Summary
Introduction
Insomnia is a global health problem among university students which is associated with various psychiatric problems like depression and anxiety. While different developed and developing countries assessed the prevalence of insomnia in youth, currently there is hardly systematic review of studies found based on the prevalence of insomnia in South Asia.
Aims
The aim of this study is to systematically review the evidence relating to the prevalence rate of insomnia in university students in South Asian countries.
Methods
Electronic searches of three databases, PubMed, Cochrane library, and Worldwide science were performed from 2010 to 2020 before April. In total, seven studies were included for evaluating insomnia in South Asian region among university students.
Results
The prevalence rates of insomnia of the seven studies ranged between 35.4% (95% CI: 32.4-38.5%) and 70% (95% CI: 65.7-74.1%). The pooled prevalence of insomnia among university students was 52.1% (95% CI: 41.1-63.1%).
Conclusions
This review emphasized that insomnia in university students might be a common health issue to give full concentration in their studies and academic performance. Thus, more attention should be given to the determinants of insomnia among university students, so that it could be helpful to identify the main causes of insomnia and effective measures could be taken.
Keywords: Insomnia, Prevalence, University students, Systematic review, South Asia
Introduction
Insomnia is a disease condition when an individual finds difficulty in sleeping or remaining asleep [1] and it is associated with various psychiatric conditions like depression, anxiety, etc. [2-4]. Many recent studies have found that insomnia is a common psychiatric problem among young adults and university students [5, 6]. Other studies found that the prevalence rate of the poor sleeping condition is high among undergraduate students in the world [7]. Sleep quality and quantity among young adults especially university students has been changed due to the rapid development of technology such as using social media, the internet, etc. [8, 9] and there is a positive relationship between insomnia and the use of social media through the internet [10]. It is believed that poor sleep quality has an effect on physical and mental health and also causes mental problems such as anxiety and depression [11, 12]. Another study found that the effects of sleep disturbance have secondary behavioral consequences such as impaired social relationships, increased risk-taking behavior, and road accidents, etc. [13]. Sleep restriction among healthy young adults has been suffered from deleterious effects on endocrine functions, metabolic and inflammatory responses [14]. Many studies have shown that sleep is associated and affected by increasing years in university education [15, 16]. As university students represent the future of the society, the cost of sleep disturbance is high [17, 18].
Although the prevalence rate of insomnia increases day by day among adolescents, adults and university students, university students have received a little attention than others [5, 19, 20]. In a study which has found that 30% of the adult population from different countries have had symptoms of insomnia [21]. Other studies reported that the incidence of sleeping problem among university students was 14.9 to 70.3% [22, 23]. The variations of the prevalence of sleep problems appear to be affected by many factors such as geographical location, methods of assessment etc. [6, 24]. The evaluation method of insomnia varied from studies to studies. Some studies showed a low prevalence of insomnia using Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) or international classification of sleep disorder [6], some studies showed a high prevalence of insomnia without using any restrictive and standardize criteria [24, 25] and some studies evaluate the rate of insomnia using quantitative scales only [5, 26].
The present systematic review was aimed at to evaluate and explore high-quality studies and identify the prevalence of insomnia among university students in the South Asian Region from 2010 to 2020.
Methods
The reporting of this review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
SEARCH STRATEGY
The following electronic databases were searched: PubMed, Cochrane library and Worldwide science to identify peer reviewed articles, published between January 2010 and April 2020, reporting sleeping quality among university students. We used combinations of medical subject headings (MeSH) and free text words. Searches used the keywords (“insomnia” or “sleep quality” or “sleep disturbance” or “sleep disorder”) AND (“prevalence” or “cross-sectional study”) AND (“university student” or “undergraduate” or “young adult” or “medical student”) AND (“Afghanistan” or “Bangladesh” or “Bhutan” or “Nepal” or “India” or “Maldives” or “Sri Lanka” or “Pakistan”). Searches were limited to articles published in English.
