Abstract
Unmet need for postpartum contraception in rural Nepal remains high and expanding access to sexual and reproductive healthcare is essential to achieving universal healthcare. We evaluated the impact of an integrated intervention that employed community health workers aided by mobile technology to deliver patient-centred, home-based antenatal and postnatal counselling on postpartum modern contraceptive use. This was a pre–post-intervention study in seven village wards in a single municipality in rural Nepal. The primary outcome was modern contraceptive use among recently postpartum women. We performed a multivariable logistic regression to examine contraceptive use among postpartum women pre- and one-year post-intervention. We conducted qualitative interviews to explore the implementation process. There were 445 postpartum women in the pre-intervention group and 508 in the post-intervention group. Modern contraceptive use increased from 29% pre-intervention to 46% post-intervention (p < 0.0001). Adjusting for age, caste, and household expenditure, time since delivery and sex of child in the index pregnancy, postpartum women one-year post-intervention had twice the odds (OR 2.3; CI 1.7, 3.1; p < 0.0001) of using a modern contraceptive method as compared to pre-intervention. Factors at the individual, family, and systems level influenced women’s contraceptive decisions. The intervention contributed to increasing contraceptive use through knowledge transfer, demand generation, referrals to healthcare facilities, and follow-up. A community-based, patient-centred contraceptive counselling intervention supported by mobile technology and integrated into longitudinal care delivered by community health workers appears to be an effective strategy for improving uptake of modern contraception among postpartum women in rural Nepal.
Keywords: family planning, postpartum contraception, Nepal, implementation science, reproductive health, community health workers, contraceptive counselling
Résumé
Les besoins insatisfaits en contraception postpartum dans le Népal rural restent élevés et il est essentiel d’élargir l’accès aux soins de santé sexuelle et reproductive pour parvenir à une couverture santé universelle. Nous avons évalué l’impact d’une intervention intégrée qui a employé des agents de santé communautaires secondés par une technologie mobile pour dispenser des conseils prénatals et postnatals à domicile et axés sur les patientes en matière d’utilisation de contraceptifs modernes pendant le postpartum. Il s’agissait d’une étude avant et après l’intervention dans sept villages d’une seule municipalité du Népal rural. Le principal résultat était l’emploi de contraceptifs modernes chez des femmes ayant récemment accouché. Nous avons réalisé une régression logistique multivariable pour examiner l’emploi de contraceptifs chez les jeunes accouchées avant et une année après l’intervention. Nous avons mené des entretiens qualitatifs pour explorer le processus de mise en œuvre. Le groupe pré-intervention comptait 445 femmes en postpartum, contre 508 dans le groupe post-intervention. L’emploi de contraceptifs modernes est passé de 29% avant l’intervention à 46% après l’intervention (p < 0,0001). Après ajustement en fonction de l’âge, de la caste et des dépenses du ménage, du délai écoulé depuis l’accouchement et du sexe de l’enfant dans la grossesse examinée, les femmes en postpartum une année après l’intervention avaient deux fois plus de probabilités (Rc 2,3; IC 1,7, 3,1; p < 0,0001) d’utiliser une méthode contraceptive moderne qu’avant l’intervention. Des facteurs aux niveaux individuel, familial et systémique influaient sur les décisions contraceptives des femmes. L’intervention a contribué à augmenter l’emploi de contraceptifs par le transfert de connaissances, la création de demande, les aiguillages vers les centres de soins de santé et le suivi. Une intervention relative aux conseils contraceptifs axés sur les patientes et à assise communautaire, soutenue par une technologie mobile et intégrée dans les soins longitudinaux dispensés par des agents de santé communautaires, semble être efficace pour améliorer le recours à une contraception moderne parmi les femmes en postpartum dans le Népal rural.
Resumen
La necesidad insatisfecha de anticoncepción posparto en las zonas rurales de Nepal continúa siendo alta y la ampliación del acceso a los servicios de salud sexual y reproductiva es esencial para lograr cobertura médica universal. Evaluamos el impacto de una intervención integrada que empleó a agentes de salud comunitaria ayudados por tecnología móvil para brindar consejería prenatal y posnatal domiciliaria centrada en la paciente sobre el uso de anticonceptivos modernos posparto. Este estudio pre- y post-intervención fue realizado en siete subdivisiones en una sola municipalidad de Nepal rural. El principal resultado fue el uso de anticonceptivos modernos entre mujeres en posparto reciente. Realizamos una regresión logística multivariable para examinar el uso de anticonceptivos entre mujeres posparto antes de la intervención y un año después. Realizamos entrevistas cualitativas para explorar el proceso de ejecución. Había 445 mujeres posparto en el grupo pre-intervención y 508 en el grupo post-intervención. El uso de anticonceptivos modernos aumentó del 29% pre-intervención al 46% post-intervención (p < 0.0001). Ajustando por edad, casta y gastos del hogar, tiempo desde el parto y sexo del niño en el índice de embarazos, las mujeres posparto un año después de la intervención tuvieron el doble de probabilidades (RM 2.3; IC 1.7, 3.1; p < 0.0001) de usar un método anticonceptivo moderno, comparadas con las mujeres en el grupo pre-intervención. Los factores a nivel individual, familiar y sistémico influyeron en las decisiones anticonceptivas de las mujeres. La intervención contribuyó a aumentar el uso de anticonceptivos mediante la transferencia de conocimientos, generación de demanda, referencias a unidades de salud y seguimiento. La intervención comunitaria, centrada en la paciente, para brindar consejería anticonceptiva apoyada por tecnología móvil e integrada en atención longitudinal domiciliaria brindada por agentes de salud comunitaria parece ser una estrategia eficaz para mejorar la aceptación de anticonceptivos modernos entre mujeres posparto en las zonas rurales de Nepal.
Introduction
The World Health Organization (WHO) recommends 24 months of spacing between births, as shorter pregnancy intervals are associated with adverse maternal and child health outcomes.1–3 Despite the benefits of birth spacing, there continues to be significant unmet need for postpartum contraception worldwide.4 Access to modern contraceptive methods facilitates a woman’s ability to decide freely and for herself whether, when, and how many children she wants to have.5 Universal health coverage for women, girls, and adolescents, a cornerstone of the Sustainable Development Goals, requires the expansion of sexual and reproductive health services.6,7 Expanding access to postpartum contraception, especially in remote areas, will be one critical component towards this end.
In Nepal, 52% of women had an unmet need for contraception in the 24 months following delivery.8 While 95% of postpartum women desired to delay pregnancy for at least two years, only 39% reported using a modern contraceptive method.8 Among women who had live births in the preceding five years, a mere 13% reported being counselled on family planning after delivery.9 The postpartum period presents an important missed opportunity to meet women’s needs for contraception.10 Existing data suggest that strategies to improve postpartum contraception in low- and middle-income countries that bridge the continuum of reproductive healthcare – antenatal care (ANC), labour and delivery, postnatal care (PNC), and infant care – are more effective than short term, stand-alone interventions.10–13
Nepal’s geographic diversity poses challenges to service delivery and manifests in disparities in healthcare coverage.14 Similar to other resource-limited settings, challenges include low follow-up rates, poor patient tracking systems, and physical barriers to access healthcare facilities.15,16 Nepal has long recognised community health workers (CHWs) as an important cadre of healthcare workers where human resources are scarce and as such they are well positioned to bridge barriers to universal health coverage, especially in the arena of sexual and reproductive services.17,18 The existing national CHW system, also known as the Female Community Health Volunteers (FCHVs) programme, while recognised as instrumental in helping Nepal to achieve its reproductive health goals to date, has also faced issues including variable quality of care and lack of uniform supervision and training. As Nepal works to achieve access to universal health coverage it is looking to design, implement, and evaluate models to improve the FCHV system.18
In collaboration with Nyaya Health Nepal and Possible, we implemented patient-centred contraceptive counselling and care coordination within an integrated longitudinal CHW intervention that spans ANC, PNC, and infant care. Nyaya Health Nepal is a Nepal-based non-governmental organisation that operates in partnership with the Ministry of Health and Population to advance integrated care delivery systems. Possible, an American non-profit organisation, provides technical and financial support. The integrated intervention, developed in partnership with the Ministry of Health and Population and designed as a national pilot, is ongoing and will ultimately reach a population of 250,000 in two districts of Nepal. The pilot has the potential to inform the design of a new system for government CHWs in Nepal.18
In this paper, we looked specifically at the impact of the intervention on postpartum modern contraceptive use after one year of implementation and described the mechanisms of impact using a mixed-methods approach in a sub-population of the national pilot. Additional outcomes from the overall integrated intervention will be presented in subsequent publications.
