Abstract
We assessed the presence of Rickettsia spp., Coxiella burnetii and Anaplasma phagocytophilum in reptiles, their ectoparasites and in questing ticks collected in a nature preserve park in southern Italy, as well as in a peri-urban area in another region. We also investigated the exposure to these pathogens in forestry workers, farmers and livestock breeders living or working in the nature preserve park given the report of anecdotal cases of spotted fever rickettsioses. Rickettsia spp. were molecularly detected in Podarcis muralis and Podarcis siculus lizards (i.e., 3.1%), in Ixodes ricinus (up to 87.5%) and in Neotrombicula autumnalis (up to 8.3%) collected from them as well as in I. ricinus collected from the environment (up to 28.4%). Rickettsia monacensis was the most prevalent species followed by Rickettsia helvetica. An undescribed member of the family Anaplasmataceae was detected in 2.4% and 0.8% of the reptiles and ectoparasites, respectively. Sera from human subjects (n = 50) were serologically screened and antibodies to Rickettsia spp. (n = 4; 8%), C. burnetti (n = 8; 16%) and A. phagocytophilum (n = 11; 22%) were detected. Two ticks collected from two forestry workers were positive for spotted fever group (SFG) rickettsiae. Ixodes ricinus is involved in the transmission of SFG rickettsiae (R. monacensis and R. helvetica) in southern Europe and lizards could play a role in the sylvatic cycle of R. monacensis, as amplifying hosts. Meanwhile, N. autumnalis could be involved in the enzootic cycle of some SFG rickettsiae among these animals. People living or working in the southern Italian nature preserve park investigated are exposed to SFG rickettsiae, C. burnetii and A. phagocytophilum.
Author summary
Zoonotic pathogens such as Rickettsia spp., Coxiella burnetii and Anaplasma phagocytophilum are associated with ticks, lice, fleas and mites and may infect a wide range of vertebrate species. There are still many knowledge gaps concerning the arthropod vectors and amplifying hosts of these pathogens. Reptiles are known to host infected ticks with these zoonotic pathogens and eventually become infected themselves by these bacteria. Hence to address this question from a broad One-Health perspective, we assessed the molecular prevalence of Rickettsia spp., C. burnetii and A. phagocytophilum in reptiles, ticks and mites from both hosts and environment and seroprevalence in humans living or working near the same area. Rickettsia DNA was detected in lizards’ tails, Ixodes ricinus ticks and in Neotrombicula autumnalis mites collected from them and in questing ticks. Although DNA of C. burnetii and A. phagocytophilum was not detected in lizards and their ectoparasites, sera samples of human subjects tested positive for the antibodies against these zoonotic pathogens. These findings indicate the epidemiological role of lizards in spreading SFG rickettsiae as well as I. ricinus, and hence representing a potential public health concern in geographical areas where lizards, ticks and humans share the same environment.
Introduction
Many examples of tick-borne diseases highlight the pivotal role of adoption of a One-Health approach for understanding the ecology of pathogens transmitted by ticks to human and animal populations, living in the same environment [1]. Rickettsioses caused by Rickettsia spp. represent a paradigmatic example for that. Similarly, other intracellular bacteria of public health concern, mainly in the USA and Europe, are Coxiella burnetii causing coxiellosis/ Q fever and Anaplasma phagocytophilum causing human granulocytic anaplasmosis (HGA) [2,3]. These pathogens are associated with arthropod vectors (i.e., ticks, lice, fleas and mites) and may infect a wide range of vertebrate species [4–6]. Pets (i.e., dogs and cats), reptiles, ticks, rodents and birds are known to contribute, at different extent, in the dissemination of these pathogens [3,7]. The epidemiology of rickettsioses, coxiellosis and HGA are intimately related to the corresponding pathogen, arthropod vector, vertebrate host, and the environment where they thrive. While a considerable amount of information on the ecology of these pathogens has been acquired in the last decades [7–10], there are still many knowledge gaps concerning the arthropod vectors and amplifying hosts. In humans, Rickettsia spp. infection causes conditions of various degrees of severity according to different factors such as the bacterial species, the individual susceptibility and the immune status [8,11–13]. Mediterranean spotted fever (MSF) by Rickettsia conorii causes the most prevalent and severe form of rickettsiosis, in Europe. Typical manifestations in human patients are fever, cutaneous maculo-papular rash, and eschar at the site of tick bite accompanied by regional lymphadenopathies. Sometimes, unspecific flu-like symptoms may be the only manifestations, but severe or lethal outcomes may occur if proper diagnosis is not performed and antibiotic therapy is delayed [14,15]. Rickettsioses caused by Rickettsia slovaca and Rickettsia raoultii are responsible for so-called SENLAT (scalp eschar and neck lymphadenopathy after tick bite) syndrome, also known as TIBOLA (tick-borne lymphadenopathy) or DEBONEL (Dermacentor-borne necrosis erythema lymphadenopathy). Other rickettsiae in Europe (e.g., Rickettsia aeschlimannii, Rickettsia helvetica and Rickettsia massiliae) are responsible for less common and, probably, under-reported febrile illnesses. Furthermore, Rickettsia monacensis was reported in Europe as a cause of MSF-like illness in Italy and Spain [16,17]. The gamma-proteobacterium Coxiella burnetii is the causative agent of Q fever, a flu-like disease manifesting from self-limiting non-specific fever to atypical pneumonia, hepatitis, endocarditis and neurological manifestation. HGA causes nonspecific febrile illness, which could lead to a fatal outcome [7,10]. Though, Q fever was primarily considered a regionally restricted zoonotic disease, it has been widely diagnosed in most countries by serological analyses [18].
Most rickettsiae are primarily hosted and transmitted by ticks. Rickettsia conorii is usually transmitted by the brown dog tick (Rhipicephalus sanguineus sensu lato), and Rickettsia slovaca and R. raoultii by Dermacentor spp. [9], although non-specific carriage was also identified for many rickettsial species, especially when different tick species live in sympatry [19]. Coxiella burnetii infections are reported in livestock, domestic and wild mammals, birds and a wide variety of ticks [20]. Although ticks are not considered essential in the natural cycle of this pathogen, it multiplies in the gut cells of tick genera such as Ixodes, Haemaphysalis, Rhipicephalus and Dermacentor and is shed in tick faeces [21,22].
Because many tick-borne rickettsiae are primarily associated to ticks infesting wildlife, rickettsioses, coxiellosis and HGA are often diagnosed in people living or working in the proximities of forested areas (e.g., park rangers, foresters and hunters) and occupational farmers, veterinarians, laboratory technicians, slaughterhouses and cheese factories personnel. For instance, seroprevalence of Rickettsia and Coxiella antibodies may be up to 37% and up to 23.8%, respectively, in this occupational risk group in southern regions of Italy [3,23,24], where tick bites are often reported [25]. In a large survey conducted on human infested by ticks in Italy, I. ricinus was the most frequently retrieved species (i.e., 59.5%) carrying the highest number of pathogens, including Rickettsia spp. [25]. This tick has a catholic feeding behaviour, being found infesting a wide range of hosts, including reptiles and humans [26]. Meanwhile, I. ricinus-associated rickettsiae (e.g., R. helvetica and R. monacensis) have been detected in synanthropic reptiles, especially lacertid lizards [26,27]. Indeed, reptiles are known to act as hosts of ticks carrying Rickettsia spp., C. burnetii, A. phagocytophilum, Borrelia lusitaniae and eventually become infected themselves by these bacteria [7,10,11,26–31,32]. Nonetheless, the significance of reptiles, such as lizards, in the ecology of Rickettsiales and in the epidemiology of human infections is still to be ascertained.
