Abstract
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has reached pandemic proportions with negative impacts on global health, the world economy and human society. The clinical picture of COVID-19, and the fact that Angiotensin converting enzyme 2 (ACE2) is a receptor of SARS-CoV-2, suggests that SARS-CoV-2 infection induces an imbalance in the renin–angiotensin system (RAS). We review clinical strategies that are attempting to rebalance the RAS in COVID-19 patients by using ACE inhibitors, angiotensin receptor blockers, or agonists of angiotensin-II receptor type 2 or Mas receptor (MasR). We also propose that the new MasR activator BIO101, a pharmaceutical grade formulation of 20-hydroxyecdysone that has anti-inflammatory, anti-fibrotic and cardioprotective properties, could restore RAS balance and improve the health of COVID-19 patients who have severe pneumonia.
Teaser
By rebalancing the renin–angiotensin system (RAS), BIO101 (20-hydroxyecdysone) could improve cardio-respiratory functions, limit the requirement for mechanical ventilation and reduce mortality in severely ill COVID-19 patients who are infected by SARS-CoV-2.
Introduction
The outbreak of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first detected in Wuhan, China in December 2019 [1]. The vast majority (around 80%) of patients infected with SARS-CoV-2 are asymptomatic or display only mild illness. Nevertheless, the approximately 20% of patients who have more severe COVID-19 illness may require hospitalization, sometimes in an intensive care unit (ICU). COVID-19 mortality occurs mainly in elderly patients and/or in patients with underlying comorbidities such as hypertension, cardiovascular diseases or diabetes at an estimated rate of between 26% and 62% [2]. Severe COVID-19 illness and fatal outcomes are associated with acute respiratory disease syndrome (ARDS), myocardial injury, cardiac dysfunction, arrhythmias and renal alterations [3]. Excessive expression of inflammatory cytokines and mediators (cytokine storm) also contribute to lung dysfunction and shock in COVID-19 patients [4]. As SARS-CoV-2 is transmitted between humans aerially and because only a limited fraction of the world population has been infected to date, the numbers of COVID-19-positive cases and associated deaths are expected to increase in the months and even years to come. Unfortunately, despite intensive research efforts, we are still lacking effective treatment modalities that can substantially reduce mortality in patients suffering from severe forms of COVID-19. Therapeutic alternatives that can be used to treat this devastating disease are thus urgently required. Here, we review clinical attempts to restore the balance of the renin-angiotensin system (RAS), which is altered following SARS-CoV-2 infection.
SARS-CoV-2 and the renin–angiotensin system
SARS-CoV-2 infects human cells through the cellular receptor angiotensin-converting enzyme 2 (ACE2), a key element of the RAS 4, 5. ACE2 is expressed to varying degrees in nearly all human organs, but the preeminent infection of the lungs by SARS-CoV2 is closely related to the propagation of the virus via aerosols and to the high levels of ACE2 expression in airway epithelial cells, endothelial cells and alveolar epithelial type II cells 4, 6. Moreover, ACE2 expression in the brain, gut, heart, or kidney can also explain both the broad tissue tropism of SARS-CoV-2 and the variety of clinical manifestations observed in COVID-19 patients [7].
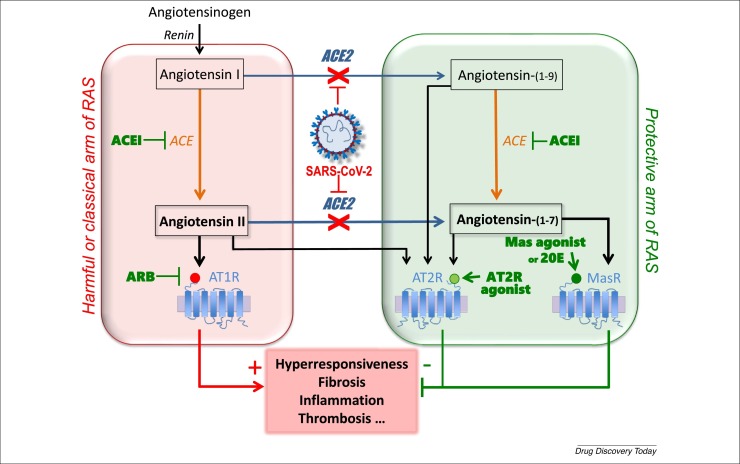
Angiotensin-I (Ang-I) is converted into Angiotensin-II (Ang-II) by ACE. The ACE/Ang-II/Ang-II receptor type 1 (AT1R) axis is usually referred to as the ‘harmful’ or classical arm of the RAS. Ang-II binds a second receptor (AT2R), the effects of which mainly oppose those of AT1R. AT2R is part of the ‘protective’ arm of the RAS and can also be activated by Angiotensin-(1–9) and Angiotensin-(1–7), which are formed by ACE2 from Ang-I and Ang-II, respectively. Although AT2R has been demonstrated to be upregulated under pathological conditions and to counteract the effects of AT1R (thereby protecting tissues against inflammation, apoptosis and oxidative stress) [8], its expression declines after birth and it is present at much lower expression levels than AT1R in adult tissues. Thus AT1R rather than AT2R is predominantly activated by Ang-II. Fortunately, the ‘protective’ arm of RAS also involves activation of the highly expressed Mas receptor (MasR) by Ang-(1–7). Ang-(1–7) is able to counteract the effects of Ang-II and shows anti-inflammatory, anti-oxidative and vasodilatory properties [9]. The ACE2/Ang-(1–7)/MasR axis is thus the major ‘protective’ arm of the RAS (Fig. 1 ) [6].
