Background
Coping is defined as a set of cognitive and behavioral efforts made to master stressful specific demands. Adaptation to chronic diseases, such as Multiple Sclerosis (MS), depends on the effectiveness of coping.
Objective: To assess the psychometric properties of the Coping Responses Inventory (CRI-A) in persons with MS (PwMS), verifying the transferability of the measure, already validated in the Argentine general population, and to describe the types of coping strategies available for PwMS.
Methods: 90 PwMS were included.
Outcome measures: CRI-A Inventory, Expanded Disability Status Scale (EDSS), Beck Depression Inventory, Fatigue Severity Scale and MS International Quality of Life questionnaire.
Results: Descriptive data is as follows: mean age (years): 40.97 ± 12.85; years of education: 13.46 ± 3.93; EDSS: 2.48 ± 1.79; disease evolution (years): 10.76 ± 9.72; depression: 13.92 ± 10.45; fatigue 3.77 ± 1.72. The psychometric properties of the CRI-A Inventory observed in the Argentine general population are present in the MS sample as well, with adequate validity and reliability. The respondents most frequently utilized a problem-focused coping style.
Conclusions: Results showed the CRI-A has good transferability properties from the Argentine general population to the MS population.
Keywords: Coping, psychometric properties, transferability, depression, multiple sclerosis
Introduction
Multiple Sclerosis (MS) is a chronic neurological disease affecting mainly young adults, producing a set of physical, emotional and cognitive symptoms that alter quality of life.1,2 Traditionally, a substantial amount of clinical data related to symptoms, diagnostic and therapeutic measures are registered throughout the course of the disease. However, little information is collected from patients’ reports, even though they represent meaningful, reliable data. In this line, Patient Reported Outcome Measures (PROMs) are used to assess the individual’s level of disability, and to improve quality of life by identifying the aspects of life patients consider the most relevant.3,4
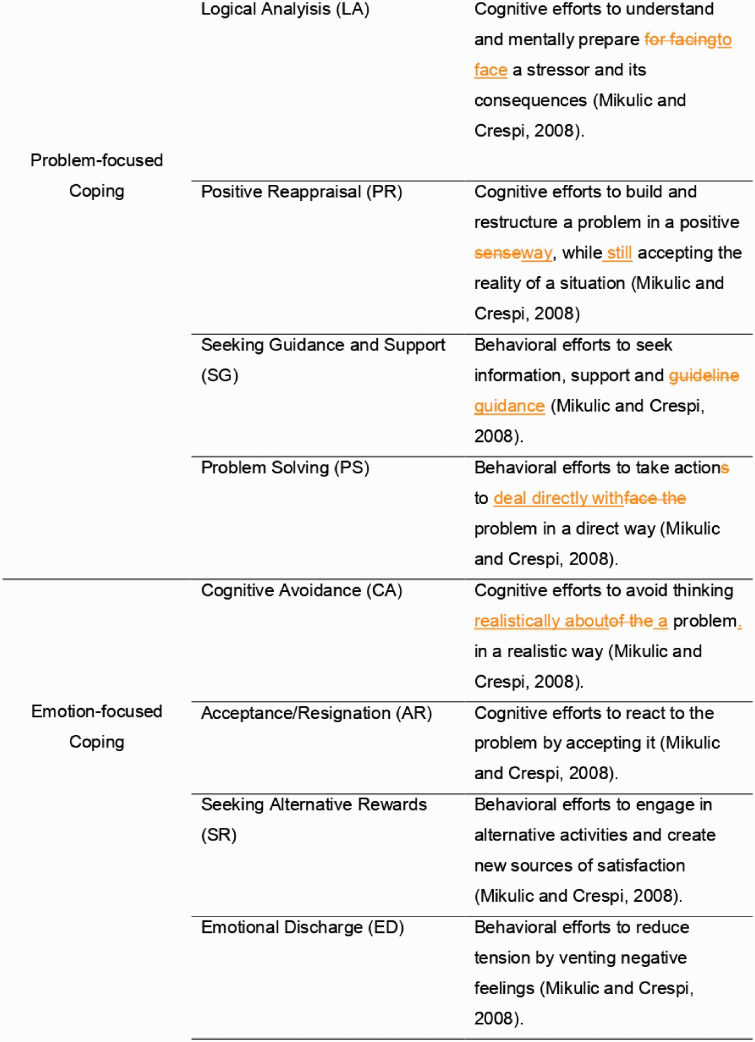
Persons with MS (PwMS) are constantly exposed to a variety of stressful situations. Living with such a disabling disease requires constant coping with disabilities and dysfunctions on a daily basis, which creates a continual process of adjustment.5 Stress arises from the relationship between individuals and one or many unfavorable situations that are perceived as exceeding their own resources.6 The concept of coping refers to the cognitive and behavioral efforts to manage internal or external stressful demands, which can be appraised as aggravating or exceeding personal resources.7 Coping is thus presented as a stabilizing factor that may help individuals maintain their psychosocial adaptation during periods of high levels of stress, working as a mediating or regulatory variable on the destabilizing effects of stress.7 Contemporary theories emphasize the multidimensional aspects of coping strategies by addressing different perspectives for their classification. There are basically two main conceptual perspectives regarding coping. One perspective emphasizes orientation or focus, differentiating active and passive ways of dealing with a problem. Based on the focus of coping, a second classification comprises approach responses – defined as cognitive or behavioral efforts to deal directly with the stressful event –, and avoidance coping responses, which encompass cognitive and/or behavioral efforts to avoid thinking of the stressor or to reduce tension through escape behaviors.8 The second classification perspective focuses on the method of coping.9 The coping model proposed by Moos8 introduces two coping styles. The first one represents the problem-focused coping, also known as approach strategy, and comprises logical analysis, positive reappraisal, seeking guidance and support, and problem solving strategies, which contribute to actively resolve stressors. The second style represents the emotion-focused coping, also known as avoidance strategy, and comprises cognitive avoidance, acceptance-resignation, seeking alternative rewards, and emotional discharge strategies, aimed at avoiding thinking of a stressor and its implications. These styles and strategies are depicted in Figure 1.
