from the population described by Hengen et al. (2018) and included those who accepted continued participation. Participants with hearing impairment were recruited at the hearing clinic at Linköping University Hospital, and the control group was recruited through public advertisements and by inviting family members of the participants in the hearing-impaired groups. The recruitment took place between May 2015 and February 2017. None of the participants received any compensation.
The participants with hearing impairment received information on the project and an invitation to participate through a letter included in the standard call for a hearing-aid evaluation. The inclusion criteria were as follows: for the STB FT user group that they had never used hearing aids and for the Experienced users that they had a minimum of 2 years’ experience of using a hearing aid.
Interested patients were contacted by phone, and their eligibility for participation was determined before their appointment. If they passed the initial inclusion criteria, then information, consent forms, and questionnaires were sent out by mail to the participant’s home address. By the end of the recruitment period, the participation invitation slips were sent out to participants according to a more strictly limited age range (older STB FT users and younger Experienced users) to achieve a closer match in average age between the STB FT users and Experienced users. The resulting average age for was approximately 74 years for STB FT users, 75 years for the Experienced users, and 71 years for the control group (Table 1).
Table 1.
Participant Characteristics and Data About the Hearing-Aid Fitting Process.
| First-time users | Experienced users | Control group | |
|---|---|---|---|
| No. | 70 | 70 | 70 |
| Gender distribution | 46 M/24 F | 48 M/22 F | 31 M/39 F |
| Age (mean, years) | 74 (SD = 6.3) | 75 (SD = 9.1) | 71 (SD = 7) |
| % living with partner/spouse | 80 | 75 | 90 |
| Years with hearing loss | 11 (SD = 12) | 22 (SD = 15) | – |
| Years of HA use | – | 12.5 (SD = 8) | – |
| Typical current HA use | n (% of group) | n (% of group) | n/a |
| Weekly or less | 9 (13) | 7 (10) | |
| Up to 4 hr per day | 20 (29) | 11 (16) | |
| 4–10 hr per day | 25 (36) | 22 (31) | |
| More than 10 hr per day | 16 (23) | 30 (43) | |
| Data about the fitting of the hearing aids | |||
| Number of visits | 3.7 (SD = 1.3) | 4.1 (SD = 2.2) | |
| Fitting period (days) | 116 (SD = 64) | 110 (SD = 77) | |
| Unilateral or bilateral fitting | 10 unilateral/60 bilateral | 9 unilateral/61 bilateral | |
| Insert | 50 domes/20 molds | 21 domes/49 molds | |
| Average vent diameter for molds (mm) | 2.3 (SD = 0.9) (right); 2.4 (SD = 0.9) (left) | 1.8 (SD = 1.1) (right); 2.1 (SD = 1.2) (left) | |
| Hearing aid type | 69 BTE vs. 1 ITE (left); 63 BTE vs. 1 ITE (right) | 52 BTE vs. 11 ITE (left); 46 BTE vs. 13 ITE (right) |
Note. HA = hearing aid; BTE = behind-the-ear; ITE = in-the-ear.
The participants were encouraged to read through the information and consent form and complete the questionnaires before the appointment. They also had the option of contacting the researcher before the appointment to ask questions. Written consent was either completed at the first appointment at the clinic or returned together with the questionnaires. In a few cases, the questionnaires were completed at the clinical visit with the help of the test leader, due to problems with poor vision or dexterity.
No knowledge was available beforehand regarding which patients would opt to continue with hearing aids, and some dropouts were expected. Therefore, the number of patients recruited and accepted before hearing aid fitting was greater than the final number after the hearing-aid fitting had been concluded. The response rate was 22% for the patient groups and 19% for the control group.
A more detailed overview of the flow of participants during the recruitment process and reasons for dropouts can be found in Supplemental Digital Content 1. Out of 1,901 invitations, a total of 402 individuals (including the control group) returned the completed participation slip. Of these, 88 were either eliminated or dropped out before any data collection was conducted. At the follow-up visit after the hearing-aid fitting had been concluded, an additional 104 participants were eliminated. Some eligible participants, who had completed the first session, opted not to continue participation for the second session after the hearing-aid fitting. The most common reasons for dropout included personal illness, lack of time, and limited use of hearing aids. The enrolled patients who remained in the study received their follow-up questionnaires within a week after their hearing-aid fitting had been concluded.
Participants in the control group had their hearing tested before receiving the questionnaires. The criteria for inclusion in the control group were hearing thresholds up to 25 dB HL at and below 1 kHz, 30 dB HL at 2 kHz, 40 dB HL at 4 kHz, and 50 dB HL at 6 kHz, based on the study of Laugesen et al. (2011), with the rationale that it would include individuals with age-appropriate hearing but exclude individuals who were likely to benefit from hearing aids. The unaided hearing thresholds of the participants were measured at frequencies between 0.125 and 8 kHz with a clinical audiometer (Otometrics Auricle and Interacoustics AC40). The thresholds for the hearing-aid users were evaluated at the same frequencies in the clinic by an audiologist as a part of the standard hearing-aid fitting. The average hearing thresholds for the three groups are displayed in Figure 1.
Figure 1.
Audiograms Displaying the Average Hearing Thresholds (dB HL) With Bold Lines, Minimum/Maximum Values in Thin Lines, Whiskers for Standard Deviations for the Frequencies 0.125, 0.25, 0.5, 1, 2, 4, and 8 kHz for the Three Different Groups. Inclusion criterion thresholds for the control group are plotted with a red “x.”
Because the authors had no reason to expect any change in the control group over the time span of a typical hearing-aid fitting, they completed the questionnaires only once. The study sample consisted of 70 FT users, 70 Experienced hearing-aid users, and 70 control participants. Domes were more common than molds in the FT user group (50 domes vs. 20 molds), and mold inserts dominated among the Experienced users (49 molds vs. 21 domes). An overview of the participants is shown in Table 1.
Description of the Hearing-Aid Fitting Process
The hearing-aid fitting took an average of approximately four visits (Table 1). The time between starting a hearing-aid fitting and concluding it was, on average, 3.5 months. Neither the number of visits to the clinic nor the time period for the fitting varied markedly between the two hearing-aid groups, although there was variability within the groups (Table 1).
Most patients were bilaterally fitted with behind-the-ear (BTE) hearing aids. While some other styles were represented in the Experienced group, only one FT user was fitted with a non-BTE hearing aid.
Questionnaires and Procedure
The data were collected through forms and questionnaires and included information regarding the participants’ self-reported hearing problems, voice functions, perceived sound quality of their voices, demography, and relevant medical backgrounds. A detailed description of the forms and questionnaires can be found in Supplemental Digital Content 2. A brief description of the various tools is presented later.
Self-assessed hearing problems were measured with the HHIE questionnaire, developed by Ventry and Weinstein (1982), and translated and validated in Swedish by Öberg (2016).