Figure 1.
Therapeutic strategies targeting the ‘harmful’ or classical (red box) and ‘protective’ (green box) arms of the renin–angiotensin system (RAS), and the potential beneficial role of 20-hydroxyecdysone in addressing lung injury in patients with COVID-19. 20E, 20-hydroxyecdysone; ACE, angiotensin converting enzyme 1; ACE2, angiotensin converting enzyme 2; AT1R, angiotensin-II receptor type 1; AT2R, angiotensin II receptor type 2; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor AT1R blocker; MasR, Mas receptor; RAS, renin–angiotensin system; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
SARS-CoV-2 infection, by downregulating ACE2 expression and activity [10], reduces the conversion of Ang-II to Ang-(1–7), resulting in significantly higher levels of Ang-II in COVID-19 patients 11, 12. Importantly, these excessive levels of Ang-II are linearly associated with SARS-Cov-2 viral load and severity of lung injury during COVID-19 13, 14. In addition, the plasma levels of Ang-(1–7) and potentially those of Ang-1–9 15, 16 are significantly lower in COVID-19 patients than in healthy controls, and these levels are particularly low in COVID-19 patients who are admitted to ICUs. As a consequence, a general imbalance between the ‘harmful’ and ‘protective’ arms of the RAS, resulting from excessive activation of AT1R and limited activation of AT2R and MasR, has been proposed, and this hypothesis is supported by the clinical picture reported in COVID-19 patients [12]. Therefore, it has been suggested that restoration of the balance of the RAS could be a particularly relevant way to treat patients who are infected with SARS-CoV-2.
Rebalancing the RAS using ACE inhibitors and/or angiotensin receptor blockers in COVID-19 patients
The initial proposal to restore an adequate balance of the RAS involves inhibiting its ‘harmful’ ACE/Ang-II/AT1R arm, either with angiotensin converting enzyme inhibitors (ACEIs) that limit the formation of Ang-II or by using angiotensin receptor blockers (ARBs) to inhibit AT1R activation (Fig. 1). Notably, one of the most preeminent COVID-19-associated comorbidities is hypertension, meaning that many SARS-CoV2-infected patients are already taking ACEI or ARB medication.
The risks of using ACEIs and ARBs in the context of Sars-CoV2 infection have been much debated. Indeed, it was feared that ACEI and ARBs might increase the expression level of ACE2 and consequently facilitate the infection of hosts cells by SARS-CoV-2 3, 17. However, a large-scale study of ACE2 gene expression in the lungs of ACEIs and ARBs users has been performed and did not support this hypothesis [18]. Indeed, it was shown that ACEI use was associated with significantly lower ACE2 expression, whereas ARBs did not affect ACE2 expression. Interestingly, the use of ARBs was associated with increased expression of ACE and decreased expression of AGTR1 (the gene coding for AT1R) [18]. Jointly, the Heart Failure Society of America, the American College of Cardiology, and the American Heart Association recommend continuation of RAS antagonists for patients infected with SARS-CoV-2 and suffering of heart failure, hypertension, or ischemic heart disease, for which these agents are the standard care [19]. This confirms the safety of using ACEIs and ARBs such as losartan as an approach to treat COVID-19 patients through inhibition of the harmful arm of the RAS.
As previously described in SARS-CoV infection, ACEI and ARBs can control the stimulation of the ACE/Ang-II/AT1R axis, thereby reducing the production of pro-inflammatory cytokines including IL-1, IL-6 and TNF-α, and can modulate the activation of innate and adaptive immunity [20]. In addition, ACEI and ARBs, by reducing the formation of Ang-II, are expected to inhibit the vasoconstrictive and prothrombotic actions of Ang-II. Numerous clinical trials to test the efficacy of maintaining versus stopping ACEI and ARB treatments in COVID-19 patients who have hypertension are actively recruiting [21]. Lists of clinical trials using ARBs and ACEIs to inhibit the ‘harmful’ arm of the RAS are presented in Table 1, Table 2 , respectively. Interestingly, it has been reported that the antithrombotic effects of the ACEI captopril and the ARB losartan were indirectly mediated by Ang-(1–7), and were abolished by the MasR antagonist A-779 [22]. The stimulated formation of Ang-(1–7), a protective anti-inflammatory metabolite, in response to ACEIs and ARBs is mediated by ACE2. This suggests an indirect beneficial effect of ACEI and ARBs by activating the ‘protective’ arm of the RAS [3], which could be exploited for the treatment of cardio-respiratory failure in COVID-19 patients.
Table 1.
Ongoing clinical trials using angiotensin receptor AT1R blockers (ARBs) to inhibit the ACE/Ang-II/ATR1 axis of the renin–angiotensin system (RAS).
