Abstract
Introduction:
Severe acute respiratory syndrome coronavirus 2 also called coronavirus disease 2019 was first reported in the African continent on 14 February 2020 in Egypt. As at 18 December 2020, the continent reported 2,449,754 confirmed cases, 57,817 deaths and 2,073,214 recoveries. Urban cities in Africa have particularly suffered the brunt of coronavirus disease 2019 coupled with criticisms that the response strategies have largely been a ‘one-size-fits-all’ approach. This article reviewed early evidence on urban health nexus with coronavirus disease 2019 preparedness and response in Africa.
Methods:
A rapid scoping review of empirical and grey literature was done using data sources such as ScienceDirect, GoogleScholar, PubMed, HINARI and official websites of World Health Organization and Africa Centres for Disease Control and Prevention. A total of 26 full articles (empirical studies, reviews and commentaries) were synthesised and analysed qualitatively based on predefined inclusion criteria on publication relevance and quality.
Results:
Over 70% of the 26 articles reported on coronavirus disease 2019 response strategies across Africa; 27% of the articles reported on preparedness towards coronavirus disease 2019, while 38% reported on urbanisation nexus with coronavirus disease 2019; 40% of the publications were full-text empirical studies, while the remaining 60% were either commentaries, reviews or editorials. It was found that urban cities remain epicentres of coronavirus disease 2019 in Africa. Even though some successes have been recorded in Africa regarding coronavirus disease 2019 fight, the continent’s response strategies were largely found to be a ‘one-size-fits-all’ approach. Consequently, adoption of ‘Western elitist’ mitigating measures for coronavirus disease 2019 containment resulted in excesses and spillover effects on individuals, families and economies in Africa.
Conclusion:
Africa needs to increase commitment to health systems strengthening through context-specific interventions and prioritisation of pandemic preparedness over response. Likewise, improved economic resilience and proper urban planning will help African countries to respond better to future public health emergencies, as coronavirus disease 2019 cases continue to surge on the continent.
Keywords: Coronavirus disease 2019, pandemic preparedness, response strategies, Africa, urban health
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) also called coronavirus disease 2019 (COVID-19) was first reported in China in the latter part of 2019 and has so far infected over 73 million people, killed over 1.6 million victims globally as at 17 December 20201 and rapidly overwhelmed health systems globally. COVID-19 was first reported in the African continent on 14 February 2020 in Egypt.1 As at 18 December 2020, Africa reported 2,449,754 confirmed cases, 57,817 deaths and 2,073,214 recoveries.2 Southern Africa region remains the worst affected with over 1 million cases followed by North Africa with over 848,500 recorded cases; Eastern Africa with 304,400 cases and West Africa with approximately 224,000 recorded cases. The least affected region being central Africa with approximately 69,900 recorded cases.2 Figures 1–3 show details of the COVID-19 pandemic situation in Africa, at the time of writing this article. Urban cities in this era of globalisation face a triple health burden of non-communicable and communicable diseases, including COVID-19.3,4 Evidence suggests that most emerging infectious diseases either originate in urban settings (e.g. the emergence of COVID-19 in Wuhan, China) or they rapidly propagate because of urbanisation.5,6
Figure 1.
African COVID-19 situation: cases.
Source: CDC Africa Official Website.2
Total confirmed cases = 2,449,754; total recoveries = 2,073,214; total deaths = 57,817. Reported figures are all rounded off.
Figure 2.
African COVID-19 situation: deaths.
Source: CDC Africa Official Website.2
Reported figures are all rounded off.
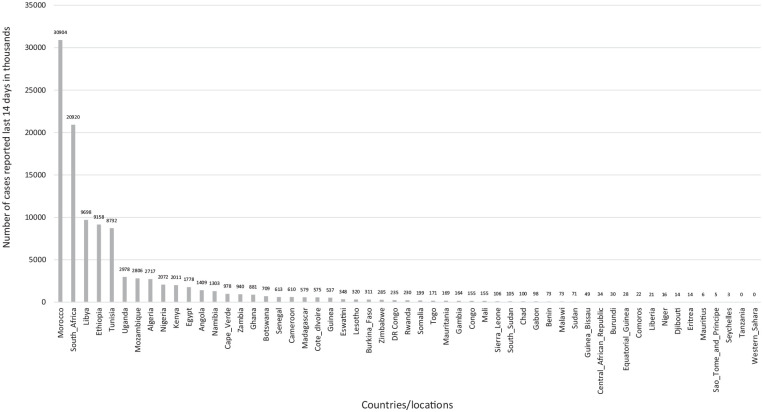
Figure 3.
African COVID-19 situation: Cases in the last 14 days.
Source: European CDC Official Website (accessed on 29 September 2020) from https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
Urban cities easily become epicentres of global pandemics due to several factors, key of them being overcrowding, poor housing and urban sanitation. In the early COVID-19 literature, poor housing has been a major cause of COVID-19 spread due to poor ventilation and communal living.7 Strict adherence to personal hygiene practices and social distancing among urban dwellers is also low because of insufficient social amenities.8,9 It is estimated that barely 56% of urban populations in Africa have access to pipe water,10,11making routine handwashing practically impossible especially among the urban poor.
Similarly, population density in urban cities impedes strict adherence to social distancing in the wake of COVID-19.7–9,12 The situation is aggravated by the inability of health authorities to effectively trace the routes and circulation of infected people in urban settlements because of poor street naming and address systems even in national capitals. Consequently, contact tracing under these circumstances has largely been unsuccessful, thus resulting in early and unabated community spread of COVID-19.12 Alegbeleye8 intimated that observing social distancing in many urban communities in Africa is virtually not feasible. This challenge according to Alegbeleye8 is due to high urban population densities coupled with contrary African societal and cultural norms, which are inherently communal and do not respect social distancing protocols.
Furthermore, in many African countries, urban poverty, illiteracy, ignorance, misconceptions and cultural belief systems have negatively affected the fight against global pandemics, including COVID-19. In most cases, these conditions promoted the easy spread of these pandemics. Spiritual dimensions to global pandemics have also reversed gains made by African countries on COVID-19 and during Ebola outbreak in Liberia,13,14 Sierra Leone15,16 and Guinea,17,18 where index cases and families preferred seeking care from faith healers and spiritualists instead of mainstream healthcare systems.
