Abstract
Evidence of the health system challenges to promoting respectful maternity care (RMC) is limited in Ethiopia and globally. This study investigated the health system constraints to RMC in three Southern Ethiopian hospitals. We conducted a qualitative study (7 focus group discussions (FGDs) with providers of RMC and 12 in-depth interviews with focal persons and managers) before and after the implementation of an RMC intervention. We positioned childbirth services within the health system and applied complex adaptive system theory to analyse the opportunities and constraints to the promotion of RMC. Both system “hardware” and “software” factors influencing the promotion of RMC were identified, and their interaction was complex. The “hardware” factors included bed availability, infrastructure and supplies, financing, and health workforce. “Software” factors encompassed service providers’ mindset, staff motivation, and awareness of RMC. Interactions between these factors included privacy breaches for women when birth companions were admitted in labour rooms. Delayed reimbursement following the introduction of fee-exemption for maternity services resulted in depleted revenues, supply shortages, and ultimately disrespectful behaviour among providers. Other financial constraints, including the insufficient and delayed release of funds, also led to complex interactions with the motivation of staff and the availability of workforce and supplies, resulting in poor adherence to RMC guidance. Interventions aimed at improving only behavioural components fall short of mitigating the mistreatment of women. System-wide interventions are required to address the complex interactions that constraint RMC.
Keywords: respectful maternity care, health system, complex adaptive system, system hardware, system software
Résumé
Les données sur les difficultés rencontrées par le système de santé pour promouvoir des soins de maternité respectueux sont restreintes en Éthiopie et dans le monde. Cette étude a enquêté sur les obstacles du système de santé qui contrarient des soins de maternité respectueux dans trois hôpitaux du sud de l’Éthiopie. Nous avons mené une étude qualitative (sept discussions par groupe d’intérêt avec des prestataires de soins et 12 entretiens approfondis avec des agents de liaison et des gestionnaires) avant et après la mise en œuvre d’une intervention de soins de maternité respectueux. Nous avons positionné les services d’obstétrique dans le système de santé et appliqué une théorie de systèmes complexes adaptatifs pour analyser les possibilités et les limitations de la promotion de soins de maternité respectueux. Des facteurs aussi bien matériels qu’immatériels influençant la promotion de soins de maternité respectueux ont été identifiés et leur interaction était complexe. Les facteurs «matériels» comprenaient la disponibilité de lits, les infrastructures et les fournitures, le financement et le personnel de santé. Les facteurs «immatériels» englobaient l’état d’esprit des prestataires de services, la motivation du personnel et la connaissance des soins de maternité respectueux. Parmi les interactions entre ces facteurs figuraient des violations de l’intimité des femmes lors de l’admission d’accompagnants dans les salles d’accouchement. Les délais dans les remboursements après l’introduction de l’exonération des frais pour les services de maternité ont provoqué une baisse des revenus, des pénuries de fournitures et, en fin de compte, un comportement irrespectueux des prestataires. D’autres obstacles financiers, notamment le décaissement tardif de fonds insuffisants, ont aussi provoqué des interactions complexes avec la motivation du personnel et la disponibilité du personnel de santé et des fournitures, ce qui a abouti à une piètre observance des conseils sur des soins de maternité respectueux. Les interventions visant à améliorer uniquement les composantes comportementales ne suffisent pas pour atténuer les mauvais traitements subis par les femmes. Des mesures englobant l’ensemble du système sont nécessaires pour s’attaquer aux interactions complexes qui limitent les soins de maternité respectueux.
Resumen
En Etiopía y mundialmente existe evidencia limitada de los retos que enfrenta el sistema de salud para promover atención respetuosa de la maternidad (ARM). Este estudio investigó las limitaciones del sistema de salud con relación a la ARM en tres hospitales de Etiopía meridional. Realizamos un estudio cualitativo (siete discusiones en grupos focales con prestadores de servicios de ARM y 12 entrevistas a profundidad con personas focales y administradores) antes y después de la ejecución de la intervención de ARM. Posicionamos los servicios de atención durante el parto dentro del sistema de salud y aplicamos la teoría del sistema adaptativo complejo para analizar las oportunidades y limitaciones para promover ARM. Se identificaron los factores de “hardware” y “software” del sistema que influyen en la promoción de ARM, y su interacción era compleja. Los factores de “hardware” eran: disponibilidad de camas, infraestructura y suministros, financiamiento y fuerza laboral de salud. Los factores de “software” abarcaban la mentalidad de los prestadores de servicios, la motivación del personal y la conciencia de ARM. Un ejemplo de las interacciones entre estos factores era el incumplimiento de privacidad de las mujeres al admitir acompañantes del parto en las salas de parto. El reembolso retrasado después de la introducción de exención de tarifas por servicios de atención de la maternidad causó agotamiento de ingresos, escasez de suministros y comportamiento irrespetuoso entre prestadores de servicios. Otras limitaciones financieras, entre ellas la insuficiente y retrasada liberación de fondos, también propiciaron complejas interacciones con la motivación del personal y la disponibilidad de fuerza laboral y suministros, lo cual produjo incumplimiento de la orientación sobre ARM. Las intervenciones destinadas a mejorar solo los componentes conductuales no llegan a mitigar el maltrato de las mujeres. Para abordar las complejas interacciones que limitan la ARM, es necesario ejecutar intervenciones en todo el sistema.
Introduction
Despite the implementation of a range of maternal health interventions, maternal mortality remains high in many low- and-middle-income countries (LMICs), including those of sub-Saharan Africa.1 Key to achieving the sustainable development goal target of reducing the global maternal mortality ratio to 70 per 100,000 live births by 20302 is improving the quality of both clinical and non-clinical care women receive during the time of pregnancy, childbirth, and in the immediate postpartum period.3
The World Health Organization (WHO) defines the quality of care as “the extent to which health care services provided to individuals and patient populations improve desired health outcomes” and outlines that safety, effectiveness, timeliness, efficiency, equity, and people-centredness of health services are integral to achieving quality.4 Applying this definition to maternal and newborn health services helps to view quality from two standpoints: quality from the perspective of the provision of care (clinical care) and quality from the perspective of how women and their families experienced the care (interpersonal care).5 Historically, however, most quality improvement interventions have focused on the clinical dimensions of maternity care while overlooking the interpersonal and social aspects of care.6
The mistreatment of women during facility-based childbirth has been reported as both a violation of women’s human rights and a significant deterrent to the utilisation of skilled birth services.7–9 Several studies from sub-Saharan Africa, including WHO-led studies, reported high levels10,11 and diverse manifestations7,12 of the mistreatment of women. Similarly, the worryingly high level of mistreatment of women in Ethiopia13–16 highlights the need for a focused strategy if the country is to improve maternal health and reduce maternal mortality. In 2019, only 47.5% of pregnant women gave birth in health facilities in Ethiopia although 74% of pregnant women received at least one antenatal care visit from a skilled provider.17 A portion of this missed opportunity may be addressed by preventing the mistreatment of women.7,18
Respectful maternity care (RMC) is one of the eight domains of WHO’s framework for quality of maternal and newborn health care and refers to care that includes the right to dignity; respect; privacy; confidentiality; equality; informed consent; autonomy; and timeliness.5,19 Additionally, within the 2018 WHO Intrapartum Care for Positive Childbirth Experience recommendations, RMC is recommended to improve the quality and woman-centredness of care during childbirth.8 In addition to framing these recommendations, there should be a mechanism for fostering accountability to achieve sustainable change.20 These efforts need to happen in the context of comprehensive quality of care improvements, including the technical dimension.21
Given the diverse contributors to the mistreatment of women during childbirth,22 system complexity-informed strategies need to be designed to advance context-specific and evidence-based maternal health interventions.3 Although RMC, as a non-clinical aspect of quality care,5 relies on the practice of service providers, it is open to the interactions between other system components such as infrastructure, information and referral systems, financing, and motivation, among others.23,24
Positioning RMC in a complex system helps to explore the constraints and patterns of interaction between system elements that directly or indirectly affect the delivery of RMC in health facilities.25 In this study, the maternity care system is regarded as a complex adaptive system. Accordingly, the concepts of complex adaptive systems were used to guide data analysis and interpretation of the findings of this study.26
The concepts of complexity science are rooted in disciplines including biology, chemistry, physics, and sociology, among others. Consequently, several theories including evolutionary theory in biology, self-organisation theory in chemistry, and chaos theory in mathematics contributed to the complexity science construct, the latter resulting in a heightened interest in complexity science among social scientists to study change, evolution, adaptive, and emergent behaviours in social and organisational phenomena such as healthcare.27–29 Complexity science resulted in the paradigm shift from the linear cause and effect inquiry underlying traditional formal approaches, to synthetic reasoning and modelling of complex systems.27
A complex adaptive system is a dynamic system that consists of a wide variety of elements, and in which the behaviour of each is responsive to the actions of others within the system (adaptive); interactions are nonlinear; and responses or changes are unpredictable (complex).23,26,28 Table 1 shows a brief description of selected complex adaptive system concepts. Nonlinearity refers to the heterogeneous and multiple levels of interaction between system agents which makes system behaviour unpredictable.26,30 Small changes in inputs may lead to large changes in outputs. Conversely, large changes in inputs may result in small changes in output.28 Gear and colleagues describe feedback loops as “recursive mechanisms arising from multiple agent interactions over time that either reinforce (positive) or undermine (negative) each other. Positive feedback loops support a change trajectory while negative feedback loops tend to undermine or negate change”.26 When system elements interact, the system displays a new aggregate behaviour that cannot be seen at the individual element level. This property is called emergence23,26 and such repeated interactions over time make the system adapt to the behaviour of its elements; this is labelled as self-organisation.28 Sometimes, past system events or circumstances manifest their desirable or undesirable influence on current system behaviours or events – path dependence.30,31
Table 1.