Figure 1.
Description of coping styles and strategies measured by the CRI-A.
Adaptation to chronic illness depends on coping effectiveness. PwMS are more likely to use emotion-focused strategies than problem-focused ones.5 Furthermore, they adopt avoidance strategies more frequently than active strategies to improve their health.10 Findings have shown that emotion-focused coping and avoidance coping are associated with low levels of quality of life, while problem-focused coping is related to high levels of quality of life.11 In addition, a consistent relationship between depression, anxiety and emotion-focused strategies has been identified.5 Moos introduces the idea that the specific characteristics of a crisis or vital transition contextualize the selection of specific coping responses.12 According to Holahan, Moos and Brennan,13 a high number of negative vital life events and chronic stressors lead to a greater use of avoidance responses. Thus, coping responses are influenced by the type, severity and assessment of the stressor, which shows that the relationship between coping styles and the specific characteristics of the situation must be taken into account.13 Coping styles have also been associated with adherence to medication. Grytten and colleagues14 have revealed that patients recently diagnosed with MS who adopt avoidance strategies are less likely to start pharmacological treatment. Furthermore, as far as different treatments are concerned, patients who implement active coping strategies are more likely to exhibit greater adherence to treatment with injectable drugs than those who rely on emotion-focused strategies.15
To date, there are no studies in Argentina focused on coping styles adopted by PwMS and the influence these styles may have on health-related quality of life (HRQoL). There are several coping measurement instruments available, among which the “Ways of Coping Checklist”,16 “Coping with Health, Injuries and Problems Scale”,17 “Coping Inventory for Stressful Situations”18 and “Coping Responses Inventory (CRI-A)”8 instruments stand out. The only instruments validated in Argentina is the CRI-A and the Ways of Coping Checklist has been validated, but although the authors have not reported the procedure followed to carry out the adaptation.19
The CRI-A has also been administered to patients with other diseases as well as to healthy population samples,20,21 providing a significant contribution to the study of coping processes in the adult population.9 From a social ecological conceptual framework, the CRI-A combines the two coping perspectives, assessing both the coping orientation or focus and, the coping method.8 Moreover, Mikulic and Crespi9 administered the Argentine Spanish version of the CRI-A to the adult population, and the results showed adequate coefficients of consistency on both the overall test and on each specific dimension. The authors report that the obtained alpha indexes are consistent with those of the original validation of the scale,8 and assert that the instrument meets sufficient requirements for factorial validity.9 Given the presence of the Argentine validation of the CRI-A instrument, the objectives of this study were: (1) to evaluate the psychometric properties of the CRI-A in the subpopulation of PwMS, in order to verify the transferability of the instrument, which has had already been validated in the Argentine general population: (1.a) to assess construct validity, (1.b) to assess reliability, (1.c) to assess external criterion validity, by studying the relationship between coping styles and physical disability, depression, fatigue, disease evolution and clinical course, and health-related quality of life of PwMS, and (2) to describe the types of coping strategies adopted by PwMS.
Methods
Design
A cross-sectional, descriptive-correlational and analytic design was implemented in this study. The sample consisted of 90 patients diagnosed with MS, who were recruited through an incidental strategy of non-probabilistic sampling. All the subjects who attended to their neurological consultations and met the inclusion and exclusion criteria were invited to participate.
Inclusion criteria were: 1) age ≥18 years, and 2) MS diagnosis according to the 2010 revisions of McDonald criteria,22 including any of the 3 clinical types of the disease (RelapsingRemitting (RRMS), Primary-Progressive (PPMS) or Secondary-Progressive (SPMS). Exclusion criteria included: 1) severe visual or hearing impairment, 2) medical history that may affect cognition or personality, such as a psychiatric or a neurological disease other than MS, 3) history of alcohol or drug abuse, 4) uncontrolled systemic disease, and 5) history of relapses or corticoids administration within four weeks preceding the study.
Written informed consent was provided by all participants. The study as well as the informed consent form were approved by the Institutional Ethics Committee.
Measurement instruments
Coping was measured using the Argentine Spanish version of the CRI-A.9 The instrument was translated and adapted to our context in a sample of 805 healthy adults. The reliability coefficient was the alpha coefficient, calculated by assessing the internal consistency of the elements. Cronbach’s alpha coefficient was high (.85), and the coefficients of the eight coping dimensions were acceptable (ranging from .51 to .81). The scale assesses eight strategies: logical analysis, positive reappraisal, seeking guidance and support, problem solving, cognitive avoidance, acceptance/resignation, seeking alternative rewards, and emotional discharge. These strategies are depicted in Figure 1. The strategies are operationalized as eight separate variables. The procedure is detailed below.
