Abstract
Located in the South West Pacific region, with a population of 7.5 million, Papua New Guinea (PNG) is among a group of Pacific countries with sub-optimal health status. The maternal mortality ratio is 171 per 100,000 live births. Unmet need for contraception and family planning services, although poorly understood in PNG, may be one of the underlying causes of poor maternal health. This study set out to measure the prevalence and trends in unmet need for contraception and the identified socioeconomic factors associated with contraceptive use among women of reproductive age (15–49 years) in PNG. Data available from the Integrated Health and Demographic Surveillance System (IHDSS) were used in this study. A sub-population data set was extracted of 1434 women who gave birth in the preceding two years and resided in four rural surveillance sites: Asaro, Hides, Hiri and Karkar. Analyses of unmet need for contraception were performed with respect to birth spacing and limiting the number of births. Unmet need for contraception was 34% for the previous birth, 37% for the current pregnancy, and 49% for future family planning. The total unmet need for contraception was 35%, of which 49% was for spacing births and 51% for limiting births. Women’s age, education and household wealth are the most significant determinants of unmet need for contraception. The high level of unmet need for contraception may contribute to women’s poor health status in PNG. Urgent programming responses from the health sector for supporting effective interventions to increase availability and utilisation of contraceptives are required.
Keywords: unmet need for contraception, Papua New Guinea, Sustainable Development Goals, universal health coverage
Résumé
Située dans la région du Pacifique Sud-Ouest, avec une population de 7,5 millions d’habitants, la Papouasie-Nouvelle-Guinée (PNG) fait partie d’un groupe de pays du Pacifique avec un état de santé sous-optimal. Le taux de mortalité maternelle y est de 171 pour 100 000 naissances vivantes. Les besoins insatisfaits de contraception et de services de planification familiale, même s’ils sont mal compris en PNG, pourraient être l’une des causes sous-jacentes de la mauvaise santé maternelle. Cette étude a entrepris de mesurer la prévalence et les tendances des besoins insatisfaits de contraception et les facteurs socio-économiques identifiés qui sont associés à l’emploi de contraceptifs chez les femmes en âge de procréer (15-49 ans) en PNG. L’étude a utilisé les données disponibles dans le système de surveillance sanitaire et démographique intégrée (IHDSS). Des données sur un sous-groupe de population ont été obtenues auprès de femmes qui avaient accouché pendant les deux années précédentes et résidaient dans quatre sites ruraux de surveillance: Asaro, Hides, Hiri et Karkar, soit 1434 femmes au total. L’analyse des besoins insatisfaits de contraception a été réalisée en rapport avec l’espacement des naissances et la limitation du nombre d’enfants. Les besoins insatisfaits de contraception étaient de 34% pour la naissance précédente, 37% pour la grossesse actuelle et 49% pour la planification familiale future. Les besoins totaux insatisfaits de contraception étaient de 35%, dont 49% concernaient l’espacement des naissances et 51% la limitation du nombre d’enfants. L’âge des femmes, leur niveau d’instruction et le revenu du ménage sont les principaux déterminants des besoins insatisfaits de contraception. Il est possible que le niveau élevé de besoins insatisfaits de contraception contribue au mauvais état de santé des femmes en PNG. Des réponses urgentes de programmation sont requises de la part du secteur de la santé pour soutenir les interventions capables d’élargir la disponibilité et l’utilisation des contraceptifs.
Resumen
Situada en la región del Pacífico sudoccidental, con una población de 7.5 millones, Papúa Nueva Guinea (PNG) es parte de un grupo de países del Pacífico con nivel de salud subóptimo. La razón de mortalidad materna es de 171 por cada 100,000 nacimientos vivos. La necesidad insatisfecha de servicios de anticoncepción y planificación familiar, aunque mal entendida en PNG, podría ser una de las causas subyacentes de mala salud materna. Este estudio se propuso medir la prevalencia y tendencias de la necesidad insatisfecha de anticoncepción y los factores socioeconómicos identificados asociados con el uso de anticonceptivos entre mujeres en edad reproductiva (15 a 49 años) en PNG. Este estudio utilizó los datos disponibles del Sistema Integrado de Vigilancia de Salud y Demográfica (IHDSS). Se extrajo un conjunto de datos de la subpoblación de mujeres que dieron a luz en los dos años anteriores y que residían en cuatro sitios de vigilancia rurales: Asaro, Hides, Hiri y Karkar, un total de 1434 mujeres. Se realizaron análisis de la necesidad insatisfecha de anticoncepción con respecto al espaciamiento de nacimientos y la limitación del número de partos. La necesidad insatisfecha de anticoncepción fue de 34% para el parto anterior, de 37% para el embarazo actual y de 49% para planificación familiar futura. El total de necesidad insatisfecha de anticoncepción fue de 35%, del cual el 49% fue para espaciar nacimientos y el 51% para limitar partos. La edad, el nivel de escolaridad y la riqueza doméstica de las mujeres son los determinantes más significativos de la necesidad insatisfecha de anticoncepción. El alto nivel de necesidad insatisfecha de anticoncepción podría contribuir al bajo nivel de salud de las mujeres de PNG. Se necesitan urgentes respuestas programáticas del sector salud para apoyar intervenciones eficaces para ampliar la disponibilidad y utilización de métodos anticonceptivos.
Introduction
Family planning (FP) and contraceptive methods have been identified as essential interventions for improving maternal and child health. Following the Millennium Development Goals (MDG) 2000–2015, the United Nations launched the Sustainable Development Goals (SDGs), in which Goal 3, Target 3.7 is to realise sexual and reproductive health and rights for all, and to promote the rapid reduction in fertility to replacement level or below through exclusively voluntary means. This target is assessed by tracking indicator 13: Met demand for family planning, which is a modification based on the previous MDG indicator on unmet need for family planning,1 and as specified in WHO Global Reference List of 100 Core Health Indicators: “Demand for family planning satisfied with modern methods”.2
Universal health coverage (UHC) aims to ensure all people have access to quality healthcare services, including preventive and treatment services, while ensuring that the users of services do not suffer any financial hardship. Today, more than 50% of the world’s population do not have access to the health services they need. Every year, about 100 million people are pushed into extreme poverty because of health service related expenses.3 Access to health services is crucial for maintaining and improving health, especially for adolescents and young people. At the same time, people need to be protected from being pushed into poverty because of the cost of health care.