Methods
Study site
The sub-population of the national pilot where we conducted this study was in Kamalbazaar, a rural municipality in Achham District with an estimated population of 20,000. Achham, one of Nepal’s poorest districts, is located in Province 7 (Figure 1).19 Affected by residual consequences of civil war and long-standing poverty, this province has the nation’s highest neonatal and under-five mortality rates at 41 per 1000 live births and 69 per 1000 live births, respectively.9 At the time of the study, Kamalbazaar consisted of seven wards, each with a village clinic (known locally in Nepal as health posts) that provided basic outpatient primary care services. As Kamalbazaar is geographically expansive with minimal road infrastructure, women walked up to four hours to reach the primary healthcare centre (PHCC), the next higher-level facility. Women who were referred from the PHCC travelled an additional three hours by motor vehicle to the government district hospital or four to five hours to the district-level hospital supported by Nyaya Health Nepal. By foot, the walk could take up to a day. Travel times were significantly lengthened during the monsoon season, which is three months of the year.
Figure 1.
Map of Nepal
WHO-specified modern contraceptive methods used in Achham included: condoms, combined oral contraceptive pills, emergency contraception, progestin-only injectables, copper intrauterine devices (IUDs), implants, female sterilisation, male sterilisation, and lactational amenorrhea method (LAM).20 Progestin-only pills are not included in the family planning methods supplied by the Nepal government. Post-placental IUDs were not provided by facilities in the study area. During the study period, condoms, pills, and injectables were available at all village clinics. One of the seven village clinics provided IUDs and implants. Both the PHCC and district hospital provided condoms, pills, injectables, implants, and IUDs. Male sterilisations were performed at the Nyaya Health Nepal-supported hospital and at the PHCC when trained staff were available. Female sterilisations were only provided at the Nyaya Health Nepal-supported hospital.
Intervention
This study was nested within an implementation research study evaluating an integrated reproductive, maternal, newborn, and child health (RMNCH) intervention implemented by CHWs.18 In contrast to the national FCHV system, these CHWs are employed by Nyaya Health Nepal. FCHVs only need to be married women who live within the communities they serve without any additional eligibility criteria. They work three hours per day or two days per week without compensation and supervision varies from site to site.21 The Nyaya Health Nepal CHWs are full-time, salaried local women with a minimum 10th-grade education level. They are supervised by community health nurses (CHNs) employed by Nyaya Health Nepal. These CHWs have a lower CHW to population ratio – one per 2000 individuals – as compared to one FCHV per 500 individuals. FCHVs continued to operate in the study area without any changes.21
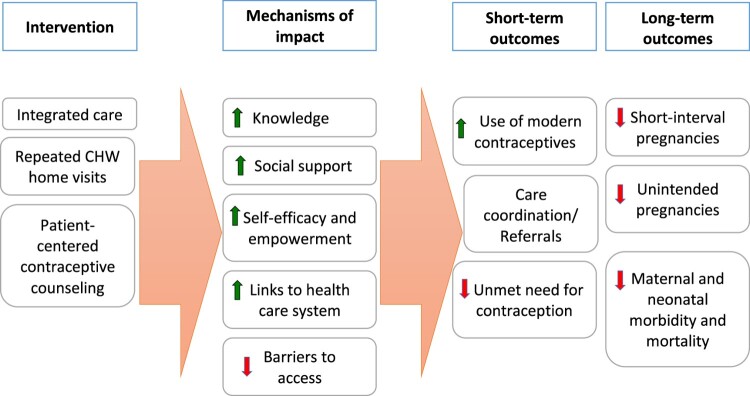
The integrated intervention includes active pregnancy identification, home-based ANC and PNC counselling and care coordination, patient-centred contraceptive counselling using the Balanced Counseling Strategy (BCS), group ANC, and home-based childcare and counselling. Between June and September of 2016, all married women of reproductive age living in Kamalbazaar were offered enrolment into the integrated intervention. CHWs actively identified pregnancies through three-monthly home visits of all married reproductive-aged women in the catchment. Beginning in February 2017, women with desired pregnancies received home-based ANC and PNC counselling and care coordination. Due to staff and capacity issues, additional planned components of the integrated intervention, which included group ANC and childcare and counselling, were not implemented until September 2017 and December 2017, respectively. General contraceptive counselling occurred at the eighth month ANC home visit and patient-centred contraceptive counselling using BCS, as detailed below, was offered at PNC months 1, 5, and 10. CHWs referred women who chose a contraceptive method to the nearest healthcare facilities where the methods were available. At subsequent home visits, CHWs followed up to see whether women initiated their chosen method, helped to address barriers to access, and provided ongoing support and counselling on potential side effects (Figure 2). CHWs did not distribute contraception at home visits.
Figure 2:
Conceptual model
We adapted the BCS, a toolkit developed by the Population Council to facilitate high-quality, individualised contraceptive counselling.22–24 The BCS uses a series of questions to narrow method choices to those that are most consistent with a woman’s reproductive values and preferences. Visual aids are used to guide counselling and illustrate the relative effectiveness of the methods. In Nepal, the BCS has been used in facility-based post-abortion care settings to improve uptake of long-acting reversible methods.25 We adapted the BCS for community-based, CHW-delivered, postpartum contraceptive counselling. Adaptations included the addition of materials focused on the lactational amenorrhoea method (Supplemental File 3), training of CHWs to involve husbands and mother-in-laws, and repeat counselling sessions, if desired by the woman, at multiple time points during the first year postpartum. Women who reported high-risk medical conditions such as hypertension were referred to the village clinic or received a home visit by a CHN who reviewed safety of methods chosen.
All CHW counselling and data collection were supported by CommCare, an open-source platform that enabled us to build a customised mobile application to collect data offline and display counselling content.26 We created an additional module in CommCare for the BCS. The BCS questions were displayed, and depending on a woman’s responses, the application provided instructions for the CHW to set aside less relevant contraceptive options and individualise the counselling. The CHW then recorded the woman’s chosen method in the mobile application. At subsequent visits, the CHW collected information on initiation, barriers to access, and continuation. All counselling materials were translated into Nepali and adjusted to ensure accuracy based on feedback from the CHWs.
Nyaya Health Nepal’s mobile systems engineer (author S. Pandey) provided a week-long training for the CHWs and CHNs on CommCare use and data collection. The CHWs received a two-day clinical training conducted by the CHNs on contraceptive methods and use of the BCS algorithm. Clinical topics included recommendations and reasons for birth spacing, contraceptive efficacy, contra-indications, timing for initiation of methods postpartum, and facilities where each method could be accessed. We developed training materials based on WHO and Nepal national guidelines. Training materials emphasised best practices for contraceptive counselling, such as shared decision-making, respect for patient autonomy, and anticipatory guidance on potential side effects.27–29 We held a one-day follow-up clinical training for the CHWs after three months of implementation. In addition to the scheduled trainings, the mobile systems engineer was routinely available to troubleshoot technical challenges and provided ongoing improvement of the mobile application. CHNs held weekly individual meetings with CHWs to review home visit schedules, discuss difficult cases, and review patients with medical conditions. Study staff periodically accompanied the CHNs on CHW supervisory home visits to oversee fidelity of counselling to the model and the data collection processes.
Study design
We measured modern contraceptive use of recently postpartum women in our catchment area pre- and one-year post-implementation of the intervention. To contextualise our quantitative findings, we used qualitative methods to explore factors influencing women’s contraceptive decision-making, perceived impact of the intervention, mechanisms of impact, and acceptability of the intervention.