Description of important concepts
| Concepts | Description* |
|---|---|
| Complex adaptive system | A type of system which comprises diverse agents (complex), and where the behaviour of each agent is responsive to the interactions with other agents within the system (adaptive) |
| Self-organisation | The way in which agents interact to coordinate their own forms, or patterns of behaviour arising from repeated agent interactions over time |
| Nonlinearity | The heterogeneous and multiple levels of interaction between agents which makes agent response unpredictable |
| Feedback loop | Recursive mechanisms as a result of multiple agent interactions over time that create reciprocal behaviour either reinforcing (positive feedback loop) or undermining (negative feedback loop) each other |
| Emergence | New system behaviours (larger entities) generated by the interactions of smaller or simpler entities |
| Path Dependence | Past experiences influence the responses to new events |
| System hardware | Constituent of health system that includes human resources, financing, technology, service delivery, infrastructure, and supplies |
| System software | Constituent of health system that includes tangible (leadership, management, and governance knowledge and skills, rules and procedures) and intangible (values and norms, power relationships, and information communication) elements that interplay with system hardware elements to influence the system |
Despite the recent attention, evidence on the effectiveness of RMC interventions is meagre both in Ethiopia and globally.8 Identifying the health system constraints to the promotion of RMC would contribute to the development of evidence-based approaches. Our qualitative study was undertaken to provide a better understanding of health system constraints to the promotion of RMC in Ethiopian hospitals. We aim to contribute to the body of evidence that can be used in the design and implementation of RMC programs in Ethiopia and other similar settings.
Methods
This study is part of a broader mixed-methods intervention study which was conducted between March 2018 and August 2018 to explore health system factors influencing RMC and to develop and assess mitigation approaches in southern Ethiopia. The study was conducted in collaboration with the Federal Ministry of Health and the Southern Nations Nationalities and Peoples Region (SNNPR) Health Bureau, Ethiopia. This paper reports on the qualitative component of the study exploring the health system constraints to implementing RMC. We used the WHO’s health system building blocks (service delivery, health financing, leadership and governance, health workforce, medical technologies, and health information) to identify the constraints.34
Study setting
According to the three-tiered Ethiopian health service system, primary hospitals, along with their catchment health centres and health posts, constitute the first tier. Primary hospitals are designed to provide primary level services with a minimum capacity of 35 beds and 24-h emergency services, including comprehensive emergency obstetric care. In the second tier, there are general hospitals which provide the same services as primary hospitals, but have over 50 beds, and are designed to provide a range of specialist services including gynaecology and obstetrics, paediatrics, internal medicine, surgery, psychiatry and emergency services, and include diagnostic facilities and therapeutic interventions. Specialised hospitals form the third tier and serve as referral centres for general hospitals.35
The study was conducted in three public hospitals (two general and one primary hospital) and their corresponding programme administrative units. The hospitals were selected based on the primary author’s familiarity with the settings and intention to have an appropriate mix of primary and referral facilities. The hospitals admit women with or without a referral for both normal and caesarean delivery services and share similar characteristics with other hospitals of their levels in the country. See Table 2 for profiles of the study hospitals.
Table 2.
Profiles of study hospitals
| Characteristics | Hospital I | Hospital II | Hospital III |
|---|---|---|---|
| Geographical and population profile (2017) | |||
| Location (urban/rural) | Urban | Semi-urban | Semi-urban |
| Catchment population | 359,358 | 261,271 | 267,589 |
| Expected pregnancies in the catchment | 12,434 | 9,040 | 9,259 |
| Number of public hospitals in the catchment (including current one) | 03 | 01 | 01 |
| Number of health centres in the catchment | 05 | 09 | 11 |
| Facility profile | |||
| Total number of births attended in the last quarter of 2017 | 1081 | 433 | 713 |
| Total number (%) of caesarean births in the last quarter of 2017 | 164 (14.9) | 62 (14.3) | 138 (19.4) |
| Upgraded from a lower-level facility (Yes/No) | Yes | Yes | No |
| Number of labour wards | 02 | 01 | 01 |
| Total number of beds in the labour ward | 10 (5 in each) | 05 | 05 |
| Number of delivery rooms | 01 | 01 | 01 |
| Total number of birthing beds in the delivery room | 04 | 04 | 3 |
| Type of delivery room (Partitioned/Non-partitioned)* | Non-partitioned | Non-partitioned | Non-partitioned |
| Number of functional showers in the labour ward | 0 | 02 | 01 |
| Number of functional handwash basins in the labour ward | 01 | 02 | 01 |
| Designated waiting area for accompanying family members (Yes/No) | Yes | Yes | Yes |
*Open plan with multiple beds per room with no curtains/partitions.
The intervention
The rationale for this intervention arises from the lack of (1) a stand-alone RMC promotion package in Ethiopia and (2) evidence on the effectiveness and implementation challenges of RMC interventions in Ethiopia and globally. There were three components to the RMC intervention: a three-day offsite staff training on RMC; placement of wall posters in labour wards; and onsite supportive supervision. The intervention focused on the interpersonal aspect of care, including the recommendation for the admission of birth companions, but did not involve structural or hardware components. Further detail about the evaluation of the intervention from women's and service providers’ perspectives is available in other studies published elsewhere.36,37 Implementation of the whole set of components of the intervention lasted for three months. All service providers who assist women in the study hospitals (n = 69) were invited to participate in the intervention. Eventually, 64 service providers received all the intervention components including the training; five service providers did not attend the training for personal reasons. The participants comprised 51 midwives (79.7%), 4 general practitioners (6.3%), 4 integrated emergency surgical officers (6.3%), 3 nurses (4.7%), and 2 health officers (3.1%); 44 (68.8%) were female and a similar percentage were aged between 22 and 29 years. Table 3 shows details of the components and participants of the intervention.
