Abstract
Despite progress in increasing the use of modern contraceptives in most Latin American countries over the last few decades, important challenges remain, including the heavy reliance on out-of-pocket spending to access contraceptives, which may expose consumption to macroeconomic fluctuations. Out-of-pocket spending on contraceptives and/or the proportion of women aged 15–49 who received free contraceptives at a public health facility or as part of statutory health insurance were estimated for 13 Latin American countries using the most recently available household budget surveys and demographic and health or similar household surveys. Data on contraceptive retail sales in 12 countries over the 2006–2010 period and publicly available macroeconomic indicators were used to examine the relationship between changes in sales and macroeconomic indicators using multiple regression models. On average, women aged 15–49 spent close to US$1 per month out-of-pocket on contraceptives. However, almost three out of five women received them free of charge. A 1% increase in the percentage of the population living on less than US$ 3.2/day (2011 PPP values), or the percentage unemployed in the labour force, predicted about a 2% decrease in the growth of contraceptive retail sales (measured in couple-years of protection, CYP, per capita) the subsequent year. The analysis revealed the sensitivity of contraceptive retail sales to changes in macroeconomic variables, particularly changes in poverty levels. Achieving universal access to family planning by 2030 will require improving contraceptive financing schemes.
Keywords: contraceptives, out-of-pocket expenses, Latin America, access to care, family planning financing
Résumé
En dépit de l’accroissement de l’emploi de contraceptifs modernes dans la plupart des pays d’Amérique latine ces dernières décennies, d’importantes difficultés demeurent, notamment le fait que l’accès aux contraceptifs occasionne d’importantes dépenses personnelles, ce qui peut exposer la consommation à des fluctuations macro-économiques. Les enquêtes les plus récentes sur le budget des ménages ou les enquêtes démographiques et de santé ou autres menées auprès des familles ont permis d’estimer les dépenses à la charge des utilisateurs de contraceptifs et/ou la proportion de femmes âgées de 15 à 49 ans qui ont reçu des contraceptifs gratuits dans un centre de santé publique ou dans le cadre d’un régime obligatoire d’assurance maladie dans 13 pays latino-américains. Les données sur les ventes au détail de contraceptifs dans 12 pays au cours de la période 2006–2010 et les indicateurs macro-économiques disponibles publiquement ont été utilisés pour examiner la relation entre l’évolution des ventes et les indicateurs macro-économiques, au moyen de différents modèles de régression. En moyenne, les femmes âgées de 15 à 49 ans dépensaient près d’un dollar par mois pour des contraceptifs. Néanmoins, près de trois femmes sur cinq les recevaient gratuitement. Une augmentation de 1% dans le pourcentage de la population vivant avec moins de 3,2 dollars par jour (valeurs PPP 2011) ou le pourcentage de chômeurs dans la population active laissait prévoir une diminution de 2% de la croissance des ventes de contraceptifs au détail (mesurée en couple-année de protection, par habitant) l’année suivante. L’analyse a révélé que les ventes de contraceptifs au détail étaient sensibles aux modifications des variables macro-économiques, en particulier aux changements des niveaux de pauvreté. Pour mettre en place un accès universel à la planification familiale d’ici à 2030, sera nécessaire d’améliorer les plans de financement des contraceptifs.
Resumen
A pesar del progreso logrado para incrementar el uso de métodos anticonceptivos modernos en la mayoría de los países latinoamericanos en las últimas décadas, aún existen retos importantes, entre ellos la gran dependencia de gastos de bolsillo para acceder a los anticonceptivos, que podría exponer el consumo a fluctuaciones macroeconómicas. Los gastos de bolsillo en anticonceptivos y/o la proporción de mujeres de 15 a 49 años que recibieron anticonceptivos gratuitos en una unidad de salud pública o como parte de seguro médico obligatorio fueron estimados para 13 países latinoamericanos utilizando las encuestas domiciliarias más recientes sobre presupuestos, así como encuestas domiciliarias demográficas y de salud o encuestas similares. Se utilizaron datos sobre las ventas minoristas de anticonceptivos en 12 países durante el período de 2006 a 2010 e indicadores macroeconómicos disponibles públicamente para examinar la relación entre los cambios en ventas y los indicadores macroeconómicos utilizando diferentes modelos de regresión. En promedio, las mujeres de 15 a 49 años gastaron casi un dólar al mes de su propio bolsillo en anticonceptivos. Sin embargo, casi tres de cada cinco mujeres los recibieron sin costo alguno. Un aumento del 1% en el porcentaje de la población que vive con menos de US$ 3.2 al día (valores PPP para el año 2011) o en el porcentaje de personas desempleadas en la fuerza laboral predijo una disminución de un 2% en el crecimiento de ventas minoristas de anticonceptivos (medido por año de protección por pareja, CYP, per cápita) el año subsiguiente. El análisis reveló la sensibilidad de las ventas minoristas de anticonceptivos a los cambios en variables macroeconómicas, en particular cambios en niveles de pobreza. Para lograr acceso universal a los servicios de planificación familiar para el 2030, será necesario mejorar los esquemas de financiamiento de anticonceptivos.