Family Planning (FP) is often referred to as one of the most cost-effective interventions for global health and development due to its high cost–benefit ratio. For every $US1 invested in FP there is an economic return of $US20–120.4,5 Moreover, for every dollar spent to reduce unmet need for FP in the Pacific, there would be savings of $US10–23 in health and education costs.6 A global burden of diseases analysis shows that reduced unmet need for contraception could prevent around 30% of maternal deaths and reduce child mortality by 20%.7
Access to and utilisation of FP services and appropriate contraceptive methods are essential for the health and wellbeing of women and young girls, contributing to gender equity and overall poverty reduction. Unmet need for FP can lead to unintended pregnancy, unsafe abortion and/or increased risk of death during labour and delivery, particularly among young women, posing serious risks to their health.8,9 Meeting the global commitment to achieve universal access to reproductive health by 2030 will require intensified support for FP, including through the implementation of effective government policies, programmes and interventions. The integration of FP services within the context of UHC is considered to be an essential element in the implementation of the SDGs Agenda.10 When couples can make informed decisions on whether, when and how often to become pregnant, they will enjoy better health, achieve higher levels of education, expand their participation in the workforce, and generate more income for their families.11
Concept and definition
The concept of unmet need for FP emerged in the late 1970s and developed in the context of supply and demand for FP services and commodities for married women.9 In this paper, we use the United Nations’ definition of unmet need for FP and contraception:
“The number of women with unmet need for family planning expressed as a percentage of women of reproductive age who are married or in union, who are fecund and sexually active, but are not using any method of contraception, and report not wanting any more children or wanting to delay the birth of their next child.”1
The terms “family planning” and “contraception” are used interchangeably in this paper.
Scope of unmet need for contraception
The magnitude of unmet need for contraception is profound. In 2002, global estimates suggested that over 100 million women, or about 17% of the total female population, preferred to avoid pregnancy yet were not using any contraception method.12 A study of women in lower- and middle-income countries (LMICs) estimated that about 28% of pregnancies were unintended and approximately 21% of maternal deaths from unintended pregnancies occurred through unsafe abortions or inadequate obstetric care.13 Data compiled by the Population Reference Bureau in 2008 indicated that the proportion of women with unmet need for FP had not changed significantly over time, with the total number of women experiencing unmet need for FP around 183 million.14 Worldwide in 2017, 63% of women were using some form of contraception, but more than 10% of married or in-union women had an unmet need for FP, with as many as 20% of these women in Africa. It is projected that global unmet need for FP will remain above 10% by 2030 despite the reductions anticipated for some regions such as Eastern Africa, where unmet need is projected to fall from 22% to 16%, and in Polynesia, from 37% to 31% between 2015 and 2030.15 Access to health care services and the realisation of reproductive rights for all people will be essential to fulfil the pledge of the 2030 Agenda for Sustainable Development that “no one will be left behind”.
Unmet need for contraception in Papua New Guinea
The unmet need for contraception among women in Papua New Guinea (PNG) is poorly understood and the estimates of unmet need derived from national data are often seen as inaccurate because data from key minority groups of women, especially those from rural and remote areas, were not included in the estimation. The 2016 Demographic and Health Survey (DHS) indicates that unmet need for contraception was 26% among married women but 65% among sexually active unmarried women.16 These figures show a large variance in the documentation of unmet need in PNG that needs to be further investigated. There is a pressing need to reinvestigate the level of unmet need at the national and sub-national levels, using a more adaptable definition of unmet need for contraception, that is more appropriate in the PNG local context, to generate more accurate and reliable estimates of unmet need for contraception among PNG women.
PNG has one of the highest maternal mortality ratios (MMR) in the world, currently estimated at 171 per 100,000 live births (95% CI: 95–247).16 However, this estimate was made based on a small number of maternal deaths, as reflected in the wide confidence interval. Other estimates of MMR range from 98 to 733 per 100,000 live births.17,18 The large differentials in MMR estimates based on various data sources and using different estimation methods are a potential source of confusion for policy makers and international development partners. In an attempt to verify MMR estimates and determine a reliable estimate for PNG, Mola and Kirby reviewed the maternal death records of the National Health Information System and found that the MMR varied across the health facility levels, but the national estimate could be about 500 per 100,000 live births.17 Papua New Guinea Institute of Medical Research’s integrated Health and Demographic Surveillance System database provides verbal autopsy data for analysing maternal deaths. However, the current number of observations is still limited, resulting in an inadequate estimation of MMR.19 The main causes of maternal death are post-partum haemorrhage, eclampsia, unsafe abortion and sepsis.18,20,21 For women living in rural areas, the risk of dying in childbirth is four to eight times higher compared to urban areas. Less than 60% of pregnant women have access to antenatal care and only 40% of births are supervised by a skilled birth attendant.22 The 2016 DHS reported that 78% of pregnant women had at least one antenatal care visit and 54% of births were delivered in a health facility with the assistance of a skilled birth attendant.16 Primary health care is often sub-optimal, with poor facilities, lack of supplies and a shortage of health staff with adequate skills to effectively provide essential healthcare services. Geographical barriers and a widely dispersed population add further challenges to delivery of healthcare services. Sensitivity surrounding sexual and reproductive health, cultural barriers and a highly religious society can make it difficult to provide FP services and address the unmet need for contraception.23–25 From 2011 to 2015, only 6.9% of the total caseload of healthcare services provided at primary health facilities in rural areas of PNG were for FP services.26
Lessons learned from LMICs suggest that achieving UHC for FP services remains a challenge.3,15 Access to and utilisation of contraception is often under-represented in broader public health discussions in PNG. There has been a longstanding neglect of the need for contraception among women, particularly those who live in rural and remote areas.
Research objective, methods and materials
The objective of this study was to assess unmet need for contraception: the prevalence, trends, and relationships with household socioeconomic status among women of reproductive age, 15–49 years, who live in rural areas of PNG.
Data
Data used in this report were extracted from the integrated Health and Demographic Surveillance System (iHDSS), developed by Papua New Guinea Institute of Medical Research (PNGIMR) in the period 2011–2017. The system was set up to cover the population living in four rural sites: Hiri (Central Province) in the Southern region, Asaro (Eastern Highland Province) and Hides (Hela Province) in the Highlands region, and Karkar (Madang Province) in the Momase region (Figure 1). These sites are a representative sample for the rural population of PNG as the sample includes rural areas of the major provinces in PNG. The design of the iHDSS has been published elsewhere.19
Figure 1.