SELECTION PROCESS
Two researchers have screened the titles and abstracts and then full texts were retrieved for selected records. Finally, a quality assessment was performed during data extraction by another researcher.
DATA EXTRACTION
Articles were considered for inclusion if the study was cross-sectional study; studies included students in medical college or university; studies included an aim to provide the prevalence of sleeping quality, studies measured the sleeping quality with some quantitative and validated scales, studies carried out in South Asian region (Bangladesh, India, Afghanistan, Bhutan, Nepal, Pakistan, Sri Lanka and Maldives). The exclusion criteria were: a) failure to provide the separate prevalence of sleeping quality; b) studies didn’t include response rate; c) other epidemiological studies such as clinical trials. Demographic data, response rate, sample size, diagnostic scales used and prevalence data on student’s sleeping quality were abstracted.
QUALITY ASSESSMENT
The quality assessment instruction used in our study which was adopted from the article Ibrahim et al. [27]. The instruction included: 1) defined the population of study clearly; 2) selected the population randomly; 3) represented university students; 4) response rate ≥ 70%; 5) used validated scales for measuring sleeping quality; 6) sample size ≥ 300; 7) reported standard deviation (SD) or confidence interval (CI).
STATISTICAL ANALYSIS
Heterogeneity by reporting the I2 (% residual variation due to heterogeneity) and τ2 (method of moments estimates of between-study variance) of the pooled estimate were assessed. A random effects model was used to pool the prevalence of insomnia as higher heterogeneity was expected. The 95% CI had been reported in a pooled analysis. All analysis was done by using MetaXL software version 5.3 in the Excel sheet.
Results
In this review, 787 peer reviewed articles were identified and after examining the titles, abstracts, and reference lists, 27 articles were retrieved. After careful reading and quality assessment, seven articles [28-34] were included in this study. Twenty articles were excluded as they didn’t maintain the criteria we followed (Fig. 1).
Fig. 1.
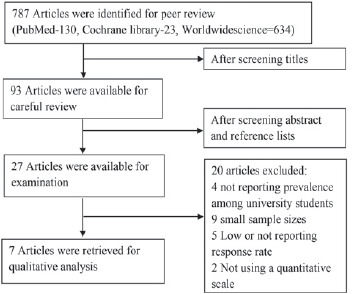
The flowchart of searching and selecting articles for systematic review and meta-analysis.
Table I represents the demographic and methodological information of the selected studies from 2010 to 2020 before April. The overall sample size in the current review was 3,739 with a minimum of 308 and a maximum of 937. The mean age was ranged from 19 to 24 years. The percentage of males in the studies ranged from 37.1 to 57.14%. Three out of the seven studies were carried out in India, two in Pakistan and one in Nepal and Bangladesh. Among the seven studies, five studies used a simple random sampling method and two used a convenience sampling method. Moreover, all studies were cross-sectional studies.
Tab. I.
The information on the demographic and methodologies of selected studies from 2010 to 2020.
| Research | Amina et al. | Parash et al. | Amer et al. | Ashwini et al. | Amit et al. | Arif et al. | Syeda et al. |
|---|---|---|---|---|---|---|---|
| Year | 2018 | 2017 | 2019 | 2019 | 2016 | 2015 | 2019 |
| Country | Pakistan | Nepal | India | India | India | Pakistan | Bangladesh |
| Sample | 1AB | 1A | 1A | 1B | 1B | 2B | 2A |
| Insomnia scale | PSQI | PSQI | PSQI | PSQI | PSQI | PQSI, ESS | PQSI |
| Cut-off | > 5 | > 5 | > 5 | > 5 | > 5 | > 5, > 10 | > 5 |
| Sample size | 520 | 937 | 617 | 463 | 308 | 504 | 390 |
| Response rate | 85.8% | 92% | 95.07% | 92.6% | 96.25% | 77.5% | 75% |
| Sex male (%) | 37.1 | 45.4 | 51 | 38.2 | 57.14 | 40.5 | 40.3 |
| Mean age(± ± ± SD) | 20.25 (1.5) | 21.01 (2.18) | 23.4 (3.6) | 19.55 (1.04) | 21.4 (1.85) | 20 (1.4) | NR |
| Total Prevalence(%) | 59.04 | 35.4 | 51 | 70 | 39.6 | 39.5 | 69.5 |
| Covariates measured | Sleep quality was higher among non-medical students than in medical students | Depression, internet addiction | Physical activity, depression, anxiety | Computer vision syndrome, headache, light sensitivity, double vision | Analgesic self-medication, headache | Poor sleep quality was higher among females | Association of social status and internet use with sleep quality was measured |
PSQI = Pittsburgh Sleep Quality Index; ESS = Epworth Sleepiness Scale; SD = Standard Deviation; 1 = random sampling; 2 = convenience sampling; A = university sample; B = medical sample; NR = Not Reported.