Table 3.
Description of the RMC intervention
| Component | Description | Participants | Intervention period |
|---|---|---|---|
| RMC training | The RMC training manual included contents on an overview of maternal health in Ethiopia; human rights and law in the context of reproductive health; RMC rights and standards; professional ethics; and continuous quality improvement. The manual was designed after a thorough review of RMC implementation programmes in Kenya, Tanzania, and Nigeria; and WHO’s recommendations of Intrapartum Care for Positive Childbirth Experience; and national guidelines and professional ethics codes. |
64 service providers at the participating hospitals who assist women during childbirth (in two rounds) | First round: 25–27 April 2018 Second round: 2–4 May 2018 |
| Wall posters | Four wall posters
|
All (64) training participants The wall posters were included in the RMC training manual and all participants were briefed on these. |
25 April–4 May 2018 Posters were handed over to the hospitals’ MCH coordinators at the end of the second round training session. |
| Onsite supportive supervision | Two rounds of post-training quality improvement supportive supervision were conducted to appraise the action plan implementation, and to set actions for the next cycle with the long-term aim of developing a culture of continuous quality improvement actions. Guidance on a facility-led assessment of RMC using a structured checklist that was part of the RMC training manual. Guidance on action plan development to address actionable gaps identified by the assessment checklist. |
All (64) service providers who attended the RMC training. (There were service providers who attended both rounds of the supervision.) | First round: June 2018 Second round: July 2018 |
The RMC intervention goes in line with the core themes of the caring, respectful, and compassionate (CRC) health workforce initiative, one of the four transformation agendas of Ethiopia’s Health Sector Transformation Plan (2015–2020).35 A 2019 government review indicated that lack of ownership and engagement of stakeholders at all levels, lack of system-wide implementation, lack of finance, weak monitoring and evaluation systems, lack of research and evidence in the field, and resistance among providers were among the key challenges in implementing the initiative.38 While the CRC initiative is generic and designed for the entire health service in the country, it lacks depth and focus to address the core themes of RMC. In contrast, the study intervention dealt with promoting all components of the RMC charter19 and involved the mechanisms to track progress and take improvement actions.
Sampling and recruitment
We conducted 7 focus group discussions (FGDs) with service providers (4 FGDs before the RMC intervention and 3 FGDs after the RMC intervention) and 12 in-depth interviews (IDIs) with key informants. As the IDIs aimed to explore the status of respectful care in the hospitals and existing challenges to providing RMC from the perspectives of key informants who hold a managerial position, all were conducted before the RMC intervention.
Focus group discussions
Participants of the FGDs were service providers who provide care during labour, childbirth, and immediate postpartum periods in the maternity care unit of the study hospitals. The pre-RMC intervention FGDs were conducted in three public hospitals; two FGDs were conducted in one of the hospitals, while one FGD was conducted in each of the other hospitals. A total of 32 participants took part in the pre-RMC intervention FGDs (6–10 participants in each FGD); 24 of the participants were female, while the remaining 8 were male (Table 4). A total of 21 participants took part in the post-RMC intervention FGDs (6–8 participants in each FGDs; 1 in each intervention hospital) that were conducted two months after the intervention; 15 of the participants were female, while the remaining 6 were male. Participant selection for the pre-intervention FGDs was conducted based on the availability of service providers and depending on their duty assignment. The maternity care unit coordinators invited all service providers who were not on day-time duty and those who turned up were included. All participants (32) of the pre-RMC intervention FGDs received the RMC training, making 50% of the RMC training participants. For the post-RMC intervention FGDs, candidate participants (those who attended the RMC training and who were not on day-time duty) were invited to participate in an FGD (Table 4). The pre-intervention FGDs were conducted to explore the knowledge of service providers on quality maternity care, RMC, and the mistreatment of women; health system challenges; service providers’ experience in the provision of RMC; the contributors to the mistreatment of women in health facilities; de/motivators of RMC provision; and seek for their recommendations of what needs to be done to improve RMC. The post-intervention FGDs explored the challenges service providers experienced during implementation of the RMC training and further actions required to promote RMC.
Table 4.
Summary of participants and topic areas investigated during FGDs and IDIs
| Category | Facility | No. of FGDs/IDIs | Total no. of participants* | Topic areas explored |
|---|---|---|---|---|
| Pre-intervention FGDs | Hospital I | 2 | 16 (14 midwives, 2 nurses) | Features of quality maternity care; twice and perception of mistreatment; twice and perception of respectful care; contributors to mistreatment; challenges experienced in labour wards; motivators and demotivators to provide respectful care; actions required to promote respectful care |
| Hospital II | 1 | 8 (7 midwives, 1 integrated emergency surgical officer) | ||
| Hospital III | 1 | 8 (7 midwives, 1 health officer) | ||
| Post-intervention FGDs | Hospital I | 1 | 7 (6 midwives, 1 nurse) | Perceived behavioural influences of the training; challenges encountered, and new behaviours emerged in implementing the training; additional actions required to implement the training; partakers of RMC |
| Hospital II | 1 | 8 (8 midwives) | ||
| Hospital III | 1 | 6 (5 midwives, 1 general practitioner) | ||
| Pre-intervention IDIs | Hospital I | 4 | 4 (MCH** coordinator, quality focal person, medical director, and chief executive officer) | Features of quality maternity care; twice and perception of mistreatment; twice and perception of respectful care; contributors to mistreatment; perceived status of respectful care; respectful care initiatives; challenges in advancing respectful care |
| Hospital II | 4 | 4 (MCH coordinator, quality focal person, medical director, and chief executive officer) | ||
| Hospital III | 3 | 3 (MCH coordinator, quality focal person, and medical director) | ||
| Regional health bureau | 1 | 1 (senior maternal health expert) |
*Most FGD participants were midwives because 80% of service providers who assist women during childbirth in the study hospitals were midwives.
**MCH: Maternal and child health.
The preliminary analysis of the formative data set – 4 pre-intervention FGDs and 12 pre-intervention IDIs – helped us to contextualise the RMC training, notably the addition of a consultative discussion with training participants, hospital administrators, and programme managers on the last day of the training sessions.
In-depth interviews
All IDIs were conducted before the RMC intervention with key informants at hospital and programme levels. Key informants at the hospital level were maternal and child health coordinators, institutional quality focal persons, medical directors, and chief executive directors of the three intervention hospitals. The programme level IDI was conducted with a senior maternal health expert at the SNNPR Health Bureau (Table 4). The key informants were selected aiming at obtaining rich information from both hospital and programme levels that could enable us to meet the study objective. The IDIs explored the constraints to the promotion of RMC from the perspectives of programme managers and administrators who look after the programming and operation of maternal health services at hospital, zonal, and regional levels.
Data collection
Pre-intervention FGDs and IDIs were conducted from March 2018 to April 2018, and post-intervention FGDs were conducted in July 2018. Initially, semi-structured interview guides were developed in English after a thorough literature review. The key topic areas explored during the FGDs and IDIs are presented in Table 4. The FGDs lasted 45 minutes to one hour while the IDIs lasted 20–30 min.
The guides were then reviewed for content and clarity by two of the co-authors. The primary author translated the final version interview guides for both the FGDs and IDIs into Amharic language and used these versions to collect data in Amharic. Data were collected and digitally audio recorded by the primary author, who is familiar with the local context. Participants were provided with compensation for local transportation.
