Abstract
The European Association of Cardiothoracic Anaesthesiology (EACTA) and the Society of Cardiovascular Anesthesiologists (SCA) aimed to create joint recommendations for the perioperative management of patients with suspected or proven severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection undergoing cardiac surgery or invasive cardiac procedures.
To produce appropriate recommendations, the authors combined the evidence from the literature review, reevaluating the clinical experience of routine cardiac surgery in similar cases during the Middle East Respiratory Syndrome (MERS-CoV) outbreak and the current pandemic with suspected coronavirus disease 2019 (COVID-19) patients, and the expert opinions through broad discussions within the EACTA and SCA. The authors took into consideration the balance between established procedures and the feasibility during the present outbreak. The authors present an agreement between the European and US practices in managing patients during the COVID-19 pandemic.
The recommendations take into consideration a broad spectrum of issues, with a focus on preoperative testing, safety concerns, overall approaches to general and specific aspects of preparation for anesthesia, airway management, transesophageal echocardiography, perioperative ventilation, coagulation, hemodynamic control, and postoperative care.
As the COVID-19 pandemic is spreading, it will continue to present a challenge for the worldwide anesthesiology community. To allow these recommendations to be updated as long as possible, the authors provided weblinks to international public and academic sources providing timely updated data.
This document should be the basis of future task forces to develop a more comprehensive consensus considering new evidence uncovered during the COVID-19 pandemic.
Key Words: COVID-19; SARS CoV 2; cardiac anesthesia; cardiac surgery; recommendations; PPE, safety; safety
IN DECEMBER 2019, a novel coronavirus-related disease outbreak was reported in the China province of Hubei, presenting most of the time as a “flu-like” illness. Twenty percent of the infected patients had mild symptoms such as fever or chills, headache, new loss of taste, nasal congestion, sore throat, nausea or vomiting, and diarrhea; and in severe cases, respiratory insufficiency occurred, and eventually acute respiratory distress syndrome (ARDS) necessitating respiratory support and invasive ventilation [click here].
The virus rapidly was identified and classified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease it causes is now called "coronavirus disease 2019 (COVID-19)", with a potential death rate of the infected currently monitored by the Johns Hopkins University [click here], mainly depending on age and underlying comorbidities.
For its elevated contagiousness (R0, the reproduction number of transmitted infections to new people >two) and the fact that asymptomatic carriers played a crucial role in spreading, COVID-19 in late February 2020 rapidly proliferated to South Korea and Italy.
Massive disruptions in public services forced the governments to impose drastic restrictions on social and economic life to prevent the collapse of healthcare systems and death.
As of March 2020, the infection gained a new dark primacy as it was declared a pandemic by the World Health Organization, causing the infection of millions of people and hundreds of thousands of deaths worldwide.1 The second surge of COVID-19 is affecting different worldwide countries, mainly in Europe and the United States. Imposed restrictions to prevent the spread of COVID-19 infection have resulted in delays in the perioperative care of patients requiring cardiovascular procedures, and healthcare units providing high levels of inpatient care (such as intensive care units [ICUs]) have been stretched beyond capacity in many places throughout the world.
Because the virus is believed to disseminate through aerosolized droplets diffused in the environment by coughing, sneezing, or talking, many healthcare workers have become infected, especially during maneuvers leading to aerosol generation.2 , 3
There are several published consensus statements4, 5, 6 and joint recommendations on the perioperative management of COVID-19 patients during different varieties of surgery.7 , 8 EACTA and SCA believe that it was important to develop this joint consensus for the perioperative management of patients undergoing cardiac surgery and minimally invasive cardiac interventions during the COVID-19 pandemic, based on the best evidence available until now. First, this consensus could serve as a guide to cardiac anesthesiologists in light of continuing cardiovascular care delivery services during the evolving second and, perhaps, subsequent waves of COVID-19. Second, this document provided a foundation for future task forces to develop a more comprehensive consensus considering new evidence uncovered during the COVID-19 pandemic [click here].
Methods
The principal methodologies to produce these recommendations included expert opinions through broad discussions within EACTA and SCA, reevaluating the clinical experience of routine cardiac surgery in similar cases during the Middle East Respiratory Syndrome (MERS- CoV) outbreak and the current pandemic with suspected COVID-19 patients, and reviewing the literature and public institutional and academic sources. Because the COVID-19 situation is very fluid, the authors aimed to avoid this document being outdated in a short period by providing web links to the public sources so that the information herein provided could remain “live” for the anesthesiology community as long as the sources were updated. A complete list of the web links is provided in Supplemental Table 1.
Literature Review
The authors performed a literature review for direct and indirect evidence on the management of COVID-19, SARS, MERS-CoV, and H1N1 patients. Major databases—MEDLINE, Embase, and Google Scholar—were explored to identify recent consensus recommendations, guidelines, relevant systematic reviews, randomized controlled trials, observational studies, and case series. These electronic searches were performed looking for studies published in English from inception to February 6, 2021. The authors used recently published articles to implement airway management recommendations and asked the expert panel to identify any new relevant studies. Publicly accessible sources relevant to the COVID-19 pandemic, such as WHO, universities, and scientific societies websites, were linked and displayed as a [click here] tag throughout the document.
Recommendation Formulation
The authors realize that there are important variations in the healthcare system structure between European and US centers. Thus, the authors present an agreement between both the European and US practice in managing patients during the COVID-19 pandemic, and these recommendations were considered best practices as of the completion of this manuscript's writing on February 6, 2021.
The group considered a broad spectrum of issues regarding cardiac anesthesia in patients who are suspected or diagnosed to have COVID-19 infection and decided to focus on overall approaches to general and specific aspects (Table 1 ) of preparation for cardiac anesthesia, airway management, perioperative ventilation, coagulation, and hemodynamic control and postoperative intensive care.
Table 1.
Areas Covered by EACTA/SCA Recommendations
| Hospital and Pathway Planning |
|---|
| Protection of healthcare providers |
| Protection of the patient |
| Transcatheter approaches |
| Postoperative management |
Abbreviation: EACTA/SCA, European Association of Cardiothoracic Anaesthesiology/Society of Cardiovascular Anesthesiologists.
To produce appropriate recommendations, the authors combined the evidence from the literature and expert opinions. The recommendations considered safety concerns for patients and healthcare providers, the balance between established procedures, and the feasibility during the present outbreak. As the goal was to make this preliminary consensus rapidly available to all cardiac surgical teams, the authors acknowledge the adopted methodology's limitations.
Disclaimer: The information set forth herein is not intended to replace the considered judgment of a licensed professional with respect to patients, procedures, or practices. The information found in this document may not be appropriate for all patients, and neither the EACTA, the SCA, nor the individual contributors make any warranty, guarantee, or other representation, express or implied, with respect to their fitness for any particular purpose.
All statements that are not specifically referenced are based on expert opinion.
Hospital and Pathway Planning
The hospital organization should provide separate perioperative pathways for non–COVID-19 and COVID-19–positive patients.9 These pathways apply also to patients transferred from other institutions.
-
•
Every patient should be screened clinically10 and virologically for SARS-CoV-2 infection. The current practice is to collect a specimen from the pharyngeal or nasal mucosa with a swab to confirm the virus's presence with polymerase chain reaction (PCR) quantification to reveal the viral genome. [click here]. Testing should be performed as close to surgery as possible (preferably fewer than 48 hours) to decrease the risk that a patient becomes positive while waiting for the surgical procedure.11
-
•
When dealing with positive-tested COVID-19 patients, hospital planning and organization should consider if surgery is emergent or elective [click here].
-
•
The authors recommend that in cardiac patients with clinical symptoms suggestive of infection with SARS-CoV-2 (eg, cough, fever) and a negative PCR test result, a computerized chest tomography (CT) is performed.12
-
•
Suppose surgery is urgent and necessary in a patient with suspected or confirmed infection found before proceeding to the operating room. In that case, providers should ensure that appropriate perioperative care units are notified and plans established to care safely for patients with known or suspected COVID.9
-
•
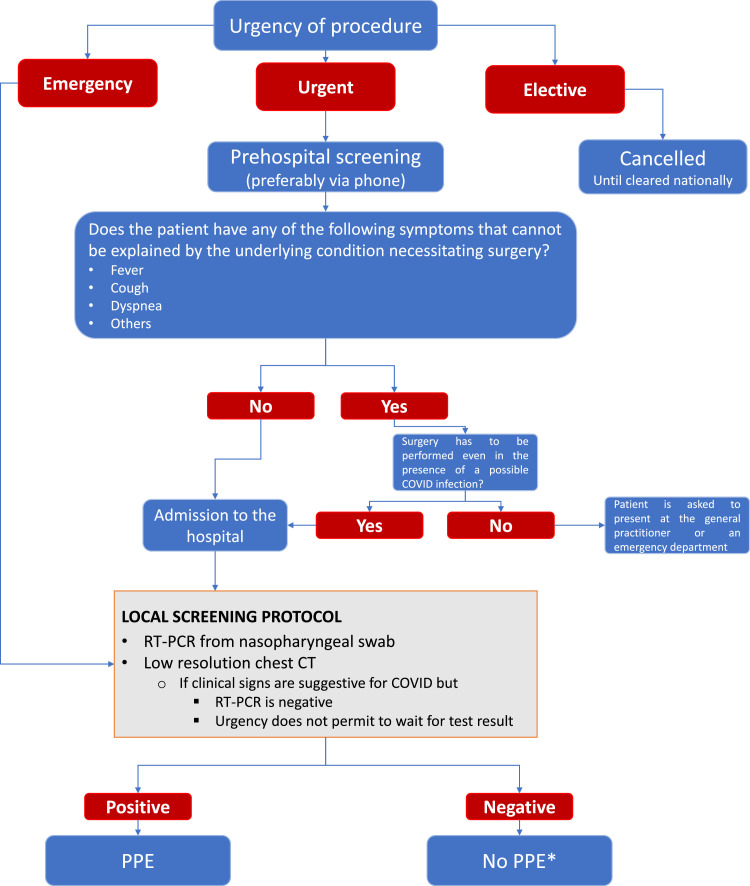
Symptomatic patients with urgent or emergent indications for cardiac surgery and CT signs suspected for COVID-19 should be considered COVID-19-positive even in the presence of a negative PCR test result (Fig 1 ). [click here] In patients undergoing surgery after contracting coronavirus, the Centers for Disease Control and Prevention (CDC) advises that retesting patients is no longer a recommended approach, but a clinical evaluation based on time passed since symptom onset, last fever, and improvement of symptoms should be applied [click here].
Fig 1.
A systematic approach to preoperative testing. Abbreviations: CT, computerized scanning; PPE, personal protective equipment; RT-PCR, reverse transcription-polymerase chain reaction. *Given the very high rate of asymptomatic carriers and that various types of COVID tests are used throughout the world with different sensitivities/specificities, with false negatives periodically occurring, anesthesiologists should remain vigilant and wear PPE during aerosol-generating procedures.
Postoperative Care
-
•
After a patient is transferred, the breathing circuit should be discarded.
-
•
The soda-lime canister and airway breathing system (ABS)/airway generation system (AGS) of the ventilator should be decontaminated according to the manufacturers’ recommendations.
-
•
All consumables should be discarded.
-
•
All reusable materials should be sent for decontamination according to the manufacturers’ recommendations.
-
•
A waiting period of 20 minutes is necessary to disinfect the operating room, all uncovered surfaces including the ABG, ACT, thrombelastography machines, TEE and CPB machines, and OR table using 3% - 5% chlorine solution, or plastic covers should be exchanged.
Protection of Healthcare Providers
Operating Room and Equipment Management
-
•
Ideally, a dedicated COVID-19 operating room with negative pressure and >12 air cycles/hour should be used for cardiac surgery.
-
•
In rooms with positive pressure, the pressure should be set at the lowest level assuring adequate air treatment. The doors should be kept closed so that the high exchange rate of air in operating rooms limits aerosols’ dispersion outside the room, despite the airflow directed from inward to outward.
-
•
During surgery, the operating room temperature level should be reduced to 18°-to-20°,13 and humidity is kept between 40% and 60%.14
-
•
A closed system for tracheal suction should be used.
-
•
Transesophageal echocardiography and anesthesia machines, computers, ABG, ACT, bedside coagulation POC instruments, etc, could be covered with disposable transparent plastic sheets.
-
•
The breathing circuit should be checked as a standard practice. Antiviral filters, such as the high-efficiency particulate air (HEPA) or heat and moisture exchanger (HME) filters, should be attached between the face mask/tracheal tube and the Y-shaped connector and at the expiratory outlet of the breathing circuit. The CO2 sample line should remain near the Y-connector proximal to the ventilator to avoid contamination.
Staff Planning
Inside the room, preferably there might be three staff members, including the most experienced cardiac anesthesiologist to intubate the patient's trachea; a second doctor should be present for unanticipated difficulty, and a circulating nurse or anesthesia assistant/technician should help to administer drugs and monitor the patient.
-
•
There must be a “runner” available directly outside the room in case of need for handling any equipment or medicines.
-
•
Surgeons, perfusionists, and scrub nurses should wait outside the room until the airway has been secured, ventilation started, and the TEE and esophageal temperature probes have been inserted
-
•
There should be a dedicated area outside the operating room in which the operators can safely doff the personal protective equipment (PPE), and an observer has to be present to monitor the process.
-
•
The room turnover should be minimized (ie, the same anesthesia personnel should remain in the operating room for the entirety of the case, if possible).
-
•
Due to a higher risk for the infection to become fatal, practitioners with significant vulnerability, including those aged >60 years, immunosuppressed, pregnant, or having multiple comorbidities, as described according to the WHO criteria, [click here] should have personal discussions within their work units, ultimately with decisions whether being included in the team operating on suspected or diagnosed COVID-19 patients made by them and their respective institutions.
-
•
Strengthening effective communications should be agreed on in advance, as the PPE renders information exchange among practitioners very difficult.
-
•In suspected or diagnosed patients, during aerosol-generating procedures (AGP); namely intubation, noninvasive ventilation (NIV) or continuous positive airway pressure (CPAP), bronchoscopy, and TEE, it is suggested to wear the following PPE, including: [click here]
-
○Hair cover/hood
-
○Well-fitted filtering mask (FFp3/N95/FFp2) or powered air-purifying respirator (PAPR) [click here]
-
○Goggles and/or face shield
-
○Long-sleeve, fluid-resistant gown or protective suit as directed by the local regulations and availability
-
○Double gloves
-
○Overshoes
-
○
-
•
Respecting the sequence for donning and especially doffing is crucial to avoid contamination. An example is shown in Table 2 . This process can be challenging, especially for inexperienced care providers; the authors recommend hospital institutions to organize and run frequent donning/doffing courses or simulations for personnel directly involved in the care of COVID-19 patients. Moreover, donning and doffing should be assisted by cognitive aids.
-
•
It is recommended that experienced personnel supervise donning and doffing.
-
•
Airway management should be performed by the most experienced staff available [click here].
-
•
The staff not immediately involved in airway management should not enter the operating room until after the airway has been secured.
-
•
After securing the airway, the regular contact and droplet precautions (longsleeves, fluid-resistant gown, gloves, N95 or surgical mask in case of shortages of N95, and eye protection using goggles or face shield) around suspected or COVID-19-positive patients should be worn by both anesthesiologists and surgeons during the entire surgical procedure.
-
•
All staff including surgeons, perfusionists, and nurses, must don PPE for all suspected or COVID-19–positive patients including masks (N95, FFP2), eye protection, double nonsterile gloves, gowns, and hair and shoe covers15 or as per the regularly updated WHO recommendations [click here]. These recommendations are extended to interventions done under sedation without securing the airway
Table 2.
Donning and Doffing Sequences of PPE
| Donning PPE | Doffing PPE |
|---|---|
| Hand hygiene | Remove shoe covers |
| Inner gloves | Remove gown |
| Hand hygiene | Remove outer glove |
| Hair covers /hood | Hand hygiene |
| Shoe covers | Remove eye protection |
| Gown | Remove mask |
| Mask fit check | Remove hair covers/hood |
| Eye protection: fit check again | Remove inner glove |
| Hand hygiene + outer glove | Hand hygiene |
NOTE. Modified from https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf.
Abbreviation: PPE, personal protective equipment.
Staff Welfare
-
•
Operating on COVID-19 patients is likely to be a long-lasting procedure and emotionally demanding. Psychological counseling should be available virtually, if possible16 [click here].
-
•
Staff should consider their hydration and use of the toilet before starting the long cases.
-
•
Staff should be given appropriate break time before the next cases.
-
•
Urgent further cases may be best performed by a new team, if possible.
Protection of the Patient
Thrombosis Prophylaxis in the Perioperative Period
-
•
Patients with COVID-19 infection demonstrated a high number of arterial and venous thromboembolic events in 7.7% of hospitalized patients (cumulative rate of 21.0%) diagnosed within 24 hours of admission.17 Many institutions apply thrombosis prophylaxis with high prophylactic doses, eg, enoxaparin two times 40 mg/day under anti-Xa activity monitoring.18 Currently, there is no consensus on the ideal anticoagulant or appropriate dose [click here].
-
•
Strict application of pharmacologic thrombosis prophylaxis is recommended for all suspected or diagnosed COVID-19 patients admitted to the ICU either preoperatively or after surgery in the absence of bleeding.
-
•
All doses of anticoagulants may need adjustments based on renal function, mainly in patients who experienced acute kidney injury during noninvasive ventilation during the preoperative period. Caution should be exercised when the platelets fall below than 30,000/μmL for prophylaxis or below 50,000/μmL for therapeutic heparin.
