Abstract
Background
Gastric adenocarcinoma is associated with H. pylori infection and inflammation that can result in the dysbiosis of gastric microbiota. The association of intestinal microbiota with gastric adenocarcinoma subtypes or with gastric gastrointestinal stromal tumors (GIST) is however not well known. Therefore, we performed 16S rRNA gene sequencing on DNA isolated from stool samples of Finnish patients and controls to study differences in microbiota among different histological subtypes of gastric adenocarcinoma, gastric GIST and healthy controls.
Results
We found that gut microbiota alpha diversity was lowest in diffuse adenocarcinoma patients, followed by intestinal type and GIST patients, although the differences were not significant compared to controls. Beta-diversity analysis however showed significant differences in microbiota composition for all subtypes compared to controls. Significantly higher abundance of Enterobacteriaceae was observed in both adenocarcinoma subtypes, whereas lower abundance of Bifidobacteriaceae was seen only in diffuse adenocarcinoma and of Oscillibacter in intestinal adenocarcinoma. Both GIST and adenocarcinoma patients had higher abundance of Enterobacteriaceae and lower abundance of Lactobacillaceae and Oscillibacter while lower abundance of Lachnoclostridium, Bifidobacterium, Parabacteroides and Barnesiella was seen only in the adenocarcinoma patients.
Conclusions
Our analysis shows association of higher Enterobacteriaceae abundance with all types of gastric tumors. Therefore it could be potentially useful as a marker of gastric malignancies. Lower gut microbiota diversity might be indicative of poorly differentiated, invasive, advanced or aggressive tumors and could possibly be a prognostic marker for gastric tumors.
Keywords: Diffuse gastric adenocarcinoma, Intestinal gastric adenocarcinoma, GIST, Gut microbiota
Background
Gut microbiota has an important role in the maintenance of healthy gut, via its role in host metabolism, nutrient absorption, pathogen protection, immunity and local gut environment [reviewed in 1]. Composition of gut microbiota is mainly influenced by diet, ethnicity, and disease state [reviewed in 2]. Helicobacter pylori (H. Pylori) infection is strongly associated with gastric inflammation and with the carcinogenesis of gastric cancer. The most common type of gastric cancer (GC) is gastric adenocarcinoma, which is histologically grouped, according to Lauren’s classification, into two main subtypes; ‘diffuse’ and ‘intestinal’, with some cases exhibiting features of both diffuse and intestinal i.e. with ‘indeterminate’ or ‘mixed’ phenotype [3]. Both subtypes are associated with H. pylori infection, although it is more common in intestinal subtype [4]. However, the two subtypes have different carcinogenic pathway and pathogenesis. Intestinal adenocarcinoma is usually linked with a history of past inflammation of the stomach and is preceded by many premalignant stages, including intestinal metaplasia, while diffuse adenocarcinoma has poorly differentiated cell morphology and is often associated with poor prognosis and survival, compared to intestinal adenocarcinoma [5]. At molecular level, intestinal adenocarcinoma has more genetic imbalance, including microsatellite instability (MSI) and chromosomal instability [6, 7] than diffuse adenocarcinoma, which is genetically more stable but is associated with small-sized amplifications and mutations in E-cadherin gene (CDH1) [8, 9].
Gastrointestinal stromal tumors (GIST) are rare and are very different from gastric adenocarcinoma. They are commonly located in stomach, although they can also be present in other parts of the gastrointestinal tract. They originate from stromal cells and have KIT or PDGRA mutations [reviewed in 10].
Changes in gastric microbiota are seen in patients with gastric adenocarcinoma [reviewed in 11], however, very little is known about changes in intestinal microbiota of gastric adenocarcinoma and GIST patients. Since diffuse adenocarcinoma, intestinal adenocarcinoma and GIST of stomach differ in histology and pathology, we analyzed and compared gut microbiota from stool samples of gastric cancer patients in order to study changes in gut microbiota associated with these gastric cancer types/subtypes.
Results
Microbiota diversity
Alpha-diversity
Gut microbiota richness and diversity were studied for different gastric cancer groups (adenocarcinoma and GIST) and the results (Fig. 1) showed lower microbiota richness and diversity in patients with gastric adenocarcinoma and gastric GIST patients compared to controls. We observed significant differences in microbiota richness between cancer patients and controls (Chao1; Fig. 1a). A similar trend was observed in microbiota diversity but this was not significant (Shannon index; Fig. 2b). No significant differences were observed between adenocarcinoma and GIST patients for richness (Fig. 1a) or diversity (Fig. 1b).
Fig. 1.