Data analysis
The primary author did the simultaneous translation (from Amharic to English) and transcription of the audio recordings. The transcribed data were then imported into NVivo software (QSR International, Version 12 Plus) for analysis. Data from the pre-and post-intervention FGDs and IDIs were analysed concurrently. Data were coded inductively and deductively using standard qualitative methodology,39 and analysed in two steps, first inductively to identify themes emerging from the transcripts and then deductively using the complex adaptive systems theory.26 Additionally, complexity theory helps to synthesise the constraints to RMC through the lens of inherent organisational complexities in hospitals; evidence from such synthesis can later be translated to tackle implementation problems.31 Coding of data was undertaken by the primary author after reading and rereading the transcripts to identify themes that impede RMC; the themes were then reviewed by one of the researchers (AM). The agreed-upon themes were then grouped into either system hardware or system software categories, according to Elloker et al.40 In this context, system hardware refers to supply, health workforce, facilities, and financing, whereas system software refers to knowledge and mindset, referral system, support and motivation, and service delivery guidelines. Following the thematic analysis, we used complex adaptive system theory as a framework to explore and map the complex interactions within and between the system hardware and system software elements.26 This approach of data- and theory-driven analysis is suggested by scholars to improve rigour in thematic analysis.41 The primary author developed a causal loop model using Vensim software to visualise the interactions between different system elements in the maternity care system that affect the delivery of RMC. The developed model was then reviewed by all authors. We used the consolidated criteria for reporting qualitative research to report important aspects of this study.42
Ethical considerations
Ethical approval for this study was obtained from the University of Melbourne (Australia) and the SNNPR Health Bureau (Ethiopia). Participants were given a plain language statement about the study that they read before consenting to participate; all participants gave written consent before participating in the study.
Findings and interpretations
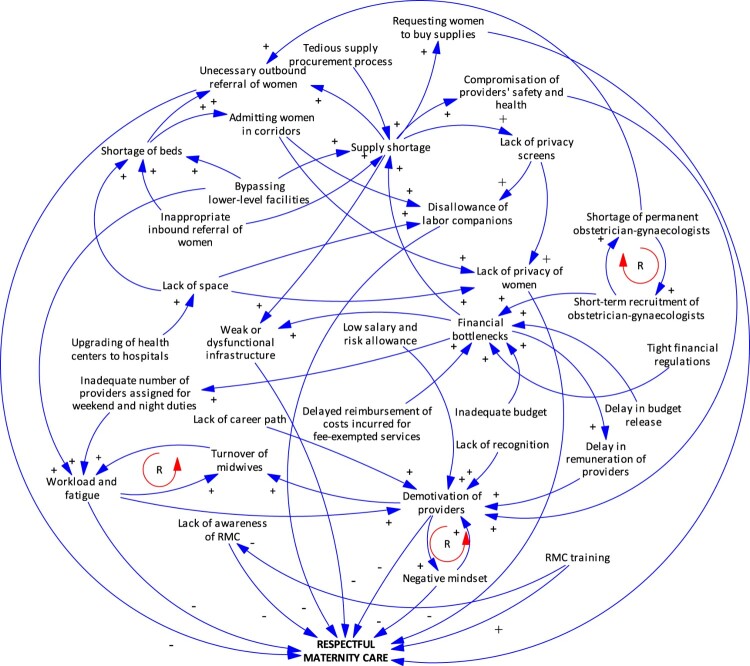
We identified seven health system factors influencing the promotion of RMC belonging to the categories of system hardware (bed availability; infrastructure and supplies; financing; and health workforce) and system software (staff motivation; service providers’ mindset; and awareness of RMC). These elements exhibited complex interactions with each other, amplifying the challenges of implementing RMC. Limited responsiveness within the maternity care system constrained implementation of the RMC recommendations. In the following sections, we report on the system interactions by identifying where complex adaptive system processes were at play, which are depicted in Figure 1. Consistent with complex systems, some of the themes have shared causal factors and intersect with each other.
Figure 1.
Causal loop diagram of factors influencing respectful maternity care in hospitals*
Notes: “+” sign on the blue arrows indicates the causing variable increases the outcome variable. “−” sign on the blue arrows indicates the causing variable reduces the outcome variable. “R” in the red rotating arrows indicates the variables have a reinforcing effect on each other in the direction of the arrow.
Bed availability
All study hospitals have only one labour ward and one delivery ward (separate from the labour ward) where women stay together; there are four to six hospital beds in each labour ward and three to four birthing beds in each delivery room (Table 2). In response to the rising client flow, one of the hospitals had previously built a new maternal and child health unit which helped to separate obstetrics and gynaecology wards while the remaining two have renovated their labour wards to accommodate more beds.
“We are restructuring the wards using partition boards to add two more beds. As a long-term solution, we are constructing a new hospital building that will take about two years to be available for service.” (Coordinator, Hospital I)
Despite these facility-level remedies to increase bed capacities, all study hospitals experienced patient numbers that exceeded bed capacity:
“ … the main challenge is the shortage of beds, especially during the night-time; there is a huge complaint from staff and the community in this regard. Sometimes, it is the gatekeepers who tell women coming by ambulance to turn around and look for other hospitals in the city.” (Coordinator, Hospital I)
Although women can give birth in lower-level health facilities, participants reported that most women who come to hospitals for childbirth bypass health centres, assuming that they will receive better service in hospitals, an important factor explaining the shortage of beds and overcrowding in hospitals. Participants also said that many women are referred from lower-level facilities without any clinical indications requiring referral and could have given birth safely at primary level health services and that bypassing these facilities increases pressure on the hospitals.
“More than half of the women who give birth in our hospital can give birth at health centre levels. Women bypass these facilities, and there is also an inappropriate referral of women from these facilities. Last month, 59 women who were referred from ‘health centre A’ gave birth in our hospital without any particular procedure for an assisted delivery (vacuum or forceps). ” (Coordinator, Hospital III)
In response to the overcrowding, health workers are faced with the following choices to manage excess client flow: admitting women who are in labour to wait in corridors until someone gets discharged, or referring women to other facilities, including those who have already been referred to them from other facilities.
Infrastructure and supplies
In all hospitals, in addition to the overcrowding described above, there were both space constraints and supply shortages. The absence of privacy screens was a key constraint to the provision of respectful care, especially maintaining women’s privacy during vaginal examinations. In the two upgraded hospitals, there was only limited expansion of the labour wards, delivery rooms, and waiting areas for families, meaning that the renovations have not equipped the hospitals with adequate space given the expansion of services.
“This hospital was a clinic 57 years ago; it was then upgraded to a health centre and later to a primary hospital and then general hospital without significant expansions. That is why the buildings/rooms are not conducive to provide services to the level that a general hospital should do.” (Manager, Hospital I)
Following the RMC training, all hospitals allowed labour companions to accompany women in labour wards, which meant there were several companions in one labour ward. The willingness among staff indicates that there is a real opportunity to promote labour companionship in the long run. However, participants said that it was challenging to maintain women’s privacy during vaginal examinations because there are several “strangers” in the labour wards which are already considered small, given the number of beds they accommodate, as indicated in Table 2. Thus, while the admission of labour companions likely benefited women during labour, it simultaneously had an undesirable effect on the privacy of other women. As a result, service providers faced a dilemma of which aspect of RMC to prioritise – privacy or labour companionship. Eventually, labour companions were denied admission in labour wards, especially in two of the hospitals, because of the privacy concerns.
