Abstract
Background
The complete contact tracing of coronavirus disease-19 (COVID-19) cases in South Korea allows a unique opportunity to investigate cluster characteristics. This study aimed to investigate all reported COVID-19 clusters in the Seoul metropolitan area from January 23 to September 24, 2020.
Methods
Publicly available COVID-19 data was collected from the Seoul Metropolitan City and Gyeonggi Province. Community clusters with ≥5 cases were characterized by size and duration, categorized using K-means clustering, and the correlation between the types of clusters and the level of social distancing investigated.
Results
A total of 134 clusters comprised of 4033 cases were identified. The clusters were categorized into small (type I and II), medium (type III), and large (type IV) clusters. A comparable number of daily reported cases in different time periods were composed of different types of clusters. Increased social distancing was related to a shift from large to small-sized clusters.
Conclusions
Classification of clusters may provide opportunities to understand the pattern of COVID-19 outbreaks better and implement more effective suppression strategies. Social distancing administered by the government may effectively suppress large clusters but may not effectively control small and sporadic clusters.
Keywords: COVID-19, Cluster, Type, Contact tracing, Social distancing, Republic of Korea
Introduction
In the week before October 27, 2020, an exponential increase in the number of new weekly coronavirus disease-19 (COVID-19) cases was reported worldwide, with over 2.8 million new cases and approximately 40 000 deaths (WHO, 2020). As of October 27, a cumulative total of >42 million COVID-19 cases and 1.1 million deaths had been reported worldwide (WHO, 2020); among these, a total of 22 364 cases and 460 deaths were reported in South Korea (Korea Disease Control and Prevention Agency, 2020). During the initial COVID-19 epidemic phase in South Korea from February to March 2020, a massive outbreak in Daegu accounted for the majority of cases, whereas cases in the Seoul metropolitan area were not prominent, despite outbreaks at the Guro-gu customer service call center and Itaewon night clubs (Jung et al., 2020, Park et al., 2020). However, from mid-August, daily new cases in the Seoul metropolitan area increased dramatically, reaching 200-300 daily reported cases from large outbreaks in churches and the National Liberation Day rally on August 15. From mid-August to late September, most new COVID-19 cases have occurred in the Seoul metropolitan area.
To contain the spread of COVID-19, it is crucial to understand the circumstances under which the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is transmitted (i.e. setting and activities) and the measures available to reduce the spread of the disease. During the early phase of the COVID-19 pandemic, Pung et al. (2020) reported 3 COVID-19 clusters in Singapore and recommended expanding the surveillance system for imported cases to cover local cases. Liu et al. (2020) systematically reviewed 65 studies on 108 COVID-19 clusters (790 cases) from 13 countries and revealed that infection clusters might play an important role in modifying transmission patterns of COVID-19. However, the individual studies included in this review were limited to specific types of clusters, including family clusters and cluster outbreaks at specific gatherings or places such as conferences, religious events or shopping malls.
The contact tracing of every individual COVID-19 case in South Korea allows a unique opportunity to investigate cluster characteristics. To better understand the patterns of SARS-CoV-2 transmission, we conducted a comprehensive cluster analysis on all community clusters that have been reported in the Seoul metropolitan area. We categorized the clusters according to size and duration and investigated the relationship between cluster type and government-administered social distancing levels.
Methods
Data source
Data on COVID-19 cases from January 23 to September 24, 2020, in Seoul and the Gyeonggi province, was provided by the Seoul Metropolitan Government and Gyeonggi Provincial Office. Because we accessed publicly available de-identified data on COVID-19 cases, collected as part of the public health response and released for risk communication purposes, written informed consent was not required. The data included case number in the order of diagnosis, laboratory-confirmed COVID-19 diagnosis date, residential area, and transmission route. The data used in this study were generated through telephone or person-to-person interviews with individuals infected with COVID-19, as a part of the epidemiological investigation; thus, the transmission route is verified for each case directly by a contact tracer or epidemiological investigator. The diagnosis of COVID-19 was confirmed via real-time reverse transcription-polymerase chain reaction testing from nasopharyngeal or oropharyngeal swab specimens. Since the number of new daily cases dramatically increased after August 11, we divided the time-series into two time periods: before (phase 1) and after August 11 (phase 2).
Approximately 42% of the South Korean population resides in the Seoul metropolitan area, including Seoul, Incheon, and the Gyeonggi Province. Data on COVID-19 cases in the region is collected by the municipal offices; the data covers a population of 22.9 million, including 9.66 million from Seoul and 13.24 million from the Gyeonggi Province. Data from Incheon was excluded since information on transmission routes was only partially available.