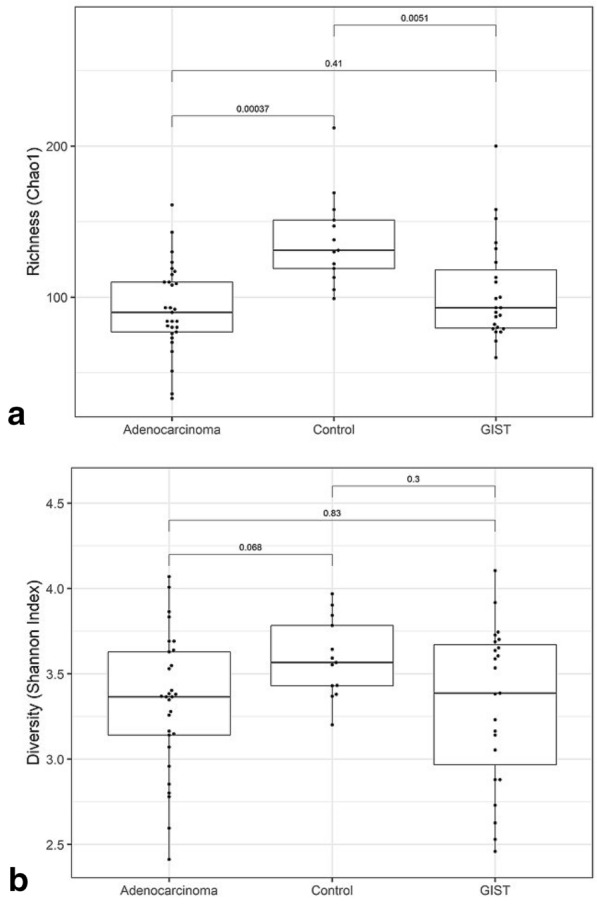
Gut microbiota richness and diversity in cancer patients and controls. Comparison of microbiota. a Richness (Chao1) and b diversity (Shannon index) in stool samples of patients with gastric adenocarcinoma, GIST and controls. The adjusted p-values are shown for each pairwise comparison
Fig. 2.
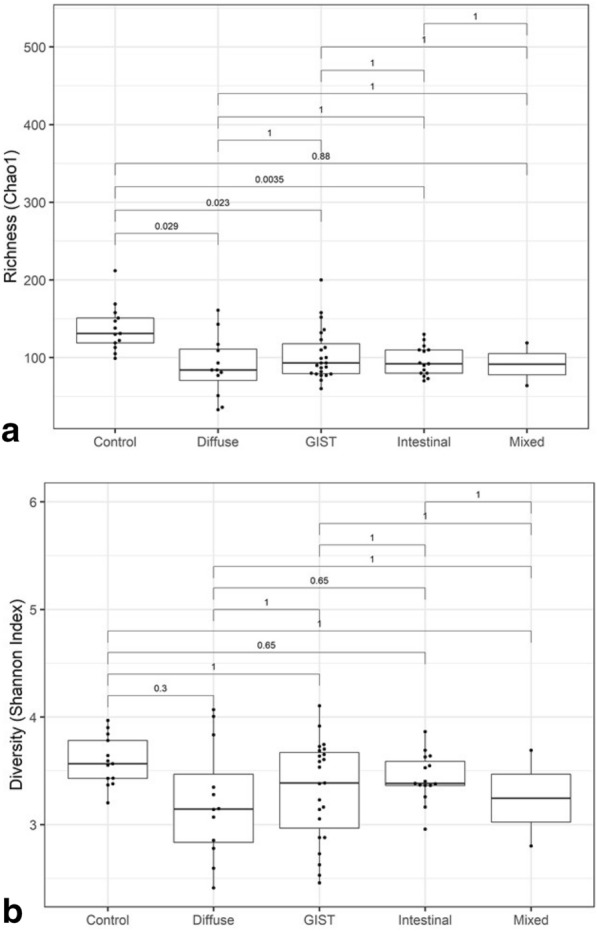
Gut microbiota richness and diversity in gastric cancer sub-groups. Comparison of microbiota. a Richness (Chao1) and b diversity (Shannon index) in stool samples of patients with diffuse gastric adenocarcinoma, intestinal gastric adenocarcinoma, mixed gastric adenocarcinoma, GIST and controls. The adjusted p-values are shown for each pairwise comparison
Patients with diffuse adenocarcinoma had the lowest microbiota diversity amongst the gastric cancer subgroups (diffuse, intestinal, mixed & GIST) (Fig. 2). Although all cancer subgroups had lower alpha diversity and a significantly lower microbiota richness (Chao1; Fig. 2a) compared to controls, the differences were not significant for diversity (Shannon index; Fig. 2b).
Beta-diversity
Differences in microbiota composition were compared between controls and different GC groups and GC subgroups. The beta-diversity showed significant differences in microbiota composition between controls and adenocarcinoma (p = 0.03), and between controls and different adenocarcinoma subgroups (Table 1). However, no significant differences in microbiota composition were observed between the adenocarcinoma subgroups (Table 1, Fig. 3).
Table 1.
Beta diversity analysis (PERMANOVA) for differences in gut microbiota between different gastric cancer sub-groups
| Groups compared | R2 | Adjusted p-value |
|---|---|---|
| Control vs Diffuse adenocarcinoma | 0.08 | 0.05 |
| Control vs GIST | 0.05 | 0.05 |
| Control vs Intestinal adenocarcinoma | 0.07 | 0.05 |
| Control vs Mixed adenocarcinoma | 0.13 | 0.05 |
| Diffuse adenocarcinoma vs GIST | 0.02 | 0.89 |
| Diffuse vs Intestinal adenocarcinoma | 0.04 | 0.58 |
| Diffuse adenocarcinoma vs Mixed | 0.07 | 0.66 |
| GIST vs Intestinal adenocarcinoma | 0.03 | 0.32 |
| GIST vs Mixed adenocarcinoma | 0.04 | 0.54 |
| Intestinal vs Mixed adenocarcinoma | 0.08 | 0.20 |
Fig. 3.