Surveillance sites: Hides (Hela Province) vs. Asaro (Eastern Highlands Province) in the highlands, Hiri (Central Province) vs. Karkar (Madang Province) in the coastal areas, PNGIMR’s iHDSS, 2016
Data used for analysis of unmet need for contraception were primarily from the women’s health data component of the iHDSS database, collected by the iHDSS team in the period July-December 2015 through individual interviews, using the Women of Reproductive Age, 15–49 years Questionnaire. This questionnaire was developed by PNGIMR in 2014, based on various existing data collection tools in use across international organisations such as the INDEPTH Global Surveillance Network, the United Nations Multi-Indicator Cluster Survey and Measure Evaluation’s Demographic and Health Survey. The questionnaire comprises eight data modules: Household identification information, including geographic positioning system data, Women’s Background, Marriage and Family, Sexual Behaviour, Domestic Violence, Child Mortality, Unmet Need for Contraception, and Maternal and Newborn Health.
The questionnaire was pre-tested and post-tested with women in the community prior to data collection, and also translated back into Tok-Pisin by national scientific officers to facilitate the interviews with local women. The unmet need data module provides a range of variables relevant to the examination of unmet need for contraception among women, that are defined based on the specific questions asked in the questionnaire that elicit fertility behaviours and women’s preferences pertaining to the last birth, the current pregnancy, and the current use of contraceptive and future family planning.
Measuring level of unmet need
Unmet need for contraception was measured as the proportion of women who have unmet need for contraception (numerator) among the total number of women aged 15–49 years (denominator). However, based on a review of PNG’s policies and standards and the questions asked in the iHDSS, some adjustments were made to the measurement of unmet need for contraception. In this paper, unmet need for contraception was calculated among women of reproductive age, 15–49 years, who reported giving birth in the last two years, including women who are married, or live in union, or are single but sexually active, meaning all women who are currently in need of contraception regardless of their marital or family status.
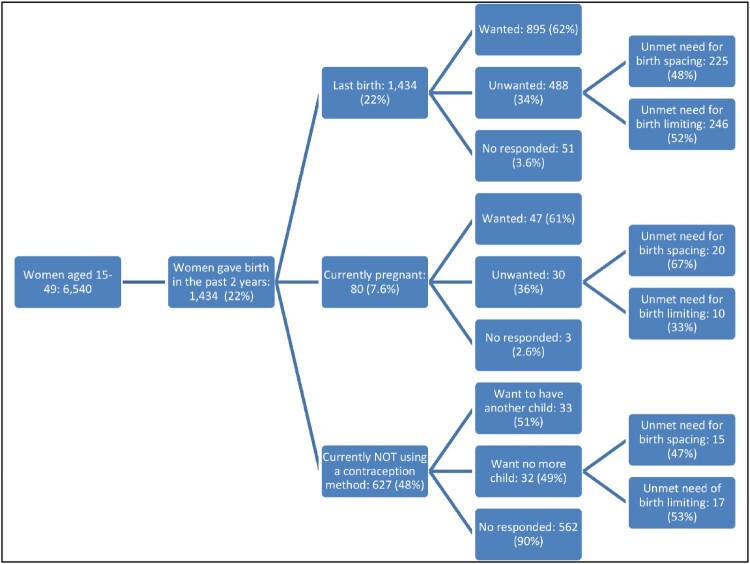
As shown in Figure 2, unmet need for contraception was calculated for three sub-groups:
Women who gave birth within the past 24 months and reported that the last birth was mistimed or unwanted;
Women, who were currently pregnant and reported that the current pregnancy is mistimed or unwanted at the time of conception; and
Women, who are not currently using any contraception method, but want to delay pregnancy or to have no more children.
Figure 2.
Analytical framework of unmet need for contraception among women who gave birth in the previous two years, PNGIMR’s iHDSS, 2016
To measure the magnitude of unmet need for contraception within this well-defined group of women, we estimated the level of unmet need for contraception for three separate categories: (i) unmet need for contraception in the last birth, resulting in a child born unwanted in the two years prior to the interview; (ii) unmet need for contraception in the current pregnancy, resulting in unwanted pregnancy among women who were currently pregnant; and (iii) unmet need for contraception in future family planning when women want to cease or delay their child bearing, but are currently not using any contraception method (Figure 2).
Unmet need for contraception was further analysed by unmet need for spacing between births and unmet need for limiting number of children. This analysis examines the nature of unmet need for contraception, hence provides practical guidance for interventions for improvement.
Unmet need for birth spacing included: (i) women who reported giving birth in the last two years, but wanted to get pregnant later; (ii) women who were currently pregnant, but wanted to get pregnant later; and (iii) women who were currently not using any contraception method, but wanted to delay pregnancy (or not decide the time of the next pregnancy).
Unmet need for limiting the number of children included: (i) women who gave birth in the last two years, but wanted no more children at that time; (ii) women who were currently pregnant, but did not want to have a child; (iii) women who were currently not using any contraception method, and wanted no more children.
Total unmet need for contraception was the sum of all these three forms of unmet need for contraception: at the last birth; at the current pregnancy; and for future family planning. This also represents the sum of unmet need for spacing and unmet need for limiting. This measurement does not take into account failure of contraception, whether modern or traditional methods.
Cross-table analyses and generalised linear models were constructed, using Statistical Package for the Social Sciences (SPSS) version 20.0. Generalised linear modelling was used to identify demographic factors associated with level of unmet need for contraception as well as the social determinants of unmet need for contraception in PNG. Parameters were calculated using the maximum likelihood estimation method to predict probability of unmet need for contraception in the last birth among women, by providing relative risk estimates of unmet need for contraception. The dependent variable represents the unmet need for contraception (for both birth spacing and birth limiting) at the last birth. The independent variables were the women’s socioeconomic characteristics, including resident location, age group, highest educational level attainment, marital status, number of children born alive and household wealth quintile. The levels of significance with 95% CI were estimated for each parameter.
Two other indicators related to unmet need for contraception were also measured and reported: (i) Contraceptive Prevalence Rate (CPR) and (iii) Modern Contraceptive Method Mix (MCMM), which is the distribution of various modern contraceptive methods (%) currently being used by women aged 15–49.