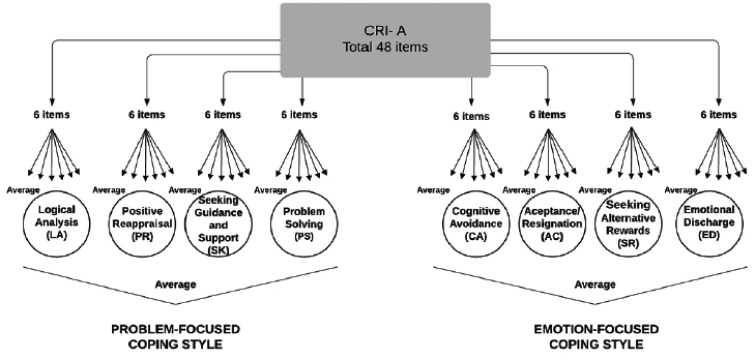
Following the CRI-A instructions, examinees were required to complete the first part of the scale, answering ten items on the assessment of the stressor or problem they have defined. In this study, the diagnosis of MS was assigned as the stressor to all participants. The second part is composed of 48 items that must be answered using a scale that ranges from 0 ("never") to 3 ("several times"). These 48 items are grouped into eight variables that represent eight coping strategies (see Figure 1), and these, in turn, are divided into two coping styles (problem and emotion styles). Regarding the scoring procedure, the values of the six items that make up each of the eight variables are added and then divided by the number of items answered. Then, the scores of the four strategies that make up each coping style (problem-focused style and emotion-focused style) are added and divided by four.9 Figure 2 illustrates the scoring procedure of the eight strategies and the two copying styles It should be clarified that the first ten items in the problem description part of the scale are not included in the final score.
Figure 2.
Description of the procedure for obtaining CRI-A scores.
CRI-A: Coping Responses Inventory-Adult.
HRQoL was measured using the Multiple Sclerosis International Quality of Life questionnaire (MusiQol).23 In the validation manuscript of the scale – which includes the participation of Argentina –the Cronbach Index ranges from 0.68 to 0.92 for all the dimensions of the instrument.23 The MusiQoL includes 31 items describing nine dimensions of HRQoL, which are as follow: activities of daily living, psychological well-being, symptoms, relationships with friends, relationships with family, relationships with health care system, sentimental and sexual life, coping, and rejection.
Additionally, the Expanded Disability Status Scale (EDSS),24 the Argentine version25 of the Fatigue Severity Scale (FSS)26 and the Argentine version27 of the Beck Depression Inventory28 were administered.
A MS neurologist collected the clinical data, performed the neurological examination and assessed the EDSS. An experienced psychologist assisted in the administration of self-report questionnaires to assess coping, HRQoL, fatigue and depression scales.
Statistical analysis
Data were analyzed using the IBM SPSS Statistics, 20.0 version and the STATA, 13 version. Descriptive and inferential analyses were performed to address every objective.
Cronbach’s alpha of the six items comprising each of the eight strategies (variables) were analyzed and compared to the findings of the original validation study (see Table 2). An exploratory factor analysis was performed (see operationalization of the eight variables -strategies- in 2.2 Measurement Instruments).
Table 2.
CRI-A’s Cronbach's alpha coefficients for PwMS and the general population.
| PwMS | General population | ||
|---|---|---|---|
| Problem-focused coping | 4 strategies | .81 | .81 |
| 5 strategies | .83 | ||
| Emotion-focused coping | 4 strategies | .53 | .79 |
| 3 strategies | .59 | ||
| Logical analysis | .77 | .57 | |
| Positive reappraisal | .69 | .59 | |
| Seeking guidance and support | .44 | .51 | |
| Problem solving | .69 | .68 | |
| Cognitive avoidance | .68 | .65 | |
| Acceptance/resignation | .53 | .59 | |
| Seeking alternative rewards | .64 | .67 | |
| Emotional discharge | .55 | .52 |
CRI-A: Coping Responses Inventory-adult; PwMS: persons with multiple sclerosis.
The objectives of this study were to assess the psychometric properties of the instrument, already validated, in a particular subpopulation of the country,29 and to prove its transferability. For this reason, the exploratory factor analysis was used for construct validity of the eight variables derived from the CRI-A instrument, based on the publication of the instrument9 (see operationalization in 2.2 Measurement Instruments). Specifically, we conducted an exploratory factor analysis with Oblimin rotation for three reasons: the strategies (variables) are not independent, it is the type of analysis used in the original study9 and it is a method that has been widely accepted by international literature.30
Although the original study established that four strategies (variables) were problem-oriented and four strategies were emotion-oriented, the authors also reported that five variables were loaded on the problem-focused style factor, and three were loaded on the emotion-focused style factor.9 Therefore, we decided to calculate Cronbach’s alpha coefficient for the eight variables as a whole, divided in two groups of four variables, and in two groups of five and three variables.
Pearson correlations were implemented for external criterion validity on the average score of the eight strategies (variables) to study the association between demographic and clinical variables, and quality of life. Pearson correlations were chosen because the variables are continuous and the sample size is over 30. Therefore, according to the central limit theorem, even if the variables do not show a normal distribution, the method is still robust. To compare the results of the correlations, Cohen’s ranges for effect sizes were calculated. Based on Cohen,31 the effect sizes for the correlation coefficient r are the following: small (0.10), medium (0.30) and large (0.50).
Calculation of sample size
According to the literature,32 exploratory factor analyses require a minimum of 10 cases per variable and no less than 50 in total.33 Our minimum sample size was 80 and the study was carried out with 90 cases.