Epidemiological investigation
The response to COVID-19 in South Korea is administered under the Infectious Diseases Control and Prevention Act (Ministry of Government Legislation, 2020, Son et al., 2020). When a new case is diagnosed, the institution that confirms the initial diagnosis is obligated to report it to the municipal office and the Korea Disease Control and Prevention Agency (KDCA). The local public health center then conducts a case study under the supervision of the Immediate Response Team. The case study includes contact tracing from 2 days before symptoms onset up to the SARS-CoV-2 test date. For asymptomatic cases, contact tracing is conducted from 2 days before the SARS-CoV-2 test date. Within 24 h after identifying a new case, contacts are identified and isolated, and prior visits to medical institutions or commercial facilities are reviewed (Seoul Metropolitan Government, 2020). Transmission routes and contacts are identified via case interviews and supplementary data such as GPS, CCTV and credit card use, permitted under the Infectious Diseases Control and Prevention Act (Article 76-2) (Ministry of Government Legislation, 2020, Ministry of Health and Welfare, 2020a).
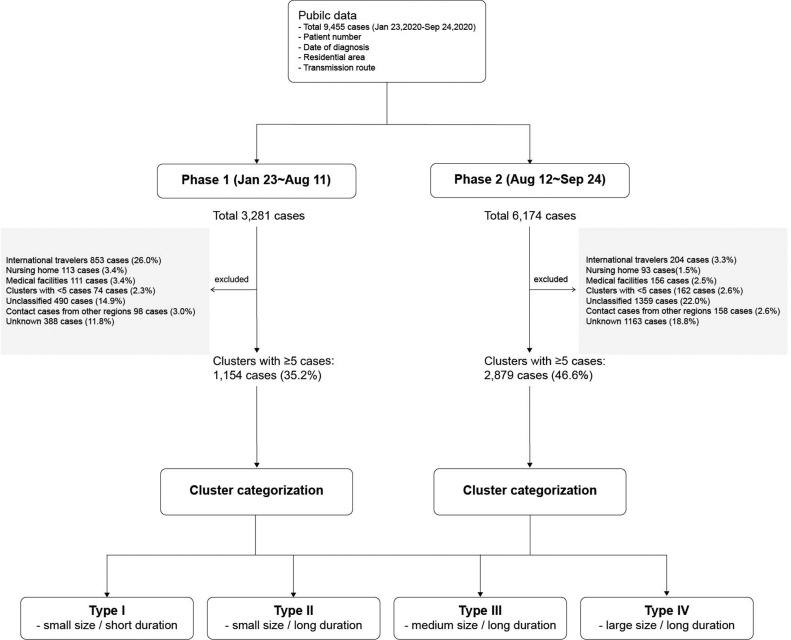
Definition of clusters and selection of cases
We defined a cluster as a group of ≥5 cases that share a common transmission route such as a place and event, excluding cases with secondary epidemiological links such as within- household transmission (Furuse et al., 2020). The process for the selection of cases for analysis is shown in Figure 1 . The analysis was limited to community outbreaks, with cases through transmission at nursing homes and medical facilities, including hospitals and clinics, excluded due to the different transmission patterns in terms of population susceptibility and infection opportunities (Duque et al., 2020). Imported cases were not included in the analysis since those entering South Korea are controlled through COVID-19 testing and quarantine at temporary living facilities (Ministry of Health and Welfare, 2020b), resulting in a limited number of local contacts (Korea Disease Control and Prevention Agency, 2020). Cases with undefined transmission routes were excluded from the analysis.
Figure 1.
Flow diagram showing the process of selecting cases for clusters with ≥5 cases.
Levels of social distancing
The South Korean government introduced social distancing measures on February 29, 2020, and strengthened the measures to “high level” on March 22, 2020. As the number of daily new cases dropped to <20, social distancing was eased to “moderate level” on April 20, 2020. As new daily cases were maintained at <5 from mid-April to early May, 2020, social distancing was further eased on May 6, 2020, and the concept of “social distancing in life” adopted (Jung et al., 2020). “Social distancing in life” aimed to maintain a balance between the economy and social activities, and infection prevention and containment, in order to prepare the society for a long-term fight against COVID-19 (Ministry of Health and Welfare, 2020c).
On June 28, the South Korean government adopted a new 3-level social distancing scheme: level 1 – applied when new daily cases <50; level 2 – daily cases 50 to <100; and level 3 – daily cases >100 or doubling twice a week. The size of social gatherings, including sporting events, and the operation of public facilities, education/nursery facilities, and workplaces were restricted according to the level of social distancing. Therefore, “level of social distancing” is a multi-dimensional measure in this study, capturing complex changes to social circumstances. The details of the measures for the 3-level social distancing regime are presented in the Supplementary Materials.
For the purpose of comparison, we categorized the levels of social distancing before June 28 as low, moderate, and high, and the levels of social distancing adopted on June 28 as low for level 1, moderate for level 2, and high for level 3. Therefore, the measure of social distancing adopted in this study is relative rather than absolute because the criteria for social distancing were not uniform from January to September.