Introduction
Despite the progress seen in most Latin American countries in the increased use of modern contraceptives, the prevalence of which is estimated to be close to 60%,1 important challenges remain, including large differences between and within countries and persistently high adolescent fertility rates.1–4 Furthermore, most of the increase in contraceptive prevalence has been driven by an increase in short-acting contraceptives (such as pills, injectables, condoms, and emergency contraception) rather than long-acting reversible contraceptives (intrauterine devices and subdermal implants) or permanent contraception (male and female sterilisation).5,6 Some of these issues may be partially explained by the way contraceptives are paid for. Indeed, access to contraceptives in the region relies heavily on out-of-pocket expenditures.3,5
As an important part of the health financing landscape in most Latin American countries, out-of-pocket spending can detrimentally affect access to required care and impose undue financial burdens on households.7–10 While this negative effect has been highlighted mostly in relation to the so-called catastrophic health events, deleterious effects on access to preventive and reproductive health services have been documented as well.11 Several analysts, for instance, have pointed out that the uptake of long-acting reversible contraceptives (LARCs) has been lower that could be expected given prevailing reproductive preferences and the evidence of LARCs’ safety and efficacy.1,5,12 The high upfront cost of LARCs has been identified as an important barrier for this uptake. Evidence from recent experiences among adolescents in the US suggests that when financial barriers are removed, both LARC uptake and unintended pregnancy rates are favourably impacted.13,14
The widespread use of short-acting contraceptives coupled with the reliance on out-of-pocket spending to pay for them can increase the exposure of contraceptive consumption to macroeconomic fluctuations, which tend to be recurrent in the region.15–17 While the negative effect of these fluctuations on the consumption of any kind has been well established,18 their effect on contraceptive use, in particular, has not been examined previously. As the region is set to achieve the Sustainable Development Goal (SDG) 3.7 of ensuring universal access to sexual and reproductive health care services by 2030, it is important to understand how existing contraceptive financing schemes in the region could hinder this plan.
The aim of this study is two-fold. First, we estimated out-of-pocket spending for contraceptives, as well as a closely related indicator, the proportion of women receiving contraceptives free of charge at a public health facility or as part of the statutory health insurance, for several countries in the region using the most recently available household surveys. Second, we examined the extent to which contraceptive retail sales are sensitive to changes in macroeconomic variables, including inflation, growth, and poverty rates, taking advantage of data on retail contraceptive sales from several countries during a period that included the global financial crisis of 2007–2008.
Methods
Sample
We focused on 14 out of the 33 Latin American countries, where close to 90% of the region’s population is concentrated, for which relevant data were available: Argentina, Brazil, Colombia, Chile, Costa Rica, Ecuador, El Salvador, Guatemala, Honduras, Mexico, Panama, Peru, Uruguay, and Venezuela. Depending on the analysis, the information required was available for between 9 and 12 out of the 14 countries. In particular, the regression of retail sales on macroeconomic variables did not include Brazil or Mexico. Sales were available from 2006 to 2010. For the out-of-pocket estimation, we used the most recent information over the last 15 years.
Measures and sources
Out-of-pocket spending for contraceptives was estimated using the most recently available household budget survey in each country, which ranged from 2005 to 2018. National statistical agencies periodically conduct this type of survey, which provides important inputs for consumer price indices and national accounts. These household surveys typically involve multiple questionnaires to capture expenditures that occur at different frequencies and are incurred by either the household or its individual members.19 Questions about contraceptive spending are generally included in an individual questionnaire (except for Colombia, where such questions were included in the household questionnaire). There is some level of harmonisation, with national statistical agencies in this sample building on international classifications.20,21 All surveys distinguish at least between mechanical (e.g. intrauterine device, diaphragm) and hormonal (e.g. pill, injectable, patch) contraceptives, although some include further distinctions. Additional details on the definitions in each country are provided in Table S1 in the supplementary materials. The surveys were implemented in different years and recorded in local currency that we converted to 2011 purchasing power parity (PPP) dollars to ensure comparability.22 Spending on condoms may be at least partially directed toward sexual transmitted disease prevention rather than contraception.