An adapted version of the OVQ questionnaire was used to study the participants’ experience of their own voice. There were three versions of the OVQ with differences in wording, depending on whether the participant had one or two hearing aids, or none at all. The hearing aid version of OVQ instructed the respondent to answer based on situations when using their hearing aids. This version included additional items regarding the users’ perception in the period immediately after they received their current hearing aid as well as in situations when they were not using their hearing aids.
Some changes were made to all three versions of the original OVQ questionnaire. While the intention was to stay as close to the original form as possible to facilitate comparisons, some revisions were needed for the purpose of this study (see Supplemental Digital Content 3, which describes the changes from the original questionnaire).
The questions were divided into the following categories of own-voice issues, created during the original development of the OVQ:
Overall rating of own-voice satisfaction or problems.
Voice intensity control (the ability to produce an adequate voice intensity for the occasion) and whispering (the ability to use whispering as a form of communication), consisting of 11 statements altogether.
Speak and hear (the ability to speak and hear at the same time, e.g., in rapid turn-taking, as in a heated discussion), consisting of five items.
Disturbing sound qualities (DSQ), consisting of 13 sound qualities such as hollow and metallic. This section was referred to as “specific sound qualities” during the original development of OVQ when it contained a mix of positive and negative sound qualities. The current study omitted the positively coded sound qualities in the analysis and included only sound qualities with a significant correlation with own-voice complaints, which is the reason for the name change.
Section N (own-voice experience with no hearing-aid use, only intended for hearing-aid users) was not used in this study, as many of the Experienced users returned it unanswered. A few specified that this was because they almost always wore their hearing aids and therefore could not answer the questions.
Problems with one’s own voice were also measured with the VHI. The reason for using this questionnaire was that, unlike the OVQ, it is a standardized tool which can be used to assess clinical voice disorders, and it offers more insight into the physical, functional, and emotional consequences of having a voice problem.
Information regarding the hearing aids and details regarding the participants’ hearing status were collected from the medical records. This included the number of visits to the hearing clinic for adjustments, the starting and concluding dates for hearing-aid fitting, the type of hearing aid(s) (BTE or in-the-ear), hearing aid fit, vent size, hearing aid brand and model, and audiograms.
Analysis
The majority of the items on the OVQ and the other questionnaires used in this study are constructed so that a high score means more problems. The few items for which a high score was positive (e.g., A1 “My own voice sounds good to me”) were recoded in reverse to facilitate pooling scores within categories. Thus, a higher score always indicated lower own-voice satisfaction. Scores from different items within the same category were pooled to a composite score. The composite scores were then divided by the number of scale items to convert the scores back to the 0 to 8 OVQ scale. In this way, all the items and categories could be presented on the same scale and in the same format to facilitate comparisons.
Both nonparametric and parametric methods were used to analyze the data. No consensus exists regarding the appropriateness of parametric tests for data collected using questionnaires (e.g., Pimentel, 2019; Simon, 2009). In the current study, scores for individual questionnaire items were analyzed using nonparametric statistics, as the scores were ordinal and tended not to be normally distributed.
Nonparametric tests were also used for the pooled scores of the HHIE and VHI, as their scores were considerably skewed and had nonnormally distributed residuals. The effect size calculation was z/√n for the Mann–Whitney U and z/√(2n) for the Wilcoxon signed-rank test, where z is the value of the normal approximation. The other pooled score variables were investigated with parametric statistics.
Age was used as a covariate factor in the parametric models, as the control group was on average 3 to 4 years younger than the hearing-aid users (Table 1). As aging affects voice quality and function (Galluzzi & Garavello, 2018), the variable Age was included in the models regardless of its statistical significance. As the covariate was not significant in any of the statistical tests, its specific significance for each analysis was omitted in the results.
The rationale for using parametric tests for composite score variables (with close to normal distribution of scores and residuals) was that the response scale is a Likert construction, the sample size was relatively large, and it was a pooled score of several measures. While the appropriateness of parametric tests on Likert scales is debatable (Mircioiu & Atkinson, 2017), pooled scores and large sample sizes are generally accepted conditions that allow the use of parametric statistics (Pimentel, 2019; Simon, 2009). In each parametric test, Levene’s test and normality checks were carried out to verify that the assumptions for conducting the tests were met. One of the assumptions for the parametric tests used in this article is a normal distribution of residuals. The distribution assumption was examined with the Shapiro–Wilks test. The Shapiro–Wilks test will often show significant results in larger samples with minor deviations, which is why it is recommended to interpret the Q-Q plots to assess whether the violation is substantial (Ghasemi & Zahediasl, 2012). In addition, some authors argue that distribution shape can be ignored if the sample exceeds 100 subjects (Altman & Bland, 1995).
The Shapiro–Wilks test for distribution of residuals was significant for the DSQ-variables. The authors reviewed the Q-Q plots and found that it was consistent with approximate normality and therefore proceeded with the planned parametric tests.
Data were analyzed with SPSS (version 24.0; IBM, Chicago, IL, USA). Values of p < .05 or the Bonferroni-adjusted level suggested by SPSS were considered statistically significant. Descriptive statistics were used to illustrate distributions for the two main groups as well as the dome/mold subgroups.