Figure 2 shows the forest plots of insomnia among university students. The prevalence rates of insomnia of the seven studies ranged between 35.4% (95% CI: 32.4-38.5%) and 70% (95% CI: 65.7-74.1%). The pooled prevalence of insomnia among university students was 52.1% (95% CI: 41.1-63.1%).
Fig. 2.
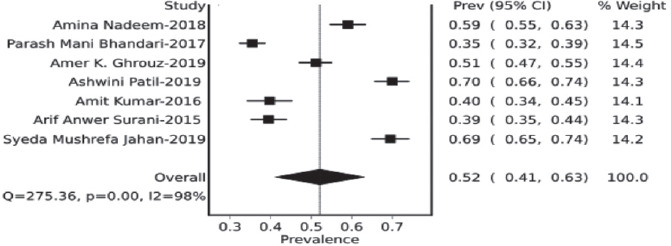
Forest plots about Insomnia studies among university students.
Discussion
In the 27 studies examined, some studies failed to report the prevalence of insomnia, some didn’t use proper measurement scales, and some did not show a response rate. A higher prevalence of insomnia (52.1%, 95% CI: 41.1-63.1%) was observed in this review than normal people of similar age (7.4%, 95% CI: 5.8-9.0%) [6]. Some studies outside of South Asia, reported that the prevalence of insomnia was 51.8% in Chile [35] and 58.7% in Lebanon [36] which was similar and higher than our findings respectively. Another study in Pakistan found that the poor sleeping quality among medical students was 77% and among them, 7.6% reported self-medication as a cause of insomnia [37]. Some developed countries showed a low prevalence of insomnia among university students than our findings in this review. In the USA, the prevalence of insomnia was 12% and among them 8% were males and 14% were females [38]. In China, the rate of insomnia prevalence was 18.80% [39] and in Japan, it was 25.6% [40].
Some factors were related to the high prevalence of insomnia among university students reported in many studies and these contributing factors were stress for concerning their future and employment, late night work on the computer, social interactions with friends, environmental noise, etc. [41-45]. A study in Nepal found that 31.5% of medical students suffered from sleep deprivation due to late night internet use [46]. Among the seven selected studies, one study reported that females had a higher prevalence of insomnia compared with males which was similar to many previous studies [47-50]. Good sleep quality reported by participants is a good sign, as according to WHO good health and wellbeing could be maintained by good sleep hygiene [51].
Pittsburgh Sleep Quality Index (PSQI) is a widely used instrument for assessing sleep quality and it measures sleep quality along with seven components [52]. In our review, all the studies have used PSQI for measuring the prevalence of insomnia among university students. However, different types of scales can be used to measure the prevalence of insomnia and many differences are observed in the prevalence of insomnia when using different scales. So, more well-designed studies are required for the evaluation of insomnia prevalence among university students.
This review has several strengths and limitations. As high-quality studies were used, there is no possibility of publication bias. The limitation of this review is, missed the studies which were not published in English and did not include all studies reporting the prevalence of insomnia as they did not use a formal and standard scale and did not define the sample accurately.
