Abstract
If universal health coverage (UHC) cannot be achieved without the sexual and reproductive health (SRH) needs of the population being met, what then is the current situation vis-à-vis universal coverage of SRH services, and the extent to which SRH services have been prioritised in national UHC plans and processes? This was the central question that guided this critical review of more than 200 publications between 2010 and 2019. The findings are the following. The Essential Package of Healthcare Services (EPHS) across many countries excludes several critical SRH services (e.g. safe abortion services, reproductive cancers) that are already poorly available. Inadequate international and domestic public funding of SRH services contributes to a sustained burden of out-of-pocket expenditure (OOPE) and inequities in access to SRH services. Policy and legal barriers, restrictive gender norms and gender-based inequalities challenge the delivery and access to quality SRH services. The evidence is mixed as to whether an expanded role and scope of the private sector improves availability and access to services of underserved populations. As momentum gathers towards SRH and UHC, the following actions are necessary and urgent. Advocacy for greater priority for SRH in government EPHS and health budgets aligned with SRH and UHC goals is needed. Implementation of stable and sustained financing mechanisms that would reduce the proportion of SRH-financing from OOPE is a priority. Evidence, moving from descriptive towards explanatory studies which provide insights into the “hows” and “whys” of processes and pathways are essential for guiding policy and programme actions.
Keywords: universal health coverage, sexual and reproductive health, health financing, access, gender
Résumé
S’il n’est pas possible de réaliser une couverture santé universelle (CSU) sans satisfaire les besoins de santé sexuelle et reproductive (SSR) de la population, quelle est donc la situation actuelle vis-à-vis de la couverture universelle des services de SSR et dans quelle mesure les services de SSR ont-ils été priorisés dans les plans et processus nationaux de CSU? Telle était la question centrale qui a guidé cette analyse critique de plus de 200 publications entre 2010 et 2019. Les conclusions sont les suivantes: dans beaucoup de pays, le panier de services de santé essentiels exclut plusieurs services fondamentaux de SSR (par exemple les services d’avortement sûr, les cancers reproductives qui sont déjà peu disponibles. L’insuffisance du financement public national et international des services de SSR contribue à un fardeau persistant de dépenses à la charge des patients et à des inégalités dans l’accès aux services de SSR. Les obstacles politiques et juridiques, les normes sexuelles restrictives et les inégalités fondées sur le genre contrarient la prestation de services de SSR de qualité et l’accès à ceux-ci. Les données ne sont pas concluantes pour déterminer si un élargissement du rôle et de la portée du secteur privé améliore la disponibilité et l’accès aux services des populations sous-desservies. Alors que la dynamique s’accélère autour de la SSR et de la CSU, les mesures suivantes sont nécessaires et urgentes. Un plaidoyer est requis pour qu’une priorité accrue soit accordée à la SSR dans les paniers publics de services essentiels et que les gouvernements alignent leur budget de santé sur les objectifs de la SSR et de la CSU. La mise en œuvre de mécanismes de financement stables et soutenus, qui réduiraient la proportion de financement de la SSR à la charge des patients est prioritaire. Des éléments d’information, en passant d’études descriptives à des études explicatives, qui donnent des indications sur le fonctionnement et la raison d’être des processus et des parcours, sont essentiels pour guider les mesures politiques et programmatiques.
Resumen
Si la cobertura universal de salud (CUS) no puede lograrse sin satisfacer las necesidades de salud sexual y reproductiva (SSR) de la población, ¿entonces cuál es la situación actual con relación a la cobertura universal de los servicios de SSR y la medida en que los servicios de SSR han sido priorizados en los planes y procesos nacionales de CUS? Ésta es la interrogante central que guió esta revisión crítica de más de 200 publicaciones entre los años 2010 y 2019. A continuación, se exponen los hallazgos. El Paquete Esencial de Servicios de Salud (PESS) en muchos países excluye varios servicios críticos de SSR (ej., servicios de aborto seguro, cánceres reproductivos) que ya están escasos. El financiamiento público inadecuado a nivel internacional y nacional de los servicios de SSR contribuye a la continua carga de gastos corrientes y desigualdades en el acceso a los servicios de SSR. Las barreras políticas y legislativas, las normas de género restrictivas y las desigualdades de género obstaculizan la prestación y accesibilidad de los servicios de SSR de calidad. La evidencia es contradictoria en cuanto a si la ampliación del rol y alcance del sector privado mejora la disponibilidad y accesibilidad de los servicios para las poblaciones desatendidas. A medida que la SSR y CUS cobran impulso, las siguientes acciones son necesarias y urgentes. Es imperativo abogar por asignar mayor prioridad a la SSR en el PESS del gobierno y en los presupuestos de salud alineados con los objetivos de SSR y CUS. Se debe priorizar la implementación de mecanismos de financiamiento estable y continuo, que reducirían la proporción de financiamiento de SSR de los gastos corrientes. Las evidencias, que varían desde descriptiva hasta estudios explicativos que facilitan comprender los “cómo” y “por qué” de los procesos y las vías, son esenciales para guiar las acciones relacionadas con políticas y programas.
Background
At the International Conference on Population and Development (ICPD) in Cairo (1994), the global community adopted a Programme of Action, which affirmed that choice and self-determination, gender equality and human rights constitute the keystone of population policies.* Recognising that realising the right to reproductive health for all, without discrimination, is critical to exercising choice, the Programme of Action committed to achieving universal access to sexual and reproductive health (SRH) by 2015. This commitment is far from fulfilled, and the ICPD+25 summit was convened in November 2019 to mobilise the political will and the financial allocations urgently needed to do so. While substantial progress has been made in the reduction of maternal mortality and in meeting the demand for contraceptive services, and in providing antiretroviral therapy for HIV, there has been little attention to diverse health needs of vital importance such as comprehensive sexuality education, gender-based violence, safe abortion services, treatment of sexually transmitted infections and reproductive cancers. As Starrs et al (p.7)1 argue “Ultimately, almost all 4·3 billion people of reproductive age worldwide will have inadequate sexual and reproductive health services over the course of their lives.”
Target 3.7 of the Sustainable Development Goal (SDG) 3 on health reaffirms the ICPD commitment of universal access to SRH, extending the deadline for its achievement to 2030. However, rather than being a stand-alone commitment as in ICPD, universal access to SRH services in SDGs stands alongside Target 3.8, of achieving universal health coverage (UHC). Universal Health Coverage is achieved when “All people obtain the health services they need – prevention, promotion, treatment, rehabilitation, and palliation – without risk of financial ruin or impoverishment, now and in the future”.2
Many advocates for sexual and reproductive health and rights (SRHR) have acknowledged that progress towards universal access to SRH services would not be possible without progress towards UHC.3 Universal access to SRH services calls for a well-functioning health system with adequate human and financial resources, which is responsive to the needs of all sections of the population. This is also what UHC entails. Conversely, UHC can hardly be achieved if the SRH needs of the population are not met. In other words, SRH and UHC are mutually reinforcing. The global commitment to achieving both these SDG targets offers a renewed opportunity to forge new alliances to move the SRH agenda forward.
Despite the crucial role of SRH services for achieving UHC, SRH services have not always been on the agenda when global and national-level discussions and decisions related to UHC are made on financing health care, allocating resources and setting priorities.4–7
This paper draws on a review commissioned by the Department of Sexual and Reproductive Health and Research (World Health Organization) which aimed to explore the literature on universal coverage of SRH services within the context of UHC, to synthesise what is known and to identify the gaps. The paper focuses on lower- and middle-income countries (LMICs) for the following reasons. The first relates to relatively poorer access to and higher unmet need for SRH services in LMICs. As noted by WHO (p.2),8 “Sub-Saharan Africa and Southern Asia accounted for approximately 86% (254,000) of the estimated global maternal deaths in 2017”. Second, well-functioning and well-resourced health services are an important prerequisite for advancing towards UHC. However, many LMICs and especially low-income countries continue to be dependent on external funding to support their health systems. As argued by Starrs et al. (p.16)1 “scarce human and financial resources, and a paucity of political commitment in some cases, have prevented health-care systems in low-income and middle-income countries from offering comprehensive sexual and reproductive health services”.
The paper is structured as follows. Following this introduction, the second section presents the methodology adopted for the review. The third section presents the findings of the review in four sub-sections or major thematic areas. The thematic areas emerged through a combination of a priori themes informed by the research questions (i.e. deductive analysis) and an analysis of the literature (i.e. inductive analysis). The following thematic areas are presented in the findings; (1) inclusion of SRH services in essential packages of health services (EPHS); (2) financing of SRH services; (3) challenges in the implementation of SRH services; and (4) accountability mechanisms. The fourth section summarises the key findings and their implications, while the fifth section highlights gaps in the literature and presents an agenda for future research.
Methods
The main objective of the review was to explore the current situation vis-à-vis universal coverage of SRH services, and the extent to which SRH services have been prioritised in national UHC plans and processes. This main objective translated into a series of research questions on which the literature search was based. The research questions sought to examine the range of SRH services included in the Essential Packages of Health Services (EPHS) and in the Health Benefit Packages (HBPs) of LMICs; how financing arrangements and reforms affected population and service coverage and financial risk protection for SRH services; the key implementation challenges in delivering SRH services; and accountability mechanisms and initiatives for SRH services. The reason for carrying out searches pertaining to multiple research questions was that the literature on SRH and UHC was fragmented across specific components of SRH services, and specific dimensions of UHC such as financing or EPHS.
The complex nature of the review, involving multiple research questions, answering each of which necessitated scanning a vast array of sources to identify and extract relevant information, required us to develop a suitably tailored methodology. We did not find the search processes laid out in standard guidelines such as the PRISMA suitable for our purpose. We describe in some detail below, how the search terms were identified and the search conducted.
We developed a set of search terms corresponding to each research question, combining specific components of SRH services with various aspects of EPHS, financing, implementation challenges and accountability. Appendix Table A1 presents the research questions and the search terms corresponding to each research question explored in this paper. The search was conducted combining each SRH search term with each UHC search term for all questions except the questions related to unique service delivery challenges.
The inclusion criteria for the review were :
Publications in English;
Published during 2010 –2019; This period was selected for two reasons. Firstly, this period includes the adoption of the SDGs and SRHR and UHC as global priorities in 2015. Second, preceding and during this period (i.e. 2010–2019), there has been significant health systems, including UHC-related, reform with implications for SRHR and correspondingly an increase in the evidence base.