The estimation of women receiving contraceptives free of charge at a public health facility or as part of statutory or social health insurance was based on the most recent household survey focused on health or reproductive health available in each country, which ranged from 2004 to 2017. This includes the USAID-sponsored Demographic and Health Survey (DHS) and the US Centers for Disease Control-supported Reproductive Health Survey (RHS). In contrast, UNICEF’s Multiple Indicator Cluster Survey (MICS) does not inquire about the source of contraception.23 Local surveys were used in the cases of Argentina, Mexico, and Chile. In the first two cases, the surveys were roughly comparable to the DHS or RHS, with questions about the source of contraception following a set of questions about contraceptive knowledge and use. In the case of Chile, the question was embedded in a broader question about the source for drugs currently used by the respondent, included in a survey focused on health issues rather than reproductive health in particular. Additional details on the response items indicating the public source in each country are provided in Table S2 in the supplementary materials.
Retail sales data from 2006 to 2010 were obtained from IQVIA (at the time, IMS Health), a global consultancy firm widely recognised as an authoritative source of data by the pharmaceutical industry. While the de facto standard and, frequently, at least within the region, the only source for this information, their reliability has occasionally been questioned.24 The information for the present study encompassed pharmaceutical products in the categories G02B (intrauterine devices and vaginal rings) and G03A (pills, patches, implants and emergency contraception) from the Anatomical Therapeutic Chemical Classification (ATC). Condom retail sales were not included. IQVIA methodology is not publicly available but the estimation in each country is presumably based on sales records from a panel of pharmaceutical wholesalers and retailers. IQVIA measured pharmaceutical sales volumes in terms of the number of commercial packs, a unit that is difficult to compare across contraceptive methods or even within a single method (e.g. in the case of pills, a package generally but not always corresponds with a single cycle). Based on information on the pharmaceutical form, we re-expressed the volume in terms of the number of couple-years of protection (CYP) rather than the number of commercial packs.25 All the macroeconomic predictors were obtained from publicly available online databases.26,27 Table S3 in the supplementary materials provides additional details on the definitions of variables used.
Analysis
Estimations of out-of-pocket spending and the public provision of contraceptives were based on household surveys that used complex sample designs. As such, information on the design was incorporated into the estimation. While the specific characteristics of these household surveys vary, they are generally based on multistage cluster samples of households (with relatively compact area segments as the primary sampling unit to facilitate fieldwork). The segments are usually stratified before selection, for example, into rural and urban. Micro datasets always include weights that reflect the specific probability of inclusion of each unit as well as additional adjustments such as post-stratification. These weights were incorporated both on point and interval estimations. Cluster and stratum identifiers were generally (but not always) released to allow for correct interval estimation. When unavailable, such as in microdata from Argentina, Panama, and Uruguay, we used alternative indicators (large geographic identifiers, temporal identifiers, and quantiles of income) to approximately incorporate clustering in the interval estimation.
To assess the relationship between macroeconomic variables and contraceptive retail sales, we used different regression approaches, including ordinary least squares (OLS), mixed-effect models fitted by restricted maximum likelihood (ME), and hierarchical models estimated using a fully Bayesian approach (BH). We regressed contraceptive sales on each candidate macroeconomic predictor separately, one at a time. In all cases, we used first differences, that is, the change in the value of each variable with respect to the previous year. For the outcome variable (i.e. contraceptive retail sales) as well as for inflation, we focused on the relative change (rather than the absolute change) to deal with more comparable figures across countries. However, we used the absolute difference in the case of unemployment and poverty rates. All predictors are lagged one period (i.e. they correspond to their value in the previous year) since we are interested in assessing the extent to which changes in the purchase of contraceptives can be anticipated. Using the first difference is a frequent approach to address residual serial correlation, which would otherwise invalidate the OLS estimation. Nevertheless, both the ME and BH models incorporated random intercepts by country and a first-order autoregressive process for the residuals. For Bayesian estimation, the choice of prior distributions for the model parameters favors simpler models over more complex ones when compatible with the data.28 Posterior distributions were estimated using nested Laplace approximation.29 All analysis was implemented with R,30 including the packages survey,31,32 nlme,33 and INLA.29
Results
Estimated mean and the 95% confidence intervals of out-of-pocket spending for contraceptives as well as the proportion of women aged 15–49 using a modern contraceptive who received it free at a public health facility or as part of statutory health insurance are included in Table 1. On average, they spent about US$ 12 per year on out-of-pocket contraceptives, although the distribution appears to be bimodal, which translates into a rather wide confidence interval. As a percentage of the GDP per capita, out-of-pocket spending ranged from .01% in Chile or Colombia, to 0.15% in Uruguay. Almost three out of five women obtained them free of charge. Out-of-pocket spending was at or above the median in Argentina, Brazil, Costa Rica, Panama, and Uruguay. Public provision was well below the median in Argentina, Ecuador, and Honduras.