Results
Self-Rated Impact on Hearing and Voice Problems
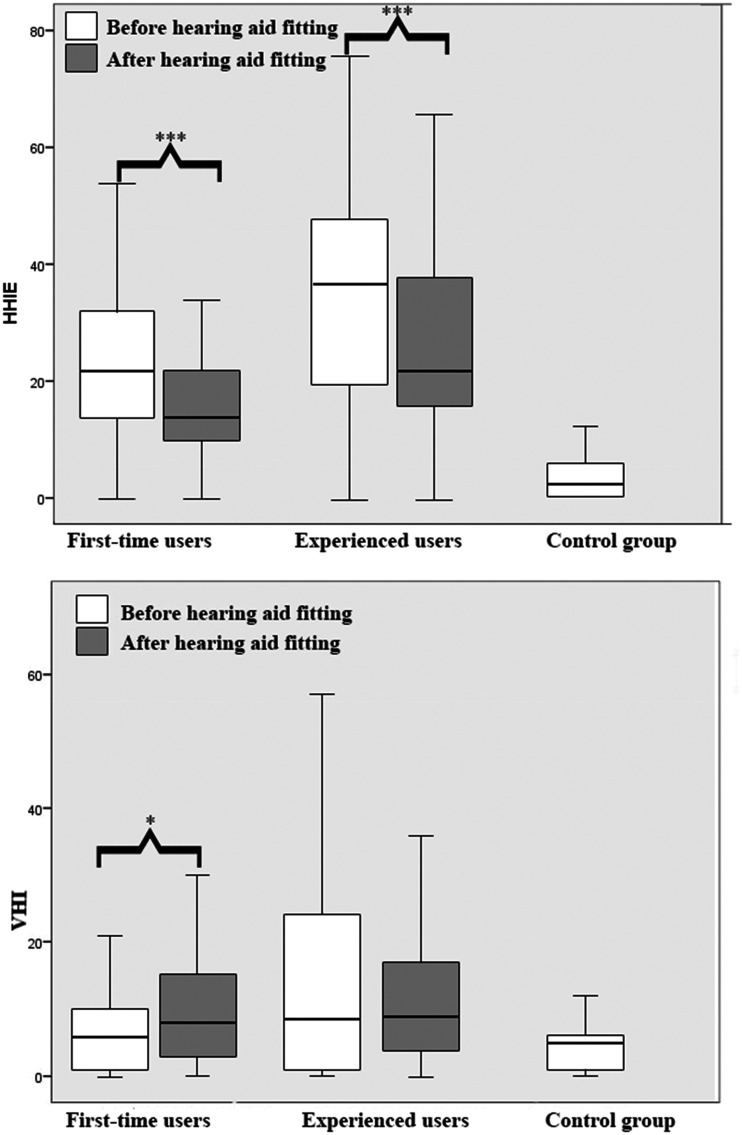
The general effect of the hearing-aid fitting (and refitting for the Experienced users) on perceived hearing ability (based on scores for the HHIE) was assessed using the Wilcoxon signed-rank test. Postfitting scores were significantly lower than prefitting scores for both FT users (z = –4.203, r = .4, p < .001) and Experienced users (z = –3.528, r = .3, p < .001); see Figure 2. This indicates that both groups on average perceived an improvement of their hearing ability after having a new hearing aid fitted. While the pre- and postfitting/refitting scores were on average higher for the Experienced users than for the FT users (Figure 2), an independent t test confirmed that the degree of improvement (the difference between pre- and postfitting/refitting scores) did not significantly differ (p > .05) between the groups. This indicates that the average perceived improvement in hearing function did not differ between FT users and Experienced users.
Figure 2.
Boxplot Showing the Median, Upper, and Lower Quartiles and Minimum/Maximum Values for Scores on the VHI and HHIE for Each Group Before and After Hearing-Aid Fitting/Refitting.
HHIE = Hearing Handicap Inventory for the Elderly; VHI = Voice Handicap Index.
The difference in self-rated voice problems (as rated on the VHI) between the groups before hearing-aid fitting/refitting was examined using a Kruskal–Wallis test. There was a significant difference in VHI scores between the three groups (χ2 = 8.343, p < .05). Post hoc Mann–Whitney U tests indicated that degree of voice problems was significantly higher for the Experienced users (Mdn = 8.5) than for to the control group (Mdn = 5, p < .001, U = 1,903). There was no significant difference between the FT users (Mdn = 6) and either of the other two groups (p > .05).
A Wilcoxon signed-rank test showed that postfitting scores on the VHI were significantly higher than prefitting scores for the FT users (z = –2.189, r = .2, p = .003), but no significant effect was found for the Experienced users (Figure 2). This indicates that the FT users experienced a small increase in voice problems after being fitted with their first hearing aids. A Mann–Whitney U test showed no significant differences in total score on the VHI between the FT users and the Experienced users after hearing-aid fitting (p > .05).
Overall Prevalence of Own-Voice Complaints
The OVQ Item I1 (The sound of my own voice is a problem for me) was selected as the questionnaire’s most general statement regarding own-voice complaints. A Spearman’s correlation test revealed that the reverse-coded score on Item A1 (“My own voice sounds good to me”) was correlated with perceiving the sound of one’s own voice as a problem (Item I1), both before (rho = 0.59, p < .001) and after (rho = 0.48, p < .001) hearing-aid fitting.
A Kruskal–Wallis test showed a statistically significant difference in responses to Item A1 between groups before hearing-aid fitting/refitting, χ2 (2) = 46.392, p < .001. Post hoc comparisons with Mann–Whitney U tests indicated that the control group on average agreed more with the statement “My own voice sounds good to me” than STB FT users and Experienced users (Table 2). Another Mann–Whitney U test was conducted after hearing-aid fitting to explore any potential differences between the FT users and the Experienced users. The test showed that a small, but significant difference remained (Table 2 and Figure 3A).
Table 2.
Results of Nonparametric Groupwise and Pairwise Comparisons Using Mann–Whitney U Tests and Wilcoxon Signed-Rank Test for Items A1 (“My Own Voice Sounds Good To Me”) and I1 (“The Sound of My Own Voice Is a Problem for Me”).
| A1. My own voice sounds good to me (reverse coded). |
I1. The sound of my own voice is a problem for me. |
||||||
|---|---|---|---|---|---|---|---|
| Group (n) | Mdn ± Q | Test statistics | Group | Mdn ± Q | Test statistics | ||
| Before hearing-aid (re)fitting | |||||||
| STB FTU (70) | 2 ± 0 | *** U = 1,351 z = –4.771 r = –.403 |
STB FTU (70) | 0 ± 1 | *** U = 783 z = –7.111 r = –.6 |
||
| EXP. (70) | 3 ± 1 | EXP. (67) | 2 ± 0 | ||||
| STB FTU (70) | 2 ± 0 | *** U = 994 z = –6.217 r = –.5 |
STB FTU (70) | 0 ± 1 | NS | ||
| CG (70) | 1 ± 1 | CG (70) | 0 ± 1 | ||||
| EXP. (70) | 3 ± 1 | ** U = 1,803 z = –2.910 r = –.3 |
EXP. (67) | 2 ± 0 | *** U = 806 z = –7.028 r = –.6 |
||
| CG (70) | 1 ± 1 | CG (70) | 0 ± 1 | ||||
| After hearing-aid (re)fitting | |||||||
| FTU (66) | 2 ± 1 |
* U = 1,663 z = –2.443 r = –.21 |
FTU (67) | 1 ± 2 | NS | ||
| EXP. (66) | 2 ± 1.25 | EXP. (66) | 2 ± 2 | ||||
| Before (1) and after (2) hearing-aid (re)fitting | |||||||
|
|
Mdn1 ± Q1 |
Mdn2 ± Q2 |
Test statistics |
Group |
Mdn1/Q1 |
Mdn2/Q2 |
Test statistics |
| FTU (66) | 2 ± 0 | 2 ± 1 | NS | FTU (67) | 0 ± 1 | 1 ± 2 | z = –4.340, r = –.4*** |
| EXP. (66) | 3 ± 1 | 2 ± 1.25 | NS | EXP. (64) | 2 ± 0 | 2 ± 2 | z = –2.809, r = –.3** |
Note. NS = nonsignificant (p > .05); STB FTU = soon-to-be first-time users of hearing aid; FTU = first-time users; EXP. = experienced users; CG = control group; Mdn = median; Q = interquartile range.
*p = .015. **p < .01. ***p < .001.