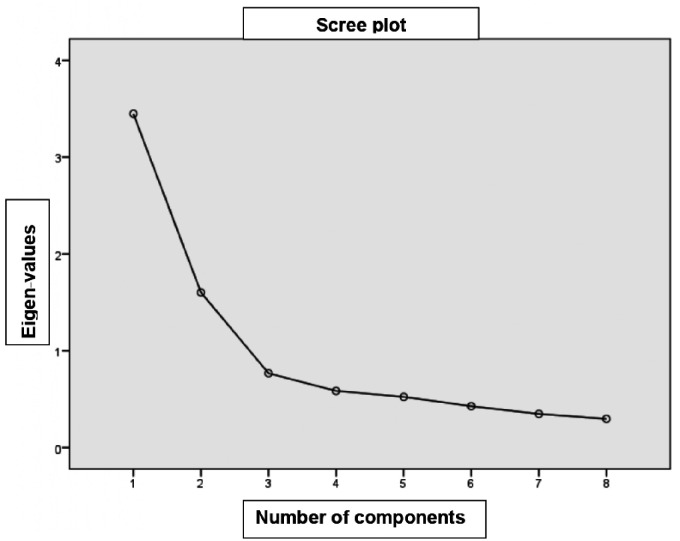
Results
Descriptive data are as follows: 95.56% of the patients had RRMS, 2.22% PPMS, and 2.22% SPMS. The group comprised of 59 women (65.56%), with a mean age of 40.97 ± 12.85 years and a mean education of 13.46 ± 3.93 years. The mean disease evolution was 10.76 ± 9.72 years. The group exhibited a mean depression score of 13.92 ± 10.45 for, a mean fatigue score of 3.77 ± 1.72, and a mean disability score of 2.48 ± 1.79. Bartlett’s test of sphericity displayed a KMO = 0.795 index and a value of p = 0.00001, allowing for a factor analysis using the means of the eight coping strategies, which resulted in a structure matrix with two factors. Factor loadings of each variable varied between 0.68 and 0.82, as presented in Table 1. A scree plot was developed to determine the number of factors to retain (Figure 3). The Kaiser criterion (to retain factors with eigenvalues greater than 1) was also taken into consideration, and both methods agreed on the retention of two factors. The first factor refers to the problem-focused coping style and comprises the following strategies (operationalized as variables, as explained above): logical analysis, positive reappraisal, seeking guideline and support, problem solving and seeking alternative rewards. However, according to the original author of the inventory (CRI-A), the strategy of seeking alternative rewards belongs to the emotion-focused coping style. In the validation study of the CRI-A on the validation in the general population of Argentina, this strategy also loaded on the problem-focused factor, as in other studies.9 The second factor refers to the emotion-focused coping style and comprises the following strategies (operationalized as variables, as explained above): cognitive avoidance, acceptance-resignation, and emotional discharge.
Table 1.
Factor loadings of each coping strategy.
| Pattern matrix |
Structure matrix |
||||
|---|---|---|---|---|---|
| Component |
Component |
||||
| Item | 1 | 2 | Item | 1 | 2 |
| LA | .597 | .460 | LA | .685 | .574 |
| PR | .809 | –.015 | PR | .806 | .139 |
| SG | .792 | .088 | SG | .808 | .239 |
| PS | .854 | –.156 | PS | .824 | .007 |
| CA | –.086 | .748 | CA | .057 | .731 |
| AR | –.112 | .848 | AR | .050 | .827 |
| SR | .789 | –.099 | SR | .770 | .052 |
| DE | .391 | .540 | DE | .494 | .615 |
LA: logical analysis; PR: positive reappraisal; SG: seeking guidance and support; PS: problem solving; CA: cognitive avoidance; AR: acceptance/resignation; SR: seeking alternative rewards; ED: emotional discharge.
Figure 3.
Scree plot of eigenvalues determine the number of factors to retain.
Both coping styles were analyzed using Cronbach’s alpha coefficient to assess the reliability of the instrument. Cronbach's index of the eight strategies (variables) is 0.786. Originally, each style comprised four strategies (variables). After the previously described factor analysis, it was determined that the problem-focused coping style comprises five strategies (variables) and emotion-focused coping style combines three strategies (variables). Cronbach’s alpha coefficient was calculated as a coefficient of reliability based on the internal consistency of the elements. Cronbach’s alpha coefficients for both coping styles (consisting of four strategies each) were computed. The results obtained were α = .816 for problem-focused coping and α = .532 for emotion-focused coping. The same procedure was performed with the five-factor problem-focused coping style, and the three-factor emotion-focused coping style. Results showed acceptable Cronbach’s alpha coefficients (minimum value of 0.6)33 for the five-factor problem-focused coping style (α = 0.839) and the three-factor emotion-focused coping style (α = 0.596). Cronbach’s alpha coefficients exhibited lower scores for four-factor coping styles (see Table 2), which is explained by the inclusion of the seeking alternative rewards strategy in the emotion-focused coping style. With the purpose of assessing the reliability of the instrument, a comparison was made between the values obtained in the present study and the ones reported in the general population study,9 as shown in Table 2. It must be noted, though, that the analyses in the Mikulic and Crespi study were carried out based on the total amount of items, as a global score, whereas a factorial analysis taking into account the eight strategies was performed in this study.