Peer-reviewed journal articles, reports, fact sheets, and working papers of multilateral and bilateral agencies, international non-governmental organisations and universities;
Covering one or more sexual and reproductive health services;
Covering one or more of the following dimensions of Universal Health Coverage: EPHS, HBPs, financing, implementation challenges and accountability mechanisms.
The databases searched included PubMed and Scopus, websites of multilateral organisations (WHO, UNFPA, UNOHCHR, UNICEF), The World Bank, bilateral organisations (DFID and USAID), international SRHR non-governmental organisations (NGO)s, and Google Scholar. Original articles cited in systematic reviews and useful articles from articles selected for the review were followed up and included. Although the search was not exhaustive in terms of the databases included, we are fairly certain that a vast majority of relevant articles and publications have been included, based on scanning references cited in systematic reviews and recent articles.
Two researchers scanned the abstracts, selected those that fitted the inclusion criteria and obtained the full texts. Full texts were also scrutinised by two researchers; the first researcher carried out a quick read to verify if the document fulfilled the inclusion criteria. The second researcher carried out a quality check based on the following broad criteria:
Are the aims and objectives of the research clearly stated?
Is the research design clearly specified and appropriate for the aims and objectives of the research?
Do the researchers provide a clear account of the process by which their findings were produced?
Do the researchers display enough data to support their interpretations and conclusions?
Is the method of analysis appropriate and adequately explicated?9
The review included 253 publications. Unlike the case of systematic reviews, where rigorous quality standards are applied so that specific questions may be answered (e.g. “what works”? “what is the incidence of impoverishment … ”?), our purpose was to get a comprehensive overview of what is known. Therefore, we tended to be inclusive and rejected only papers that did not help answer the research questions because of poor quality.
Data was coded and analysed based on thematic analysis. The framework of analysis was based on the research questions. Codes and subsequent sub-themes were generated from the review and analysis of the literature, which were then checked against the framework. Sub-themes were named and refined and these were finally related back to the study objectives.
Findings
Inclusion of SRH services in Essential Packages of Health Services (EPHS) and Health Benefit Packages (HBP)
EPHS and HBPs
One of the biggest challenges when planning for UHC relates to how governments of LMICs with a limited budget would provide priority health care services that will be available to all its people with financial risk protection. Many LMIC governments have sought to do so by developing an “Essential Package of Healthcare Services (EPHS).”
The EPHS† are defined by the countries themselves and represent the range of health services that are to be made available, usually through government health services, to all people, at no cost or minimal cost at the point of receiving the service. In practice, however, not all services mentioned in the EPHS are available in public health facilities, and users have to pay for these in private facilities. This has led to a revised, more pragmatic, definition of EPHS as a policy statement of intent and commitment, which may or may not be supported by adequate financing.
The term Health Benefit Package (HBPs) is used to refer to services that are linked to a financing mechanism such as Social or Voluntary Health Insurance to which enrolees are entitled, or available at no/subsidised charges through government or international donor funding.10 Inclusion of a service in an HBP is a better indicator of its availability with financial risk protection. EPHS documents tend to list broad health care needs, while HBPs have to be more precise about exactly what is covered or not covered by a specific scheme and in some instances, at what level of care.
Inclusion of SRH services in the EPHS of selected LMICs
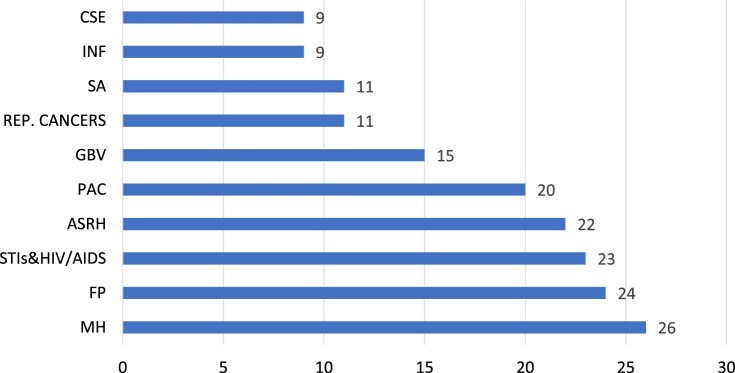
The present review found that EPHS across many countries exclude many SRH services that are already poorly available. An analysis based on 24 LMICs,11–34 ‡ shows that almost all countries included maternal health care including obstetric emergencies, and family planning services (Figure 1). Some SRH services for adolescents are included in 21 countries, mainly family planning and STI/HIV prevention and management. However, over 60% of the EPHS do not even mention services related to safe abortion, infertility, and screening for cervical and breast cancers. Comprehensive sexuality education (CSE) is effectively absent, with weak mentions of SRH awareness, education, and/or counselling. However, it is possible that CSE is not mentioned in the EPHS because it is a part of the education sector's mandate in many countries.
Figure 1.
Inclusion of SRH services in EPHS packages of countries (N = 26)
Source: Wright 11–12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34, Sundewall35
CSE - any education related to sexuality and reproduction for adolescents & young people
INF - counselling, testing and management of infertility
SA - safe abortion
REP CANCERS - screening (and treatment) for cervical / breast cancers
GBV - services related to the prevention and management of sexual and gender-based violence
PAC - post-abortion care
ASRH - adolescent sexual and reproductive health services
STIs & HIV/AIDS - prevention and treatment, including PMTCT and ARV
FP - contraceptive services
MH - maternal health including emergency obstetric care
The mention of a specific SRH service in the EPHS may not be accompanied by all or even the essential minimum services. While the EPHS in 13 of 24 countries included gender-based violence, services for addressing intimate partner violence were specifically included in only three countries. Similarly, of the nine countries that have included reproductive cancers, only two countries include treatment for cervical and breast cancer.11–34
Since inclusion of an SRH service in the EPHS of a country does not guarantee the availability of the service with financial risk protection, it is important to examine whether or not an SRH service is included in the HBP of mandatory and voluntary insurance schemes, in tax-funding by the government, or donor funding. Wright and Holtz found that of 22 countries for which data were available, there was only a 30% alignment between SRH services included in the EPHS of a country and those included in the HBPs of the same countries.10
Two studies are the source of information on the inclusion of SRH services in countries’ HBPs. One is a review of SRH services in the UHC plans of six countries§ of the Asia-Pacific, and the second, a review of the inclusion of family planning in the HBPs of nine Latin American countries.36,37 ¶
Across the six Asia-Pacific countries, maternal health services, including emergency obstetric care, were covered by the insurance schemes and also available in government health facilities without user fees, at least at the primary care level. Diagnostic services and treatment for sexually transmitted infections (STIs) were fully covered in four and three of five countries, respectively. Support for HIV-related services in all countries except Thailand was from pooled external donor support. Coverage for safe abortion services was available only in Thailand, for indications that are legal in the country, and absent in some countries with relatively liberal abortion laws such as Cambodia, India and Vietnam. Contraceptive services were not included in the HBPs of two government insurance schemes, and available to a limited extent in a third.36
Contraceptive services were fully covered in five of the nine LAC countries in all social insurance schemes, covered for all methods except sterilisation in one, covered but largely unavailable in one and not covered in two countries. In contrast, private insurance schemes covered contraceptive services only in two countries: Chile and Colombia, and in both instances, co- payment was involved.37
Actors and processes for evolving an EPHS
An ideal EPHS should be developed through transparent and deliberative processes, in consultation with all the stakeholders, and especially the users, or civil society organisations representing users, including those from vulnerable groups.38 From the available evidence, the actors involved in developing EPHS included (in all but five of 16 countries for which we had the information) appear to be limited to government, international donors, and national and international technical experts. There appears to be less involvement of communities and civil society organisations (CSOs); they participated in the EPHS process of five (of 16) countries. Not much is known about how they influenced the process.35,39
One study provided some information on the priority-setting processes for developing the EPHS in Ghana. The study found a disconnect between SRH actors in the Ministry of Health, and the priority-setting processes for EPHS. SRH actors from the government were not invited nor sought to be involved in the EPHS process, perhaps because SRH services were mainly funded by international donors. Priority-setting was carried out based on disease-ranking by DALYs, which resulted in the inclusion of a narrow range of SRH services related to HIV, maternal health and contraception, leaving out a majority of SRH services defined in the ICPD Programme of Action.40
There is both a need, and scope for civil-society participation in country processes for development of EPHS and HBPs. Such participation should include the representation of the voices of the most marginalised groups (see Box 1).
Box 1: Advocacy for the inclusion of SRH services in a National Insurance Services package.
In Zambia, the Centre for Reproductive Health and Education (CRHE), a national NGO, was supported by Population Action International (PAI) to engage with the UHC processes in the country and to advocate for prioritising SRH services. Zambia's National Health Insurance Scheme (NHIS) has been implemented as part of progressing towards UHC, but civil society organisations (CSOs) working on SRH issues were not part of any of the consultative processes.
CRHE convened engagement which brought together government, NGOs, and medical associations to advocate for the inclusion of all existing SRH services in the NHIS benefits package. They were also able to convince the authorities to include CSO representatives in the National Health Insurance Authority’s board. As a consequence, there are now CSO representatives in various technical committees and working groups related to NHIS. They have been giving regular feedback to the authorities on the non-availability of guaranteed SRH services in specific settings and continue to be engaged in advocacy for strengthening SRH services for workers in the informal sector; and inclusion of contraceptive services and adolescent SRH education in the NHIS benefits package.
Source: Population Action International.41
The review did not find information on the criteria for inclusion of services in EPHS. A paper from Thailand, which has comprehensive coverage of SRH services in its Universal Health Coverage Scheme, proposes a decision-making framework for prioritising SRH services to be included in an EPHS, bearing in mind the budgetary implications and availability of resources. The framework examines SRH service needs, demand and supply, and proposes making a start with SRH services that are needed, demanded and available.42 ** This framework may be a starting point that could be suitably adapted to be used as a part of deliberative processes involving a wide range of stakeholders.
Financing SRH services
To progress towards UHC and ensure both equitable access to health services, financial protection and overall sustainability, health services should be funded through predominantly domestic public funding which combines taxes and prepayment mechanisms.43 As described below, particularly in low-income countries, domestic public funding of SRH services remains a challenge, contributing to inequities in financing and access to SRH services.
Overall patterns of SRH financing
Most countries rely on a mix of different sources of revenue to finance the health system. Sources of revenue include government taxes; external funding by bilateral and multilateral donors and private foundations; mandatory social insurance schemes, which raise revenue from payroll deductions of employees and contributions from employers; voluntary insurance schemes; and payment by households at the point of seeking care, known as out-of-pocket expenditure (OOPE).