Conclusions
Despite all limitations, this systematic review provided the evidence of the prevalence rates of insomnia among the university student in South Asian countries. As the pooled prevalence of insomnia is considerably higher than the general population, this review emphasized that insomnia in university students is a common health issue and more attention should be given to reduce insomnia among university students.
Figures and tables
Acknowledgements
All the authors whose research participated in this systematic review.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
AIC has designed the study and contributed on the data extraction, data analysis, interpretation and the manuscript writing. SG has contributed on the data extraction and analysis. She has also helped in the manuscript writing and critically review the manuscript as well. MFH and KKAS contributed on data extraction. FA contributed on data extraction and data analysis.
References
- [1].Roth T. Insomnia: definition, prevalence, etiology, and consequences. JCSM 2007;3(Suppl. 5):S7 https://doi.org/10.5664/jcsm.26929 10.5664/jcsm.26929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mason EC, Harvey AG. Insomnia before and after treatment for anxiety and depression. J Affect Disord 2014;168:415-21. https://doi.org/10.1016/j.jad.2014.07.020 10.1016/j.jad.2014.07.020 [DOI] [PubMed] [Google Scholar]
- [3].Øyane NM, Pallesen S, Moen BE, Åkerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One 2013;8(8). https://doi.org/10.1371/journal.pone.0070228 10.1371/journal.pone.0070228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Terauchi M, Hiramitsu S, Akiyoshi M, Owa Y, Kato K, Obayashi S, Matsushima E, Kubota T. Associations between anxiety, depression and insomnia in peri-and post-menopausal women. Maturitas 2012;72:61-5. https://doi.org/10.1016/j.maturitas.2012.01.014 10.1016/j.maturitas.2012.01.014 [DOI] [PubMed] [Google Scholar]
- [5].Wali S, Krayem A, Samman Y, Mirdad S, Alshimemeri A, Almobaireek A. Sleep disorders in Saudi health care workers. Ann Saudi Med 1999;19:406-9. https://doi.org/10.5144/0256-4947.1999.406 10.5144/0256-4947.1999.406 [DOI] [PubMed] [Google Scholar]
- [6].Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002;6:97-111. https://doi.org/10.1053/smrv.2002.0186 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- [7].Jiang XL, Zheng XY, Yang J, Ye CP, Chen YY, Zhang ZG, Xiao ZJ. A systematic review of studies on the prevalence of insomnia in university students. Public Health 2015;129:1579-84. https://doi.org/10.1016/j.puhe.2015.07.030 10.1016/j.puhe.2015.07.030 [DOI] [PubMed] [Google Scholar]
- [8].Siomos KE, Avagianou PA, Floros GD, Skenteris N, Mouzas OD, Theodorou K, Angelopoulos NV. Psychosocial correlates of insomnia in an adolescent population. Child Psychiatry Hum Dev 2010;41:262-73. https://doi.org/10.1007/s10578-009-0166-5 10.1007/s10578-009-0166-5 [DOI] [PubMed] [Google Scholar]
- [9].Brunborg GS, Mentzoni RA, Molde H, Myrseth H, Skouverøe KJ, Bjorvatn B, Pallesen S. The relationship between media use in the bedroom, sleep habits and symptoms of insomnia. JJ Sleep Res 2011;20:569-75. https://doi.org/10.1111/j.1365-2869.2011.00913.x 10.1111/j.1365-2869.2011.00913.x [DOI] [PubMed] [Google Scholar]