| Study title | Phase | Interventions | Sponsor | ClinicalTrials.gov identifier |
|---|---|---|---|---|
| Inhibition of the harmful arm of the RAS with ARBs | ||||
| Study of Open Label Losartan in COVID-19 | I | Losartan | University of Kansas Medical Center, USA | NCT04335123 |
| Chloroquine + Losartan Compared to Chloroquine Alone for the Treatment of COVID-19 Pneumonia | II | Chloroquine phosphate plus losartan vs. chloroquine phosphate | Hospital Universitario José E. Gonzalez Monterrey, Nuevo Leon, Mexico | NCT04428268 |
| Early Treatment with Ivermectin and LosarTAN for Cancer Patients With COVID-19 Infection (TITAN) | II | Ivermectin plus losartan vs. placebo | Instituto do Cancer do Estado de Sao Paulo Sao Paulo, Brazil | NCT04447235 |
| Telmisartan for Treatment of COVID-19 Patients | II | Standard care plus telmisartan vs. standard care | Laboratorio Elea Phoenix S.A., Argentina | NCT04355936 |
| Losartan for Patients With COVID-19 Requiring Hospitalization | II | Losartan vs. placebo | University of Minnesota, USA | NCT04312009 |
| Losartan for Patients With COVID-19 Not Requiring Hospitalization | II | Losartan vs. placebo | University of Minnesota, USA | NCT04311177 |
| Pilot Clinical Trial of the Safety and Efficacy of Telmisartan for the Mitigation of Pulmonary and Cardiac Complications in COVID-19 Patients | II | Telmisartan vs. placebo | University of Hawaii, USA | NCT04360551 |
| COVID MED Trial – Comparison of Therapeutics for Hospitalized Patients Infected With SARS-CoV-2 (COVIDMED) | II/III | Losartan vs. lopinavir/ritonavir vs. hydroxychloroquine sulfate vs. placebos | Bassett Healthcare, USA | NCT04328012 |
| Coronavirus Response – Active Support for Hospitalised Covid-19 Patients (CRASH-19) | III | Standard of care vs. aspirin vs. losartan vs. simvastatin | London School of Hygiene and Tropical Medicine, UK | NCT04343001 |
| Efficacy of Hydroxychloroquine, Telmisartan and Azithromycin on the Survival of Hospitalized Elderly Patients With COVID-19 (COVID-Aging) | III | Standard of care vs. hydroxychloroquine vs. azithromycin vs. telmisartan |
University Hospital, Strasbourg, France | NCT04359953 |
| Treatments to Decrease the Risk of Hospitalization or Death in Elderly Outpatients with Symptomatic SARS-CoV-2 Infection (COVID-19) (COVERAGE) | III | Dietary supplement: vitamins vs. imatinib vs. telmisartan |
University Hospital, Bordeaux, University of Bordeaux, France | NCT04356495 |
| Do Angiotensin Receptor Blockers Mitigate Progression to Acute Respiratory Distress Syndrome With SARS-CoV-2 Infection | IV | Losartan | Sharp HealthCare, La Mesa, California, USA | NCT04340557 |
| Valsartan for Prevention of Acute Respiratory Distress Syndrome in Hospitalized Patients With SARS-COV-2 (COVID-19) Infection Disease | IV | Valsartan vs. placebo | Radboud University, The Netherlands | NCT04335786 |
| Controlled evaLuation of Angiotensin Receptor Blockers for COVID-19 respIraTorY Disease (CLARITY) | IV | Standard of care plus angiotensin receptor blockers vs. standard of care | The George Institute, Australia | NCT04394117 |
Table 2.
Ongoing clinical trials using angiotensin-converting enzyme inhibitors (ACEIs) to inhibit the ACE/Ang-II/ATR1 axis of the renin–angiotensin system (RAS).
| Study title | Phase | Interventions | Sponsor | ClinicalTrials.gov Identifier |
|---|---|---|---|---|
| Inhibition of the harmful arm of the RAS with ACEI | ||||
| Ramipril for the Treatment of COVID-19 (RAMIC) | II | Ramipril vs. placebo | University of California, San Diego, USA | NCT04366050 |
| Efficacy of Captopril in Covid-19 Patients with Severe Acute Respiratory Syndrome (SARS) CoV-2 Pneumonia (CAPTOCOVID) | II | Captopril vs. standard of care | Assistance Publique – Hôpitaux de Paris, France | NCT04355429 |
| Angiotensin Converting Enzyme Inhibitors in Treatment of COVID 19 | III | Captopril or enalapril vs. choloroquine | Tanta University, Egypt | NCT04345406 |
Potential beneficial effects of restoring RAS balance through AT2R and MasR activation in COVID-19
Stimulating the protective axis of the RAS instead of blocking the harmful arm with ACEIs or ARBs is an alternative possibility to restore RAS equilibrium. The RAS ‘protective’ arm has a pleiotropic effect and controls many biological functions. Thus, activating this axis seems to be a particularly interesting alternative to attempts to activate more specific molecules that act on only one clinical feature of the disease, for instance anti-inflammatory drugs such as tocilizumab specifically targeting IL-6R to prevent the cytokine storm observed in severely ill COVID-19 patients.
In order to restore the balance of the RAS, the use of AT2R agonists to stimulate the protective arm can be proposed. However, as AT2R is weakly expressed in adults and even more so in elderly people, its activation by agonists might have a limited effect in restoring RAS balance. Nevertheless, both Ang-(1–9) and Ang-(1–7) stimulate AT2R formation, and elevated plasma levels of these two peptides have been found in survivors of ARDS [23], suggesting that they could indeed provide potential beneficial effects in COVID-19 patients. Supporting this idea, Ang-(1–9) ameliorates pulmonary arterial hypertension via AT2R [24]. However, it has been shown that some Ang-(1–9) can also be converted to Ang-II and can enhance arterial thrombosis in rats [25], which could be deleterious during COVID-19. This ambivalent activity may explain why no clinical attempt is underway to treat COVID-19 through administration of Ang-(1–9) itself. By contrast, a synthetic cyclized AT2R agonist demonstrated anti-inflammatory effects and anti-hypertrophic effects in a chronic lung injury animal model [26]. In addition, C21 (a non-peptide synthetic agonist) [27], showed beneficial effects in animal models of pulmonary hypertension 28, 29. A Phase 2 clinical trial evaluating the efficacy and safety of C21 in COVID-19 patients (ClinicalTrials #NCT04452435) has been completed, but the results have not yet been reported [30] (Table 3 ).