The collection of lizards infested by I. ricinus and mites (Neotrombicula autumnalis) in woody areas of southern Italy [32], along with anecdotic reports of people complaining of MSF-like clinical signs in the same areas stimulated the present investigation. Our main objective was to detect these rickettsial microorganisms in reptiles, their ectoparasites, and free-living ticks from the same environment. To address this question from a broad One Health perspective, the seroprevalence of antibodies against Rickettsia, C. burnetii and A. phagocytophilum was also assessed in humans living or working near the same woody area.
Methods
Ethics statement
The study was conducted in accordance with ethical principles (Declaration of Helsinki), written informed consent was obtained from the participants and the research protocol was approved by the ethics committee of the University Hospital of Bari (n. 6394, prot. n., 0044469–23062020). Protocols for lizard collection and sampling were approved by the Commission for Bioethics and Animal Welfare of the Department of Veterinary Medicine of the University of Bari and authorized by the Ministry for Environment, Land and Sea Protection of Italy (approval number 0016973/2018), the Societas Herpetologica Italica (approval number SHI-aut-ER-12-2018) and the “Istituto Superiore per la Protezione e la Ricerca Ambientale” (approval number 41180).
Study area and sample collection
The study was conducted from 2018 to 2020 in the Basilicata region in southern Italy in the Gallipoli Cognato Forest (site 1, 40°32’17"N, 16°07’20.17"E), which belongs to the Parco Regionale di Gallipoli Cognato e delle Piccole Dolomiti Lucane (27,027 ha in extension), where a great diversity of animals and plants is present. With a vegetation coverage varying according to altitude, this forest of Turkey oak (Quercus cerris) is a known habitat for a plethora of parasites, including ticks [33–35].
All reptiles’ samples (i.e., blood and tail tissue) and ectoparasites were collected under the frame of previous studies [32,33]. The first site (site 1) from where lizards and ticks were collected was a meadow habitat within an enclosure inhabited by roe deer (Capreolus capreolus) (40°32’17”N, 16°07’20.17”E). The collection site was bordered by or within the forest, being selected on authors’ observations of environmental features (e.g., vegetation cover), as well as the experience in previous studies on tick ecology [33,36]. In brief, ticks (n = 250 I. ricinus) were collected from the environment by dragging and flagging as detailed in a previous study [36] and morphologically identified [37,38]. In this location, lizards (n = 128) and snakes (n = 4) were captured and checked for ectoparasites as described elsewhere [32]. In addition, two adult females of I. ricinus and one adult male of Dermacentor marginatus collected from two park rangers were also screened. The second collection site (site 2) was represented by a peri-urban area in the surroundings of the Department of Veterinary Medicine, University of Bari “Aldo Moro” (41°1’31.584"N, 16°54’3.6288"E), in the province of Bari, where lizards (n = 40) were captured and found infested solely by mites [32].
DNA extraction, polymerase chain reaction (PCR) and phylogenetic analyses
Genomic DNA was extracted from ticks and mites using a lysis with guanidine isothiocyanate protocol (GT) [39], and eluted in AE elution buffer (50 μl for mites and ticks). Whilst, DNA from reptile blood (~20 μl) and from tail tissue (25 mg) of lizards was extracted by using a Qiagen Mini kit and Qiagen DNeasy Blood & Tissue kit (Qiagen, Hilden, Germany), respectively.
DNA samples were tested by PCR using a pair of primers (CS-78F and CS-323R) targeting a fragment (401bp) of the gene citrate synthase (gltA), present in all species of Rickettsia [40]. The PCR runs were performed in the Master cycler Gradient (Eppendorf California) thermocycler using the following thermal cycling conditions: 95° C for 5 minutes, followed by 40 cycles of 95° C for 30 seconds, 58° C for 30 seconds and 72° C for 40 seconds and 72° C for 7 minutes. Positive samples were tested by a second PCR using a pair of primers as previously described [41,42] (Rr190.70F and Rr190.701R) targeting a fragment of the outer membrane protein A (ompA) gene (632 bp), present only in spotted fever group (SFG) Rickettsiae. The cycling conditions for the ompA gene were: 95° C for 5 minutes, followed by 35 cycles of 95° C for 40 seconds, 58° C for 30 seconds, 72° C for 45 seconds and 72° C for 10 minutes. Samples were also screened for C. burnetii and for species of the Anaplasmataceae family using primer pairs (CAPI-844-F and CAPI-844-R; EHR16SD and EHR16SR) which amplified a 601 bp fragment of the CAPI gene [43] and 345 bp of 16S rRNA gene [44], respectively. The cycling conditions used for CAPI gene were 95° C for 10 minutes followed by 35 cycles of 95° C for 45 seconds, 60° C for 45 seconds and 72° C for 45 seconds and 72° C for 7 minutes while that of 16S rRNA gene were 95° C for 10 minutes followed by 35 cycles of 95° C for 30 seconds, 60° C for 30 seconds and 72° C for 30 seconds and 72° C for 10 minutes. In all PCR runs negative (Milli-Q water) and positive controls of the respective pathogens were included.
Amplified DNA were subjected to electrophoresis in a 2% agarose gel stained with GelRed (VWR International PBI, Milano, Italy) and viewed on a GelLogic 100 gel documentation system (Kodak, New York, USA). Amplicons were purified using 10 μl of PCR product mixed with 0.5 μl of Escherichia coli exonuclease I (ExoI; MBI, Fermentas, Lithuania), 1 μl of shrimp alkaline phosphatase (SAP) and 0.5 μl of SAP reaction buffer (MBI, Fermentas, Lithuania) to remove unused primers and unincorporated dNTPs. This mix was incubated at 37°C for 20 min, following enzymes inactivation at 85°C for 15 min. PCR purified products were sequenced using the Taq Dye Doxy Terminator Cycle Sequencing Kit (v.2, Applied Biosystems, California, USA) in an automated sequencer (ABI-PRISM 377). Sequences were analysed by Geneious version 11.1.4 software and compared with those available in Genbank database by Basic Local Alignment Search Tool (BLAST) [45].
Rickettsial ompA and gltA as well as 16S rRNA genes from Anaplasma spp. were amplified and the sequences were separately aligned against those closely related species available from GenBank database using the ClustalW application within MEGA6 software [46]. The Akaike Information Criterion (AIC) option in MEGA6 [46] was used to establish the best nucleotide substitution model adapted to each sequence alignment. Tamura 3-parameter model with a discrete Gamma distribution (+G) [47] was used to generate the ompA, gltA and the 16S rRNA trees. A maximum likelihood (ML) phylogenetic inference was used with 1000 bootstrap replicates to generate the phylogenetic tree in MEGA6 [46]. Homologous sequences of Rickettsia were used as outgroup to root the trees, including the gltA sequences from Rickettsia belli and Rickettsia canadensis (JQ664297, AB297809), the ompA sequence of Rickettsia felis (AY727036) and the 16S sequence of Rickettsia parkeri (NR118776).