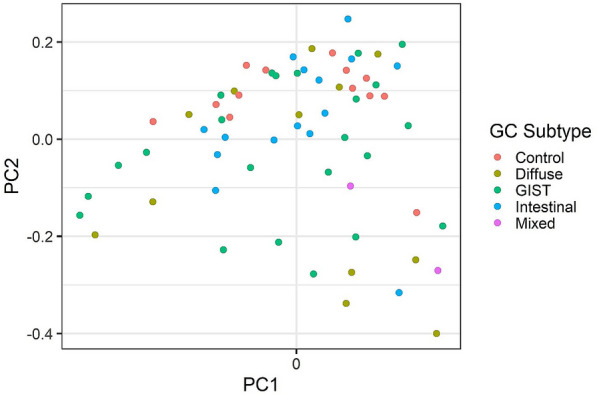
Microbiota community similarity between the samples. Principal coordinates analysis (PCoA) visualizes the variation in sample dissimilarity (Bray–Curtis beta-diversity based on genus-level bacterial profiles). The gastric cancer subtypes are indicated by color
Significant taxa with differential relative abundance in adenocarcinoma, GIST and control
In order to identify taxa that had significant differences in relative abundance in pair-wise comparisons between the groups, we performed the ALDEx2 differential abundance analysis (Table 2).
Table 2.
Taxonomic groups with significant differences (p ≤ 0.05) in pair-wise comparison of gastric cancer types
| Taxa | Adjusted p-value | Effecta | Groups compared |
|---|---|---|---|
| Family | |||
| Lactobacillaceae | < 0.01 | 0.64 | Adenocarcinoma vs Control |
| Enterobacteriaceae | < 0.01 | − 1.22 | Adenocarcinoma vs Control |
| Oscillospiraceae | 0.01 | 0.64 | Adenocarcinoma vs Control |
| Bifidobacteriaceae | 0.03 | 0.85 | Adenocarcinoma vs Control |
| Eubacteriaceae | 0.04 | 0.71 | Adenocarcinoma vs Control |
| Lactobacillaceae | 0.03 | − 0.75 | Control vs GIST |
| Enterobacteriaceae | 0.03 | 1.01 | Control vs GIST |
| Genus | |||
| Oscillibacter | < 0.01 | 1.21 | Adenocarcinoma vs Control |
| Lachnoclostridium | < 0.01 | 0.88 | Adenocarcinoma vs Controls |
| Bifidobacterium | 0.01 | 0.91 | Adenocarcinoma vs Controls |
| Parabacteroides | 0.03 | 0.60 | Adenocarcinoma vs Controls |
| Barnesiella | 0.05 | 0.62 | Adenocarcinoma vs Controls |
| Oscillibacter | < 0.01 | − 1.30 | Control vs GIST |
aALDEx2 standardized effect size (see Methods)
Higher abundance of bacteria belonging to Enterobacteriaceae and lower abundance of those belonging to Lactobacillaceae was commonly observed in adenocarcinoma and GIST patients (Table 2, Fig. 4) compared to controls. Additionally, lower abundance of Oscillospiraceae, Bifidobacteriaceae, and Eubacteriaceae was seen in adenocarcinoma patients compared to controls.
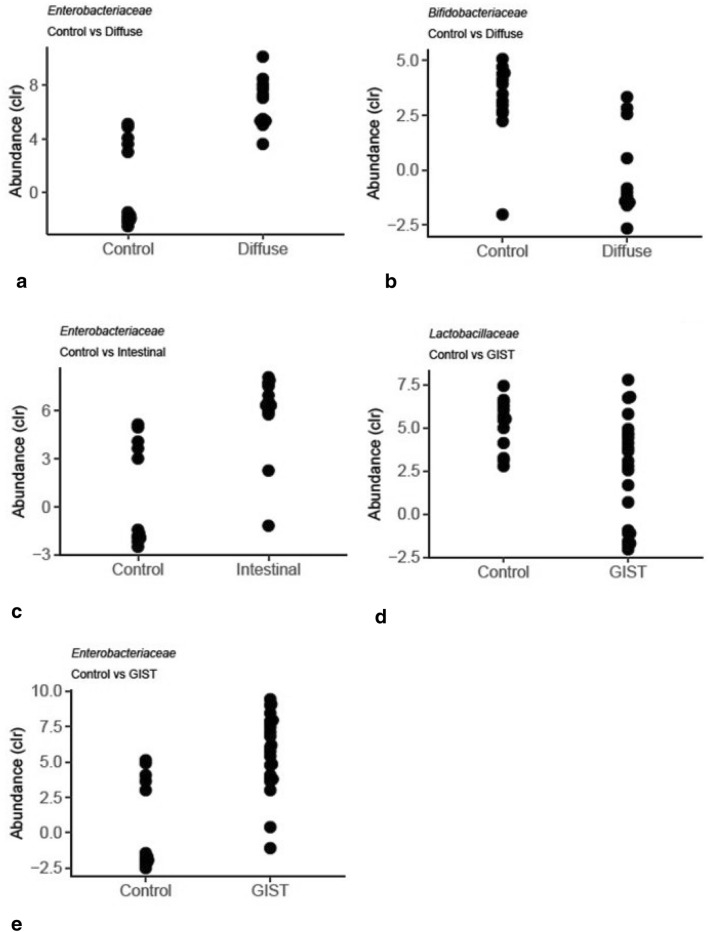
Fig. 4.