Statistical analysis
Cluster characterization and the following analyses were conducted separately for phase 1 and 2. Clusters were characterized by 2 variables, size (the total number of cases in a cluster) and duration (the time between the first and last confirmed cases in a cluster). Cluster duration was estimated based on the diagnosis date rather than the symptoms onset date because approximately 33.3% of confirmed cases were reported to be asymptomatic at the time of diagnosis, in part due to proactive testing (Workman, 2020). Clusters were categorized into 4 groups by K-means clustering using the variables of size and duration. The process for selecting the variables and categorizing the clusters is elaborated in the Supplementary Materials (Supplementary Table 1 and Supplementary Figure 1).
The individual epidemic curves of clusters were investigated by cluster type, defined by K-means clustering, and the time period of each cluster mapped against the social distancing level(s) applicable at that time. If more than 2 levels of social distancing were implemented over a cluster period, the social distancing level during the peak of the epidemic curve for that cluster was selected. Spearman’s rank correlation coefficient was used to analyze the correlation between the cluster types and the concurrent social distancing level. We used R software (v4.0.2) (R Development Core Team, https://cran.r-project.org/) for statistical analyses. P-value <0.05 was used as the significance level.
Results
Clusters of COVID-19 in the Seoul metropolitan area during the two phases
A total of 3281 and 6174 cases were reported in the Seoul metropolitan area during phase 1 and 2, respectively. Community clusters with ≥5 cases were identified after excluding imported cases, cases associated with nursing homes or medical facilities, and unclassified cases or cases with unknown transmission routes (Figure 1). As a result, a total of 43 clusters comprised of 1154 cases (35.2% of total cases) were identified in phase 1, and 91 clusters of 2879 cases (46.6% of total cases) in phase 2.
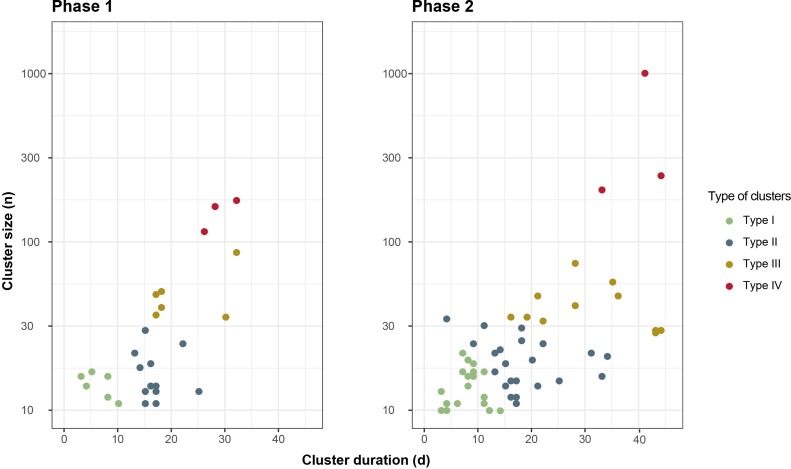
Cluster distribution showed a J–shape with large clusters with long duration and small clusters spanning over short and long duration (Supplementary Figure 2). All large clusters showed a long duration; thus, clusters with large size and short duration were not observed. Clusters were effectively categorized into 4 and 5 types in phase 1 and 2, respectively. Type I-IV showed similar patterns of distribution in both phases. A type V cluster in phase 2 corresponded to a particularly large cluster from the Sarang Jeil church with 1010 cases. We combined type IV and V as the large cluster type (type IV) in phase 2 (Figure 2 and Supplementary Figure 2). We plotted clusters against size and duration and indicated the types of clusters designated by K-means clustering. As a result, each type of cluster was distributed as in Figure 2: type I – small size <30 cases, short duration <2 weeks; type II – small size <30 cases, long duration ≥ 2 weeks; type III – medium size 30–99 cases, long duration ≥ 2 weeks; and type IV – large size ≥100 cases, long duration ≥ 2 weeks (Table 1 ). The characteristics and distribution of the 4 cluster types are shown in Table 2 .
Figure 2.
Types of COVID-19 clusters categorized by K-means clustering from January to September 2020 in the Seoul metropolitan area (see Appendix Figure 2) in phase 1 (January 23 to August 11, 2020) and phase 2 (August 11 to September 24, 2020). Cluster duration refers to the time between the first and the last case reported within a cluster. Cluster size refers to the number of cases per cluster. *Number of cases are in log scale.
Table 1.
Categorization of types of COVID-19 clusters with 5 or more cases from January to September 2020 in the Seoul metropolitan area.
| Duration of cluster | |||
|---|---|---|---|
| <2 weeks | ