Abstract
Papua New Guinea (PNG) is the most populous country in the Pacific with more than 9 million people. Difficult terrain, poor roads and limited infrastructure mean providing effective health care – especially in rural areas, where most people live – is challenging. Women and newborns in PNG experience high rates of preventable morbidity and mortality; however, reliable data are often limited or unavailable. The aim of this paper is to provide an overview of research on key maternal and neonatal health (MNH) indicators conducted approximately over the past 11 years in PNG comparing research findings to global MNH estimates of the indicators. There was considerable variation in mortality indicators (maternal mortality ratio, neonatal mortality rate and stillbirth) reported across studies in PNG. Mortality was generally higher in rural areas. Rates of sexually transmitted infections (STIs) in pregnancy were consistently high, while anaemia in pregnancy, preterm birth and low birth weight varied widely between studies and settings. Breastfeeding seems to have been under-researched. There was a lack of data available on other indicators such as the adolescent birth rate, postnatal care provided to women and newborns, intermittent preventative treatment to prevent malaria in pregnancy and treatment to prevent mother-to-child transmission of HIV. Studies demonstrate the high burden of preventable maternal and newborn morbidity and mortality across PNG. Efforts to improve MNH outcomes need to be escalated.
Keywords: maternal and neonatal health, newborns, postpartum, prenatal, antenatal
Résumé
La Papouasie-Nouvelle-Guinée (PNG) est le pays le plus peuplé du Pacifique, avec plus de 9 millions d’habitants. La géographie accidentée, le mauvais état des routes et les infrastructures limitées rendent difficile d’y prodiguer des soins de santé efficaces, particulièrement dans les zones rurales où vit la plupart de la population. Les femmes et les nouveau-nés en PNG connaissent des taux élevés de morbidité et de mortalité évitables, néanmoins les données fiables sont souvent limitées ou indisponibles. Le but de cet article est de donner un aperçu des recherches sur les indicateurs clés de santé maternelle et néonatale (SMN) réalisées approximativement au cours des 11 dernières années en PNG et qui comparent les conclusions de la recherche avec les estimations mondiales de santé maternelle et néonatale des indicateurs. On a observé des variations considérables dans les indicateurs sur la mortalité (taux de mortalité maternelle, taux de mortalité néonatale et mortinaissance) déclarés dans les études en PNG. La mortalité était en général plus élevée dans les zones rurales. Les taux d’infections sexuellement transmissibles (IST) pendant la grossesse étaient uniformément élevés, alors que l’anémie pendant la grossesse, les naissances avant terme et l’insuffisance pondérale à la naissance variaient largement entre études et lieux. L’allaitement maternel semble avoir fait l’objet de trop rares recherches. On manquait de données disponibles sur d’autres indicateurs tels que le taux de natalité chez les adolescentes, les soins postnatals prodigués aux femmes et aux nouveau-nés, le traitement préventif intermittent du paludisme chez la femme enceinte et le traitement pour prévenir la transmission mère-enfant du VIH. Les études démontrent la lourde charge de morbidité et de mortalité maternelles et néonatales dans l’ensemble du pays. Il faut redoubler d’efforts pour améliorer les résultats de santé maternelle et néonatale.
Resumen
Papúa Nueva Guinea (PNG) es el país más poblado del Pacífico, con más de 9 millones de habitantes. Terreno difícil, carreteras en mal estado e infraestructura limitada dificultan proporcionar servicios de salud eficaces, especialmente en zonas rurales, donde vive la mayoría de la población. Las mujeres y recién nacidos de PNG sufren altas tasas de morbilidad y mortalidad evitables; sin embargo, datos fidedignos a menudo no están disponibles o son limitados. El objetivo de este artículo es proporcionar una visión general de las investigaciones sobre los indicadores clave de salud materna y neonatal (SMN) realizadas en los últimos 11 años en PNG, y comparar los hallazgos de las investigaciones con las estimaciones mundiales de los indicadores de SMN. Se observó considerable variación entre los indicadores de mortalidad (razón de mortalidad materna, tasa de mortalidad neonatal y mortinatalidad) reportados en los estudios realizados en PNG. Por lo general, las zonas rurales tuvieron mayor tasa de mortalidad. Las tasas de infecciones de transmisión sexual (ITS) durante el embarazo fueron más elevadas en todos los estudios, mientras que las tasas de anemia durante el embarazo, parto prematuro y bajo peso al nacer variaron en gran medida entre estudios y entornos. Al parecer, se investigó poco la lactancia. Hubo escasez de datos sobre otros indicadores, tales como la tasa de partos en adolescentes, atención posnatal brindada a mujeres y recién nacidos, tratamiento preventivo intermitente para prevenir la malaria durante el embarazo y tratamiento para prevenir la transmisión del VIH de la madre al niño. Los estudios demuestran la considerable carga que representa la morbimortalidad materna y neonatal evitable en PNG. Es imperativo escalar los esfuerzos por mejorar los resultados de SMN.
Introduction
Papua New Guinea (PNG) is the most populous country in the Pacific with more than 9 million people.1,2 It has one of the highest maternal mortality ratios (MMR) and infant mortality rates (IMR) in the Asia-Pacific region.3–5 The leading causes of maternal death are obstetric haemorrhage (30%), sepsis (5%), embolism (15%) eclampsia (14%) and abortion (7%).2,6
There are four regions in PNG that are made up of 22 provinces and one autonomous region. The majority of the population (80%) live in rural and remote areas with poor roads making access to health care challenging. Health care services are provided at aid posts, health centres, district hospitals and referral hospitals. More than 800 languages are spoken across the country7 making the provision of health care additionally challenging. There are inadequate healthcare facilities, including a lack of an available workforce, equipment, drugs and commodities, and limited water and sanitation infrastructure.2,8 There is a limited national health information system with many hospitals collecting data from paper-based records. Other factors affecting health outcomes include lower status and limited autonomy of women in society, the illegality of abortion, and high rates of early marriage, gender-based violence, poverty and adolescent pregnancy. Lower education and literacy of women exist, as well as a high fertility rate (3.7 per woman).2,9,10 A recent analysis of the available health workforce for reproductive, maternal, newborn, adolescent and child health indicates that PNG only has 24% of the workforce required to meet current needs.11
Maternal and neonatal health are mutually dependent. Childbirth is a crucial time for both mother and child. Essential interventions such as antenatal care visits and skilled birth attendance can prevent the most common causes of maternal and neonatal mortality.12 Moreover, newborns that lose their mothers during or shortly after birth have a greater risk of premature death compared to non-orphaned neonates.12
Maternal health is influenced by a number of direct factors including pregnancy-related complications and communicable diseases, such as HIV and malaria; and non-communicable diseases, such as diabetes, hypertension and depression.13 Access to quality care during pregnancy, labour and birth and in the postnatal period as well as availability of modern contraceptives and subsequent reduced fertility improve maternal health.14,15 Broader social, economic and political determinants such as education for girls, gender equity and poverty reduction are all strongly linked to maternal health.16 It is increasingly recognised that environmental and climate changes broadly affect human health and that women are disproportionally impacted thus affecting maternal health.17,18
Research has shown that integrating maternal and newborn care can improve overall health outcomes19 although this can be challenging in many countries, including PNG. Improving maternal and neonatal health is also crucial for PNG to meet the Sustainable Development Goals (SDG) targets for MNH indicators. In 2009, maternal health was considered a national emergency due to the high MMR9 and a number of strategies were implemented including midwifery education, improving access to modern forms of contraception, and emergency obstetric training. It is not clear whether significant improvements have been made since this time due to challenges with measurement. Identifying the key areas of concern and highlighting the areas of greatest need and focus are essential. However, there has not been a comprehensive review of research related to maternal and neonatal health indicators in PNG2, 3, 6,8,10 nor an assessment of how levels of maternal and newborn outcomes identified in these studies relate to corresponding global metrics, for example, the World Health Organization's (WHO) 100 Core Health Indicators, also known as the Global Reference List.20 The WHO Global Reference List is a standard set of core indicators prioritised by the global community to provide concise information on the health situation and trends, including responses at national and global levels.20 The list includes the key indicators of relevance for country, regional and global reporting across the full spectrum of global health priorities, including the new and emerging priorities reflected in the health and health-related SDGs, such as universal health coverage, non-communicable diseases and other key health-related environmental, social, economic and behavioural risk factors. The indicators address health status, risk factors, service coverage and health systems measures and include more than 33 indicators specifically related to reproductive, maternal, newborn, child and adolescent health.