In addition, rural–urban labour mobility historically promotes the rapid spread of pandemics in urban settings.19 In the case of COVID-19, partial lockdown in the two biggest cities in Ghana witnessed huge labour migrants escaping these cities to rural areas on the eve of the lockdown. This migrant mobility raised concerns on the effectiveness of the lockdown measure since carriers of the virus probably escaped with it into other parts of the country.20,21 Similarly, unabated rural–urban migration for better health, social and economic opportunities in urban cities has resulted in overstretching existing health infrastructure in many African countries. It was predicted in the early days of COVID-19 that, in the United States, at least 200,000 intensive care unit (ICU) beds were needed in the case of a moderate outbreak of the pandemic.22 Uganda, on the contrary, had 55 ICU beds in 12 operational units23 with 80% of these ICU beds were located in the capital Kampala.24 Likewise, in Ghana, the number of isolation and quarantine centres remain inadequate, given the COVID-19 case counts25 and the fact that the country is only second to Nigeria in terms of case count in the West-African subregion.2 Similarly, in an international survey by Tabah et al.,26 on personal protective equipment (PPE) and ICU workers’ safety, it was found that out of the 2711 respondents, 52% of them indicated at least one piece of standard PPE was unavailable for use, while 30% reported reusing single-use PPE. In addition, Tabah et al.26 found that over 50% reported at least one PPE item missing or out of stock, while 80% reported adverse effects of PPE. These empirical studies, among others, elucidate the existing challenge of limited health infrastructure in fragile health systems in Africa as the continent continues the battle against COVID-19. See Table 1 on index COVID-19 cases in selected African countries.
Table 1.
Index cases of COVID-19 in selected African Countries.
| Country | Date | Case history |
|---|---|---|
| China (Global index) | 17 November 2020 | 55-year-old from Wuhan in the Hubei Province |
| Algeria | 25 February 2020 | Italian national who travelled to Algeria |
| Egypt | 14 February 2020 | Chinese national |
| Ethiopia | 13 March 2020 | Japanese national travelling from Japan to Burkina Faso |
| Ghana | 12 March 2020 | Two cases imported from Norway and Turkey |
| Ivory Coast | 11 March 2020 | Ivorian travelling from Italy |
| Kenya | 12 March 2020 | Kenyan travelling from the United States via the United Kingdom |
| Nigeria | 27 February 2020 | Italian citizen from Milan to Lagos |
Source: Aggregated by authors based on reviewed literature (August 2020).
COVID-19: coronavirus disease 2019.
This scoping review synthesised and analysed available evidence on urban health nexus with COVID-19 preparedness and response by African countries. This rapid review is expected to contribute to early scientific evidence on the COVID-19 pandemic and further inform public health policy dialogues on post-COVID-19 interventions to improve health systems resilience against future public health emergencies in Africa and across the globe.
Methods
Review rationale and justification
This is a rapid scoping review aimed at understanding the scope and existing body of evidence on urbanisation nexus with COVID-19 preparedness and response in Africa. This review will therefore adduce broad evidence on urbanisation nexus with COVID-19 preparedness and response in Africa. Consequently, this evidence will help inform the formulation and implementation of effective policies that are specific to the African region as a whole.
Review question development
In line with Joanna Briggs Institute (JBI) guideline for comprehensive systematic reviews (see Supplementary File 1), the review questions and components were based on population, concept and context (PCC) principles since it is a systematic scoping review of the available evidence. The population in the milieu of this review is the various countries in Africa and their health systems while the concept is the COVID-19 preparedness and response strategies; the context milieu is Africa. Population, Intervention, Comparator and Outcome (PICO) was not applied in this article since the review does not seek to answer questions on effectiveness. Moreover, the review is not an umbrella review, which makes PICO inappropriate under the circumstance.
Eligibility and exclusion criteria
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart (2009) was used to determine the eligibility criteria for literature inclusion and exclusion (see Figure 4). Reviewed literature comprised of peer-reviewed publications and grey literature on COVID-19 preparedness and response strategies in Africa and the relationship with urbanisation. Search for relevant literature was done in the English language using keywords/terms together with the Boolean search terms ‘and’, ‘or’ and ‘not’. The search terms and keywords were as follows: ‘Coronavirus’, ‘Coronavirus disease’, ‘COVID-19’, ‘preparedness’, ‘response’, ‘urban health’, ‘urbanisation’ and ‘Africa’. The inclusion criteria for the review were as follows: publications written in the English language, and articles focusing on COVID-19 in the context of urbanisation and articles published in the African context not earlier than December 2019 when the first confirmed case of COVID-19 was recorded in China. Conversely, exclusion criteria for the reviewed publications were as follows: publications not written in English language, not published on COVID-19 and not focused on Africa or urbanisation nexus with COVID-19.
Figure 4.
PRISMA 2009 flow diagram.
Source: Moher D, Liberati A, Tetzlaff J, et al. The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. DOI: 10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org.
Information sources and literature selection
An electronic search was conducted using relevant databases such as PubMed, ScienceDirect, GoogleScholar and HINARI. The Medical Subjects Heading (MeSH) search terms were ‘coronavirus’, ‘coronavirus disease’ and ‘COVID-19’, while the non-MeSH search terms were ‘preparedness’, ‘response’, ‘Africa’, ‘urbanisation’ and ‘urban health’. In addition, grey literature from official websites of international institutions such as the World Health Organization (WHO) and Africa Centres for Disease Control and Prevention (CDC) were used to access relevant publications. Time frame for the literature was since the outbreak of COVID-19 in December 2019 till 31 December 2020. Furthermore, snowballing technique was used as a manual search strategy. The snowballing involved manually tracing relevant literature from the list of references cited in a primary reviewed publication up to the point of saturation (i.e. no new information emerged from subsequent articles manually searched).
Screening and literature quality
JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses was used to promote quality in the review process. Publications that did not meet at least 70% of the criteria were dropped from the final synthesis and analysis. In the case of empirical peer-reviewed publications, the critical appraisal quality checks per the JBI Critical Appraisal Checklist for non-experimental studies included publications having explicitly stated research questions/objectives/aims, inclusion/exclusion criteria, literature search sources, study setting and study subjects. Other quality checks were methodology employed, outcome measures and confounders, and appropriateness of statistical analysis. The remaining quality checks were as follows: recognised limitations and mitigating measures, ethical considerations and interpretation of findings. In addition, published literature should have been peer-reviewed (or undergoing review in preprint). Commentaries, perspectives and reviews were included because of the paucity of publications on COVID-19 at the time of writing this scoping review.