-
•
Bleeding events are observed in 7.8% of patients with COVID-19 infection, which are sensitive to the use of escalated doses of anticoagulants.19 Point-of-care monitoring of coagulation, including thromboelastography,20 can be considered to manage hemostasis in the perioperative period.
Preparation for Tracheal Intubation
-
•
Preparing a dedicated cart is recommended for tracheal intubation of the suspected or confirmed COVID-19-infected patient. Disposable devices (eg, single-use blades, single-use video laryngoscopes, laryngoscopes, video laryngoscopes with remote screens, front-of-neck airway/cricothyroidotomy access set, and disposable flexible bronchoscopes) should be preferred. Anesthesia induction and tracheal intubation in the COVID-19 patients undergoing cardiac surgery are high-risk procedures for the anesthetic team because of the risks of aerosol transmission of the infection during placement of the endotracheal tube.
-
•
The procedure should be safe for the operators and the patient and fast enough to minimize aerosol diffusion.
-
•
Before tracheal intubation, a complete evaluation of the airways and optimization of the patient's position, oxygenation, and hemodynamic status should be performed.
Preoxygenation
-
•
NIV or CPAP, reported being beneficial before intubation, especially in obese patients,21 can be considered to preoxygenate the patient only if the induction room is put in a negative-pressure environment.22 The Italian Society of Anesthesiology and Intensive Care (SIAARTI) suggests using a helmet as a less aerosol-generating interface, if available.23
-
•
Face mask ventilation should be avoided unless needed. If necessary, a two-person, low-flow/low-pressure technique should be used. A two-person, two-handed mask ventilation should be performed to improve the seal.
-
•
Another measure of adequate pre-oxygenation is to assess the fraction of exhaled oxygen (measured from the patient's exhaled breath) that should exceed 80%.
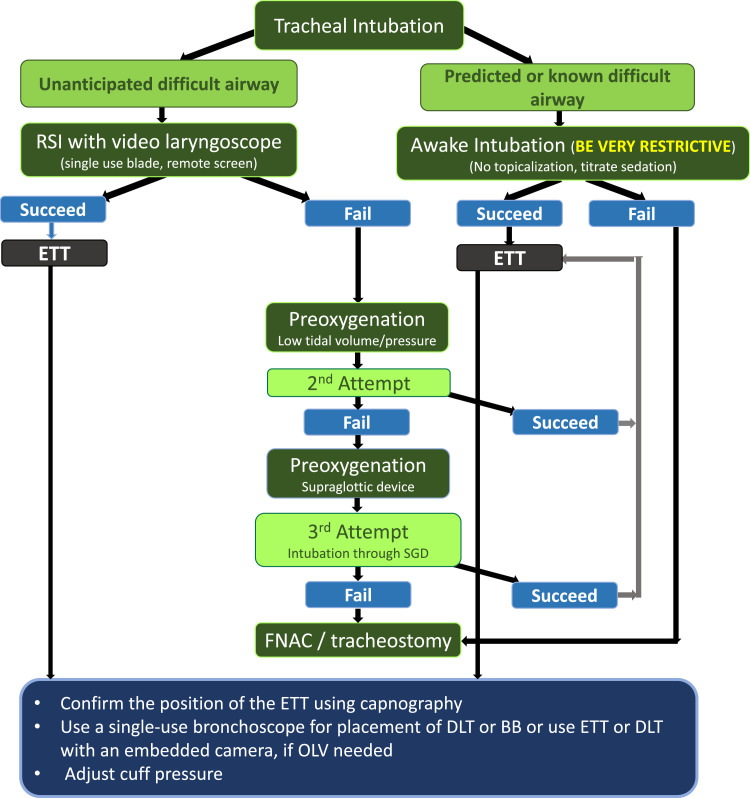
Tracheal Intubation (Fig 2)
Fig 2.
Systematic approach for tracheal intubation. Abbreviations: BB, bronchial blocker; DLT, double-lumen endobronchial tube; ETT, endotracheal tube; FNAC, front neck access; OLV, one lung ventilation; RSI, rapid-sequence induction.
-
•
Intubation preferably could be performed using a video laryngoscope with a remote screen to maximize the distance from the anesthesiologist and the patient's mouth and avoid aerosol transmission.23
-
•The unanticipated difficult airway should be treated similarly to ordinary patients as per institution practice or internal guidelines. The authors recommend the suggested approach by SIAARTI and UK joint societies23 , 24 as follows:
-
○The first laryngoscopy attempt should be performed with an endotracheal tube preloaded on a stylet.
-
○If it fails, a reoxygenation period can be needed, which has to be applied with a low-tidal- volume/pressure to avoid leakage of contaminated air.
-
○If a third attempt is necessary, an early switch to a second-generation intubating supraglottic airway device should be considered.25 Intubation through this device should be performed with a flexible (preferably disposable) endoscope, again with a separate remote screen.
-
○
-
•Anticipated difficult airway
-
○No aerosol or vaporization should be used for airway topical anesthesia.
-
○A titrated sedation with monitoring sedation depth has to be performed.23
-
○For intubation, a flexible (preferably disposable) endoscope with a separate remote screen should be used.
-
○Rescue intubation through a second-generation supraglottic airway device
-
○Surgical tracheostomy or cricothyrotomy can be necessary.
-
○Tracheal intubation should be confirmed with continuous-waveform capnography.
-
○
-
•Lung isolation for minimally invasive cardiac surgery
-
○In patients in whom lung isolation is necessary, as in minimally invasive cardiac surgery, the airway should be manipulated as infrequently as possible and all providers should maintain appropriate precautions and described previously.
-
○Appropriate sizes of double-lumen tubes, bronchial blocker, and fiberoptic bronchoscopes also should be ready and prepared.26
-
○Placement of a double-lumen tube can be the first choice for patients with no predicted airway difficulty intubated inside the OR.
-
○Bronchial blockers are recommended as the first choice for patients who arrive in the OR while already intubated.
-
○If a double-lumen tube is used, the position of the device could be confirmed with a disposable flexible bronchoscope using a swivel with a valve to maintain a better seal during the maneuver and, if possible, putting the ventilator on standby mode with pausing the gas flow to reduce the aerosolizing of contaminated air, while continuing to ventilate the other lumen.27 An HME filter should be placed on the clamped, not ventilated, lumen, which is open to the air, to facilitate lung collapse.26
-
○
After-Intubation Care
-
•
A nasogastric tube can be placed if needed.
-
•
If the diagnosis of COVID-19 is not already confirmed, a deep tracheal aspirate for virology should be taken using closed suction.
-
•
Esophageal temperature and TEE probes with adequate covers then should be inserted.
-
•
The patient should remain connected to the breathing circuit as much as possible.
-
•
A closed system with an infraglottic catheter tip should be positioned after tracheal intubation and used for suction.28 , 29
-
•
If discontinuation of the ventilation is needed, the ventilator should be placed in standby mode, and the endotracheal tube should be clamped. Before clamping the endotracheal tube, muscle relaxation should be confirmed such that the patient will not attempt to breathe against an occluded airway.
-
•
The PPE should be kept until the end of the surgery. Hand hygiene and changing the outer layer of the gloves must be performed before and after all patient contact.
-
•
Debriefing should be considered.
Ventilation Strategy
-
•
Intraoperative protective ventilation strategy may be warranted in asymptomatic positive SARS-CoV-2 patients, as they still are at risk for postoperative pulmonary complications.
-
•
In patients with diagnosed COVID-19 infection with pulmonary pathology and for whom surgery cannot be postponed, intraoperative and postoperative ventilation should be individualized based on lung mechanics to minimize further damage to the lungs and according to the recommendation of national and international societies of anesthesia and critical care: [click here for ESICM, SCCM, ASA, and ESA weblinks]. Recent findings in patients with COVID-19 pneumonia confirm the need for a tailored ventilatory strategy based on lung-compliance measurement.30
-
•EACTA recommendations on the intraoperative management of one-lung ventilation include26:
-
○The fraction of inspired oxygen of 100%
-
○A low tidal volume of 4-to-6 mL/kg of predicted body weight
-
○Some degree of hypercapnia can be permitted by adjusting the respiratory frequency (pH >7.2).
-
○Potentially, a higher PEEP may be required than that for a patient without COVID-19: approximately 13-to-15 cmH2O; a PEEP titration strategy is suggested but should be performed very cautiously so as not to cause a decrease in cardiac output in higher PEEP levels.
-
○Patients may benefit from the application of an alveolar recruitment maneuver, and a trial is recommended; it should be kept in mind, however, that the recruitment strategy can impair the hemodynamic stability in a more extended way than in “healthy” patients.
-
○
Some cardiac patients with suspected or confirmed COVID-19 infection are intubated before arrival in the OR. The same ventilation settings should be considered intraoperatively as much as possible. Transferring ventilated patients to the OR should follow the local institutional regulations by using either a portable ventilator or a self-inflating resuscitation bag with the ventilation settings used in the ICU. Viral filters are to be maintained on the patient throughout transportation.
Transesophageal Echocardiography [click here]31
-
•
TEE should be limited to selected patients; its application is based on a risk/benefit balance.
-
•
A focused transesophageal examination using a step-by-step approach should be considered.
-
•
The authors recommend that the TEE probe with an adequate cover is inserted only after endotracheal intubation.32
-
•
If not used, the TEE probe should be available in the room as it could be necessary as a subsequent step or aid during unexplained hemodynamic instability.
-
•
After the examination is concluded, the probe and machine's proper disinfection are mandatory, as recommended by the manufacturers.
Special Recommendations for Transcatheter Approaches
-
•
In the case of a suspected or diagnosed COVID-19 patient with structural heart disease amenable to a transcatheter procedure, a multidisciplinary team discussion among the cardiac anesthesiologist, surgeons, and interventional cardiologist is advocated, as the majority of procedures (eg, transcatheter aortic valve implantation/replacement (TAVI/TAVR) might not be recommended for the elderly comorbid COVID-19 patient.
-
•
For transcatheter procedures, the authors recommend the same level of PPE for the operators as in the operating room, independent of the type of anesthesia technique applied.
-
•
It has been debated which anesthesia technique, sedation or general anesthesia (GA), is better, especially for fragile patients, and the most recent investigations seem to favor light sedation with local anesthesia and avoidance of tracheal intubation.33
-
•
For GA, either a laryngeal mask airway (LMA) or tracheal intubation might be considered.34
-
•
In patients undergoing procedures under sedation with an unprotected airway, the clinicians should take into consideration the risk of aerosolization from the various methods of delivering supplemental oxygen (nasal cannula, high-flow nasal cannula, nonrebreathing face mask, etc).35 Hudson and Venturi masks, nasal cannulae, and helmets carry a lower risk of transmission when compared with high-flow nasal oxygen (HFNO) and noninvasive ventilation with facemasks or hoods.23
-
•
Several noninvasive options are available for respiratory support, including HFNO, CPAP, or NIV. Data from the SARS36 and MERS-CoV37 outbreaks cautioned against the use of HFNO35 or noninvasive ventilation, although this recently has been questioned by data demonstrating no increased dissemination of bacteria with HFNO, yet viral spread has remained unexplored .38
-
•
If a nonintubation procedure is considered, the authors recommend that the patient wear a surgical mask to avoid environmental contamination and reduce the risk of contagion for healthcare providers who should wear full PPE. A local protocol including early mobilization, accelerated reconditioning, and early discharge planning should be developed.39
Recommendation After Cardiac Surgery: Extubation
Indications for Extubation
-
•
Multidisciplinary discussions involving cardiac anesthesiologists, surgeons, and intensivists should be considered to define the feasibility of immediate extubation of patients after surgery if that is the local practice at the center and in case of drained resources in terms of shortages of ICU beds.
-
•
In general, patients with suspected and confirmed COVID-19 diagnosis should be left intubated and ventilated after surgery, particularly those who already were intubated before surgery, patients with COVID-19 pneumonia with low Pao 2/Fio 2 ratio, or those with an anticipated or unanticipated airway difficulty.