The aim of this paper was to provide an overview of research on MNH indicators conducted approximately over the past decade in PNG; to assess the available data against key global MNH indicators from the Global Reference List; and to identify current knowledge gaps that require action for the future. We also examined where the studies had been undertaken to highlight areas where little evidence was available. The purpose of the review was to have, for the first time, a compilation of all the evidence related to the key indicators for MNH in PNG.
Methods
Databases, search strategy and selection criteria
This narrative review was informed by the guidelines of Snilstveit et al.21 and Green et al.22 We conducted a systematic search to identify eligible articles according to pre-specified eligibility criteria, including randomised controlled studies and observational studies (i.e. cohort, cross-sectional or case–control studies). We searched Medline (Ovid), Emcare Ovid, Scopus and the Cochrane Library using keywords related to pregnant and labouring women, newborns and postnatal care in Papua New Guinea (Box 1).
Box 1: Search terms.
| Topic | Search terms |
|---|---|
| Maternal and reproductive health | antenatal or prenatal or perinatal, maternal, reproductive, antenatal care, pre, peri- and postnatal care, postpartum, family planning, breastfeed*, breastfed, breast feed*, labour, labor, birth, preterm, obstetric, caesarean, c section, miscarriage, abort*, contracept*, midwife*, midwiv*, hiv, aids, human immunodeficiency, malaria*, anemi*, anaemi* |
| Neonatal health | infant, infancy, newborn, neonate*, stillbirth*, fetal, fetus, foetal, foetus, neonatal, ART, intermittent preventative treatment, ipt |
| Country/location | Papua New Guinea |
Grey literature was searched on Google Scholar (first 10 hits) and OpenGrey. We also hand-searched relevant local and regional journals that may not have been indexed including the Papua New Guinea Medical Journal, Pacific Journal of Reproductive Health and the Australian and New Zealand Journal of Obstetrics and Gynaecology for eligible articles. Reference lists of included studies were screened to identify any other eligible studies. Only articles in English were considered as in our experience most research conducted in PNG is by English-speaking researchers and hence published in English.
Studies published or available online (pre-prints) between 1st January 2008 to 31st December 2018 which addressed the populations of interest (pregnant or labouring women, neonates within the first 28 days of life, midwives, nurses, obstetricians and other relevant MNH healthcare providers) were included. Research papers that were published within the selected time frame but included research data that were exclusively collected before 2008, were excluded. Data from the 2006 Demographic Health Survey were included as comparators as these data were the most recent national data available.23 Studies of non-pregnant populations, or populations where pregnant women were not described separately, were not eligible. Articles were excluded if they did not focus or report data separately for neonates within the first 28 days. Commentaries, letters to the editor, narratives, case reports, case series, reviews or studies that focused primarily on knowledge, attitudes, experiences and perceptions of the targeted population with regard to MNH were also not eligible.
Data extraction
Two reviewers independently screened titles, abstracts and full texts of identified citations and excluded those that were not eligible. Disagreements were resolved by discussion or consultation with a third reviewer. Data from included articles were extracted into an Excel spreadsheet. For each included study, we extracted information on study characteristics, aim, design, sample size, population, setting and findings. Study findings were reported narratively; meta-analysis was not feasible due to the diversity of studies, designs and findings.
Selection of indicators from the WHO Global Reference List
We assessed the Global Reference List of 100 Core Health Indicators and selected 21 key indicators most proximally related to MNH (Table 1). These indicators were used to assess the progress of maternal and neonatal health outcomes in PNG.20
Table 1. Maternal and newborn health indicator framework.
| Domain | Indicator | Measure |
|---|---|---|
| Mortality | 1. Maternal mortality ratio (MMR) | per 100,000 live births |
| 2. Neonatal mortality rate (NMR) | per 1000 live births | |
| 3. Stillbirth rate | per 1000 live births | |
| Reproductive health | 4. Contraception prevalence rate (CPR) | % |
| 5. Obstetric and gynaecological admissions owing to abortions | % | |
| Pregnancy | 6. Adolescent birth rate | % and per 1000 live births |
| 7. STI prevalence in pregnancy | % | |
| 8. HIV prevalence in pregnancy | % | |
| 9. Malaria prevalence in pregnancy | % | |
| 10. Anaemia prevalence in pregnancy | % | |
| 11. Antenatal care coverage | % | |
| 12. Prevention of mother-to-child transmission of HIV/ pregnant women on ART | % | |
| 13. Intermittent preventative treatment (IPT) in pregnancy | % | |
| Birth | 14. Births attended by skilled health personnel | % |
| 15. Caesarean section rate | % | |
| 16. Preterm rate | % | |
| 17. Low birthweight prevalence | % | |
| Postpartum | 18. Postpartum care for mothers | % |
| 19. Postpartum care for neonates | % | |
| 20. Early initiation of breastfeeding | % | |
| 21. Exclusive Breastfeeding | % |
Data analysis
Included literature was searched for data to inform these 21 maternal and neonatal health indicators. We determined the number and characteristics of studies addressing each indicator and reported relevant results from these studies against the relevant national estimate for that indicator. Where available, corresponding national and regional estimates derived from the relevant United Nations estimates were provided, as well as results from the last PNG Demographic Health Survey (DHS) in 2006 as described earlier.23
Results
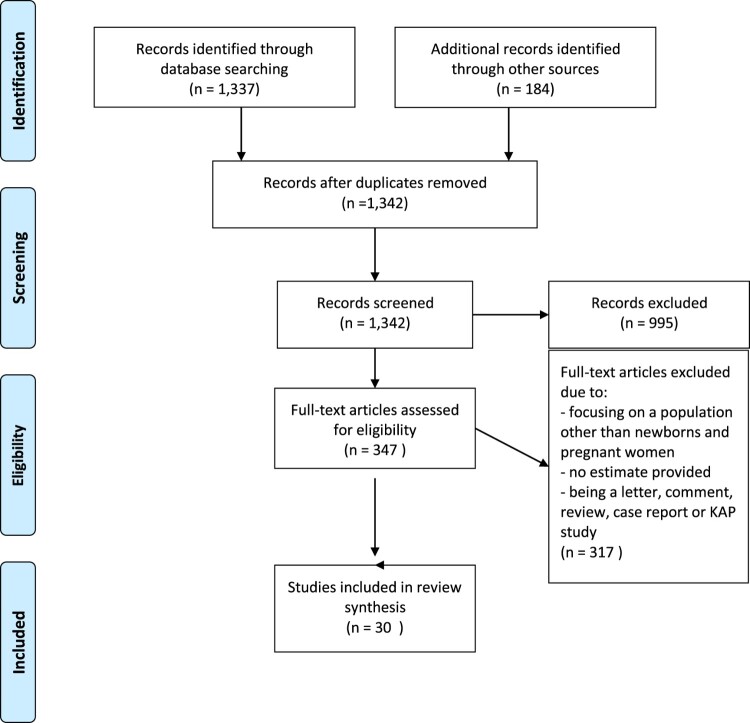
The literature search resulted in 1521 articles. After the removal of 179 duplicates, 1342 abstracts were screened. In total, 995 records were excluded. Full-text screening resulted in articles being excluded mainly due to the study focus not being on newborns or pregnant women, when the outcome was not being reported or when the article was an opinion piece, a review, case report or a KAP study. This reduced the included literature to 30 articles (Figure 1).
