Abstract
Objectives
Individuals often manage chronic conditions in middle and later life that may diminish well-being. Little is known, however, about discordant conditions (i.e., two or more conditions with competing self-management requirements) among older couples and their links to depressive symptoms. We considered discordant conditions at both the individual level and the couple level (i.e., between spouses), along with their long-term implications for depressive symptoms.
Methods
The U.S. sample included 1,116 middle-aged and older couples drawn from five waves (2006–2014) of the Health and Retirement Study. Longitudinal actor-partner interdependence models evaluated whether individual-level and couple-level discordant chronic health conditions were concurrently linked to depressive symptoms, and whether these associations became stronger over time. Models controlled for age, minority status, education, prior wave depressive symptoms, and each partner’s baseline report of negative marital quality and number of chronic conditions in each wave.
Results
Wives and husbands reported significantly greater depressive symptoms when they had individual-level discordant conditions about 2 years after baseline, and these links intensified over time. Beyond this association, husbands had significantly greater depressive symptoms when there were couple-level discordant conditions.
Discussion
Individual-level and couple-level discordant conditions may have lasting implications for depressive symptoms during midlife and older adulthood.
Keywords: Depression, Morbidity, Multimorbidities, Spouses
Multimorbidity, defined as having two or more chronic diseases, affects about half of adults aged 45–64 and over 80% of adults aged 65 and older (Buttorff, Ruder, & Bauman, 2017). On average, people with multimorbidity report significantly greater depressive symptoms and have a two- to threefold increased risk of a depressive disorder relative to those with one or no chronic conditions (Read, Sharpe, Modini, & Dear, 2017). Middle-aged and older adults with chronic illness commonly have spouses managing at least one health condition of their own (Piette, Rosland, Silveira, Kabeto, & Langa, 2010). Spouses influence one another’s long-term mental and physical health (Polenick, Brooks, & Birditt, 2017; Polenick, Renn, & Birditt, 2018; Thomeer, 2016), yet little is known about how each partner’s chronic conditions are linked to well-being within the couple. Multiple chronic conditions are more challenging when they require discordant self-management goals (e.g., lowering blood pressure vs reducing pain) that are not directly related and increase care complexity (Bowling et al., 2017; Boyd & Fortin, 2010; Goodman et al., 2016; Lagu et al., 2008; Piette & Kerr, 2006). Consequently, discordant conditions at both individual and couple levels may have enduring associations with depressive symptoms. This study considered individual-level and couple-level discordant conditions, their links to depressive symptoms across 8 years, and whether these links become stronger over time.
Discordant Chronic Conditions and Depressive Symptoms
According to the concordant–discordant model of comorbidities, multiple chronic conditions are more difficult to manage when they involve discordant treatment requirements (Piette & Kerr, 2006). Concordant conditions such as diabetes and heart disease share similar self-management strategies (e.g., a low-salt diet to lower cardiovascular risk) that are synergistic and simplify treatment plans. By contrast, discordant conditions such as diabetes and arthritis require a wider range of self-management strategies (e.g., a low-salt diet vs physical therapy exercises) that compete with limited time and resources. Discordant conditions increase self-management burden because they cannot be managed synergistically. Having one or more discordant conditions also complicates decisions about prioritizing self-management tasks, which may heighten distress and contribute to detrimental health outcomes (Boyd & Fortin, 2010; Piette & Kerr, 2006). Indeed, a study of multimorbidity patterns among older adults found that two discordant condition combinations (arthritis–pulmonary and arthritis–pulmonary–heart) show the strongest association with depression (Pruchno, Wilson-Genderson, & Heid, 2016).
Taken together, the current literature suggests that middle-aged and older adults with discordant conditions may report higher depressive symptoms than those without discordant conditions. Furthermore, this association may intensify as the negative consequences of discordant conditions accumulate. People managing discordant conditions, for instance, might find it increasingly difficult to prioritize a low-sugar diet for diabetes when they also cope with arthritis pain that becomes more severe with age. Poorer self-management combined with increasing illness severity may amplify depressive symptoms over time.
Discordant Chronic Conditions in the Couple Context
Interdependence theory proposes that spouses influence one another’s thoughts, feelings, and behaviors in ways that mutually affect their well-being (Rusbult & Van Lange, 2008). Previous studies have demonstrated that medical morbidity and depressive symptoms among middle-aged and older wives and husbands are interrelated and show cross-partner associations over time (Polenick et al., 2017, 2018; Thomeer, 2016). Such interdependence suggests that one partner’s discordant conditions may lead to emotional strain for both members of the couple. Supporting this hypothesis, greater illness intrusiveness (i.e., interference with daily life) has been positively linked to both individual-level depressive symptoms (Devins et al., 1993) and spousal strain (Masters et al., 2013). One spouse’s discordant self-management requirements potentially hinder and complicate the daily lives of both partners, which might raise their susceptibility to depressive symptoms.
Over and above individual-level discordant conditions, discordant conditions between spouses may contribute to psychological distress. Couple-level discordant conditions occur when partners have chronic conditions with self-management requirements that differ from one another. A husband with arthritis, for example, likely manages pain with physical therapy exercises or medications, but might not need to follow the low-salt diet recommended for his wife with heart disease. Compatibility theories of marriage suggest that spouses who differ in their everyday goals and behaviors may encounter more marital conflict and perceive less partner support (Levinger & Rands, 1985). In accord with these theories, studies have found positive links between marital satisfaction and shared leisure time and activities (Crawford, Houts, Huston, & George, 2004; Hill, 1988) and negative associations between marital satisfaction and discordant alcohol consumption among couples (Homish & Leonard, 2008; Rodriguez, Neighbors, & Knee, 2014). Chronic conditions with differing self-management requirements between spouses add complexity to daily routines and may strain their relationship, potentially elevating both partners’ depressive symptoms.