Table 3.
Ongoing clinical trials using stimulation of the AT2R or ACE2/Ang-1–7/MasR axis of the renin–angiotensin system (RAS).
| Study title | Phase | Interventions | Sponsor | ClinicalTrials.gov Identifier |
|---|---|---|---|---|
| Stimulation of the protective arm of the RAS with an angiotensin II receptor type 2 (AT2R) agonist | ||||
| Safety and Efficacy of C21 in Subjects With COVID-19 | II | C21 vs. placebo | Vicore Pharma AB, Sweden | NCT04452435 |
|
Stimulation of the protective arm of the RAS with MasR agonists and activators | ||||
| Treatment of Angiotensin Peptide (1–7) for COVID-19 | I | Standard of care plus Angiotensin peptide (1–7)-derived plasma vs. standard of care | Kanuni Sultan Suleyman Training and Research Hospital, Turkey | NCT04375124 |
| TXA COVID-19 Clinical Trial | II | TXA127 vs. placebo | Columbia University, USA | NCT04401423 |
| Angiotensin-(1,7) Treatment in COVID-19: the ATCO Trial | II/III | Angiotensin 1–7 vs. placebo | Erasme University Hospital Brussels, Belgium | NCT04332666 |
| Testing the Efficacy and Safety of BIO101 for the Prevention of Respiratory Deterioration in COVID-19 Patients (COVA) | II/III | BIO101 vs. placebo | Biophytis, France | NCT04472728 |
More than 35 years ago, it was shown that Ang-(1–7) is a key component of the RAS and not merely a degradation product of Ang-I and Ang-II [31]. Ang-(1–7) is part of the protective arm and counteracts the harmful arm of the RAS by binding to AT2R and MasR. As AT2R expression is limited, activation of the MasR by Ang-(1–7) may predominantly explain the effects of Ang-(1–7) in rebalancing the RAS. Accordingly, it has been proposed that Ang-(1–7), and MasR agonists more generally, could be used as a treatment for patients with severe COVID-19 illness [9]. In support of this hypothesis, many in vitro and in vivo studies have demonstrated that MasR is expressed in the epithelium and smooth muscles of the airways, in alveolar cells, and in the endothelium and smooth muscle cells of vascular tissues [32]. Thus stimulation of the ACE2/Ang-(1–7)/MasR axis has the potential to produce beneficial effects on respiratory functions, arterial oxygenation, and lung tissue [32]. This is notably the case in the context of pulmonary emphysema [33], lung fibrosis [34], pulmonary hypertension [35], lung inflammation [36], chronic asthma [32] and cigarette smoking [37]. Indeed, it has been shown that MasR activation by Ang-(1–7) plays an important role in opposing the pro-thrombotic and pro-inflammatory effects of Ang-II [38], by reducing the synthesis of pro-inflammatory cytokines and by inhibiting the migration of inflammatory cells to the lungs, leading to a better respiratory function [39]. Interestingly, in a murine model of ARDS, Ang-(1–7) has also been shown to reduce collagen deposition in the lungs [39]. In addition, the Ang-(1–7)/MasR axis inhibits pulmonary fibrosis [40] and induces apoptosis of neutrophils [41]. Moreover, the ACE2/Ang-(1–7)/Mas axis protects against thrombosis [42], as demonstrated in animals in which MasR had been knocked out, which show a shorter bleeding time and increased size of thrombi [43].
A potential additional beneficial effect of Ang-(1–7) relates to the diaphragm dysfunction observed in some COVID-19 patients. Indeed, mechanical ventilation, the main supportive therapy for ARDS patients, induces ventilator-induced diaphragmatic dysfunction (VIDD) [44], which is characterized by a contractile dysfunction and a rapid muscular atrophy [45]. Muscular disorders may result from a RAS imbalance [46]. It has been shown that Ang-II induces diaphragm muscle wasting and respiratory muscle dysfunction [47], whereas Ang-(1–7) exerts a protective action in a rat model of VIDD [48] and could improve muscular functions in patients infected by SARS-CoV-2 [46].
Unfortunately, Ang-(1–7) has a very short half-life (less than one minute in human plasma) [49] and some studies point out a lack of specificity. Hence, there is a need to develop improved formulations or modified versions of Ang-(1–7) that have similar biological effects but a longer half-life than the endogenous peptide. For instance, hydroxypropyl-β-cyclodextrin–Ang-(1–7) complexes act as a long-lasting release system in which Ang-(1–7) is protected from inactivation by digestive tract enzymes, thus allowing oral administration [50]. This complex has shown many of the beneficial cardiovascular and metabolic effects of Ang-(1–7) in orally treated spontaneously hypertensive rats [43], as well as improvement of muscular function in a mouse model of hindlimb immobilization and Duchenne muscular dystrophy [51]. Similarly, intravenous infusion of cyclic Ang-(1–7), a form that is more resistant than Ang-(1–7) to enzymatic hydrolysis, has demonstrated long-term vasorelaxant effects in a rat model of myocardial infarction [52]. Moreover, continuous Ang-(1–7) infusion for 2 days resulted in improvement of endothelial cell functions in preeclamptic patients [53]. Other MasR agonists have similar pleiotropic protective effects. The two peptides CGEN-856 and CGEN-857 have been reported to have ex vivo vasorelaxant properties in mouse aortic rings or antihypertensive and cardioprotective effects in spontaneously hypertensive rats [54]. In addition, the orally active non-peptidic Mas receptor agonist AVE0991 was able to mimic the effects of Ang 1–7 on several organs, such as blood vessels [55], kidneys [56], and heart [57].