Figure 1.
PRISMA flow diagram for MNH indicators review
Characteristics of included studies
In total, 30 studies that addressed MNH indicators in PNG were included. The majority of the studies (22/30) were published within the last five years (2013–2018). Most studies were conducted in four provinces of PNG – Madang (n = 12), Central and National Capital District (n = 9) and the Eastern Highlands (n = 7) (Table 2). There were seven studies set in mainly rural areas. Twenty-one were hospital-based. One province (Madang) had more research conducted in health centres or posts (n = 5) and in rural areas (n = 2) compared to other provinces. The majority of PNG provinces had limited data for the indicators of interest. One province, Jiwaka, had no data, although the province was only officially formed in 2012.
Table 2. Studies reporting maternal and neonatal health (MNH) indicators.
| Impact | Health focus | Indicator | Number of studies* | References |
|---|---|---|---|---|
| Mortality | Maternal health | Maternal mortality ratio (MMR) | 4 | 24–27 |
| Neonatal health | Neonatal mortality rate (NMR) | 1 | 26 | |
| Stillbirth rate | 8 | 24–26, 28–32 | ||
| Reproduction | Reproductive health | Contraception prevalence rate (CPR) | 3 | 33–35 |
| Obstetric and gynaecological admissions owing to abortions | 2 | 36, 37 | ||
| Pregnancy | Maternal health | Adolescent birth rate | 0 | n/a |
| STI prevalence in pregnancy | 6 | 25, 38–42 | ||
| HIV prevalence in pregnancy | 7 | 25, 28, 32, 35, 39, 41, 43 | ||
| Malaria prevalence in pregnancy | 7 | 27, 29, 31, 32, 44–46 | ||
| Anaemia prevalence in pregnancy | 6 | 25, 29, 31, 32, 35, 46 | ||
| Antenatal care coverage | 3 | 27, 47, 48 | ||
| Prevention of mother-to-child transmission of HIV/pregnant women on ART | 0 | n/a | ||
| Intermittent preventative treatment (IPT) in pregnancy (prevalence) | 0 | n/a | ||
| Birth | Maternal health | Births attended by skilled health personnel | 2 | 24, 48 |
| C-section rate | 5 | 28, 30, 40, 49, 50 | ||
| Neonatal health | Preterm rate | 3 | 32, 43, 44 | |
| Low birthweight prevalence | 5 | 29, 31, 32, 43, 51 | ||
| Postpartum | Maternal health | Postpartum care for mothers | 0 | n/a |
| Neonatal health | Postpartum care for neonates | 0 | n/a | |
| Early initiation of breastfeeding | 2 | 52, 53 | ||
| Exclusive breastfeeding | 1 | 53 |
*Some studies are counted more than once when they address several MNH indicators.
The 30 studies addressed 15 of the 21 Core Health Indicators (Table 2). Nine indicators were reported in several studies, including stillbirth rate (n = 8); HIV prevalence in pregnancy (n = 7); malaria in pregnancy (n = 7); anaemia in pregnancy (n = 6); STI prevalence in pregnancy (n = 6); caesarean section rate (n = 5) and low birthweight prevalence (n = 5). Few studies addressed the other indicators.
Mortality indicators
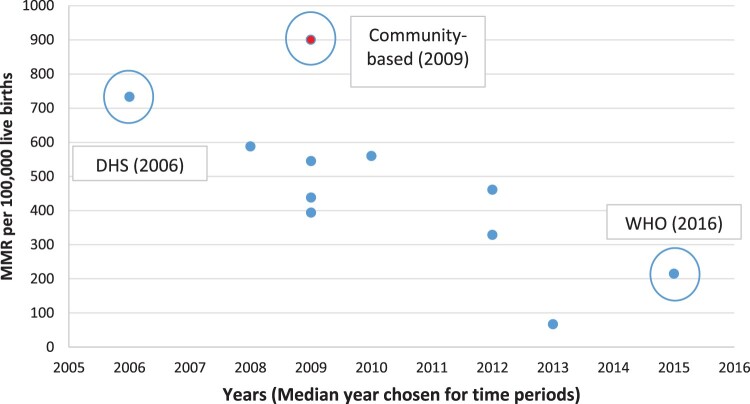
Mortality indicators (MMR, NMR and stillbirth) had a range of estimates (68–900 per 100,000 live births). Of the four studies that provided MMR data, three reported on facility-based estimates and only one study gave a community-based estimate. All three facility-based studies were conducted either at the Modilon General Hospital (2008–2012/2009–2014) or the Port Moresby General Hospital (2012–2013) with estimates for MMR ranging from 68 to 588 per 100,000 live births.25,27 The only community-based study had an even higher MMR estimate, ranging between 600–900 per 100,000 live births in rural settings.24 Three of the four studies were based on case notes of major hospitals such as the Modilon General Hospital in Madang and the Port Moresby General Hospital in the National Capital District. While the sample of births was generally high (10,000–20,000), the actual number of included cases for the calculation of estimates is often small, such as a maternal near-miss study at Modilon General Hospital conducted by Bolnga et al based on 52 near-miss case reviews.27
The official estimates for MMR vary greatly in PNG. The WHO's MMR estimate is 215 per 100,000 live births (2015)10 and the DHS (2006) estimate is 733 per 100,000 live births for facility- and community-based births.23 These are very different from local PNG research estimates which range from 68 to 900, although some of the local estimates are facility-based and others community-based surveys.24 Figure 2 provides a graphical view of the MMRs from facility-based studies and WHO/DHS reports which include facility and community deaths. Details of each study are provided in Appendix 1 (see Supplemental data).
Figure 2.
Dispersion of MMR in PNG over time, by different studies, DHS, and WHO reports
Notes: (1) Each point represents a specific MMR provided in a study, DHS or UN report for facility-based births. DHS and WHO data includes facility and community-based estimations. (2) There are 4 studies that reported estimates for MMR but one study24 gives 6 estimates. As each dot point re-presents one estimate, there are more dot points than studies. The red dot is a community-based study, the blue dots are facility based and the green dot is the DHS data. (3) The DHS data23 is out of the reference period but is included as being the only government reference point during the time period.
Only one facility-based study provided information on NMR estimates based on primary research26 with an estimate of 14 deaths per 1000 live births (2016). The UN estimate for NMR differs greatly and is estimated to be 48.4 per 1000 live births in 2012 using a facility-based estimate from Modilon Hospital in 2014.5
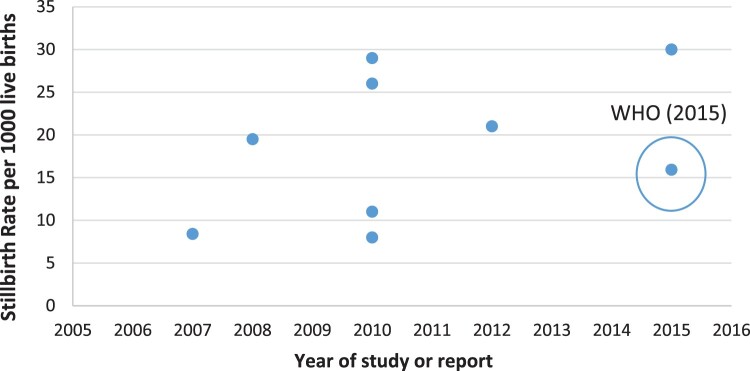
Most stillbirth indicator estimates (5 of 8 studies) originate from hospital settings such as the Goroka General Hospital (Goroka province), Port Moresby General Hospital (National Capital District) and the Modilon Hospital (Madang province) with a range of 8–30 per 1000 live births.25,26,28,30,43 Only one study provides a rural estimate for the catchment area of health centres with an estimate of 8 per 1000 live births.29 Three included studies, which took place at health care centres, did not specify whether the region was considered rural, peri-rural, urban or peri-urban and again showed a range of 8–26 per 1000 live births.31,32,43 Overall, five of the eight studies estimated the stillbirth rate between 20 and 30 per 1000 live births.25,26,30,31,43.
The WHO estimate for stillbirth of 15.9 per 1000 live births in 2015,54 using facility-based studies, lies at the mid-range of estimates from local PNG research. There is no DHS or WHO Western Pacific Regional estimate available. Figure 3 provides a graphical view of the estimated stillbirth rate in the studies and the UN/WHO estimates.
Figure 3.
Dispersion of stillbirth rates in PNG over time by different studies, and WHO reports
Notes: (1) Each point represents an estimate from a study, or UN report for PNG. All estimates are facility-based. (2) The 8.4 per 1000 live births for 2008 includes some data (combined) for 2007 and therefore is included as 2008.
Indicators with consistent estimates
A number of indicators were supported by reasonably consistent data from multiple, independent studies showing consistently high rates of STIs in pregnancy especially chlamydia, gonorrhoea and syphilis. The rate of chlamydia was 20–23% in three studies 38,39,41 and 11% in one.42 These studies covered six provinces across the country from 2011–2015. Similarly, the prevalence of gonorrhoea was measured in four studies with a range of 10–14%.38,41,42,55 These were rural and urban populations in the same provinces over the same time frame. There were four studies that examined the rates of syphilis with a range from 2.0% to 4%.12,25,28,41 These data were from four provinces, but half of the studies included the national capital, Port Moresby. The slightly lower rates were from outside the capital.
The HIV prevalence in pregnancy was examined in seven studies with a range of 0.3–4.8%.25,28,32,35,40,41,43 The higher rate (4.8%) was reported from Goroka, a regional town in the rural Eastern Highlands Province which provided data for 2005–2008.35 The lowest rate (0.3%) was reported from women attending the Port Moresby General Hospital (in the capital) between 2006 and 2010.28 Five of the seven studies were conducted more than five years ago (2006–2012) with two studies conducted more recently; one showing a prevalence rate of 1.6% in an urban area41 and the other a rate of 0.8% in a rural and semi-rural area.31
Antenatal care coverage (ANC) was reported in three studies with a range of 35–80%.27,47,48 Two of these studies did not indicate the number of the total ANC visits of women during pregnancy, with one that reported the lowest ANC coverage (35% of 52 reviewed cases at Modilon General Hospital)27 and the other that reported a higher ANC coverage of 55–71% in East Sepik Province. 2007/2010.48 Only one study, with 390 women attending maternal health care services in East Sepik Province in 2009, showed that 79% of women had at least one ANC visit during their last pregnancy and overall, 66.4% had more than three ANC visits during their last pregnancy.47 None of the included studies reported on the timing of ANC visits during pregnancy or the updated (as of 2016) number of recommended ANC visits by the WHO, which is eight contacts in total56 although this recommendation is probably too recent to be reflected in the studies.
Indicators with some variability
Some indicators showed more variability, probably related to differences in study context and sample population. For example, while the prevalence of anaemia in pregnancy was higher than in many other settings, there was still a wide range in the six studies identified. Overall, the rate of any anaemia (that is, haemoglobin levels <11 g/dL) ranged from 84% of women at their first antenatal visit (2008–2011) to 16% in women from a number of rural health facilities.29,46 In Port Moresby General Hospital, the rate was 23%25 which was the same as the district hospital in Madang with a rate of 23% from 2009 to 2012.31 Goroka district hospital had a rate of 47% of anaemia (haemoglobin <10 g/dL) and 33% severe anaemia (haemoglobin <8 g/dL) from 2005–2008.35 Data for 2009–2012 from the Madang province showed a rate of 73% (using <11 g/dL).32 There have been no studies reporting the prevalence of anaemia in the general pregnant population since 2012.
The rate of preterm birth was reported from three studies with a range from 6.6% to 18%.32,43,44 The majority were from district hospitals between 2006 and 2012.32,43 One study with a preterm birth rate of 8.4% among 1451 women in Madang did not indicate the setting of preterm births, that is health facility vs. hospital or rural vs. urban (Table 3).44 The prevalence of low birth weight was included in five studies and was consistently high although with a variation from 15% to 24%.29,31,32,43,51 The highest prevalence (24%) was found from pregnant women with newborns admitted to the Special Care Nursery at the Modilon Hospital, Madang (2009–2013).51 The other rates ranged from 15% to 18%.29,31,32,43 These studies were conducted between 2006 and 2013. The national data from the UN/WHO gives a rate of 11% (2008–2012),57 which is considerably lower than some estimates from local research.