Table 1. Out-of-pocket spending for contraceptives and public provision of contraceptives.
| Country | Out-of-pocket spending | Proportion of women aged 15–49 using a modern contraceptive who obtained it free of charge | |||
|---|---|---|---|---|---|
| 2011 US$ PPP (95% CI) | % per capita GDP | Survey, Year | % (95% CI) | Survey, Year | |
| Argentina | 12.2 (6.3–18.1) | 0.06 (0.03-0.09) | ENGHo, 2012–2013 | 32.2 (28.7–35.8) | ENSSyR, 2013 |
| Brazil | 12.6 (11.6–13.7) | 0.09 (0.08-0.10) | POF, 2008–2009 | ||
| Chile | 2.9 (2.1–3.7) | 0.01 (0.01-0.02) | EPF, 2017 | 57.8 (47.5–67.5) | ENS, 2017 |
| Colombia | 2.0 (0.3–3.7) | 0.01 (0.00-0.03) | ENPH, 2016–2017 | 56.0 (54.7–57.4) | DHS, 2015 |
| Costa Rica | 17.2 (14.1–20.2) | 0.12 (0.10-0.15) | ENIGH, 2013 | ||
| Ecuador | 34.5 (32.7–36.4) | RHS, 2004 | |||
| El Salvador | 72.6 (71.0–74.2) | RHS, 2008 | |||
| Guatemala | 60.7 (59.2–62.2) | DHS, 2014 | |||
| Honduras | 54.1 (52.7–55.5) | DHS, 2011 | |||
| Mexico | 1.8 (1.1–2.6) | 0.01 (0.01-0.02) | ENGASTO, 2013 | 68.6 (68.0–69.2) | ENADID, 2014 |
| Panama | 16.0 (8.4–23.5) | 0.11 (0.06-0.17) | EIGH, 2007–2008 | ||
| Peru | 1.8 (1.3–2.3) | 0.02 (0.01-0.02) | ENAPREF, 2008–2009 | 62.0 (60.2–63.8) | DHS, 2012 |
| Uruguay | 18.8 (15.7–22.0) | 0.15 (0.12-0.17) | ENGIH, 2005–2006 | ||
| Median | 12.2 (8.4–13.1) | 0.06 (0.03-0.09) | 57.8 (55.1–61.5) | ||
Note: DHS: Demographic and Health Survey; RHS: Reproductive Health Survey; ENGHo: Encuesta Nacional de Gastos de los Hogares; ENSSyR: Encuesta Nacional sobre Salud Sexual y Reproductiva; POF: Pesquisa de Orçamentos Familiares; EPF: Encuesta de Presupuestos Familiares; ENS: Encuesta nacional de salud; ENPH: Encuesta Nacional de Presupuestos de los Hogares; ENIGH: Encuesta Nacional de Ingresos y Gastos de los Hogares; ENGASTO: Encuesta Nacional de Gastos de los Hogares; ENADID: Encuesta Nacional de la Dinámica Demográfica; EIGH: Encuesta de Ingresos y Gastos de los Hogares; ENAPREF: Encuesta Nacional de Presupuesto Familiar; ENGIH: Encuesta Nacional de Gastos e Ingresos de los Hogares.
The results from the regression of retail contraceptive sales on each predictor (i.e. previous year GDP growth rate, inflation, variation in poverty, unemployment rate overall, and female-specific unemployment rate) are summarised in Table 2. The previous year general inflation was not predictive of contraceptive sales. Changes in the GDP growth rate were somewhat more predictive, although 95% confidence interval did not entirely rule out a complete lack of association. Variations in poverty and unemployment rates were the most important predictors of variations in contraceptive sales. A one percentage point increase in the percentage of the population living on less than US$ 3.2 per day (2011 PPP values), or in the percentage unemployed in the labour force, predicted about a two percentage point decrease in contraceptive retail sales growth (measured in CYP per capita) the subsequent year.
Table 2. Contraceptive sales growth regressed on macroeconomic indicators in 12 Latin American countries during 2007–2010.
| Macroeconomic indicator | OLS | ME | BH |
|---|---|---|---|
| Estimate (95% CI) | |||
| GDP growth rate (%) | 0.61 (−0.11–1.32) | 0.43 (−0.29–1.15) | 0.61 (−0.09–1.30) |
| Inflation (%) | −0.05 (−0.51–0.42) | −0.14 (−0.69–0.41) | −0.05 (−0.50–0.40) |
| Poverty variation (pp) | −1.73 (−2.91 to −0.54) | −1.51 (−2.72 to −0.29) | −2.03 (−3.01 to −1.06) |
| Unemployment rate variation (pp) | −2.21 (−4.21 to −0.20) | −1.68 (−3.62–0.26) | −2.35 (−4.35 to −0.35) |
| Female unemployment rate variation (pp) | −1.91 (−3.51 to −0.31) | −1.18 (−2.64–0.28) | −2.10 (−3.74 to −0.47) |
Note: OLS: ordinary least square; ME: mixed effect fitted by restricted maximum likelihood; BH: Bayesian hierarchical model; pp: absolute difference in percentage points; %: relative percentage difference.
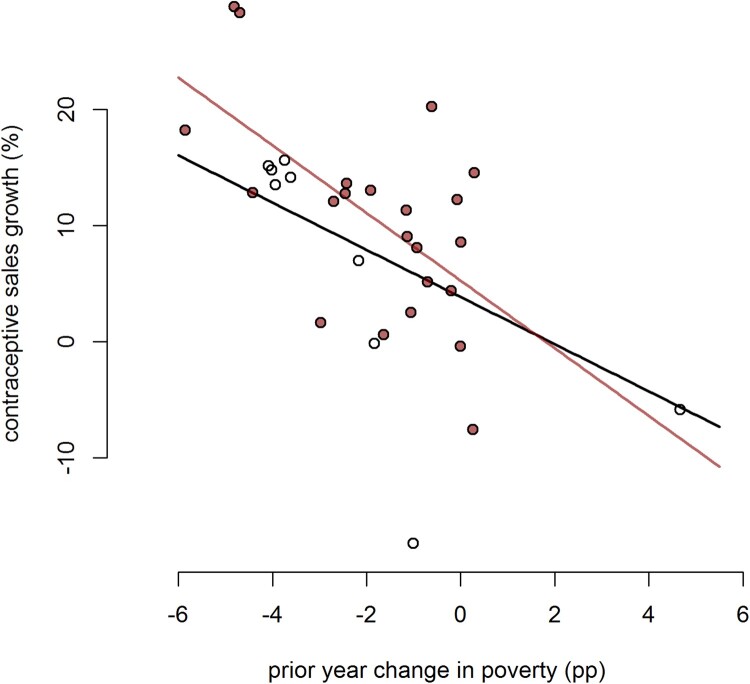
Finally, Table 3 includes the results from the same regression analysis on a subsample of countries, which includes only countries with above-median out-of-pocket spending on contraceptives and/or below-median public provision of contraceptives. The results are somewhat comparable to the result with the overall sample although estimates are less precise, as could be expected given the substantial reduction in sample size. In most cases, confidence intervals (or credible intervals for the Bayesian case) include zero. Only the estimated influences of the changes in poverty are both larger and more precisely estimated in this subsample. Figure 1 represents the regression line estimated using the Bayesian hierarchical model, both for the overall sample and for the countries with above-average out-of-pocket spending.
Table 3. Contraceptive sales growth regressed on macroeconomic indicators in six Latin American countries with above average out-of-pocket spending.
| Macroeconomic indicator | OLS | ME | BH |
|---|---|---|---|
| Estimate (95% CI) | |||
| GDP growth rate (%) | 0.26 (−0.69–1.21) | 0.21 (−0.78–1.20) | 0.26 (−0.63–1.14) |
| Inflation (%) | −0.58 (−1.86–0.69) | −0.84 (−2.15–0.47) | −0.58 (−1.77–0.61) |
| Poverty variation (pp) | −2.91 (−4.72 to −1.11) | −2.95 (−4.77 to −1.13) | −2.91 (−4.59 to −1.24) |
| Unemployment rate variation (pp) | −1.28 (−4.00–1.45) | −1.18 (−3.99–1.62) | −1.28 (−3.81–1.25) |
| Female unemployment rate variation (pp) | −1.29 (−3.14–0.56) | −1.09 (−2.95–0.77) | −1.41 (−3.30–0.47) |
Note: OLS: ordinary least square; ME: mixed-effect fitter by restricted maximum likelihood; BH: Bayesian hierarchical model.
Figure 1.
Estimated regression line of contraceptive sales growth on previous year change in poverty. Note: Entire sample (black line). Countries with above-average out-of-pocket spending (grey line). Circles are country-year observations; circles from countries with above-average out-of-pocket spending are filled. Increases in poverty were associated with subsequent decreases in the growth of contraceptive retail sales, particularly among countries with above-average out-of-pocket spending.