Human blood collection and serological testing
In February 2020, serum samples (n = 50) were collected from forestry workers and tour guides operating within site 1, and among farmers and livestock breeders employed in the municipalities included in regional park area. All workers were asked to fill a questionnaire providing socio-demographic characteristics, working history, previous exposure to tick bites as well as medical history with special focus on the three months prior to the study. All the participants were fully informed about the research aims and features and were provided with an informed consent to take part, before filling the questionnaire, in accordance with the Helsinki Declaration (WMA 2013). Blood samples (10 ml) were collected in a Vacutainer tube for each participant and transported at 4°C to the laboratory where serum samples were obtained by centrifugation at 3000 × g for 30 min. Serum samples were stored in 2 ml tubes at -20°C until serological analyses were performed.
All human sera were screened for five selected tick-borne bacteria belonging to the Rickettsiales and Legionellales orders using the quantitative indirect immunofluorescence antibody test (IFAT). IFAT is the reference method in diagnosing these infections [18] which have been proven to be 100% sensitive. First, two-fold dilutions (1:50 and 1:100) of sera (including positive and negative sera) were prepared in phosphate buffered saline (PBS), and a dilution of 1:100 was selected as the cut-off value. Briefly, each slide well was sensitized using in-house generated following antigens: R. conorii (strain Malish 7, ATCC VR-613), R. felis (strain Marseille, ATCC VR-1525), and Rickettsia typhi (strain Wilmington), R. helvetica (strain C9P9), phases I and II of C. burnetii (Nine Mile RSA493 strain) and A. phagocytophilum (Webster strain). The antigens were deposited separately as microdroplets all around the periphery of each well following the same order in all slides. In a second step, each human serum was investigated separately for both IgG and IgM. Twenty microliters of each human serum dilution was applied per well and slides were then incubated for 30 min at 37°C. After incubation, slides were washed twice with PBS for 5 minutes and once with distilled water. Twenty microliters of mouse anti-human total immunoglobulin (Ig) conjugated with fluorescein isothiacyanate (FITC) (Sigma-Aldrich, St Louis, MO, USA) were added into each well. Slides were immediately incubated at 37° C for 30 minutes and then washed following the same procedure described above. Positive sera at the cut-off of 1:100 were further investigated for IgG and IgM using a five 2-fold serial dilution 1:200 to 1: 3400.
Results
Of the snakes (n = 4; 2 Elaphe quatuorlineata, 1 Hierophis carbonarius, 1 Natrix natrix) and lizards (n = 128; 5 Lacerta viridis, 15 Podarcis muralis, 106 Podarcis siculus, 2 Tarentola mauritanica) captured in site 1, 94.7% (125/132) were infested with mites and ticks. In particular, 123 (93.2%) (1 E. quatuorlineata, 5 L. viridis, 15 P. muralis, 102 P. siculus) reptiles were infested with I. ricinus (Fig 1) and/or N. autumnalis (Fig 2). Only lizards (n = 40; 1 P. muralis, 29 P. siculus, 10 T. mauritanica) were captured in site 2, with 37 (92.6%) (1 P. muralis, 29 P. siculus, 9 T. mauritanica) of them being infested with mites and, particularly, 10 P. siculus (25%) by N. autumnalis. The mean intensity (5.5, 95% CI: 5.4–6.2%) and abundance (5, 95% CI: 4.45–5.6%) were calculated on a total of 120 reptiles from site 1, which were infested with I. ricinus. Of the 172 reptile samples, Rickettsiales DNA was assessed molecularly from 158 (91.9%) infested with I. ricinus and/or N. autumnalis.
Fig 1. Ixodes ricinus larvae and nymphs in the axillary region of adult Podarcis muralis.
Fig 2. Neotrombicula autumanlis larvae in the ventral region of adult Podarcis siculus.
The Rickettsia gltA gene was amplified from tail tissues of four (i.e., 3.1%; 95% CI: 0.6–5.8%) lizards (i.e., one P. muralis and two P. siculus from site 1; one P. siculus from site 2). Rickettsia gltA gene sequences from specimens from site 1 displayed 100% of nucleotide identity with that of R. monacensis (KU586332), whereas sequence from site 2 was 100% identical to that of R. helvetica (KU310588). None of the four snakes tested positive for Rickettsia spp.
In addition, 87.5% (105/120; 95% CI: 80.2–92.8%) of I. ricinus collected from reptiles were positive for the Rickettsia gltA gene, of which 65.8% (79/120; 95% CI: 56.6–74.3%) also for the Rickettsia ompA gene. Out of 96 N. autumnalis larvae, eight (8.3%; 95% CI: 38.3–56.8%) yielded positive results for the Rickettsia gltA gene and four (4.2%; 95% CI: 1.1–10.3%) for the Rickettsia ompA gene (Table 1). Rickettsia monacensis was the only rickettsial species identified using the ompA gene in both ticks and mites of lacertids.
Table 1. Number and percentage of ectoparasites (Ixodes ricinus and Neotrombicula autumnalis) positive for Rickettsia spp. collected on reptile hosts.
Percentage of sequence identity for gltA and ompA genes with sequences available in GenBank.
| Host (infested/total) |
Hosts infested by ectoparasite species % (infested/total) |
gltA (n positive/total) sequence identity |
ompA (n positive/total) sequence identity |
|---|---|---|---|
| Podarcis siculus (Italian wall lizard) (112/135) |
Ixodes ricinus 88.3 (99/112) |
(64/99) Rickettsia monacensis 100% (KU586332) (24/99) Rickettsia helvetica 100% (KU310588) |
(64/99) Rickettsia monacensis 100% (MK922661) |
| Neotrombicula autumnalis 77.7 (87/112) | (5/87) Rickettsia monacensis 100% (KU586332) | (2/5) Rickettsia monacensis 100% (MK922661) | |
| Podarcis muralis (common wall lizard) (15/16) | Ixodes ricinus 100 (15/15) | (8/15) Rickettsia monacensis100% (KU586332) (3/15) Rickettsia helvetica 100% (KU310588) |
(8/15) Rickettsia monacensis 100% (MF383610) |
| Neotrombicula autumnalis 33.3 (5/15) | (2/15) Rickettsia monacensis 100% (KU586332) | (2/15) Rickettsia monacensis 100% (MK922661) | |
| Lacerta bilineata (western green lizard) (5/5) | Ixodes ricinus 100 (5/5) | (5/5) Rickettsia monacensis 100% (KU586332) | (5/5) Rickettsia monacensis 100% (MK922661) |
| Neotrombicula autumnalis 80 (4/5) | (1/4) Rickettsia monacensis 100% (KU586332) | ||
| Elaphe quatuorlineata (four-lined snake) (1/2) | Ixodes ricinus 100 (1/1) | (1/1) Rickettsia helvetica 100% (KU310588) |
Of the 250 questing I. ricinus collected from the environment, 28.4% (71/250; 95% CI: 25.7–30.1%) yielded positive results for the gltA gene and 8.8% (22/250; 95% CI: 3.4–7.1%) for the ompA gene. Two different Rickettsia species, namely R. helvetica (9/71; only for the gltA gene) and R. monacensis (62/71) were identified with 100% nucleotide identity with GenBank reference sequence KU310588 and MK922661, respectively. Of the three ticks collected from park rangers, two scored positive for Rickettsia ompA gene, with I. ricinus for R. monacensis (100% nucleotide identity with MK922661) and D. marginatus for R. slovaca (100% nucleotide identity with MH532257).