To assess the external criterion validity, and using the factor analysis included in this manuscript (transferability) as well as the one of the validation in the general population of Argentina,9 correlations were performed between the five-strategy problem-focused coping style consisting of five strategies –logical analysis, positive reappraisal, seeking guidance and support, problem solving, and seeking alternative rewards–, and the three-strategy emotion-focused coping style, consisting of three strategies –cognitive avoidance, acceptance-resignation, and emotional discharge– (see Table 3). When analyzing the association with demographic variables, a significant moderate positive correlation was found between the problem-focused coping style and years of education (r = 0.31, p < 0.01), whereas no relation to patients’ age was identified. As regards to clinical variables, a significant small to moderate positive correlation was found between the emotion-focused coping style and fatigue severity (r = 0.21) and a significant moderate to large correlation was observed with depression symptoms (r = 0.43). No significant correlation was established between coping styles and disease evolution and disability clinical variables. Nevertheless, when studying each of the eight coping strategies separately, a significant small to moderate positive correlation was found between two strategies of the emotion-focused coping style, avoidance (r = 0.27), acceptance (r = 0.27) and a moderate to large correlation with the emotional discharge strategy (r = 0.42). In addition, the seeking alternative rewards strategy exhibited a small to moderate correlation with the disease evolution and fatigue severity (r = 0.24 and r = −0.22 respectively). When analyzing the relationship between coping and HRQol dimensions, several associations were observed between problem-focused coping and the following dimensions: significant small to moderate positive correlations relationships with family (r = 0.24), relationships with friends (r = 0.23), and medium correlation with sentimental and sexual life (r = 0.32, p < 0.01). Furthermore, the emotion-focused coping style presented significant medium to large negative correlations with psychological well-being (r = −0.39, p < 0.05) and coping (r = −0.43, p < 0.01), and a significant small to moderate negative correlation with rejection (r = −0.23, p < 0.01) and the total quality of life index (r = −0.23, p < 0.05). After a detailed study of the relationship between the eight coping strategies and HRQol, a significant small to moderate positive relation was identified between the seeking alternative rewards strategy and activities of daily living dimension (r = 0.25), a medium correlation with sentimental and sexual life dimension (r = 0.33) and relationships with friends dimension (r = 0.31). The positive reappraisal strategy displayed a small to moderate correlation with relationships with friends dimension (r = 0.23). The problem solving strategy was moderately correlated with sentimental and sexual life (r = 0.30) and the emotional discharge strategy displayed a high negative association with psychological well-being dimension (r = 0.50) and also presented a small to moderate correlation with symptoms dimension (r = −0.27). No significant associations were observed between the remaining coping strategies and HRQol.
Table 3.
Correlations between the CRI-A and clinical and HRQoL variables.
| PFC | EFC | LA | PR | SG | PS | SR | CA | AR | ED | |
|---|---|---|---|---|---|---|---|---|---|---|
| Education | 0.31** | 0.09 | 0.30** | 0.18 | 0.20* | 0.25* | 0.22* | –0.006 | –0.09 | 0.12 |
| Disease evolution (years) | 0.03 | 0.07 | 0.04 | –0.03 | –0.01 | 0,11 | 0.24* | –0.14 | –0.001 | 0.10 |
| Fatigue | 0.03 | 0.21* | 0.17 | –0.03 | 0.10 | –0.14 | –0.22* | 0.19 | 0.11 | 0.16 |
| Depression | 0.05 | 0.43* | 0.15 | –0.11 | 0.05 | –0.02 | –0.11 | 0.27** | 0.27** | 0.42** |
| Total HRQoL | 0.14 | –0.23* | 0.03 | 0.21* | 0.05 | 0.18 | 0.28* | –0.07 | –0.16 | –0.29* |
| ADL | 0.14 | 0.02 | 0.08 | 0.20 | –0.01 | 0.15 | 0.25* | –0.04 | –0.01 | –0.16 |
| Psychological well-being | –0.03 | –0.39* | –0.15 | 0.05 | –0.05 | 0.06 | 0.17 | –0.20 | –0.18 | –0.50** |
| Symptoms | 0.02 | –0.23* | –0.01 | 0.04 | 0.04 | 0.01 | 0.02 | –0.09 | –0.16 | –0.27* |
| Relationships with friends | 0.23* | 0.21 | 0.06 | 0.23* | 0.13 | 0.18 | 0.31* | 0.14 | 0.01 | 0.06 |
| Relationships with family | 0.24* | 0.05 | 0.18 | 0.20 | 0.21 | 0.23 | 0.13 | 0.14 | –0.07 | –0.11 |
| Relationships with health care system | –0.03 | 0.11 | –0.03 | –0.06 | 0.02 | –0.02 | 0.06 | –0.08 | 0.17 | 0.15 |
| Sentimental and sexual life | 0.32** | 0.19 | 0.20 | 0.30* | 0.16 | 0.30** | 0.33** | 0.08 | 0.01 | 0.07 |
| Coping | –0.11 | –0.43** | –0.10 | –0.01 | –0.15 | –0.13 | –0.05 | 0.27* | 0.27** | 0.42** |
| Rejection | 0.02 | –0.23* | –0.10 | 0.11 | –0.07 | 0.12 | 0.13 | –0.12 | –0.15 | –0.26 |
HRQoL: Health-related quality of life; ADL: activities of daily living; PFC: problem-focused coping; EFC: emotion-focused coping; LA: logical analysis; PR: positive reappraisal; SG: seeking guidance and support; PS: problem solving; CA: cognitive avoidance; AR: acceptance/resignation; SR: seeking alternative rewards; ED: emotional discharge.
**Significant correlation of p < 0.01 (bilateral).
*Significant correlation of p < 0.05 (bilateral).