Ethics approval
The iHDSS was granted ethics approvals from the Internal Review Board of PNG Institute of Medical Research (IRB Approval No. 11.13) and the Medical Research Advisory Committee of Papua New Guinea (MRAC Approval No. 11.20). These approvals covered all the data components under the iHDSS, including data of women of reproductive age (15–49 years) which were used in this manuscript. Informed consent was sought from self-identified household heads and woman participants. Women were informed about their right to withdraw from the study at any stage.
Results
Overall socioeconomic and demographic characteristics of women aged 15–49, living in the surveillance sites have been presented elsewhere.19
Level of unmet need for contraception
Among 6540 women aged 15–49 years recorded in the iHDSS, 1434 (22%) had given birth in the past two years. Among these, 488 women reported that their last birth was unwanted, accounting for 34%. Regarding this last pregnancy, 225 women (46%) reported the pregnancy was mistimed and 246 women (54%) reported that they did not want another child (Table 1). Among 1058 women who gave birth in the last two years, 80 (7.6%) were pregnant again at the time of being questioned. Of these women, 30 reported their current pregnancy was unwanted (36.4%). Two-thirds of these women (20/30) reported wanting to delay the pregnancy and 10 women wanted no more children.
Table 1.
Unmet need for contraception among women participants, PNGIMR’s iHDSS, 2016
| N | % | |||
|---|---|---|---|---|
| Unmet need for contraception in the previous birth | Women gave birth in last two years | Yes | 1434 | 21.9 |
| No | 2331 | 35.6 | ||
| Total | 3765 | 57.6 | ||
| Missing system | 2775 | 42.4 | ||
| Total | 6540 | 100.0 | ||
| Wanted birth | Yes | 895 | 62.4 | |
| No | 488 | 34.0 | ||
| Total | 1383 | 96.4 | ||
| Missing system | 51 | 3.6 | ||
| Total | 1434 | 100.0 | ||
| Type of unmet need for contraception | Spacing | 225 | 47.8 | |
| Limiting | 246 | 52.2 | ||
| Total | 471 | 100.0 | ||
| Unmet need for contraception in currently pregnancy | Have current pregnancy | Yes | 80 | 7.6 |
| No | 977 | 92.3 | ||
| Don’t know | 1 | 0.1 | ||
| Total | 1058 | 100.0 | ||
| Wanted pregnancy | Yes | 47 | 61.0 | |
| No | 30 | 36.4 | ||
| Missing | 3 | 2.6 | ||
| Total | 80 | 100.0 | ||
| Type of unmet need for contraception | Spacing | 20 | 66.7 | |
| Limiting | 10 | 33.3 | ||
| Total | 30 | 100.0 | ||
| Unmet need for contraception for future family planning | Current use of contraceptive | Yes | 326 | 34.2 |
| No | 627 | 65.8 | ||
| Total | 953 | 100.0 | ||
| Missing | 318 | |||
| Total | 1271 | |||
| Future family planning | Want another child soon | 33 | 50.8% | |
| Want no more children | 17 | 26.2% | ||
| Want a child later | 15 | 23.1% | ||
| Total | 65 | 100.0% | ||
| Missing | 562 | |||
| Total | 627 | |||
| Type of unmet need for contraception | Spacing | 15 | 46.9% | |
| Limiting | 17 | 53.1% | ||
| Total | 32 | 100.00% | ||
| Total unmet need for contraception | Want a child/ birth/ pregnancy | Yes | 975 | 61.7% |
| No | 550 | 34.8% | ||
| Total | 1579 | 100.0% | ||
| Type of unmet need | Spacing | 260 | 48.8% | |
| Limiting | 273 | 51.2% | ||
| Total | 533 | 100.0% |
Only 953 women responded to the question about current contraception use, and of those, 627 (66%) were not using any form of contraception. Among women who were not using any contraception, just over half (51%) wanted more children in the near future, justifying their reason for not using contraception. However, 26% of the women wanted no more children and 23% wanted to delay pregnancy. The unmet need for future family planning was 49%.
The total unmet need for contraception among the women who gave birth in the previous two years was 35%, of which unmet need for spacing birth accounted for 49%, and 51% was unmet need for limiting birth.
Contraceptive prevalence rate
Table 2 shows that the CPR among the 1434 women who gave birth in the last two years was 31%, comprising 29% from modern contraception methods and only 1.7% from traditional contraception methods. Among modern contraception methods, the most commonly used were implants (11.5%) and injectables (9.0%) (Table 3).
Table 2.
Contraceptive prevalence rate among women, who gave birth in the past 2 years, PNG IMR’s iHDSS, 2016
| Total of women observed | N = 1434 | 100% | |
|---|---|---|---|
| Modern contraceptive methods | Female sterilisation Male sterilisation Intra uterus device (IUD) Injectables Implants Oral pill Male condom Female condom Diaphragm Lactational amenorrhoea method (LAM) Foam / Jelly |
30 2 2 129 165 42 32 15 1 1 0 |
2.1 0.1 0.1 9.0 11.5 2.9 2.2 1.0 0.1 0.1 0 |
| Total | 419 | 29.2 | |
| Traditional contraception method | Periodic abstinence / Rhythm Withdrawal Other |
11 10 3 |
0.8 0.7 0.2 |
| Total | 24 | 1.7 | |
| Contraceptive Prevalence Rate | 443 | 30.9 | |
Table 3.
Modern contraceptive prevalence rate among women who gave birth in the past 2 years by surveillance site, PNGIMR’s iHDSS, 2016
| Hiri | Asaro | Karkar | Hides | All sites | ||
|---|---|---|---|---|---|---|
| Total of women | 587 | 326 | 296 | 225 | 1434 | |
| Implant | N | 74 | 12 | 78 | 1 | 165 |
| % | 12.6 | 3.7 | 26.4 | 0.4 | 11.5 | |
| Injectable | N | 47 | 20 | 43 | 19 | 129 |
| % | 8.0 | 6.1 | 14.5 | 8.4 | 9.0 | |
| Oral pill | N | 18 | 14 | 7 | 3 | 42 |
| % | 3.1 | 4.3 | 2.4 | 1.3 | 2.9 | |
| Male condom | N | 1 | 27 | 4 | 0 | 32 |
| % | 0.2 | 8.3 | 1.4 | 0.0 | 2.2 | |
Factors predicting unmet need for contraception
Table 4 shows the relative risks of unmet need for contraception in the last birth among women in rural areas of PNG. Women’s age was predictive of their likelihood of having an unmet need for contraception, with the result statistically significant across all age groups. Education inversely predicted the unmet need for contraception with lowest educated women (preparatory and elementary education) having the highest unmet need. This relationship persisted after controlling for place of residence, age, wealth quintile and number of surviving children. Marital status was another key predictor for unmet need for contraception for the groups of women who were currently married and who were living in union with a man. However, women who were unmarried or not in a union with a man had a significantly higher risk of having unmet need compared to married women.