We performed a power calculation for the planned evaluation of the pre–post-intervention data. Our pre-intervention group had 450 women within one-year postpartum. We assumed birth rates would remain relatively stable over the intervention period, so anticipated 450 postpartum women in our post-intervention group. Using a baseline modern contraceptive prevalence of 34% (obtained from a neighbouring catchment area) and a two-sided p-value of 0.05, we had 80% power to detect a 10% change in modern contraceptive use. In prior studies in this setting, the intra-cluster correlation coefficient had been sufficiently small to leave out of the power calculation.30
Data collection
Between June and September 2016, we enrolled all married women ages 15–49 living in Kamalbazaar into the integrated RMNCH intervention. Data for the pre-intervention group were collected by CHWs over this three-month period. This included an exhaustive sample of recently postpartum women living in Kamalbazaar who were available, not pregnant on the day of the home visit, and consented to participate in the integrated intervention and use of their data for research. The CHWs obtained verbal consent at home visits and documented consent in CommCare. We defined recently postpartum as women who were within one year of a live birth. There were no other inclusion or exclusion criteria. Individual and family socio-demographic data including age, caste, and household expenditure were collected at the time of enrolment.
We rolled out the integrated RMNCH intervention with the adapted BCS in February 2017. We used programmatic data collected from January to April 2018 as the post-intervention group. Our primary outcome was modern contraceptive use among recently postpartum women. We included data of women who had at least one CHW home visit during January to April 2018 were not pregnant on the day of the home visit, and were within one-year postpartum from a live birth. Women who had stillbirths were excluded from the analysis for both pre- and post-intervention groups, as there is limited evidence on optimal birth spacing after a stillbirth.31 Pre- and post-intervention data were collected by CHWs assigned to each ward. CHWs entered data into CommCare, which we subsequently exported for analysis. CHNs oversaw the data collection process via weekly team meetings and monthly supervision home visits. We initiated monthly data quality checks approximately six months into the implementation time period.
In April and May 2018, we conducted individual semi-structured interviews with CHWs, CHNs, women receiving the intervention, and husbands who were present for at least one of the contraceptive counselling sessions. We explored factors influencing contraceptive decision-making, participants’ impressions of the intervention, and perceived impact of the intervention on women’s use of modern methods. CHWs assisted in the recruitment of participants. A Nepali research analyst (author A.Tiwari), who was not a part of the care delivery team, collected verbal participant consent and conducted the interviews. We conducted all interviews in Nepali. The interviews were audio-recorded, transcribed, and translated into English, and coded in English.
Ethics approval and consent to participate
The study protocol was approved by the institutional review board of the Nepal Health Research Council (461/2016) and Brigham and Women's Hospital (2017P000709/PHS) The Boston Medical Center (H-38196) institutional review board exempted the study. The first author moved from Brigham and Women's Hospital to Boston Medical Center after the data collection process was already complete. At that point only de-identified data were being used for analysis and manuscript preparation. The study already had approval from the Nepal Health Research Council and Brigham and Women's institutional review boards; therefore Boston Medical Center did not feel that the primary author's scope of work constituted research activities that the institution was engaged in and exempted it.
Community health workers obtained verbal consent for participation in the pre-post study. Non-clinical research staff obtained verbal informed consent for the qualitative interviews. Verbal informed consent was obtained by non-clinical research staff members for qualitative interviews, during which consent to use de-identified quotes for publication purposes was obtained.
Data analysis
We performed bivariate analyses to examine characteristics that differed significantly between the pre- and post-intervention groups. We utilised T-tests and Wilcoxon rank-sum tests, where appropriate, for continuous variables and Fisher’s exact test for categorical variables. Socio-demographic characteristics included age, caste, and monthly household expenditure. Brahmin and Chhetri, traditionally considered to be privileged levels of the social stratification system, were classified as “upper”* and all other castes were classified as “other”.32 Additionally, we looked at the sex of child in the index pregnancy, time since delivery, and location of birth of the index pregnancy of the two groups. We included sex of child in the index pregnancy because son preference remains prevalent in Nepal and therefore may have influenced women’s desire for another pregnancy.33,34 We expected that contraceptive method mix would differ by time since delivery, as LAM is an effective method only in the early postpartum time period. We created a dichotomous variable for time from delivery to CHW visit or “time since delivery” in order to stratify our analysis by “early postpartum”, defined as 0–5 months after delivery and “late postpartum”, defined as 6–11 months after delivery. We included location of birth, as prior studies in similar settings suggested that non-institutional birth may be associated with socioeconomic vulnerability and structural barriers to healthcare access.35 We defined “institutional birth” as a delivery that took place at a public or private healthcare facility.
We utilised the definition of modern contraceptive methods as defined by the WHO. Withdrawal and rhythm methods were classified as traditional methods.20 We considered LAM to be an effective modern contraceptive method only if reported by women who were less than six months postpartum. Otherwise, they were reclassified as contraceptive non-users. Women who reported use of more than one contraceptive method were classified according to the most effective method they were using.
Adjusting for age, caste, monthly household expenditure, sex of child in the index pregnancy, and time since delivery, we used multivariable logistic regression to examine the use of modern contraception among postpartum women pre- and post-intervention. We first conducted the regression including all postpartum women and then we stratified by early and late postpartum time. Categorical variables for age and monthly household expenditure were used in the regression analysis as we expected non-linear relationships between these covariates and contraceptive use. We selected our covariates based on existing literature and content knowledge of the research team. All significant variables in the bivariate analyses were also included in the regression. We looked specifically at the impact of institutional birth on our planned outcome, as institutional birth rate (IBR) is a primary outcome of the integrated RMNCH study, within which this study is nested.18 We hypothesised that institutional birth may be a potential predictor for modern contraceptive use, as women who are able to reach a facility to deliver may be more likely to return to a facility to access contraception. Therefore, we compared our multivariable logistic regression models with and without IBR as a covariate in order to determine its impact on our primary outcome.
There was a 15-month gap between our pre- and post-intervention data collection time periods. Forty-eight women in the pre-intervention group had a subsequent short interval pregnancy and were within one year postpartum again during the post-intervention period. This accounted for 5% of the effective sample size. We compared our model using a function in the statistical software (PROC GENMOD) that accounted for these women as repeated measures to standard multivariable logistic regression that assumes independence of the two samples. As the two approaches yielded similar results with minimal difference in standard errors, we present only the results from standard logistic regression below.
All quantitative data analysis was performed using SAS version 9.4 (Cary, NC).
Qualitative data were manually coded and analysed using a thematic approach.36,37 Two researchers independently reviewed the data and developed initial codes, then collaboratively reconciled codes and developed the final codebook. Coded data were then grouped into thematic categories. Recurrent and emergent themes relevant to the research questions are summarised below.
Results
Quantitative results
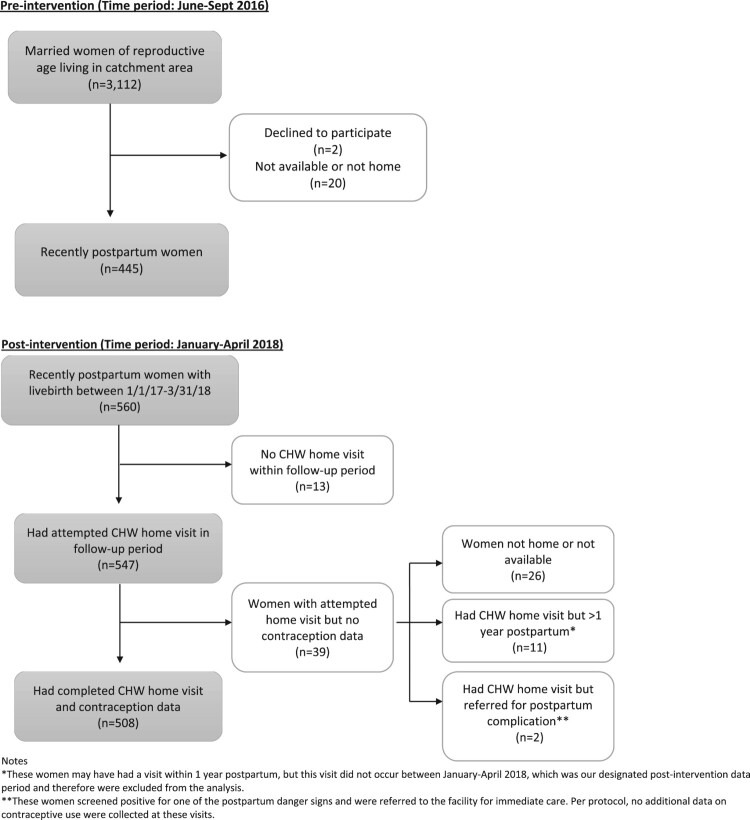
Between June and September 2016, 3112 married women of reproductive age were identified in Kamalbazaar and offered enrolment into the integrated RMNCH intervention. Two women declined to participate and 20 women were not home or unavailable (<1%). There were 445 recently postpartum women in the pre-intervention group and 508 in the post-intervention group (Figure 3). Women who were pregnant on the day of the CHW visit were excluded from the pre- and post-intervention groups. Eight women were excluded from the pre-intervention group and 2 women from the post-intervention group.