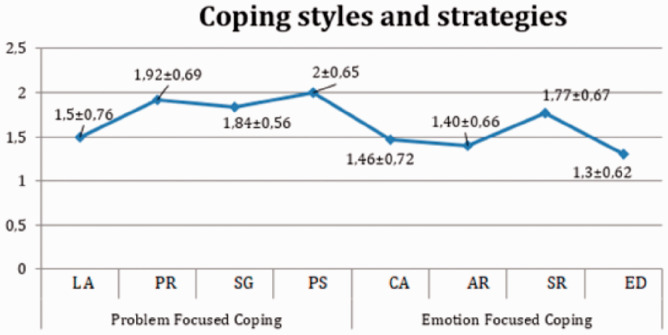
In relation to the second objective, regarding the type of coping style adopted, PwMS employed more problem-focused (with a mean of 1.81 ± 0.54) than emotion-focused strategies (with a mean of 1.48 ± 0.43). The most frequently used problem-focused strategies were: problem solving (2 ± 0.65), positive reappraisal (1.92 ± 0.69), seeking guidance and support (1.84 ± 0.56), seeking alternative rewards (1.77 ± 0.67) and logical analysis (1.50 ± 0.76).The least frequently used emotion-focused strategies were: cognitive avoidance (1.46 ± 0.72), acceptance (1.40 ± 0.66), and emotional discharge (1.30 ± 0.62) (Figure 4).
Figure 4.
Results of CRI-A’s problem-focused and emotion-focused coping strategies.
LA: logical analysis; PR: positive reappraisal; SG: seeking guidance and support; PS: problem solving; CA: cognitive avoidance; AR: acceptance/resignation; SR: seeking alternative rewards; ED: emotional discharge.
Discussion and conclusion
The aim of this study was to analyze the psychometric properties of the CRI-A instrument. It has been demonstrated that the CRI-A maintains similar psychometric properties in both the Argentine general population and PwMS, particularly in patients with RR clinical form. These findings reflecting adequate validity and reliability, advocate for the inventory’s transferability to the PwMS population. As regards to construct validity, the change in the number of strategies per style should be mentioned, since the seeking alternative rewards strategy that originally placed within the emotion-focused coping style in the CRI-A was loaded on the problem-focused coping style in the present study, replicating the findings of the general Argentine population validation study9 and other studies, such as the Spanish validation.34 A section of the Spanish version was used on PwMS, given that the research focused only on stressor-induced stress, and the findings indicated associations between the scores on this scale, depression and social functioning values.35
Regarding the second objective, findings showed that patients with a higher education level were more likely to adopt problem-focused coping styles. They tended to cope adaptively with the disease, utilizing their resources to actively master or resolve the source of stress, seeking information, support, guideline and alternative activities to create new sources of satisfaction. These results are in line with Goretti and colleagues.10
As far as clinical aspects are concerned, patients with high levels of fatigue or depression were more likely to exhibit the emotion-focused coping style. Such patients adopted strategies that may help them change the level of distress and manage the emotional states caused by the stressor by attempting to avoid thinking of the disease, venting their emotions by crying, and resigning themselves to the disease. The relationship between depression and coping styles has been researched for a long time, the consensus is that patients with depression employ emotion-focused strategies and are less likely to use active coping.36
Several significant correlations were found between coping styles and different aspects of HRQoL. Although many are weak correlations, the observed magnitude is broadly in line with the average effect-size reported in the context of psychological testing.37 Patients with closer relationships with family and friends, and better sentimental and sexual lives obtained higher scores in problem-focused coping strategies, adopting an active approach against the stressor. On the other hand, patients with lower psychological well-being and lower scores in quality of life related to coping and the feeling of rejection dimensions obtained higher scores in emotion-focused strategies, which denotes greater efforts to avoid thinking of a stressor – which, in this study, is the diagnosis of MS – and its implications. Evidence of patients with an increased use of problem-focused coping strategies showing better HRQoL38 is consistent throughout the literature.38
Regarding coping styles and strategies adopted by PwMS, findings showed that these patients prefer to use problem-focused strategies. Some subjects employed emotion-focused strategies, especially cognitive avoidance and acceptance mechanisms. Coping styles are not independent or mutually exclusive, but rather, they complement each other when facing most stressful events, such as living with a chronic disease.39 Similar results were reported by Moreau et al.40 on RRMS patients, who largely opted for problem-focused strategies. However, other PwMS from the same sample employed emotion and avoidance-focused strategies.40 On the contrary, other studies, such as Montel and colleagues publication16 reported different results, describing a preference for emotion-focused strategies. One of the possible reasons patients adopted less effective, emotion-focused strategies may have been associated with the presence of more severe clinical symptoms and the uncertainty surrounding the availability of pharmacological treatment for SPMS at the time the research was conducted. PwMS recruited for the present study exhibited low levels of depressive symptoms, which could partially explain the high prevalence of problem-focused strategies. The reported findings are consistent with Moreau’s40 who also observed a preference for problem-solving strategies and excluded PwMS with severe depression from his sample, as we did in this study. Our findings on the relationship between depression and emotion-focused style are supported by Rabinowitz and Arnett36. Taken together, these data indicate that, had our sample included greater depressive symptoms, PwMS might have opted for emotion-focused strategies. Evidence for coping strategies used by MS patients is inconsistent,38 probably due to the multidimensionality of coping and the sociocultural variability of each population.
The current sample displays a high prevalence of RRMS patients and no evidence of recent exacerbation or relapse, suggesting the recruited patients might present a less active form of MS. Therefore, the obtained results herein might be interpreted as being similar to those of the general population. However, patients still have to cope with the diagnosis of a chronic illness such as MS, regardless of the specific clinical manifestations of each patient. As Ambrosio et al.41 explained, living with a chronic illness is a complex, dynamic, cyclical and multidimensional process aimed at achieving “positive living”. Therefore, persons with chronic illnesses need to learn to take better care of themselves given their circumstances.42 Study comparing PwMS and control subjects such as Lode et al.43 observed that patients employed fewer problem-focused coping strategies than healthy controls.
Even though this study provides novel, valuable contributions to the description of coping mechanisms in PwMS in Argentina, limitations arose when trying to compare the different studies on the subject matter, since each study employed different instruments and the population is represented mainly by RRMS patients.
