1. Introduction
Starting in January 2020, the COVID-19 pandemic has strained many healthcare systems, including our own in New York City, United States. Utilizing load balancing among 23 integrated hospitals, we increased capacity by 40% caring for upwards 15,000 COVID-19 inpatients [1]. Here we describe the coordinated deployment of our procedural trainees in anesthesiology and surgery to COV-ICUs as a framework for others.
2. Multidisciplinary anesthesiology/surgical trainees COVID response team
Mid-March 2020, elective inpatient surgeries were suspended and emergency cases also perplexingly declined. Residency program directors assembled the “Multidisciplinary Anesthesia/Surgical Trainees COVID Response Team (MASC)” to assure that trainees were being deployed within the boundaries of their capability. Within 48-h 158 trainees (8.4% total trainees) across general surgery, cardiothoracic surgery, plastics, orthopedics, urology, podiatry, OMFS and anesthesiology were staffing COV-ICUs. MASC was able to increase coverage from 8% to 35% of ICU support shifts by April 6.
2.1. Adaptation
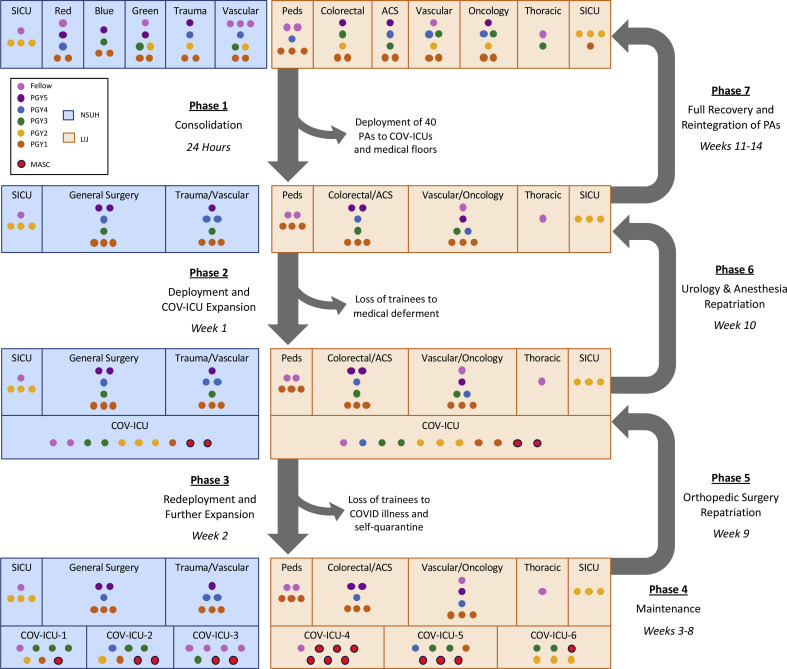
A tiered staffing strategy provided by the Society of Critical Care Medicine was the model for how COV-ICUs were staffed [2,3]. MASC trainees were deployed in parallel with acute care surgeons (Fig. 1 ). Due to the surge of acutely sick patients, elements of trauma and mass casualty management must be employed. Our success hinged on leveraging strong hierarchical relationships built on shared experiences in the SICUs and ORs. In addition to being familiar with such elements via training, the rapid adaptation was also attributable to the team-based approach that is core to these specialties.
Fig. 1.
Restructuring of general surgical services and trainee teams at NSUH and LIJ.
Note: This figure represents the restructuring of general surgical teams and COV-ICUs at NSUH and LIJ. Other surgical subspecialty teams and anesthesiology were restructured similarly; residents from those specialties who provided coverage in COV-ICUs are represented as MASC (red dots). Duration of rotation for interns followed pre-COVID block diagrams. Duration of rotation for mid-level residents in the COV-ICUs was one (urology) to two (orthopedics) to four (pgy2 general surgery) week blocks. Senior and chief residents and occasionally fellows had longer duration of rotations to maintain continuity, oversight and increased responsibility akin to attending faculty. All MASC trainees were repatriated to their original services by mid-May 2020.
Red = General Surgery/Colorectal Surgery, Blue = Hepatobiliary/Pancreatic Surgery/Transplant, Green = General Surgery/Minimally Invasive Surgery; MASC = Multidisciplinary Anesthesia/Surgical Trainees COVID Response Team; ACS = Acute Care Surgery; SICU = Surgical Intensive Care Unit; Peds = Pediatric Surgery, PAs = Physician Assistants.
Medical deferment was determined by a trainee's primary care doctor's assessment of increased risk based on contemporary CDC guidelines (see www.cdc.gov for details). The reason for medical deferment was not accessible to program directors. Medically deferred trainees were assigned to non-COV-patient care units.