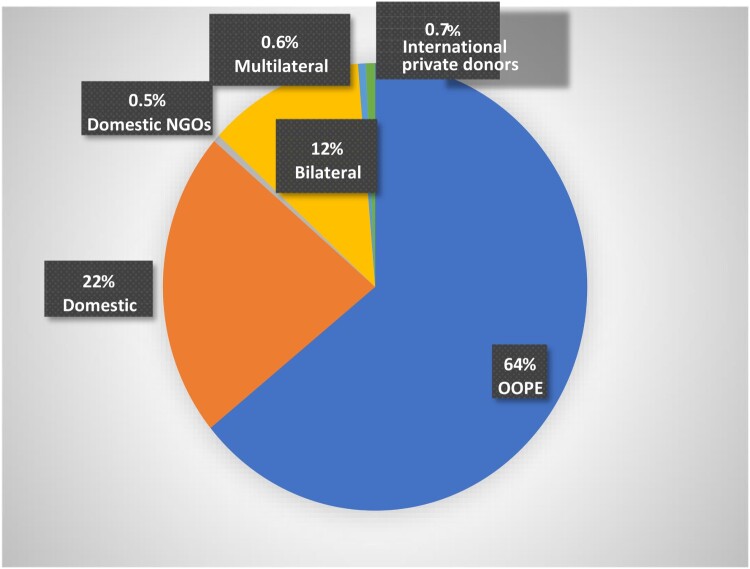
Information on aggregate patterns of SRH financing is available for a limited range of SRH services, known as the “costed package”†† of ICPD services. In 2012, almost two-thirds of all expenditure on SRH services in developing countries was from out-of-pocket expenditure by households.44,45 Government spending accounted for about 22%. International public funding from bilateral and multilateral sources was around 13.5%. This aggregate picture holds in general, except in some countries which are heavily dependent on donors (Figure 2).
Figure 2.
Financing of the ICPD costed package, 2012. Source: Drawn based on data from IPPF.20
In terms of national patterns of funding, information from nine countries on financing reproductive‡‡ health services showed considerable inter-country variations.47–50 OOPE was the largest source of RH financing (as seen in the overall pattern for developing countries) in three countries (Kenya, 38%; Uganda, 48% (2006); Burundi, 43% (2007)). International public funding contributed most to SRH financing in three countries in 2006 (Ethiopia, about 45%; Malawi, 57%; Rwanda; 80%). Government funding was the main source of RH financing in Mexico (44.3% in 2012), the Indian states of Bihar (59%) and Karnataka (76%) in 2010–2011 and in Tanzania (45% in 2006). Social and private insurance schemes contributed to less than 5% of RH financing in 2006 in six sub-Saharan African countries,47 while in Mexico, social security funds from social insurance schemes for formal sector employees accounted for 37% of RH financing in 2012.50 The unit cost of providing modern contraception and meeting unmet need for family planning in developing countries was estimated to be US$16 in 2003, and yet most study countries spent less than US$16 for all RH services and commodities, with Ethiopia’s spending as low as US$4.47
Out of pocket expenditure
From the perspective of UHC, OOPE is the least desirable mode of financing. It makes access to healthcare contingent on ability to pay at the time of illness and acts contrary to the UHC objective of “financial risk protection”. OOPE is inequitable since households and individuals without significant disposable income and savings might not be able to afford health services even when there is need.51 For reasons of gender and claims over household resources and spending decisions, OOPE typically limits women's access to health care. According to WHO (p.23),43 “[w]omen incur more out-of-pocket payments than men … paying for delivery care and other reproductive health services places a higher financial burden on women … [and] out-of-pocket expenditure may prevent more women than men from utilizing essential services”. To move towards UHC, countries have to reduce the proportion of OOPE in total health spending, moving towards pre-payment mechanisms such as tax-funding and Social Health Insurance.
A large number of studies show that high OOPE for obstetric emergencies and complications of unsafe abortion, when safe abortion services are not available, results in catastrophic health expenditures.52–59 Even where there is fee waiver, non-medical expenditure, informal payments and expenditure on drugs, consumables and diagnostics result in high OOPE.60–73 The incidence of catastrophic health expenditure is found to be much higher among the poorest sections of the population,60,61,64,65,69 contributing to widening inequities in health. However, there is very limited evidence on the OOPE and catastrophic health expenditure relating to SRH. One of the studies that have tracked this expenditure over time is from India, focusing on free maternal health care (see Box 2).65
Box 2: Tracking out-of-pocket expenditure and catastrophic health expenditure relating to free maternal health care in India.
The study compares OOPE and catastrophic health expenditure (CHE) for 2004 and 2014 using data from the National Sample Surveys. In 2011, the government of India introduced the Janani Shishu Suraksha Karyakram (JSSK), which provides free pregnancy, delivery, and post-partum and neonatal care, including emergency obstetric care and caesarean-sections and emergency neonatal care. The programme also covers transportation and food costs. This was in addition to a conditional cash transfer programme for institutional deliveries, the Janani Suraksha Yojana. The study found significant increases in the utilisation of maternal health care and steep declines in the incidence of CHE. Utilisation of antenatal care, institutional delivery and post-natal care increased from 75.4% to 90.4%; 43.3% to 82.6% and 64.4% to 79.3% respectively. The incidence of catastrophic health expenditure declined from 56.2% to 29.4% for households where the women had exclusively used public health facilities for all ANC, institutional delivery, and PNC. The incidence of CHE declined for all income quintiles except the poorest; however, there was a significant gap in the incidence between the poorest and richest households. While 74.6% of the poorest households using maternal health services from public health facilities experienced catastrophic health expenditure in 2014, only 0.4% of the richest households did. The comparable figures for households using private maternal health care were 95.8% and 20.7%, respectively.
Source: Mohanty and Kastor.65
International funding
International public funding has been an important source of SRH financing especially in low- and lower-middle income countries. USAID accounts for the major share of SRH funding, and in 2012, contributed to 57% of the total development assistance towards the ICPD costed package.74 Dependence on USAID funds has resulted in much volatility in funding received for SRH services. This is because during every Republican Presidency since the mid-1980s, funding from USAID is subject to the condition that the recipient will not carry out any activities related to the provision of safe abortion services.75
Further, while the overall funding for the ICPD “costed package” increased, most of the funding was for HIV/AIDS. Between 1994 and 2014, international public funding for the ICPD costed package increased from US$0.6 to US$7.0 per woman of reproductive age living in developing countries. However, 65% of the funding was for HIV/AIDS and STIs (2012). The share of family planning services was only 9% and had fallen steadily as a proportion of international funding between 1994 and 2012.74 Moreover, international SRH funding to individual countries could fluctuate wildly. For example, Kenya received US$15.9 million as international contribution for SRH services in 2005, which fell to US$0.5 million in 2007 and rose again to US$14.5 million in 2010.76
To address the funding gap, global initiatives such as the Global Financing Facility (GFF) support national ministries of health to identify and scale-up high impact, cost-effective interventions that can be sustainably funded through a combination of increased domestic and international funding.77,78 Although blended financing, and specifically GFF, has enabled the inclusion and prioritisation of SRH services, several concerns have been raised. These include the focus on maternal health and family planning services and the exclusion of other critical (e.g. safe abortion, sexual and gender-based violence) services.79 In addition, in the absence of viable domestic public funding, the focus on domestic financing can shift the burden of financing SRH services and products to OOPE by the poorest and most vulnerable groups.45,80
Government funding
Government funding is the second-most important source of SRH financing in many LMICs. Because of the limited number of countries with RH sub-accounts, information on government-funding for SRH services is scarce. Available evidence from nine countries suggests that the proportion of government funding for SRH can fluctuate from year to year, even when the overall health budget increases. For example, government contribution to SRH financing increased in three countries: in Burundi, from 15% in 2010 to 19% in 2012;48 in Kenya, from 34% in 2005–2006, to 40% in 2009–201076 and in Mexico, from 11.4% in 2003 to 44.3% in 2012.50 It decreased in Rwanda, Tanzania, and Malawi during 2002–2006.47
A study from Mexico shows that increased spending and allocation favouring households without social security resulted in greater financial risk protection, especially to poorer households.50 During 2003–2012, there was a three-fold increase in government expenditure on health and a steep decrease in OOPE as a proportion of total expenditure (from 51.5% in 2003 to 16.3% in 2012). This was the period immediately following the introduction of health reforms to enrol pregnant women without social security coverage in a social health protection scheme (Seguro Popular or SP), which entitled them to free services at the point of care. OOP spending on childbirth and complications reduced by over 80% for households without social security. Comparable figures for antenatal care and family planning were 61% and 64%, respectively. OOPE for all these services also decreased for households with social security, but the reductions were modest when compared to households without social security.
Health insurance
Health insurance is a pre-payment mechanism that allows for pooling revenue across people at high and low risk of having a healthcare need. Mandatory insurance schemes such as the deduction of a fixed proportion of the salary also allow for cross-subsidising across income groups. The intention is to enable access to health care irrespective of the ability to pay at the time when a healthcare need arises, with financial risk protection. There are very few studies directly addressing the issue of SRH services in public, private, and community-based insurance schemes, and this represents a major evidence gap.
Studies from HIC show that many SRH services (e.g. contraception and abortion services) may be excluded from private insurance plans.81 Another study observed that the exclusion of safe abortion services from Medicaid following the Hyde Amendment in 1977 has resulted in delays in seeking abortion services, catastrophic health expenditures, and impoverishment, or unintended pregnancies carried to term.82 However, there are few studies on the coverage of SRH services by public and private insurance schemes in LMICs.
The design of insurance schemes and the process of enrolling beneficiaries may give rise to inequities in access to insurance coverage. Moreover, the exclusion of many SRH services including those that women need to protect their health and wellbeing is discriminatory. A study of Rwanda’s Mutual Health Insurance scheme found that female-headed households across all income quintiles were two-thirds less likely to have Mutual Health Insurance.83 Experience with voluntary private insurance in South Africa revealed intersectional inequalities based on gender and other axes of vulnerability. The heads of partially insured households§§ were more likely to be female, unmarried, with primary-school education or no education, unemployed, and Black.84 Encouragingly, however, studies from Ghana on its National Health Insurance Scheme, which covers all sections of the population, report a higher female than male enrolment.85,86 The higher enrolment may be the result of a waiver of premiums for pregnant women and the indigent, a majority of whom were women.87 Providing premium exemptions may be the route to ensuring the enrolment in insurance schemes of groups without access to cash incomes.88 However, the extent to which premium-exemptions would result in increased utilisation may depend on whether affordability is a major barrier to accessing the specific SRH service under consideration.89
Demand-side financing mechanisms
Many LMICs have introduced demand-side financing (DSF) mechanisms to remove financial barriers to accessing health care services and to reduce OOPE. The objective is to increase the use of essential health services by the poor and under-serviced groups. The services usually covered by DSF are those with significant externalities such as family planning, maternal healthcare, and immunisations.90 Some examples of DSF mechanisms include conditional cash transfers (CCTs), voucher schemes and publicly funded health insurance schemes (PFHIS) for the poor and indigent. An implicit assumption underlying DSF mechanisms is that financial barriers, including transportation and food costs, are the most important reason for underutilisation of services.90 While many of the DSF mechanisms have improved overall access to services, the benefits of these mechanisms often elude the poorest and the most vulnerable populations.