Table 4.
Relative risks with 95% confident interval in generalised linear model predicting probability of unmet need for contraception in the last birth, PNGIMR’s iHDSS, 2016
| Factor | N | Per cent | RR | 95% CI | Sig. | Adjusted RR | 95% CI | Sig. (2-tailed) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||||||
| Surveillance site | Hiri | 501 | 52.0% | .186 | −.024 | .395 | .083 | .186 | .061 | .311 | .007 |
| Asaro | 208 | 21.6% | .352 | .157 | .548 | .000 | .352 | .238 | .455 | .001 | |
| Karkar | 229 | 23.8% | .388 | .196 | .581 | .000 | .388 | .279 | .492 | .001 | |
| Hides | 26 | 2.7% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
| Age group | 15–19 | 75 | 7.8% | .354 | .016 | .692 | .040 | .354 | −.012 | .709 | .034 |
| 20–24 | 251 | 26.0% | .292 | −.030 | .613 | .076 | .292 | −.062 | .621 | .065 | |
| 25–29 | 271 | 28.1% | .285 | −.032 | .603 | .078 | .285 | −.082 | .609 | .070 | |
| 30–34 | 200 | 20.7% | .235 | −.082 | .551 | .146 | .235 | −.124 | .550 | .149 | |
| 35–39 | 104 | 10.8% | .282 | −.040 | .604 | .086 | .282 | −.052 | .626 | .084 | |
| 40–44 | 54 | 5.6% | .141 | −.190 | .472 | .403 | .141 | −.219 | .496 | .390 | |
| 45–49 | 9 | .9% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
| Educational level | Preparatory | 17 | 1.8% | .072 | −.278 | .422 | .688 | .072 | −.290 | .453 | .687 |
| Elementary | 18 | 1.9% | .008 | −.339 | .355 | .963 | .008 | −.352 | .412 | .971 | |
| Primary | 535 | 55.5% | −.072 | −.343 | .200 | .604 | −.072 | −.358 | .241 | .621 | |
| Lower secondary | 328 | 34.0% | −.059 | −.330 | .213 | .672 | −.059 | −.350 | .249 | .667 | |
| Upper secondary | 47 | 4.9% | −.188 | −.486 | .110 | .215 | −.188 | −.499 | .133 | .221 | |
| Vocational training | 7 | .7% | −.255 | −.691 | .181 | .252 | −.255 | −.701 | .217 | .247 | |
| College/University | 12 | 1.2% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
| Marital family status | In marriage | 627 | 65.0% | −.316 | −.412 | −.220 | .000 | −.316 | −.423 | −.216 | .001 |
| In union | 216 | 22.4% | −.269 | −.378 | −.159 | .000 | −.269 | −.385 | −.157 | .001 | |
| Not in marriage/Union | 121 | 12.6% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
| Number of live births | 0 | 28 | 2.9% | −.131 | −.340 | .078 | .220 | −.131 | −.332 | .072 | .206 |
| 1 | 255 | 26.5% | −.205 | −.348 | −.063 | .005 | −.205 | −.348 | −.063 | .005 | |
| 2 | 227 | 23.5% | −.151 | −.286 | −.015 | .029 | −.151 | −.294 | −.003 | .038 | |
| 3 | 163 | 16.9% | −.154 | −.288 | −.020 | .025 | −.154 | −.297 | −.018 | .028 | |
| 4 | 136 | 14.1% | −.105 | −.239 | .028 | .123 | −.105 | −.250 | .034 | .161 | |
| 5 | 74 | 7.7% | −.022 | −.170 | .126 | .771 | −.022 | −.182 | .148 | .784 | |
| 6+ | 81 | 8.4% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
| Household wealth | 1st quintile | 122 | 12.7% | −.052 | −.200 | .095 | .489 | −.052 | −.203 | .096 | .516 |
| 2nd quintile | 178 | 18.5% | −.131 | −.264 | .003 | .056 | −.131 | −.263 | .003 | .060 | |
| 3rd quintile | 189 | 19.6% | −.099 | −.206 | .009 | .073 | −.099 | −.197 | −.001 | .049 | |
| 4th quintile | 214 | 22.2% | −.048 | −.133 | .038 | .276 | −.048 | −.136 | .040 | .262 | |
| 5th quintile | 261 | 27.1% | 0 | 0 | |||||||
| Total | 964 | 100.0% | |||||||||
The association between total number of live births and unmet need for contraception was statistically significant across all categories from zero to four live births, except for the group of women with five live births. The likelihood of unmet need was highest among women with one live birth (adjusted RR at −0.205 and 95% CI: −0.348, −0.063). The level of unmet need for contraception was highest among women in the second and the third household wealth quintiles, adjusted RR at −0.131 (95% CI: −0.263, 0.003) and −0.099 (95% CI: −0.197, −0.001), respectively.
Discussion
Definition and measurement of unmet need for contraception
The 2006 DHS in PNG reported unmet need for FP only among married women but there is growing evidence that the number of adolescent and unmarried but sexually active women is increasing and that they are in high need of contraception.5 In the 2016 DHS in PNG, unmet need for contraception was extended to women who are fecund, unmarried but sexually active.16 The definition we used in this paper extends beyond the definition of unmet need for FP used in the 2006 and 2016 DHS. In a tribal, conservative and traditional society such as PNG, “living with a man” implies a de facto relationship, which is commonly and socially accepted and in some regions polygamy is accepted. To predict the true unmet need, we included both married women and those who live in a consensual union with a man and used this group as the denominator for measuring unmet need. This is strength of our study compared to previous population-based surveys, which exclude data from adolescents (aged 15–19 years) and unmarried but sexually active women.