Extubation Procedures
-
•
The patient should meet all criteria for extubation after cardiac surgery.
-
•
Extubation is an AGP; thus, two staff members should stay in PPE during recovery and extubation.
-
•
It has been reported that the patients usually have excessive retained secretions, especially during the weaning phase, with increased risks for the need for reintubation.30 Gentle suctioning through a closed suction circuit (eg, suction through a 15-mm swivel connector or a tracheal tube with a subglottic suction port) or pausing the flow by switching the ventilator to “standby mode” should be considered before extubation, without precipitating cough. An alveolar recruitment maneuver could follow.26
-
•
Some drugs (eg, dexmedetomidine, lidocaine, magnesium sulfate) can decrease the risks for coughing during and after extubation, with dexmedetomidine being the most effective pharmaceutical strategy.40
-
•
Gas flow to the surrounding area should be minimized as much as possible. Patients immediately should be put on a facemask with oxygen (eg, Venturi, Hudson, or nonrebreathing masks with the lowest possible gas flow) and wear a standard surgical mask over it.41
-
•
AGP, such as noninvasive ventilation (NIV) or high-flow nasal oxygen (HFNO), should be avoided, if possible. Otherwise, a negative-pressure environment should be available, or a high level of PPE should be considered.
-
•
Barriers to limit environmental aerosolization during extubation can be used as reported in the literature.42
A dedicated elevator/lifter for the COVID-19 patients should be used with the corridors’ cleared for one meter from other personnel by an accompanying person without PPE. [click here]
Destination After Transferring
-
•
After completing surgery, the patient usually is transferred to a dedicated ICU for COVID-19 patients in case of a proven or suspected COVID-19 infection.
-
•
COVID-19 patients with no available dedicated ICU beds for COVID-19 preliminarily could remain in the operating room in which routine care after cardiac surgery should be provided with donning the routine PPE levels previously described.
Transferring Intubated Patients
-
•
Transferring patients with COVID-19 pneumonia could be challenging due to the difficulty of maintaining the required ventilation settings as previously described.
-
•
A HEPA or HME viral filter should be connected between the tracheal tube and the portable ventilator or self-inflating resuscitation bag.
-
•
Using a portable ventilator allowing to adjust FiO2, tidal volume, and PEEP levels is recommended.
-
•
Otherwise, ventilation using a resuscitation bag and valve can be considered by incorporating an antiviral filter and reservoir to minimize the aerosol transmission risks.
-
•
Airway disconnections should be minimized and the tracheal tube clamped when possible.
Transferring Freshly Extubated Patients
-
•
Transferring extubated patients should follow the local regulations.
-
•
Gas flow to the surrounding area should be minimized as much as possible by using a surgical or N95 mask over the patient's mouth41 and nose or using a Coronavirus Safety during Intubation and Extubation (COSIE) COVID-19 aerosol box.43
-
•
Patients should be transferred with a facemask with oxygen, if needed, (eg, Venturi, Hudson, or nonrebreather masks with the lowest possible gas flow).
Patients undergoing surgery after contracting coronavirus are at greatly increased risk of postoperative cardiovascular (myocarditis, cardiogenic shock, vasoplegic shock, acute coronary syndrome, right ventricular dysfunction/failure)9 , 44 , 45 and pulmonary complications, thrombotic events18 and death.3
-
•
Postoperative care of intubated and extubated COVID-19 patients after cardiac surgery, including rewarming, hemodynamic stabilization, and bleeding control, should follow the clinical judgment and be consistent with the standard of care.
-
•
Ventilation strategy and hemodynamic considerations: see previously noted recommendations.
-
•
Personnel should wear the low PPE level as previously recommended except for aerosol-generating procedures in which a high-level PPE should be donned.
Hemodynamic Considerations
Myocarditis and Cardiogenic Shock
-
•
Patients with severe COVID-19 may present with cardiogenic shock secondary to myocarditis and/or pericarditis.45 That could be associated with significant ST-segment changes, increased serum levels of cardiac troponin and brain natriuretic peptides (BNP), and severe hypokinesia.46 Elevations in troponin levels have been shown to predict mortality in patients with COVID-19.47
-
•
Preoperative hemodynamic control should be considered using either pharmacologic (eg, inotropes, vasopressors, or angiotensin II) or mechanical circulatory support (eg, venoarterial extracorporeal membrane oxygenation [VA-ECMO] or Impella).
Vasoplegic Shock
-
•
Patients with COVID-19 infection might present preoperatively with vasoplegic shock secondary to sepsis (10% to 15%) and/or disordered function of the renin-angiotensin-aldosterone system.44 , 48 That should be taken into account during preoperative assessment, emphasizing conduction abnormalities, the presence of acute kidney injury, and correction of electrolyte and pH disturbances [click here].
-
•
Recommendation and updates of Surviving Sepsis Campaign guidelines for fluid therapy, ventilation, and hemodynamic support of critically ill COVID-19 patients should be followed49 [click here].
Acute Coronary Syndrome
-
•
Acute coronary arteritis might be a clinical feature of COVID-19.
-
•
Patients with COVID-19 infection are at increased risk of thrombosis of coronary stents, which require emergency coronary angiography for diagnosis and management.45
-
•
Right ventricular dysfunction is common in COVID-19 patients, with an estimated prevalence of 25% to 50%.45
-
•
Preoperative optimization of right ventricular function, with the possible use of inhaled nitric oxide50 or inhaled epoprostenol or milrinone, may be considered in these patients. The viral filter should be positioned appropriately to limit contamination of inhaled medication delivery systems.
In-hospital cardiopulmonary resuscitation should follow the precautions provided by the American Heart Association [click here].
Conclusions
As the COVID-19 pandemic is spreading, it will continue to represent a challenge for the worldwide anesthesiology community, and, most likely, the authors all will need to deal with it at some point in the future.