- [10].Jha RK, Shah DK, Basnet S, Paudel KR, Sah P, Sah AK, Adhikari K. Facebook use and its effects on the life of health science students in a private medical college of Nepal. BMC Res Notes 2016;9:378 https://doi.org/10.1186/s13104-016-2186-0 10.1186/s13104-016-2186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Carney CE, Moss TG, Lachowski AM, Atwood ME. Understanding mental and physical fatigue complaints in those with depression and insomnia. Behav Sleep Med 2014;12:272-89. https://doi.org/10.1080/15402002.2013.801345 10.1080/15402002.2013.801345 [DOI] [PubMed] [Google Scholar]
- [12].Sivertsen B, Krokstad S, Øverland S, Mykletun A. The epidemiology of insomnia. Associations with physical and mental health: the HUNT-2 study. J Psychosom Res 2009;67:109-16. https://doi.org/10.1016/j.jpsychores.2009.05.001 10.1016/j.jpsychores.2009.05.001 [DOI] [PubMed] [Google Scholar]
- [13].Sweileh WM, Ali IA, Sawalha AF, Abu-Taha AS, Sa’ed HZ, Al-Jabi SW. Sleep habits and sleep problems among Palestinian students. Child Adolesc Psychiatry Ment Health 2011;5:25 https://doi.org/10.1186/1753-2000-5-25 10.1186/1753-2000-5-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Tootoonchian F. Evaluation of effect of sleep hygiene education program on insomnia, daytime sleepiness and sleep quality in shift work nurses. J QUMS 2015. [Google Scholar]
- [15].Tsai L-L, Li S-P. Sleep patterns in college students: gender and grade differences. J Psychosom Res 2004;56:231-7. [DOI] [PubMed] [Google Scholar]
- [16].Galambos NL, Vargas Lascano DI, Howard AL, Maggs JL. Who sleeps best? Longitudinal patterns and covariates of change in sleep quantity, quality, and timing across four university years. Behav Sleep Med 2013;11:8-22. https://doi.org/10.1080/15402002.2011.596234 10.1080/15402002.2011.596234 [DOI] [PubMed] [Google Scholar]
- [17].Jhaveri M, Seal B, Pollack M, Wertz D. Will insomnia treatments produce overall cost savings to commercial managed-care plans? A predictive analysis in the United States. Curr Med Res Opin 2007;23:1431-43. https://doi.org/10.1185/030079907X199619 10.1185/030079907X199619 [DOI] [PubMed] [Google Scholar]
- [18].Siriwardena AN, Apekey T, Tilling M, Harrison A, Dyas JV, Middleton HC, Ørner R, Sach T, Dewey M, Qureshi ZM. Effectiveness and cost-effectiveness of an educational intervention for practice teams to deliver problem focused therapy for insomnia: rationale and design of a pilot cluster randomised trial. BMC Fam Pract 2009;10:9 https://doi.org/10.1186/1471-2296-10-9 10.1186/1471-2296-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].BaHammam A, Bin Saeed A, Al-Faris E, Shaikh S. Sleep duration and its correlates in a sample of Saudi elementary school children. Singapore Med J 2006;47:875. [PubMed] [Google Scholar]
- [20].Navelet Y. Insomnia in the child and adolescent. Sleep 1996;19(Suppl. 3):S723-S8. [PubMed] [Google Scholar]
- [21].Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep 1999;22:S347-53. [PubMed] [Google Scholar]
- [22].Schlarb AA, Kulessa D, Gulewitsch MD. Sleep characteristics, sleep problems, and associations of self-efficacy among German university students. Nat Sci Sleep 2012;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Buboltz WC, Jr, Brown F, Soper B. Sleep habits and patterns of college students: a preliminary study. J Am Coll Health 2001;50:131-5. https://doi.org/10.1080/07448480109596017 10.1080/07448480109596017 [DOI] [PubMed] [Google Scholar]
- [24].Ohayon MM, Hong S-C. Prevalence of insomnia and associated factors in South Korea. J Psychosom Res 2002;53:593-600. https://doi.org/10.1016/S0022-3999(02)00449-X 10.1016/S0022-3999(02)00449-X [DOI] [PubMed] [Google Scholar]
- [25].Kim WH, Kim BS, Kim SK, Chang SM, Lee DW, Cho MJ, Bae JN. Prevalence of insomnia and associated factors in a community sample of elderly individuals in South Korea. Int Psychogeriatr 2013;25:1729-37. [DOI] [PubMed] [Google Scholar]