Data extraction and analysis
Data extraction from the accessed literature was done using an extraction form developed by the authors based on JBI guidelines for scoping reviews. For objectivity and reduction of chance effect bias, literature search, screening and data extraction were concurrently done by two independent reviewers who later reconciled the extracted information for convergence. Synthesis and analysis were guided by the recurrent themes from the reviewed literature. Where applicable, data extraction categories included authors, year of publication, study location/context, outcome measures, study type and participants/subjects. Main thematic areas that emerged from the review on COVID-19 were preparedness, response strategies and the COVID-19 nexus with urban health. Key findings/conclusions and thrusts of each publication were also captured in the extraction form as shown in Table 3.
Table 3.
Data extraction and review summary..
| Authorship and publications information | Key perspectives on COVID-19 | Findings/conclusions on COVID-19 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Author | Year | Location/context | Study design/type | Participants/focused group | Outcome measures | Preparedness | Response | Urbanisation | Key findings |
| Afulani et al.27 | 2020 | Ghana | Empirical article (cross-sectional) | HCWs (n = 472) | Perceived preparedness to respond to COVID-19 | X | Increase HCWs’ preparedness to respond to COVID-19/pandemics | ||
| Ahmed et al.28 | 2020 | Global | Empirical article (cross-sectional) | Dentist (n = 669) | Anxiety and fear of getting infected while working on COVID-19 outbreak Knowledge about various practice modifications to combat COVID-19 |
X | Truncated dental care services | ||
| Akseer et al.29 | 2020 | LMICs | Review article | Women and children | Maternal and child nutrition during and in the aftermath of COVID-19 | X | X | COVID-19 direct effect on maternal/child health nutrition | |
| Alegbeleye9 | 2020 | SSA | Systematic review | HCWs | Factors impacting hand hygiene practice | X | Non-compliance with protocolsa | ||
| Ayebare et al.30 | 2020 | SSA | Review | Health system | Ebola preparedness for COVID-19 | X | Leveraging Ebola experiences to combat COVID-19 | ||
| Biccard et al.31 | 2020 | Africa | Prospective observational cohort study | Patients (n = 1243) Hospitals (n = 38) Countries (n = 6) |
Mortality in critically ill COVID-19 African patients | X | Mortality in critically ill COVID-19 African patients is higher than any other region and is associated with limited resources and severity of organ dysfunction at admission | ||
| Bonful et al.32 | 2020 | Ghana | Empirical article Exploratory, observational |
Public transport stations (n = 45) | Adherence to COVID-19 safety protocols | X | X | Low compliance with protocols | |
| Bong et al.10 | 2020 | LMICs | Review | Health system | Effect of COVID-19 on LMICs | X | X | Fragile health systems | |
| Cash and Patel33 | 2020 | LMICs | Perspective | Health system | Socio-economic impact of COVID-19 response strategies | X | X | Fragile economies | |
| Chersich et al.34 | 2020 | Africa | Review | HCWs | Staff motivation and retention through carefully managed risk ‘allowances’ or compensation | X | X | Fragile health economies/health systems | |
| Seifu Estifanos et al.35 | 2020 | Ethiopia | Commentary | Community | Social, cultural and economic conditions that place significant limitations to adhering to lockdown as a public health strategy for containing the spread of COVID-19 | X | Political and socio-economic crisis from lockdown | ||
| Gilbert et al.13 | 2020 | Africa | Empirical article (air travel data) | Countries (n = 10) | Preparedness and vulnerability of African countries against their risk of importation of COVID-19 | X | Low capacity, high vulnerability | ||
| Iwuoha and Aniche36 | 2020 | Nigeria | Empirical article (descriptive) | Urban slum dwellers | Experience of suburban slum residents on COVID-19 in selected states in Nigeria | X | X | Elitist/western contexts of COVID-19 lockdown and physical distancing | |
| Jewell et al.37 | 2020 | SSA | Empirical article (modelling)b | HIV/AIDS populations | Effects of COVID-19 disruptions on HIV-related deaths and new infections in SSA | X | Interruption in supply of ARTs/services due to COVID-19 | ||
| Joska et al.38 | 2020 | South Africa | Field notes | PLWHIV (women) | Effect of lockdown on ‘fattening the curve’ on mental health and well-being of the South African population | X | COVID-19 negative impact on mental health of populations | ||
| Kigatiira39 | 2020 | Kenya | Empirical article (case study) | Public motorcycle riders (n = 17) | Fear appeals and adoption of COVID-19 preventive measures | X | X | Fear-based messaging/communication | |
| Kim et al.40,c | 2020 | South Africa | Empirical article (modelling)b | Adults (n = 957) | Perceived COVID-19 risk and depression | X | X | Mental health impact of COVID-19 on urban adults | |
| Lee et al.6 | 2020 | Global | Commentary | Urban populations | Preparedness and challenges to pandemics in urban settings | X | X | Urbanisation and population effects on health systems | |
| Martinez-Alvarez et al.41 | 2020 | SSA | Commentary | Health system | Resource capacity of countries to fight COVID-19 pandemic | X | Response capacity of resource-poor countries | ||
| Nachega et al.42 | 2020 | DRC | Perspective | Health system | Response to COVID-19 and associated challenges, priorities and innovations for infectious disease control | X | Infectious and non-infectious diseases negative impact on countries’ economies | ||
| Nepomnyashchiy et al.43 | 2020 | Liberia | Commentary | CHWs | Support for CHWs to interrupt virus transmission while maintaining essential services and shielding vulnerable populations | X | Urgent need for investment in CHWs and PHC | ||
| Nyarko et al.44 | 2020 | Global | Review | Country economies | Effect of lockdown on the public health policies that can bring massive and tremendous change to health systems and general economy of African countries | X | X | Negative impact of lockdowns on economies of countries | |
| Paintsil45 | 2020 | Africa | Viewpoint | Heath system | Potential impact of the COVID-19 epidemic on already fragile health systems in SSA | X | X | Low capacity of Africa towards COVID-19 fight | |
| Rosenthal et al.46 | 2020 | Africa | Editorial | Health system | Challenges in implementing COVID-19 measures | X | Need for context-specific COVID-19 mitigating measures | ||
| Roberton et al.47 | 2020 | LMICs | Empirical article (modelling)b | Women and children | Additional maternal and under-5 child deaths resulting from the potential disruption of health systems and decreased access to food due to COVID-19 | X | Indirect effects of COVID-19 on maternal and child mortality | ||
| Tabah et al.26 | 2020 | LMICs | Empirical article (PPE availability for ICU staff caring for COVID-19 patients) | Healthcare staff (n = 2711) | Availability of PPE for ICU staff caring for COVID-19 patients | X | HCWs reported widespread shortages, frequent reuse of and adverse effects related to PPE | ||
| Total | 7/26 (27%) | 20/26 (77%) | 10/26 (38%) | ||||||
Source: Aggregated by authors based on reviewed literature (2020).