Figure 3.
Study enrolment
Socio-demographic characteristics of the pre- and post-intervention groups are presented in Table 1. Age and institutional birth rate were the only statistically different characteristics between the two groups. The majority of women in both groups were 20–34 years old, but in the post-intervention group there were more women in the 15–19 and 35–49 years age groups. IBR was 51% in the pre-intervention group and 82% in the post-intervention group (p < 0.0001). This was an anticipated increase as it was a desired programmatic outcome of the integrated RMNCH intervention. The two groups were similar in terms of caste, monthly household expenditure, sex of child in the index pregnancy, and time since delivery.
Table 1. Sample characteristics of pre- and post-intervention groups.
| Characteristic | Pre-intervention (n = 445) |
Post-intervention (n = 508)a |
|---|---|---|
| Age (years), median (Q1, Q3) | 25 (21, 30) | 24 (20, 30) |
| Age (years), n (%)* | ||
| 15–19 | 43 (10) | 87 (17) |
| 20–34 | 350 (79) | 325 (64) |
| 35–49 | 52 (12) | 96 (19) |
| Caste | ||
| “Upper” n (%) | 281 (63) | 323 (64) |
| Monthly household (HH) expenditureb, n (%) | ||
| <5000/month | 226 (51) | 238 (47) |
| 5000–9999/month | 155 (35) | 177 (35) |
| >/= 10,000/month | 64 (14) | 87 (17) |
| Sex of child in index pregnancy | ||
| Female, n (%) | 230 (52) | 237 (49) |
| Time since delivery (days), mean (SD) | 188 (107) | 193 (119) |
| Early postpartum (0-5 mo), n (%) | 215 (48) | 240 (47) |
| Institutional birth rate, n (%)* | 227 (51) | 414 (82) |
aForty-eight repeated measures. These are women who were in both the pre-intervention and post-intervention groups. Represents 5% of the total sample size.
bMonthly household expenditure measured in Nepali Rupees (NPR). 110 NPR = 1 USD
*Statistically significant (p < 0.05) differences between the two groups with Chi-square test.
Seventy-nine percent of women in the post-intervention group received balanced counselling at least one time in the postpartum period. Of the 508 women, seven were not offered balanced counselling (1.4%) and 101 declined counselling (20%). Postpartum modern contraceptive method use increased from 29% pre-intervention to 46% post-intervention (p < 0.0001) (Table 2). None of the women reported simultaneous use of more than one contraceptive method. In the pre-intervention group, 22/96 (23%) women who reported using LAM were more than 6 months postpartum. We reclassified these women as contraceptive non-users. In the post-intervention group, 4/139 (0.03%) women were similarly reclassified. In the unadjusted analysis, women in the post-intervention group had twice the odds of using a modern contraceptive method (OR = 2.1; CI 1.6, 2.7; p < 0.0001) as compared to the pre-intervention group. With respect to method mix, use of LAM, injectables, and implant increased significantly. Condom use decreased significantly from 4.5% to 1.6% (p = 0.01) (Table 2).
Table 2. Unadjusted modern contraceptive use and method mix pre- and post-intervention.
| Contraceptive Method | Pre-intervention (n = 445) n (%) |
Post-intervention (n = 508) n (%) |
p-value |
|---|---|---|---|
| Any modern method | 131 (29.4) | 235 (46.3) | <0.0001 |
| LAM | 74 (16.6) | 135 (26.6) | 0.003 |
| Condom | 20 (4.5) | 8 (1.6) | 0.01 |
| Combined oral pills | 2 (0.5) | 1 (0.2) | 0.6 |
| Injectables | 23 (5.2) | 63 (12.4) | <0.0001 |
| IUD | 5 (1.1) | 3 (0.6) | 0.48 |
| Implant | 2 (0.5) | 15 (3.0) | 0.003 |
| Female sterilisation | 3 (0.7) | 8 (1.6) | 0.24 |
| Male sterilisation | 2 (0.5) | 2 (0.4) | 1.00 |
| Non-use | 314 (70.6) | 273 (53.7) | <0.0001 |
| Traditional methods | 16 (3.6) | 9 (1.8) | 0.1 |
| None | 298 (67) | 264 (52.0) | <0.0001 |
When adjusted for age, caste, and monthly household expenditure at the time of enrolment, time since delivery, and sex of child in the index pregnancy, the difference in modern contraceptive use pre- and post-intervention remained significant. The adjusted OR for any modern contraceptive use of women in the post-intervention group as compared to pre-intervention group was 2.3 (CI 1.7, 3.1; p < 0.0001). When we added IBR as an additional covariate, we found the adjusted OR of modern contraceptive remained similar: 2.2 (CI 1.6, 2.9; p < 0.0001). Of the contraceptive non-users in the post-intervention group, 72% stated it was because their “husbands were away”.
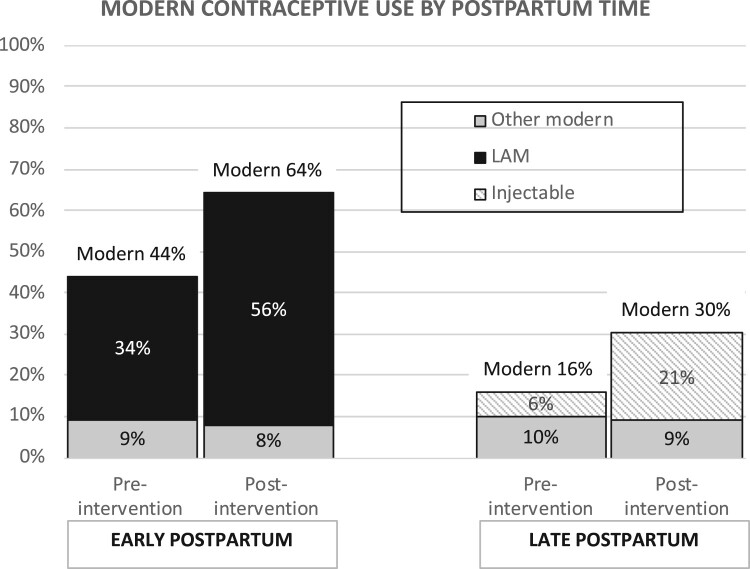
The regression analysis showed that women in the early postpartum period had almost four times the odds of using a modern contraceptive method as compared to those in the late postpartum period. In a stratified sub-analysis of modern contraceptive use by time since delivery, early postpartum women in the pre-intervention group had a 44% modern contraceptive use rate as compared to 64% in the post-intervention group (p < 0.0001) (Figure 4). The increase in modern contraceptive use was mostly due to LAM, which increased from 34% to 56% (p < 0.0001). Adjusting for the same covariates as above, early postpartum women in the post-intervention group had 2.3 times the odds of using a modern contraceptive (CI 1.5, 3.5; p = 0.0001) as compared to women in the pre-intervention group (Table 3). In this group, women who are from households with monthly expenditure >10,000 Nepali Rupees had twice the odds (CI 1.1, 3.6; p = 0.02) of using a modern contraceptive method.
Figure 4.