Significant taxa in paired group comparison. Taxa with significant differences (p ≤ 0.05; ALDEx2) in pair-wise comparison between gastric cancer subgroups and controls
At the genus level, significantly lower abundances of Oscillibacter, Lachnoclostridium, Bifidobacterium, Parabacteroides and Barnesiella were observed in adenocarcinoma patients compared to controls. In GIST patients, we observed a significantly lower abundance of Oscillibacter compared to controls.
Significant taxa with differential relative abundance in diffuse, intestinal, mixed, GIST and controls
We also compared microbiota composition in patients grouped according to adenocarcinoma subgroups (diffuse, intestinal and mixed) and the taxa with significant differential abundance in various pair-wise group comparisons are shown in Table 3.
Table 3.
Taxa with significant differences (p ≤ 0.05) in pair-wise comparison of gastric cancer subgroups
| Taxa | Adjusted p-value | Effecta | Groups compared |
|---|---|---|---|
| Family | |||
| Enterobacteriaceae | 0.02 | 1.24 | Control vs Diffuse adenocarcinoma |
| Bifidobacteriaceae | 0.05 | − 1.13 | Control vs Diffuse adenocarcinoma |
| Lactobacillaceae | 0.03 | − 0.76 | Control vs GIST |
| Enterobacteriaceae | 0.03 | 1.02 | Control vs GIST |
| Enterobacteriaceae | 0.04 | 1.15 | Control vs Intestinal adenocarcinoma |
| Genus | |||
| Oscillibacter | < 0.01 | − 1.40 | Control vs GIST |
| Oscillibacter | 0.01 | − 1.26 | Control vs Intestinal adenocarcinoma |
| Holdemania | 0.02 | 1.75 | Control vs Mixed adenocarcinoma |
| Holdemania | < 0.01 | 1.39 | GIST vs Mixed adenocarcinoma |
| Holdemania | 0.03 | 1.21 | Intestinal vs Mixed adenocarcinoma |
aALDEx2 standardized effect size (see Methods)
Significantly higher abundance of Enterobacteriaceae was seen in both of the adenocarcinoma subgroups; diffuse (Fig. 4a) and intestinal (Fig. 4c), and in GIST (Fig. 4e) compared to the controls, while significantly lower abundance of Bifidobacteriaceae was seen only in the diffuse subgroup (Fig. 4b). The genera with significant differential abundance in cancer subgroups were: Oscillibacter, having lower abundance in intestinal subgroup and in GIST compared to control, and Holdemania, having higher abundance in mixed subgroup compared to controls and also compared to GIST and intestinal subgroup.
Discussion
Adenocarcinoma of stomach is associated with gastric inflammation and H. pylori infection [12] that changes the stomach environment and can subsequently have an effect on the composition of the intestinal microbiota. On the other hand, intestinal microbiota plays an important role in the host immunity and inflammation. There are very few studies regarding changes in the intestinal microbiota in patients with gastric tumors, although changes in gastric microbiota have been reported previously [13]. Moreover, there are no gut microbiota studies, to the best of our knowledge, that have been carried out in different subtypes of gastric adenocarcinoma (diffuse and intestinal) and GISTs, which are quite different histologically and pathologically.
Our microbiota analysis from stool samples showed lowest alpha diversity and richness in patients with gastric adenocarcinoma, followed by patients with gastric GIST, and highest in controls. The alpha diversity (Shannon index) in adenocarcinoma and gastric GIST patients was however not significantly lower compared to controls (Fig. 1b) although the differences were significant for richness (Chao1, Fig. 1a). When analyzed separately, diffuse subtype had the lowest microbiota diversity, followed by intestinal subtype of adenocarcinoma and then gastric GIST (Fig. 2), although the diversity (Shannon index) was not significantly lower than controls. On the other hand, beta-diversity analysis showed that all cancer subgroups had significant differences in microbiota composition compared to controls (Table 1). A progressive decrease in gastric microbiota richness has been reported in premalignant GC stages with significant differences seen in intraepithelial neoplasia and GC compared to control [13, 14], while no significant changes in stool microbiota diversity is reported in patients with gastritis or metaplasia and controls [15].
In our study, the healthy controls were of younger age compared to the patients which could have confounding effect on the microbiota diversity results. However, among the cancer subgroups, patients with diffuse adenocarcinoma had lower microbiota diversity compared to intestinal adenocarcinoma patients, although the average age of patients with diffuse types was lower (69 years) than those with intestinal type (75 years). The lower microbiota diversity in diffuse adenocarcinoma thus seems to be more related to its undifferentiated cell morphology and aggressive tumor characteristics.