COVID-19: coronavirus disease 2019; HCWs: healthcare workers; LMICs: low- and middle-income countries; SSA: Sub-Saharan Africa; PLWHIV: people living with HIV; DRC: Democratic Republic of Congo; CHWs: community health workers; PPE: personal protective equipment; ICU: intensive care unit; ART: anti-retroviral therapy; PHC: primary health care.
COVID-19 safety and preventive protocols include wearing of nose masks, use of alcohol-based sanitiser, social distancing, hand hygiene/washing.
Mathematical modelling.
Pre-print article.
The “X” is used to denote applicable key perspectives in columns 7, 8 and 9.
Findings
Synthesis and analysis of results
Out of nearly 200,000 initial search output from the various databases, 26 full-text publications (see Table 3) were retained, synthesised and analysed. Retained articles were arrived at after removing repetitive and irrelevant publications based on the predefined inclusion and exclusion criteria explained earlier. These articles included empirical studies, systematic reviews and commentary publications. The 26 publications were synthesised and analysed based on relevance to the African context and quality; all publications were published in 2020. Eleven out of 26 publications were empirical studies, which were mostly cross-sectional descriptive studies, with one being a case study and three publications based on secondary data. The largest sample size for the publications based on primary data was 2711 and lowest was 10.
In terms of context distributions of reviewed articles, most of the publications focused on Africa as a continent (n = 5) followed by Sub-Saharan Africa (SSA; n = 4). Eight publications focused on global context with interest on Africa and other low- and middle-income countries (LMICs). A few others specifically focused on Ghana (n = 2), South Africa (n = 2), Ethiopia (n = 1), Nigeria (n = 1), Kenya (n = 1), Democratic Republic of Congo (DRC; n = 1) and Liberia (n = 1).
Concerning the type of study participants investigated, majority of the publications focused broadly on health systems (n = 7) and community participants such as slum/urban dwellers, women, children and people living with HIV (PLWHIV; n = 7). Other articles focused on healthcare workers (HCWs) such as community health workers (n = 5), while dentists (n = 1) and critically ill COVID-19 patients had one article each. Two publications concentrated on public transport vehicles and motorcycle riders, while two others broadly investigated COVID-19 impact on economies of countries in Africa as shown in Table 2.
Table 2.
Challenges and opportunities for global pandemics response in urban settings in Africa.
| Dimensions | Challenges | Opportunities |
|---|---|---|
| Urban population density | • Ease of disease spread between humans due to congestions • Difficulties in contact tracing • Urban inequalities resulting in poor housing/environments |
• Urban planning/design should factor in health emergency preparedness • Leveraging technological advances for more effective contact tracing and health supplies distribution (i.e. medical drones) |
| Urban transportation/mobility | • Congestions in public transport systems • Inefficiency in public transport system |
• Cities with efficient transport networks can be used to rapidly move supplies to outbreak in epicentres |
| Interface between animals and humans | • Poor sanitation in urban slums with high exposure of humans to rodents, unvaccinated animals and other animal vectors • Expansion into previously untouched ecosystems and encounters with wildlife via food markets |
• Improved sanitation and rodent control including vaccination of domestic animals for common zoonotic infections • Enhanced regulation of fresh markets and slaughterhouses |
| Governance by local authorities | • Insufficient epidemic preparedness capacities at local government levels • Reliance on national level for response measures |
• Increased investment in local governance for self-reliance in health emergency response • Effective decentralisation of local governance and health systems |
| High mobility of urban populations | • Unrelenting rural–urban migration • Increased risk of rapid export of disease to other parts of the country and neighbouring countries |
• Evidence-based points of entry measures and exit screening measures (e.g. mass testing, mandatory quarantines) • Inter-sectoral collaborations |
| Health communication/education | • Multiple information sources leading to misinformation and false information might spread quickly • Fear and stigma can discourage voluntary positive health-seeking behaviour |
• Unconventional but reliable information channels and social media can be used for risk communication • Trust can be built through anti-stigma messages |
Source: Modified based on Jamison DT, Gelband H, Horton S, et al. (eds). Disease control priorities: improving health and reducing poverty. Disease control priorities (3rd ed.), Vol. 9. Washington, DC: World Bank, 2018. DOI: 10.1596/978-1-4648-0527-1.
Synthesis by themes revealed that majority of the publications (77%) predominantly examined COVID-19 response strategies in Africa with a few others looking at the combine spectra of preparedness, response and urbanisation. Ten out of 26 synthesised publications primarily focused on COVID-19 nexus with urbanisation, while 27% primarily focused on health system preparedness for COVID-19 in Africa.
Furthermore, the review revealed that most recurrent themes were on impact of COVID-19 on health service provision (mental health, maternal and child health services, mortality outcomes among the critically ill), health logistics and supplies, including HIV/AIDS medications. Another most recurrent theme was health systems resilience in Africa towards COVID-19 and future pandemics. Other recurrent theme was spillover effects of COVID-19 response strategies on economies and livelihoods. Literature on Africa’s approach to COVID-19 was also apt in many of the publications.
Additional recurrent themes were health sector human resources to fight the pandemic and lack of compliance with COVID-19 prevention and safety protocols. One publication emphasised leveraging Africa’s past experiences with Ebola and HIV/AIDS in the prevention and control of COVID-19. Finally, another publication examined the nexus between urbanisation and COVID-19 in Africa’s urban slums and informal settlements, while one other prospective cohort study examined the association between limited critical care resources and COVID-19-related mortalities (see Table 3 and Figure 5).
Figure 5.
Recurrence of main themes from reviewed literature.
Source: Aggregated by authors based on reviewed literature (2020).
Discussion
Summary of evidence
Globally, it has been established that sufficient preparedness for pandemics by countries is a crucial investment since the cost is comparatively smaller than an unmitigated impact of health emergencies like COVID-19. For instance, the global financing gap for health emergency preparedness, estimated at US$4.5 billion per year, is minuscule compared with the estimated pandemic costs of US$570 billion per year.27 Health emergency preparedness activities in Africa with more fragile health systems are particularly crucial48,49 because of increasing urban populations and the attendant negative public health implications.50 Thus, opportunities in urban environments thus need to be leveraged to enhance the preparedness of urban settings for health emergencies like COVID-19. Table 2 presents the challenges and opportunities for urban settings in raising preparedness for public health emergencies in Africa.
In many parts of Europe and the Americas, strict COVID-19 prevention and control measures have been enforced, including total lockdowns. Unfortunately, many African countries spontaneously adopted same lockdown measures without requisite knowledge of the COVID-19 infection rate and the context-specific relevance of these measures.30,33,34,41,43,45,46 Ghana, for instance, observed three weeks partial lockdown in the two most urbanised regions as part of the early control measures without sufficient evidence. Unlike other continents, Africa was fortunate to record COVID-19 cases months after other continents recorded cases. The continent thus had the benefit of time and hindsight to prepare and respond differently to the pandemic based on lessons learnt. However, reviewed literature predominantly suggests that Africa’s response strategies were largely not context-specific but can best be described as a carbon copy of interventions adopted in China, other Asian countries, Europe and the Americas, albeit the circumstances and epidemiology of the virus are different.5–8 Consequently, a ‘one-size-fits-all’ approach was spontaneously adopted by many countries in Africa. Indeed, some of the COVID-19 response measures were needless and turned out to be ineffective.51
Restrictions in social gatherings have also been imposed to control the spread of the virus particularly church activities, funerals, weddings and closure of schools.52 Compulsory wearing of face masks and use of hand sanitisers are other pervasive COVID-19 preventive measures in Africa even though strict compliance remains problematic due to ignorance, poverty, resource constraints and unfavourable belief systems.28,36,53–55 Although some successes have been achieved in respect of these response strategies, critics have described them as ‘one-size-fit-all’ and ‘Western elitist’ approach because of their relevance to Africa’s local settings vis-à-vis trends in other parts of the world.
For example, in many African countries, hand sanitisers have been misconceived as a replacement for regular hand hygiene mainly due to ignorance and lack of education. Likewise, enforcement of social distancing in crowded urban communities is proving to be impracticable just like self-isolation in congested households. These measures have largely been ineffective partly due to poor living standard particularly in urban slums. Also, the ‘work from home’ mantra immediately embraced by already fragile economies in Africa is equally, arguably, an ineffective response strategy relative to more resilient economies outside Africa. For instance, over 70% of Africa’s workforce is in the informal sector and predominantly engaged in manual labour. In view of the huge informal sector in Africa, the ‘work from home’ policy at the initial phase of the pandemic rather worsened the plight of many citizens already in the lower wealth quintiles.44,56–58
Other COVID-19 mitigating measures questioned and heavily criticised in Africa are mass closure of schools without established e-learning systems and infrastructure, enforcement of handwashing protocols when over 50% of households in Africa do not have access to portable water,51 temperature checks of travellers at borders and airports without accounting for asymptomatic carriers of the virus and mass testing capacities coupled with ability to pay for COVID-19 testing upon arrival at airports.
Moreover, many countries in Africa are still battling fear-based messaging and misinformation on COVID-1959 similar to Ebola and HIV/AIDS.13 Available literature maintains that misinformation and fear-based communication cause anxiety and possibly deaths39 of which COVID-19 is not an exception. Over the years, in pandemics response, fear has rarely been a good motivator for people’s adherence to safety precautions. Indeed, people generally respond better to calm and fact-based messages/information.39 Unfortunately, many countries in Africa have not performed optimally well in respect of COVID-19, Ebola and HIV/AIDS, and stigma management. In effect, misinformation and fear-based messaging associated with COVID-19 continue to break stigma, discouraging infected persons to declare their status and seek early treatment. Similarly, fear of disclosure potentially promotes community spread of the virus.
Notwithstanding these challenges, Africa is praised for some positives in the COVID-19 fight. For instance, countries with more recent experience with Ebola appear to be leveraging this expertise in response to COVID-19. Liberia, Sierra Leone, DRC and Guinea are currently re-purposing existing structures used during Ebola as COVID-19 isolation and treatment centres.30,34 In DRC, single-patient-transparent cubes originally designed for isolation of Ebola cases are re-purposed for COVID-19 isolation and treatment centres.41 Likewise, inter-sectoral collaboration with government institutions, non-governmental organisations (NGOs), religious bodies, industry players and national security agencies have been effectively leveraged in many countries in Africa towards COVID-19 fight.12,33,43,45,46,51,52 The role of the media and civil society in propagating health education and communication on COVID-19 prevention and control has equally been phenomenal in Africa.51 In addition, the ingenuity of many African countries in developing locally manufactured handwashing devices and PPE is especially commended in the bit to promote self-reliance and sustainability in the wake of COVID-19.53
Finally, lessons learnt from Ebola in West Africa show that balancing urgent clinical care with the general well-being of the community is the best prescription for containing pandemic outbreaks, particularly in urban settings which have so far suffered most from the pandemic. In light of this, some African countries have incorporated community engagement approach in the prevention and control of COVID-19.30,42,60,61 Some reports suggest that lockdown impositions in Africa were executed with human considerations and social support for the less privileged through community mobilisation. These community-centred response strategies have contributed to high compliance with the COVID-19 preventive measures in some countries62 and must be encouraged and sustained.
Irrespective of these important achievements chalked in Africa, the reviewed literature also reports instances of spillover effects from the COVID-19 mitigation measures especially in urban settings. First, urban dwellers working in the informal sector (and are predominantly labour migrants) are so far the worst affected by COVID-19 in Africa since approximately 85% of workers in Africa are not on regular wages and do not have the option to work from home.63 For instance, during the lockdowns, these underprivilege majority did not earn a wage throughout the period. The story of the Kenyan widow of many children boiling stones for her children during the lockdown elucidates this point.64
Furthermore, many countries in Africa recorded an interruption in food supply chain especially in urban cities, which often relied on rural communities for food supplies. Countries like Ghana witnessed an escalation in food prices by nearly 30% during the partial lockdowns65,66 due to panic buying and disruptions in food supply chain. Even though lockdowns might have helped curb the virus transmission, these measures also pushed millions of people into extreme poverty to the extent that hunger, rather than COVID-19, had a greater chance of killing already impoverished individuals during the lockdowns.63–67 The review also found that human rights abuse during lockdowns54,67 were excesses that emanated from the COVID-19 response measures in many parts of Africa.