Figure 3.
Boxplots Showing the Median, Upper, and Lower Quartiles and Minimum/Maximum Values for Scores for Statements A1 and I1 and the Categories “Voice Intensity Control,” “Speak and Hear,” and “DSQ”. Scores from composite variables have been divided by the number of category items to display all results on the 0- to 8-step scale used in the questionnaire and to facilitate comparisons between the different sections. Significant values from ANCOVA post hoc tests are shown with asterisks and brackets at the top of the graphs, while significant values from ANOVA post hoc tests are shown with asterisks and brackets at the bottom of the graphs.
DSQ = disturbing sound qualities.
A Kruskal–Wallis test based on the scores for Item I1 (“The sound of my own voice is a problem for me”) showed that there was a significant difference between groups before hearing-aid fitting, χ2 (2) = 68.978, p < .001 (Figure 3B). Post hoc comparisons with Mann–Whitney U tests indicated a higher score (more problems) for the Experienced users than for the other two groups (Table 2 and Figure 3B). At the follow-up after hearing-aid fitting, there were no significant differences (when examined with Mann–Whitney U tests) in scores for Item I1 between FT users and Experienced users (Table 2 and Figure 3B).
Using the prefitting and postfitting scores from the hearing-aid user groups, a Wilcoxon signed-rank test showed that the level of own-voice complaints (Item I1) differed significantly between the two sessions. This difference was particularly apparent within the FT user group, who were more likely, on average, to agree that the sound of their own voice was a problem after hearing-aid fitting (Table 2).
The responses to Item I1 were also analyzed descriptively by inspecting the distribution along the 5-point disagree–agree scale before and after hearing-aid fitting. The response distributions for the groups of FT and Experienced users are displayed in Figure 4A. Before being fitted with new hearing aids, almost all (93%) of the STB FT users answered no or very low agreement to statement I1. The remaining STB FT users answered some agreement (7%). After the hearing-aid fitting, only 55% of the FT users answered no or very low agreement. Although 45% reported some to moderate agreement, none answered that they completely or strongly agreed with the statement.
Figure 4.
Response distributions before and after hearing-aid fitting for the statement “The sound of my own voice is a problem to me,” divided into main groups (A) and subgroups (B). Asterisks denote number of missing responses.
The Experienced users agreed to a larger extent than FT users that the sound of their own voice was a problem for them before hearing-aid refitting—only 24% in total indicated no or very low agreement with the statement, although most (61%) indicated only some agreement. Among the Experienced users, more participants indicated the sound of their own voice to be a nonissue after hearing-aid fitting than before. The proportion who indicated no or very low agreement rose from 24% to 42%. An equal proportion (42%) indicated some agreement with the statement, while the remaining 15% indicated moderate to complete agreement (Figure 4A).
An investigation was made between groups fitted with molds and domes (open fittings). Among the FT users, the difference in responses before and after hearing-aid fitting was most prominent for those participants fitted with molds, who went from 90% to 22% in the “No or very low agreement” category (compared with the dome users who went from 94% to 67% in the same categories); see Figure 4B. The Experienced users showed an approximately equal increase of 20 percentage points of participants in the “No or very low agreement” category, for both the dome and mold subgroups, indicating an overall improvement in perceived own-voice sound quality (Figure 4B).
Voice Intensity Control
A one-way analysis of covariance (ANCOVA) model with Age as a covariate showed a significant difference between groups in the perceived difficulty of vocal intensity control (Section E) before fitting/refitting, F(2, 194)= 19.414, p < .001, ηp2 = 0.169. Post hoc tests indicated that the estimated marginal mean was significantly higher for the Experienced users than for the STB FT users and the control group. The STB FT users also had a significantly higher score than the control group (Figure 3C). An ANCOVA on the postfitting/refitting scores showed no significant difference between First-Time users and Experienced users.
The effect of hearing aids on voice intensity control was investigated using a two-way analysis of variance (ANOVA) with User Group (FT/EXP users) and Intervention (before and after) as fixed factors and Age as a covariate. There was a significant main effect of User Group, F(1, 137) = 7.506, p = .007, ηp2 = 0.052, Experienced users reporting more problems with voice intensity control overall (for the pre-refitting and post-refitting scores combined) than FT users (Table 3 and Figure 3C). There was no significant main effect of Intervention, with a similar overall score before and after hearing-aid fitting (Table 3).
Table 3.
An Overview of Main- (Group, Hearing Aid Intervention) and Interaction (Hearing Aid Intervention × Group) Effects on the Variables “Voice Intensity Control,” “Speak and Hear,” and “Disturbing Sound Qualities.”
| Voice Intensity Control | Speak and Hear | Disturbing Sound Qualities | |
|---|---|---|---|
| HAI | NS | NS | NS |
| Group | p = .01 | p < .01 | p = .022 |
| HAI × Group | p = .012 | NS | p < .013 |
Note. NS = nonsignificant; HAI = hearing aid intervention.
There was a significant interaction between Intervention and User Group, F(1, 137) = 5.973, p = .012, ηp2 = 0.046 (Table 3). Descriptive statistics showed that while FT users had slightly higher postfitting scores than prefitting scores, the reverse was true for the Experienced users (Figure 3C). Post hoc pairwise comparisons revealed that the difference in scores was significant only for the Experienced users, t(68)=2.157, p = .034 (Figure 3C).
Examination of the mean scores for the individual items in the “voice intensity control” section revealed that participants in both groups with hearing impairment experienced relatively high difficulty in voice intensity control, even before hearing-aid fitting/refitting. The highest scoring items before hearing-aid fitting/refitting were E6, E7, E8 (difficulty finding a correct voice intensity in different sound environments), and E9 (difficulty speaking in noise). These were also the highest scoring items after fitting/refitting, although the scores were slightly lower for the Experienced users and slightly higher for the FT users compared with before the fitting.
Speak and Hear
The participants were asked to rate their agreement with five statements regarding their ability to participate in conversations where their own speech overlapped with that of other speakers (e.g., D5 “I can easily hear what people are saying to me if they interrupt me before I am finished speaking” and D6 “When I participate in a discussion, my own voice is too dominant in comparison with what I want to hear”). The pooled item scores are referred to as speak and hear.
A one-way ANCOVA model with Age as a covariate was run to examine any groupwise differences in the perceived ability to simultaneously speak and hear before hearing-aid fitting/refitting. There was a significant difference in self-rated difficulty, F(1, 199)= 32.350, p < .01 ηp2 = 0.320, between the three groups.
Post hoc tests revealed significant differences between the Experienced users and the STB FT users (p < .01) and the control group (p < .001). The STB FT users also gave significantly higher scores than the control group (p < .001; Figure 3D). An ANCOVA on the FT and Experienced users’ postfitting/refitting scores showed that the Experienced users still had a significantly higher score than the FT users, F(2, 137)=9.2, p < .01, ηp2= 0.063. For descriptive statistics, see Table 3 and Figure 3D.