Discussion
We obtained estimates of out-of-pocket spending for contraceptives and the proportion of women receiving contraceptives free of charge at a public health facility or as part of statutory health insurance for several countries in the region based on recent household surveys. Our estimate of out-of-pocket spending is close to recent estimations of private spending per user in 24 low and middle-income Latin American and Caribbean countries by the Reproductive Health Supplies Coalition (RHSC).34 In contrast, Fagan and colleagues3 estimation for seven countries (four of them in our sample), is considerably higher. Their estimation approach, however, is far more indirect than ours, relying on input from key informants at several steps, and, as the author acknowledged, does not capture reimbursement in the private sector. Our estimation of the proportion of women who received contraceptives free of charge is somewhat higher than the one from the RHSC, but consistent with the estimation by Ugaz and colleagues,5 who showed the proportion of users obtaining their method from the public sector has slowly increased since the early nineties. The discrepancy between the sources partly reflects differences in focus and definitions. For example, we assumed that a Colombian woman who received contraceptives at an “EPS health center” received them free of charge as part of the statutory health insurance, a mandate introduced at the end of 2007.35 The discrepancy is also driven by RHSC projection of a rather low level of public provision of contraceptives in Brazil. The latest DHS in Brazil dates back to 1996 and was therefore not included in our study. However, the high estimated out-of-pocket spending we estimated is consistent with low levels of public provision assumed by RHSC.
This analysis also reveals the sensitivity of contraceptive retail sales to changes in macroeconomic variables, particularly changes in poverty levels. The sensitivity is likely due to the heavy reliance on out-of-pocket spending to finance access to contraceptives in the region. Indeed, we found evidence of a stronger sensitivity of sales to poverty in countries with above-average out-of-pocket spending on contraceptives and/or below-average public provision. While not possible to test directly with our data, it is reasonable to hypothesise that the poorest and youngest women among private sector users are the most affected, particularly in a context of high-income inequality.2,4
The findings have important implications, particularly regarding the ability of Latin American countries to reach the SDG of universal access to family planning by 2030, as illustrated using a quick back-of-the-envelope calculation. Based on this sample’s average number of CYPs acquired through retail (7.6 million per year) as well as the average yearly change (7%), the estimated change in sales following a one percentage point increase in poverty translates into 155 thousand less CYPs annually (95% CI 81–230) or, equivalently, 1.8 million women aged 15–49 not being able to access protection during a month (95% CI 1–2.8). This may be partially offset by an increase in the provision by the public sector, assuming the resources to respond to this additional demand are available especially during periods of macroeconomic strain.
An array of measures could be implemented to address this situation. For example, in the US, the Affordable Care Act mandates private health insurance plans to cover prescription contraceptives with no consumer cost sharing, which was recently shown to deliver large reductions in out-of-pocket spending on contraceptives.36 Whether this measure will result in increased uptake of LARCs, or impact fertility rates, has yet to be assessed. Increasing LARCs uptake, for example, may require concurrent interventions, such as information campaigns beyond the removal of financial barriers.6
The results should be interpreted in the context of the limitations of this study. First, while the sample of Latin American countries is broad and diverse, some information was not available for all of them. Specifically, the two largest pharmaceutical markets were not included in the regression analysis because it was not possible to obtain sales information. Therefore, while the regression results are suggestive, their generalisability is not guaranteed. Second, the most recent survey available for out-of-pocket spending estimation was relatively spread over a ten-year span. Using constant dollars only partially improves the comparability of these figures, particularly in a growing market. This situation should improve as many national statistical agencies are scheduled to update their household budget surveys over the next few years. Finally, as previously discussed, while there is considerable harmonisation in the way contraceptive expenditures are collected across countries and overtime, there are still substantial differences. This is also the case of the complementary indicator, acquisition of contraceptives from a public source, which is not currently collected by one of the large international surveys in the field.
Despite the advancement in the region in terms of access to modern contraception, several challenges remain. Financing schemes that heavily rely on out-of-pocket spending can leave family planning at the whim of factors that should not play any role. The achievement of SDG 3.7 will undeniably require improving such schemes.
Acknowledgements
FT, LGG and IRB conceived the idea for the paper and planned the analysis. LGG advised on and conducted the analysis and drafted the paper with input from all authors. All authors approved the final draft. This study did not require ethical approval since it was entirely based on de-identified secondary data.