Other spillover effect of the COVID-19 response measures in Africa was the effect on already fragile health systems. Neglect of the public health needs of populations in the wake of COVID-19 has already been reported with unprecedented reduction in health service utilisation, including HIV/AIDS services.68 Utilisation of mental health,37,38,40,69 maternal/child health and related outpatient department (OPD) services29,40,47,70–72 have equally been adversely affected in Africa. There are equally fears of imminent post-COVID 19 negative impact on African economies with a possible gross domestic product (GDP) growth rate dropping to record low of single digits.23,36,44,46
Finally, evidence adduced by Biccard et al.31 on a relatively higher case mortality in critically ill COVID-19 African patients than any other regions in the world suggests the urgent need to resource healthcare facilities in Africa to improve on the quality of healthcare for COVID-19 victims. Biccard et al.,31 for instance, found that there is an excess mortality of 18 and 29 deaths per 100 COVID-19 African patients compared to other parts of the world with an even worrying evidence of a positive correlation between COVID-19-related mortalities and limited critical care resources. Since the impact of COVID-19 has so far been most severe in urban settings which do not also have the requisite healthcare facilities to promote strict adherence to the COVID-19 safety protocols in many parts of Africa including Ghana,32 there is the need for greater commitment to health systems strengthening to avert possible humanitarian catastrophe as the pandemic continues to strike harder on Africa.
Limitations
This review included commentaries, editorials, perspectives and some grey literature because of the novel nature of COVID-19 and the fact that not many empirical publications are yet available, especially on Africa. Africa therefore needs a rigorous research agenda on COVID-19 to inform evidence-based policies during and after the pandemic to help address this existing limitation.
Conclusion
Evidence from the reviewed literature suggests that countries, particularly in Africa, need to improve health infrastructure, human resources and medical technology using local resources to enable the continent respond adequately to public health emergencies. COVID-19 has taught the world, including Africa, that pandemic preparedness should be prioritised over response. A relatively less expensive yet effective investment should be community-level preparedness and response strategies long before pandemics strike.
Improving health sector human resource capacity at the primary healthcare level such as community health workers has particularly proven to be an effective approach to early containment of global pandemics and must be prioritised as Africa’s trump-card in pandemics response. Trillions of dollars have already been committed in just a little over a year for the COVID-19 response globally. Meanwhile, a COVID-19 vaccine or treatment might take months if not years to become commercially available and accessible to resource-poor settings mostly in Africa.
Moreover, a readily available and accessible COVID-19 vaccine today does not guarantee acceptance and adoption in many African countries where there are shortages of health sector human resources to effectively deliver COVID-19 vaccines. A comparative US$2 billion annual investment in African health systems to bolster CHWs for primary care is minuscule compared to the current global cost of health systems response to the current pandemic. These practical nuances elucidate the need for prioritisation of efficient and effective community-level interventions particularly for the urban poor in resource-constrained countries in Africa which are often the worst affected victims of global pandemics.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_2050312121994360 for Urban health nexus with coronavirus disease 2019 (COVID-19) preparedness and response in Africa: Rapid scoping review of the early evidence by Robert Kaba Alhassan, Jerry John Nutor, Aaron Asibi Abuosi, Agani Afaya, Solomon Salia Mohammed, Maxwel Ayindenaba Dalaba, Mustapha Immurana, Alfred Kwesi Manyeh, Desmond Klu, Matilda Aberese-Ako, Phidelia Theresa Doegah, Evelyn Acquah, Edward Nketiah-Amponsah, John Tampouri, Samuel Kaba Akoriyea, Paul Amuna, Evelyn Kokor Ansah, Margaret Gyapong, Seth Owusu-Agyei and John Owusu Gyapong in SAGE Open Medicine
Acknowledgments
The authors appreciate and acknowledge important institutional repositories such as the Ghana Health Service (GHS) COVID-19 (coronavirus disease 2019) update platform and likewise the Africa Centres for Disease Control and Prevention (CDC) and the official website of the World Health Organization (WHO).
Footnotes
Author contributions: R.K.A. provided conceptualisation direction, literature search, synthesis and analysis, and manuscript write-up. J.J.N., A.A.A., A.A., S.S.M., M.A.D., M.I., A.K.M., D.K., M.A.-A., P.T.D., E.A., E.N.-A., J.T., S.K.A., P.A., E.K.A., M.G., S.O.-A. and J.G. read and peer-reviewed the manuscript based on their respective technical knowledge and expertise.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data availability: All required information is contained in the manuscript.
Ethical approval and informed consent: No human subjects were used for this review; hence, no ethical clearance required as per local ethics committees’ guidelines.
ORCID iDs: Robert Kaba Alhassan  https://orcid.org/0000-0003-4227-4854
https://orcid.org/0000-0003-4227-4854
Agani Afaya  https://orcid.org/0000-0002-7918-2999
https://orcid.org/0000-0002-7918-2999
Supplemental material: Supplemental material for this article is available online.
References
- 1. WHO and Regional Office for Africa. A second COVID-19 case is confirmed in Africa, https://www.afro.who.int/news/second-covid-19-caseconfirmed-africa (accessed 7 December 2020).
- 2. African Union (AU). Africa CDC, Official Website, https://africacdc.org/covid-19/ (accessed 17 December 2020).
- 3. World Health Organization. 2016. Global report on urban health: equitable healthier cities for sustainable development. WHO Library Cataloguing-in-, https://apps.who.int/iris/handle/10665/204715 (accessed 13 December 2020). [Google Scholar]
- 4. Ithnin M, Mohamad nor NA, Juliana N, et al. Knowledge, attitudes and practices on risk factors of non-communicable diseases (NCDs): a cross-sectional survey among urban and rural adults in Negeri Sembilan, Malaysia. Int J Health Prom Educ 2020; 1–1. DOI: 10.1080/14635240.2020.1749526. [DOI] [Google Scholar]
- 5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. New Engl J Med. 2020; 382: 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cho SY, Kang JM, Ha YE, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet 2016; 388(10048): 994–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nikolich-Zugich J, Knox KS, Rios CT, et al. SARS-CoV-2 and COVID-19 in older adults: what we may expect regarding pathogenesis, immune responses, and outcomes. Geroscience 2020; 42: 1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Metsky HC, Matranga CB, Wohl S, et al. Zika virus evolution and spread in the Americas. Nature 2017; 546(7658): 411–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alegbeleye BJ. Coronavirus disease-19 outbreak: barriers to hand hygiene practices among healthcare professionals in sub-Saharan Africa. Int J Sci Adv 2020; 1(1). DOI: 10.51542/ijscia.v1i1.5. [DOI] [Google Scholar]
- 10. Bong CL, Brasher C, Chikumba E, et al. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg 2020; 131(1): 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Armah FA, Ekumah B, Yawson DO, et al. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon 2018; 4(11): e00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eberhard R. Part I (synthesis report): access to water and sanitation in sub-Saharan Africa, review of sector reforms and investments, key findings to inform future support to sector development. Deutsche Gesellschaft fur Internationale Zusammenarbeit GIZ GmbH, https://www.oecd.org/water/GIZ_2018_Access_Study_Part%20I_Synthesis_Report.pdf (2019, accessed 24 August 2020). [Google Scholar]
- 13. Gilbert M, Pullano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. Lancet 2020; 395(10227): 871–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Oyeyemi SO, Gabarron E, Wynn R. Ebola, twitter, and misinformation: a dangerous combination? Bmj 2014; 349: g6178. [DOI] [PubMed] [Google Scholar]
- 15. Manguvo A, Mafuvadze B. The impact of traditional and religious practices on the spread of Ebola in West Africa: time for a strategic shift. Pan Afr Med J 2015; 22(Suppl 1): 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bangura JB. Hope in the midst of death: charismatic spirituality, healing evangelists and the Ebola crisis in Sierra Leone. Missionalia 2016; 44(1): 2–18. [Google Scholar]
- 17. James PB, Wardle J, Steel A, et al. Ebola survivors’ healthcare-seeking experiences and preferences of conventional, complementary and traditional medicine use: a qualitative exploratory study in Sierra Leone. Complement Ther Clin Pract 2020; 39: 101127. [DOI] [PubMed] [Google Scholar]
- 18. Balde A. How elements of culture have contributed to the construction of health meanings in regards to the 2014 Ebola outbreak (Doctoral dissertation). Masters Thesis, Indiana University, Bloomington, IN, 2016. [Google Scholar]
- 19. Park C. Traditional funeral and burial rituals and Ebola outbreaks in West Africa: a narrative review of causes and strategy interventions. J Health Soc Sci 2020; 5(1): 073–090. [Google Scholar]
- 20. Neiderud CJ. How urbanization affects the epidemiology of emerging infectious diseases. Infect Ecol Epidemiol 2015; 5: 27060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. VOA. Ghana’s decision to lift partial COVID-19 lockdown criticized by some, https://www.voanews.com/africa/ghanas-decision-lift-partial-covid-19-lockdown-criticized-some (accessed 20 April 2020).