This document provided recommendations on hospital and staff planning, safety, and protection of healthcare providers and patients, management of transcatheter approaches, and postoperative management and care. Further, the authors provided focused considerations on major hemodynamic and thrombotic complications related to COVID-19.
The authors sincerely hope that these recommendations will be of help in everyday clinical practice.
Conflict of Interest
None.
Footnotes
This document was reviewed by the members of the European Association of Cardiothoracic Anaesthesiology (EACTA) Board of Directors, Society of Cardiovascular Anesthesiologists (SCA) Guidelines and Standards Subcommittee, SCA Board of Directors, and SCA Executive Committee, and endorsed by the Chinese Society of Cardiothoracic and Vascular Anesthesiology (CSCTVA).
The SCA Guidelines and Standards Subcommittee reviewers included: Michael Boisen (Chair), Bruce Bollen, Shiva Sale, Theodore Cios, Thomas Gentilcore, Jonathan Zoller, Dmitri Vladinov, and Marco Aguirre.
Supplementary material associated with this article can be found, in the online version, at doi:10.1053/j.jvca.2021.02.039.
Appendix. Supplementary materials
References
- 1.Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036. [DOI] [PubMed] [Google Scholar]
- 2.Lancet The. COVID-19: Protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng H, Hébert HL, Chatziperi A, et al. Perioperative management of patients with suspected or confirmed COVID-19: Review and recommendations for perioperative management from a retrospective cohort study. Br J Anaesth. 2020;125:895–911. doi: 10.1016/j.bja.2020.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeng H, Li G, Weng J, et al. The strategies of perioperative management in orthopedic department during the pandemic of COVID-19. J Orthop Surg Res. 2020;15:474. doi: 10.1186/s13018-020-01978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solanki SL, Thota RS, Garg R, et al. Society of Onco-Anesthesia and Perioperative Care (SOAPC) advisory regarding perioperative management of onco-surgeries during COVID-19 pandemic. Indian J Anaesth. 2020;64(Suppl 2):S97–102. doi: 10.4103/ija.IJA_447_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaylor R, Verenkin V, Matot I. Anesthesia for patients undergoing anesthesia for elective thoracic surgery during the COVID-19 pandemic: A consensus statement from the Israeli Society of Anesthesiologists. J Cardiothorac Vasc Anesth. 2020;34:3211–3217. doi: 10.1053/j.jvca.2020.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He Y, Wei J, Bian J, et al. Chinese Society of Anesthesiology expert consensus on anesthetic management of cardiac surgical patients with suspected or confirmed coronavirus disease 2019. J Cardiothorac Vasc Anesth. 2020;34:1397–1401. doi: 10.1053/j.jvca.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donatelli F, Miceli A, Glauber M, et al. Adult cardiovascular surgery and the coronavirus disease 2019 (COVID-19) pandemic: The Italian experience. Interact Cardiovasc Thorac Surg. 2020;31:755–762. doi: 10.1093/icvts/ivaa186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel V, Jimenez E, Cornwell L, et al. Cardiac surgery during the coronavirus disease 2019 pandemic: Perioperative considerations and triage recommendations. J Am Heart Assoc. 2020;9 doi: 10.1161/JAHA.120.017042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Engelman DT, Lother S, George I, et al. Adult cardiac surgery and the COVID-19 pandemic: Aggressive infection mitigation strategies are necessary in the operating room and surgical recovery. J Thorac Cardiovasc Surg. 2020;160:447–451. doi: 10.1016/j.jtcvs.2020.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shao JM, Ayuso SA, Deerenberg EB, et al. A systematic review of CT chest in COVID-19 diagnosis and its potential application in a surgical setting. Colorectal Dis. 2020;22:993–1001. doi: 10.1111/codi.15252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He H, Zhao S, Han L, et al. Anesthetic management of patients undergoing aortic dissection repair with suspected severe acute respiratory syndrome COVID-19 Infection. J Cardiothorac Vasc Anesth. 2020;34:1402–1405. doi: 10.1053/j.jvca.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quraishi SA, Berra L, Nozari A. Indoor temperature and relative humidity in hospitals: Workplace considerations during the novel coronavirus pandemic. Occup Environ Med. 2020;77:508. doi: 10.1136/oemed-2020-106653. [DOI] [PubMed] [Google Scholar]
- 15.Tan L, Kovoor JG, Williamson P, et al. Personal protective equipment and evidence-based advice for surgical departments during COVID-19. ANZ J Surg. 2020;90:1566–1572. doi: 10.1111/ans.16194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muller AE, Hafstad EV, Himmels JPW, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiménez D, García-Sanchez A, Rali P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: A systematic review and meta-analysis [e-pub ahead of print] Chest. 2021 doi: 10.1016/j.chest.2020.11.005. Accessed February 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo Z, Sun L, Li B, et al. Anticoagulation management in severe coronavirus disease 2019 patients on extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2021;35:389–397. doi: 10.1053/j.jvca.2020.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gedeon M, Gomes S, Roy K, et al. Use of noninvasive positive pressure ventilation in patients with severe obesity undergoing esophagogastroduodenoscopy: A randomized controlled trial. Surg Obes Relat Dis. 2019;15:1589–1594. doi: 10.1016/j.soard.2019.06.027. [DOI] [PubMed] [Google Scholar]
- 22.Fogarty M, Kuck K, Orr J, et al. A comparison of controlled ventilation with a noninvasive ventilator versus traditional mask ventilation. J Clin Monit Comput. 2020;34:771–777. doi: 10.1007/s10877-019-00365-1. [DOI] [PubMed] [Google Scholar]
- 23.Sorbello M, El-Boghdadly K, Di Giacinto I, et al. The Italian coronavirus disease 2019 outbreak: Recommendations from clinical practice. Anaesthesia. 2020;75:724–732. doi: 10.1111/anae.15049. [DOI] [PubMed] [Google Scholar]