“Because we do not have adequate [privacy] screens, we are asking all labour companions to go out of the ward whenever a woman is to have an examination … ” (Service provider, post-RMC intervention FGD, Hospital III)
The interaction between the lack of privacy and the admission of labour companions in labour wards proved to be competing forces, a manifestation of non-linear inter-relationships. Service providers’ understanding of privacy seemed to extend only to the companions of other women in the ward, not to the other women (residing) in the ward, who are also strangers. This implies privacy is still lacking, although the degree may be less than when companions are in the room. In a different context, there might be a positive relationship between the presence of labour companions and RMC, but in a context in which available supplies, especially privacy screens, were often lacking, the expected relationship is modified and effectively reversed. In effect, this particular hardware issue is among the key system elements jeopardising RMC.
Other supply issues identified were the shortage of bed linen; infection prevention supplies including aprons, gloves, soap and chlorine solutions; blood packs; essential medicines including ergometrine; and foetal monitoring equipment. Furthermore, lengthy procurement procedures and the supply of low-quality medical equipment were additional challenges to the continuous availability of supplies:
“ … a respectful midwife cannot address all requirements of respectful care alone. He/she must be provided with required supplies … ” (Coordinator, Hospital II)
In the case of acute stockouts of recurrent supplies, hospitals adapted to these situations by commissioning special purchase of supplies using their internal revenue, asking for support from non-governmental partner organisations, and borrowing from nearby health facilities. To initiate an independent purchase of missing supplies mentioned above, hospitals require an out-of-stock clearance from the Ethiopian Pharmaceutical Supply Agency. Once hospitals are granted permission, meeting the requirements of government procurement guidelines43 was reported to be very challenging.
“We have allocated a budget for the purchase of supplies. However, it is tough to get these in the market. How could I admit a woman for labour when I do not have a glove to use? A mother will get referred without her will and consent … ” (Manager, Hospital I)
Additionally, participants described several facility constraints including dysfunctional or complete absence of utilities like shower and sinks, shortage of water supply, no waiting area for companions, and poorly ventilated wards. These challenges were also the reason why service providers did not allow women and their families to perform cultural ceremonies/practices that they would do if the woman had birthed at home. Hospital administrators have indicated that they have budget limitations for regular maintenance and renovation works. Accordingly, the supply and facility constraints in the hospitals were influenced by complex interactions between various agents such as leadership, governance, and financing, which are complex systems themselves.
These supply, space, and facility constraints have direct (denying women the required level of services and resulting in unnecessary referrals) and indirect (damaging providers’ commitment to provide care due to health and safety concerns) negative effects on RMC.
Healthcare financing
All hospitals were implementing a financing recommendation set forward by the Ethiopian government to make antenatal, delivery, and postnatal care services available free of charge in public health facilities although there were some inconsistencies before the CRC initiative.44 As part of the government’s initiative to promote CRC, the hospitals waived the fee for investigations conducted during pregnancy and childbirth, including obstetric ultrasound.
“Investigations, including ultrasonography, for women are provided free of charge with a special consideration not only to make them happy and encourage them to give birth in health facilities but also to provide the services that they are entitled to get from hospitals.” (Coordinator, Hospital III)
The fee-exemption was introduced first in health centres and then in hospitals between 2005 and 2010. In principle, hospitals apply to the Ministry of Health at the end of every quarter for reimbursement for the costs incurred to deliver fee-exempted services. While the fee-exemptions were regarded as positive in promoting equity, challenges arose to meet the expectations for services. For example, delays in reimbursement were reported in all hospitals and contributed to supply shortages because hospitals were not able to accumulate funds that they could use for procurement. We identified an emergent behaviour in response to the implementation gap of the fee-exemption policy for maternal health services – requesting women to buy supplies:
“ … now, we are in the second quarter of the current budget year. However, we did not yet get reimbursed by the Ministry for our expenses of the second quarter of the previous budget year. We are in a big challenge currently.” (Manager, Hospital II)
Insufficient and delayed release of budgeted funds were the two other key challenges affecting the management and delivery of childbirth services in the hospitals. The beginning of a fiscal year is the most challenging period when hospitals encounter difficulties in paying compensation for services such as night and weekend duties, as the new fiscal year’s budget is not usually released for use on time. Consequently, service providers wait for months to get paid for their weekend and night duties, and this has resulted in demotivation of service providers and a negative relationship between service providers and administrators.
Financial bottlenecks also resulted in the assignment of a substandard number of midwives for night and weekend duties to minimise expenses. As such, the assigned service providers bear a higher workload than they are supposed to; this often leaves them frustrated and eventually results in the mistreatment of women.
“ … in some hospitals and most health centres, an adequate number of midwives are not assigned for night duties; this practice is totally against the standard, and it happens because health facilities do not want to pay for night duty. There are occasions five or more labouring women come in a single night, and the workload makes us ‘health providers’ to behave disrespectfully.” (Service provider, pre-RMC intervention FGD, Hospital I)
These complex interactions between different agents in the financing system left hospitals in financial bottlenecks which in turn added to the complexity in the maternity care system (affecting the availability of supplies, deployment of adequate staff, timely payment of remuneration, etc.), making it difficult to practice RMC. The delay in providers’ night and weekend duty payments made providers feel disrespected, further compounding the complexity of RMC delivery.
Staff motivation
As part of the CRC initiative, all hospitals have introduced staff appraisal and recognition ceremonies which occur every six months to give awards to the best performing staff from each unit of the hospitals, including maternity units. The coordinator of one of the hospitals reported that they also have a fortnightly coffee ceremony in which women and their families are involved and best practices and gaps identified are discussed. This recognition was important to improve staff morale.
“ … there are CRC focal persons in each unit who appraise respectful care, deal with breach of professional ethics, and hold group meetings with their team. The best performer professional is selected every six months from each unit, and a certificate of appreciation is awarded to motivate them.” (Coordinator, Hospital I)
However, there were simultaneously weak staff incentives and a lack of motivation schemes in hospitals, which had a negative effect on RMC by damaging providers’ enthusiasm to provide respectful care. These included: low salaries; risk allowance gaps among professions; lack of support and recognition by managers; lack of career opportunities; undefined career path (especially for midwives and integrated emergency surgical officers); low and delayed remuneration for night and weekend duties; and lack of a positive work environment.
“Sometimes, you keep on doing and discharging your responsibilities appropriately, but no one from the senior managers comes to you and sees what you do and gives you recognition.” (Service provider, post-RMC intervention FGD, Hospital I)
Hospital administrators reported that they use the national pay scale, and they do not have the authority to adjust salaries and other payments however they share providers’ complaints.
“Because what is being paid here is low, service providers look for part-time jobs elsewhere. That, in turn, compromises the quality of service in our hospital as service providers get fatigued … I know this is a national problem and cannot help it … ” (Coordinator, Hospital I)
Midwives reported that there is an unfair gap of risk allowance among different professions; midwives report receiving 470 birr (∼17 USD) per month while health officers and emergency nurses receive a higher risk allowance, 1250 birr (∼46 USD) and 1200 birr (∼44 USD), respectively. Managers have also expressed the gap as inappropriate and creating dismay among midwives. Midwives claimed that they are exposed to a higher level of professional risk, such as infections, compared to health officers and emergency nurses. Because of these dissatisfactions, the lack of career opportunities, and the relatively better pay that other non-health professional graduates (such as accountants) of the same years of employment receive, participants said that fellow midwives are leaving the profession.
“Practicing midwifery is difficult in Ethiopian facilities; as a midwife, you are supposed to work for 24 hours if you have night duty, the workload is exceptionally high, you take care of several women at a time. Disproportionately, your salary is very low, as is your risk payment.” (Service provider, pre-RMC intervention FGD, Hospital II)
The interaction between high workload and attrition of midwives exhibited a positive feedback loop: the more midwives resign, the higher the workload becomes, which in turn leads the remaining midwives to resign. This emergence of behaviour (resignation) among midwives due to the longstanding problem of staff motivation, including a lack of career path, further makes the delivery of RMC complex. Given the shortage of midwives in the country, such preventable attrition would again add to the complexity of health workforce availability and quality and is a barrier to promoting RMC.