In conclusion, the results obtained confirm the transferability of CRI-A to patients with RRMS. Patients with more years of education tended to cope with the disease more adaptively, and PwMS prefer to use coping strategies focused on the problem, which suggests an approach to stressful situations.
Acknowledgements
We would like to thank Professor Mikulic and Crespi for authorizing us to use the CRI-A instrument and to Tartaglini Florencia, PhD, for her theoretical contributions.
Footnotes
Conflicts of Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was carried out with the support of the Health Research Scholarship “Dr Abraam Sonis”, granted by the Ministry of Health and Social Development, Resolution 2018-49 APN-SGS # MSYDS.
ORCID iDs: Maria Barbara Eizaguirre https://orcid.org/0000-0002-7817-2772
Ricardo Alonso https://orcid.org/0000-0001-9955-8343
Berenice Silva https://orcid.org/0000-0001-5866-2419
Contributor Information
Sandra Vanotti, Multiple Sclerosis Unit, José María Ramos Mejía General Hospital, Buenos Aires, Argentina; Research Institute of Psychology, School of Psychology, Buenos Aires University, Buenos Aires, Argentina.
Nadia Cabral, Multiple Sclerosis Unit, José María Ramos Mejía General Hospital, Buenos Aires, Argentina.
Maria Barbara Eizaguirre, Multiple Sclerosis Unit, José María Ramos Mejía General Hospital, Buenos Aires, Argentina; Research Institute of Psychology, School of Psychology, Buenos Aires University, Buenos Aires, Argentina.
Aldana Marinangeli, Multiple Sclerosis Unit, José María Ramos Mejía General Hospital, Buenos Aires, Argentina.
Maria Sol Roman, Multiple Sclerosis Unit, José María Ramos Mejía General Hospital, Buenos Aires, Argentina; Research Institute of Psychology, School of Psychology, Buenos Aires University, Buenos Aires, Argentina.
References
- 1.Brownlee WJ, Hardy TA, Fazekas F, et al. Diagnosis of multiple sclerosis: progress and challenges. Lancet 2017; 389: 1336–1346. [DOI] [PubMed] [Google Scholar]
- 2.Benito-Leon J, Mitchell AJ, Rivera-Navarro J, et al. Impaired health-related quality of life predicts progression of disability in multiple sclerosis. Eur J Neurol 2013; 20: 79–86. [DOI] [PubMed] [Google Scholar]
- 3.Black N. Patient reported outcome measures could help transform healthcare. Bmj 2013; 346: f167–5. [DOI] [PubMed] [Google Scholar]
- 4.Khurana V, Sharma H, Afroz N, et al. Patient‐reported outcomes in multiple sclerosis: a systematic comparison of available measures. Eur J Neurol 2017; 24: 1099–1107. [DOI] [PubMed] [Google Scholar]
- 5.Keramat KM, Whitehead L, Smith C. Characteristics and correlates of coping with multiple sclerosis: a systematic review. Disabil Rehabil 2017; 41: 250–264. [DOI] [PubMed] [Google Scholar]
- 6.Bulacio JM. Ansiedad, estrés y práctica clínica [anxiety, stress and clinical practice]. 2nd ed Buenos Aires: Akadia, 2011. [Google Scholar]
- 7.Lazarus RS, Folkman S. Estrés y procesos cognitivos [stress, appraisal and coping]. Barcelona: Martínez Roca, 1986. [Google Scholar]
- 8.Moos RH. Coping responses inventory: CRI-Adult form, professional manual. Odessa, TX: Psychological Assessment Resources, 1993. [Google Scholar]
- 9.Mikulic IM, Crespi MC. Adaptación y validación del inventario de respuestas de afrontamiento de Moos (CRI-A) para adultos. Anuario de investigaciones - Universidad de Buenos Aires (en línea) 2008; 15: 305–312. [Adaptation and Validation of Moos’ Coping Responses Inventory (CRI-A) for Adults. Research Yearbook – Buenos Aires University (online) 2008; 15:305-312] [Google Scholar]
- 10.Goretti B, Emilio P, Valentina Z, et al. Coping strategies, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol Sci 2009; 30: 15–20. [DOI] [PubMed] [Google Scholar]
- 11.Farran N, Ammar D, Darwish H. Quality of life and coping strategies in Lebanese multiple sclerosis patients: a pilot study. Mult Scler Relate Disord 2016; 6: 21–27. [DOI] [PubMed] [Google Scholar]
- 12.Moos RH. Development and applications of new measures of life stressors, social resources, and coping responses. Eur J Psychol Assess 1995; 11: 1–13. [Google Scholar]
- 13.Holahan CJ, Moos RH, Holahan CK, et al. Social context, coping strategies, and depressive symptoms: an expanded model with cardiac patients. J Pers Soc Psychol 1997; 72: 918–928. [DOI] [PubMed] [Google Scholar]
- 14.Grytten N, Aarseth JH, Espeset K, et al. Stoppers and nonstarters of disease-modifying treatment in multiple sclerosis. Acta Neurol Scand 2013; 127: 133–140. [DOI] [PubMed] [Google Scholar]
- 15.Corallo F, Bonanno L, Di Cara M, et al. Therapeutic adherence and coping strategies in patients with multiple sclerosis: an observational study. Medicine (Baltimore) 2019; 98: e16532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Montel SR, Bungener C. Coping and quality of life in one hundred and thirty five subjects with multiple sclerosis. Mult Scler 2007; 13: 393–401. [DOI] [PubMed] [Google Scholar]
- 17.Devy R, Lehert P, Varlan E, et al. Improving the quality of life of multiple sclerosis patients through coping strategies in routine medical practice. Neurol Sci 2015; 36: 85–90. [DOI] [PubMed] [Google Scholar]