- 24.Cook TM, El-Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020;75:785–799. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chae YJ, Lee H, Jun B, et al. Conversion of I-gel to definitive airway in a cervical immobilized manikin: Aintree intubation catheter vs long endotracheal tube. BMC Anesthesiology. 2020;20:152. doi: 10.1186/s12871-020-01069-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Şentürk M, El Tahan MR, Szegedi LL, et al. Thoracic anesthesia of patients with suspected or confirmed 2019 novel coronavirus infection: Preliminary recommendations for airway management by the European Association of Cardiothoracic Anaesthesiology Thoracic Subspecialty Committee. J Cardiothorac Vasc Anesth. 2020;34:2315–2327. doi: 10.1053/j.jvca.2020.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tryphonopoulos P, McFaul C, Gagne S, et al. COVID-19 and one-lung ventilation. Anesth Analg. 2020;131:e90–e91. doi: 10.1213/ANE.0000000000004915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brewster DJ, Chrimes N, Do TB, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020;212:472–481. doi: 10.5694/mja2.50598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rasmussen SA, Smulian JC, Lednicky JA, et al. Coronavirus disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am J Obstet Gynecol. 2020;222:415–426. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicoara A, Maldonado Y, Kort S, et al. Specific considerations for the protection of patients and echocardiography service providers when performing perioperative or periprocedural transesophageal echocardiography during the 2019 novel coronavirus outbreak: Council on Perioperative Echocardiography supplement to the statement of the American Society of Echocardiography endorsed by the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2020;33:666–669. doi: 10.1016/j.echo.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Markin NW, Cawcutt KA, Sayyed SH, et al. Transesophageal echocardiography probe sheath to decrease provider and environment contamination. Anesthesiology. 2020;133:475–477. doi: 10.1097/ALN.0000000000003370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harjai KJ, Bules T, Berger A, et al. Efficiency, safety, and quality of life after transcatheter aortic valve implantation performed with moderate sedation versus general anesthesia. Am J Cardiol. 2020;125:1088–1095. doi: 10.1016/j.amjcard.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 34.Azad SS, Cobey FC, Price LL, et al. Supraglottic airway use for transfemoral-transcatheter aortic valve replacement. J Cardiothorac Vasc Anesth. 2020;34:3243–3249. doi: 10.1053/j.jvca.2020.04.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haymet A, Bassi GL, Fraser JF. Airborne spread of SARS-CoV-2 while using high-flow nasal cannula oxygen therapy: Myth or reality? Intensive Care Med. 2020;46:2248–2251. doi: 10.1007/s00134-020-06314-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568–576. doi: 10.1007/s12630-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alraddadi BM, Qushmaq I, Al-Hameed FM, et al. Noninvasive ventilation in critically ill patients with the Middle East respiratory syndrome. Influenza Other Respir Viruses. 2019;13:382–390. doi: 10.1111/irv.12635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leung CCH, Joynt GM, Gomersall CD, et al. Comparison of high-flow nasal cannula versus oxygen face mask for environmental bacterial contamination in critically ill pneumonia patients: A randomized controlled crossover trial. J Hosp Infect. 2019;101:84–87. doi: 10.1016/j.jhin.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 39.Lauck S, Forman J, Borregaard B, et al. Facilitating transcatheter aortic valve implantation in the era of COVID-19: Recommendations for programmes. Eur J Cardiovasc Nurs. 2020;19:537–544. doi: 10.1177/1474515120934057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tung A, Fergusson NA, Ng N, et al. Medications to reduce emergence coughing after general anaesthesia with tracheal intubation: A systematic review and network meta-analysis [e-pub ahead of print] Br J Anaesth. 2021 doi: 10.1016/j.bja.2019.12.041. Accessed February 28. [DOI] [PubMed] [Google Scholar]
- 41.Binks AC, Parkinson SM, Sabbouh V. Oxygen: Under or over a surgical facemask for COVID-19 patients? Anaesthesia. 2020;75:1691–1692. doi: 10.1111/anae.15166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sorbello M, Rosenblatt W, Hofmeyr R, et al. Aerosol boxes and barrier enclosures for airway management in COVID-19 patients: A scoping review and narrative synthesis. Br J Anaesth. 2020;125:880–894. doi: 10.1016/j.bja.2020.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leyva Moraga FA, Leyva Moraga E, Leyva Moraga F, et al. Aerosol box, an operating room security measure in COVID-19 pandemic. World J Surg. 2020;44:2049–2050. doi: 10.1007/s00268-020-05542-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiong T-Y, Redwood S, Prendergast B, et al. Coronaviruses and the cardiovascular system: Acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Augoustides JG. Cardiovascular consequences and considerations of coronavirus infection—Perspectives for the cardiothoracic anesthesiologist and intensivist during the coronavirus crisis. J Cardiothorac Vasc Anesth. 2020;34:1713–1716. doi: 10.1053/j.jvca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao B-C, Liu W-F, Lei S-H, et al. Prevalence and prognostic value of elevated troponins in patients hospitalised for coronavirus disease 2019: A systematic review and meta-analysis. J Intensive Care. 2020;8:88. doi: 10.1186/s40560-020-00508-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Majure DT, Gruberg L, Saba SG, et al. Usefulness of elevated troponin to predict death in patients with COVID-19 and myocardial injury. Am J Cardiol. 2021;138:100–106. doi: 10.1016/j.amjcard.2020.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chow JH, Mazzeffi MA, McCurdy MT. Angiotensin II for the treatment of COVID-19–Related vasodilatory shock. Anesth Analg. 2020;131:102–105. doi: 10.1213/ANE.0000000000004825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alhazzani W, Evans L, Alshamsi F, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: First update. Crit Care Med. 2021;49:e219–e234. doi: 10.1097/CCM.0000000000004899. [DOI] [PubMed] [Google Scholar]
- 50.Heuts S, Ubben JF, Banks-Gonzales V, et al. Nitric oxide ventilation improves recirculation and right ventricular function during veno-venous extracorporeal membrane oxygenation in a COVID-19 patient [e-pub ahead of print] J Cardiothorac Vasc Anesth. 2021 doi: 10.1053/j.jvca.2020.09.137. Accessed February 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.