Evidence suggests that voucher schemes improved access to maternal health services and FP and also reduced OOPE.91–94 Conditional cash transfers have been found to increase utilisation of maternal and neonatal health services,95–97 but not family planning services.98 Studies have found that CCTs may fail to benefit the most marginalised or provide financial risk protection for all.99–101 and their impact on improving health outcomes has been mixed.95,96,98 PFHIS for the poor seem to experience gender-based barriers to enrolment, similar to other insurance schemes.102–104 Further, design elements such as limiting enrolment to five members of a household, and a fixed financial coverage which is allocated by the households to its members, may result in the exclusion of the less powerful household members such as women and the elderly from enrolment or use of insurance benefits.105
Implementation of SRH services
The review examined the literature on service-delivery challenges unique to (or predominantly affecting) SRH services (i.e. policy and legal barriers and restrictive gender norms and gender-based inequalities) and the role of the private sector as an implementer.
Legal and policy barriers
Legal and policy barriers that deter access to SRH services affect a significant proportion of the world’s population. The requirement of parental or spousal consent poses a barrier to contraceptive services in about 5–10% of the world's countries,106 and two-thirds of the women live in countries where there are one or more restrictions as to the reasons for seeking safe abortions.107 The other side of the coin to forfeited use is coerced or involuntary use, prevalent in the case of sterilisations for vulnerable population groups such as persons living with disabilities,108 which erode users’ trust in the health system and can affect SRH service utilisation as a whole. The criminalisation of same-sex sexual conduct and sex-work109,110 and barriers to legal gender recognition for transgender people enhance the exposure to health risks of these groups.111 They also result in leaving vulnerable populations out of the realm of accessible and affordable SRH care.
Restrictive gender norms
Restrictive gender norms influence behaviours related to sexuality and reproduction, and alongside gender-based inequalities in access to resources and decision-making, they often erect barriers to the use of health services by women,112–114 men115,116 and transgender persons.117–120
An important dimension of gender norms and inequalities is gender-biased attitudes and practices in the health system, which remain important barriers to effective and timely use of SRH services. Some of these practices include requiring spousal consent for providing contraceptive and abortion services121 and denial of services to adolescents and to young unmarried persons (even in the absence of legal restrictions). Among adolescents and young unmarried women and men, lack of privacy and confidentiality; provider attitudes disapproving of sexual activity; and provider-disclosure to parents were major deterrents to access to SRH services.122,123 LGBTQ persons frequently experienced discriminatory hostile behaviour and “micro-aggression” from health providers and were at times treated as mentally unstable because of their “deviant” behaviour.124–126 Disrespect and abuse of women seeking delivery or abortion services is an extreme manifestation of gender-biased attitudes and impacts negatively on the use of institutional delivery and safe abortion services.127–130
Challenges of private sector engagement
Practically all LMICs have mixed health systems, with the public-private mix varying in nature and extent, both in financing and in service delivery. One of the critical challenges for countries is to identify and ensure an appropriate role for the private sector that aligns with and does not detract from the country's UHC goals.
In the case of SRH service delivery, the private sector accounts for a large share in many LMICs.131,132 Since the late 1990s, many international donors and the International Finance Corporation (IFC) of the World Bank, and more recently, the GFF, have made deliberate and concerted efforts to engage the private health sector in SRH service provision.77,133
The most common modes of private sector engagement found in the literature are (1) contracting with private sector SRH service providers, (2) social franchising networks, (3) social marketing programmes and (4) voucher schemes. All four are aimed at expanding availability and access to essential health care for underserved populations by expanding the pool of providers and service delivery points. Voucher schemes are primarily intended to provide financial risk protection (discussed earlier in the paper). To what extent do these modalities of engagement with the private sector expand coverage and utilisation especially for the underserved populations, offer good quality services with financial risk protection?
Systematic reviews of the outcomes of various modes of private sector engagement for the provision of SRH services highlight that the quality of the evidence is weak and that only tentative conclusions may be drawn based on the evidence. We may surmise from the descriptions of these four modalities that, with the exception of social marketing, none of these modalities may increase the population or service coverage, because they often provide a narrow range of SRH services such as maternal health and family planning, through existing service delivery points. Of the four, social marketing schemes are found to increase access to knowledge, services and products,134,135 while voucher schemes increase utilisation as well as decrease OOPE.91–94 The evidence on increased utilisation through social franchising and contracting with private providers is mixed.136–147 Studies also suggest that the design of social marketing, social franchising, and contracting with the private sector may not be appropriate to reach the most marginalised groups.136,146–150 However, voucher schemes that were designed to serve specific under-served populations (e.g. adolescents, sex workers, persons living in post-conflict situations) succeeded in doing so.151,152 We do not know enough about the quality of care provided through the different modalities of private-sector engagement. An issue of major concern is the increasing investments by governments and especially international donors in these modalities of engaging the private sector in the absence of robust evidence about their contribution to UHC goals.153
The most immediate priority appears to be more robust research which takes a whole-of-health-system view and examines the nature of and interaction between the public and private sectors within the health system as a whole, which influence private sector performance and the sector's alignment with UHC goals.154
Accountability mechanisms towards universal coverage of SRH services
For more than two decades, the SRHR community globally has witnessed slow progress and uncertain gains in achieving the ICPD goals. The SDGs offer a new window of opportunity to move forward, and effective accountability mechanisms to monitor progress are an important means to achieving universal coverage of SRH services. Studies show that there are several accountability mechanisms for SRH services at the international, national, and sub-national levels.
At the international level, human rights treaty bodies and the Human Rights Council¶¶ have played an important role in holding governments accountable for improving SRH services including maternal health, abortion and family planning, through recommendations to States on periodic reports by State Parties, and on individual complaints received by the treaty bodies.155 Recommendations on SRHR by the Human Rights Council (HRC) based on Universal Periodic Reviews of adherence by State Parties to human rights standards have been implemented by many countries, making the Universal Periodic Review a useful accountability tool.38
Many voluntary networks of international entities (e.g. Countdown 2015 and FP 2020) have been tracking resource flows for Reproductive, Maternal, Newborn, Child and Adolescent Health and Nutrition (RMNCHA-N), or specific areas such as maternal health, family planning, and STIs/HIV.156 More recently, government commitments to improving RMNCHA-N are being monitored on the basis of a framework to monitor-review-act proposed by the Commission on Information and Accountability (CoIA) for Women’s and Children’s Health.
At the national and sub-national level, there are examples of initiatives for examining performance accountability,157,158 social accountability156,159,159–160 as well as legal accountability.161–162 *** Most of the studies reviewed were descriptive, and only some provided information on the outcomes. In general, the studies did not analyse reasons for success or lack of it.
Overall, performance accountability initiatives enabled health system action at the district level to improve performance,157,158 and social accountability initiatives showed an increase in service utilisation and greater user-satisfaction with services.163–164,165 Legal accountability mechanisms in India used for seeking individual redress, were able to bring about policy changes setting quality standards for government’s maternal health and family planning services.161,162 Some social accountability initiatives have also improved the capabilities of women from marginalised populations to demand accountability, an outcome with potentially more long-term impact than immediate gains in quality and availability of services.159,160
An important learning is that accountability mechanisms and initiatives are context-specific and dependent on the democratic space available, the relationship between the state and civil society actors, the extent to which health systems are responsive to the concerns of service-users and the extent to which gender and SRHR are prioritised both in state policies and in civil society activism.166 Therefore, “best practices” cannot be transferred from one setting to another without suitable adaptation.
Despite the vast potential of SRHR accountability mechanisms, the picture that emerges is one of uncoordinated actions by multiple actors with a diversity of interests and capabilities. There is no information on any efforts at coordination and building synergies across international and national accountability initiatives, across civil society and government initiatives, and even among social accountability initiatives by civil society actors.162
From the perspective of accountability for universal coverage of SRH services and SRHR at the country level, a starting point would be to know more about the contexts in which accountability mechanisms and initiatives operate and factors influencing their effectiveness and to explore ways in which synergies may be built for effective enforcement of accountability for universal coverage of SRH services.
Conclusions and the way forward
The review raises many concerns related to the current pattern of financing SRH services, which are detrimental to UHC goals. These include the low per capita spending on SRH services and the high levels of OOPE and catastrophic health expenditure in the financing of SRH services. Implementing financing mechanisms that would reduce the proportion of SRH-financing from OOPE is an urgent priority. Increased international and domestic public funding for a comprehensive range of SRH services is needed. Such funding has to be stable and sustained over a period of time. Advocacy for greater priority for SRH services in government health budgets is needed, including but not limited to maternal health and family planning.
There is both a need, and scope for civil-society participation in country processes for development of EPHS and HBPs. Such participation should include the representation of the voices of the most marginalised groups.
From the perspective of advancing universal coverage of SRH services, we do not know enough about the potential of engagement with the private health sector. We need to understand the effect of private sector engagement in SRH service provision on the health system as a whole, and its overall contribution to population and service coverage, and financial risk protection. From what we know thus far, dependence on the private for-profit sector for the delivery of SRH services would pose financial barriers to those from marginalised sections. Also, services that are not profitable to provide, such as safe abortion services, may not be available from the private for-profit sector, jeopardising the comprehensiveness of SRH services. It may be prudent to wait until robust evidence is available, before making further investments on specific modalities of engagement with private sector providers.
Beyond technical tasks such as mobilising resources and setting priorities, addressing policy and legal barriers to SRH, and gender biases and issues of stigma and discrimination within SRH service provision should also be on the agenda of action towards universal coverage of SRH services. Effective enforcement of accountability for SRHR calls for better coordination and innovative strategising among like-minded actors across all levels. Women’s movements and CSOs in many LMICs have engaged in such work and are allies in this project.