Interestingly, it has been reported that Mas stimulation in different animal models can increase AT2R expression, and that this relation is reciprocal. Co-administration of a MasR agonist and an AT2R agonist could be an approach to potentiate the beneficial effects of the protective RAS axis.
Overall, the possibility of using AT2R agonists, Ang-(1–7) or other Mas agonists could provide a valuable therapeutic strategy in COVID-19, and a few clinical trials to test this hypothesis with drug candidates are ongoing (Table 3).
20-Hydroxyecdysone (20E), a new MasR activator with potentially beneficial effects against COVID-19
20-hydroxyecdysone (20E) has been described recently as a new MasR activator, thanks to pharmacological and gene interference approaches [58]. Phytoecdysteroids are polyhydroxylated steroids analogous to arthropod molting hormones that are widely distributed in plants throughout the world and are present in significant amounts (up to >2% of dry weight) in 5–6% of randomly investigated plant species [59]. 20-hydroxyecdysone is the most frequently encountered and abundant representative. Ecdysteroids are present in numerous medicinal plants and have been found to have beneficial effects in mammals [59], opening new therapeutic opportunities in the context of the COVID-19 pandemic.
Of particular interest, 20E has shown anti-inflammatory effects in vivo in a mouse model of acute lung injury (ALI) [60]. Indeed, 20E treatment reduced the expression of inflammatory cytokines (TNF-α, IL-2, IL-6, IL-8) and increased the expression of anti-inflammatory cytokines (IL-4, IL-10) [60]. Modulation of inflammation by 20E was associated with a decrease in lung damage, as shown by histological examination of animal lungs. Similarly, two other studies in rat models of ALI demonstrated that 20E treatment protected the animals by increasing both the serum level of an anti-inflammatory cytokine (IL-10) and the expression of IL-10 mRNA in the lung tissue [61]. Moreover, Li and collaborators [62] demonstrated that 20E inhibited the TLR4 pathway, leading to the promotion of surfactant protein A release by pneumocytes that finally improves respiratory functions.
Interstitial fibrosis of lung tissue is one of the hallmarks of COVID-19. Fibrosis in lung tissue is associated with organizing pneumonia, which eventually evolves into widespread fibrotic change leading to severe ALI. This progression has been shown to be linked with the development of ARDS [63]. Interestingly, 20E has demonstrated significant anti-fibrotic activity in heart and kidney by reversing the downstream effects of TGF-β1 on the activity of connective tissue growth factor (CTGF) [64], a profibrotic factor. In an animal model of Duchenne muscular dystrophy, we consistently observed that myocardial expression of the CTGF gene was reduced by 20E [65]. Thus, the antifibrotic properties of 20E could also be beneficial in COVID-19 patients.
In addition, thrombosis, resulting from coagulation abnormalities (coagulopathy) has been associated with the severe hypoxia observed in COVID-19 patients [66]. Accordingly, the administration of anticoagulants was proposed for COVID-19 patients with a high thrombotic risk [67]. MasR activation opposes the pro-thrombotic effects of Ang-II [43]. Moreover, MasR stimulation has been shown to maintain a healthy vascular homeostasis [42]. Thus, by activating MasR, 20E is expected to display similar anti-thrombotic effects. Accordingly, 20E has been shown to reduce hyper-coagulation induced by intensive physical exercise [68]. This effect of 20E deserves further confirmation in models closely related to COVID-19 pathology but holds additional promise for the amelioration of patients who are infected with SARS-CoV-2.
Clinical development of BIO101, a new drug candidate based on a pharmaceutical grade formulation of 20E to improve respiratory function in COVID-19 patients
Biophytis has developed BIO101, a pharmaceutical grade oral preparation of immediate-release 20E at ≥97% purity extracted from Cyanotis sp. plants. In the light of numerous studies demonstrating the beneficial effects of 20E on muscular function [69], BIO101 is currently being assayed for treating sarcopenia in a phase 2 clinical trial. (This is a double-blind, placebo controlled, randomized interventional clinical trial (SARA-INT), ClinicalTrials #NCT03452488.) We believe that BIO101 administration could also be helpful in the prevention of the muscle disuse atrophy, severe muscle weakness, deconditioning, fatigue, and impaired motility observed in COVID-19 patients who have been immobilized in the prone position during long-term hospitalization in ICUs [70]. BIO101 treatment could also be beneficial during a patient's rehabilitation.
In addition, by using nebulization of the powerful bronchoconstrictor methacholine in mice, we demonstrated that chronic oral administration of BIO101 prevents the decline of respiratory function in mdx mice, a murine model of Duchenne muscular dystrophy [71]. BIO101 improved breathing parameters (inspiratory and expiratory time and frequency) in the mice, as demonstrated by enhanced pause (Penh) measurements [71]. Interestingly, BIO101 treatment also improved the deep airway structure and the mechanical properties of the lungs (resistance, compliance and elastance) in these mice [71]. Together, these observations strongly suggest that BIO101 could have a protective effect against the ARDS observed in humans suffering from severe forms of COVID-19.
There is, as yet, no direct evidence for beneficial effects of BIO101 in a preclinical animal model of Sars-CoV-2 infection. However, the potential anti-inflammatory, antifibrotic and anti-thrombotic effects of BIO101 administration, achieved by activating the ‘protective’ arm of RAS via MasR, allow us to believe that BIO101 could be beneficial in patients with mild and severe forms of COVID-19 (Fig. 1). BIO101 might also benefit patients who are being treated in the ICU by preserving muscle function. A Phase 2/3 clinical trial (COVA, ClinicalTrials #NCT04472728) is ongoing in the US, France, Belgium, the UK and Brazil to test the efficacy of BIO101 in COVID-19 patients who do not require mechanical ventilation.