Wives may be particularly at risk of depressive symptoms in the context of individual-level and couple-level discordant conditions. Compared with husbands, wives are less likely to care for themselves when ill, receive less partner and family support in managing their own health, and report more family-related barriers to self-care (Rosland, Heisler, Choi, Silveira, & Piette, 2010; Thomeer, Reczek, & Umberson, 2015; Thomeer, Umberson, & Pudrovska, 2013). Additionally, wives provide more spousal caregiving and health-related emotional support (Monin & Clark, 2011; Thomeer et al., 2015) that may be burdensome and lead to depressive symptoms. Bolstering this point, prior work found that wives (but not husbands) report significantly greater increases in depressive symptoms over time when their partners report greater physical pain (Polenick et al., 2017).
Previous research using the larger dataset analyzed in the present manuscript showed that individual-level and couple-level discordant conditions were linked to levels of and changes in functional disability within married or cohabiting couples (Polenick, Birditt, Turkelson, & Kales, 2019). Depressive symptoms were also found to moderate these links. Notably, husbands with discordant conditions and high-depressive symptoms (i.e., scores one standard deviation above the mean) had a significantly faster rate of increase in disability than husbands without discordant conditions who had high-depressive symptoms. A critical next step is to test whether individual-level and couple-level discordant conditions are associated with greater depressive symptoms over time, heightening risk of poor mental and physical health among aging couples.
The Present Study
Drawing from a nationally representative U.S. sample, this study considered how individual-level and couple-level discordant chronic health conditions are linked to depressive symptoms among middle-aged and older couples across an 8-year period. We focused on seven major chronic conditions that are strongly associated with morbidity and mortality (Fisher, Faul, Weir, & Wallace, 2005): arthritis, cancer, diabetes, heart disease, hypertension, lung disease, and stoke. Controlling for known predictors of depressive symptoms including sociodemographic characteristics (Vink, Aartsen, & Schoevers, 2008), negative marital quality (Rehman, Gollan, & Mortimer, 2008), and number of chronic health conditions (Read et al., 2017), we hypothesized that wives and husbands would report higher depressive symptoms when they or their partners had discordant conditions and when there were discordant conditions between spouses. We predicted that these links would become stronger over time. Finally, we predicted that the associations would be stronger for wives than for husbands.
Method
Sample and Procedures
Participants included a U.S. sample of 1,116 heterosexual married or cohabiting couples from five waves (2006–2014) of the nationally representative Health and Retirement Study (HRS). The HRS has collected data biennially with response rates of over 80% at each wave since 1992. All participants receive study information in the mail. Before each interview, participants are read a confidentiality statement and give oral consent. Since 2006, an enhanced face-to-face interview has also been conducted biennially with half of the panel respondents followed up by a self-administered psychosocial questionnaire (SAQ) with questions including the assessment of marital quality. Ethical approval was not required for the present analysis because these data are publicly available with no individual identifiers.
In 2006, phone interviews and SAQs were conducted with 7,635 participants, of whom 4,936 (65%) were married and 256 (3%) had a cohabiting partner. Of these, 4,692 (90%) had a partner who also completed a phone interview and SAQ in 2006. Twenty individuals in same-sex couples were not included to enable the estimation of effects for wives and husbands within couples and because the small sample precluded comparisons between same-sex and opposite-sex couples. Of the remaining participants, 2,598 (55.6%) were married to or cohabiting with the same partner (hereafter referenced as spouse) from 2006 to 2014 and participated in each wave.
Of the 2,598 participants, 366 were removed due to missing data, resulting in an analytic sample of 1,116 wives and husbands (see Table 1 for baseline characteristics and scores on major variables). Most (96.4%) were married at baseline. Relative to married participants, cohabiting participants were younger (women: b = −.06, p = .004; men: b = −.06, p = .013), less educated (men only: b = −.13, p = .009), reported more chronic conditions (women only: b = .42, p = .041), and had a partner with more chronic conditions (men only: b = .43, p = .043) but did not differ significantly on any other study variables.
Table 1.
Baseline Characteristics and Scores on Study Variables for Wives and Husbands
| Variable | Wives | Husbands | ||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age | 53.9*** | 8.8 | 57.3 | 8.3 |
| Education in years | 13.3 | 2.6 | 13.4 | 3.0 |
| Negative marital quality | 2.0** | 0.6 | 1.9 | 0.6 |
| Number of chronic health conditions | 1.6** | 1.2 | 1.7 | 1.2 |
| Functional disability | 0.2 | 0.8 | 0.2 | 0.7 |
| Depressive symptoms | 1.1*** | 1.7 | 0.9 | 1.4 |
| % | % | |||
| Minority status | 11.3 | 11.6 | ||
| Individual-level discordant conditions | 44.0 | 43.3 | ||
| Couple-level discordant conditions | 60.9 | 60.9 |
Note: N = 1,116 couples.
**Significant gender difference at p < .01. ***Significant gender difference at p < .001.
We conducted a power analysis using G*Power 3.1.9.2. There were 11,160 observations (2,232 individuals × 5 waves). With a design effect of 2.45 calculated using the intraclass correlation coefficient from the data, the effective sample size was 4,555 (11,160 observations divided by 2.45). The power to detect associations between discordant conditions and depressive symptoms was .98 with an effect as small as .01 and a maximum of 32 predictors/covariates.
We tested whether the study participants were significantly different from the 2,308 married or cohabiting couples not included in this study because one or both spouses had missing data on study variables in one or more waves after baseline. Wives and husbands who were younger (wives: b = −.06, p < .001; husbands: b = −.07, p < .001), had more education (wives: b = .08, p < .001; husbands: b = .05, p < .001), reported fewer chronic conditions (wives: b = −.13, p = .03; husbands: b = −.17, p = .003), had a spouse with fewer chronic conditions (wives: b = −.22, p < .001; husbands: b = −.19, p = .003), reported fewer depressive symptoms (wives: b = −.06, p = .02; husbands: b = −.10, p = .002), and had couple-level discordant conditions (wives: b = .23, p < .001; husbands: b = .22, p = .001) were significantly more likely to be included. Both wives (b = −.23, p = .002) and husbands (b = −.20, p = .006) were significantly more likely to be included when wives reported lower negative marital quality.