- [26].Vand HDA, Gharraee B, Farid A-AA, Bandi MG. Prediction of insomnia severity based on cognitive, metacognitive, and emotional variables in college students. Explore 2014;10:233-40. https://doi.org/10.1016/j.explore.2014.04.005 10.1016/j.explore.2014.04.005 [DOI] [PubMed] [Google Scholar]
- [27].Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res 2013;47:391-400. https://doi.org/10.1016/j.jpsychires.2012.11.015 10.1016/j.jpsychires.2012.11.015 [DOI] [PubMed] [Google Scholar]
- [28].Nadeem A, Cheema MK, Naseer M, Javed H. Comparison of quality of sleep between medical and non-medical undergraduate Pakistani students. JPMA 2018;68:1465-70. [PubMed] [Google Scholar]
- [29].Bhandari PM, Neupane D, Rijal S, Thapa K, Mishra SR, Poudyal AK. Sleep quality, internet addiction and depressive symptoms among undergraduate students in Nepal. BMC Psychiatry 2017;17:106 https://doi.org/10.1186/s12888-017-1275-5 10.1186/s12888-017-1275-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ghrouz AK, Noohu MM, Manzar MD, Spence DW, BaHammam AS, Pandi-Perumal SR. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath 2019;23:627-34. https://doi.org/10.1007/s11325-019-01780-z 10.1007/s11325-019-01780-z [DOI] [PubMed] [Google Scholar]
- [31].Kumar A, Vandana ANA. Analgesics self-medication and its association with sleep quality among medical undergraduates. JCDR 2016;10:FC07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Surani AA, Zahid S, Surani A, Ali S, Mubeen M, Khan RH. Sleep quality among medical students of Karachi, Pakistan. J Pak Med Assoc 2015;65:380-2. [PubMed] [Google Scholar]
- [33].Patil A, Bhavya SC, Srivastava S. Eyeing computer vision syndrome: awareness, knowledge, and its impact on sleep quality among medical students. Ind Psychiatry J 2019;28:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Jahan SM, Hossain SR, Sayeed UB, Wahab A, Rahman T, Hossain A. Association between internet addiction and sleep quality among students: a cross-sectional study in Bangladesh. Sleep Biol Rhythms 2019;17:323-9. https://doi.org/10.1007/s41105-019-00219-y 10.1007/s41105-019-00219-y [DOI] [Google Scholar]
- [35].Vélez JC, Souza A, Traslaviña S, Barbosa C, Wosu A, Andrade A, Frye M, Fitzpatrick AL, Gelaye B, Williams MA. The epidemiology of sleep quality and consumption of stimulant beverages among Patagonian Chilean college students. Sleep Disord 2013;2013 https://doi.org/10.1155/2013/910104 10.1155/2013/910104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kabrita CT, Duffy JF, Hajjar-Muça T. Predictors of poor sleep quality among Lebanese university students: association between evening typology, lifestyle behaviors, and sleep habits. Nat Sci Sleep 2014;6:11-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. Peer J 2015;3:e840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Gaultney JF. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Health 2010;59:91-7. https://doi.org/10.1080/07448481.2010.483708 10.1080/07448481.2010.483708 [DOI] [PubMed] [Google Scholar]
- [39].Xu Z, Su H, Zou Y, Chen J, Wu J, Chang W. Sleep quality of Chinese adolescents: distribution and its associated factors. J Paediatr Child Health 2012;48:138-45. https://doi.org/10.1111/j.1440-1754.2011.02065.x 10.1111/j.1440-1754.2011.02065.x [DOI] [PubMed] [Google Scholar]