- 22. The Guardian. Easing of lockdown a relief to Ghana’s poor – despite fears it is premature, https://www.theguardian.com/global-development/2020/may/03/coronavirus-easing-of-lockdown-a-relief-to-ghanas-poor-despite-fears-it-is-premature (accessed 21 May 2020).
- 23. New York Times. Here’s the Biggest Thing to Worry about with Coronavirus, https://www.nytimes.com/2020/03/12/upshot/coronavirus-biggest-worry-hospital-capacity.html (accessed 12 March 2020).
- 24. Monitor. ICU bed capacity in Uganda, https://www.monitor.co.ug/News/National/ICU-bed-capacity-Uganda/688334-5495822-dkw5rc/index.html (accessed 18 March 2020).
- 25. Atumanya P, Sendagire C, Wabule A, et al. Assessment of the current capacity of intensive care units in Uganda; A descriptive study. J Crit Care 2020; 55: 95–99. [DOI] [PubMed] [Google Scholar]
- 26. Tabah A, Ramanan M, Laupland KB, et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): an international survey. J Crit Care 2020; 59: 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Afulani PA, Gyamerah AO, Aborigo RA, et al. Perceived preparedness to respond to the COVID-19 pandemic: a study with healthcare workers in Ghana. J Global Health Sci 2020; 2(2): e24. [Google Scholar]
- 28. Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat Novel Coronavirus disease (COVID-19) outbreak. Int J Envir Res Public Health 2020; 17(8): 2821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Akseer N, Kandru G, Keats EC, et al. COVID-19 pandemic and mitigation strategies: implications for maternal and child health and nutrition. Ame J Clin Nutr 2020; 112(2): 251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ayebare R, Waitt P, Okello S, et al. Leveraging investments in Ebola preparedness for COVID-19 in sub-Saharan Africa. AAS Open Res 2020; 3: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Biccard B, Miller MG, Michell WL, et al. An African, multi-centre evaluation of patient care and clinical outcomes for patients with COVID-19 infection admitted to high-care or intensive care units. Lancet; Epub ahead of print 22 October 2020. https://www.researchgate.net/publication/345336480_An_African_Multi-Centre_Evaluation_of_Patient_Care_and_Clinical_Outcomes_for_Patients_with_COVID-19_Infection_Admitted_to_High [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bonful H, Addo-Lartey A, Aheto J, et al. Limiting spread of COVID-19 in Ghana: compliance audit of selected transportation stations in the Greater Accra region of Ghana. PLoS One 2020; 15(9): e0238971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cash R, Patel V. Has COVID-19 subverted global health? Lancet 2020; 395(10238): 1687–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chersich MF, Gray G, Fairlie L, et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Glob Health 2020; 16: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Seifu Estifanos A, Alemu G, Negussie S, et al. ‘I exist because of we’: shielding as a communal ethic of maintaining social bonds during the COVID-19 response in Ethiopia. BMJ Glob Health 2020; 5(7): e003204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iwuoha VC, Aniche ET. COVID-19 lockdown and physical distancing policies are elitist: towards an indigenous (Afro-centred) approach to containing the pandemic in sub-urban slums in Nigeria. Local Envir 2020; 25(8): 631–640. [Google Scholar]
- 37. Jewell BL, Mudimu E, Stover J, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. Lancet HIV 2020; 7(9): e629–e640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Joska JA, Andersen L, Rabie S, et al. COVID-19: increased risk to the mental health and safety of women living with HIV in South Africa. AIDS Behav 2020; 24(10): 2751–2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kigatiira KK. Efficacy of fear appeals on adoption of COVID-19 preventive measures: a case of boda boda riders in Nairobi county, Kenya. Int J Res Granth 2020; 8(6): 219–228. [Google Scholar]
- 40. Kim AW, Nyengerai T, Mendenhall E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. medRxiv. Epub ahead of print 1 January 2020. DOI: 10.1101/2020.06.13.20130120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Martinez-Alvarez M, Jarde A, Usuf E, et al. COVID-19 pandemic in west Africa. Lancet Glob Health 2020; 8(5): e631–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nachega JB, Mbala-Kingebeni P, Otshudiema J, et al. Responding to the challenge of the dual COVID-19 and Ebola epidemics in the Democratic Republic of Congo – priorities for achieving control. Am J Trop Med Hyg 2020; 103(2): 597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nepomnyashchiy L, Dahn B, Saykpah R, et al. COVID-19: Africa needs unprecedented attention to strengthen community health systems. Lancet 2020; 396(10245): 150–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nyarko RO, Boateng E, Kahwa I, et al. The impact on public health and economy using lockdown as a tool against COVID-19 pandemic in Africa: a perspective. J Epidemiol Public Health Rev 2020; 5(3). DOI: 10.16966/2471-8211.188. [DOI] [Google Scholar]
- 45. Paintsil E. COVID-19 threatens health systems in sub-Saharan Africa: the eye of the crocodile. J Clin Invest 2020; 130(6): 2741–2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Rosenthal PJ, Breman JG, Djimde AA, et al. COVID-19: shining the light on Africa. Am J Trop Med Hyg 2020; 102(6): 1145–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020; 8(7): e901–e908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. World Health Organization. Support to countries for strengthening public health capacities required under the International Health Regulations (2005): WHO Lyon Office, department of global capacities, alert and response: activity report January 2015-September 2016. World Health Organization 2016. https://apps.who.int/iris/handle/10665/333792
- 49. So AD, Ruiz-Esparza Q. Technology innovation for infectious diseases in the developing world. Infect Dis Poverty 2012; 1(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lee VJ, Ho M, Kai CW, et al. Epidemic preparedness in urban settings: new challenges and opportunities. Lancet Infect Dis 2020; 20(5): 527–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wilkinson A. Local response in health emergencies: key considerations for addressing the COVID-19 pandemic in informal urban settlements. Envir Urban 2020;32: 503–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Arakpogun E, El Sahn Z, Prime KS, et al. Africa’s resilience in the face of COVID-19 pandemic: let’s talk about it!. SSRN 3640311, https://www.researchgate.net/publication/342688644_Africa’s_Resilience_in_the_Face_of_COVID-19_Pandemic_Let’s_Talk_about_It (accessed 1 July 2020).