The effect of hearing aids on the ability to speak and hear was investigated using a two-way ANOVA with User Group and Intervention as fixed factors and Age as a covariate. There was a significant effect of User Group, F(1, 138) = 16.5, p < .001, ηp2 = 0.107, Experienced users reporting more issues than FT users.
There was no significant effect of Intervention (Table 3 and Figure 3D). There was no significant interaction between Intervention and User Group.
Disturbing Sound Qualities
The participants were asked to describe the sound of their own voice by rating their agreement with 13 items describing different sound qualities. The average score for these sound qualities had a correlation with perception of the sound of one’s own voice as problematic (Item I1), both before (rho = 0.297, p < .001) and after (rho = 0.485, p < .001) hearing-aid fitting/refitting. Therefore, this section is referred to as DSQ and a high total score is interpreted as a negative rating of own-voice sound quality.
A one-way ANCOVA with Age as a covariate was used to identify any differences between groups in prefitting experience of DSQ. There was a significant effect of group before fitting, F(2, 206)= 25.333, p < .001, ηp2 = 0.197 (Table 3).
Post hoc tests revealed significant differences between the Experienced users and the STB FT users (p < .001) and the control group (p < .001). The STB FT users did not have a significantly different DSQ score from the control group (p > .05). An ANCOVA model based on postfitting/refitting scores revealed no significant difference between the FT and Experienced users (Figure 3E).
A two-way ANOVA model with User Group and Intervention as fixed factors and Age as a covariate was used to examine the effects of hearing-aid fitting/refitting on the DSQ scores for the FT and Experienced hearing-aid users. There was a significant effect of User Group, F(1, 137) = 11.392, p = .001, ηp2 = 0.077, Experienced users giving slightly higher DSQ scores than the FT users.
There was no significant effect of Intervention (Table 3). There was, however, a significant interaction between Intervention and User Group, F(1, 137) = 7.632, p = .003, ηp2 = 0.051. Descriptive statistics showed that both FT users and Experienced users had higher DSQ scores after hearing-aid fitting than before (Figure 3E). Post hoc tests showed that the difference in scores before and after hearing-aid fitting/refitting was significant for both the FT users, t(68) = –2.871, p = .005, and Experienced users, t(68)=1.821, p = .035 (Figure 3E).
Discussion
The aim of this study was to examine how individuals with hearing impairment experience their own voice before and after being fitted or refitted with a hearing aid. Dissatisfaction with the sound of one’s own voice has long been one of the most common factors affecting hearing-aid satisfaction (Kochkin, 2002, 2005, 2010). Own-voice complaints persevere among all types of hearing-aid users, even those who reasonably should not be affected by the occlusion effect (Laugesen et al., 2011). Considering these facts, the phrase Own-voice complaints needs to be explored as an umbrella term covering several different concepts.
Prevalence of Own-Voice Complaints
In the current study, there was a small, but significant increase in the average total score on the VHI after fitting for the FT users. While the average score was relatively low (m = 10; SD = 11) compared with the suggested cutoff for a voice disorder (score of 20, based on Jacobson et al., 1997), the increase in score makes it hard to rule out potential maladaptive voice behavior following hearing-aid fitting.
The Experienced hearing-aid users had a significantly higher average score for the item “The sound of my own voice is a problem for me” prior to hearing-aid refitting than both the control group and the STB FT users. After the FT users were fitted and the Experienced users were refitted with new hearing aids, the difference between the two groups was no longer significant. The FT users had a significantly higher average score after than before fitting, indicating a worse experience of their own voice. The Experienced users had the same median score before and after hearing-aid refitting but a significantly different distribution of scores (a larger interquartile range).
Very few of the STB FT users agreed with the statement “The sound of my own voice is a problem for me” before hearing-aid fitting—93% reported no or very low agreement with this statement, compared with 24% of the Experienced hearing-aid users. After hearing-aid fitting, the proportion of FT users who reported no or very low agreement went down to 55%, indicating that at least 38% of participants who previously did not perceive any problem with the sound of their own voice now agreed somewhat with the statement. A different trend was observed among the Experienced users, for whom a larger proportion (42%) did not experience any own-voice problems after hearing-aid refitting, an increase of 19 percentage points (Figure 4A).
The observation that most FT users (after being fitted with hearing aids) only rated themselves as partially agreeing with the statement, and that none indicated the strongest level of agreement, is encouraging. However, a sizeable proportion of FT users had some own-voice complaints after being fitted with hearing aids. Based on the lower ratings among STB FT users and Experienced users (compared with the control group) on Item A1 (“My own voice sounds good to me”) before hearing-aid fitting/refitting, it is suggested that hearing impairment may affect the sound quality of one’s own voice to some degree. Both the Experienced hearing-aid users and the STB FT users scored significantly more poorly than the control group before hearing-aid fitting/refitting, where the main difference between the control group and the STB FT users was that the latter had unaided hearing impairment at this point. This is in line with previous literature suggesting that a typical high-frequency hearing impairment is likely to alter the perception of one’s own voice due to the reduced audibility and loss of high-frequency features of the voice (Dillon, 2012b).
Figure 4B shows the responses to I1 (“The sound of my own voice is a problem for me”) based on four subgroups. Due to an uneven distribution of domes versus molds in the hearing-aid groups, the authors elected not to use statistical tests for these comparisons. The greatest difference before and after hearing-aid fitting in own-voice dissatisfaction was apparent among the FT-mold users. The postfitting scores for this group indicate that only 22% of the participants responded no or very low agreement with the statement after hearing-aid fitting, which (by subtracting the 10% who deemed their voice to be an issue at the start) leaves 58% of the FT-mold users who found the sound of their own voice to be a greater problem (however small or large) after fitting with hearing aids.
For the FT-dome users, there was an increase of 27 percentage points in users who found the sound of their own voice to be more problematic with hearing aids. This is in line with the conclusion drawn by Laugesen et al. (2011) that, while occlusion is important, some users have own-voice complaints that are unrelated to occlusion.
No substantial differences were found between the Experienced dome users to the Experienced mold users. Both groups experienced fewer own-voice problems after refitting than to before. One explanation for this is that the Experienced users did not have optimally fitted hearing aids at the start of the study. As described in the Materials and Methods section, hearing-aid users who come in for a refit of hearing aids generally do so because their current hearing aids are too old, are malfunctioning, or in some way do not meet their current hearing needs. Technological developments and better fittings could therefore explain why fewer Experienced users reported own-voice problems after being refitted with new hearing aids. However, by the end of their hearing-aid refitting, the majority of the participants in both the Experienced mold group (58%) and the Experienced dome group (56%) still reported that they perceived the sound of their own voice to be a problem to some extent. This may be due to the group’s higher average degree of hearing impairment (Figure 1), which implies more powerful amplification and perhaps more impact on own-voice sounds by nonlinear signal processing, for example, dynamic range compression. Increased low-frequency hearing loss has in previous studies been correlated with decreased perception of occlusion (Dillon, 2001), but it is unknown how this affects the perception of own-voice problems originating from nonocclusion related causes. One question is whether a portion of the Experienced dome users would have experienced fewer own-voice problems with molds: The Experienced dome group’s mean Four-frequency pure tone average (PTA4) was approximately equal to that of the FT-mold users. According to the audiologists at our clinic (who fitted the participants with hearing aids in the current study), some users will request domes even when the indication for their level of hearing impairment is to use molds.