Health workforce
Both program coordinators and administrators emphasised that the shortage of staff, especially midwives and obstetrician-gynaecologists, needs to be resolved if respectful care is to improve. Hospitals recruit obstetrician-gynaecologists on a short-term and often expensive contract basis to fill the acute shortages of these specialists, and that is draining their revenues.
A manager of one of the hospitals reported that obstetrician-gynaecologists do not want to work on a permanent basis in order to take advantage of the higher salary, sometimes more than three times the regular salary that hospitals offer on a contract basis. The more the hospitals pay for contract-based recruitment, the less likely specialists are to take full-time positions.
The shortage of professionals has created an increased workload, fatigue and negligence, unnecessary referrals, and failure to respond to women’s preference of service providers. Dissatisfaction with the work climate and dysfunctional professional hierarchy, in addition to the low pay, were also identified as the key reasons for the high turnover of service providers in the hospitals.
“ … It is the standard to have two providers for a labouring woman; one for the mother and one for the newborn. However, we do not practice that always since there is a shortage of workforce … this makes providers nervous at the end.” (Coordinator, Hospital III)
Service providers’ mindset
Service providers who participated in the intervention showed a willingness to implement practices to support RMC. These included allowing support by labour companions, allowing women to birth in their preferred position, and seeking women’s consent before procedures, and reflected a level of agency amongst the staff and a commitment to quality improvement initiatives.
“ … we used to provide care with force if women refused to have a procedure or an examination. After the training, there is no such practice; we provide services with consent and respect.” (Service provider, post-RMC intervention FGD, Hospital II)
Yet health workers also faced entrenched interpersonal hierarchies of care that constrained RMC. Because of an intergenerational trend of hierarchical patient-provider and provider-provider relationships and the lack of awareness of the constituents of RMC, participants said they were mistreating women intentionally and unintentionally.
“Junior professionals adopt behaviour of their seniors. The trend so far was distancing and hierarchy between different professionals and between professionals and patients; that finally leads to the designation of providers as “bosses” who order patients what to do.” (Coordinator, Hospital III )
“ … there is a wrong tradition of regarding health professionals as kings among service users; ‘no one can talk to them’ type of thought. That resulted in some providers feeling proud of their professional status and undermining others … ” (Manager, Hospital II)
The post-intervention FGDs revealed that some providers have reservations about the feasibility of fully respecting the universal rights childbearing women should have in health facilities. Providers reported that the rights of women could not be entertained given the existing multidimensional constraints reported in this study. Additionally, providers required their rights also be defined and guaranteed.
“ … in 99% of the cases, health facility management attend only to the rights of clients; they do not emphasise the rights of professionals … ” (Service provider, pre-RMC intervention FGD, Hospital I)
After the RMC training, some providers opposed the distribution of a pamphlet on The Universal Rights of Childbearing Women (Amharic version)19 that had been endorsed by the Ministry of Health. Eventually, none of these pamphlets were distributed. Participants said that women and their companions demand to exercise the rights included in the pamphlet and that providers are not able to address these due to system hardware constraints despite most rights on the declaration being related to interpersonal care.
“ … for example, I had a long night assisting women, but I am not paid fairly. Is it fair to accuse me of violating women’s rights? I do not think … a lot must be done from top to bottom in responding to providers right before trying to maintain women’s right.” (Service provider, post-RMC intervention FGD, Hospital III)
Even after receiving the RMC training, some service providers continued to express the idea that it is acceptable to disrespect women when providers are not also respected.
Awareness of RMC
Before the RMC training, RMC was a new terminology to participants of the FGDs and IDIs; similar were “mistreatment” and “disrespect and abuse”. Participants had an awareness of what respectful care means, mostly in its interpersonal aspect, while they lacked awareness of its systemic aspects. As supported by participants of the post-intervention FGDs, short-term RMC trainings like the one implemented in this study play a key role in improving service providers’ awareness of RMC and the rights of childbearing women in health care settings.
“I am now aware that I may disrespect women in various ways. On the other hand, I have also understood that I can serve women very nicely and make them satisfied with little efforts. I have also learned what makes women displeased.” (Service provider, post-RMC intervention FGD, Hospital II)
Participants recommended that support staff who have a direct or indirect role in maternity care, including the reception at the hospital entrance gate, should also receive the training, with the justification that RMC cannot only be achieved by the care in maternity wards. A programme coordinator at the regional level outlined that there is a gap in knowledge of RMC because the existing service delivery guidelines lack content on RMC.
Discussion
Service providers’ lack of knowledge of RMC and an unconscious normalisation of disrespectful care highlights the need for tailored RMC education. Nonetheless, it is important to emphasise the non-behavioural challenges that also need to be addressed to ensure that knowledge is translated into practice. We conducted this study to outline the system constraints to the promotion of RMC in public hospitals from the perspectives of service providers and managers. The pre- and post-RMC intervention qualitative enquiries benefited this study in identifying the complex interactions between various system elements in the absence of and with the intervention. Notably, the post-RMC intervention FGDs helped to demonstrate how the interaction between various system constraints could mark the implementation of RMC recommendations.
In two other studies, we have reported on the evaluation of the RMC intervention (survey of women before and after the intervention)37 and the lessons learned through its implementation, including the enablers of RMC (mixed-methods study among service providers who participated in the intervention).36 The survey of women revealed that the number of mistreatment components women experienced during childbirth in the study hospitals was reduced by 18% after the RMC intervention.37 The mixed-methods study revealed that service providers’ awareness of the rights of childbearing women, perceptions and attitudes about RMC, and motivation to provide respectful care improved after the RMC intervention.36
To our knowledge, this is the first study to explore the status of RMC through the theoretical lens of complex adaptive systems, which allowed us to focus both on structures and functions (processes) of the maternity care system and the interplay between these. We have synthesised the findings of this study using a causal loop diagram that shows the complex relationships between different system elements in the RMC system (Figure 1).