Gaps in evidence and directions for future research
This review indicates significant gaps in the evidence on SRH services in UHC, despite a relatively large number of publications. There is a clustering of studies around specific themes (i.e. maternal health and family planning), while many areas (i.e. access to safe abortion services, adolescent SRH, STI, and breast and cervical cancer) remain poorly explored and understood. Of all dimensions of UHC, there is relatively more evidence including systematic reviews on financing SRH services and specifically financing arrangements for maternal health and family planning and on OOPE and (to a smaller extent) catastrophic health expenditure, while little is known about other financing mechanisms and their impact on access to SRH services.
Given the increasing prominence of the private sector in SRH services, robust studies which assess the scope of various modalities of engagement with the private sector and their impact on population and service coverage and financial risk protection for the population as a whole are urgently required.
There is a need for more rigorous studies of the outcomes of specific financing (e.g. Global Financing Facility) and service provision initiatives, and effective accountability initiatives. Many studies are based on a cross-sectional design that precludes attribution of causality or is before-and-after studies without a comparison group.
There is an urgent need to go beyond descriptive and exploratory studies. Explanatory research - which provide insights into the “hows” and “whys” of the contextual factors (i.e. political, economic and social context) and the processes and pathways that helped, or have the potential to help, a country advance towards UHC and universal access to SRH services – are required to aid policy and programme planning and implementation.
To conclude, only a small proportion of the vast technical literature on UHC has any reference to SRH, or to engaging with and examining the concepts of gender, rights and discrimination. There is a separate body of literature from the SRH world, on the importance of prioritising SRH in national UHC plans, but only a small proportion of these throw light on the extent to which LMICs have realised the prioritisation of SRH services in UHC or describe country experiences of doing so. This requires engagement within the SRH literature with concepts central to UHC such as progressive realisation167 and progressive universalism,168 and moving away from fragmenting SRH into silos (e.g. family planning, gender-based violence, maternal health care, etc.) towards comprehensive SRH which considers the unique SRH service needs of girls and women across the over the life course.169 There is a lengthy and unaddressed research agenda that demands urgent attention.
Appendix.
Table A1. Research questions and search-terms.
| Research questions | Search terms related to SRH components | Search terms related to UHC dimensions |
| 1. What are the key themes addressed by the SRH literature on UHC? | Sexual and reproductive health services Sexual and reproductive health Sexual and reproductive health and rights |
Universal Health Coverage |
| 2. Which SRH services have been included in EPHS of different LMICs? What were the processes through which they were included? |
|
Essential package of health services; essential services packages; basic services packages; Health benefit packages Priority-setting |
| 3. What are the major sources of financing for SRH services? How does this pattern of financing affect population and service coverage and financial risk protection? |
Same as above | Financing mechanisms National Health Accounts; SRH sub-accounts; User fees; Social Health Insurance; national health insurance; community-based health insurance; micro-insurance; Conditional cash transfers; Out of pocket expenditure; Catastrophic health expenditure |
| Research questions | Search terms related to SRH components | Search terms related to UHC dimensions |
| 5. What has been researched on some service delivery challenges unique to/ predominantly affecting SRH services such as restrictive gender norms and gender inequality? Restrictive legal and policy environment? Private sector as a major service provider? | Gender norms; gender inequality; abortion laws; LGBTQI and legal status / criminalisation; disrespect/abuse and maternity; obstetric violence; coercive/ forced sterilisation; third-party authorisation; adolescents; stigma; discrimination; Contracting with private providers; Social marketing; Social franchising; Voucher schemes (for each of the SRH components presented above) |
|
| 4. What are the accountability mechanisms that have been used w.r.t. to universal access to SRH services at the international, national, and sub-national levels? What were the issues addressed? Who were the actors involved, and what were the processes? What were the outcomes? |
Same as above | Accountability Performance accountabilitySocial accountabilityLegal accountability |
Footnotes
Principle 1 and Principle 4, respectively, of the ICPD Programme of Action, uphold human rights and gender equality and equity and women’s empowerment. UNFPA (1995). International Conference on Population and Development – ICPD. Programme of Action. A/CONF.171/13/Rev.1. http://www.unfpa.org/public/home/publications/pid/1973
EPHS also referred to as core, on minimum or basic packages, may also be represented by standards of care to be provided at different levels of the health system. A country may have more than one EPHS, corresponding to different vertical health programmes.
For this paper, we examined 24 case studies of the inclusion of SRH services in EPHS, authored by Wright 2015. Each of the case study documents provided the policy document on EPHS as Annex A. We mapped the SRH services mentioned for each country against the ICPD Programme of Action package of SRH services (UN 2004). To this, we added any additional countries and information in Sundewall.35 There was an overlap of four countries between the two studies, and Eswatini and S. Africa were the additional countries added on. The countries referred to in figure 11 are for 26 countries: Afghanistan, Bangladesh, DR Congo, Eswatini, Ethiopia, Ghana, Haiti, India, Indonesia, Kenya, Liberia, Madagascar, Malawi, Mali, Mozambique, Nepal, Nigeria, Rwanda, Senegal, South Africa, South Sudan, Tanzania, Uganda, Yemen and Zambia. We have counted even a mention of a particular area of service as "included" in the EPHS.
Countries included Bangladesh, Cambodia, Indonesia, Mongolia, Thailand and Vietnam.
Countries included Chile, Colombia, Costa Rica, Dominican Republic, Guatemala, Haiti, Honduras, Jamaica, and Peru.
“Need” is defined on the basis of DALYs lost for major SRH conditions, and arranged in order of DALYs lost, from the highest to the lowest. “Demand” was what people asked for and assessed on the basis of SRH service utilisation data from private health facilities. Supply was defined as the range of services included in Thailand’s HBP for the Universal Health Care (UHC) programme.
The ICPD “costed package” included only a limited number of SRH services based on data availability. The package did not include all interventions or all costs necessary to achieve the ICPD goal of universal access to SRH services. For example, adolescent sexual and reproductive health services; screening and management of reproductive cancers; infertility treatment, and even obstetric emergencies are not a part of the costed package.46
Data pertain to reproductive health services and not sexual and reproductive health services.
Partially insured households were those with only some members of the household covered under the insurance scheme.
Some human rights treaty bodies related to SRHR include the Commission on the Elimination of All Forms of Discrimination Against Women (CEDAW), Child Rights Committee (CRC) and the Committee Against Torture and Ill-treatment (CAT). The Human Rights Council (HRC) is concerned with all human rights concerns, including those related to SRHR.
Performance accountability refers to a government holding the health sector answerable for delivering quality care, through measures such as quality assurance, death reviews, surveillance systems, staff performance review, and disciplinary measures. In social accountability, citizens/communities hold the service providers and the government to account. Community monitoring and scorecards, public-hearings, citizen monitoring of health facilities, and budget-tracking are some examples. Legal accountability is about holding governments accountable for violations of human rights or for not upholding the constitutional rights of citizens. Strategic litigation is one of the commonly used interventions to enforce legal accountability.
References
- 1.Starrs AM, Ezeh AC, Barker G, et al. . Accelerate progress – sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. Lancet. 2018;391:2642–2692. Available from: https://www.thelancet.com/commissions/sexual-and-reproductive-health-and-rights. [DOI] [PubMed] [Google Scholar]
- 2.The World Health Report . Research for universal health coverage. Geneva: World Health Organization; 2013. [Google Scholar]
- 3.Repoliticising sexual and reproductive health and rights. In: Report of a global meeting, Langkawi,3-6 August 2010. London, Reproductive Health Matters and Asian-Pacific Resource& Research Centre for Women (ARROW) , 2011.