To minimise recall bias, we only used data on fertility preference and contraceptive use from women who had given birth in the preceding two years. This condition is an alternative for the DHS definition, which is based on the self-reported information of “sexually active in the last 12 months, fecundity, having no hysterectomy or menopause”, all of which are not easy to identify and confirm in the PNG context, where asking women about their sexual and reproductive behaviours is considered insulting. Women who gave birth within the past two years are more vulnerable to unintended pregnancy if not using contraception. They are in need of contraception, either to delay their next pregnancy or cease their childbearing. Many would expect to delay their next childbearing for at least two years, as recommended by the PNG health policy.23,24 By contrast, women who had children more than two years ago, are likely to have already accessed contraception. Limiting data analysis to women who gave birth in the previous two years also minimised misinformation, providing more reliable and accurate estimates of the level of unmet need for contraception.
Further categorising unmet need for contraception into the unmet need for spacing births (49%) and the unmet need for limiting births (51%) provided valuable information to inform strategies to address unmet need. For example, temporary short-term and reversible contraceptive methods such as condoms (male and female), contraceptive foam/jelly, injectables and oral contraceptive pills are more relevant to women who have unmet need for birth spacing. On the other hand, permanent or long-term contraceptive methods including sterilisation (male and female), intra-uterine devices (IUD) and implants are more appropriate interventions to address unmet need for limiting the number of births, by ceasing childbearing in the case of sterilisation or increasing the space between births with IUD and implant.
Variation and trend of unmet need for contraception
The unmet need varied across women’s age groups with the highest level of risk found in the age group of 15–19 and lowest in the age group of 40–44 (see Table 4). This trend is consistent with findings of the 2016 DHS, which reported a drop by half from the youngest to the oldest age group. These data reconfirm adolescents and young girls are most affected by the highest unmet need. Although the PNG National Family Planning Policy advocates enhancing access to contraception for women from the age of 16,23,24 this may not be occurring. In PNG, social and cultural norms and gender inequity are barriers for young girls in accessing contraception. There is a need for more youth-friendly health services and community-based support programmes targeting young people.27
Our results confirm the trend of declining unmet need for contraception by women’s educational level. The 2016 DHS results show the unmet need was highest for women with no schooling. However, we found more complex interactions between education and unmet need, with non-significant association observed at preparatory, elementary and primary education levels, but significant negative associations observed at the upper secondary and higher educational levels. This means that only women with upper secondary or higher education have a lower unmet need. This could be because more educated women have better information and access to FP services and in particular to contraception. Interpretations of the relationship of women’s education to unmet need for contraception require caution.
Similarly we found a significant association between unmet need for contraception and household wealth, with women from the poorest households demonstrating the highest risk of having unmet need. Integration of FP into primary health services may help to reduce the unmet need for contraception among the poor by circumventing barriers associated with the cost of contraception.28
Using more exclusive methods, we estimated the unmet need for contraception was 35%, which is higher than those reported in the 2016 DHS (26%). There are several reasons for this finding. First, we redefined women who are in need of contraception, including those who were married and who lived in union, which appears acceptable and practical in the PNG context. Second, we measured three separate categories of unmet need: at the last birth, in the current pregnancy, and for future family planning. Third, we exclusively measured the unmet need among a sub-group of women who gave birth in the last two years as these women are considered as most in need of contraception. Fourth, we reported only on women who lived in rural areas while the DHS covered rural and urban sectors. Unmet need for contraception has been shown higher in rural than in urban areas of PNG.16
Compared to national level data from other Oceanic countries, the unmet need for contraception in PNG was among the lowest in the region and similar to smaller island nations such as Kiribati, Tonga, Nauru, Tuvalu and Vanuatu (Table 5). However, our findings suggest that these sources underestimated the unmet need for contraception in PNG and that true unmet need is actually similar to that of Samoa and the Solomon Islands (35%), which is among the highest in the region.29
Table 5.
Unmet need for family planning among married women aged 15–49 in selected countries in Oceania, Population Reference Bureau’s Family Planning Worldwide 2019 Datasheet14
| Spacing | Limiting | Total | Data source | |
|---|---|---|---|---|
| Kiribati | 14.4 | 15.6 | 28.0 | National Survey 2009 |
| Marshall Islands | 3.0 | 5.0 | 8.0 | National Survey 2007 |
| Nauru | 16.4 | 7.1 | 23.5 | National Survey 2007 |
| PNG | – | – | 27.4 | National Survey 2006a |
| Samoa | 16.5 | 18.3 | 34.8 | National Survey 2014 |
| Solomon Islands | 20.0 | 14.7 | 34.7 | National Survey 2015 |
| Tonga | 13.2 | 12.0 | 25.2 | National Survey 2012 |
| Tuvalu | 12.1 | 12.1 | 24.2 | National Survey 2017 |
| Vanuatu | 11.5 | 12.7 | 24.2 | MICS 2013 |
The DHS 2016 show 26% among married women and 65% among sexually active unmarried women16.
Our data show that the level of the last birth (34%) is similar to the level of unmet need at the current pregnancy (36%), suggesting that the trend of unmet need for contraception has not improved in the past two years in PNG, at least among the women in this study. The estimated level of unmet need for future family planning (49%) was even higher, suggesting that there would be more unintended pregnancies in rural areas of PNG in coming years if no supportive effective interventions were in place (Table 1).
Our results reveal a trend toward limited options of contraception in PNG, with the dominance of long-term contraceptive methods such as implants and injectables. There has been an imbalance in the Modern Contraceptive Method Mix (MCMM), with only 22% of short-term contraceptive methods being utilised (male and female condom, and oral pill) compared to 78% of long-term contraceptive methods (female sterilisation, injectable and implant) (see Figure 3). These findings suggest that the provision of FP services does not meet the short- or long-term demand for contraception among the women studied. The skewed MCMM toward long-term methods for women indicates a major factor limiting women’s voluntary choice of contraception.
Figure 3.