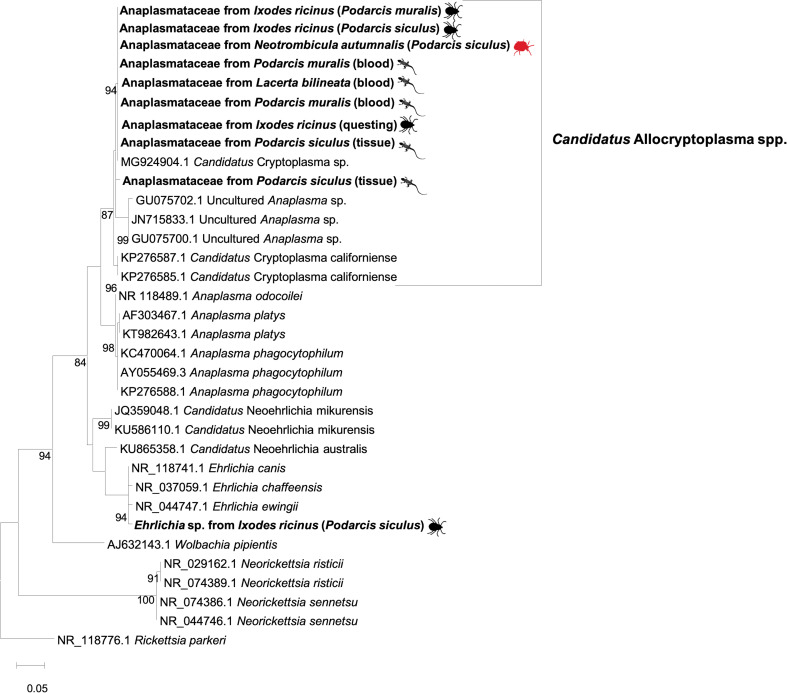
None of the reptiles and ectoparasites scored positive for A. phagocytophilum and for C. burnetii. Yet, an undescribed member of the family Anaplasmataceae, originally designated as Candidatus Cryptoplasma sp. was detected in four lizards (n = 3 blood, n = 1 tail) and in ectoparasites 1 mite and 3 ticks (nucleotide identity ranging from 99.8% to 100% with MG924904; see Discussion). In addition, one tick (from lizard) scored positive for Ehrlichia sp. (99.3% nucleotide identity with E. canis, MN922610) and a lizard to the same undescribed microorganism (99.0% nucleotide identity with MG924904 and GU734325).
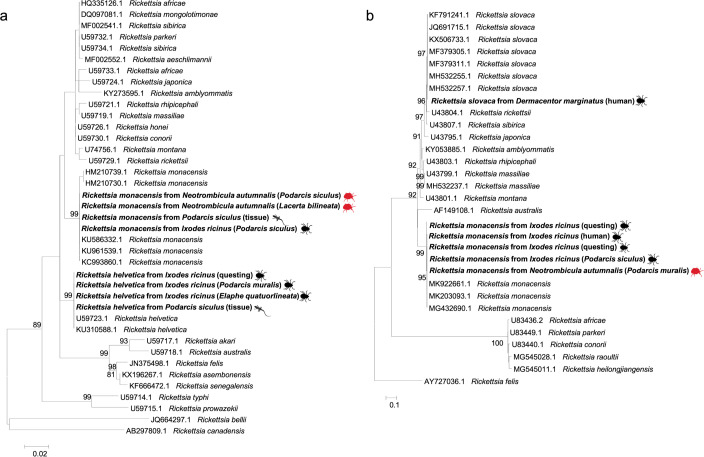
Rickettsia gltA sequences obtained from ticks and reptiles clustered within the same clades of R. monacensis and R. helvetica, respectively, as distinct paraphyletic clades with the exclusion of the other Rickettsia spp. (Fig 3A). Similarly, Rickettsia ompA sequences clustered with R. monacensis and R. slovaca, supported by high bootstrap values (i.e., 93%; Fig 3B). The 16S rRNA gene sequences clustered with those from a group of undescribed organisms belonging to the family Anaplasmataceae, with the exception of a sequence that clustered within the clade of Ehrlichia spp. (Fig 4). Outgroups were consistently resolved as paraphyletic species for both trees. Representative sequences herein generated have been deposited in GenBank under accession numbers from MT829281 to MT829303.
Fig 3.
Maximum-likelihood phylogenetic trees of gltA (A) and ompA (B) genes of Rickettsia spp. Bootstrap values (>70%) are shown near the nodes. Rickettsia belli, Rickettsia canadensis (A) and Rickettsia felis (B) were used as outgroups. Scale bar indicates nucleotide substitution per site. Rickettsia spp. sequenced in this study are in bold. Further details on the origin of samples are in brackets.
Fig 4. Maximum-likelihood phylogenetic tree of 16S rRNA sequences of Anaplasmataceae.
Bootstrap values (>70%) are shown near the nodes. Rickettsia parkeri was used as outgroup. Scale bar indicates nucleotide substitution per site. Anaplasmataceae sequenced in this study are in bold. Further details on the origin of samples are in brackets.
Of the 50 human subjects (Table 2), 18 (36%) were exposed to at least one pathogen of whom four individuals had an IgG titre for more than one pathogen (i.e., 1 for C. burnetii, R. typhi and A. phagocytophilum; 1 for R. felis and A. phagocytophilum; 2 for C. burnetii and A. phagocytophilum). The remaining 14 patients showed IgG against A. phagocytophilum (n = 7), C. burnetii (n = 5), R. felis (n = 1) and R. conorii (n = 1). Of the 50 human serum samples, four had IgG titres against Rickettsia spp.: two to R. felis (titres 1:100 and 1:200), one to R. conorii (1:100) and another to R. typhi (1:400). The last serum also was found reactive when tested with R. helvetica antigen with, however, lower titre (1:100). Eleven sera contained antibodies against A. phagocytophilum (titres 1:100 to 1:800). No patients had IgM that exclude acute or recent infection. Eight sera reacted with C. burnetii antigens (titres 1:200 to 1:6400). No IgM was detected which excluded acute Q fever. However, two patients showed high antibody titres against Phase I of C. burnetii (one of 1:1600 and another of 1:6400), with >98% of predictive value suggestive of chronic Q fever.
Table 2. Anamnestic data on studied human population (age, sex, profession, tick exposure, location).