Measures
Depressive symptoms
Depressive symptoms were assessed at each wave using the eight-item Center for Epidemiologic Studies Depression Scale (CES-D; Steffick, 2000). Responses to this scale among older adults have shown good reliability and validity (Karim, Weisz, Bibi, & ur Rehman, 2015; Steffick, 2000). Participants reported whether they had experienced the following much of the time during the past week: felt everything was an effort, had restless sleep, could not get going, felt depressed, felt lonely, felt sad, was happy, enjoyed life. Ratings for the two positive items were reverse coded and items were summed (wives: α range = .79– .81; husbands: α range = .71–.76). Total scores ≥4 reflect clinically relevant depressive symptoms (Steffick, 2000).
Individual-level and couple-level discordant chronic conditions
At each wave, participants reported whether they had been diagnosed by a physician with seven major chronic health conditions: arthritis, cancer, diabetes, heart disease, hypertension, lung disease, and stroke. These conditions were selected because of their prevalence and strong associations with morbidity and mortality among older adults (Fisher et al., 2005). Individual-level discordant conditions occurred when participants had one or more conditions with discordant management requirements (1 = yes, −1 = no) based on prior literature (Bowling et al., 2017; Lagu et al., 2008; Piette & Kerr, 2006). Diabetes, heart disease, hypertension, and stroke are all considered to be concordant with one another because they share the common self-management goal of cardiovascular risk reduction, whereas the remaining combinations of conditions are considered to be discordant. In total, there were 15 possible pairs of discordant conditions (see Supplementary Table 1). We considered both own and partner reports of individual-level discordant conditions. Couple-level discordant conditions assessed whether participants reported having one or more conditions that are discordant from one or more of their partners’ conditions (1 = yes, −1 = no).
Time
Time (year centered at baseline in 2006) was considered as a moderator to determine whether the associations in this study became stronger across the 8-year period.
Covariates
Covariates included baseline sociodemographic characteristics: age, minority status (1 = racial/ethnic minority, −1 = non-Hispanic White), and education in years. We also controlled for individual-level depressive symptoms in the previous wave to consider significant increases from one wave to the next. We controlled for own and partner reports of baseline negative marital quality and number of chronic health conditions in each wave. Negative marital quality was measured with four brief, but widely used, items (Schuster, Kessler, & Aseltine, 1990; Walen & Lachman, 2000). Participants reported how often their spouse makes too many demands on them; criticizes them; lets them down when counted upon; and gets on their nerves from 1 (a lot) to 4 (not at all). Items were reverse coded and averaged (wives: α = .78; husbands: α = .76). Responses to this measure have shown good reliability and construct validity (Bertera, 2005; Schuster et al., 1990; Walen & Lachman, 2000).
In post hoc tests, we considered own and partner functional disability at each wave. Participants reported whether they had difficulty (1 = yes, 0 = no) with six activities of daily living (ADL; walking across the room, dressing, bathing, eating, getting in and out of bed, using the toilet) and five instrumental activities of daily living (IADL; preparing meals, shopping for groceries, making phone calls, taking medications, and handling money). Summed scores for total ADL/IADL disability were created.
Statistical Analysis
We estimated longitudinal actor-partner interdependence models (APIMs) using the MIXED procedure in SPSS version 24. This multilevel approach evaluates whether individual and partner variables predict outcomes within couples over time (Kenny, Kashy, & Cook, 2006). The lower level of the model represented variability due to within-person repeated measures for wives and husbands, whereas the upper level represented between-couple variability. Correlated errors between wives and husbands were permitted within a given wave using a heterogeneous compound symmetry error structure. Thus, the models accounted for nonindependence within couples and across time. We used maximum likelihood estimation to facilitate model comparison. We determined whether there was a significant difference in fit between Step 1 of Models 1 and 2 and between Step 1 and Step 2 of Models 1 and 2 by subtracting their −2 log likelihood estimations and examining differences on a chi-square distribution with degrees of freedom equaling the change in number of parameters (Singer & Willett, 2003).
In this study, actor effects represent how wives’ and husbands’ discordant conditions predict their own depressive symptoms, whereas partner effects represent how their partners’ discordant conditions predict their own depressive symptoms. Model 1 included own and partner individual-level discordant conditions in the same wave as predictors and controlled for time (centered at baseline), baseline age, minority status, education in years, own and partner baseline negative marital quality, both partners’ number of chronic health conditions at each wave, and previous wave depressive symptoms. In Step 1, we assessed how own and partner individual-level discordant conditions are concurrently linked to depressive symptoms over time. In Step 2, we considered whether the associations between own and partner individual-level discordant conditions and depressive symptoms became stronger over time by adding two interaction terms (own individual-level discordant conditions × time; partner individual-level discordant conditions × time). In Model 2, we considered whether couple-level discordant conditions predict depressive symptoms among wives and husbands. Couple-level discordant conditions in the same wave were added as a predictor (in addition to Model 1 predictors and covariates) in Step 1 to determine their concurrent links to depressive symptoms over and above individual-level discordant conditions. Step 2 included an interaction term (couple-level discordant conditions × time) to consider whether the association between couple-level discordant conditions and depressive symptoms became stronger over time.
Separate intercepts and slopes for wives and husbands were estimated using spouse gender (1 = wife, −1 = husband) as a distinguishing variable. Continuous baseline covariates were grand mean centered and continuous time-varying covariates were person-level mean centered (Kenny et al., 2006). We evaluated the nature of two-way significant interactions between discordant conditions and time by using the Johnson–Neyman region of significance approach (Johnson & Fay, 1950; Preacher, Curran, & Bauer, 2006) to determine the time range during the study period when individual-level and couple-level discordant conditions were significantly associated with depressive symptoms. We also estimated simple slopes for wives and husbands at the baseline wave (2006), the middle wave (2010), and the final wave (2014).
Results
Baseline characteristics and scores on major study variables are given in Table 1. We conducted paired t tests and McNemar tests in preliminary analyses to evaluate baseline differences between wives and husbands. Relative to husbands, wives were significantly younger and reported higher negative marital quality, higher depressive symptoms, and fewer chronic conditions. Supplementary Table 1 shows the frequency of the 15 combinations of individual-level and couple-level discordant conditions at baseline and at the final wave. Mean depressive symptoms and the prevalence of clinically relevant depressive symptoms at each study wave are shown in Supplementary Table 2. The rates of clinically relevant depressive symptoms were relatively low for wives (range = 8.8%–10.8%) and husbands (range = 5.7%–7.1%).
Discordant Conditions Within Couples and Depressive Symptoms Over Time
Wives’ depressive symptoms
Table 2 shows that wives reported significantly higher depressive symptoms when they had discordant conditions in the same wave in Model 1 (b = .16, p < .001). Husbands’ discordant conditions were not significantly linked to wives’ depressive symptoms in the same wave.
Table 2.
Longitudinal Actor-Partner Interdependence Model Examining the Dyadic Effects of Individual-Level and Couple-Level Discordant Conditions on Depressive Symptoms for Wives and Husbands
| Parameter | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Wife depressive symptoms | Husband depressive symptoms | Wife depressive symptoms | Husband depressive symptoms | |||||
| b | SE | b | SE | b | SE | b | SE | |
| Step 1 | ||||||||
| Actor Age | −.02*** | .00 | −.01** | .00 | −.02*** | .00 | −.01** | .00 |
| Actor Minority status | .08 | .06 | .07 | .05 | .08 | .06 | .07 | .05 |
| Actor Education in years | −.13*** | .01 | −.09*** | .01 | −.13*** | .01 | −.08*** | .01 |
| Actor Negative marital quality at baseline | .46*** | .06 | .26*** | .06 | .46*** | .06 | .26*** | .06 |
| Partner Negative marital quality at baseline | .12 | .07 | .27*** | .06 | .12 | .07 | .27*** | .06 |
| Actor Total chronic conditions in same wave | .01 | .06 | .01 | .04 | .00 | .06 | −.01 | .04 |
| Partner Total chronic conditions in same wave | −.02 | .05 | −.06 | .05 | −.02 | .05 | −.07 | .05 |
| Time | .00 | .02 | .00 | .02 | .00 | .02 | .00 | .02 |
| Actor Depressive symptoms in previous wave | −.35*** | .02 | −.30*** | .02 | −.35*** | .02 | −.30*** | .02 |
| Actor Individual-level discordant conditions | .16*** | .04 | .12*** | .03 | .15*** | .04 | .09** | .03 |
| Partner Individual-level discordant conditions | −.01 | .03 | .02 | .03 | −.02 | .04 | −.01 | .03 |
| Couple-level discordant conditions | .03 | .04 | .12*** | .03 | ||||
| −2 Log Likelihood | 29603.818 | 29590.974 | ||||||
| Change in −2 Log Likelihood (Model 1 ➔ Model 2) | 12.844** | |||||||
| Step 2 | ||||||||
| Actor Individual-level discordant conditions × Time | .05* | .02 | .04* | .02 | .05* | .02 | .05** | .02 |
| Partner Individual-level discordant conditions × Time | −.00 | .02 | .00 | .02 | −.00 | .02 | .01 | .02 |
| Couple-level discordant conditions × Time | −.01 | .03 | −.03 | .02 | ||||
| −2 Log Likelihood | 29591.554 | 29575.920 | ||||||
| Change in −2 Log Likelihood (Step 1 ➔ Step 2) | 12.264* | 15.054* |
Note: N = 1,116 couples. Estimates are presented from each step of the models.
*p < .05. **p < .01. ***p < .001.
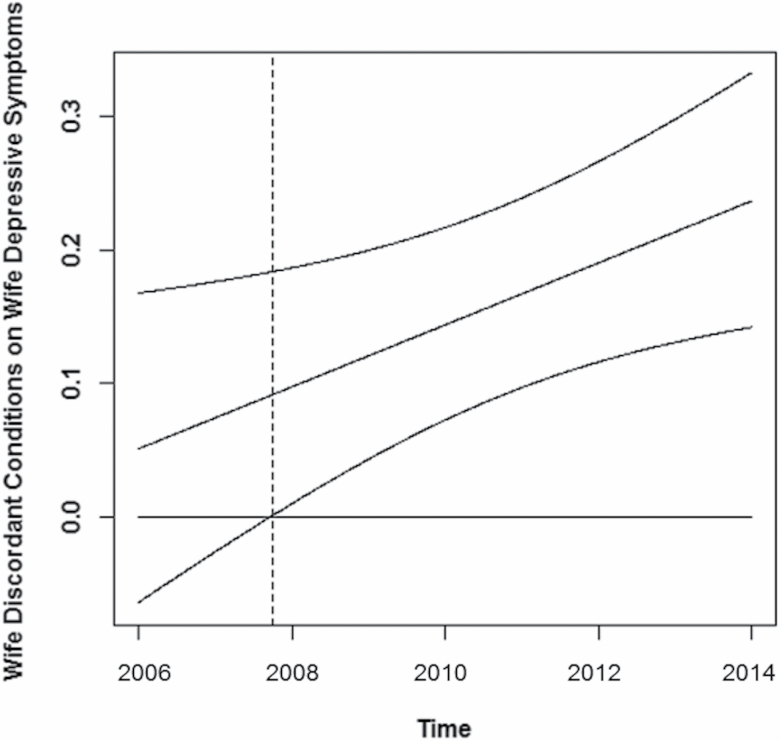
In Model 1, the interaction between wives’ discordant conditions and time was significant (b = .05, p = .02). The region of significance for time (centered at baseline) was −19.40 to 0.88. Scores above and below this region are statistically significant at p < .05. The lower bound is outside the possible time range. Therefore, wives with discordant conditions reported significantly higher depressive symptoms slightly less than 2 years after baseline (i.e., 2008), and this significant association increased in strength across subsequent waves (Figure 1). Wives who had discordant conditions reported significantly higher depressive symptoms than their counterparts without discordant conditions in 2010 (b = .14, p < .001) and in 2014 (b = .24, p < .001) but not in 2006 (b = .05, p = .39), Supplementary Figure 1.
Figure 1.
Confidence bands for the observed sample values of time and the simple slope for wives’ individual-level discordant chronic conditions on their own depressive symptoms. The area to the right of the dotted line represents statistical significance at p < .05.
Couple-level discordant conditions were not significantly associated with depressive symptoms in Model 2. The interaction between couple-level discordant conditions and time was not significant.
Husbands’ depressive symptoms
As given in Table 2, husbands reported significantly higher depressive symptoms when they had discordant conditions in the same wave in Model 1 (b = .12, p < .001). Wives’ discordant conditions were not significantly associated with husbands’ depressive symptoms in the same wave.
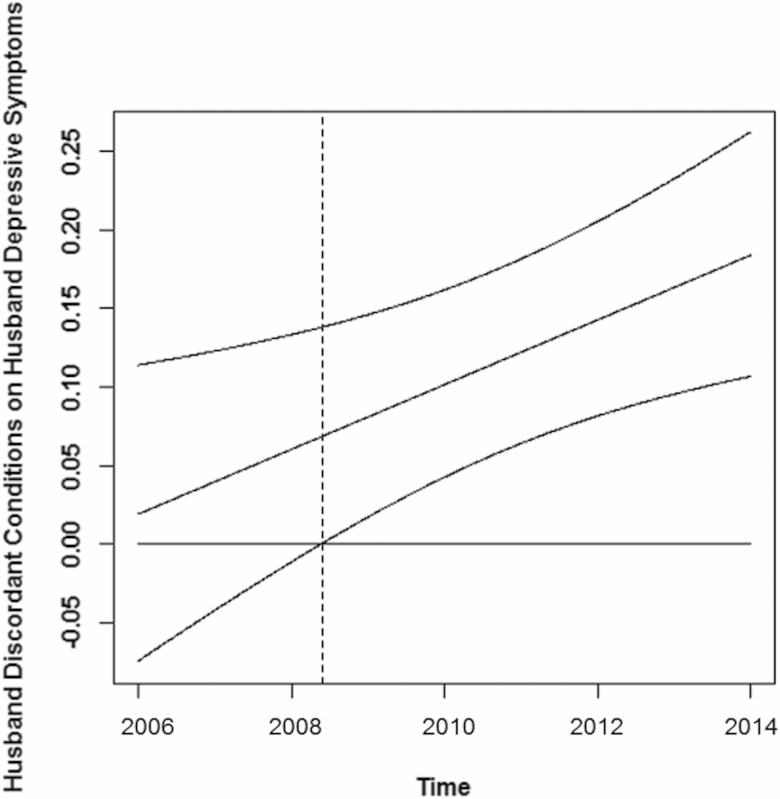
The interaction between husbands’ discordant conditions and time was significant in Model 1 (b = .04, p = .01). The region of significance for time (centered at baseline) was −9.84 to 1.20. Scores above and below this region are statistically significant at p < .05. The lower bound is outside the possible time range. Thus, husbands with discordant conditions reported significantly higher depressive symptoms slightly more than 2 years after baseline (i.e., 2008), with this association becoming stronger in later waves (Figure 2). Husbands who had discordant conditions reported significantly higher depressive symptoms than their counterparts without discordant conditions in 2010 (b = .10, p < .001) and in 2014 (b = .18, p < .001) but not in 2006 (b = .02, p = .69), Supplementary Figure 2.
Figure 2.
Confidence bands for the observed sample values of time and the simple slope for husbands’ individual-level discordant conditions on their own depressive symptoms. The area to the right of the dotted line represents statistical significance at p < .05.
In Model 2, husbands also reported significantly higher depressive symptoms when there were couple-level discordant conditions in the same wave (b = .12, p < .001). The interaction between couple-level discordant conditions and time was not significant.
Post Hoc Tests
To consider whether the association between own individual-level discordant conditions and depressive symptoms varied on the basis of partner individual-level discordant conditions, we added interaction terms in Step 1 (own discordant conditions × partner discordant conditions) and Step 2 (own discordant conditions × partner discordant conditions × time) of Model 1. In Step 2, we included all two-way interaction terms within the three-way interaction. None of the interaction terms were significant, indicating that the link between individual-level discordant conditions and depressive symptoms was not significantly stronger among wives and husbands when their partners also had discordant conditions.
We also estimated the main models with own and partner functional disability at each waves as additional covariates. The findings did not change, which shows that the links between discordant conditions and depressive symptoms are independent of both spouses’ functional disability over time.
Discussion
The present study extends research on multimorbidity by demonstrating that individual-level discordant chronic conditions are associated with depressive symptoms among middle-aged and older wives and husbands over time. Above and beyond this link, couple-level discordant conditions were associated with husbands’ depressive symptoms. These associations were observed when controlling for sociodemographic characteristics, each partner’s perceived marital quality, and own and partner number of chronic conditions and functional disability over time. Hence, this study shows that the concordant–discordant model of comorbidities can be expanded using interdependence theory and compatibility theories of marriage to consider the distinct implications of both individual and couple patterns of chronic conditions for well-being.