Gut bacteria are reported to affect immune response in tumor environment. A reduced gut microbiota diversity in breast cancer patients is linked to low immune infiltrate in breast tumors [16]. The diffuse subtype of gastric adenocarcinoma is characterized by undifferentiated cell phenotype, is highly invasive, and has poor immune cells infiltration, while both GIST [17] and intestinal adenocarcinoma have higher immune cells infiltration compared to diffuse type [18]. Poor tumor immune infiltrate, common in diffuse type, might be linked to the lower gut microbiota diversity seen in these patients in our study. The other reason could be that 58% of patients with diffuse, compared to 36% with intestinal type in our study had metastatic disease and the lower diversity might as well be related to advanced stage of cancer in diffuse type. Moreover, only diffuse subtype had significantly low abundances of bacteria belonging to Bifidobacteriaceae family. Bifidobacterium, an important member of this family and widely used as probiotic, is reported to suppress metastasis in mouse model via its effect on IL-11 expression and subsequent effect on circRNA/microRNA/sox9 axis and epithelial-mesenchymal transition genes [19]. Abundance of gut Bifidobacterium is also associated with the accumulation of activated antigen-specific T cells in the tumor microenvironment and its low abundance is related to more aggressive tumors in mice [20]. This is similar to our observation of lower abundances of Bifidobacteriaceae in diffuse adenocarcinoma, which have low immune cell infiltrate and are also more aggressive. Moreover, oral administration of Bifidobacterium is reported to control tumor growth in mice by increasing T cell accumulation in tumor microenvironment and increasing the efficacy of programmed cell death protein 1 (PD-L1) specific antibody therapy [20]. The abundance of gut Bifidobacterium thus seems to have an effect on tumor growth via its influence on host immunity and administration of Bifidobacterium supplements could have beneficial effects in cancer patients.
Significantly higher abundances of Enterobacteriaceae compared to controls were common in all cancer subgroups i.e. diffuse and intestinal adenocarcinoma and GIST. Increased abundance of gut Enterobacteriaceae is strongly related to gut inflammation, which reprograms their metabolism to confers them growth advantage over other bacteria to survive in inflammatory environment [21]. Recently, association between increased Enterobacteriaceae abundance and long-term mortality risk is reported in a large Finnish population cohort [22]. Abundance of gut Enterobacteriaceae is also reported to increase with the severity of premalignant gastric cancer stages, with significantly increased abundances at metaplasia stage [15]. Similar to our results, higher abundance of gut Enterobacteriaceae is reported in preoperative Chinese gastric cancer patients compared to healthy controls [23]. However, low abundance of Bacteroidaceae in gastric cancer patients reported in this study [23] was not observed in our samples, while adenocarcinoma and GIST patients in our study had significantly low abundance of Lactobacillaceae. Lactobacillus a member of this family and a probiotic is one of the dominant bacteria in fermented dairy products especially yogurts, the intake of which is associated with a reduced risk of many types of cancer [24].
At the genus level, low abundances of Oscillibactor, Lachnoclostridium, Bifidobacterium, Parabacteroides and Barnesiella were seen in overall adenocarcinoma patients compared to controls. Similar to our findings, low abundances of gut Parabacteroides and Barnesiella is reported to be associated with the increasing severity of gastric lesions [15], while low abundances of Bifidobacteria, Lactobacilli, and higher abundances of Escherichia coli, Staphylococci, Enterococci and Peptostreptococci are reported in gastric cancer patients [25].
To the best of knowledge, our study is the first to analyze gut microbiota in GIST patients. GISTs are thought to arise from interstitial cells of Cajal that control the muscular movement of the gastrointestinal tract. Other than the abdominal pain and non-specific symptoms, bleeding and obstruction are among the commonly reported symptoms in GIST patients [26]. However, the role of microbiota is poorly documented. Probiotic treatment is reported to increase the number of Interstitial cells of Cajal in cats with chronic constipation [27]. Similarly, Clostridium butyricum has been found to regulate TLR2 expression in Interstitial cells of Cajal in ulcerative colitis [28]. We found that, alpha diversity in stool samples of GIST patients was not significantly different from that of controls. However, GIST patients had increased abundance of gut Enterobacteriaceae and reduced abundance of Lactobacillaceae and Oscillibacter compared to the controls, similar to that seen in gastric adenocarcinoma patients. Oscillibacter that showed lower abundance in GIST and intestinal adenocarcinoma in our study, is related to metabolic and inflammatory diseases, with lower levels seen in obese individuals [29] and high abundances in ulcerative colitis mice that correlate with serum interleukin IL6 and IL- levels [30]. Probiotics intake is reported to increase Oscillibacter abundance and changes gut microbiota composition that suppresses growth of hepatocellular carcinoma in mice model [31].
Higher abundance of Holdemania was seen in patients with mixed adenocarcinoma compared to the controls and also compared to the other cancer groups. Abundance of Holdemania is associated with heavy alcohol drinking [32], and with anxiety and stress [33], while a significant increased risk of gastric cancer with heavy drinking is reported [34]. As there were only two patients with mixed adenocarcinoma, it is difficult to draw any conclusions for this subgroup.
Conclusion
Our study shows that higher abundance of Enterobacteriaceae is a common feature seen in all subtypes of cancer of the stomach; diffuse, intestinal and gastric GIST. Patients with diffuse adenocarcinoma have lower gut microbiota diversity which could be related to their more aggressive tumor type or advanced stage of tumor. Further studies would be helpful in evaluating their role as a marker of tumor progression.
Methods
Patients and sample collection
Stool samples were collected by clinicians (AK and PP) from Finnish patients with gastric cancer or GIST, at Surgical and Meilahti Hospitals in Helsinki Uusimaa Hospital District, Finland. Only those patients who had no antimicrobial medication during the last 6 months prior to sample collection and had not started any cancer treatment were included in the study. The patients included were: GIST (N = 23) and gastric adenocarcinoma (N = 29). Of these, sequencing data of 6 GIST and 25 adenocarcinoma patients from our previous study [35], that compared microbiota in patients based on location of tumor in gastrointestinal tract (stomach, colon and rectum), were included in the present study. For controls, stool samples of 13 healthy Finnish individuals were collected and their sequencing data used in previous studies [35, 36] were included in the present study. All samples were collected and processed for DNA isolation and next generation sequencing (NGS) following same protocol and in the same laboratory. The details of the patient groups and control included in the analysis is described in Table 4.