Modern contraceptive use by time since delivery
Table 3. Multivariable logistic regression for modern contraceptive use by time since delivery.
| Variable | Early postpartum | Late postpartum | ||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Post-intervention (Ref: Pre-intervention) | 2.3** | 1.5, 3.5 | 2.0* | 1.3, 3.2 |
| Covariates | ||||
| Age (Ref: 15–19 years) | ||||
| Age 20–34 | 1.2 | 0.7, 2.2 | 0.6 | 0.4, 1.2 |
| Age 35–49 | 1.1 | 0.5, 2.2 | 0.6 | 0.3, 1.2 |
| Monthly HH expenditure, (NPR) (Ref: <5k/month) | ||||
| 5000–9999/month | 1.1 | 0.7, 1.7 | 1.0 | 0.6, 1.7 |
| >/=10,000/month | 2.0* | 1.1, 3.6 | 1.2 | 0.7, 2.2 |
| Caste (Ref: “other”) | ||||
| “Upper”, n (%) | 0.8 | 0.5, 1.2 | 1.3 | 0.8, 2.0 |
| Sex of child in index pregnancy (Ref: male) | ||||
| Female | 1.0 | 0.6, 1.4 | 1.2 | 0.8, 1.9 |
| Institutional Birth Rate (IBR), n (%) (Ref: home birth) | 1.1 | 0.7, 1.8 | 1.4 | 0.9, 2.3 |
*p-value <= 0.5.
**p-value <= 0.0001.
For women in the late postpartum period, modern contraceptive use increased from 16% pre-intervention to 30% post-intervention (p = 0.0002), with increase in injectable use accounting for the majority of the change (Figure 4). Injectable use for late postpartum women increased from 6% pre-intervention to 21% (p < 0.0001) post-intervention. Late postpartum women in the post-intervention group had twice the odds of using a modern contraceptive method (OR = 2; CI 1.3, 3.2; p = 0.003) as compared to the pre-intervention group (Table 3). For late postpartum women there was no difference in contraceptive use by expenditure group.
Qualitative results
We conducted ten individual interviews: three care providers, which included two community health nurses or CHNs and one community health worker or CHW, four women enrolled in the programme, and three husbands who were present for contraceptive counselling.
Contraceptive decision-making
Interviewees identified factors that influence contraceptive decision-making at individual, family, and systems levels, which are summarised in Supplemental File 1 with supporting participant quotes.
At the individual level, concern for side effects, reproductive intentions, and gaps in knowledge, influenced women’s contraceptive use. At the family level, attitudes and beliefs of husbands and mothers-in-laws were noted to be important factors. All women mentioned the need to involve spouses and/or other family members in the decision-making process. One woman described how son preference by her mother-in-law was a barrier to contraceptive use. Spouses being away from the home for long periods of time for work also affected women’s decisions regarding contraceptive initiation postpartum. Participants brought up challenges in predicting when husbands might return home. On a systemic level, interviewees identified lack of access due to physical distance from facilities, unpredictable facility closures and stock-outs, and limited availability of long-acting and permanent methods at lower level facilities as barriers.
Mechanisms of impact
The primary perceived mechanisms through which the intervention increased contraceptive use were knowledge transfer through counselling at home visits, demand generation, referrals to health facilities, and follow-up. Providers, women, and husbands all commented on how use of visual aids improved contraceptive counselling. As one husband put it, “The good thing was that they accompanied counselling with the cards. It made it easier to understand because the pictures would illustrate what she was saying” (Husband #3).
CHWs counselled on available methods, including the use of LAM and benefits of breastfeeding: “[The CHW] tells us that Copper-T works for 12 years, implant works for five years, and Depo works for three months … We know these things because of her” (Woman #2). CHWs focused on the criteria for effective LAM use and transitioning from LAM to another effective method: “She tells us … [LAM] works for 6 months if we exclusively breastfeed the baby without supplements. She also teaches that after 6 months or after the return of menses, we can start thinking about using injectables or doing sterilization” (Woman #1). CHW counselling also focused on birth spacing and limiting. As one woman stated, “My age is such that I can have 2–3 more babies. If there had been no program, if they had not come with counseling, we would have given birth to 3–4 more children” (Woman #3).
In addition, CHWs attempted to address perceptions of risk in their counselling. One CHN stated,
“Women misunderstand that inserting the big rubber [implants] will be painful and cause difficulty while working. They don’t know that it is tiny, made of plastic or rubber, and won’t cause any discomfort … Women get scared that it will sting as they have to move their hands up and down while working.” (CHN #1)
Data also suggested that women use the information provided to facilitate contraceptive decision-making: “[CHWs] do not pressure us … It is up to us to decide how many children we want to have. We have to know what is right for us … .” (Woman #1). As noted by one CHW, “We tell them about the benefits and side effects of each method. This eases their decision-making process because they can use our inputs in the decision-making process” (CHW).
The knowledge transfer extended to family members who participated in the counselling sessions along with the postpartum women. One woman reported:
“We knew nothing in the past. My mother-in-law did not know anything either … We have people in the village who give birth to more children after having 2–3 children. My in-laws now wonder why people continue to give birth so fast despite having many health facilities here. Even the attitudes of our in-laws have improved.” (Woman #4)
Knowledge transfer contributed to demand generation for contraceptive use. According to one husband, “People may not know about contraceptives and so they might not be using them. I think, after the implementation of this program things have changed for the better” (Husband #1). And one CHN explained,
“I think [contraceptive use] is increasing nowadays. The increase in knowledge of contraceptive methods may have contributed to the increase in contraceptive use rates, right? It is easier for [women] to choose when they learn about all the [contraceptive] methods in balanced counselling.” (CHN #1)
Participants reflected in general terms on how the longitudinal nature of the intervention, including the relationship with CHWs contributed to improving the health situation. One woman noted, “The volunteers come and provide counselling to us … They visit us frequently and check on us. They urge us to go to the hospital so that we will not have a problem in the future” (Woman #3). Another woman confirmed: “You come here every year to check what people are doing or if people are following your advice or not. This will automatically improve [the health situation]” (Woman #1). The relationship-building appeared to be mutual. One CHW expressed feeling an increased sense of commitment to the community she was working in: “When I fail to receive their calls, they tell me so … I didn't call people back in the past. After I started this job, I call them back as soon as I can, thinking that they might be in trouble” (CHW). The same CHW added, “They look for me when they need and ask for my counselling when their husbands are coming home” (CHW). One CHN reiterated the importance of referrals and follow-up:
“Only telling them about the available contraceptives won’t be sufficient. We have to tell them where they can get them. Our [CHWs] told them about how to access them … We have to follow up, for example, to see if they have been using the contraceptive … When we go for follow-up counselling, we have to ascertain that they have been using the contraceptive.” (CHN #2)
Intervention acceptability
The contraceptive counselling showed some acceptance by participants: “The information improves our lives, the lives of our children … You teach us and we teach our children” (Woman #4). Participants appreciated, and some even preferred, counselling in the home as opposed to the health facility. According to one husband, “It is better to provide counselling at home than at the health post because it will be cheaper as you do not have to pay for the bus … This is easier for us” (Husband #2). Another husband expressed, “ … [CHWs] come here and provide us with important information about family planning. I like what they say … I think it will be better for us and our children” (Husband #1).
More specifically, several women and their partners found the contraceptive counselling to be acceptable: “I think [contraceptive counseling] is a good method. Because of that, you can make a decision about what is the best method for you and what does not fit you” (Husband #2). All women and husbands interviewed perceived CHW counselling to be non-coercive. As one woman put it, “But you should go for whatever is suitable for you. There is no compulsion for you to choose a particular contraceptive. They have educated us about everything and urged us to go for what is suitable for us” (Woman #3).
Participants also noted several recommendations for ways to improve the programme, which are summarised in Supplemental File 2.