Table 3. Origin and characteristics of included studies.
| Region | Provinces (n = 23) | Capital | References | No. of studiesa (total) per Province |
Number of studies per category | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | Health centre or post | Hospital and health care or post | Setting not stated | Urban | Rural | Urban and rural | Area not stated | |||||
| Highlands | Hela | Tari | 38, 39 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 1 |
| Southern Highlands | Mendi | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| Enga | Wabag | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | |
| Western Highlands | Mount Hagen | 24, 38 | 2 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | |
| Jiwaka | Banz | n/a | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Chimbu | Kundiawa | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | |
| Eastern Highlands | Goroka | 36, 38 | 8 | 4 | 3 | 1 | 0 | 0 | 1 | 2 | 5 | |
| Southern Region | Western | Daru | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Gulf | Kerema | 24, 52 | 2 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | |
| Central | Port Moresby | 24, 25, 28, 33, 38, 40, 49, 50 | 9 | 6 | 2 | 1 | 0 | 6 | 0 | 2 | 1 | |
| National Capital District | ||||||||||||
| Milne Bay | Alotau | 24, 41 | 2 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | |
| Oro | Popendetta | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| Momase | Morobe | Lae | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Madang | Madang | 26, 27, 29–32, 42, 44–46, 51, 53 | 12 | 4 | 7 | 0 | 1 | 0 | 3 | 2 | 7 | |
| East Sepik | Wewak | 24, 34, 47, 48 | 4 | 0 | 3 | 1 | 0 | 0 | 2 | 1 | 1 | |
| West Sepik | Vanimo | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| New Guinea Islands | Manus | Lorengau | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| New Ireland | Kavieng | 24 | ||||||||||
| 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | ||||
| East New Britain | Kokopo | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| West New Britain | Kimbe | 24 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| Bougainville | Buka | 24 | ||||||||||
| 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | ||||
| Studies at Multi-provincial level (PNG)b | 24, 38, 39, 53 | 4 | 0 | 3 | 1 | 0 | 0 | 1 | 2 | 1 | ||
| Total per categoryc | 13 | 14 | 1 | 1 | 7 | 6 | 4 | 13 | ||||
aSome studies are counted more than once when they were conducted in several provinces/categories.
bStudies are also counted towards each province category where applicable.
cWithout studies at multi-provincial level, all references are only counted once for total number per category.
Note: Some studies do not disclose information for individual categories e.g. urban/rural, in that case these studies are omitted from count for the respective category.
The rate of caesarean section was mostly consistent across the five studies at less than 10%, except for one study from the Modilon Hospital in Madang which reported a rate of 27% between 2014 and 2016.30 The remaining studies were from Port Moresby General Hospital.28,40,49,50 Two of these studies were conducted over several decades giving an estimate of 3.9% (1977–2010)40 and 4.4% (1977–2015)50 respectively. The most recent study from Port Moresby General Hospital indicated a caesarean section (CS) rate of 3.8% (2015).50 Two older studies from the same hospital indicated the CS rate each at 4.9% (2007) (29) and 7.3% (2007–2008)28 despite being conducted in a similar time period.
Indicators where there are gaps in knowledge
The proportion of births attended by a skilled birth attendant is one important measure of access to care but has received very little attention in PNG in formal research. There were only two studies with an estimate of 28% (2007–2010)48 and 39.1% (2009–2012).24
Indicators for breastfeeding (early initiation and exclusive breastfeeding) seem to have had little attention in previous research conducted in PNG. The indicator for early initiation of breastfeeding was informed by two studies conducted in 2013 and 2017.52,53 The percentage of early initiation of breastfeeding ranged widely between the two studies indicating a prevalence of 36.1% (2017)52 to 69% (2013),53 in rural and isolated communities in Madang Province and Gulf Province, respectively. The Western Pacific regional average of 42%28 lies at the midrange of data derived from PNG-based research. However, the DHS (2006) estimate for breastfeeding, 94% in urban and 97% in rural areas of PNG,23 is significantly higher and in contrast to the more contemporary estimate of included studies in two rural provinces. Exclusive breastfeeding is similarly deficient of research as only one study was identified.53 The study (data from 2012)53 indicated a prevalence of only 17% and included mothers living in rural areas of the Eastern Highlands and Madang Provinces. This estimate is lower than the PNG estimate by the WHO (56% in 2012),58 the PNG DHS estimate (80% in 2006)23 and the Western Pacific regional average (38%).59
Gynaecological admissions owing to terminations of pregnancy are a difficult indicator to determine, due to the illegality of abortion in PNG except when the woman's life is at risk.60 No estimate by the WHO/UN, DHS or for the Western Pacific Region could be identified. However, two included studies showed an institution-level prevalence of 26.7% for induced abortions at the Goroka Hospital in 201137 and 24% at the Eastern Highlands Provincial Hospital in 2012,36 indicating a hidden and largely under-researched issue within PNG.
There were five key areas where no data were identified in this review. These were: adolescent birth rate; postnatal care for the mother or for the baby; the prevalence of women receiving intermittent preventative treatment (IPT) to prevent malaria in pregnancy; and treatment to prevent mother-to-child transmission of HIV. Appendix 1 (see Supplemental data) provides further in-depth information with regard to international, national and local indicators in PNG within the last 10 years.
Discussion
This is the first study to have collated the research related to the key indicators for MNH in PNG. Our review relied on articles published within the last 11 years. Given the known high rates of morbidity and mortality and the overall high burden of disease, the lack of research, especially in key areas, is concerning. The MMR in PNG is considered the highest in the region, despite studies reporting widely varying MMR. The estimated MMR within communities ranged from 215 to over 900 per 100,000 live births, suggesting the WHO estimate of 215 per 100,000 live births may be under-estimating the true burden. Some of the variation is expected as some study samples were hospital-based or derived from rural populations. Given that only 55% of women in PNG give birth in a health facility,61 the estimation of deaths in the community (at home or in the village) may be limited especially for stillbirths and maternal and neonatal deaths.
Our findings support the conclusions of Mola and Kirby in 2013,24 which highlighted the discrepancies in estimations and showed how not knowing the national MMR was an additional challenge for health workers, policymakers and development partners in agreeing on strategies to meet the Sustainable Development Goals.62 It also undermines efforts to know whether maternal mortality reduction strategies are effective or not. Despite the measurement challenges, it is unquestioned that the MMR is too high – efforts to reduce preventable maternal mortality need to be escalated.
The rate of stillbirth is another area of uncertainty. In recent years there has been increasing interest in the area of stillbirth especially counting and measuring the global and national burden and identifying ways to end preventable stillbirth.63 In this review stillbirth rate ranged from 8 to 30 per 1000 live births. A recent analysis in a prospective study from South Africa showed that the main causes of stillbirth were maternal medical conditions (21%), primarily hypertensive disease, infections of the placenta and fetus (19%), pathological placental conditions (19%) and obstetric complications (18%). Numerous specific bacteria were also implicated, most commonly Enterococcus faecalis (14%) and Escherichia coli (10%).64 Given the low coverage of antenatal care in PNG and the high rates of STIs and potentially other infections, it is likely that these causes would be similar. Scaling up quality antenatal and intrapartum care is essential to addressing preventable stillbirth regardless of the rate.55
Data are lacking in a number of important indicators, which means the capacity for the country to develop evidence-based policy is limited. For example, there were no studies found assessing adolescent birth rate despite PNG being a country with a high rate of adolescents. Postnatal care for mother and baby is another area lacking evidence even though this is a critical time period, especially for the neonate with 40% of deaths of children globally occurring in the first week of life.65 Research addressing exclusive breastfeeding is limited.53
The proportion of women who have a “skilled birth attendant” is another area with few studies. The measure is often used interchangeably with birth in a facility, although this may not always be true. A birth that occurs in a facility does not mean it is supervised by a skilled birth attendant and a health care provider at the facility may not have the necessary skills to support a safe birth. The Demographic Health Survey for PNG (2016–2018), which was published outside this study's time frame, reported that only 56.5% had a “skilled provider” at the birth; however, the definition of a skilled provider includes doctors, midwives, nurses or trained village health volunteers. It is possible that not all these providers have the necessary skills or access to resources for care. There is now a new definition of skilled health personnel providing care during childbirth from the World Health Organization and partners. If this is applied in PNG, it is likely to further reduce the levels as it requires competent MNH professionals who are educated, trained and regulated to national and international standards.66 Research on the application and implementation of this new indicator is needed in many counties, including PNG.