The interaction between system hardware and software constraints in maternity settings was complex and warrants a systems approach to improve RMC. A system constraint can affect both clinical and non-clinical maternity care components at the same time or may have spill-over from one of these components to another due to the existence of interactions between the components.45 Similarly, an intervention component that aims at improving a system component may have a positive or negative consequence on other components. For example, weak implementation of the fee exemption for maternity care services resulted in a lack of revenue and supply shortages in the hospitals; in response, women were asked to buy supplies in direct contradiction to the policy.28 Not only is this disrespectful, but it may also offset the intended aim of the fee removal, which is to improve service utilisation.46,47
System hardware and software constraints challenged the implementation of RMC recommendations. For example, financial limitations in the study hospitals led to a complex relationship affecting recruitment and motivation of staff, availability of supplies, and maintenance of facilities. A study from Kenya also demonstrated that financial limitations negatively impacted service providers’ and hospital administrators’ motivation to implement hospital initiatives.48 According to Clark, such complex problems necessitate complex interventions (interventions that encompass different parts such as financing, supply, workforce, infrastructure, and others) but cannot be solved by behavioural interventions alone.49 Therefore, as outlined by the WHO, implementing context-based complex interventions to improve the quality of services is instrumental in promoting RMC.5
Evidence reviews report that having a labour companion during labour and childbirth helps women to have a positive childbirth experience.50,51 In this study, service providers encountered the problem of sustaining practices of admitting labour companions and allowing cultural practices in labour wards, due to space and privacy constraints, and because an admission of companions inadvertently fed back negatively on the privacy of women. Such constraints are also critical challenges in promoting the culture of labour companionship in health facilities globally.51 These constraints also indicate that women’s privacy is already in jeopardy in the absence of adequate infrastructure. Addressing these barriers plays a crucial role in promoting RMC and quality of care52 and contributes to the improved uptake of maternity care services.53,54 Furthermore, taking a contextualised and proactive approach to planning for health systems infrastructure improvement is required to improve the quality of care, mitigate the consequential and unintended impacts of innovations, and respond to the evolving needs in LMICs, including Ethiopia.3,49
Women bypass lower-level health facilities, as indicated in this study, due to lack of confidence in lower facility providers, perceived low-quality of service, and fear of referral processes in case of a birth complication in lower-level facilities.55 When this is coupled with the lack of bed capacity in hospitals, it predisposes women to mistreatment by denying them the timely and quality care they deserve. It also results in a second referral and hospitals have to deal with client overflow. A study conducted in three regions in Ethiopia reported that 86.4% of patients visited hospitals without referral, and bypassing was common among maternal and child health care seekers.56 Similarly, a Tanzanian study also found that 44% of women bypassed primary health facilities for childbirth mainly due to concern about the quality of care at health centres.57 It is, therefore, essential to improve the quality of maternity care services in lower-level primary health facilities and to build communities’ confidence in these facilities.55 Without these actions, improving RMC only in hospitals means more women keep on bypassing primary facilities because of preferences for hospital-level care in the community, generating factors which impede improvement of quality of care in hospitals.
While it is appropriate that regulatory and financial control mechanisms aim at ensuring governance and reducing corruption in the health system,43 they may also result in lengthy bureaucratic processes if poorly designed and/or implemented, which can lead to disrespectful behaviours among service providers.35,58 Nothing justifies disrespectful or abusive treatment of women, but these working conditions make it more likely. A review by Reader and Gillespie reported that such institutional causes result in normalisation of patient neglect and abuse among providers and should therefore be addressed from both behavioural and organisational interventions.59
A noteworthy finding of this study is the importance of involving health managers in any health worker behaviour intervention. Service providers reported being demotivated as they were improving services as per the RMC training guideline. Yet, no one from the facility management recognised these efforts – a missed opportunity to keep up the enthusiasm for change. A study from Benin reported that management support and recognition of midwives and other staff was vital in sustaining positive changes gained from a humanised childbirth intervention.60
Strengths and limitations
Exploring service providers’ perspectives of applying new knowledge into practice is of paramount importance to plan for future interventions that can be applied in the real world.61 In this regard, the conduct of FGDs both before and after the RMC intervention is the main strength of this study as it profoundly helped us to have a richer understanding of how multiple interactions between various system constraints could offset the implementation of RMC recommendations and other similar quality improvement initiatives in maternity settings. Additionally, the use of complexity theory in the data analysis surpassed the depth of evidence that would be obtained by the traditional approaches of exploring single cause and effect relationships; it brought the wider picture of how various entities interact with each other and directly or indirectly affect RMC in the real-world setting. However, this study only reflects scenarios at primary and general hospitals and may, therefore, lack the breadth to cover system constraints in referral and teaching hospitals and health centres in Ethiopia. Additionally, since the post-intervention FGDs were conducted two months following the intervention, our study is unable to explore how systems adapted further after that point. In the current study, complexity theory was applied post hoc for data analysis but did not guide the development of data collection tools; this might have limited the completeness of the data collected and the opportunity to explore alternative frames of analysis. Furthermore, participants of the post-intervention FGDs might have reported their experiences of the RMC training in a way that would please the investigator who moderated the FGDs, from social desirability bias.
Conclusions
This study identified complex health system constraints that hinder the promotion of RMC in hospitals. Although quality of maternity care embodies both clinical and interpersonal aspects of care, this study highlights that interventions aimed at improving only interpersonal or behavioural components fall short of mitigating the mistreatment of women unless they also address the system-wide constraints. As indicated in the study, there is scope for real improvement if the health system components are part of the solution to promote RMC and end the mistreatment of women. To enhance the status of maternal health in Ethiopia, we recommend the implementation of RMC from a health system strengthening viewpoint. We also recommend future implementation research in the field of RMC to bridge the discourse between theory and practice in the local context. Finally, we believe that the findings of this study inform policies and strategies to promote RMC in Ethiopia and other LMICs.
Acknowledgements
The intervention part of this study was financially supported by the Institute for Healthcare Improvement Ethiopia country office. The authors are indebted to the Federal Ministry of Health, the SNNPR Health Bureau, the Institute for Healthcare Improvement, the study hospitals, and Hawassa University College of Medicine and Health Sciences for their technical support during the conduct of this study. The authors would also like to thank participants of the study for their willingness to take part in this study.
Funding Statement
The intervention part of this study was financially supported by the Institute for Healthcare Improvement Ethiopia country office.
References
- 1.World Health Organization . Trends in maternal mortality: 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva, Switzerland: World Health Organization; 2019. [Google Scholar]
- 2.United Nations . Sustainable development goals. New York: United Nations Development Programme; 2015; Available from: http://www.un.org/sustainabledevelopment/sustainable-development-goals/. [Google Scholar]
- 3.World Health Organization . Strategies toward ending preventable maternal mortality (EPMM). Geneva: World Health Organization; 2015. [Google Scholar]
- 4.Tuncalp Ö, Were WM, MacLennan C, et al. Quality of care for pregnant women and newborns-the WHO vision. BJOG. 2015;122(8):1045–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Standards for improving quality of maternal and newborn care in health facilities. Geneva: World Health Organization; 2016. [Google Scholar]
- 6.Hanefeld J, Powell-Jackson T, Balabanova D.. Understanding and measuring quality of care: dealing with complexity. Bull World Health Organ. 2017;95(5):368–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bohren MA, Vogel JP, Hunter EC, et al. The mistreatment of women during childbirth in health facilities globally: a mixed methods systematic review. PLoS Med. 2015;12(6):e1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . WHO recommendations: intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 9.World Health Organization . The prevention and elimination of disrespect and abuse during facility-based childbirth. Geneva: World Health Organization; 2014. [Google Scholar]