Conclusions
Because most of the deleterious effects of SARS-CoV-2, including inflammation, fibrosis, thrombosis and pulmonary damage, point towards an imbalance in the RAS, we strongly believe that inhibiting the ‘harmful’ arm of the RAS (with ARBs or ACEIs) and/or activating the ‘protective’ arm (through activation of AT2R or MasR downstream of ACE2) could have a beneficial effect in COVID-19-infected patients and could improve their ARDS outcome. Among these strategies, BIO101 could offer a new therapeutic option in COVID-19 patients by improving their respiratory and muscular functions, and might ultimately promote the survival of patients who are at high risk of developing very severe forms of this devastating disease.
Funding
This work was supported by Biophytis.
Conflicts of interest
ML, SC, RL, SV, and PD are employees of Biophytis. They declare, however, that their potential commercial interests had no impact on the rational scientific conduct of this review.
Acknowledgements
The contribution of Dr L.N. Dinan in critically reading the manuscript and language improvement is acknowledged.
References
- 1.Zhou P., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta S., et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern. Med. 2020;180:1–12. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo T., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu X., et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020;63:457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffmann M., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santos R.A.S., et al. The ACE2/angiotensin-(1-7)/MAS axis of the renin–angiotensin system: focus on angiotensin-(1-7) Physiol. Rev. 2018;98:505–553. doi: 10.1152/physrev.00023.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ni W., et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care. 2020;24:422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsutsumi Y., et al. Angiotensin II type 2 receptor is upregulated in human heart with interstitial fibrosis, and cardiac fibroblasts are the major cell type for its expression. Circ. Res. 1998;83:1035–1046. doi: 10.1161/01.res.83.10.1035. [DOI] [PubMed] [Google Scholar]
- 9.Magalhaes G.S., et al. Activation of Ang-(1-7)/Mas receptor is a possible strategy to treat coronavirus (SARS-CoV-2) infection. Front. Physiol. 2020;11:730. doi: 10.3389/fphys.2020.00730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banu N., et al. Protective role of ACE2 and its downregulation in SARS-CoV-2 infection leading to macrophage activation syndrome: therapeutic implications. Life Sci. 2020;256:117905. doi: 10.1016/j.lfs.2020.117905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miesbach W. Pathological role of angiotensin II in severe COVID-19. TH Open. 2020;4:e138–e144. doi: 10.1055/s-0040-1713678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verdecchia P., et al. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Y., et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Z., et al. Elevation of plasma angiotensin II level is a potential pathogenesis for the critically ill COVID-19 patients. Crit. Care. 2020;24:290. doi: 10.1186/s13054-020-03015-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muslim S., et al. Treatment options available for COVID-19 and an analysis on possible role of combination of rhACE2, angiotensin (1-7) and angiotensin (1-9) as effective therapeutic measure. SN Compr. Clin. Med. 2020:1–6. doi: 10.1007/s42399-020-00407-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henry B.M., et al. Coronavirus disease 2019 (COVID-19) is associated with low circulating plasma levels of Angiotensin 1 and Angiotensin 1,7. J. Med. Virol. 2020;93:678–680. doi: 10.1002/jmv.26479. [DOI] [PubMed] [Google Scholar]
- 17.Fang L., et al. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Milne S., et al. SARS-CoV-2 receptor ACE2 gene expression and RAAS inhibitors. Lancet Respir. Med. 2020;8:e50–e51. doi: 10.1016/S2213-2600(20)30224-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bozkurt B., et al. Joint HFSA/ACC/AHA statement addresses concerns re: using RAAS antagonists in COVID-19. J. Card. Fail. 2020;26:370. doi: 10.1016/j.cardfail.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuba K., et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopes R.D., et al. Continuing versus suspending angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: impact on adverse outcomes in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the BRACE CORONA trial. Am. Heart J. 2020;226:49–59. doi: 10.1016/j.ahj.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kucharewicz I., et al. Antithrombotic effect of captopril and losartan is mediated by angiotensin-(1-7) Hypertension. 2002;40:774–779. doi: 10.1161/01.hyp.0000035396.27909.40. [DOI] [PubMed] [Google Scholar]
- 23.Reddy R., et al. Circulating angiotensin peptides levels in Acute Respiratory Distress Syndrome correlate with clinical outcomes: a pilot study. PLoS One. 2019;14:e0213096. doi: 10.1371/journal.pone.0213096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cha S.A., et al. Angiotensin-(1-9) ameliorates pulmonary arterial hypertension via angiotensin type II receptor. Korean J. Physiol. Pharmacol. 2018;22:447–456. doi: 10.4196/kjpp.2018.22.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kramkowski K., et al. Angiotensin-(1-9), the product of angiotensin I conversion in platelets, enhances arterial thrombosis in rats. J. Physiol. Pharmacol. 2010;61:317–324. [PubMed] [Google Scholar]