While data was limited in a number of areas, hospital-based annual reports have collated data on a number of indicators. For example, the Port Moresby General Hospital, which has more than 14,000 births per year, produces annual reports.67 Data from these reports over the last decade (2009–2018) show an MMR of between 82 and 149 per 100,000 live births, which is considerably lower than the other estimates included in this review, and a stillbirth rate of 15.4–21.3 per 1000 live births, which is reasonably consistent with other estimates. The data from 2018 show that 2.7% of women attending the antenatal clinics in this referral hospital (in the National Capital District) had HIV infection (compared with 2.8% prevalence nationally). The rate of severe anaemia (<8 g/dL) was 7% with an overall rate of any anaemia (<11 g/dL) of 33%, which is lower than some estimates from different provinces. The caesarean section rate was 5.6%, a figure that has been consistent over the past decade (range 4.0–6.5%). National data that combine the annual reports from all maternity settings would considerably add to the body of knowledge regarding MNH in PNG.
The key indicators report from the Papua New Guinea Demographic and Health Survey (2016–2018) has recently been released61 and the findings are similar to the research synthesised in this paper and highlight the ongoing challenges. The DHS reports a neonatal mortality rate in the previous five years of 20 per 1000 live births but the rate of stillbirth or maternal death was not reported. The contraceptive prevalence rate (CPR) among married women ranged from 18% among women age 15–19 to a peak of 42% among women age 30–39 before declining to 33% among women age 45–49. Urban women were more likely to use a contraceptive method than women in rural areas (50% and 35%, respectively). Adolescent pregnancy was common with more than one in 10 (12%) women aged 15–19 having begun childbearing. This is similar to the 2006 DHS where the proportion was 13%.23 More than three-quarters (76%) of women who gave birth in the five years preceding the DHS received antenatal care from a skilled provider at least once for their last birth. This is similar to the 2006 DHS and in the mid-range of the other research found for this paper (35–79%). Less than half (49%) of women had four or more ANC visits which is lower than the 2006 DHS (55%).23 The challenges with the definition of a skilled provider remain as discussed earlier. A postnatal check-up within two days after birth was reported by 46% of women. This is the first time this estimate has been reported which is important.
While the indicators included in this paper provide a snapshot of the current state of health care in a country, other research is also necessary to better understand the mechanisms to improve or address indicators. In MNH this includes addressing availability, accessibility, affordability and quality of care.68 A clearer understanding of the capacity of the health workforce to deliver effective reproductive, maternal, newborn, child and adolescent health (RMNCAH) interventions at scale is also needed especially in a complex environment such as PNG.69 PNG is facing significant health workforce shortages which will considerably hamper any efforts to provide quality care that has the capacity to improve outcomes.11 Research is needed to determine how best to build a quality RMNCAH workforce, especially for midwives and their deployment within an enabled environment, especially in rural and remote settings.
Strengths and limitations
This is the first systematic attempt to better understand the status of MNH research in PNG using the WHO's Core Health Indicators as a framework. We aimed to include all eligible studies conducted within the stated timeframe, including reviewing papers from PNG scientific journals. We recognise the residual possibility of missing potential eligible studies although the broad search strategy should have mitigated against this. We chose to focus only on studies that directly addressed the selected indicators. It may be that there are implementation or intervention studies (for example, addressing the treatment of malaria) that include prevalence estimates. We have endeavoured to use these where possible by reviewing all MNH studies in PNG for a broader analysis but it is possible that some were missed.
Conclusion
This is the first study to have collated MNH studies in PNG and compared their findings with 21 of the 100 Core Health Indicators from WHO. We have shown that there is significant variation in some of the key MNH indicators and some areas lack adequate data on which to base policy decisions.
Despite the variations, the studies included in this analysis show the high burden of disease across the country. There are high rates of malaria, STIs, anaemia, preterm birth and low birth weight. These all have long term significance for the health of the country and the capacity to contribute to economic benefits in the future. PNG, and other LMICs, need access to up-to-date data from national surveys and research in order to be able to address the SDGs and improve health in their own countries.
Role of the funding source
The funder of this review had no role in study design, data collection, data analysis, data interpretation, or writing of the report. GR. JV, GM, JB and CH had full access to all the data of the review and had final responsibility for the decision to submit for publication.
Supplementary Material
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data
Supplemental data for this article can be accessed at https://doi.org/10.1080/26410397.2019.1686199.
ORCID
Joshua P. Vogel http://orcid.org/0000-0002-3214-7096
Glen Mola http://orcid.org/0000-0002-9500-7234
Caroline S. E. Homer http://orcid.org/0000-0002-7454-3011
References
- 1.UNDP About Papua New Guinea: United Nations Development Programme. Available from: http://www.pg.undp.org/content/papua_new_guinea/en/home/countryinfo.html. 2019 [cited 2018 Oct 12].
- 2.Department of National Planning and Monitoring , Papua New Guinea – millenium development goals fund summary report 2015. 2015, Waigani: Government of PNG.
- 3.Williams C. Maternal deaths and their impact on children in Papua New Guinea. Aust N Z J Public Health. 2014;38:405–407. doi: 10.1111/1753-6405.12263 [DOI] [PubMed] [Google Scholar]
- 4.Dennis A. Reducing maternal mortality in Papua New Guinea: contextualizing access to safe surgery and anesthesia. Anesth Analg. 2018;126(1):252–259. doi: 10.1213/ANE.0000000000002550 [DOI] [PubMed] [Google Scholar]
- 5.United Nations ESCAP A.U., Making it happen – Asia-Pacific Regional MDGs Report 2014/15 – Technology, finance and statistics for sustainable development in Asia and the Pacific 2015, Bangkok: United Nations ESCAP, ADB & UNDP.
- 6.Countdown 2030 Countdown country dashboards – Papua New Guinea. 2018 [cited 2019 Apr 24]; Available from: http://profiles.countdown2030.org/#/ds/PNG.
- 7.Eberhard D, Gary F, Charles D. Ethnologue: languages of the World Papua New Guinea. 2019 [cited 2019 Feb 10]. Available from: https://www.ethnologue.com/country/PG.
- 8.World Bank Reproductive health at a glance Papua New Guinea. 2011, New York (NY): World Bank.
- 9.National Department of Health Ministerial Taskforce on maternal health in Papua New Guinea. 2009, Port Moresby: Government of Papua New Guinea.
- 10.World Health Organization Trends in maternal mortality 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Division. 2015, Geneva: World Health Organization.