Individual-Level Discordant Conditions and Depressive Symptoms
Consistent with our hypothesis, wives and husbands reported significantly higher depressive symptoms when they had their own discordant conditions; however, these links were not observed at baseline but developed and intensified across the 8-year period. These findings indicate that individual-level discordant conditions may not have immediate consequences for depressive symptoms; rather, this link appears to unfold and build over time. The emotional strain of conditions with competing self-management goals might accumulate, especially if illness management worsens (Lagu et al., 2008) or increasingly disrupts everyday life (Devins et al., 1993). Bidirectional links may also occur such that distressed individuals become less able to self-manage (Ciechanowski, Katon, & Russo, 2000; Detweiler-Bedell, Friedman, Leventhal, Miller, & Leventhal, 2008; Harrison et al., 2012; McKellar, Humphreys, & Piette, 2004), which in turn perpetuates and amplifies depressive symptoms.
Counter to our prediction, individual-level discordant conditions managed by one’s partner were not significantly linked to depressive symptoms among wives or husbands. This indicates that one’s own individual-level discordant conditions are more consequential for depressive symptoms in middle and later life. Moreover, post hoc tests revealed that individual-level discordant conditions were not more strongly associated with depressive symptoms when both partners managed discordant conditions, further underscoring the key importance of one’s own chronic condition discordance.
Couple-Level Discordant Conditions and Depressive Symptoms
In partial support of our hypothesis, over and above individual-level discordant conditions, husbands (but not wives) reported higher concurrent depressive symptoms when there were discordant conditions between spouses. Counter to prediction, this link did not become stronger over time, indicating that couple-level discordant conditions have more proximal and sustained implications for well-being among husbands. Relative to women, men depend more on partners for emotional support and assistance in managing their health (August & Sorkin, 2010; Monin & Clark, 2011; Umberson, 1992). When wives have chronic conditions with self-management goals which diverge from their husbands’ self-management, the time that wives spend providing support to maintain husbands’ well-being may diminish. A wife with arthritis, for example, must allocate time and energy toward managing her own physical pain and stiffness, which detracts from supporting her husband who has different self-management needs for an arthritis-discordant condition such as diabetes or lung disease.
Although, we predicted that the link between couple-level discordant conditions and depressive symptoms would be stronger among wives as a result of receiving less and giving more health-related partner support (e.g., Monin & Clark, 2011; Rosland et al., 2010), couple-level discordant conditions were not significantly linked to wives’ depressive symptoms. It therefore seems that wives are generally able to preserve their own well-being when faced with illness self-management demands that differ from husbands’ self-management activities, even though this may magnify husbands’ need for health-related support. Considering that older women frequently provide spousal caregiving (Monin & Clark, 2011), this finding is encouraging and indicates psychological resilience among wives who likely help to manage their partners’ complex chronic conditions along with their own health problems.
Strengths and Limitations
Strengths of this study include a relatively large number of couples drawn from a nationally representative sample and our consideration of both individual-level and couple-level discordant chronic conditions. Of note, multilevel models controlled for sociodemographic characteristics, baseline negative marital quality, and the number of chronic health conditions reported by each partner across waves. As such, the findings are robust and indicate that discordant conditions within couples have distinct implications for depressive symptoms beyond established predictors of well-being and medical morbidity burden.
We acknowledge six primary limitations. First, chronic conditions were assessed by self-report, which may introduce bias. Second, the assessment of chronic health conditions in the HRS was limited to seven major conditions, possibly underestimating the occurrence of individual-level and couple-level discordant conditions. Third, average levels of depressive symptoms and rates of clinically relevant symptoms were low in this sample. As a result, it is unknown whether the findings generalize to couples in which one or both partners have clinically significant depression. Furthermore, some associations (e.g., the link between partner discordant conditions and one’s own depressive symptoms) may not have been detected due to low overall levels of depressive symptoms; thus, the present study should be replicated in a sample with higher depressive symptoms reported by one or both spouses. Fourth, couples in this study were married or cohabiting and heterosexual, limiting generalizability to non-cohabiting and same-sex couples. Fifth, most couples were non-Hispanic White, and so the findings may not generalize to more ethnically diverse couples. Sixth, there were significant differences in sociodemographic and health characteristics between couples in this study and couples who were excluded because of missing data. Couples in this study, for instance, were younger, more educated, had fewer chronic conditions, had fewer depressive symptoms, and included wives who reported lower negative marital quality. Given these differences, the findings may not apply to couples who are older, less educated, have greater medical morbidity and psychological distress, and have poorer quality marriages. Nevertheless, this study generates novel information on aspects of multiple chronic conditions managed among middle-aged and older couples that warrants additional research attention.
Future Directions
Future studies should consider potential pathways which may explain the current findings. In particular, it will be important to understand daily elements of illness self-management and the marital relationship that are linked to psychological distress among couples managing individual-level and couple-level discordant conditions. Wives and husbands who have discordant conditions, for example, might report higher depressive symptoms on days when they feel less confident about managing their own health problems. Similarly, when there are couple-level discordant conditions, husbands may report higher depressive symptoms on days when they perceive less spousal support. Learning more about proximal processes would allow for an in-depth understanding of individuals and couples who are more vulnerable to experiencing depressive symptoms.
Determining short-term mechanisms might also pinpoint modifiable factors to target during interventions. For instance, integrated care focused on broadly beneficial lifestyle behaviors (e.g., exercise to manage both arthritis and heart disease) may improve well-being and self-management among individuals with discordant conditions, whereas couple therapy to address illness-related relationship challenges might attenuate husbands’ depressive symptoms in the presence of couple-level discordant conditions. Interventions to reduce depressive symptoms among people with multiple chronic conditions have been found to be effective in improving long-term health (Gallo et al., 2016; Smith, Wallace, O’Dowd, & Fortin, 2016). Identifying how spouses individually and jointly manage chronic illness in ways that may make them more or less resilient would enhance the delivery of innovative care models that account for partner and family contexts.
Conclusion
In summary, the present study demonstrates that both individual-level and couple-level discordant chronic conditions are common and show long-term associations with depressive symptoms in midlife and later life. Most middle-aged and older adults with chronic illness are married and have a partner who manages one or more health conditions (Piette et al., 2010). As a consequence, routine clinical care and interventions to protect the well-being of individuals with chronic illness should consider the conditions managed by both members of a couple. Understanding spousal interdependence in the daily self-management of complex conditions would facilitate more personalized treatment of chronic illness and multimorbidity.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health (grant number R03AG057838-01 to C.A.P.).