- 18.Van der Hiele K, Van Gorp D, Benedict R, et al. Coping strategies in relation to negative work events and accommodations in employed multiple sclerosis patients. Mult Scler J Exp Transl Clin 2016; 2: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Minzi MCR, Sacchi C. Stressful situations and coping strategies in relation to age. Psychol Rep 2005; 97: 405–418. [DOI] [PubMed] [Google Scholar]
- 20.Torrecilla NM, Casari LM, Rivas J. Afrontamiento y calidad de vida en mujeres pacientes oncológicas [coping and quality of life in women with cancer]. Psiencia 2016; 8: 1–16. [Google Scholar]
- 21.Cassullo GL, García L. Estudio de las competencias socio emocionales y su relación con el afrontamiento en futuros profesores de nivel medio [study of socio-emotional competencies and their relationship to coping in future secondary school teachers]. Reifop 2015; 18: 213–228. [Google Scholar]
- 22.Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 2011; 69: 292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simeoni M, Auquier P, Fernández O, et al. ; MusiQol Study Group. Validation of the multiple sclerosis international quality of life questionnaire. Mult Scler 2008; 14: 219–230. [DOI] [PubMed] [Google Scholar]
- 24.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983; 33: 1444–1452. [DOI] [PubMed] [Google Scholar]
- 25.Aznar V, Cáceres F, Gold L. Multiple sclerosis council for clinical practice guidelines. Fatiga y esclerosis múltiple (boletín pautas de manejo clínico). [Fatigue and Multiple Sclerosis (Guidelines for Clinical Management Bulletin]. Buenos Aires: MSC-Multiple Sclerosis Council for Clinical Practice Guidelines, 2001. [Google Scholar]
- 26.Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989; 46: 1121–1123. [DOI] [PubMed] [Google Scholar]
- 27.Brenlla ME, Rodríguez CM. Adaptación argentina del inventario de depresión de beck (BDI-II) In: AT Beck, RA Steer, G Brown. (eds) BDI-II. Inventario de depresión de beck. 2nd ed Buenos Aires: Paidós, 2006. [Google Scholar]
- 28.Beck AT, Steer RA, Brown G. BDI-II. Inventario de depresión de beck. 2nd ed Buenos Aires: Paidós, 2006. [Google Scholar]
- 29.Grogan S, Conner M, Norman P, et al. Validation of a questionnaire measuring patient satisfaction with general practitioner services. Qual Health Res 2000; 9: 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.G, García JC, López NZ, Calvo J. Estadística básica Para estudiantes de ciencias [basic statistics for science students]. Madrid: Universidad Complutense de Madrid, 2009. [Google Scholar]
- 31.Cohen J. A power primer. Psychol Bull 1992; 112: 155–159. [DOI] [PubMed] [Google Scholar]
- 32.Streiner LD. Figuring out factors: the use and misuse of factor analysis. Can J Psychiatry 1994; 39: 135–140. [DOI] [PubMed] [Google Scholar]
- 33.Hair JF, Tatham RL, Black WC. Análisis multivariante. [Multivariate Data Analysis]. 5th ed Pretince-Hall, Ibérica: Madrid, 1999. [Google Scholar]
- 34.Kirchner T, Forns M, Muñoz D, et al. Psychometric properties and dimensional structure of the Spanish version of the coping responses inventory – adult form. Psicothema 2008; 20: 902–909. [PubMed] [Google Scholar]
- 35.Kirchner T, Lara S. Stress and depression symptoms in patients with multiple sclerosis: the mediating role of the loss of social functioning. Acta Neurol Scand 2011; 123: 407–413. [DOI] [PubMed] [Google Scholar]
- 36.Rabinowitz AR, Arnett PA. A longitudinal analysis of cognitive dysfunction, coping, and depression in multiple sclerosis. Neuropsychology 2009; 23: 581–591. [DOI] [PubMed] [Google Scholar]
- 37.Meyer GJ, Finn SE, Eyde LD, et al. Psychological testing and psychological assessment: a review of evidence and issues. Am Psychol 2001; 56: 128–165. [PubMed] [Google Scholar]
- 38.Wilski M, Gabryelski J, Brola W, et al. Health-related quality of life in multiple sclerosis: links to acceptance, coping strategies and disease severity. Disabil Health J 2019; 19: 1936–6574. [DOI] [PubMed] [Google Scholar]
- 39.Kristofferzon ML, Engström M, Nilsson A. Coping mediates the relationship between sense of coherence and mental quality of life in patients with chronic illness: a cross-sectional study. Qual Life Res 2018; 27: 1855–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moreau T, Schmidt N, Joyeux O, et al. Coping strategy and anxiety evolution in multiple sclerosis patients initiating interferon-beta treatment. Eur Neurol 2009; 62: 79–85. [DOI] [PubMed] [Google Scholar]
- 41.Ambrosio L, Senosiain García JM, Riverol Fernández M, et al. Living with chronic illness in adults: a concept analysis. J Clin Nurs 2015; 24: 2357–2367. [DOI] [PubMed] [Google Scholar]
- 42.Whittemore R, Dixon J. Chronic illness: the process of integration. J Clin Nurs 2008; 17: 177–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lode K, Bru E, Klevan G, et al. Coping with multiple sclerosis: a 5-year follow-up study. Acta Neurol Scand 2010; 122: 336–342. [DOI] [PubMed] [Google Scholar]