Modern contraceptive method mix of women participants, PNGIMR's iHDSS, 2016
Availability of and access to modern contraception methods are limited in rural areas of PNG. Unmet need for contraception was higher in the highlands compared with coastal areas. This can be directly linked to limited access to health services as a result of geographical barriers. A targeted outreach FP programme conducted in Karkar Island of Madang Province in the period 2012–2014, resulted in an increased uptake of implant and injectable contraception among the women in this site. However, to sustain and replicate such programmes across the rural areas of PNG would be costly and is unlikely to occur in the near future. This imposes further challenges to the implementation of national health policies and guidelines. A previous study showed that national FP policy had great impact on the contraception practice, reproductive choice and fertility behaviour of women.30
Long-term reversible contraceptive methods are often promoted in LMICs, where FP programmes advocate for women to use them because they are considered the most effective methods in term of higher couple-years of protection (CYP) (see Table 6), with fewer side effects and long-term consequences, and easy return to fertility when needed. However, in PNG the use of implant and injectable contraceptives appears more prevalent, accounting for 40% and 30% of the MCMM, respectively. The majority of the MCMM (92%) is achieved through methods administered to women such as implant, injectable, oral pill, female sterilisation and female condom, with only 8% coming from male-led methods such as male condom. From the supply side, FP services and commodities are often not available in health facilities in the iHDSS sites, many of which are run by religious-based organisations that do not support modern contraception. In an attempt to improve women’s access to contraception to achieve the Millennium Development Goals’ unmet need indicator in 2015, the PNG Government increased the supply of implants and injectables to public health facilities across the country. This resulted in higher proportions of these methods in the MCMM. The higher uptake of implants may reflect limited access to alternative methods such as the pill and condoms rather than a true preference for the implants.
Table 6.
Couple-year of protection among women who gave birth in the past 2 years, PNGIMR’s iHDSS, 2016
| Modern contraception methods | No. of contraceptive userb | Couple-Year of Protection per unit31 | Couple-Year of Protection |
|---|---|---|---|
| Female sterilisationa | 30 | 10 | 300 |
| Male sterilisationa | 2 | 10 | 20 |
| Intra uterus device (IUD) | 2 | 4.6 | 9.2 |
| Injectables | 129 | 0.25 (4 doses per CYP) | 32.25 |
| Implants | 165 | 2.5 | 412.5 |
| Oral pill | 42 | 0.067 (15 cycles per CYP) | 2.8 |
| Male condom | 32 | 0.08 (120 units per CYP) | 2.58 |
| Female condom | 15 | 0.08 (120 units per CYP) | 1.2 |
| Diaphragm | 1 | 0.56 (15 units per CYP) | 0.56 |
| Lactational amenorrhoea method (LAM) | 1 | 0.25 (4 users per CYP) | 0.25 |
| Foam / Jelly | 0 | 0.08 (120 units per CYP) | 0.0 |
| Total Couple-Year of Protection | 781.34 |
CYP for sterilisation varies by country and by region, based on differences in median age at sterilisation. In this estimation, CYP sterilisation global estimate was used for PNG.
Number of contraceptive users is used as an alternative proxy for the quantity of contraceptive methods used.
A particular concern in this study are rural women who are yet to have their first child (reported as having no live birth in our data) and who wish to delay their first pregnancy. The common assumption amongst FP services providers in PNG is that women who have no child have no need for contraception, meaning this group is often neglected in FP programmes.32,33 This trend often stems from socio-cultural norms and judgments about sexual activity among adolescent girls and young women.34,35 This is particularly true in the rural PNG context, where the negative influence of and pressure from conservative religious groups and from community myths and misperceptions about contraception use are common.36
Further examination of the use of long-term modern contraception methods by surveillance sites showed that there is no consistent modality of contraceptive use across the sites. The kind of contraceptive method used depends on individual circumstances, knowledge or preference as well as availability in the health systems. Service providers need to understand an individual’s need for contraception and women’s preferences for particular modern contraceptive methods should be considered in designing interventions. FP services should provide a full range of contraception, including short-term and long-term, reversible and permanent modern contraceptive methods to meet different needs of birth spacing and limiting among PNG women and couples.
Conclusion
The paper provides an update on access to and utilisation of contraceptive methods in PNG. This is useful planning information for international and national development partners, health policy makers and healthcare service providers, programme managers, communities and individuals. The high level of unmet need for contraception requires urgent programme responses and interventions from the health sector to increase access to and utilisation of contraceptives for all PNG women and men. The PNG government should further incorporate the provision of FP services and contraceptive supply into UHC, targeting the most vulnerable groups such as young women in rural areas. Action must be taken beyond the health sector to foster change in social norms and policy interventions to advocate for sexual and reproductive rights. Cooperation and collaboration between public health facilities and faith-based health facilities should be further encouraged to enhance access to a range of modern contraceptive methods without incurring high costs.
The results from this study can potentially be used to assist the PNG government in monitoring the goal of UHC at the national and sub-national levels. The PNGIMR should repeat the collection of data on unmet need for contraception every three years, using consistent methods and indicators. This will allow for tracking the country’s progress towards the implementation of the SDGs, especially the goals for improvement of maternal and child health. Researchers are encouraged to further explore this data in conjunction with this paper, and to identify practical solutions that would lead to reduction in the currently high level of unmet need for contraception in PNG as well as other LMICs.
Acknowledgements
The iHDSS was operated under the Partnership in Health Project with financial support from ExxonMobil PNG LNG Project. The funder had no role in study design, data collection and analysis, or writing of the manuscript.
Author distribution
BNP designed the study and supervised the fieldwork, collected and analysed the data, drafted, revised, finalised and submitted the manuscript. MW conceptualised the paper, interpreted the data, and provided the inputs. ADO reviewed the manuscript, provided comments and edited the final version. WP directed the iHDSS, reviewed and approved submission of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- 1.United Nations . Sustainable development goals 2015 [cited 2019 Nov 12]. Available from: http://www.who.int/topics/reproductive_health/en/.
- 2.WHO . 2015 Global reference list of 100 core health indicators. Geneva; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Universal Health Coverage [Internet]. WHO . 2019 [cited 2019 Nov 12]. Available from: https://www.who.int/health-topics/universal-health-coverage#tab=tab_1.