- 4.Kowalski S. Universal health coverage may not be enough to ensure universal access to sexual and reproductive health beyond 2014. Glob Public Health. 2015;9:661–668. [DOI] [PubMed] [Google Scholar]
- 5.Sen G, Govender V, El-Gamal S.. Universal health coverage, gender equality and social protection: A health systems approach. New York (NY) UN Women; 2018. [Google Scholar]
- 6.Fried ST, Khurshid A, Tarlton D, et al. . Universal health coverage: necessary but not sufficient. Reprod Health Matters. 2013;21:50–60. [DOI] [PubMed] [Google Scholar]
- 7.Adewole I, Gavira A.. Sexual and reproductive health and rights for all: an urgent need to change the narrative. Lancet. 2018;391:2585–2587. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, world bank group and the united nations population division: executive summary. World Health Organization; 2019. [Google Scholar]
- 9.Dixon-Woods M, Cavers D, Agarwal S, et al. . Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35. [cited 2019 May 24]. Available from: https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright J, Holtz J.. Essential package of health services in 24 countries: findings from a cross-country analysis. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2017. [Google Scholar]
- 11.Wright J. Essential package of health services country snapshot: Afghanistan. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 12.Wright J. Essential package of health services country snapshot: Bangladesh. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 13.Wright J. Essential package of health services country snapshot: The democratic republic of the Congo. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 14.Wright J. Essential package of health services country snapshot: Ethiopia. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 15.Wright J. Essential package of health services country snapshot: Ghana. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 16.Wright J. Essential package of health services country snapshot: Haiti. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 17.Wright J. Essential package of health services country snapshot: India. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 18.Wright J. Essential package of health services country snapshot: Indonesia. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 19.Wright J. Essential package of health services country snapshot: Kenya. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 20.Wright J. Essential package of health services country snapshot: Liberia. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 21.Wright J. Essential package of health services country snapshot: Madagascar. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 22.Wright J. Essential package of health services country snapshot: Malawi. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 23.Wright J. Essential package of health services country snapshot: Mali. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 24.Wright J. Essential package of health services country snapshot: Mozambique. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 25.Wright J. Essential package of health services country snapshot: Nepal. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 26.Wright J. Essential package of health services country snapshot: Nigeria. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 27.Wright J. Essential package of health services country snapshot: Pakistan. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 28.Wright J. Essential package of health services country snapshot: Rwanda. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 29.Wright J. Essential package of health services country snapshot: Senegal. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 30.Wright J. Essential package of health services country snapshot: The republic of South Sudan. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 31.Wright J. Essential package of health services country snapshot: Tanzania. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 32.Wright J. Essential package of health services country snapshot: Uganda. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 33.Wright J. Essential package of health services country snapshot: Yemen. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 34.Wright J. Essential package of health services country snapshot: Zambia. Bethesda (MD): Health Finance & Governance Project Abt Associates Inc; 2015. [Google Scholar]
- 35.Sundewall J. Prioritizing essential packages of health services in six countries in sub-Saharan Africa. Implications and lessons for SRHR. 2019. PMNCH and Swedish International Development Agency. Unpublished report. [Google Scholar]
- 36.Mongkolchati A. Universal health coverage for sexual and reproductive health in the Asia-pacific region. Belgium: HERA Right to Health & Development; 2018. [Google Scholar]
- 37.Fagan T, Dutta A, Rosen J, et al. . Family planning in the context of Latin America’s universal health coverage agenda. Global Health: Sci Pract. 2017;5:382–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murthy R. Presentation on accountability mechanisms – SRH services in the context of UHC and inequalities. In: Technical consultative meeting on guidance for integrating sexual and reproductive health and rights (SRHR) within national UHC plans, Geneva, 15–16 May 2019. Geneva: World Health Organization; 2019. [Google Scholar]
- 39.Todd G, Mamdani M, Loewenson R.. Literature review: Essential health benefits in EAST and Southern Africa. EQUINET Discussion paper 107, IHI, Tanzania, TARSC, EQUINET, Harare, 2016. [Google Scholar]
- 40.Mayhew SH, Adjei S.. Sexual and reproductive health: challenges for priority-setting in Ghana’s health reforms. Health Policy Plan. 2004;19:i50–i61. [DOI] [PubMed] [Google Scholar]
- 41.Population Action International . Seizing the moment. How Zambian sexual and reproductive health advocates are accelerating progress towards universal health coverage financing, 2019. [cited 2019 Aug 15]. Available from: https://pai.org/wp-content/uploads/2019/04/Zambia-Report_Apr-2019.pdf. [Google Scholar]
- 42.Teerawattananon Y, Tangcharoensathien V.. Designing a reproductive health services package in the universal health insurance scheme in Thailand: match and mismatch of need, demand and supply. Health Policy Plan. 2004;19:i31–i39. [DOI] [PubMed] [Google Scholar]
- 43.The World Health Report . Health systems financing: The path to universal coverage. Geneva: World Health Organization; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoehn K, Stratmann J, Schaffler P.. New actors, financial mechanisms and reformed aid reporting: what role for SRHR in post-2015 financing for development? Reprod Health Matters. 2015;23:78–89. [DOI] [PubMed] [Google Scholar]
- 45.Financing demystified . International Planned Parenthood Federation (IPPF), 2015. [cited 2019 Jun 7] Available from: https://www.ippf.org/sites/default/files/ippf_financingdemystified_1.pdf. [Google Scholar]
- 46.Revised Cost Estimates for the Implementation of the Programme of Action of the International Conference on Population and Development: A Methodological Report. New York, United Nations Population Fund, 2009. [Google Scholar]
- 47.Nguyen H, Snider J, Ravishankar N, et al. . Assessing public and private sector contributions in reproductive health financing and utilization for six sub-Saharan african countries. Reprod Health Matters. 2011;19:62–74. [DOI] [PubMed] [Google Scholar]
- 48.Chaumont C, Muhorane C, Moreira-Burgos I, et al. . Maternal and reproductive health financing in Burundi: public-sector contribution levels and trends from 2010 to 2012. BMC Health Serv Res. 2015;15:446. [cited 2019 Jun 13] Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-1009-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rout SK, Pradhan J, Choudhury S.. Estimating financial resources for universal access to sexual reproductive health care: evidence from two states in India. Sexual Reprod Health Care. 2016;9:1–6. [DOI] [PubMed] [Google Scholar]
- 50.Avila-Burgos L, Cahuana-Hurtado L, Montañez-Hernandez J, et al. . Financing maternal health and family planning: are we on the right track? Evidence from the reproductive health subaccounts in Mexico, 2003–2012. PLoS ONE. 2016;11(1):e0147923 doi: 10.1371/journal.pone.0147923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McIntyre D, Kutzin J.. Health financing country diagnostic: a foundation for national strategy development. Geneva: World Health Organization; 2016; (Health Financing Guidance No. 1). Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 52.WHO . Gender, women and primary health care renewal – a discussion paper. Geneva, Switzerland; 2010. [Google Scholar]
- 53.Ntambue AM, Malonga FK, Dramaix-Wilmet M, et al. . Commercialization of obstetric and neonatal care in the democratic republic of the Congo: a study of the variability in user fees in lubumbashi, 2014. PLoS One. 2018;13, doi: 10.1371/journal.pone.0205082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Honda A, Randaoharison PG, Matsui M.. Affordability of emergency obstetric and neonatal care at public hospitals in Madagascar. Reprod Health Matters. 2011;19:10–20. [DOI] [PubMed] [Google Scholar]
- 55.Sundaram A, Vlassoff M, Mugisha F, et al. . Documenting the individual- and household-level cost of unsafe abortion in Uganda. Int Perspect Sex Reprod Health. 2013;39:174–184. [DOI] [PubMed] [Google Scholar]
- 56.Leone T, Coast E, Parmar D, et al. . The individual level cost of pregnancy termination in Zambia: a comparison of safe and unsafe abortion. Health Policy Plan. 2016;31:825–833. [DOI] [PubMed] [Google Scholar]
- 57.Moore AM, Dennis M, Anderson R, et al. . Comparing women’s financial costs of induced abortion at a facility vs. seeking treatment for complications from unsafe abortion in Zambia. Reprod Health Matters. 2018;26:138. DOI: 10.1080/09688080.2018.1522195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roberts SC, Gould H, Kimport K, et al. . Out-of-pocket costs and insurance coverage for abortion in the United States. Womens Health Issues. 2014;24(2):e211–e218. [DOI] [PubMed] [Google Scholar]
- 59.Ilboudo PG, Greco G, Sundby J, et al. . Costs and consequences of abortions to women and their households: A cross-sectional study in Ouagadougou, Burkina Faso. Health Policy Plan. 2015;30:500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Akalu T, Guda A, Tamiru M, et al. . Examining out of pocket payments for maternal health in rural Ethiopia: paradox of free health care un- affordability. Ethiopian J Health Dev. 2012;26:251–257. [Google Scholar]
- 61.Arsenault C, Fournier P, Philibert A, et al. . Emergency obstetric care in Mali: catastrophic spending and its impoverishing effects on households. Bull World Health Organ. 2013;91:207–216. [cited 2019 May 15]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3590618/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dalaba MA, Akweongo P, Aborigo RA, et al. . Cost to households in treating maternal complications in northern Ghana: a cross sectional study. BMC Health Serv Res. 2015;15:34. [cited 2019 Jun 12]. Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-014-0659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Goli S, Rammohan A.. Out-of-pocket expenditure on maternity care for hospital births in Uttar Pradesh, India. Health Econ Rev. 2018;8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hoque ME, Dasgupta SK, Naznin E, et al. . Household coping strategies for delivery and related healthcare cost: findings from rural Bangladesh. Trop Med Int Health. 2015;20:1368–1375. [DOI] [PubMed] [Google Scholar]
- 65.Mohanty SK, Kastor A.. Out-of-pocket expenditure and catastrophic health spending on maternal care in public and private health centres in India: a comparative study of pre and post national health mission period. Health Econ Rev. 2017;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mukherjee S, Singh A, Chandra R.. Maternity or catastrophe: a study of household expenditure on maternal health care in India. Health. 2013;05:109–118. [Google Scholar]