Table 4.
Characteristics of patients and controls included in the gut microbiota analysis
| Group | No of casesa | Average age (years) | Sex (M/F) |
|---|---|---|---|
| Gastric adenocarcinoma | 29 | 72 ± 11 | 14/15 |
| Diffuse adenocarcinoma | 12 | 69 ± 11 | 5/7 |
| Intestinal adenocarcinoma | 15 | 75 ± 10 | 8/7 |
| Mixed adenocarcinoma | 2 | 69 ± 11 | 1/1 |
| GIST | 23 | 67 ± 14 | 11/12 |
| Controls | 13 | 44 ± 14 | 3/10 |
aSamples from previous study: Diffuse 11, Intestinal 13, Mixed 1, GIST 6, Controls 13
16S rRNA gene sequencing
DNA was extracted from stool samples using PSP Spin Stool DNA Plus Kit (Stratec Molecular, Berlin, Germany) and quality and quantity of DNA was checked by Qubit 3.0 Fluorimeter (Thermo Fisher Scientific, Waltham, MA, USA). Sequencing libraries were prepared from 3 ng of DNA, using Ion 16S Metagenomics kit (Thermo Fisher Scientific, Waltham, MA, USA) according to the vendor’s instructions. Six hypervariable regions (Primer set V2, V4, V8 and Primer set V3, V6-7, V9) of 16S rRNA gene were amplified in two reactions/sample. After PCR, the samples were end-repaired, purified with Agencourt® AMPure® XP beads (Beckman Coulter, Brea, California, USA) and ligated to barcoded sequencing adapters according to the kit protocol. The libraries were quantified by the TapeStation (Agilent Technologies, Santa Clara, CA, USA) and samples were diluted to a 10 pM concentration. The libraries were pooled and the template preparation was performed with either Ion OneTouch 2 system/ or Ion Chef system using the Ion PGM™ Hi-Q™ OT2 Kit/ Ion PGM™ Hi-Q™ Chef Kit (Thermo Fisher Scientific, Waltham, MA, USA) following the kit protocols. The OneTouch 2/ Ion Chef system was used for emulsion PCR and the quality of resulting Ion Spheres were checked with Qubit 3.0 fluorometer (Thermo Fisher Scientific, Waltham, MA, USA). Sequencing was performed on the Ion PGM system using the Ion 318™ Chip (Thermo Fisher Scientific, Waltham, MA, USA) and Ion PGM Hi-Q Sequencing kit (Thermo Fisher Scientific, Waltham, MA, USA).
Data analysis
Raw data from 16S rRNA gene sequencing was processed for quality check and filtering using Ion Torrent Suite software (Thermo Fisher Scientific, Waltham, MA, USA). Data was further analyzed for operational taxonomic unit (OTU) clustering, taxonomic classification using IonReporter v.5.10 (Thermo Fisher Scientific, Waltham, MA, USA) with Metagenomics 16S pipeline w1.1, applying default settings, and using Curated MicroSEQ(R) 16S Reference Library v2013.1 and Curated Greengenes v13.5 databases. Consensus tables were created by summing up all read counts from different V regions with identical taxonomic rank detection. A summary statistics of sample data is provided in Additional file 1: Table S1.
Data of 65 stool samples (including 44 published earlier) were grouped as Adenocarcinoma, GIST and Controls for cancer group comparison and as Intestinal, Diffuse, Mixed, GIST and Controls for cancer subgroup comparison. Alpha diversity (Shannon index) and richness (Chao1) of the gut microbiota among different groups was studied at the genus level using the microbiome [37] and vegan R packages [38]. The differences in the group comparison were tested for significance by the Wilcoxon-Mann–Whitney testand corrected for multiple testing with the Benjamini–Hochberg FDR method [39].
Unsupervised principal coordinates analysis (PCoA) was conducted with the phyloseq R package [40] and based on Bray–Curtis dissimilarity index [41]. Only the genera that were detected in at least 20% of all samples were included in the analysis. We used ALDEx2 [42] to identify taxonomic groups that showed significant (p < = 0.05) differences in paired group comparisons. The ALDEx2 R implementation takes advantage of the clr transformation for relative abundances to remove compositionality bias, and provides empirical p-values with Benjamini–Hochberg FDR correction. The standardized effect size and p-value estimation is based on a probabilistic sampling procedure described in [42]. In summary, the standardized effect size refers to the between group difference, scaled by the maximum within group difference.
Supplementary Information
Additional file 1: Table S1. Summary statistics of the sample data.
Acknowledgements
We wish to thank Homa Ehsan, Omar Youssef and Lauri Lehtimäki for their help with sample handling.
Authors’ contributions
The study was conceived and designed by SK, PP, AK and VS. Patients’ samples and clinical data were collected by AK and PP. Laboratory analysis was performed by MT, TK and VS. BM and LL performed data analysis. VS, SK, HR were the main responsible authors for writing/revising of the manuscript. All the authors read and approved the final manuscript.
Funding
The study was funded by grant received from Sigrid Jusѐlius Foundation, Finland to SK, Helsinki University Hospital Research Funds to PP, and Academy of Finland (295741) to LL.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical permission of the study was obtained from the Hospital District of Helsinki and Uusimaa (HUS) review board (ethical permission number 351/13/03/02/2014) and all patients gave their consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13099-021-00403-x.