Discussion
This study evaluated the impact of an integrated RMNCH intervention, including use of the Balanced Counseling Strategy, delivered by CHWs at home visits, on postpartum modern contraceptive use in rural Nepal. Recently postpartum women post-intervention had twice the odds of using any modern contraceptive method compared to recently postpartum women pre-intervention. LAM accounted for the majority of modern contraceptive use in the early postpartum period and the rates of reported LAM increased significantly from pre- to post-intervention. In the late postpartum period, overall rates of modern contraceptive use were lower than the early postpartum period as many women do not transition from LAM to another effective method of contraception. Regardless, even in the late postpartum period, women post-intervention had twice the odds of using a modern contraceptive method compared to pre-intervention, with increased injectable use accounting for the majority of the increase.
Being in the highest household expenditure group was predictive of modern contraceptive use for early postpartum women, but not for late postpartum women. Given that LAM was the primary modern method used by early postpartum women, we presume that being in the highest expenditure group was associated with higher odds of LAM use. Prior studies in Nepal have not demonstrated a consistent relationship between socioeconomic status and breastfeeding practices.38–40 In one study, higher socioeconomic status was associated with higher rates of any modern contraceptive use for rural women in Nepal, but it was not specific to postpartum women and LAM was not included as a method in the study.41 Wealth is correlated with higher education and literacy level, which may be associated with better knowledge of LAM and higher rates of self-report.9 In addition, women from wealthier families are less likely to work in the agriculture sector and their husbands are less likely to be away for work.9 Perhaps these women spend less time in the field away from their babies and have increased social support from their husbands, which may facilitate exclusive breastfeeding.9
The primary reason that women in the post-intervention group mentioned for not using contraception was that their husbands were away. In Province 7, 36.5% of married women cited that their spouses were away, with more than 50% away for greater than 12 months.9 It may be unpredictable when husbands will return home and, as described in the qualitative data, this plays a role in contraceptive choice. In this setting, women’s self-perceived risks for pregnancy and need for contraception may fluctuate more than a demographically stable population.42,43 This rationale may contribute to low uptake of long-acting contraceptive methods. While implant use did increase significantly from pre- to post-intervention, the absolute numbers were small. The study was not powered to detect a difference in long-acting and permanent methods used. Of note, condom use decreased between the pre- and post-interventions groups. It is possible that condom use decreased because women opted for an alternative method or there is under-reporting of dual contraceptive use. Given the importance of condom use in protecting against sexually transmitted infections, perhaps CHW counselling should include more directed discussion of dual contraceptive use.
Opinions of spouses and family members emerged as important influencers of contraceptive use. None of the women interviewed thought of contraceptive decision-making as solely an individual decision. While women noted increased knowledge helped to facilitate their ability to make decisions on contraceptive use, many women in this context have limited agency and require permission from husbands and other family members.44,45 Although with women’s consent, CHWs tried to encourage husbands to be present for counselling, spouses are often not at home. Additional directed efforts are needed to involve male partners and other family members.46 Women’s limited agency may also be reflected in their reluctance to answer open-ended questions related to how to improve the current situation and our intervention. Notably, providers and husbands provided the majority of the recommendations for programme improvements (Supplemental File 1). Future research is needed to determine how best to achieve shared decision-making in this context and support women in meeting their reproductive goals.
Demand generation, knowledge transfer, referrals to healthcare facilities, and follow-up were the primary mechanisms by which the intervention affected modern contraceptive use. CHW counselling helped to facilitate women’s contraceptive decision-making by taking into account each woman’s individual circumstances and reproductive intentions. All participants noted lack of coercion in the CHW counselling.47 One important feature of the intervention was longitudinal care initiated antepartum continuing through the first year postpartum. This longitudinal care is likely to be important in addressing women’s changing needs for contraception during the first year postpartum and allowing for CHWs to tailor counselling accordingly. For instance, the unpredictable nature and timing of when husbands return home necessitates long-term follow-up to assist women in anticipating their shifting contraceptive needs. The transition from LAM to another effective contraceptive method also appears to be a critical time for decisional support. The majority of women reported using LAM during the first six months postpartum, but we were unable to confirm whether women met the criteria for exclusive breastfeeding and postpartum amenorrhea. National data indicates only 41% of women are exclusively breastfeeding by 4–5 months postpartum. The median duration of postpartum amenorrhea is six months.9 This suggests that CHW counselling should include more directed conversations on the transition from LAM to another method earlier in the postpartum period and emphasis that LAM use can be continued as another method is initiated. Since the time of this publication the integrated intervention has shifted to include a visit for women at three months postpartum when family planning counselling can occur.
Our findings are consistent with prior literature that supports continuity of care for women at multiple contact points across the continuum of reproductive healthcare as opposed to isolated counselling sessions in improving postpartum contraceptive use.10–12 The longitudinal care model facilitates development of relationships between CHWs and the communities they serve and responds to women’s shifting contraceptive needs during the first year postpartum. Better characterisation of the fluid nature of contraceptive need in settings with high rates of migration will help improve future interventions. Furthermore, while our findings suggest that demand generation interventions can contribute to increases in modern contraceptive use, structural barriers to access remain and need to be concurrently addressed. Given the strong influence of spouses and family members on women’s contraceptive decision-making, demand generation interventions focused on women alone are inadequate. Further consideration of factors that influence women’s reproductive decision-making, including agency and the role of family, can help providers further tailor their counselling, improve quality of care, and work towards shared decision-making.
To our knowledge this is the first intervention of this kind in rural Nepal. Our study adds to the existing evidence base supporting community-level postpartum family planning interventions and offers an example of an intervention integrated into a broader RMNCH programme.13,48 This community-based strategy may inform Nepal’s efforts to improve counselling and access to postpartum contraception. Furthermore, designed as a component of a national pilot, these study findings have the potential to inform Nepal’s national strategy in use of CHWs to reach rural populations. A well-deployed and well-supervised cadre of CHWs will likely feature prominently in strategies to achieve universal sexual and reproductive healthcare coverage and this study presents one possible model for implementation. Future analyses from the integrated RMNCH intervention will evaluate the impact on contraceptive continuation rates, post-abortion contraceptive use, and institutional birth. This model is currently being implemented in a second district within Nepal and final recommendations from the integrated intervention are expected to be available for the Ministry of Health and Population in early 2021.
Limitations
There are several limitations to this study. We chose to implement the intervention for all married women in our catchment area, given the relatively poor maternal health indicators in the study context and the known efficacy of modern contraceptive methods. Without a control group, we cannot account for secular trends and causal inference is difficult to establish. Furthermore, as this is an integrated intervention it is difficult to isolate whether a specific component of the intervention or the combined effect of the integrated intervention led to our primary outcome. All women included in the analysis received at least one CHW home visit, but only 79% of women received balanced counselling. Anecdotally, CHWs stated that they sometimes conducted BCS counselling for women during months that were not the intervention designated PNC months 1, 5, or 10. Due to the design of the initial forms, these additional counselling sessions would not have been recorded. Some of the 21% of women who were documented as declining the BCS may have received it during other PNC months. Since this publication, we have made changes to CommCare to allow for more flexibility for CHWs to document when they provide the BCS. It is also worthwhile to note that in our study area, we did not implement group antenatal care and home-based child visits, which are additional components of the integrated RMNCH intervention, until September and December 2017, respectively. Therefore, given the time period when our follow-up data were collected, these additional components of the intervention likely had minimal contribution to the primary outcome.
We relied on self-reported contraceptive use data collected by CHWs for our primary outcome. Data collection by CHWs who also delivered care may have introduced social desirability bias that led to overestimation of contraceptive use. Self-reported data are particularly problematic in the interpretation of LAM use.49 While we limited LAM use to the first six months postpartum in our analysis, we did not verify whether reported LAM users met the additional criteria of exclusive breastfeeding and postpartum amenorrhea. Conversely, we were unable to account for women who met the criteria for effective LAM use, but self-reported as contraceptive non-users. Compared to pre-intervention, fewer late postpartum women post-intervention reported LAM use and were reclassified as contraceptive non-users. This is likely due to improved education around LAM as a part of the intervention. Given these limitations, it is difficult to determine whether the increase between the pre- and post-intervention groups represents a true increase in the practice of LAM or the result of improved self-reporting. Future analyses should attempt to account for differences in self-reported LAM and correct-practice LAM use as well as actual increases in exclusive breastfeeding rates.