- 67.Myint ANM, Liabsuetrakul T, Htay TT, et al. . Impoverishment and catastrophic expenditures due to out-of-pocket payments for antenatal and delivery care in Yangon region, Myanmar: A cross-sectional study. BMJ Open. 2018;8. DOI: 10.1136/bmjopen-2018-022380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Perkins M, Brazier E, Themmen E, et al. . Out-of-pocket costs for facility-based maternity care in three African countries. Health Policy Plan. 2009;24:289–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prinja S, Bahuguna P, Gupta R, et al. . Coverage and financial risk protection for institutional delivery: how universal is provision of maternal health care in India? PLoS One. 2015;10:e0137315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Radovich E, Dennis ML, Barasa E, et al. . Who pays and how much? A cross-sectional study of out-of-pocket payment for contraception in Kenya. BMJ Open. 2019;9:e022414. DOI: 10.1136/bmjopen-2018-022414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ravit M, Philibert A, Tourigny C, et al. . The hidden costs of a free caesarean section policy in West Africa (Kayes region, Mali). Matern Child Health J. 2015;19:1734–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Shukla M, Kumar A, Agarwal M, et al. . Out-of-pocket expenditure on institutional delivery in rural Lucknow. Indian J Community Health. 2015;27:241–246. [Google Scholar]
- 73.Skordis-Worrall J, Pace N, Bapat U, et al. . Maternal and neonatal health expenditure in Mumbai slums (India): a cross sectional study. BMC Public Health. 2011;11:150. doi: 10.1186/1471-2458-11-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Financing the ICPD Programme of Action . Data for 2012. Estimates for 2013/14. Projections for 2015. New York (NY): United Nations Population Fund; 2014 [Google Scholar]
- 75.Barot S, Cohen SA.. The global gag rule and fights over funding UNFPA: the issues that won’t go away. Guttmacher Policy Review. Available from: https://www.guttmacher.org/sites/default/files/article_files/gpr1802715.pdf. [Google Scholar]
- 76.Sidze EM, Pradhan J, Beekink E, et al. . Reproductive health financing in Kenya: an analysis of national commitments, donor assistance, and the resources tracking process. Reprod Health Matters. 2013;21:139–150. [DOI] [PubMed] [Google Scholar]
- 77.Country portfolio update . Sixth Investors Group Meeting. Global Financing Facility, The World Bank Group, 2017. [cited 2019 Sep 22]. Available from: https://www.globalfinancingfacility.org/sites/gff_new/files/documents/GFF-IG6-3.pdf. [Google Scholar]
- 78.Global Financing Facility . Fact sheet: sexual and reproductive health and rights. Washington (DC): World Bank Group; 2018. [cited 2020 Apr 21] Available from: https://www.globalfinancingfacility.org/sites/gff_new/GFF-Annual-report/pdf/SRHR_GFF-FactSheet-EN.pdf. [Google Scholar]
- 79.Taking Stock: IPPF Recommendations on the Global Financing Facility (GFF) . International Planned Parenthood Federation, 2018. [cited 2019 September 21]. Available from: https://www.ippf.org/sites/default/files/2018-09/GFF_Recommendations_IPPF_Feb2018.pdf [Google Scholar]
- 80.Mutunga A, Sundaram P.. How will the global financing facility deliver for sexual and reproductive health and rights? Bretton Woods Project, 31 March 2015. Available from: https://www.brettonwoodsproject.org/2015/03/how-will-the-global-financing-facility-deliver-for-sexual-and-reproductive-health-and-rights/. [Google Scholar]
- 81.Kurth A, Bielinski L, Graap K, et al. . Reproductive and sexual health benefits in private health insurance plans in Washington state. Fam Plann Perspect. 2001;33:153–179. [PubMed] [Google Scholar]
- 82.Boonstra HD. Abortion in the lives of women struggling financially: why insurance coverage matters. Guttmacher Policy Review. 2016;19:46–52. [cited 2019 May 15]. Available from: https://www.guttmacher.org/sites/default/files/article_files/gpr1904616_0.pdf. [Google Scholar]
- 83.Finnoff K. Gender disparities in access to the Rwandan mutual insurance scheme. Fem Econ. 2015. DOI: 10.1080/13545701.2015.1088658. [DOI] [Google Scholar]
- 84.Govender V, Ataguba JE, Alaba OA.. Health insurance coverage within households: the case of private health insurance in South Africa. Geneva Pap Risk Insur – Issues Pract. 2014;39:712–726. [Google Scholar]
- 85.Dake FAA. Examining equity in health insurance coverage: an analysis of Ghana’s national health insurance scheme. Int J Equity Health. 2018;17:85. [cited 2019 Jun 18]. Available from: https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-018-0793-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Duku SKO. Differences in the determinants of health insurance enrolment among working-age adults in two regions in Ghana. BMC Health Serv Res. 2018;18:384. DOI:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gobah F, Zhang L.. The national health insurance scheme in Ghana: prospects and challenges: a cross-sectional evidence. Glob J Health Sci. 2011;3. DOI: 10.5539/gjhs.v3n2p90. [DOI] [Google Scholar]
- 88.Waddington C, Sambo C.. Financing health care for adolescents: a necessary part of universal health coverage. Bull World Health Organ. 2015;93:57–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Karra M, Canning D, Hu J, et al. . Community-based financing of family planning in developing countries: A systematic review. Stud Fam Plann. 2016;47:325–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gupta I, Joe W, Rudra S.. Demand side financing in health: How far can it address the issue of low utilization in developing countries? Geneva: World Health Organization; 2010; Background paper no. 27 to World Health Report 2010. [Google Scholar]
- 91.Bellows N, Bellows B, Warren C.. Systematic review: the use of vouchers for reproductive health services in developing countries: systematic review. Trop Med Int Health. 2011;16:84–96. [DOI] [PubMed] [Google Scholar]
- 92.Bellows BW, Conlon CM, Higgs ES, et al. . A taxonomy and results from a comprehensive review of 28 maternal health voucher programmes. J Health, Popul Nutr. 2013;31:S106–S128. [PubMed] [Google Scholar]
- 93.Bellows B, Bulaya C, Inambwae S, et al. . Family planning vouchers in low and middle income countries: a systematic review. Stud Fam Plann. 2016;47:357–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Grainger C, Gorter A, Okal J, et al. . Lessons from sexual and reproductive health voucher program design and function: a comprehensive review. Int J Equity Health. 2014;13:33. [cited 2019 May 30]. Available from: https://equityhealthj.biomedcentral.com/articles/10.1186/1475-9276-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Glassman A, Duran D, Fleisher L, et al. . Impact of conditional cash transfers on maternal and newborn health. J Health, Popul Nutr. 2013;31: S48–S66. [PubMed] [Google Scholar]
- 96.Ekezie CC, Lamont K, Bhattacharya S.. Are cash transfer programs effective in improving maternal and child health in Sub-saharan Africa? A systematic review of randomized controlled trials. J Global Health. 2017. [cited 2019 May 5]. Available from: http://www.ghjournal.org/are-cash-transfer-programs-effective-in-improving-maternal-and-child-health-in-sub-saharan-africa-a-systematic-review-of-randomized-controlled-trials/. [Google Scholar]
- 97.Lim SS, Dandona L, Hoisington LA, et al. . India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: An impact evaluation. Lancet. 2010;375(9730):2009.– DOI: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 98.Khan ME, Hazra A, Kant A, et al. . Conditional and unconditional cash transfers to improve use of contraception in low and middle income countries: a systematic review. Stud Fam Plann. 2016;47(4):371–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ved R, Sundararaman T, Gupta G, et al. . Program evaluation of the Janani Suraksha Yojna. BMC Proc. 2012;6(Suppl 5):O15. Available from: http://www.biomedcentral.com/1753-6561/6/S5/O15. [Google Scholar]
- 100.Witter S, Govender V, Ravindran T, Yates R.. Minding the gaps: health financing, universal health coverage and gender. Health Policy Plan . 2017; 32:v4–v12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Balasubramanian P, Ravindran TKS.. Pro-poor maternity benefit schemes and rural women: findings from Tamil Nadu. Econ Political Weekly. 2012;25:19. [Google Scholar]
- 102.Cerceau S. Gender equity in access to health care. How social health protection can tackle access barriers for women and improve gender related inequities. A case study on India’s national health insurance scheme Rashtriya Swasthya Bima Yojana (RSBY). France: Ecoles des Hautes Etudes en Sante Publique; June 2012. [cited 2019 May 25]. Available from https://documentation.ehesp.fr/memoires/2012/mph/cerceau.pdf. [Google Scholar]
- 103.Karpagam S, Vasan A, Seethappa V.. Falling through the gaps: women accessing care under health insurance schemes in Karnataka. Indian J Gend Stud. 2016;23:69–86. [Google Scholar]
- 104.Ramprakash R. Gender analysis of publicly-funded health insurance schemes: a study of the Chief Minister’s Comprehensive Health Insurance of Tamil Nadu. Tata Institute of Social Sciences, Mumbai, 2018. (unpublished PhD dissertation). [Google Scholar]
- 105.Philip NE, Ravindran TKS.. Government sponsored health insurance coverage and out-of-pocket spending among elderly in Kerala: a cross-sectional study. J Aging Res Healthcare. 2017;2:15–27. [Google Scholar]
- 106.Reproductive health policies 2017 data booklet. New York, Department of Economic and Social Affairs, Population Division, United Nations, 2017. (ST/ESA/ SER.A/396). [cited 2019 Aug 12]. Available from: https://www.un.org/en/development/desa/population/publications/pdf/policy/reproductive_health_policies_2017_data_booklet.pdf [Google Scholar]
- 107.Singh S, Remez L, Sedgh G, et al. . Abortion worldwide 2017: uneven progress, unequal access. New York (NY): Guttmacher Institute; 2018. [Google Scholar]
- 108.Against her will: Forced and coerced sterilization of women worldwide. New York, Open Society Foundations, 2011. [cited 2019 May 20]. Available from: http://www.opensocietyfoundations.org/sites/default/files/against-her-will 20111003.pdf. [Google Scholar]
- 109.Carroll A, Mendos LR.. State sponsored homophobia 2017: a world survey of sexual orientation laws: criminalisation, protection and recognition. Geneva: International Lesbian, Gay, Bisexual, Trans and Intersex Association (ILGA); 2017. [Google Scholar]
- 110.Platt L, Grenfell P, Meiksin R, et al. . Associations between sex work laws and sex workers’ health: A systematic review and meta-analysis of quantitative and qualitative studies. PLoS Med. 2018;15:e1002680. doi: 10.1371/journal.pmed.1002680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.WHO . Sexual health, human rights and the law. Geneva; 2015. [Google Scholar]
- 112.Haque SE, Rahman M, Mostofa MG, et al. . Reproductive health care utilization among young mothers in Bangladesh: does autonomy matter? Womens Health Issues. 2012;22:e171–e180. [DOI] [PubMed] [Google Scholar]
- 113.Ameyaw EK, Tanle A, Kissah-Korsah K, et al. . Women’s health decision-making autonomy and skilled birth attendance in Ghana. Int J Reprod Med. 2016;2016:1. doi: 10.1155/2016/6569514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Obasohan PE, Gana P, Mustapha MA, et al. . Decision making autonomy and maternal healthcare utilization among Nigerian women. Int J MCH and AIDS (IJMA). 2019;8:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Skovdal M, Campbell C, Madanhire C, et al. . Masculinity as a barrier to men’s use of HIV services in Zimbabwe. Global Health. 2011;7:13. [cited 2019 May 19]. Available from: https://globalizationandhealth.biomedcentral.com/track/pdf/10.1186/1744-8603-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cornell M, McIntyre J, Myer L.. Men and antiretroviral therapy in Africa: our blind spot. Trop Med Int Health. 2011;16:828–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Heise L, Greene ME, Opper N, et al. . Gender inequality and restrictive gender norms: framing the challenges to health. The Lancet. 2019;393:2440–2454. [DOI] [PubMed] [Google Scholar]
- 118.Weber AM, Cislaghi B, Meausoone V, et al. . Gender norms and health: insights from global survey data. Lancet. 2019;393:2455–2468. [DOI] [PubMed] [Google Scholar]
- 119.Chakrapani V, Newman PA, Shunmugam M, et al. . Barriers to free antiretroviral treatment access among kothi- identified men who have sex with men and aravanis (transgender women) in Chennai, India. AIDS Care. 2011;23:1687–1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Beattie TSH, Bhattacharjee P, Suresh M, et al. . Personal, interpersonal and structural challenges to accessing HIV testing, treatment and care services among female sex workers, men who have sex with men and transgenders in Karnataka state, South India. J Epidemiol Community Health. 2012;66:ii42–ii48. [DOI] [PubMed] [Google Scholar]