- 11.UNFPA UNFPA the state of the Pacific’s reproductive, maternal, newborn, child and adolescent health workforce. 2019, Suva, Fiji: UNFPA.
- 12.Lassi Z, Majeed A, Rashid S, et al. The interconnections between maternal and newborn health – evidence and implications for policy. J Matern-Fetal Neonatal Med. 2013;26:3–53. doi: 10.3109/14767058.2013.784737 [DOI] [PubMed] [Google Scholar]
- 13.Graham W, Woodd S, Byass P, et al. Diversity and divergence: the dynamic burden of poor maternal health. The Lancet. 2016;388(10056):2164–2175. doi: 10.1016/S0140-6736(16)31533-1 [DOI] [PubMed] [Google Scholar]
- 14.Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388(10056):2176–2192. doi: 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
- 15.Campbell OM, Calvert C, Testa A, et al. The scale, scope, coverage, and capability of childbirth care. Lancet. 2016;388(10056):2193–2208. doi: 10.1016/S0140-6736(16)31528-8 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization Social determinants approach to maternal deaths. 2019 [cited 2019 Aug 4]; Available from: https://www.who.int/maternal_child_adolescent/epidemiology/maternal-death-surveillance/case-studies/india-social-determinants/en/.
- 17.Kruk M, Kujawski S, Moyer CA, et al. Next generation maternal health: external shocks and health-system innovations. Lancet. 2016;388(10057):2296–2306. doi: 10.1016/S0140-6736(16)31395-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Homer C, Hanna E, McMichael A.. Climate change threatens the achievement of the millennium development goal for maternal health. Midwifery. 2009;25(6):606–612. doi: 10.1016/j.midw.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 19.Bhutta Z, Lassi ZS., Blanc A, et al. Linkages among reproductive health, maternal health, and perinatal outcomes. Semin Perinatol. 2010;34(6):434–445. doi: 10.1053/j.semperi.2010.09.002 [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Global Reference List of 100 core health indicators (plus health-related SDGs) Report No.: CC BY-NC-SA 3.0 IGO. 2018, Geneva: World Health Organization.
- 21.Snilstveit B, Oliver S, Vojtkova M.. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Eff. 2012;4:409–429. doi: 10.1080/19439342.2012.710641 [DOI] [Google Scholar]
- 22.Green B, Johnson C, Adams A.. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101–117. doi: 10.1016/S0899-3467(07)60142-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Statistical Office of Papua New Guinea Papua New Guinea demographic and health survey 2006. 2009, Port Moresby: Government of Papua New Guinea.
- 24.Mola G, Kirby B.. Discrepancies between national maternal mortality data and international estimates: the experience of Papua New Guinea. Reprod Health Matters. 2013;21(42):191–202. doi: 10.1016/S0968-8080(13)42725-8 [DOI] [PubMed] [Google Scholar]
- 25.Tanimia H, Jayaratnam S, Mola GL, et al. Near-misses at the Port Moresby General Hospital: a descriptive study. Aust N Z J Obstet Gynaecol. 2016;56(2):148–153. doi: 10.1111/ajo.12430 [DOI] [PubMed] [Google Scholar]
- 26.Bolnga J, et al. Trends in maternal and perinatal mortality in a provincial hospital in Papua New Guinea: A 6-year review. P N G Med J. 2016;59(1/2):34–37. [Google Scholar]
- 27.Bolnga J, et al. Insights into maternal mortality in Madang province, Papua New Guinea . Int. J. Gynecol. Obstet. 2014;124(2):123–127. doi: 10.1016/j.ijgo.2013.08.012 [DOI] [PubMed] [Google Scholar]
- 28.Mola G, Kombuk B, Amoa A.. Poor weight gain in late third trimester: a predictor of poor perinatal outcome for term deliveries? P N G Med J. 2011;54:164–173. [PubMed] [Google Scholar]
- 29.Karl S, Li Wai Suen CSN, Unger HW, et al. Preterm or not – an evaluation of estimates of gestational age in a cohort of women from rural Papua New Guinea. PLoS ONE. 2015;10(5). DOI: 10.1371/journal.pone.0124286. doi: 10.1371/journal.pone.0124286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bolnga J, Morris M, Totona C, et al. Maternal near-misses at a provincial hospital in Papua New Guinea: A prospective observational study. Aust N Z J Obstet Gynaecol. 2017;57(6):624–629. doi: 10.1111/ajo.12650 [DOI] [PubMed] [Google Scholar]
- 31.Unger H, et al. Factors associated with ultrasound-aided detection of suboptimal fetal growth in a malaria-endemic area in Papua New Guinea. BMC Pregnancy Childbirth. 2015;15:83. doi: 10.1186/s12884-015-0511-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ome-Kaius M, Unger HW, Singirok D, et al. Determining effects of areca (betel) nut chewing in a prospective cohort of pregnant women in Madang province, Papua New Guinea. BMC Pregnancy Childbirth. 2015;15(0):177. doi: 10.1186/s12884-015-0615-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanga K, Mola G, Wattimena J, et al. Unintended pregnancy amongst women attending antenatal clinics at the Port Moresby General Hospital. Aust N Z J Obstet Gynaecol. 2014;54(4):360–365. doi: 10.1111/ajo.12219 [DOI] [PubMed] [Google Scholar]
- 34.Flint J, Morisause M.. Identifying barriers to accessing family planning contraception among women aged 15-49 years in Maprik District, East Sepik province, Papua New Guinea, 2014. Pacifc J Reprod Health. 2017;1(5):232–2239. doi: 10.18313/2017.902 [DOI] [Google Scholar]
- 35.Sanga K, de Costa C, Mola G.. A review of maternal deaths at Goroka General Hospital, Papua New Guinea 2005–2008. Aust N Z J Obstet Gynaecol. 2010;50(1):21––224. doi: 10.1111/j.1479-828X.2009.01116.x [DOI] [PubMed] [Google Scholar]
- 36.Vallely L, Homiehombo P, Kelly-Hanku A, et al. Hospital admission following induced abortion in Eastern Highlands province, Papua New Guinea – a descriptive study. PLoS One. 2014;9(10):e110791. doi: 10.1371/journal.pone.0110791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asa I, de Costa C, Mola G.. A prospective survey of cases of complications of induced abortion presenting to Goroka Hospital, Papua New Guinea, 2011. Aust N Z J Obstet Gynaecol. 2012;52(5):491–493. doi: 10.1111/j.1479-828X.2012.01452.x [DOI] [PubMed] [Google Scholar]
- 38.Vallely L, Toliman P, Ryan C, et al. Performance of syndromic management for the detection and treatment of genital Chlamydia trachomatis, Neisseria gonorrhoeae and Trichomonas vaginalis among women attending antenatal, well woman and sexual health clinics in Papua New Guinea: a cross-sectional study. BMJ Open. 2017;7(12):e018630. doi: 10.1136/bmjopen-2017-018630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vallely L, Toliman P, Ryan C, et al. Prevalence and risk factors of Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis and other sexually transmissible infections among women attending antenatal clinics in three provinces in Papua New Guinea: a cross-sectional survey. Sex Health. 2016;13(5):420–427. doi: 10.1071/SH15227 [DOI] [PubMed] [Google Scholar]