- 4.UNFPA . Motherhood in childhood. New York; 2013. [Google Scholar]
- 5.UNFPA, UNESCO, WHO . Sexual and reproductive health of young people in Asia and the Pacific: a review of issues, policies and programmes. Bangkok: UNFPA; 2015. [Google Scholar]
- 6.Family Planning New Zealand . Investment in family planning in Kiribati: a cost-benefit analysis. Wellington: Family Planning New Zealand; 2014. [Google Scholar]
- 7.Ahmed S, Li Q, Liu L, et al. Maternal deaths averted by contraceptive use: an analysis of 172 countries. The Lancet. 2012;380(9837):111–125. [DOI] [PubMed] [Google Scholar]
- 8.Ashford L. Unmet need for family planning: recent trends and their implications for programs. Washington (DC: ): Population Reference Bureau; 2003. [Google Scholar]
- 9.Casterline JB, Sinding SW.. Unmet need for family planning in developing countries and implications for population policy. Popul Dev Rev. 2000;26(4):691–723. [Google Scholar]
- 10.Ellen S, Norton M, Marcus R.. Investing in family planning: key to achieving the sustainable development goals. Global Health: Sci Pract. 2016;4(2):191–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadi M. Historical development of the global political agenda around sexual and reproductive health and rights: a literature review. Sex Reprod Healthc. 2017;12:64–69. [DOI] [PubMed] [Google Scholar]
- 12.Daulaire N, Leidl P, Mackin L, et al. Promises to keep – the toll of unintended pregnancies on women's lives in the developing world. Washington (DC: ): The Global Health Council; 2002. [Google Scholar]
- 13.Ross JA, Winfrey WL.. Unmet need for contraception in the developing world and the former Soviet Union: an updated estimate. Int Fam Plan Perspect. 2002;28(3):138. [Google Scholar]
- 14.Family Planning Data Sheet 2019 [Internet] . Population reference bureau. 2019 [cited 2019 Nov 12]. Available from: https://www.prb.org/fpdata/.
- 15.United Nations . World family planning 2017 – highlights (ST/ESA/SER.A/414). New York (NY: ) Department of Economic and Social Affairs, Population Division; 2017. Available from: https://www.un.org/en/development/desa/population/publications/pdf/family/WFP2017_Highlights.pdf. [Google Scholar]
- 16.National Statistics Office . Papua New Guinea demographic and health survey 2016–18: key indicators report. Port Moresby (Papua New Guinea: ): National Statistics Office; 2019. [Google Scholar]
- 17.Mola G, Kirby B.. Discrepancies between national maternal mortality data and international estimates: the experience of Papua New Guinea. Reprod Health Matters. 2013;21(42):191–202. [DOI] [PubMed] [Google Scholar]
- 18.Sanga K, de Costa C, Mola G.. A review of maternal deaths at Goroka General Hospital, Papua New Guinea 2005–2008. Aust NZJ Obstet Gynaecol. 2010;50(1):21. [DOI] [PubMed] [Google Scholar]
- 19.Pham BN, Maraga S, Boli R, et al. Partnership in health programme report: March 2016 edition on women’s health. Goroka: PNG Institute of Medical Research; 2016. [Google Scholar]
- 20.Sanga K, Mola G, Wattimena J.. Unintended pregnancy amongst women attending antenatal clinics at the Port Moresby General Hospital. Aust NZJ Obstet Gynaecol. 2014;54(4):360–365. [DOI] [PubMed] [Google Scholar]
- 21.Dennis AT. Reducing maternal mortality in Papua New Guinea: contextualizing access to safe surgery and anesthesia. Anesth Analg. 2018;126(1):252–259. [DOI] [PubMed] [Google Scholar]
- 22.Asa I, de Costa C, Mola G.. A prospective survey of cases of complications of induced abortion presenting to Goroka Hospital in PNG in 2011. Aust NZJ ObstGyn. 2012;52(5):491. [DOI] [PubMed] [Google Scholar]
- 23.National Department of Health . PNG youth and adolescent health policy. In: National Department of Health , editor. Port Moresby: National Department of Health; 2014. p. 14. [Google Scholar]
- 24.National Department of Health . National sexual reproductive health policy. In: National Department of Health , editor. Port Moresby: National Department of Health; 2014. p. 11. [Google Scholar]
- 25.Department of National Planning and Monitoring . National population policy 2015–2024. In: Department of National Planning and Monitoring , editor. Port Moresby: PNG Government; 2015. p. 17. [Google Scholar]
- 26.Boili R, Pham NB, Siba P.. Assessing the changing burden of diseases at the primary healthcare level in rural Papua New Guinea. PNG Med J. 2017;60(3-4):122–136. [Google Scholar]
- 27.Bell S, Kennedy E, Black K, et al. Youth-centred research to help prevent and mitigate the adverse health and social impacts of pregnancy amongst young Papua New Guineans. Reprod Health Matters. 2018;26(54):5–12. [DOI] [PubMed] [Google Scholar]
- 28.Singh S, Darroch JE, Ashford LS, et al. Adding it up: the costs and benefits of investing in family planning and maternal and newborn health. New York (NY: ) Guttmacher Institute and UNFPA; 2006. [Google Scholar]
- 29.Kuhlmann AS, Gavin L, Galavotti C.. The integration of family planning with other health services: a literature review. Int Perspect Sexual Reprod Health. 2010;36(4):189–196. [DOI] [PubMed] [Google Scholar]
- 30.Pham NB, Hall W, Hill SP, et al. Analysis of socio-political and health practices influencing sex ratio at birth in Viet Nam. Reprod Health Matters. 2008;16(32):176–184. [DOI] [PubMed] [Google Scholar]
- 31.Measure Evaluation . Family planning and reproductive indicators database: measure evaluation; 2020 [updated 6 May 2020]. Available from: https://www.measureevaluation.org/prh/rh_indicators/family-planning/fp/cyp.
- 32.Gillespie D, Ahmed S, Tsuia A, et al. Unwanted fertility among the poor: an inequity? Bull World Health Organ. 2007;85(2):100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Donnell O, van Doorslaer E, Wagstaff A, et al. Analyzing health equity using household survey data. Washington (DC: ): World Bank; 2008. [Google Scholar]
- 34.Solo J, Festin M.. Provider bias in family planning services: a review of its meaning and manifestations. Global Health: Sci Pract. 2019;7(3):371–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO . WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. Geneva; 2011. [DOI] [PubMed] [Google Scholar]
- 36.Vallely LM, Homiehombo P, Kelly-Hanku A.. Exploring women's perspectives of access to care during pregnancy and childbirth: a qualitative study from rural Papua New Guinea. Midwifery. 2013;29(10):1222–1229. [DOI] [PubMed] [Google Scholar]