Team training in simulated environments is an increasingly recognized necessity for the delivery of safe care in urgent situations. In addition to this foundational experience, shared “live” experiences in the OR and during trauma activations reinforce the vital importance of functioning within a team as leader, member, and scribe. To further leverage the pre-existing team dynamics, we took care to dispatch trainees only to COV-ICUs being headed by a surgical intensivist or surgeon. This preserved the hierarchy, organization, communication and approach strategies of the OR to a COV-ICU.
2.2. Insights
Procedural trainee deployment to COV-ICUs has demonstrated the vital role that our residencies can have in efficiently covering high volumes of complex patients during the current pandemic. The ability to rapidly transition from the OR to the COV-ICU has highlighted our specialties’ adaptability. It has also highlighted that the team dynamic developed in the OR can be translated to other settings. In addition to procedural expertise our trainees were also capable of providing care for complex, critically ill medical patients alongside surgical intensivists.
Given the magnitude of severity of this contagious illness with still emerging therapies, it is anticipated that our frontline trainees would feel physically, mentally and emotionally vulnerable. To support trainee wellbeing, work schedules were limited to 60-h/week and no changes were made to scheduled vacations.
Finally, in addition to meeting clinical needs, deployed trainees were able to continue a modified educational program. Pre-COVID-19 academic schedules were maintained and, in some ways, enhanced given the diminished surgical case volume. General surgery conferences transformed into protected virtual sessions moderated by subject-matter experts, which could be recorded for both synchronous and asynchronous education. Morbidity and mortality conferences and grand rounds saw a meteoric increase in both faculty and trainee attendance without the added barrier of travel other logistic considerations. Collaborative efforts across many hospitals in the city produced a robust series of shared online lectures allowing for maintenance and augmentation of pre-existing academic curricula.
3. Next steps
Effective and efficient trainee deployment is essential in responding to public health crises. We described here a unique process for the coordinated deployment of anesthesiology and surgery residents and fellows from multiple subspecialties during the early stage of this pandemic. MASC deployment to support the growing demand for critical care support demonstrates that the education provided by anesthesiology and surgery training programs can be translated to the unique environment of COV-ICUs. We considered the impact that the deployment process had on trainee education, physical wellbeing, and emotional wellbeing and engineered “COVID-Recovery” days to cushion the deployed trainees before bouncing back into the usual clockwork of the resident experience.
We hope this perspective provides a usable template for other procedural program directors in dreaded future mass casualty events for leveraging not only our procedural skills but also critical care knowledge and hierarchical team structure. We remain accountable to our trainees for ensuring their safety during the provision of altruistic care. The longer term effects of this rapid deployment on surgical case volumes and experiences remains is beyond the scope of this brief correspondence.
Ethical approval
Not applicable.
Sources of funding
This correspondence did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Michael A. Catalano: Conceptualization, formal analysis, investigation, writing – original draft, writing – review and editing, visualization. Gene F. Coppa: Conceptualization, resources, supervision. Vihas M. Patel: Conceptualization, formal analysis, writing – review and editing, project administration.
Research registration unique identifying number (UIN)
1. Name of the registry: not applicable.
2. Unique Identifying number or registration ID.
3. Hyperlink to your specific registration (must be publicly accessible and will be checked).
Guarantor
Vihas Patel, MD.
Provenance and peer review
Provenance and peer review not commissioned, internally peer-reviewed.
Data statement
Patient admission data is protected by the United States government privacy rule, also known as the Health Insurance Portability and Accountability Act of 1996.
Declaration of competing interest
All authors except Michael A. Catalano are Northwell Health employees.
Acknowledgments
Kathryn T Weber M.D., Ujas Shah M.D., Lyudmyla Demyan M.D., Judith Aronsohn M.D., Michael J Schwartz M.D., Lewis B Lane M.D., Matthew D Giangola M.D., Andrew C Yacht M.D.
References
- 1.Richardson S., Hirsch J.S., Narasimhan M., et al. And the Northwell COVID-19 research ConsortiumPresenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giangola M., Siskind S., Faliks B., et al. Applying triage principles of mass casualty events to the SARS-CoV-2 pandemic: from the perspective of the acute care surgeons at Long Island Jewish Medical Center in the COVID epicenter of the US. Surgery. 2020;168(3):408–410. doi: 10.1016/j.surg.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DePeralta D.K., Hong A.R., Choy C., et al. Primer for intensive care unit (ICU) redeployment of the noncritical care surgeon: insights from the epicenter of the coronavirus disease 2019 (COVID-19) pandemic. Surgery. 2020;168:215–217. doi: 10.1016/j.surg.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]