- [40].Pallos H, Gergely V, Yamada N, Miyazaki S, Okawa M. The quality of sleep and factors associated with poor sleep in Japanese graduate students. Sleep Biol Rhythms 2007;5:234-8. https://doi.org/10.1111/j.1479-8425.2007.00316.x 10.1111/j.1479-8425.2007.00316.x [DOI] [Google Scholar]
- [41].Voelker R. Stress, sleep loss, and substance abuse create potent recipe for college depression. Jama 2004;291:2177-9. https://doi.org/10.1001/jama.291.18.2177 10.1001/jama.291.18.2177 [DOI] [PubMed] [Google Scholar]
- [42].Schmidt RE, Gay P, Van der Linden M. Facets of impulsivity are differentially linked to insomnia: evidence from an exploratory study. Behav Sleep Med 2008;6:178-92. https://doi.org/10.1080/15402000802162570 10.1080/15402000802162570 [DOI] [PubMed] [Google Scholar]
- [43].Fernández-Mendoza J, Vela-Bueno A, Vgontzas AN, Olavarrieta-Bernardino S, Ramos-Platón MJ, Bixler EO, De la Cruz-Troca JJ. Nighttime sleep and daytime functioning correlates of the insomnia complaint in young adults. J Adolesc 2009;32:1059-74. https://doi.org/10.1016/j.adolescence.2009.03.005 10.1016/j.adolescence.2009.03.005 [DOI] [PubMed] [Google Scholar]
- [44].Schmidt RE, Gay P, Ghisletta P, Van der Linden M. Linking impulsivity to dysfunctional thought control and insomnia: a structural equation model. J Sleep Res 2010;19:3-11. https://doi.org/10.1111/j.1365-2869.2009.00741.x 10.1111/j.1365-2869.2009.00741.x [DOI] [PubMed] [Google Scholar]
- [45].Gellis LA, Arigo D, Elliott JC. Cognitive refocusing treatment for insomnia: A randomized controlled trial in university students. Behav Ther 2013;44:100-10. https://doi.org/10.1016/j.beth.2012.07.004 10.1016/j.beth.2012.07.004 [DOI] [PubMed] [Google Scholar]
- [46].Pramanik T, Sherpa M, Shrestha R. Internet addiction in a group of medical students: a cross sectional study. NMCJ 2012;14:46-8. [PubMed] [Google Scholar]
- [47].Jaussent I, Dauvilliers Y, Ancelin ML, Dartigues JF, Tavernier B, Touchon J, Ritchie K, Besset A. Insomnia symptoms in older adults: associated factors and gender differences. Am J Geriatr Psychiatry 2011;19:88-97. https://doi.org/10.1097/JGP.0b013e3181e049b6 10.1097/JGP.0b013e3181e049b6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Johansson P, Årestedt K, Alehagen U, Svanborg E, Dahlström U, Broström A. Sleep disordered breathing, insomnia, and health related quality of life - a comparison between age and gender matched elderly with heart failure or without cardiovascular disease. Eur J Cardiovasc Nurs 2010;9:108-17. https://doi.org/10.1016/2Fj.ejcnurse.2009.11.005 10.1016/2Fj.ejcnurse.2009.11.005 [DOI] [PubMed] [Google Scholar]
- [49].Yoshioka E, Saijo Y, Kita T, Satoh H, Kawaharada M, Fukui T, Kishi R. Gender differences in insomnia and the role of paid work and family responsibilities. Soc Psychiatry Psychiatr Epidemiol 2012;47:651-62. [DOI] [PubMed] [Google Scholar]
- [50].Suen LK, Ellis Hon K, Tam WW. Association between sleep behavior and sleep-related factors among university students in Hong Kong. Chronobiol Int 2008;25:760-75. https://doi.org/10.1080/07420520802397186 10.1080/07420520802397186 [DOI] [PubMed] [Google Scholar]
- [51].Bonnie R, Stroud C, Breiner H, Committee on Improving the Health, Safety and Well-Being of Young Adults; Board on Children, Youth and Families; Institute of Medicine; National Research Council Investing in the health and well-being of young adults. Washington (DC): National Academies Press (US) 2015. [PubMed] [Google Scholar]
- [52].Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med 2010;11:735-42. https://doi.org/10.1016/j.sleep.2010.02.006 10.1016/j.sleep.2010.02.006 [DOI] [PubMed] [Google Scholar]