We used programmatic data as our data source. The intervention evolved iteratively with the implementation process, which led to changes in workflows and collection forms, as well as the addition of new programmatic elements. This resulted in challenges with data processing and analysis. Data on educational level and overall parity (beyond recent two-year birth histories) were not collected on the initial versions of the mobile application. The implementation of routine data quality checks halfway through the first year of the intervention, for both research and programmatic purposes, significantly improved data quality.
In our study setting, structural forces, including poverty, gender inequality, poor road infrastructure, weak supply chains, and limited number of healthcare workers, play a major role in health outcomes.50 Facility and systemic level issues mentioned by participants in the qualitative interviews such as supply chain deficiencies, transportations barriers, and limited access to long-acting contraceptive methods, were not directly addressed by this intervention. While our intervention strengthens counselling and support for individual women and linkages between the community and facility-based care, it does not address significant upstream forces that limit the impact of downstream interventions. Nyaya Health Nepal is working with government partners to improve facility-based care in conjunction with community-based efforts in the long-term.
Supplementary Material
Acknowledgements
We wish to express our appreciation to the Nepal Ministry of Health and Population for their continued efforts to improve the public sector healthcare system in rural Nepal. We wish to give our thanks to the Population Council for developing the Balanced Counselling Strategy, to Dr Deeb Shrestha Dangol and colleagues at Ipas for input in adapting the intervention, and to our technology partners ThoughtWorks and Dimagi. Lastly, we are indebted to the community health workers and community health nurses whose commitment to serving our patients and dedication to improving reproductive, maternal, newborn, and child health outcomes in rural Nepal continue to inspire us.
Funding Statement
The research study is funded by the United States Agency for International Development (US) via a Partnerships for Enhanced Engagement in Research award (sponsor grant number AID-OAA-A-11-00012, National Academy of Science sub-award letter 2000007780). WW received support through a combined Global Women’s Health and Family Planning Fellowship that is funded by the Society of Family Planning Research Fund (grant number SFPRF17-10). The funders played no role in research design, data collection, data analysis, manuscript write-up, or decision to publish. Any opinions, findings, conclusions, or recommendations expressed in this article are those of the authors alone, and do not necessarily reflect the views of the United States Agency for International Development or the National Academy of Science.
Footnotes
Brahmin and Chhetri people are at the top of the social hierarchy. Historically, they have had more opportunities for education, held more respected occupations, and enjoyed higher socioeconomic status, than socially excluded “lower” castes. Although the caste system is not formally enforced in modern Nepal, Brahmins and Chhetris still disproportionately hold senior positions, usually have higher socioeconomic status, and in some studies have better health outcomes.
Author contributions
WW conceived the study and serves as guarantor for the work. The study grew out of discussions between WW, SM, IB, IN, AG, A. Thapa, DC, DM, SH, and S. Sapkota. RB, S. Saud, HJR, SP, and LK assisted with implementation of the intervention. A. Tiwari conducted the qualitative data collection and assisted with data analysis. SM, NC, DM, DB also assisted with data analysis. WW, SM, and A. Tiwari drafted the manuscript. All authors have reviewed and approved the manuscript.
Disclosure statement
WW is employed at an academic medical centre (Boston Medical Center) that receives public sector research funding, as well as revenue through private sector fee-for-service medical transactions and private foundation grants. WW is a faculty member at a private university (Boston University School of Medicine). A Tiwari, RB, DC, HJR, S. Sapkota, S. Saud, and A Thapa are employed by and WW, NC, SH, DM, and SM work in partnership with a non-profit healthcare organisation (Nyaya Health Nepal with support from a partner United States-based 501c3 Possible) that delivers free healthcare in rural Nepal using funds from the Government of Nepal and other public, philanthropic, and private foundation sources. DC is a faculty member at and employed part-time by a public university (University of Washington). At the time of programme implementation, IN, IB, LK, and SP were employed by Nyaya Health Nepal. NC is employed full-time and SH is employed part-time at a private university (Icahn School of Medicine at Mount Sinai). IB is employed by the Government of Nepal. IN is a student at a private university (Harvard TH Chan School of Public Health) and a member on the Board of Directors with Possible, a position for which she receives no compensation. DM and SM are faculty members at a private university (Icahn School of Medicine at Mount Sinai). DM is a non-voting member on the Board of Directors with Nyaya Health Nepal, a position for which he receives no compensation. AG is employed at an academic medical centre (Brigham and Women’s Hospital) and a non-profit organisation (Planned Parenthood League of Massachusetts) that provides reproductive healthcare in the United States and globally using public, philanthropic, and private foundation sources. All authors have read and understood Sexual and Reproductive Health Matters policy on declaration of interests, and declare that we have no competing financial interests. The authors do, however, believe strongly that healthcare is a public good, not a private commodity.
Data availability statement
De-identified quantitative data are available on request by emailing: research@possiblehealth.org and will be posted in a publicly-accessible data repository. Full transcripts of qualitative data are not available as they contain quotes and identifiable information that could compromise the identity of participants.
References
- 1.Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC.. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295(15):1809–1823. doi: 10.1001/jama.295.15.1809 [DOI] [PubMed] [Google Scholar]
- 2.Conde-Agudelo A, Rosas-Bermudez A, Kafury-Goeta AC.. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol. 2007;196(4):297–308. doi: 10.1016/j.ajog.2006.05.055 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) . Report of a WHO technical consultation on birth spacing, 2005. Geneva: WHO; 2007. [Google Scholar]
- 4.Moore Z, Pfitzer A, Gubin R, et al. Missed opportunities for family planning: an analysis of pregnancy risk and contraceptive method use among postpartum women in 21 low- and middle-income countries. Contraception. 2015;92(1):31–39. doi: 10.1016/j.contraception.2015.03.007 [DOI] [PubMed] [Google Scholar]
- 5.Hardee K, Newman K, Bakamjian L, et al. Voluntary family planning programs that respect, protect, and fulfill human rights: a conceptual framework. Washington (DC: ): Futures Group; 2013. [Google Scholar]
- 6.Starbird E, Norton M, Marcus R.. Investing in family planning: Key to achieving the Sustainable Development goals. Glob Health Sci Pract. 2016;4(2):191-210. doi: 10.9745/GHSP-D-15-00374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galati A. Onward to 2030: Sexual and reproductive health and rights in the context of the sustainable development goals. Guttmacher Policy Rev. 2015;18(4):77–84. [Google Scholar]
- 8.Mehata S, Paudel YR, Mehta R, et al. Unmet need for family planning in Nepal during the first two years postpartum. Biomed Res Int. 2014;2014:649567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health and Population, New ERA, ICF International Inc . Nepal demographic and health Survey 2016. Kathmandu: Ministry of Health and Population; 2017. [Google Scholar]
- 10.Dev R, Kohler P, Feder M, et al. A systematic review and meta-analysis of postpartum contraceptive use among women in low-and middle-income countries. Reprod Health. 2019;16:154. doi: 10.1186/s12978-019-0824-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cleland J, Shah IH, Daniele M.. Interventions to improve postpartum family planning in low- and middle-income countries: program implications and research priorities. Stud Fam Plann. 2015;46(4):423–441. doi: 10.1111/j.1728-4465.2015.00041.x [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) . Programming strategies for postpartum family plannng. Geneva: WHO; 2013. [Google Scholar]
- 13.Blazer C, Prata N.. Postpartum family planning: current evidence on successful interventions. Open Access J Contracept. 2016;7:53–67. doi: 10.2147/OAJC.S98817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mehata S, Paudel YR, Dariang M, et al. Trends and inequalities in use of maternal health care services in Nepal: strategy in the search for improvements. Biomed Res Int. 2017;2017:5079234. doi: 10.1155/2017/5079234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Citrin D, Thapa P, Nirola I, et al. Developing and deploying a community healthcare worker-driven, digitally-enabled integrated care system for municipalities in rural Nepal. Healthc (Amst). 2018;6(3):197–204. doi: 10.1016/j.hjdsi.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maru DS, Andrews J, Schwarz D, et al. Crossing the quality chasm in resource-limited settings. Global Health. 2012;8:41. doi: 10.1186/1744-8603-8-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwarz D, Sharma R, Bashyal C, et al. Strengthening Nepal's female community health volunteer network: a qualitative study of experiences at two years. BMC Health Serv Res. 2014;14:473. doi: 10.1186/1472-6963-14-473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maru S, Nirola I, Thapa A, et al. An integrated community health worker intervention in rural Nepal: a type 2 hybrid effectiveness-implementation study protocol. Implement Sci. 2018;13(1):53. doi: 10.1186/s13012-018-0741-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma P, Guha-Khasnobis B, Khanal DR.. Nepal human development report 2014: beyond geography, unlocking human potential. Kathmandu: Government of Nepal National Planning Commission; 2014. [Google Scholar]
- 20.World Health Organization (WHO) . Family planning/Contraception Factsheet, 2018. [cited 2019 Feb 11]. Available from:https://www.who.int/en/news-room/fact-sheets/detail/family-planning-contraception.