| General Characteristics | Exposed workers | ||
|---|---|---|---|
| Male (n = 41) N (%) Median Range | Female (n = 9) N (%) Median Range | Total (n = 50) N (%) Median Range | |
| Age | 40.7 21.4–69.3 | 33.5 22.7–59.7 | 39.2 21.4–69.3 |
|
Job Tour guide Animal breeder Farmer Forestry workers Farmer/Animal breeder Veterinary surgeon |
4 (9.8) 6 (14.6) 1 (2.4) 10 (24.4) 18 (43.9) 2 (4.9) |
1 (11.1) 0 (0) 1 (11.1) 5 (55.6) 2 (22.2) 0 (0) |
5 (10) 6 (12) 2 (4) 15 (30) 20 (40) 2 (4) |
|
Frequency tick bites Never Rarely Occasionally Frequently |
2 (4.9) 9 (22) 11 (26.8) 19 (46.3) |
1 (11.1) 4 (44.4) 3 (33.3) 1 (11.1) |
3 (6) 14 (28) 14 (28) 19 (38) |
|
Latest tick bite Never < 7 days < 1 month < 1 year < 5 years |
2 (4.9) 4 (9.8) 3 (7.3) 20 (48.8) 12 (29.3) |
1 (11.1) 0 (0) 2 (22.2) 6 (66.7) 0 (0) |
3 (7.3) 4 (9.8) 5 (10) 26 (43.6) 12 (29.3) |
|
Municipalities Accettura Campomaggiore Pietrapertosa Oliveto Lucano San Mauro Forte Tricarico Laurenzana Castelmezzano |
11 (26.8) 5 (12.2) 4 (9.8) 5 (12.2) 5 (12.2) 7 (17) 2 (4.9) 2 (4.9) |
1 (11.1) 1 (11.1) 1 (11.1) 0 (0) 2 (22.2) 2 (22.2) 1 (11.1) 1 (11.1) |
12 (24) 6 (12) 5 (10) 5 (10) 7 (14) 9 (18) 3 (6) 3 (6) |
Discussion
Results obtained in this study suggest that at least two tick-associated Rickettsia spp. (R. helvetica and R. monacensis) circulate in a lizard population from southern Italy (site 1) as well as in ectoparasites collected on them (i.e., I. ricinus and N. autumnalis) and in questing ticks collected from the same area. The overall picture of pathogen circulation in that area is also confirmed by the seroprevalence recorded in humans with a previous history of tick bites, as well as by the molecular detection of Rickettsia spp. in ticks collected from humans coming from the same location. Though other animal species (e.g., mice) may also act as hosts of Rickettsia spp. in this area, the prevalence of R. helvetica and R. monacensis in lizards (i.e., 3.1%) and in ticks collected on them (i.e., 87.5%) suggest that these reptiles could be acting as amplifying hosts for these bacteria. Indeed, this is also supported by the detection of rickettsiae in their blood. Present findings agree with other studies in which R. helvetica was detected in P. muralis tissue (6.2%; 1/16) from the northern Apennine area of Italy [26], and R. monacensis in 6.6% (10/151) Teira dugesii (Madeiran wall lizard) lizards’ tails in Portugal [27]. Since most ectoparasites attach and feed around the axillary region of lizards [31], the detection of R. monacensis and R. helvetica from the tail tissue may indicate a disseminated infection [26,27]. Low prevalence of Rickettsia spp. in reptiles could be explained by the usually short (i.e., for a few days or weeks), transient rickettsiemia in most vertebrates [48]. Like other small vertebrates, lizards are suitable hosts for immature stages of I. ricinus ticks across Europe [26,49,50] as recorded in L. agilis, P. muralis, and Lacerta viridis that contribute to the maintenance of I. ricinus populations in urban settings [51,52]. Therefore, other species of lizards could potentially act as amplifying hosts for Rickettsia spp. Accordingly, based on the retrieval of R. helvetica from ticks collected on a snake (E. quatuorlineata), the role of ophidian hosts deserves further investigations in order to confirm previous reports of Rickettsia spp. DNA in ticks collected from snakes [11]. Conversely, many wild (e.g., wild boars, sika deer, hedgehogs, wild rabbits, opossums, bats, rodents, bandicoots and shrews) and domestic (e.g., cattle, dogs, goat, sheep) mammals could also act as hosts and contribute to the dispersion of Rickettsia-infected ticks in different geographical areas [9,53–57]. This is corroborated by the reports of R. helvetica DNA in whole blood from mice, roe deer and wild boar [58], which also are animal species present in the studied area. In above-mentioned cases, the amplifying host status of these vertebrates for Rickettsia spp. needs confirmatory evidence, such as their natural susceptibility (e.g., antibody detection, Rickettsia isolation in culture) and transmissibility of these infectious agents to suitable vectors (i.e., xenodiagnosis) [59].
Under these circumstances, the occurrence of co-feeding of both infected and uninfected ticks could facilitate the circulation of Rickettsia spp., such as demonstrated for R. helvetica transmission in birds to feeding and co-feeding I. ricinus [60]. The detection of R. helvetica and R. monacensis in I. ricinus (free living, from reptiles and from humans), along with the high abundance of this tick in the study area [36], provides a strong circumstantial evidence of its involvement in the transmission of these rickettsiae in this part of Europe. The occurrence of Rickettsia spp. in the study area was initially confirmed in ticks collected from humans, with prevalence up to 17% [25]. However, data on tick-borne rickettsiosis in southern Italy is scarce. Indeed, although spotted fever rickettsiosis is a mandatory notifiable disease in Italy since 1990, its incidence is still unknown due to the hindrances in a specific clinical and serological diagnosis [15].
Considering that larval stages of N. autumnalis parasitize reptiles, birds and humans [61], the retrieval of Rickettsia spp. in these mites suggests the possibility of the transmission pathways between reptiles and humans. The role of chigger mites as a potential vector of Borrelia burgdorferi sensu lato has been previously hypothesized [61]. Our data is of ecological interest considering that only N. autumnalis mites were collected on lizards in site 2, where Rickettsia spp. were detected in mites and in one lizard. This raises the question whether this could represent a potential threat for human health, even in absence of I. ricinus. In any case, considering the biology of N. autumnalis, further study about the transstadial and transovarial transmission of Rickettsia spp. in this mite are needed to draw further conclusions on this matter.
Overall, R. monacensis was the most prevalent species among all screened samples, which is in line with previous studies conducted in Tuscany [62] and Emilia Romagna, Italy [63]. This species, along with other rickettsiae (e.g. R. massiliae, R. aeschlimannii and Rickettsia sibirica mongolitimonae), are considered as emerging human pathogens [64,65]. Accordingly, serological analysis of patients with a history of tick bites revealed antibody titres against Rickettsia spp. confirming the risk of human exposure in the study area.
The phylogenetic analyses of the sequences of R. helvetica and R. monacensis obtained from reptiles, ticks and mites parasitizing them as well as ticks collected on two individuals and questing ticks, revealed the clustering of these Rickettsia spp. with that from humans available in GenBank. The high similarity of Rickettsia spp. among all the samples indicates the circulation of two sequence types in the studied area, which ultimately gives a hint about the possible role of these crawling creatures for human rickettsial infection. Regardless the possible role of N. autumnalis in the ecology of Rickettsia spp., public awareness about the risk of mite and tick bites is advocated.
Negative results of PCR from reptiles and their ectoparasites for C. burnetii and A. phagocytophilum could be due to the more predominant role of the above-mentioned mammalian vertebrate hosts in the ecology and maintenance of these bacteria [66] than that played by reptiles [67]. For instance, rodents have been recorded as feasible reservoirs for C. burnetii/Q fever in central Italy [68], as well as ruminants (e.g., cattle, sheep, buffaloes) throughout the country [69]. Whereas, birds and mammals have been indicated as main reservoirs for A. phagocytophilum [70]. The high seroprevalence against A. phagocytophilum (22%, 11/55) indicates a frequent contact of high-risk group local population with this bacterium, as well as, high seroprevalence for Q fever, with at least two chronic cases.
Finally, the detection of an undescribed member of the Anaplasmataceae in lizards agrees with previous reports from Europe (Slovakia) [71] and USA [72]. This microorganism is related to genus Anaplasma, but represents a lineage distinct from all known Anaplasma spp. The putative genus “Cryptoplasma” was informally created to accommodate a microorganism originally designated as “Candidatus Cryptoplasma californiense” [72], but recently this genus was corrected to “Allocryptoplasma” [73]. Still, this genus has not been validly published as yet (as of 27 July 2020). Our results shed new light on the reptile-tick-Anaplasmataceae interactions in Italy and suggest that lizards of the genus Podarcis could act as primary hosts for the maintenance and enzootic circulation of undescribed organisms of unknown pathogenicity and zoonotic potential. In the same way, along with a previous study [11], our data suggest that the diversity of ehrlichial microorganisms infecting reptiles is presently underestimated.