- 40.Mola G, Kuk J.. Operative vaginal delivery at Port Moresby General Hospital from 1977 to 2010. P N G Med J. 2011;54(3-4):174–184. [PubMed] [Google Scholar]
- 41.Badman S, Vallely LM, Toliman P, et al. A novel point-of-care testing strategy for sexually transmitted infections among pregnant women in high-burden settings: results of a feasibility study in Papua New Guinea. BMC Infect Dis. 2016;16:250. doi: 10.1186/s12879-016-1573-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wangnapi R, Soso S, Unger HW, et al. Prevalence and risk factors for Chlamydia trachomatis, Neisseria gonorrhoeae and Trichomonas vaginalis infection in pregnant women in Papua New Guinea. Sex Transm Infect. 2015;91(3):194–200. doi: 10.1136/sextrans-2014-051670 [DOI] [PubMed] [Google Scholar]
- 43.Manape M, Saleu G, Vallely L.. Outcome of infants born to unbooked mothers: a short report from Goroka General Hospital, Eastern Highlands province, Papua New Guinea. P N G Med J. 2011;54(3):185–188. [PubMed] [Google Scholar]
- 44.Lufele E, Umbers A, Ordi J, et al. Risk factors and pregnancy outcomes associated with placental malaria in a prospective cohort of Papua New Guinean women. Malar J. 2017;16(1):427. doi: 10.1186/s12936-017-2077-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Senn M, Baiwog F, Winmai J, et al. Betel nut chewing during pregnancy, Madang province, Papua New Guinea. Drug Alcohol Depend. 2009;105(1-2):126–131. doi: 10.1016/j.drugalcdep.2009.06.021 [DOI] [PubMed] [Google Scholar]
- 46.Bardaji A, Martínez-Espinosa FE, Arévalo-Herrera M, et al. Burden and impact of Plasmodium vivax in pregnancy: A multi-centre prospective observational study. PLoS Negl Trop Dis. 2017;11(6):e0005606. doi: 10.1371/journal.pntd.0005606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maraga S, Namosha E, Gouda H, et al. Sociodemographic factors associated with maternal health care utilization in Wosera, East Sepik province, Papua New Guinea. P N G Med J. 2011;54:154–163. [PubMed] [Google Scholar]
- 48.O’Keefe D, et al. Formal and informal maternal health care: comparing the service provision of health facilities and village health volunteers in East Sepik province. P N G Med J. 2011;54(3-4):147–153. [PubMed] [Google Scholar]
- 49.Mola G, Kuk J.. A randomised controlled trial of two instruments for vacuum-assisted delivery (Vacca Re-Usable OmniCup and the Bird anterior and posterior cups) to compare failure rates, safety and use effectiveness. Aus NZ J Obstet Gynaecol. 2010;50(3):246–252. doi: 10.1111/j.1479-828X.2010.01166.x [DOI] [PubMed] [Google Scholar]
- 50.Mola G, Unger H.. Strategies to reduce and maintain low perinatal mortality in resource-poor settings – findings from a four-decade observational study of birth records from a large public maternity hospital in Papua New Guinea. Aust N Z J Obstet Gynaecol. 2019;59(3):394–402. doi: 10.1111/ajo.12876 [DOI] [PubMed] [Google Scholar]
- 51.Aipit J, et al. Causes of neonatal admissions and in-hospital mortality at Modilon hospital, Madang province: a 5-year retrospective study. PNG Med J. 2016;59:30–33. [Google Scholar]
- 52.Goris J, Zomerdijk N, Temple V.. Nutritional status and dietary diversity of Kamea in Gulf province, Papua New Guineas. Asia Pac J Clin Nutr. 2017;26(4):665–670. [DOI] [PubMed] [Google Scholar]
- 53.Kuzma J. Knowledge, attitude and practice related to infant feeding among women in rural Papua New Guinea: A descriptive, mixed method study. Int Breastfeed J. 2013;8:16. doi: 10.1186/1746-4358-8-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Health Organization Global Observatory on eHealth, Papua New Guinea key indicators. 2016 [cited 2018 Oct 15]. Available from: http://apps.who.int/gho/data/node.goe.ki-PNG?lang=en.
- 55.de Bernis L, Kinney MV, Stones W, et al. Stillbirths: ending preventable deaths by 2030. Lancet. 2016;387(10019):703–716. doi: 10.1016/S0140-6736(15)00954-X [DOI] [PubMed] [Google Scholar]
- 56.World Health Organization WHO recommendation on antenatal care contact schedules: WHO; 2018. 2018 [cited 2019 Aug 2]. Available from: https://extranet.who.int/rhl/topics/improving-health-system-performance/who-recommendation-antenatal-care-contact-schedules.
- 57.UNICEF Country profile Papua New Guinea. 2012 [cited 2018 Nov 19]. Available from: https://data.unicef.org/wp-content/uploads/country_profiles/Papua%20New%20Guinea/Maternal_PNG.pdf.
- 58.UNICEF and World Health Organization Tracking progress towards universal coverage for reproductive, newborn and child health: the 2017 report. 2017, Washington (DC): UNICEF.
- 59.World Health Organization Breastfeeding in the Western Pacific: WHO Western Pacific. 2019 [cited 2019 Aug 2]. Available from: https://www.who.int/westernpacific/health-topics/breastfeeding.
- 60.Government of PNG Criminal Code Act 1974 pp. Ordinance No. 7 of 1902, revised 1974. Chapter 1262, parts 1225, 1226, 1280. s.l. PNG, in Government of PNG. 1974: Papua New Guinea.
- 61.National Statistical Office [Papua New Guinea] and ICF Papua New Guinea demographic and health survey 2016–18: key indicators report. 2019, Port Moresby, PNG, and Rockville, Maryland, USA: National Statistical Office and ICF.
- 62.United Nations. Sustainable Development Goals 2019 2019 [cited 2019 Aug 2]. Available from: https://sustainabledevelopment.un.org/sdgs.
- 63.Lawn J, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387(10018):587–603. doi: 10.1016/S0140-6736(15)00837-5 [DOI] [PubMed] [Google Scholar]
- 64.Madhi S, Briner C, Maswime S, et al. Causes of stillbirths among women from South Africa: a prospective, observational study. Lancet Glob Health. 2019;7(4):e503–e512. doi: 10.1016/S2214-109X(18)30541-2 [DOI] [PubMed] [Google Scholar]
- 65.March of Dimes, et al. Born too soon: the global action report on preterm birth. 2012, Geneva: World Health Organization.
- 66.WHO Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA. 2018, Geneva: World Health Organization.
- 67.Division of Obstetrics and Gynaecology Port Moresby General Hospital. Annual report – 2018. 2019, Port Moresby: Port Moresby General Hospital.
- 68.Tanahashi T. Health service coverage and its evaluation. Bull World Health Organ. 1978;56(2):295–303. [PMC free article] [PubMed] [Google Scholar]
- 69.Homer C, Castro Lopes S, Nove A, et al. Barriers to and strategies for addressing the availability, accessibility, acceptability and quality of the sexual, reproductive, maternal, newborn and adolescent health workforce: addressing the post-2015 agenda. BMC Pregnancy Childbirth. 2018;18(1):55. doi: 10.1186/s12884-018-1686-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.