Voice Intensity Control
Compression, gain settings, and signal processing in hearing aids may alter the auditory feedback of one’s own voice in such a way that they impede adequate control of vocal intensity (Dillon, 2012b; Laugesen et al., 2011; Stenfelt, 2011). Based on previous research (Coelho et al., 2015), it is likely that the decreased auditory feedback resulting from an unaided hearing impairment also poses a challenge for controlling vocal intensity appropriately.
FT users reported slightly more problems with voice intensity control after hearing-aid fitting. However, the increase was not statistically significant, and the results show that some voice intensity-related issues were present even before hearing-aid fitting. This indicates that hearing aids, in general, did not affect voice intensity control.
The Experienced users reported fewer problems with regulating vocal intensity after hearing-aid refitting, which may be related to the same potential cause as their decrease in overall perceived own-voice problems (having malfunctioning or suboptimally fitted hearing aids at, or inferior hearing-aid technology at the beginning of the study).
Speak and Hear
Signal processing and automatic settings of a hearing aid can cause the user’s voice to mask the voices of other people, which creates difficulties in hearing what other speakers are saying in a conversation with rapid turn-taking or in other situations where speech overlaps (Laugesen et al., 2011). This ability could also be affected by the underlying hearing impairment, as sensorineural hearing impairment generally reduces the ability to separate complex sounds and to identify speech in noise (Grant & Walden, 2013). Both groups with hearing impairment reported significantly more issues with speak and hear than the control group, suggesting that the ability may be more affected by hearing impairment than by use of hearing aids. The Experienced hearing-aid users reported fewer problems on average after than before hearing-aid fitting/refitting, although the difference was not significant in the ANOVA model. However, the difference in pre- and postfitting scores was significant for the Experienced users when examined with a paired t test, indicating that it is possible that significant effects were obscured by the choice of statistical model.
The hearing-aid manufacturer Signia has attempted to develop a technology for detecting the user’s own voice and processing it separately from the sound of other speakers (M. Froehlich et al., 2018; Høydal, 2017; Powers et al., 2018a, 2018b). Similar features have existed in the past in hearing aids by other manufacturers, such as Oticon (n.d.). Unfortunately, no independently published studies have appeared to date regarding the efficacy of this technology.
Disturbing Sound Qualities of Own Voice
The ratings of DSQ support the hypothesis that FT users will perceive a negative alteration in sound quality of their own voice after being fitted with hearing aids. The FT users did not differ significantly from the control group before the hearing-aid fitting, so mild-to-moderate hearing impairment in itself seems to affect the perceived sound quality of one’s own voice less than a hearing aid does.
The mean score on the DSQ section was higher for the Experienced hearing-aid users than for to the two other groups. One may have expected that this group would score fewer DSQ than the FT users, as they had prior experience of hearing their own voice through a hearing aid and should have adapted to the altered sound. However, for voice alterations due to the occlusion effect, acclimation does not occur (Kiessling et al., 2005). Disregarding occlusion effect-related problems, telling patients that they “will get used to it” can be justified by arguing that an individual with an unaided hearing impairment already has altered perception of their own voice, and the hearing aid is only making it closer to normal.
The results of the current study do not support the suggestion that own-voice dissatisfaction due to hearing aid use will disappear by itself with time. The Experienced users did not differ significantly from the FT users with regard to perceived DSQ after hearing-aid refitting. They also had the highest score on the general own-voice complaints variable. Therefore, it seems unlikely that the hearing-aid users became unaware of the altered sound of their own voice, even with time. This is in line with earlier results from Laugesen et al. (2005), who found no difference between FT and Experienced users regarding own-voice complaints. Perhaps it is not a matter of hearing-aid users becoming unaware of the altered sound of their own voice with time but instead accepting the new voice as an acceptable compromise in return for the general benefit of hearing aids. Because voice characteristics are intimately tied to identity and emotions (Spreckelmeyer et al., 2009), the affective value of the sound of one’s own voice could possibly make accepting alterations harder than for other sounds.
Methodological Considerations
Supplemental Digital Material 3 lists the revisions made to the OVQ questionnaire for the purpose of this study. The authors found that administering the OVQ questionnaire in paper format rather than as an interview worked well, although it potentially limited comparisons with the original OVQ study. The possibility of administering the OVQ as a paper questionnaire probably makes its use more likely in a clinic or in a situation where time is a factor (the original OVQ took between 39 and 63 min to administer by interview). The OVQ is the only comprehensive tool currently available for measuring own-voice sound perception related to hearing-aid use, but it is not in a standardized form. This means that it has no measure of test–retest reliability, which limits the certainty of the results of a before and after comparison.
The labels extend from completely disagree (0) to completely agree (8) in the current version of the questionnaire (an example of the original and revised scales can be seen in Supplemental Digital Content 3). For Item I1, we chose to describe the distributions of scores, in addition to statistical tests, as we considered that this offered some insight into the subgroup patterns.
To avoid information overload for the reader, responses were divided into three categories (no or very little agreement, some agreement, and strong to complete agreement). This was also considered necessary to present the data graphically in a way that was easy to grasp. We speculate that having nine levels of agreement to choose from may be too much when completing the questionnaire. In the current study, few participants used the upper part of the scale, regardless of the question. Moreover, the words used to describe sound quality are rarely used in everyday conversations, and our participants were not experienced in evaluating sound quality, so it may have been unrealistic to expect them to be able to make such a precise estimate. For example, for the statement “My own voice sounds… shrill,” a participant may interpret 0 as 0% shrillness and 8 as 100% shrillness and would choose a score of 2 or 3 to indicate that shrill qualities are present but are not predominant. A score of 2 to 3 has therefore been interpreted as “some agreement” instead of “disagree.” This introduces some additional uncertainty regarding the interpretation of the results. Therefore, we would recommend using fewer response options (or a visual-analog scale) in future studies on this topic if using the OVQ as a self-administered written questionnaire.
The self-reported benefit of hearing aids, as measured by the average difference in before and after scores on the HHIE, was statistically significant, but it was also low in comparison with the findings of some other studies (Newman & Weinstein, 1988; Stark & Hickson, 2004; Taylor, 1993). The reason for this difference is currently unknown, but it may in part reflect the fact that many participants had mild-to-moderate hearing impairment and did not report very severe consequences of their impairment before the hearing-aid fitting started.