In conclusion, data presented suggest that lizards (i.e., P. muralis and P. siculus) may play a role in the spreading of SFG rickettsiae and that I. ricinus is involved in the transmission of these pathogens in southern Europe. Remarkably, lizards could act as amplifying hosts and N. autumnalis could be involved in the enzootic cycle of some SFG rickettsiae among these animals. Being I. ricinus able to parasitize humans, it may represent a potential public health concern in geographical areas where lizards, ticks and humans live in sympatry. Results herein presented advocate for a One-Health approach to assess the interactions between hosts (including humans), ectoparasites, pathogens and the environment they inhabit, that will aid efficient public health policies in specific epidemiological contexts.
Acknowledgments
The authors are grateful to Egidio Mallia veterinary responsible of the Parco Regionale di Gallipoli Cognato e Piccole Dolomiti Lucane in Basilicata and the park rangers/workers and farmers for their support in the sampling procedures and their participation in this study. Authors would also like to thank Marcelo Molento for his collaborative efforts during sampling collection.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Dantas-Torres F, Chomel BB, Otranto D. Ticks and tick-borne diseases: a One Health perspective. Trends Parasitol. 2012;28: 437–446. 10.1016/j.pt.2012.07.003 [DOI] [PubMed] [Google Scholar]
- 2.de la Fuente J, Torina A, Naranjo V, Caracappa S, Di Marco V, Alongi A, et al. Infection with Anaplasma phagocytophilum in a seronegative patient in Sicily, Italy: case report. Ann Clin Microb Anti. 2005;4: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fenga C, Gangemi S, De Luca A, Calimeri S, Lo Giudice D, Pugliese M, et al. Seroprevalence and occupational risk survey for Coxiella burnetii among exposed workers in Sicily, Southern Italy. Int J Occup Environ Health. 2015;28: 901 10.13075/ijomeh.1896.00448 [DOI] [PubMed] [Google Scholar]
- 4.Olano JP. Rickettsial infections. Ann NY Acad Sci. 2005;1063: 187–196. 10.1196/annals.1355.031 [DOI] [PubMed] [Google Scholar]
- 5.Raoult D, Fournier PE, Eremeeva M, Graves S, Kelly PJ, Oteo JA, et al. Naming of rickettsiae and rickettsial diseases. Ann NY Acad Sci. 2005;1063: 1–2. 10.1196/annals.1355.002 [DOI] [PubMed] [Google Scholar]
- 6.Sahni SK, Rydkina E. Host-cell interactions with pathogenic Rickettsia species. Future Med. 2009;4: 323–339. 10.2217/fmb.09.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin H, Wei F, Liu Q, Qian J. Epidemiology and control of human granulocytic anaplasmosis: a systematic review. Vector-Borne Zoonot Dis. 2012;12: 269–274. 10.1089/vbz.2011.0753 [DOI] [PubMed] [Google Scholar]
- 8.Parola P, Paddock CD, Raoult D. Tick-borne rickettsioses around the world: emerging diseases challenging old concepts. Clin Microbiol Rev. 2005;18: 719–756. 10.1128/CMR.18.4.719-756.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parola P, Paddock CD, Socolovschi C, Labruna MB, Mediannikov O, Kernif T, et al. Update on tick-borne rickettsioses around the world: a geographic approach. Clin Microbiol Rev. 2013;26: 657–702. 10.1128/CMR.00032-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.González-Barrio D, Jado I, Fernández-de-Mera IG, del Rocio Fernández-Santos M, Rodríguez-Vargas M, García-Amil C, et al. Genotypes of Coxiella burnetii in wildlife: disentangling the molecular epidemiology of a multi-host pathogen. Environ Microbiol Rep. 2016;8: 708–714. 10.1111/1758-2229.12431 [DOI] [PubMed] [Google Scholar]
- 11.Andoh M, Sakata A, Takano A, Kawabata H, Fujita H, Une Y, et al. Detection of Rickettsia and Ehrlichia spp. in ticks associated with exotic reptiles and amphibians imported into Japan. PLoS One. 2015;10: e0133700 10.1371/journal.pone.0133700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Novakova M, Bulkova A, Costa FB, Kristin A, Krist M, Krause F, et al. Molecular characterization of ‘Candidatus Rickettsia vini’ in Ixodes arboricola from the Czech Republic and Slovakia. Ticks Tick Borne Dis. 2015;6: 330–333. 10.1016/j.ttbdis.2015.02.006 [DOI] [PubMed] [Google Scholar]
- 13.Sánchez-Montes S, Isaak-Delgado AB, Guzmán-Cornejo C, Rendón-Franco E, Muñoz-García CI, Bermúdez S, et al. Rickettsia species in ticks that parasitize amphibians and reptiles: Novel report from Mexico and review of the worldwide record. Ticks Tick Borne Dis. 2019;10: 987–994. 10.1016/j.ttbdis.2019.04.013 [DOI] [PubMed] [Google Scholar]
- 14.Raoult D, Roux V. Rickettsioses as paradigms of new or emerging infectious diseases. Clin Microbiol Rev. 1997;10: 694–719. 10.1128/CMR.10.4.694-719.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gomez-Barroso D, Vescio MF, Bella A, Ciervo A, Busani L, Rizzo C, et al. Mediterranean spotted fever rickettsiosis in Italy, 2001–2015: Spatio-temporal distribution based on hospitalization records. Ticks Tick Borne Dis. 2019;10: 43–50. 10.1016/j.ttbdis.2018.09.001 [DOI] [PubMed] [Google Scholar]
- 16.Jado I, Oteo JA, Aldámiz M, Gil H, Escudero R, Ibarra V, et al. Rickettsia monacensis and human disease, Spain. Emerg Infect Dis. 2007;13: 1405–1407. 10.3201/eid1309.060186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madeddu G, Mancini F, Caddeo A, Ciervo A, Babudieri S, Maida I, et al. Rickettsia monacensis as Cause of Mediterranean Spotted Fever–like Illness, Italy. Emerg Infect Dis. 2012;18(4): 702–704. 10.3201/eid1804.111583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eldin C, Mélenotte C, Mediannikov O, Ghigo E, Million M, Edouard S, et al. From Q Fever to Coxiella burnetii Infection: a Paradigm Change. Clin Microbiol Rev. 2017;30:115–90. 10.1128/CMR.00045-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dantas-Torres F, Otranto D. Further thoughts on the taxonomy and vector role of Rhipicephalus sanguineus group ticks. Vet Parasitol. 2015;208: 9–13. 10.1016/j.vetpar.2014.12.014 [DOI] [PubMed] [Google Scholar]
- 20.Walker DH. Rickettsiae. Medical Microbiology. 4th ed. Edited by Baron S. Galveston (TX); 1996.