Funding Statement
This work was partially funded by the United Nations Population Fund (Latin American and the Caribbean Region) (UNFPA-LACRO). The opinions expressed in this article are the authors’ own and do not reflect the view of the UNFPA LACRO.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Country-level data and R code to reproduce the analysis are available from the corresponding author upon reasonable request. Household survey microdata are already accessible from the respective source.
References
- 1.Leon RD, Ewerling F, Serruya SJ, et al. Contraceptive use in Latin America and the Caribbean with a focus on long-acting reversible contraceptives: prevalence and inequalities in 23 countries. Lancet Glob Health. 2019;7:e227–e235. DOI: 10.1016/S2214-109X(18)30481-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caffe S, Plesons M, Camacho AV, et al. Looking back and moving forward: can we accelerate progress on adolescent pregnancy in the Americas? Reprod Health. 2017;14:83. DOI: 10.1186/s12978-017-0345-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fagan T, Dutta A, Rosen J, et al. Family planning in the context of Latin America’s universal health coverage agenda. Glob Health Sci Pract. 2017;5:382–398. DOI: 10.9745/GHSP-D-17-00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Restrepo-Méndez MC, Barros AJD, Requejo J, et al. Progress in reducing inequalities in reproductive, maternal, newborn,’ and child health in Latin America and the Caribbean: an unfinished agenda. Rev Panam Salud Publica Pan Am J Public Health. 2015;38:9–16. [PubMed] [Google Scholar]
- 5.Ugaz JI, Chatterji M, Gribble JN, et al. Regional trends in the use of short-acting and long-acting contraception accessed through the private and public sectors. Int J Gynecol Obstet. 2015;130:E3–E7. DOI: 10.1016/j.ijgo.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Shoupe D. LARC methods: entering a new age of contraception and reproductive health. Contracept Reprod Med. 2016;1:4. s40834-016-0011-8. DOI: 10.1186/s40834-016-0011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dmytraczenko T, Almeida G.. Toward universal health coverage and equity in Latin America and the Caribbean: evidence from selected countries. The World Bank; 2015. DOI: 10.1596/978-1-4648-0454-0. [DOI] [Google Scholar]
- 8.Xu K, Evans DB, Carrin G, et al. Protecting households from catastrophic health spending. Health Aff. 2007;26:972–983. DOI: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization, et al. The world health report: health systems financing: the path to universal coverage. Geneva: World Health Organization; 2010. Available from: https://www.who.int/whr/2010/en/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagstaff A, Flores G, Smitz M-F, et al. Progress on impoverishing health spending in 122 countries: a retrospective observational study. Lancet Glob Health. 2018;6:e180–e192. DOI: 10.1016/S2214-109X(17)30486-2. [DOI] [PubMed] [Google Scholar]
- 11.Rezayatmand R, Pavlova M, Groot W.. The impact of out-of-pocket payments on prevention and health-related lifestyle: a systematic literature review. Eur J Public Health. 2013;23:74–79. DOI: 10.1093/eurpub/cks034. [DOI] [PubMed] [Google Scholar]
- 12.Bahamondes L, Villarroel C, Frías Guzmán N, et al. The use of long-acting reversible contraceptives in Latin America and the Caribbean: current landscape and recommendations. Hum Reprod Open. 2018;2018. DOI: 10.1093/hropen/hox030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mestad R, Secura G, Allsworth JE, et al. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the contraceptive CHOICE project. Contraception. 2011;84:493–498. DOI: 10.1016/j.contraception.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindo JM, Packham A.. How much can expanding access to long-acting reversible contraceptives reduce teen birth rates? Am Econ J Econ Policy. 2017;9:348–376. DOI: 10.1257/pol.20160039. [DOI] [Google Scholar]
- 15.Sahay R, Goyal R.. Volatility and growth in Latin America; an episodic approach. International Monetary Fund; 2006; [cited 2020 Feb 5]. Available from: https://ideas.repec.org/p/imf/imfwpa/06-287.html. [Google Scholar]
- 16.Spinola D. Instability constraints and development traps: an empirical analysis of growth cycles and economic volatility in Latin America. United Nations University – Maastricht Economic and Social Research Institute on Innovation and Technology (MERIT); 2018; [cited 2020 Feb 5]. Available from: https://econpapers.repec.org/paper/unmunumer/2018002.htm. [Google Scholar]