- 26.Wagenaar G.T., et al. Agonists of MAS oncogene and angiotensin II type 2 receptors attenuate cardiopulmonary disease in rats with neonatal hyperoxia-induced lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 2013;305:L341–L351. doi: 10.1152/ajplung.00360.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wan Y., et al. Design, synthesis, and biological evaluation of the first selective nonpeptide AT2 receptor agonist. J. Med. Chem. 2004;47:5995–6008. doi: 10.1021/jm049715t. [DOI] [PubMed] [Google Scholar]
- 28.Bruce E., et al. Selective activation of angiotensin AT2 receptors attenuates progression of pulmonary hypertension and inhibits cardiopulmonary fibrosis. Br. J. Pharmacol. 2015;172:2219–2231. doi: 10.1111/bph.13044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rathinasabapathy A., et al. The selective angiotensin II type 2 receptor agonist, compound 21, attenuates the progression of lung fibrosis and pulmonary hypertension in an experimental model of Bleomycin-induced lung injury. Front. Physiol. 2018;9:180. doi: 10.3389/fphys.2018.00180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steckelings U.M., Sumners C. Correcting the imbalanced protective RAS in COVID-19 with angiotensin AT2-receptor agonists. Clin. Sci. (Lond.) 2020;134:2987–3006. doi: 10.1042/CS20200922. [DOI] [PubMed] [Google Scholar]
- 31.Greene L.J., et al. Brain endo-oligopeptidase B: a post-proline cleaving enzyme that inactivates angiotensin I and II. Hypertension. 1982;4:178–184. doi: 10.1161/01.hyp.4.2.178. [DOI] [PubMed] [Google Scholar]
- 32.Magalhaes G.S., et al. Angiotensin-(1-7) promotes resolution of eosinophilic inflammation in an experimental model of asthma. Front. Immunol. 2018;9:58. doi: 10.3389/fimmu.2018.00058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bastos A.C., et al. Oral formulation angiotensin-(1-7) therapy attenuates pulmonary and systemic damage in mice with emphysema induced by elastase. Immunobiology. 2020;225:151893. doi: 10.1016/j.imbio.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Shao M., et al. Exogenous angiotensin (1-7) directly inhibits epithelial-mesenchymal transformation induced by transforming growth factor-beta1 in alveolar epithelial cells. Biomed. Pharmacother. 2019;117:109193. doi: 10.1016/j.biopha.2019.109193. [DOI] [PubMed] [Google Scholar]
- 35.Daniell H., et al. Investigational new drug enabling angiotensin oral-delivery studies to attenuate pulmonary hypertension. Biomaterials. 2020;233:119750. doi: 10.1016/j.biomaterials.2019.119750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ye R., Liu Z. ACE2 exhibits protective effects against LPS-induced acute lung injury in mice by inhibiting the LPS-TLR4 pathway. Exp. Mol. Pathol. 2020;113:104350. doi: 10.1016/j.yexmp.2019.104350. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y., et al. Angiotensin-(1-7)-mediated Mas1 receptor/NF-kappaB-p65 signaling is involved in a cigarette smoke-induced chronic obstructive pulmonary disease mouse model. Environ. Toxicol. 2018;33:5–15. doi: 10.1002/tox.22454. [DOI] [PubMed] [Google Scholar]
- 38.Liang B., et al. Angiotensin-(1-7) attenuates angiotensin II-induced ICAM-1, VCAM-1, and MCP-1 expression via the MAS receptor through suppression of P38 and NF-kappaB pathways in HUVECs. Cell Physiol. Biochem. 2015;35:2472–2482. doi: 10.1159/000374047. [DOI] [PubMed] [Google Scholar]
- 39.Zambelli V., et al. Angiotensin-(1-7) improves oxygenation, while reducing cellular infiltrate and fibrosis in experimental acute respiratory distress syndrome. Intensive Care Med. Exp. 2015;3:44. doi: 10.1186/s40635-015-0044-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meng Y., et al. The angiotensin-converting enzyme 2/angiotensin (1-7)/Mas axis protects against lung fibroblast migration and lung fibrosis by inhibiting the NOX4-derived ROS-mediated RhoA/Rho kinase pathway. Antioxid. Redox Signal. 2015;22:241–258. doi: 10.1089/ars.2013.5818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reyes-Engel A., et al. Influence of gender and genetic variability on plasma angiotensin peptides. J Renin. Angiotensin Aldosterone Syst. 2006;7:92–97. doi: 10.3317/jraas.2006.015. [DOI] [PubMed] [Google Scholar]
- 42.Fang C., Schmaier A.H. Novel anti-thrombotic mechanisms mediated by Mas receptor as result of balanced activities between the kallikrein/kinin and the renin–angiotensin systems. Pharmacol. Res. 2020;160:105096. doi: 10.1016/j.phrs.2020.105096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fraga-Silva R.A., et al. An orally active formulation of angiotensin-(1-7) produces an antithrombotic effect. Clinics (Sao Paulo) 2011;66:837–841. doi: 10.1590/S1807-59322011000500021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Powers S.K., et al. Ventilator-induced diaphragm dysfunction: cause and effect. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2013;305:R464–R477. doi: 10.1152/ajpregu.00231.2013. [DOI] [PubMed] [Google Scholar]