- 10.Bohren MA, Mehrtash H, Fawole B, et al. How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys. Lancet. 2019;394(10210):1750–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sando D, Abuya T, Asefa A, et al. Methods used in prevalence studies of disrespect and abuse during facility based childbirth: lessons learned. Reprod Health. 2017;14(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bradley S, McCourt C, Rayment J, et al. Disrespectful intrapartum care during facility-based delivery in sub-Saharan Africa: a qualitative systematic review and thematic synthesis of women's perceptions and experiences. Soc Sci Med. 2016;169:157–170. [DOI] [PubMed] [Google Scholar]
- 13.Asefa A, Bekele D.. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health. 2015;12:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asefa A, Bekele D, Morgan A, et al. Service providers' experiences of disrespectful and abusive behavior towards women during facility based childbirth in Addis Ababa, Ethiopia. Reprod Health. 2018;15(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banks KP, Karim AM, Ratcliffe HL, et al. Jeopardizing quality at the frontline of healthcare: prevalence and risk factors for disrespect and abuse during facility-based childbirth in Ethiopia. Health Policy Plan. 2018;33(3):317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheferaw ED, Kim YM, van den Akker T, et al. Mistreatment of women in public health facilities of Ethiopia. Reprod Health. 2019;16(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ethiopian Public Health Institute (EPHI) . [Ethiopia] and ICF. Ethiopia Mini Demographic and health survey 2019: Key Indicators. Rockville (MD: ): EPHI and ICF; 2019. [Google Scholar]
- 18.Roro MA, Hassen EM, Lemma AM, et al. Why do women not deliver in health facilities: a qualitative study of the community perspectives in south central Ethiopia? BMC Res Notes. 2014;7:556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.White Ribbon Alliance . Respectful maternity care: the universal rights of childbearing women. Washington (District of Columbia): White Ribbon Alliance; 2011. [Google Scholar]
- 20.Afulani PA, Moyer CA.. Accountability for respectful maternity care. Lancet. 2019;394(10210):1692–1693. [DOI] [PubMed] [Google Scholar]
- 21.Austin A, Langer A, Salam RA, et al. Approaches to improve the quality of maternal and newborn health care: an overview of the evidence. Reprod Health. 2014;11(Suppl 2):S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bowser D, Hill K.. Exploring vvidence for disrespect and abuse in facility-based childbirth-a landscape analysis of the global situation of abuse and disrespect in maternity care. Boston: USAID, Traction Project; 2010. [Google Scholar]
- 23.Gomersall T. Complex adaptive systems: a new approach for understanding health practices. Health Psychol Rev. 2018;12(4):405–418. [DOI] [PubMed] [Google Scholar]
- 24.Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–2192. [DOI] [PubMed] [Google Scholar]
- 25.McMahon SA, Mnzava RJ, Tibaijuka G, et al. The "hot potato" topic: challenges and facilitators to promoting respectful maternal care within a broader health intervention in Tanzania. Reprod Health. 2018;15(1):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gear C, Eppel E, Koziol-Mclain J.. Advancing complexity theory as a qualitative research methodology. Int J Qual Methods. 2018;17:160940691878255. [Google Scholar]
- 27.Mathews KM, White MC, Long RG.. Why study the complexity Sciences in the social Sciences? Human Relations. 1999;52(4):439–462. [Google Scholar]
- 28.Begun JW, Zimmerman B, Dooley KJ.. Health care organizations as complex adaptive systems. In: Mick SS, Wyttenbach ME, editors. Advances in health care organization theory. 1 ed. San Francisco (CA: ): Jossey-Bass; 2003. p. 253–288. [Google Scholar]
- 29.Byrne D. The reality of the complex: the complexity of the real. In: Complexity theory and the social sciences: an introduction. London: Routledge; 2003. p. 35–53. [Google Scholar]
- 30.Dd Savigny, Adam T, editors. Systems thinking for health systems strengthening: alliance for health policy and systems research. Geneva: World Health Organization; 2009. [Google Scholar]
- 31.Braithwaite J, Churruca K, Ellis LA, et al. Complexity science in healthcare – aspirations, approaches, applications and accomplishments: a White Paper. Sydney: Australian Institute of Health Innovation, Macquarie University; 2017. [Google Scholar]
- 32.Braithwaite J, Churruca K, Long JC, et al. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheikh K, Gilson L, Agyepong IA, et al. Building the field of health policy and systems research: framing the questions. PLoS Med. 2011;8(8):e1001073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization . Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization; 2007. [Google Scholar]
- 35.Federal Democratic Republic of Ethiopia Ministry of Health . Health sector transformation plan: 2015/16 - 2019/20. Addis Ababa: Federal Ministry of Health; 2015. [Google Scholar]
- 36.Asefa A, Morgan A, Bohren MA, et al. Lessons learned through respectful maternity care training and its implementation in Ethiopia: an interventional mixed methods study. Reprod Health. 2020;17:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asefa A, Morgan A, Gebremedhin S, et al. Mitigating the mistreatment of childbearing women: evaluation of respectful maternity care intervention in Ethiopian hospitals. BMJ Open. 2020;10:e038871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ministry of Health-Ethiopia . Compassionate, respectful and caring health system for health sector transformation plan success. Addis Ababa: Ministry of Health; 2019; Available from: http://www.moh.gov.et/ejcc/am/node/160. [Google Scholar]
- 39.Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 40.Elloker S, Olckers P, Gilson L, et al. Crises, routines and innovations: the complexities and possibilities of sub-district management. South Afr Health Rev. 2013;2012/13: 161–173. [Google Scholar]
- 41.Fereday J, Muir-Cochrane E.. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5(1):80–92. [Google Scholar]
- 42.Tong A, Sainsbury P, Craig J.. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 43.The Federal Democratic Republic of Ethiopia Public Procurement and Property Administration Agency . Public procurement manual. Addis Ababa: Ministry of Finance and Economic Development; 2011. [Google Scholar]
- 44.Federal Democratic Republic of Ethiopia Ministry of Health . Health care financing strategy: 2017–2025. Addis Ababa: Ministry of Health; 2016. [Google Scholar]
- 45.Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McPake B, Brikci N, Cometto G, et al. Removing user fees: learning from international experience to support the process. Health Policy Plan. 2011;26(Suppl 2:):ii104-17. [DOI] [PubMed] [Google Scholar]
- 47.Bohren MA, Hunter EC, Munthe-Kaas HM, et al. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reprod Health. 2014;11(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Barasa EW, Molyneux S, English M, et al. Hospitals as complex adaptive systems: a case study of factors influencing priority setting practices at the hospital level in Kenya. Soc Sci Med. 2017;174:104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clark AM. What are the components of complex interventions in healthcare? Theorizing approaches to parts, powers and the whole intervention. Soc Sci Med. 2013;93:185–193. [DOI] [PubMed] [Google Scholar]
- 50.Hodnett ED, Gates S, Hofmeyr GJ, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2013;2013(7). [DOI] [PubMed] [Google Scholar]
- 51.Bohren MA, Berger BO, Munthe-Kaas H, et al. Perceptions and experiences of labour companionship: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2017;(3):CD003766. 10.1002/14651858.CD003766.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rubashkin N, Warnock R, Diamond-Smith N.. A systematic review of person-centered care interventions to improve quality of facility-based delivery. Reprod Health. 2018;15(1):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coast E, Jones E, Lattof SR, et al. Effectiveness of interventions to provide culturally appropriate maternity care in increasing uptake of skilled maternity care: a systematic review. Health Policy Plan. 2016;31(10):1479–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coast E, Jones E, Portela A, et al. Maternity care services and culture: a systematic global mapping of interventions. PLOS One. 2014;9(9):e108130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Murray SF, Pearson SC.. Maternity referral systems in developing countries: current knowledge and future research needs. Soc Sci Med. 2006;62(9):2205–2215. [DOI] [PubMed] [Google Scholar]
- 56.Abrahim O, Linnander E, Mohammed H, et al. A patient-centered understanding of the referral system in Ethiopian primary health care units. PLoS One. 2015;10(10):e0139024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kruk ME, Mbaruku G, McCord CW, et al. Bypassing primary care facilities for childbirth: a population-based study in rural Tanzania. Health Policy Plan. 2009;24(4):279–288. [DOI] [PubMed] [Google Scholar]
- 58.McMahon SA, George AS, Chebet JJ, et al. Experiences of and responses to disrespectful maternity care and abuse during childbirth; a qualitative study with women and men in Morogoro Region, Tanzania. BMC Pregnancy Childbirth. 2014;14:268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reader TW, Gillespie A.. Patient neglect in healthcare institutions: a systematic review and conceptual model. BMC Health Serv Res. 2013;13:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fujita N, Perrin XR, Vodounon JA, et al. Humanised care and a change in practice in a hospital in Benin. Midwifery. 2012;481–488. [DOI] [PubMed] [Google Scholar]
- 61.Peters DH, Tran NT, Adam T.. Implementation research in health: a practical guide. Alliance for health policy and systems research. Geneva: World Health Organization; 2013. [Google Scholar]