- 21.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12: 518–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fard SN, Khalili M. PCR-detection of Coxiella burnetii in ticks collected from sheep and goats in Southeast Iran. Iranian journal of arthropod-borne diseases. 2011;5: 1–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Livio M, Mobilia A, Abbate S, Saffioti G, Nicolosi L, Isaia S, et al. Ticks bite in foresters. G Ital Med Lav Ergon. 2007;29: 811–812. [PubMed] [Google Scholar]
- 24.Mancini F, Ciccozzi M, Lo Presti A, Cella E, Giovanetti M, Di Luca M, et al. Characterization of spotted fever group Rickettsiae in ticks from a city park of Rome, Italy. Ann Ist Super Sanità. 2015;51: 284–290. 10.4415/ANN_15_04_07 [DOI] [PubMed] [Google Scholar]
- 25.Otranto D, Dantas-Torres F, Giannelli A, Latrofa MS, Cascio A, Cazzin S, et al. Ticks infesting humans in Italy and associated pathogens. Parasit Vectors. 2014;7: 328 10.1186/1756-3305-7-328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tomassone L, Ceballos LA, Ragagli C, Martello E, De Sousa R, Stella MC, et al. Importance of common wall lizards in the transmission dynamics of tick-borne pathogens in the northern Apennine Mountains, Italy. Microb Ecol. 2017;74: 961–968. 10.1007/s00248-017-0994-y [DOI] [PubMed] [Google Scholar]
- 27.De Sousa R, Lopes de Carvalho I, Santos AS, Bernardes C, Milhano N, Jesus J, et al. Role of the lizard Teira dugesii as a potential host for Ixodes ricinus tick-borne pathogens. Appl Environ Microbiol. 2012;78: 3767–3769. 10.1128/AEM.07945-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Václav R, Ficová M, Prokop P, Betáková T. Associations between coinfection prevalence of Borrelia lusitaniae, Anaplasma sp., and Rickettsia sp. in hard ticks feeding on reptile hosts. Microb Ecol. 2011;61: 245–253. 10.1007/s00248-010-9736-0 [DOI] [PubMed] [Google Scholar]
- 29.Kubelová M, Papoušek I, Blohlávek T, Goüy de Bellocq J, Baird SJE, Široký P. Spotted fever group rickettsiae detected in immature stages of ticks parasitizing on Iberian endemic lizard Lacerta schreiberi Bedriaga, 1878. Ticks Tick Borne Dis. 2015;6: 711–714. 10.1016/j.ttbdis.2015.06.003 [DOI] [PubMed] [Google Scholar]
- 30.Ehlers J, Ganzhorn JU, Silaghi C, Krüger A, Pothmann D, Ratovonamana RY, et al. Tick (Amblyomma chabaudi) infestation of endemic tortoises in southwest Madagascar and investigation of tick-borne pathogens. Ticks Tick Borne Dis. 2016;7: 378–383. 10.1016/j.ttbdis.2015.12.011 [DOI] [PubMed] [Google Scholar]
- 31.Mendoza-Roldan J, Modry D, Otranto D. Zoonotic parasites of reptiles: a crawling threat. Trends in Parasitol. 2020;36(8): 677–687. 10.1016/j.pt.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mendoza-Roldan JA, Colella V, Lia RP, Nguyen VL, Barros-Battesti DM, Iatta R, et al. Borrelia burgdorferi (sensu lato) in ectoparasites and reptiles in southern Italy. Parasit Vectors. 2019;12: 35 10.1186/s13071-019-3286-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dantas-Torres F, Testini G, Di Geronimo PM, Lorusso V, Mallia E, Otranto D. Ticks infesting the endangered Italian hare (Lepus corsicanus) and their habitat in an ecological park in southern Italy. Exp Appl Acarol. 2011;53: 95–102. 10.1007/s10493-010-9387-3 [DOI] [PubMed] [Google Scholar]
- 34.Lorusso V, Lia RP, Dantas-Torres F, Mallia E, Ravagnan S, Capelli G, et al. Ixodid ticks of road-killed wildlife species in southern Italy: new tick-host associations and locality records. Exp Appl Acarol. 2011; 55: 293–300. 10.1007/s10493-011-9470-4 [DOI] [PubMed] [Google Scholar]
- 35.Falchi A, Dantas-Torres F, Lorusso V, Malia E, Lia RP, Otranto D. Autochthonous and migratory birds as a dispersion source for Ixodes ricinus in southern Italy. Exp Appl Acarol. 2012;58: 167–74. 10.1007/s10493-012-9571-8 [DOI] [PubMed] [Google Scholar]
- 36.Dantas-Torres F, Otranto D. Seasonal dynamics of Ixodes ricinus on ground level and higher vegetation in a preserved wooded area in southern Europe. Vet Parasitol. 2013;192:253–8. 10.1016/j.vetpar.2012.09.034 [DOI] [PubMed] [Google Scholar]
- 37.Manilla G. Fauna of Italy, Acari Ixodida. Edited by Bologna Calderini (Italy);1998. [Google Scholar]
- 38.Estrada-Peña A, Bouattour A, Camicas JL, Walker AR. Ticks of domestic animals in the Mediterranean region: a guide to identification of species. Zaragoza (Spain): University of Zaragoza;2004. [Google Scholar]
- 39.Chomkzynski P. A reagent for the single-step simultaneous isolation of RNA, DNA and proteins from cell and tissue samples. Biotechniques. 1993;15: 532–537. [PubMed] [Google Scholar]
- 40.Labruna MB, Whitworth T, Horta MC, Bouyer DH, McBride JW, Pinter A, et al. Rickettsia species infecting Amblyomma cooperi ticks from an area in the state of Sao Paulo, Brazil, where Brazilian spotted fever is endemic. J ClinMicrobiol. 2004;42: 90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Regnery RL, Spruill CL, Plikaytis BD. Genotypic identification of rickettsiae and estimation of intraspecies sequence divergence for portions of two rickettsial genes. J Bacteriol. 1991;173: 1576–1589. 10.1128/jb.173.5.1576-1589.1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pacheco RC, Horta MC, Moraes-Filho J, Ataliba AC, Pinter A, Labruna MB. Rickettsial infection in capybaras (Hydrochoerus hydrochaeris) from São Paulo, Brazil: serological evidence for infection by Rickettsia bellii and Rickettsia parkeri. Biomedica. 2007;27: 364–371. [PubMed] [Google Scholar]
- 43.Reeves WK, Lofits AD, Sanders F, Spinks MD, Wills W, Denison AM, et al. Borrelia, Coxiella and Rickettsia in Cario capensis (Acari: Argasidae) from a brown pelican (Pelecanus accidentalis) rookery in South Carolina, USA. Exp Appl Acarol. 2006;39: 321–32 9. 10.1007/s10493-006-9012-7 [DOI] [PubMed] [Google Scholar]
- 44.Martin AR, Brown GK, Dunstan RH, Roberts TK. Anaplasma platys an improved PCR for the detection in dogs. Exp Parasitol. 2005;109: 176–180. 10.1016/j.exppara.2004.11.007 [DOI] [PubMed] [Google Scholar]
- 45.Altschul SF, Gish W, Miller W, Myers EW, Lipman DJ. Basic local alignment search tool. J Mol Biol. 1990;215: 403–410. 10.1016/S0022-2836(05)80360-2 [DOI] [PubMed] [Google Scholar]
- 46.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013;30: 2725–2729. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tamura K. Estimation of the number of nucleotide substitutions when there are strong transition-transversion and G + C-content biases. Mol Biol Evol. 1992;9: 678–687. [DOI] [PubMed] [Google Scholar]