- 21.Ministry of Health and Population . Female community health volunteer national survey. Kathmandu: Ministry of Health and Population; 2014. [Google Scholar]
- 22.Population Council . The balanced counseling strategy plus: a toolkit for family planning service providers working in high STI/HIV prevalence settings. 3rd ed. Washington (DC: ): Population Council; 2015. [Google Scholar]
- 23.Agarwal S, Lasway C, L'Engle K, et al. Family planning counseling in your Pocket: A mobile Job Aid for community health workers in Tanzania. Glob Health Sci Pract. 2016;4(2):300–310. doi: 10.9745/GHSP-D-15-00393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liambila W, Warren C, Mullick S, et al. Feasibility, acceptability, effect, and cost of integrating counseling and testing for HIV within family planning services in Kenya. Washington (DC: ): Population Council; 2008. [Google Scholar]
- 25.Sapkota S, Rajbhandary R, Lohani S.. The impact of balanced counseling on contraceptive method choice and Determinants of long acting and reversible contraceptive continuation in Nepal. Matern Child Health J. 2017;21(9):1713–1723. doi: 10.1007/s10995-016-1920-5 [DOI] [PubMed] [Google Scholar]
- 26.Dimagi . CommCare. [cited 2019 Oct 4]. Available from: https://www.dimagi.com/commcare/.
- 27.Dehlendorf C, Krajewski C, Borrero S.. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57(4):659–673. doi: 10.1097/GRF.0000000000000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holt K, Zavala I, Quintero X, et al. Women's preferences for contraceptive counseling in Mexico: results from a focus group study. Reprod Health. 2018;15(1):128. doi: 10.1186/s12978-018-0569-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dehlendorf C, Grumbach K, Schmittdiel JA, et al. Shared decision making in contraceptive counseling. Contraception. 2017;95(5):452–455. doi: 10.1016/j.contraception.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thapa P, Bangura AH, Nirola I, et al. The power of peers: an effectiveness evaluation of a cluster-controlled trial of group antenatal care in rural Nepal. Reprod Health. 2019;16(1):150. doi: 10.1186/s12978-019-0820-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kopp DM, Bula A, Maman S, et al. Influences on birth spacing intentions and desired interventions among women who have experienced a poor obstetric outcome in Lilongwe Malawi: a qualitative study. BMC Pregnancy Childbirth. 2018;18(1):197. doi: 10.1186/s12884-018-1835-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bennett L, Dahal DR, Govindasamy P.. Caste, Ethnic, and Regional identity in Nepal: further analysis of the 2006 Nepal demographic and health survey. Calverton (MD: ): Macro Internal Inc; 2008. [Google Scholar]
- 33.Puri M, Tamang A.. Understanding factors influencing adverse sex ratios at birth and exploring what works to achieve balance: the situation in selected districts of Nepal Kathmandu, Nepal. CREPHA; 2015.
- 34.Leone T, Matthews Z, Dalla Zuanna G.. Impact and determinants of sex preference in Nepal. Int Fam Plan Perspect. 2003;29(2):69–75. doi: 10.2307/3181060 [DOI] [PubMed] [Google Scholar]
- 35.Maru S, Rajeev S, Pokhrel R, et al. Determinants of institutional birth among women in rural Nepal: a mixed-methods cross-sectional study. BMC Pregnancy Childbirth. 2016;16:252. doi: 10.1186/s12884-016-1022-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pope C, Ziebland S, Mays N.. Qualitative research in health care. Analysing qualitative data. Br Med J. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ulin PR, Robinson ET, Tolley EE.. Qualitative methods in public health: a field guide for applied research. 1st ed. San Francisco (CA: ): Jossey-Bass; 2005. [Google Scholar]
- 38.Adhikari M, Khanal V, Karkee R, et al. Factors associated with early initiation of breastfeeding among Nepalese mothers: further analysis of Nepal demographic and health survey, 2011. Int Breastfeed J. 2014;9(1):21. doi: 10.1186/s13006-014-0021-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhandari S, Thorne-Lyman AL, Shrestha B, et al. Determinants of infant breastfeeding practices in Nepal: a national study. Int Breastfeed J. 2019;14:14. doi: 10.1186/s13006-019-0208-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khanal V, Scott JA, Lee AH, et al. Factors associated with early initiation of breastfeeding in Western Nepal. Int J Environ Res Public Health. 2015;12(8):9562–9574. doi: 10.3390/ijerph120809562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang W, Alva S, Winter R, et al. Contextual influences of modern contraceptive use among rural women in Rwanda and Nepal. DHS Analytical studies No. 41. Calverton (MD: ): ICF International; 2013. [Google Scholar]
- 42.Shattuck D, Wasti SP, Limbu N, et al. Men on the move and the wives left behind: the impact of migration on family planning in Nepal. Sex Reprod Health Matters. 2019;27(1):1647398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hendrickson ZM, Owczarzak J, Lohani S, et al. The (re)productive work of labour migration: the reproductive lives of women with an absent spouse in the central hill region of Nepal. Cult Health Sex. 2019;21(6):684–700. doi: 10.1080/13691058.2018.1510546 [DOI] [PubMed] [Google Scholar]
- 44.Senarath U, Gunawardena NS.. Women's autonomy in decision making for health care in South Asia. Asia Pac J Public Health. 2009;21(2):137–143. doi: 10.1177/1010539509331590 [DOI] [PubMed] [Google Scholar]
- 45.Thapa K, Dhital R, Rajbhandari S, et al. Factors affecting the behavior outcomes on post-partum intrauterine contraceptive device uptake and continuation in Nepal: a qualitative study. BMC Pregnancy Childbirth. 2019;19(1):148. doi: 10.1186/s12884-019-2310-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harrington EK, McCoy EE, Drake AL, et al. Engaging men in an mHealth approach to support postpartum family planning among couples in Kenya: a qualitative study. Reprod Health. 2019;16(1):17. doi: 10.1186/s12978-019-0669-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Senderowicz L. I was obligated to accept: a qualitative exploration of contraceptive coercion. Soc Sci Med. 2019;239:112531. doi: 10.1016/j.socscimed.2019.112531 [DOI] [PubMed] [Google Scholar]
- 48.Scott VK, Gottschalk LB, Wright KQ, et al. Community health workers’ provision of family planning services in low- and middle-income countries: a systematic review of effectiveness. Stud Fam Plann. 2015;46(3):241–261. doi: 10.1111/j.1728-4465.2015.00028.x [DOI] [PubMed] [Google Scholar]
- 49.Fabic MS, Choi Y.. Assessing the quality of data regarding use of the lactational amenorrhea method. Stud Fam Plann. 2013;44(2):205–221. doi: 10.1111/j.1728-4465.2013.00353.x [DOI] [PubMed] [Google Scholar]
- 50.Farmer PE, Nizeye B, Stulac S, et al. Structural violence and clinical medicine. PLoS Med. 2006;3(10):e449. doi: 10.1371/journal.pmed.0030449 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
De-identified quantitative data are available on request by emailing: research@possiblehealth.org and will be posted in a publicly-accessible data repository. Full transcripts of qualitative data are not available as they contain quotes and identifiable information that could compromise the identity of participants.