Another methodological consideration is the number of dropouts. We do not know if the people who chose not to continue with hearing aids did so out of a particularly strong dissatisfaction with own-voice sounds. This may have affected the results in favor of hearing aids, as the remaining participants would have been the ones that tolerated the effect of their hearing aids on the sound of their own voice.
The recruitment of the control group was based on the same hearing threshold criterion as for the study of Laugesen et al. (2011). This criterion allowed for a mild degree of hearing impairment, as few individuals with perfect hearing were expected within the current age groups. However, this criterion was chosen to exclude participants in the control group who could potentially benefit from hearing aids. As can be seen in Figure 1, the control group’s maximum thresholds approximately follow the mean threshold line for the FT users. It is possible that the inclusion criterion allowed individuals with hearing thresholds similar to those for the FT users to be included in the control group. However, none of the control group participants reached the maximum threshold for all frequencies, and the mean threshold and standard deviation indicate that as a group they were unlikely to benefit from hearing aids. In retrospect, we realize that it would probably have been more appropriate to use a stricter inclusion criterion to ensure that individuals who potentially would benefit from hearing aids were excluded from the control group.
A possibility for future studies would be to recruit better matched participants with different types of hearing aids. In the present study, almost all the participants used BTE hearing aids, which are the most common type of hearing aid dispensed in Sweden. It would also be of interest to acquire an equal amount of dome and mold fittings for better comparisons. However, as individuals with PTAs under 60 dB HL generally use domes while individuals with PTAs over 60 dB HL generally use molds to achieve adequate amplification, this complicates separation of the effects of the inserts and the degree of hearing impairment.
Another idea is to consider using transparently fitted hearing aids on normal-hearing subjects to further investigate the influence of hearing aids separately from the hearing impairment.
Conclusions
The number of FT users who rated themselves as experiencing problems with the sound of their own voice increased significantly by 38 percentage points after hearing-aid fitting. Perception of some own-voice problems was frequent among Experienced users, as demonstrated by scores both before and after having their old hearing aid replaced. However, replacing older hearing aids with new ones decreased the number of Experienced users who found the sound of their own voice problematic by 19 percentage points. Pre- and postfitting scores on specific sections of the OVQ revealed that the ability to accurately control voice intensity may be affected by hearing aids to a degree but is likely more disturbed by the underlying hearing impairment. The perceived ability to speak and hear concurrent speech simultaneously is also probably mostly affected by hearing impairment, while hearing aids are the main contributing factor to problems relating to DSQ of one’s own voice.
Supplemental Material
Supplemental material, sj-pdf-1-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing
Supplemental material, sj-pdf-2-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing
Supplemental material, sj-pdf-3-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing
Data Accessibility Statement: Data will be made available upon a reasonable request.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Hearing Foundation, Swedish Association of Hard of Hearing People (grant number 2012–373) and by the Swedish Research Council (grant number 2017-06092).
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Johanna Hengen https://orcid.org/0000-0002-4715-6980
Stefan Stenfelt https://orcid.org/0000-0003-3350-8997
References
- Altman D. G., Bland J. M. (1995). Statistics notes: The normal distribution. BMJ (Clinical Research Ed.), 310(6975), 298. 10.1136/bmj.310.6975.298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Békésy G. (1949). The structure of the middle ear and the hearing of one’s own voice by bone conduction. Journal of the Acoustical Society of America, 21, 217–232. [Google Scholar]
- Bramsløw L. (2010). Preferred signal path delay and high-pass cut-off in open fittings. International Journal of Audiology, 49(9), 634–644. 10.3109/14992021003753482 [DOI] [PubMed] [Google Scholar]
- Coelho A. C., Medved D. M., Brasolotto A. G. (2015). Hearing loss and the voice. In Bahmad F., Jr. (Ed.), An update on hearing loss (pp. 103–128). IntechOpen. 10.5772/61217 [DOI] [Google Scholar]
- Dillon H. (2001). Hearing aids. Thieme. [Google Scholar]
- Dillon H. (2012. a). Compression systems in hearing aids. In Dillon H. (Ed.), Hearing aids (2nd ed., pp. 170–197). Thieme Medical Publishers Inc. [Google Scholar]
- Dillon H. (2012. b). Problem solving and fine-tuning. In Dillon H. (Ed.), Hearing aids (2nd ed., pp. 354–373). Thieme Medical Publishers Inc. [Google Scholar]
- Fry F. J., Barger J. E. (1978). Acoustical properties of the human skull. Journal of the Acoustical Society of America, 63(5), 1576–1590. 10.1121/1.381852 [DOI] [PubMed] [Google Scholar]
- Galluzzi F., Garavello W (2018). The aging voice: A systematic review of presbyphonia. European Geriatric Medicine, 9(10), 559–570. 10.1007/s41999-018-0095-6 [DOI] [PubMed] [Google Scholar]
- Ghasemi A., Zahediasl S. (2012). Normality tests for statistical analysis: A guide for non-statisticians. International Journal of Endocrinology and Metabolism, 10(2), 486–489. 10.5812/ijem.3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant K. W., Walden T. C. (2013). Understanding excessive SNR loss in hearing-impaired listeners. Journal of the American Academy of Audiology, 24(4), 258–273. 10.3766/jaaa.24.4.3 [DOI] [PubMed] [Google Scholar]
- Groth J. (2014). How do I adjust hearing aids for own voice complaints? https://www.audiologyonline.com/ask-the-experts/do-i-adjust-hearing-aids-12894
- Hengen J., Hammarström I. L., Stenfelt S. (2018). Perceived voice quality and voice-related problems among older adults with hearing impairments. Journal of Speech, Language, and Hearing Research, 61(9), 2168–2178. 10.1044/2018_JSLHR-S-17-0383 [DOI] [PubMed] [Google Scholar]
- Høydal E. H. (2017). A new own voice processing system for optimizing communication. Hearing Review, 24(11), 20–22. http://www.hearingreview.com/2017/10/new-voice-processing-system-optimizing-communication/ [Google Scholar]
- Jacobson B. H., Johnson A., Grywalski C., et al. (1997). The Voice Handicap Index (VHI): Development and validation. American Journal of Speech-Language Pathology, 6(3), 66–70. 10.1044/1058-0360.0603.66 [DOI] [Google Scholar]
- Keidser G., Dillon H. (2006). What’s new in prescriptive fittings Down Under? In Palmer C. V., Seewald R. (Eds.), Hearing care for adults (pp. 133–142). Phonak AG. [Google Scholar]
- Kiessling J., Brenner B., Jespersen C. T., et al. (2005). Occlusion effect of earmolds with different venting systems. Journal of the American Academy of Audiology, 16(4), 237–249. [DOI] [PubMed] [Google Scholar]
- Kochkin S. (2002). MarkeTrak VI: 10-Year customer satisfaction trends in the US hearing instrument market. Hearing Review, 9(10), 14–25. [Google Scholar]
- Kochkin S. (2005). MarkeTrak VII: Customer satisfaction with hearing instruments in the digital age. The Hearing Journal, 58(9), 30–43. [Google Scholar]
- Kochkin S. (2010). MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing. The Hearing Journal, 63(1), 19–32. 10.1097/01.Hj.0000366912.40173.76 [DOI] [Google Scholar]
- Kuk F, Ludvigsen C. (2002) Ampclusion management 101: Understanding variables. Hear Rev 9(8):22–32.