- 121.Cook RJ, Maine D.. Spousal veto over family planning services. Am J Public Health. 1987;77:339–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mbeba RM, Mkuye MS, Magembe GE, et al. . Barriers to sexual reproductive health services and rights among young people in Mtwara district, Tanzania: a qualitative study. Pan Afr Med J. 2012;13:13. [PMC free article] [PubMed] [Google Scholar]
- 123.Self A, Chipokosa S, Misomali A, et al. . Youth accessing reproductive health services in Malawi: drivers, barriers, and suggestions from the perspectives of youth and parents. Reprod Health. 2018;15:108. DOI: 10.1186/s12978-018-0549-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Alencar Albuquerque G, de Lima Garcia C, da Silva Quirino G, et al. . Access to health services by lesbian, gay, bisexual, and transgender persons: systematic literature review. BMC Int Health Hum Rights. 2016;16:2. doi: 10.1186/s12914-015-0072-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Luvuno ZPB, Ncama B, Mchunu G.. Transgender population’s experiences with regard to accessing reproductive health care in Kwazulu-Natal, South Africa: A qualitative study. Afr J Primary Health Care Family Med. 2019;11:a1933. DOI: 10.4102/phcfm.v11i1.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kattari SK, Hasche L.. Differences across age groups in transgender and gender non-conforming people’s experiences of health care discrimination, harassment, and victimization. J Aging Health. 2016;28:285–306. [DOI] [PubMed] [Google Scholar]
- 127.Bohren MA, Vogel JP, Hunter EC, et al. . The mistreatment of women during childbirth in health facilities globally: A mixed-methods systematic review. PLoS Med. 2015;12: e1001847. [cited 2019 Jun 6]. Available from: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Muñoz JT, Moreno CMR, Gil L, et al. . Obstetric violence and abortion. Contributions to the debate in Colombia. New York (NY): Global Doctors for Choice Network; 2015. [Google Scholar]
- 129.Betron ML, McClair TL, Currie S, et al. . Expanding the agenda for addressing mistreatment in maternity care: a mapping review and gender analysis. Reprod Health. 2018;15:143. [cited 2019 June 20]. Available from: https://reproductive-health-journal.biomedcentral.com/articles/10.1186/s12978-018-0584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jardim D, Modena CM.. Obstetric violence in the daily routine of care and its characteristics. Rev Lat Am Enfermagem. 2018;26:e3069. doi: 10.1590/1518-8345.2450.3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Limwattananon S. Public-private mix in health care for women and children in low-income countries: An analysis of demographic and health surveys. Bangkok: International Health Policy Program; 2008. [cited 2019 Sep 22]. Available from: https://www.r4d.org/resources/private-public-mix-woman-child-health-low-income-countries/. [Google Scholar]
- 132.Pomeroy A, Koblinsky M, Alva S.. Private delivery care in developing countries: trends and determinants. Calverton (MD): ICF Macro; 2010. [Google Scholar]
- 133.Healthy Partnerships: How Governments Can Engage the Private Sector to Improve Health In Africa. Washington, DC, International Financing Corporation (IFC), The International Bank for Reconstruction and Development/ The World Bank, 2011. [Google Scholar]
- 134.Madhavan S, Bishai D.. Private sector engagement in sexual and reproductive health and maternal and neonatal health: A review of the evidence. Human Development Resource Centre, United States of America; 2010. [cited 2019 Jul 8]. Available from: https://healthmarketinnovations.org/sites/default/files/Private%20Sector%20Engagement%20in%20SRH%20and%20MNH%202010.pdf. [Google Scholar]
- 135.Sweat MD, Denison J, Kennedy C, et al. . Effects of condom social marketing on condom use in developing countries: a systematic review and meta-analysis, 1990–2010. Bull World Health Organ. 2012;90:613–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Koehlmoos TP, Gazi R, Hossain SS, et al. . Social franchising evaluations: A scoping review. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2011. [Google Scholar]
- 137.Tougher S, Dutt V, Pereira S, et al. . Effect of a multifaceted social franchising model on quality and coverage of maternal, newborn, and reproductive health-care services in Uttar Pradesh, India: a quasi-experimental study. Lancet Global Health. 2018;6:e211. [DOI] [PubMed] [Google Scholar]
- 138.Chakraborty NM, Mbondo M, Wanderi J.. Evaluating the impact of social franchising on family planning use in Kenya. J Health, Popul Nutr. 2016;35:19. [cited 2019 July 17]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5025970/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Munroe E, Hayes B, Taft J.. Private-sector social franchising to accelerate family planning access, choice and quality: results from Marie Stopes International. Global Health: Sci Pract. 2015;3:195–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Duvall S, Thurston S, Weinberger M, et al. . Scaling up delivery of contraceptive implants in sub-Saharan Africa: operational experiences of Marie Stopes International. Global Health: Sci Pract. 2014;2:72–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gold J, Burke E, Cissé B, et al. . Increasing access to family planning choices through public-sector social franchising: The experience of Marie Stopes International in Mali. Global Health: Sci Pract. 2017;5:286–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Montagu D, Goodman C.. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? The Lancet. 2016;388:613–621. [DOI] [PubMed] [Google Scholar]
- 143.Arur A, Peters D, Hansen P, et al. . Contracting for health and curative care use in Afghanistan between 2004 and 2005. Health Policy Plan. 2010;25:135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Bloom E, Bhushan I, Clingingsmith D, et al. . Contracting for health: evidence from Cambodia. Washington (DC): Brookings Institute; 2006. [Google Scholar]
- 145.Ravindran TKS. Public private partnerships in maternal health services. Econ Political Weekly. 2011;46:43–52. [Google Scholar]
- 146.Mohanan M, Bauhoff S, La Forgia G, et al. . Effect of Chiranjeevi Yojana on institutional deliveries and neonatal and maternal outcomes in Gujarat, India: a difference-in- differences analysis. Bull World Health Organ. 2014;92:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Yasobant S, Vora KS, Shewade HD, et al. . Utilization of the state led public private partnership program “Chiranjeevi Yojana” to promote facility births in Gujarat, India: a cross sectional community based study. BMC Health Serv Res. 2016;16:266.), DOI: 10.1186/s12913-016-1510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Patoillard E, Goodman C, Hanson K, et al. . Can working with the private for-profit sector improve utilization of quality health services by the poor? A systematic review of the literature. Int J Equity Health. 2007;6:17. [cited 2019 May 14]. Available from: https://equityhealthj.biomedcentral.com/articles/10.1186/1475-9276-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Beyeler N, York De La Cruz A, Montagu D.. The impact of clinical social franchising on health services in low- and middle-income countries: a systematic review. PLoS One. 2013;8:e60669. DOI: 10.1371/journal.pone.0060669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Haemmerli M, Santos A, Penn-Kekana L, et al. . How equitable is social franchising? case studies of three maternal healthcare franchises in Uganda and India. Health Policy Plan. 2018;33:411–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Meuwissen LE, Gorter AC, Knottnerus AJ.. Impact of accessible sexual and reproductive health care on poor and underserved adolescents in Managua, Nicaragua: a quasi-experimental intervention study. J Adolesc Health. 2006;38(1):56.e1. [DOI] [PubMed] [Google Scholar]
- 152.Boddam-Whetham L, Gul X, Al-Kobati E, et al. . Vouchers in fragile states: reducing barriers to long-acting reversible contraception in Yemen and Pakistan. Global Health: Sci Pract 2016;4:S94–S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ravindran TKS, Fonn S.. Are social franchises contributing to universal access to reproductive health services in low- income countries? Reprod Health Matters. 2011;19:85–101. [DOI] [PubMed] [Google Scholar]
- 154.Morgan R, Ensor T, Waters H.. Performance of private sector health care: implications for universal health coverage. Lancet. 2016;388:606–612. [DOI] [PubMed] [Google Scholar]
- 155.Centre for Reproductive Rights (CRR) . Breaking ground 2015: human rights treaty bodies and reproductive rights. New York (NY): CRR; 2015. [Google Scholar]
- 156.Boydell V, Keesbury J.. Social accountability: What are the lessons for improving family planning and reproductive health programs? A review of the literature. Washington, DC: Population Council, Evidence Project, 2014. (Working Paper). [cited 2019 Aug 10]. Available from: (http://evidenceproject.popcouncil.org/wp-content/uploads/2014/11/2014_RightsBasedProg_SocAcctWP.pdf. [Google Scholar]
- 157.Hulton L, Matthews Z, Martin-Hilber A, et al. . Using evidence to drive action: a “revolution in accountability” to implement quality of care for better maternal and newborn health in Africa. Int J Gynaecol Obstet. 2014;127 (1):96–101. [DOI] [PubMed] [Google Scholar]
- 158.FIGO, ICM, WRA, IPA and WHO . Mother-baby friendly birthing facilities. Int J Gynaecol Obstet. 2015;128:95–99. [DOI] [PubMed] [Google Scholar]
- 159.Papp SA, Gogoi A, Campbell C.. Improving maternal health through social accountability: a case study from orissa, India. Glob Public Health. 2013;8:449–464. [DOI] [PubMed] [Google Scholar]
- 160.Frisancho A. Citizen-led accountability to improve UHC. In: World bank civil society policy forum, Washington D.C, 19 June 2017. Washington, DC: World Bank; 2017. [cited 2019 Aug 5]. Available from: http://pubdocs.worldbank.org/en/240521496934666452/FRISANCHO-Citizen-led-Accountability-for.pdf. [Google Scholar]
- 161.Kaur J. The role of litigation in ensuring women’s reproductive rights: an analysis of shanti devi judgement in India. Reprod Health Matters. 2012;20(39):21–30. [DOI] [PubMed] [Google Scholar]
- 162.van Belle S, Boydell V, George AS, et al. . Broadening understanding of accountability ecosystems in sexual and reproductive health and rights: A systematic review. PLoS One. 2018;13:e0196788. doi: 10.1371/journal.pone.0196788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Blake, Carolyn & Sarpei, Nii & Bailey, Claire & Ismaila, Yakubu & Deganus, Sylvia & Bosomprah, Samuel & Galli, Francesco & Clark, Sarah.. Scorecards and social accountability for improved maternal and newborn health services: a pilot in the Ashanti and Volta regions of Ghana. Int J Gynaecol Obstet. 2016; 135:372-379. [DOI] [PubMed] [Google Scholar]
- 164.Gullo S, Galavotti C, Sebert Kuhlmann A, et al. . Effects of a social accountability approach, CARE’s community score card, on reproductive health-related outcomes in Malawi: A cluster-randomized controlled evaluation. PLoS One. 2017;12:e0171316.), DOI: 10.1371/journal.pone.0171316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kakade D. Community-based monitoring as an accountability tool: influence on rural health services in maharashtra, India. BMC Proc. 2012;6:O9. [cited 2019 Jul 15]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3287531/pdf/1753-6561-6-S1-O9.pdf. [Google Scholar]
- 166.Boydell V, Schaaf M, George A, et al. . Building a transformative agenda for accountability in SRHR: lessons learned from SRHR and accountability literatures. Sexual Reprod Health Matters. 2019;27:64–75. doi: 10.1080/26410397.2019.1622357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Making fair choices on the path to universal health coverage . Final report of the WHO Consultative Group on Equity and Universal Health Coverage, Geneva: World Health Organization; 2014. [Google Scholar]
- 168.Gwatkin DR, Ergo A.. Universal health coverage: friend or foe of health equity? Lancet. 2011;377:2160–2161. [DOI] [PubMed] [Google Scholar]
- 169.Sen G, Govender V.. Sexual and reproductive health and rights in changing health systems. Glob Public Health, 2015; 10 (2):228–242. DOI: 10.1080/17441692.2014.986161. [DOI] [PMC free article] [PubMed] [Google Scholar]