- 53. Wango GM, Wairire G, Kimamo C. Patterns of development of COVID-19 in low- and middle-income countries: suggested psychological intervention strategies 2020; 51: 102128. [Google Scholar]
- 54. Roser M, Ritchie H, Ortiz-Ospina E, et al. Coronavirus pandemic (COVID-19). Our World in Data. Epub ahead of print 4 March 2020. https://ourworldindata.org/coronavirus
- 55. Dzisi EK, Dei OA. Adherence to social distancing and wearing of masks within public transportation during the COVID 19 pandemic. Trans Res Interdisc Persp 2020; 7: 100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Irlacher M, Koch M. Working from home, wages, and regional inequality in the light of COVID-19. CESifo Working Paper, CESifo, 22 April 2020. https://ssrn.com/abstract=3582329 [Google Scholar]
- 57. Bick A, Blandin A, Mertens K. Work from home after the COVID-19 Outbreak. Research Department working Paper, July 2020. 10.24149/wp2017r1 [DOI]
- 58. Otu A, Ebenso B, Labonte R, et al. Tackling COVID-19: can the African continent play the long game? J Glob Health 2020; 10(1): 010339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ataguba JE. COVID-19 pandemic, a war to be won: understanding its economic implications for Africa. Appl Health Econ Health Policy 2020; 18(3): 325–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bedrosian SR. Lessons of risk communication and health promotion – West Africa and United States. MMWR Suppl 2016; 65: 68–74. [DOI] [PubMed] [Google Scholar]
- 61. Gilmore B, Ndejjo R, Tchetchia A, et al. Community engagement for COVID-19 prevention and control: a rapid evidence synthesis. BMJ Glob Health 2020; 5(10): e003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mobula LM, Samaha H, Yao M, et al. Recommendations for the COVID-19 response at the national level based on lessons learned from the Ebola virus disease outbreak in the Democratic Republic of the Congo. Am J Trop Med Hyg 2020; 103(1): 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Abideen AZ, Mohamad FB, Hassan MR. Mitigation strategies to fight the COVID-19 pandemic – present, future and beyond. J Health Res 2020;34: 547–562. [Google Scholar]
- 64. The Economist. Continental contagion, Africa is woefully ill-equipped to cope with COVID-19, https://www.economist.com/middle-east-and-africa/2020/03/26/africa-is-woefully-ill-equipped-to-cope-with-covid-19 (accessed 29 March 2020).
- 65. BBC. 2020. Coronavirus: Kenyans moved by widow cooking stones for children, https://www.bbc.com/news/world-africa-52494404#:~:text=Kenyans%20have%20rallied%20to%20the,they%20waited%20for%20their%20meal (accessed 30 April 2020).
- 66. Alliance for Science. 2020. COVID-19 virus spread prompts food insecurity fears in Africa, https://allianceforscience.cornell.edu/blog/2020/03/covid-19-virus-spread-prompts-food-insecurity-fears-in-africa (accessed 20 March 2020).
- 67. IFPRI. 2020. How much will global poverty increase because of COVID-19?, https://www.ifpri.org/blog/how-much-will-global-poverty-increase-because-covid-19 (accessed 19 March 2020).
- 68. Amadasun S. COVID-19 palaver: ending rights violations of vulnerable groups in Africa. World Dev 2020; 134: 105054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. World Health Organization. 2020. Coronavirus disease (COVID-19): situation report, 182, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed 10 March 2020). [Google Scholar]
- 70. Cornish L. Interactive: who’s funding the COVID-19 response and what are the priorities, https://www.devex.com/news/interactive-who-s-funding-the-covid-19-response-and-what-are-the-priorities-96833 (accessed 14 December 2020).
- 71. Atherly D. Opinion: to deliver a COVID-19 vaccine equitably, we must start planning now. Devex, https://www.devex.com/news/opinionto-deliver-a-covid-19-vaccine-equitably-we-must-start-planningnow-97168 (accessed 7 May 2020). [Google Scholar]
- 72. USAID Center for Innovation Impact Financing Alliance for Health Dalberg Advisors. 2017. Strengthening primary health care through community health workers: closing the $2 billion gap, https://www.usaid.gov/cii/strengthening-primary-health-care-through-communityhealth-workers-closing-2-billion-gap (accessed 25 June 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_2050312121994360 for Urban health nexus with coronavirus disease 2019 (COVID-19) preparedness and response in Africa: Rapid scoping review of the early evidence by Robert Kaba Alhassan, Jerry John Nutor, Aaron Asibi Abuosi, Agani Afaya, Solomon Salia Mohammed, Maxwel Ayindenaba Dalaba, Mustapha Immurana, Alfred Kwesi Manyeh, Desmond Klu, Matilda Aberese-Ako, Phidelia Theresa Doegah, Evelyn Acquah, Edward Nketiah-Amponsah, John Tampouri, Samuel Kaba Akoriyea, Paul Amuna, Evelyn Kokor Ansah, Margaret Gyapong, Seth Owusu-Agyei and John Owusu Gyapong in SAGE Open Medicine