- Laugesen S., Jensen N. S., Maas P., et al. (2011). Own voice qualities (OVQ) in hearing-aid users: There is more than just occlusion. International Journal of Audiology, 50(4), 226–236. 10.3109/14992027.2010.547991 [DOI] [PubMed] [Google Scholar]
- Laugesen S., Vestergaard H., Nielsen C. (2005). Common conceptions about first-time versus experienced hearing-aid users: Facts or fiction? In A.N. Rasmussen, T. Poulsen, T. Andersen and C.B. Larsen (eds)Proceedings of the 21st Danavox symposium (pp. 261–297).
- M. Froehlich, T. Powers, E. Branda, J. Weber (2018). Perception of own voice wearing hearing aids: Why “natural” is the new normal. AudiologyOnline, Article 22822. https://www.audiologyonline.com/articles/perception-own-voice-wearing-hearing-22822
- Mircioiu C., Atkinson J. (2017). A comparison of parametric and non-parametric methods applied to a Likert scale. Pharmacy (Basel, Switzerland), 5(2), 26. 10.3390/pharmacy5020026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman C. W., Weinstein B. E. (1988). The Hearing Handicap Inventory for the Elderly as a measure of hearing aid benefit. Ear and Hearing, 9(2), 81–85. [DOI] [PubMed] [Google Scholar]
- Öberg, M., Lunner, L., & Andersson, G. (2016). Validation of the Swedish Hearing Handicap Inventory for the Elderly (Screening Version) and evaluation of its effect in hearing aid rehabilitation. Trends in Hearing, 20. 10.1177/2331216516639234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohlsson A. C., Dotevall H. (2009). Voice handicap index in Swedish. Logopedics Phoniatrics Vocology, 34(2), 60–66. 10.1080/14015430902839185 [DOI] [PubMed] [Google Scholar]
- Oticon. (n.. d.). Oticon Epoq [Product phamplet]. https://www.oticon.es/-/media/oticon/main/pdf/master/epoq/pbr/91016910_epoq2nd_pbr.pdf
- Pimentel J. (2019). Some biases in Likert scaling usage and its correction. International Journal of Science: Basic and Applied Research (IJSBAR), 45(1), 183–191. [Google Scholar]
- Pörschmann C. (2000). Influences of bone conduction and air conduction on the sound of one’s own voice. Acta Acustica, 86, 7. [Google Scholar]
- Powers T., Froehlich M., Branda E., et al. (2018. b). Clinical study shows significant benefit of own voice processing. Hearing Review, 25(2), 30–34. http://www.hearingreview.com/2018/01/clinical-study-shows-significant-benefit-voice-processing/ [Google Scholar]
- Powers T. A., Davis D. B., Apel D., et al. (2018. a). Own voice processing has people talking more. Hearing Review, 25(7), 42–45. http://www.hearingreview.com/2018/06/voice-processing-people-talking/ [Google Scholar]
- Reinfeldt S., Ostli P., Hakansson B., et al. (2010). Hearing one’s own voice during phoneme vocalization–transmission by air and bone conduction. Journal of the Acoustical Society of America, 128(2), 751–762. 10.1121/1.3458855 [DOI] [PubMed] [Google Scholar]
- Simon S. (2009). Use of Likert data with ANOVA. The Monthly Mean. http://www.pmean.com/09/LikertAnova.html
- Spreckelmeyer K. N., Kutas M., Urbach T., et al. (2009). Neural processing of vocal emotion and identity. Brain and Cognition, 69(1), 121–126. 10.1016/j.bandc.2008.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark P., Hickson L. (2004). Outcomes of hearing aid fitting for older people with hearing impairment and their significant others. International Journal of Audiology, 43(7), 390–398. [DOI] [PubMed] [Google Scholar]
- Stenfelt S. (2011). A model of prediction of own voice alteration with hearing aids. In T. Dau, M. L. Jepsen, J. Christensen-Dalsgaard, & T. Poulsen (Eds.), Proceedings of the Third International Symposium on Auditory and Audiological Research 2011 (pp. 323–330). Danavox Jubilee Foundation.
- Stenfelt S. (2016). Model predictions for bone conduction perception in the human. Hearing Research, 340, 135–143. 10.1016/j.heares.2015.10.014 [DOI] [PubMed] [Google Scholar]
- Stenfelt S., Goode R. L. (2005). Bone-conducted sound: Physiological and clinical aspects. Otology & Neurotology, 26(6), 1245–1261. [DOI] [PubMed] [Google Scholar]
- Stenfelt S., Reinfeldt S. (2007). A model of the occlusion effect with bone-conducted stimulation. International Journal of Audiology, 46(10), 595–608. 10.1080/14992020701545880 [DOI] [PubMed] [Google Scholar]
- Stenfelt S., Wild T., Hato N., Goode R. (2003). Factors contributing to bone conduction: The outer ear. Journal of the Acoustical Society of America 113(2), 902–913. [DOI] [PubMed] [Google Scholar]
- Stone M. A., Moore B. C. J. (1999). Tolerable hearing aid delays. I. Estimation of limits imposed by the auditory path alone using simulated hearing impairments. Ear and Hearing, 20(3), 182–192. [DOI] [PubMed] [Google Scholar]
- Taylor K. S. (1993). Self-perceived and audiometric evaluations of hearing aid benefit in the elderly. Ear and Hearing, 14(6), 390–394. [DOI] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1982). The hearing handicap inventory for the elderly: A new tool. Ear and Hearing, 3(3), 128–134. [DOI] [PubMed] [Google Scholar]
- Winkler A., Latzel M., Holube I. (2016). Open versus closed hearing-aid fittings: A literature review of both fitting approaches. Trends in Hearing, 20, 1–13. 10.1177/2331216516631741 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing
Supplemental material, sj-pdf-2-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing
Supplemental material, sj-pdf-3-tia-10.1177_2331216520932467 for Perception of One’s Own Voice After Hearing-Aid Fitting for Naive Hearing-Aid Users and Hearing-Aid Refitting for Experienced Hearing-Aid Users by Johanna Hengen, Inger L. Hammarström and Stefan Stenfelt in Trends in Hearing