References
- 1.Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar RD. Role of the normal gut microbiota. World J Gastroenterol. 2015;21:8787–8803. doi: 10.3748/wjg.v21.i29.8787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson AS, Koller KR, Ramaboli MC, Nesengani LT, Ocvirk S, Chen C, et al. Diet and the human gut microbiome: an international review. Dig Dis Sci. 2020;65:723–740. doi: 10.1007/s10620-020-06112-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 4.Wang X, Wei M, Sun Z. An association study of histological types of gastric carcinoma with Helicobacter pylori infection. Cell Biochem Biophys. 2014;70:283–287. doi: 10.1007/s12013-014-0052-z. [DOI] [PubMed] [Google Scholar]
- 5.Kunz PL, Gubens M, Fisher GA, Ford JM, Lichtensztajn DY, Clarke CA. Long-term survivors of gastric cancer: a California population-based study. J Clin Oncol. 2012;30:3507–3515. doi: 10.1200/JCO.2011.35.8028. [DOI] [PubMed] [Google Scholar]
- 6.Kim KM, Kwon MS, Hong SJ, Min KO, Seo EJ, Lee KY, et al. Genetic classification of intestinal-type and diffuse-type gastric cancers based on chromosomal loss and microsatellite instability. Virchows Arch. 2003;443:491–500. doi: 10.1007/s00428-003-0840-0. [DOI] [PubMed] [Google Scholar]
- 7.Vauhkonen M, Vauhkonen H, Sajantila A, Sipponen P. Differences in genomic instability between intestinal- and diffuse-type gastric cancer. Gastric Cancer. 2005;8:238–244. doi: 10.1007/s10120-005-0346-3. [DOI] [PubMed] [Google Scholar]
- 8.Corso G, Pedrazzani C, Pinheiro H, Fernandes E, Marrelli D, Rinnovati A, et al. E-cadherin genetic screening and clinico-pathologic characteristics of early onset gastric cancer. Eur J Cancer. 2011;47:631–639. doi: 10.1016/j.ejca.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Cancer Genome Atlas Research Network Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oppelt PJ, Hirbe AC, Van Tine BA. Gastrointestinal stromal tumors (GISTs): point mutations matter in management, a review. J Gastrointest Oncol. 2017;8:466–473. doi: 10.21037/jgo.2016.09.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iizasa H, Ishihara S, Richardo T, Kanehiro Y, Yoshiyama H. Dysbiotic infection in the stomach. World J Gastroenterol. 2015;21:11450–11457. doi: 10.3748/wjg.v21.i40.11450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang F, Meng W, Wang B, Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. 2014;345:196–202. doi: 10.1016/j.canlet.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Wang Z, Gao X, Zeng R, Wu Q, Sun H, Wu W, et al. Changes of the gastric mucosal microbiome associated with histological stages of gastric carcinogenesis. Front Microbiol. 2020;11:997. doi: 10.3389/fmicb.2020.00997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gantuya B, El Serag HB, Matsumoto T, Ajami NJ, Uchida T, Oyuntsetseg K, et al. Gastric mucosal microbiota in a Mongolian population with gastric cancer and precursor conditions. Aliment Pharmacol Ther. 2020;51:770–780. doi: 10.1111/apt.15675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao JJ, Zhang Y, Gerhard M, Mejias-Luque R, Zhang L, Vieth M, et al. Association between gut microbiota and Helicobacter pylori-related gastric lesions in a high-risk population of gastric cancer. Front Cell Infect Microbiol. 2018;8:202. doi: 10.3389/fcimb.2018.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xuan C, Shamonki JM, Chung A, Dinome ML, Chung M, Sieling PA, et al. Microbial dysbiosis is associated with human breast cancer. PLoS ONE. 2014;9:e83744. doi: 10.1371/journal.pone.0083744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pantaleo MA, Tarantino G, Agostinelli C, Urbini M, Nannini M, Saponara M, et al. Immune microenvironment profiling of gastrointestinal stromal tumors (GIST) shows gene expression patterns associated to immune checkpoint inhibitors response. Oncoimmunology. 2019;8:e1617588. doi: 10.1080/2162402X.2019.1617588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim TS, da Silva E, Coit DG, Tang LH. Intratumoral immune response to gastric cancer varies by molecular and histologic subtype. Am J Surg Pathol. 2019;43:851–860. doi: 10.1097/PAS.0000000000001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Z, Huang J, Li X, Xing J, Chen Q, Liu R, et al. Gut microbiota regulate tumor metastasis via circRNA/miRNA networks. Gut Microbes. 2020;12:1788891. doi: 10.1080/19490976.2020.1788891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science. 2015;350:1084–1089. doi: 10.1126/science.aac4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kitamoto S, Alteri CJ, Rodrigues M, Nagao-Kitamoto H, Sugihara K, Himpsl SD, et al. Dietary L-serine confers a competitive fitness advantage to Enterobacteriaceae in the inflamed gut. Nat Microbiol. 2020;5:116–125. doi: 10.1038/s41564-019-0591-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salosensaari A, Laitinen V, Havulinna A, Meric G, Cheng S, Perola M, et al. Taxonomic signatures of long-term mortality risk in human gut microbiota. medRxiv. 2019;1:1. doi: 10.1101/2019.12.30.19015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang W, Yang Y, Wang H, Wang H, Yu X, Lu Y, et al. Gut microbiota shifts in patients with gastric cancer in perioperative period. Medicine (Baltimore) 2019;98:e16626. doi: 10.1097/MD.0000000000016626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang K, Dai H, Liang W, Zhang L, Deng Z. Fermented dairy foods intake and risk of cancer. Int J Cancer. 2019;144:2099–2108. doi: 10.1002/ijc.31959. [DOI] [PubMed] [Google Scholar]