- 17.Cárcamo-Díaz R, Pineda-Salazar R.. Economic growth and real volatility: the case of Latin America and the Caribbean. Santiago: ECLAC; 2014; [cited 2020 Feb 5]. Available from: https://www.cepal.org/fr/node/25632. [Google Scholar]
- 18.Loayza NV, Rancière R, Servén L, et al. Macroeconomic volatility and welfare in developing countries: an introduction. World Bank Econ Rev. 2007;21:343–357. DOI: 10.1093/wber/lhm017. [DOI] [Google Scholar]
- 19.Heijink R, Xu K, Saksena P, et al. Validity and comparability of out-of-pocket health expenditure from household surveys: a review of the literature and current survey instruments. Geneva: World Health Organization; 2011; [cited 2020 Jan 31]. Available from: http://www.who.int/health_financing/documents/cov-dp_e_11_01-oop_errors/en/. [Google Scholar]
- 20.United Nations . Classifications of expenditure according to purpose: classification of the functions of government (COFOG), classification of individual consumption according to purpose (COICOP), classification of the purposes of non-profit institutions serving households (COPNI), classification of the outlays of producers according to purpose (COPP). New York (NY: ): United Nations; 2000. [Google Scholar]
- 21.OECD . A system of health accounts. Paris: OECD Publishing; 2000. DOI: 10.1787/9789264181809-en. [DOI] [Google Scholar]
- 22.World Bank . Purchasing power parities and the real size of world economies: a comprehensive report of the 2011 international comparison program. Washington (DC: ): World Bank Group; 2015. [Google Scholar]
- 23.Murray C, Newby H.. Data resource profile: United Nations Children’s Fund (UNICEF). Int J Epidemiol. 2012;41:1595–1601. DOI: 10.1093/ije/dys185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.U.S. Food & Drug Administration (FDA) . FDA reports quality problems for data provided by the firm IQVIA that were used to inform estimates for some controlled substances. 2018. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-reports-quality-problems-data-provided-firm-iqvia-were-used-inform-estimates-some-controlled.
- 25.Stover J, Bertrand JT, Shelton JD.. Empirically based conversion factors for calculating couple-years of protection. Eval Rev. 2000;24:3–46. DOI: 10.1177/0193841X0002400101. [DOI] [PubMed] [Google Scholar]
- 26.Economic Commission for Latin America and the Caribbean (ECLAC) . CEPALSTAT. Available from: http://interwp.cepal.org/cepalstat/WEB_CEPALSTAT/estadisticasIndicadores.asp?idioma=i.
- 27.World Bank . PovcalNet: the on-line tool for poverty measurement developed by the development research group of the World Bank. Available from: http://iresearch.worldbank.org/PovcalNet/povOnDemand.aspx.
- 28.Simpson D, Rue H, Riebler A, et al. Penalising model component complexity: a principled, practical approach to constructing priors. Stat Sci. 2017;32:1–28. DOI: 10.1214/16-STS576. [DOI] [Google Scholar]
- 29.Rue H, Martino S, Chopin N.. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J R Stat Soc Ser B Stat Methodol. 2009;71:319–392. DOI: 10.1111/j.1467-9868.2008.00700.x. [DOI] [Google Scholar]
- 30.R Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019. Available from: https://www.R-project.org/. [Google Scholar]
- 31.Lumley T. Survey: analysis of complex survey samples. 2019. Available from: https://CRAN.R-project.org/package=survey.
- 32.Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1–19. DOI: 10.18637/jss.v009.i08. [DOI] [Google Scholar]
- 33.Pinheiro J, Bates D, DebRoy S, et al. Nlme: linear and nonlinear mixed effects models. 2019. Available from: https://CRAN.R-project.org/package=nlme.
- 34.Reproductive Health Supplies Coalition , Miller N, Weinberger M, et al. Commodity gap analysis 2018. Key findings for Latin America & Caribbean LMI countries (24) [two-page snapshots]. Brussels: Reproductive Health Supplies Coalition; 2018. Available from: https://www.rhsupplies.org/fileadmin/uploads/rhsc/Projects/Global_Commodity_Gap_Analysis/Snapshots-2018/CGA_Snapshot_LAC.pdf. [Google Scholar]
- 35.Colombia . Consejo Nacional de Seguridad Social en Salud. CNSSS, Colombia. Ministerio de la Protección Social; Colombia. Ministerio de Hacienda y Crédito Público; RID-TAGCLOUD. Acuerdo 0380 de 2007. 2007. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/Acuerdo_380_de_2007.pdf.
- 36.Becker NV, Polsky D.. Women saw large decrease in out-of-pocket spending for contraceptives after ACA mandate removed cost sharing. Health Aff. 2015;34:1204–1211. DOI: 10.1377/hlthaff.2015.0127. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Country-level data and R code to reproduce the analysis are available from the corresponding author upon reasonable request. Household survey microdata are already accessible from the respective source.