Conflict of Interest
The authors have no conflicts of interest to report.
Supplementary Material
Acknowledgments
These findings were presented in part at the 2019 Claude D. Pepper Older Americans Independence Centers (OAIC) Annual Meeting in Arlington, VA. The data, analytic methods, and study materials will be made available to other researchers upon request.
References
- August, K. J., & Sorkin, D. H (2010). Marital status and gender differences in managing a chronic illness: The function of health-related social control. Social Science & Medicine (1982), 71, 1831–1838. doi:10.1016/j.socscimed.2010.08.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertera, E. M (2005). Mental health in US adults: The role of positive social support and social negativity in personal relationships. Journal of Social and Personal Relationships, 22, 33–48. doi:10.1177/0265407505049320 [Google Scholar]
- Bowling, C. B., Plantinga, L., Phillips, L. S., McClellan, W., Echt, K., Chumbler, N.,…Johnson, T. M.II (2017). Association of multimorbidity with mortality and healthcare utilization in chronic kidney disease. Journal of the American Geriatrics Society, 65, 704–711. doi:10.1111/jgs.14662 [DOI] [PubMed] [Google Scholar]
- Boyd, C. M., & Fortin, M (2010). Future of multimorbidity research: How should understanding of multimorbidity inform health system design?. Public Health Reviews, 32, 451–474. doi:10.1007/BF03391611 [Google Scholar]
- Buttorff, C., Ruder, T., & Bauman, M (2017). Multiple chronic conditions in the United States. Santa Monica, CA: RAND. doi:10.7249/TL221 [Google Scholar]
- Ciechanowski, P. S., Katon, W. J., & Russo, J. E (2000). Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs. Archives of Internal Medicine, 160, 3278–3285. doi:10.1001/archinte.160.21.3278 [DOI] [PubMed] [Google Scholar]
- Crawford, D. W., Houts, R. M., Huston, T. L., & George, L. J (2004). Compatibility, leisure, and satisfaction in marital relationships. Journal of Marriage and Family, 64, 433–449. doi:10.1111/j.1741-3737.2002.00433.x [Google Scholar]
- Detweiler-Bedell, J. B., Friedman, M. A., Leventhal, H., Miller, I. W., & Leventhal, E. A (2008). Integrating co-morbid depression and chronic physical disease management: Identifying and resolving failures in self-regulation. Clinical Psychology Review, 28, 1426–1446. doi:10.1016/j.cpr.2008.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devins, G. M., Edworthy, S. M., Paul, L. C., Mandin, H., Seland, T. P., & Klein, G. M (1993). Illness intrusiveness and depressive symptoms over the adult years: Is there a differential impact across chronic conditions?. Canadian Journal of Behavioural Science, 25, 400–413. doi:10.1037/h0078842 [Google Scholar]
- Fisher, G. G., Faul, J. D., Weir, D. R., & Wallace, R. B (2005). Documentation of chronic disease measures in the Health and Retirement Study (HRS/AHEAD). HRS/AHEAD Documentation Report. Survey Research Center University of Michigan, Ann Arbor, MI. [Google Scholar]
- Gallo, J. J., Hwang, S., Joo, J. H., Bogner, H. R., Morales, K. H., Bruce, M. L., & Reynolds, C. F.III (2016). Multimorbidity, depression, and mortality in primary care: Randomized clinical trial of an evidence-based depression care management program on mortality risk. Journal of General Internal Medicine, 31, 380–386. doi:10.1007/s11606-015-3524-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, R. A., Ling, S. M., Briss, P. A., Parrish, R. G., Salive, M. E., & Finke, B. S (2016). Multimorbidity patterns in the United States: Implications for research and clinical practice. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 71, 215–220. doi:10.1093/gerona/glv199 [DOI] [PubMed] [Google Scholar]
- Harrison, M., Reeves, D., Harkness, E., Valderas, J., Kennedy, A., Rogers, A.,…Bower, P (2012). A secondary analysis of the moderating effects of depression and multimorbidity on the effectiveness of a chronic disease self-management programme. Patient Education and Counseling, 87, 67–73. doi:10.1016/j.pec.2011.06.007 [DOI] [PubMed] [Google Scholar]
- Hill, M. S (1988). Marital stability and spouses’ shared time: A multidisciplinary hypothesis. Journal of Family Issues, 9, 427–451. doi:10.1177/019251388009004001 [Google Scholar]
- Homish, G. G., & Leonard, K. E (2008). The drinking partnership and marital satisfaction: The longitudinal influence of discrepant drinking. Journal of Consulting and Clinical Psychology, 75, 43–51. doi:10.1037/0022-006X.75.1.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, P. O., & Fay, L. C (1950). The Johnson–Neyman technique, its theory and application. Psychometrika, 15, 349–367. doi:10.1007/BF02288864 [DOI] [PubMed] [Google Scholar]
- Karim, J., Weisz, R., Bibi, Z., & ur Rehman, S (2015). Validation of the eight-item center for epidemiologic studies depression scale (CES-D) among older adults. Current Psychology, 34, 681–692. doi:10.1007/s12144-014-9281-y [Google Scholar]
- Kenny, D. A., Kashy, D. A., & Cook, W. L (2006). Dyadic data analysis. New York, NY: : Guilford Press. [Google Scholar]
- Lagu, T., Weiner, M. G., Hollenbeak, C. S., Eachus, S., Roberts, C. S., Schwartz, J. S., & Turner, B. J (2008). The impact of concordant and discordant conditions on the quality of care for hyperlipidemia. Journal of General Internal Medicine, 23, 1208–1213. doi:10.1007/s11606-008-0647-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinger, G., & Rands, M (1985). Compatibility in marriage and other close relationships. In Ickes W. (Ed.), Compatible and incompatible relationships. Springer series in social psychology (pp. 309–331). New York, NY: Springer. [Google Scholar]