- 25.Zhou G, Yang J. Correlations of gastrointestinal hormones with inflammation and intestinal flora in patients with gastric cancer. J BUON. 2019;24:1595–1600. [PubMed] [Google Scholar]
- 26.Søreide K, Sandvik OM, Søreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46. doi: 10.1016/j.canep.2015.10.031. [DOI] [PubMed] [Google Scholar]
- 27.Rossi G, Jergens A, Cerquetella M, Berardi S, Di Cicco E, Bassotti G, et al. Effects of a probiotic (SLAB51) on clinical and histologic variables and microbiota of cats with chronic constipation/megacolon: a pilot study. Benef Microbes. 2018;9:101–110. doi: 10.3920/BM2017.0023. [DOI] [PubMed] [Google Scholar]
- 28.Sui SJ, Tian ZB, Wang QC, Chen R, Nie J, Li JS, et al. Clostridium butyricum promotes intestinal motility by regulation of TLR2 in interstitial cells of Cajal. Eur Rev Med Pharmacol Sci. 2018;22:4730–4738. doi: 10.26355/eurrev_201807_15533. [DOI] [PubMed] [Google Scholar]
- 29.Hu HJ, Park SG, Jang HB, Choi MK, Park KH, Kang JH, et al. Obesity alters the microbial community profile in Korean Adolescents. PLoS ONE. 2015;10:e0134333. doi: 10.1371/journal.pone.0134333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu M, Li P, An Y, Ren J, Yan D, Cui J, et al. Phloretin ameliorates dextran sulfate sodium-induced ulcerative colitis in mice by regulating the gut microbiota. Pharmacol Res. 2019;150:104489. doi: 10.1016/j.phrs.2019.104489. [DOI] [PubMed] [Google Scholar]
- 31.Li J, Sung CY, Lee N, Ni Y, Pihlajamäki J, Panagiotou G, et al. Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice. Proc Natl Acad Sci USA. 2016;113:E1306–E1315. doi: 10.1073/pnas.1518189113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bjørkhaug ST, Aanes H, Neupane SP, Bramness JG, Malvik S, Henriksen C, et al. Characterization of gut microbiota composition and functions in patients with chronic alcohol overconsumption. Gut Microbes. 2019;10:663–675. doi: 10.1080/19490976.2019.1580097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chung YE, Chen HC, Chou HL, Chen IM, Lee MS, Chuang LC, et al. Exploration of microbiota targets for major depressive disorder and mood related traits. J Psychiatr Res. 2019;111:74–82. doi: 10.1016/j.jpsychires.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 34.Rota M, Pelucchi C, Bertuccio P, Matsuo K, Zhang ZF, Ito H, et al. Alcohol consumption and gastric cancer risk—a pooled analysis within the StoP project consortium. Int J Cancer. 2017;141:1950–1962. doi: 10.1002/ijc.30891. [DOI] [PubMed] [Google Scholar]
- 35.Youssef O, Lahti L, Kokkola A, Karla T, Tikkanen M, Ehsan H, et al. Stool microbiota composition differs in patients with stomach, colon, and rectal neoplasms. Dig Dis Sci. 2018;63:2950–2958. doi: 10.1007/s10620-018-5190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarhadi V, Lahti L, Saberi F, Youssef O, Kokkola A, Karla T, et al. Gut microbiota and host gene mutations in colorectal cancer patients and controls of Iranian and Finnish origin. Anticancer Res. 2020;40(3):1325–1334. doi: 10.21873/anticanres.14074. [DOI] [PubMed] [Google Scholar]
- 37.Lahti L and Shetty S (Bioconductor 2017). Tools for microbiome analysis in R. Microbiome package version 0.99.88. https://www.bioconductor.org/packages/devel/bioc/html/microbiome.html. 2017.
- 38.Oksanen J, Blanchet FG, Friendly M, Kindt R, Legendre P, McGlinn D, et al. vegan: community ecology package. 2017. https://cran.r-project.org/web/packages/vegan/index.html.
- 39.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Statist Soc Series B. 1995;57:289–300. [Google Scholar]
- 40.McMurdie PJ, Holmes S. Phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE. 2013;8:e61217. doi: 10.1371/journal.pone.0061217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Legendre P, Gallagher ED. Ecologically meaningful transformations for ordination of species data. Oecologia. 2001;129:271–280. doi: 10.1007/s004420100716. [DOI] [PubMed] [Google Scholar]
- 42.Fernandes DA, Reid J, Macklaim MJ, McMurrough TA, Edgell DR, Gloor BG. Unifying the analysis of high-throughput sequencing datasets: characterizing RNA-seq, 16S rRNA gene sequencing and selective growth experiments by compositional data analysis. Microbiome. 2014;2:15. doi: 10.1186/2049-2618-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Summary statistics of the sample data.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.