- 48.Levin ML, Snellgrove AN, Zemtsova GE. Comparative value of blood and skin samples for diagnosis of spotted fever group rickettsial infection in model animals. Ticks Tick Borne Dis. 2016;7: 1029–1034. 10.1016/j.ttbdis.2016.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bauwens D, Strijbosch H, Stumpel AH. The lizards Lacerta agilis and L. vivipara as hosts to larvae and nymphs of the tick Ixodes ricinus. Ecography. 1983;6: 32–40. [Google Scholar]
- 50.Tijsse-Klasen E, Fonville M, Reimerink JH, Spitzen-van der Sluijs A, Sprong H. Role of sand lizards in the ecology of Lyme and other tick-borne diseases in the Netherlands. Parasit Vectors. 2010;3: 42 10.1186/1756-3305-3-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Földvári G, Rigo K, Majlathova V, Majlath I, Farkas R, Pet’Ko B. Detection of Borrelia burgdorferi sensu lato in lizards and their ticks from Hungary. Vector Borne Zoonotic Dis. 2009;9: 331–336. 10.1089/vbz.2009.0021 [DOI] [PubMed] [Google Scholar]
- 52.Rizzoli A, Silaghi C, Obiegala A, Rudolf I, Hubálek Z, Földvári G, et al. Ixodes ricinus and its transmitted pathogens in urban and peri-urban areas in Europe: new hazards and relevance for public health. Front Public Health. 2014;2: 251 10.3389/fpubh.2014.00251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tabuchi M, Jilintai Sakata Y, Miyazaki N, Inokuma H. Serological survey of Rickettsia japonica infection in Dogs and Cats in Japan. Clin. Vaccine Immunol. 2007;14: 1526–1528. 10.1128/CVI.00333-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.D’Auria SR, Camargo MC, Pacheco RC, Savani ES, Dias MA, da Rosa AR, et al. Serologic Survey for Rickettsiosis in Bats from Sao Paulo City, Brazil. Vector Borne Zoonotic Dis. 2010;10: 459–463. 10.1089/vbz.2009.0070 [DOI] [PubMed] [Google Scholar]
- 55.Ortuno A, Pons I, Quesada M, Lario S, Anton E, Gil A, et al. Evaluation of the presence of Rickettsia slovaca infection in domestic ruminants in Catalonia, Northeastern Spain. Vector Borne Zoonotic Dis. 2012;12: 1019–1022. 10.1089/vbz.2012.0972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Milagres BS, Paditha AF, Montandon CE, Freitas RN, Pacheco R, Walker DH, et al. Spotted fever group rickettsia in small rodents from areas of low endemiciy for Brazilian spotted fever in the Eastern Region of Minas Gerais State, Brazil. Am J Trop Med Hyg. 2013;88: 937–939. 10.4269/ajtmh.12-0609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hornok S, Földvári G, Rigó K, Meli ML, Gönczi E, Répási A, et al. Synanthropic rodents and their ectoparasites as carriers of a novel haemoplasma and vector-borne, zoonotic pathogens indoors. Parasit Vectors 2015;15: 8–27. 10.1186/s13071-014-0630-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sprong H, Wielinga PR, Fonville M, Reusken C, Brandenburg AH, Borgsteede F, et al. Ixodes ricinus ticks are reservoir hosts for Rickettsia helvetica and potentially carry flea-borne Rickettsia species. Parasit Vectors. 2009;2: 41 10.1186/1756-3305-2-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tomassone L, Portillo A, Nováková M, De Sousa R, Oteo JA. Neglected aspects of tick-borne rickettsioses. Parasit Vectors. 2018;11: 263 10.1186/s13071-018-2856-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Heylen D, Fonville M, van Leeuwen AD, Sprong H. Co-infections and transmission dynamics in a tick-borne bacterium community exposed to songbirds. Env Microbiol. 2016;18: 988–996. [DOI] [PubMed] [Google Scholar]
- 61.Kampen H, Schöler A, Metzen M, Oehme R, Hartelt K, Kimmig P, et al. Neotrombicula autumnalis (Acari, Trombiculidae) as a vector for Borrelia burgdorferi sensu lato? Exp Appl Acarol. 2004;33: 93–102. 10.1023/b:appa.0000029975.92510.90 [DOI] [PubMed] [Google Scholar]
- 62.Scarpulla M, Barlozzari G, Marcario A, Salvato L, Blanda V, De Liberato C., et al. Molecular detection and characterization of spotted fever group rickettsiae in ticks from Central Italy. Ticks Tick Borne Dis. 2016;7: 1052–1056. 10.1016/j.ttbdis.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 63.Maioli G, Pistone D, Bonilauri P, Pajoro M, Barbieri I, Mulatti P, et al. Etiological agents of rickettsiosis and anaplasmosis in ticks collected in Emilia-Romagna region (Italy) during 2008 and 2009. Exp Appl Acarol. 2012;57: 199–208. 10.1007/s10493-012-9535-z [DOI] [PubMed] [Google Scholar]
- 64.Otranto D, Dantas-Torres F. Canine and feline vector-borne diseases in Italy: current situation and perspectives. Parasit Vectors. 2010;3: 2 10.1186/1756-3305-3-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kernif T, Leulmi H, Raoult D, Parola P. Emerging Tick Borne Bacterial Pathogens. Microbiol Spectr. 2016;4: EI10-0012–2016. 10.1128/microbiolspec.EI10-0012-2016 [DOI] [PubMed] [Google Scholar]
- 66.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12(4): 518–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nieto NC, Foley JE, Bettaso J, Lane RS. Reptile infection with Anaplasma phagocytophilum, the causative agent of granulocytic anaplasmosis. J Parasitol. 2009;95:1165–1170. 10.1645/GE-1983.1 [DOI] [PubMed] [Google Scholar]
- 68.Pascucci I, Di Domenico M, Dall’Acqua F, Sozio G, Camma C. Detection of Lyme disease and Q fever agents in wild rodents in central Italy. Vector Borne Zoonotic Dis. 2015;7: 404–411. 10.1089/vbz.2015.1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barlozzari G, Sala M, Iacoponi F, Volpi C, Polinori N, Rombolà P, Scarpulla M. Cross-sectional serosurvey of Coxiella burnetii in healthy cattle and sheep from extensive grazing system in central Italy. Epidemiol Infect.2020;148 10.1017/S0950268819002115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jaarsma RI, Sprong H, Takumi K, Kazimirova M, Silaghi C, Mysterud A, et al. Anaplasma phagocytophilum evolves in geographical and biotic niches of vertebrates and ticks. Parasit Vectors. 2019;1: 2019328 10.1186/s13071-019-3583-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kočíková B, Majláth I, Víchová B, Maliničová L, Pristaš P, Connors VA, et al. Candidatus Cryptoplasma Associated with Green Lizards and Ixodes ricinus Ticks, Slovakia, 2004–2011. Emerg Infect Dis. 2018;24: 2348–2351. 10.3201/eid2412.161958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Eshoo MW, Carolan HE, Massire C, Chou DM, Crowder CD, Rounds MA, et al. Survey of Ixodes pacificus ticks in California reveals a diversity of microorganisms and a novel and widespread Anaplasmataceae species. PLoS ONE. 2015;9: 0135828 10.1371/journal.pone.0135828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Oren A, Garrity GM, Parker CT, Chuvochina M, Trujillo ME. Lists of names of prokaryotic Candidatus taxa. Int J Syst Evol Microbiol. 2020;70(7): 3956–4042. 10.1099/ijsem.0.003789 [DOI] [PubMed] [Google Scholar]