- Masters, S., Oliver-Baxter, J., Barton, C., Summers, M., Howard, S., Roeger, L., & Reed, R (2013). Programmes to support chronic disease self-management: Should we be concerned about the impact on spouses? Health & Social Care in the Community, 21, 315–326. doi:10.1111/hsc.12020 [DOI] [PubMed] [Google Scholar]
- McKellar, J. D., Humphreys, K., & Piette, J. D (2004). Depression increases diabetes symptoms by complicating patients’ self-care adherence. Diabetes Educator, 30, 485–492. doi:10.1177/014572170403000320 [DOI] [PubMed] [Google Scholar]
- Monin, J. K., & Clark, M. S (2011). Why do men benefit more from marriage than do women? Thinking more broadly about interpersonal processes that occur within and outside of marriage. Sex Roles, 65, 320–326. doi:10.1007/s11199-011-0008-3 [Google Scholar]
- Piette, J. D., & Kerr, E. A (2006). The impact of comorbid chronic conditions on diabetes care. Diabetes Care, 29, 725–731. doi:10.2337/diacare.29.03.06.dc05-2078 [DOI] [PubMed] [Google Scholar]
- Piette, J. D., Rosland, A. M., Silveira, M., Kabeto, M., & Langa, K. M (2010). The case for involving adult children outside of the household in the self-management support of older adults with chronic illnesses. Chronic Illness, 6, 34–45. doi:10.1177/1742395309347804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polenick, C. A., Birditt, K. S., Turkelson, A., & Kales, H. C (2019). Individual-level and couple-level discordant chronic conditions: Longitudinal links to functional disability. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polenick, C. A., Brooks, J. M., & Birditt, K. S (2017). Own and partner pain intensity in older couples: Longitudinal effects on depressive symptoms. Pain, 158, 1546–1553. doi:10.1097/j.pain.0000000000000949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polenick, C. A., Renn, B. N., & Birditt, K. S (2018). Dyadic effects of depressive symptoms on medical morbidity in middle-aged and older couples. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 37, 28–36. doi:10.1037/hea0000573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher, K. J., Curran, P. J., & Bauer, D. J (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. doi:10.3102/10769986031004437 [Google Scholar]
- Pruchno, R. A., Wilson-Genderson, M., & Heid, A. R (2016). Multiple chronic condition combinations and depression in community-dwelling older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 71, 910–915. doi:10.1093/gerona/glw025 [DOI] [PubMed] [Google Scholar]
- Read, J. R., Sharpe, L., Modini, M., & Dear, B. F (2017). Multimorbidity and depression: A systematic review and meta-analysis. Journal of Affective Disorders, 221, 36–46. doi:10.1016/j.jad.2017.06.009 [DOI] [PubMed] [Google Scholar]
- Rehman, U. S., Gollan, J., & Mortimer, A. R (2008). The marital context of depression: Research, limitations, and new directions. Clinical Psychology Review, 28, 179–198. doi:10.1016/j.cpr.2007.04.007 [DOI] [PubMed] [Google Scholar]
- Rodriguez, L. M., Neighbors, C., & Knee, C. R (2014). Problematic alcohol use and marital distress: An interdependence theory perspective. Addiction Research and Theory, 22, 294–312. doi:10.3109/16066359.2013.841890 [Google Scholar]
- Rosland, A. M., Heisler, M., Choi, H. J., Silveira, M. J., & Piette, J. D (2010). Family influences on self-management among functionally independent adults with diabetes or heart failure: Do family members hinder as much as they help? Chronic Illness, 6, 22–33. doi:10.1177/1742395309354608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusbult, C. E., & Van Lange, P. A (2008). Why we need interdependence theory. Social and Personality Psychology Compass, 2, 2049–2070. doi:10.1111/j.1751-9004.2008.00147.x [Google Scholar]
- Schuster, T. L., Kessler, R. C., & Aseltine, R. H.Jr (1990). Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology, 18, 423–438. doi:10.1007/BF00938116 [DOI] [PubMed] [Google Scholar]
- Singer, J. D., Willett, J. B., & Willett, J. B (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: : Oxford University Press. [Google Scholar]
- Smith, S. M., Wallace, E., O’Dowd, T., & Fortin, M (2016). Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database of Systematic Reviews, 3, CD006560. doi:10.1002/14651858.CD006560.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffick, D. E (2000). Documentation of affective functioning measures in the Health and Retirement Study. HRS/AHEAD Documentation Report. Ann Arbor, MI: Survey Research Center University of Michigan. [Google Scholar]
- Thomeer, M. B (2016). Multiple chronic conditions, spouse’s depressive symptoms, and gender within marriage. Journal of Health and Social Behavior, 57, 59–76. doi:10.1177/0022146516628179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer, M. B., Reczek, C., & Umberson, D (2015). Gendered emotion work around physical health problems in mid- and later-life marriages. Journal of Aging Studies, 32, 12–22. doi:10.1016/j.jaging.2014.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomeer, M. B., Umberson, D., & Pudrovska, T (2013). Marital processes around depression: A gendered and relational perspective. Society and Mental Health, 3, 151–169. doi:10.1177/2156869313487224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D (1992). Gender, marital status and the social control of health behavior. Social Science & Medicine (1982), 34, 907–917. doi:10.1016/0277-9536(92)90259-s [DOI] [PubMed] [Google Scholar]
- Vink, D., Aartsen, M. J., & Schoevers, R. A (2008). Risk factors for anxiety and depression in the elderly: A review. Journal of Affective Disorders, 106, 29–44. doi:10.1016/j.jad.2007.06.005 [DOI] [PubMed] [Google Scholar]
- Walen, H. R., & Lachman, M. E (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17, 5–30. doi:10.1177/0265407500171001 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.