- 45.Sigurta A., et al. Renin–angiotensin system in ventilator-induced diaphragmatic dysfunction: potential protective role of angiotensin (1-7) Med. Hypotheses. 2016;94:132–137. doi: 10.1016/j.mehy.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 46.Yamamoto K., et al. ACE2, angiotensin 1-7 and skeletal muscle: review in the era of COVID-19. Clin. Sci. (Lond.) 2020;134:3047–3062. doi: 10.1042/CS20200486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rezk B.M., et al. Angiotensin II infusion induces marked diaphragmatic skeletal muscle atrophy. PLoS One. 2012;7:e30276. doi: 10.1371/journal.pone.0030276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zambelli V., et al. Angiotensin-(1-7) exerts a protective action in a rat model of ventilator-induced diaphragmatic dysfunction. Intensive Care Med. Exp. 2019;7:8. doi: 10.1186/s40635-018-0218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Namsolleck P., Moll G.N. Does activation of the protective renin–angiotensin system have therapeutic potential in COVID-19? Mol. Med. 2020;26:80. doi: 10.1186/s10020-020-00211-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lula I., et al. Study of angiotensin-(1-7) vasoactive peptide and its beta-cyclodextrin inclusion complexes: complete sequence-specific NMR assignments and structural studies. Peptides. 2007;28:2199–2210. doi: 10.1016/j.peptides.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 51.Acuna M.J., et al. Restoration of muscle strength in dystrophic muscle by angiotensin-1-7 through inhibition of TGF-beta signalling. Hum. Mol. Genet. 2014;23:1237–1249. doi: 10.1093/hmg/ddt514. [DOI] [PubMed] [Google Scholar]
- 52.Durik M., et al. The effect of the thioether-bridged, stabilized angiotensin-(1-7) analogue cyclic ang-(1-7) on cardiac remodeling and endothelial function in rats with myocardial infarction. Int. J. Hypertens. 2012;2012:536426. doi: 10.1155/2012/536426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brandão A., et al. Flow-mediated dilation of brachial artery response after 24 hours of angiotensin-(1-7) infusion in patients with severe and early-onset of preeclampsia. 10th World Congress of Perinatal Medicine; Punta del Este, Uruguay, November 8–11; 2011. [Google Scholar]
- 54.Savergnini S.Q., et al. Vascular relaxation, antihypertensive effect, and cardioprotection of a novel peptide agonist of the MAS receptor. Hypertension. 2010;56:112–120. doi: 10.1161/HYPERTENSIONAHA.110.152942. [DOI] [PubMed] [Google Scholar]
- 55.Wiemer G., et al. AVE 0991, a nonpeptide mimic of the effects of angiotensin-(1-7) on the endothelium. Hypertension. 2002;40:847–852. doi: 10.1161/01.hyp.0000037979.53963.8f. [DOI] [PubMed] [Google Scholar]
- 56.Pinheiro S.V., et al. Nonpeptide AVE 0991 is an angiotensin-(1-7) receptor Mas agonist in the mouse kidney. Hypertension. 2004;44:490–496. doi: 10.1161/01.HYP.0000141438.64887.42. [DOI] [PubMed] [Google Scholar]
- 57.Benter I.F., et al. Angiotensin-(1-7) prevents diabetes-induced cardiovascular dysfunction. Am. J. Physiol. Heart Circ. Physiol. 2007;292:H666–H672. doi: 10.1152/ajpheart.00372.2006. [DOI] [PubMed] [Google Scholar]
- 58.Lafont R., et al. 20-Hydroxyecdysone activates the protective arm of the renin–angiotensin system via Mas receptor. BioRxiv. 2020 https://www.biorxiv.org/content/10.1101/2020.1104.1108.032607v032601. [Google Scholar]
- 59.Dinan L., Lafont R. Effects and applications of arthropod steroid hormones (ecdysteroids) in mammals. J. Endocrinol. 2006;191:1–8. doi: 10.1677/joe.1.06900. [DOI] [PubMed] [Google Scholar]
- 60.Song G., et al. Protective effect of 20-hydroxyecdysterone against lipopolysaccharides-induced acute lung injury in mice. J. Pharm. Drug Res. 2019;2:109–114. [Google Scholar]
- 61.Wu X., et al. Effects of ecdysterone on the ultrastructure and IL-10 mRNA expression of lung tissue in rats with acute lung injury. Infect. Inflamm. Repair. 2012:207–211. + 257. [Google Scholar]
- 62.Li J., et al. Effect of ecdysterone on the expression of toll-like receptor 4 and surfactant protein A in lung tissue of rats with acute lung injury. Infect. Inflamm. Repair. 2013;2013:22–26. [Google Scholar]
- 63.George P.M., et al. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir. Med. 2020;8:807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hung T.J., et al. 20-Hydroxyecdysone attenuates TGF-beta1-induced renal cellular fibrosis in proximal tubule cells. J. Diabetes Complications. 2012;26:463–469. doi: 10.1016/j.jdiacomp.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 65.Dilda P., et al. Use of 20-hydroxyecdysone and the derivatives thereof in the treatment of myopathies. Biophytis. 2018 WO2018/197708. [Google Scholar]
- 66.Becker R.C. COVID-19 update: Covid-19-associated coagulopathy. J. Thromb. Thrombolysis. 2020;50:54–67. doi: 10.1007/s11239-020-02134-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Watson R.A., et al. Anti-coagulant and anti-platelet therapy in the COVID-19 patient: a best practices quality initiative across a large health system. Hosp. Pract. (1995) 2020;48:169–179. doi: 10.1080/21548331.2020.1772639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Azizov A.P. Effects of eleutherococcus, elton, leuzea, and leveton on the blood coagulation system during training in athletes. Eksp. Klin. Farmakol. 1997;60:58–60. [PubMed] [Google Scholar]
- 69.Báthori M., et al. Phytoecdysteroids and anabolic-androgenic steroids – structure and effects on humans. Curr. Med. Chem. 2008;15:75–91. doi: 10.2174/092986708783330674. [DOI] [PubMed] [Google Scholar]
- 70.Kiekens C., et al. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur. J. Phys. Rehabil. Med. 2020;56:323–326. doi: 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- 71.Dilda P., et al. BIO101 demonstrates combined beneficial effects on skeletal muscle and respiratory functions in a mouse model of Duchenne muscular dystrophy. 24th WMS Congress, Neuromuscular Disorders. 2019;29(Suppl 1):S158. [Google Scholar]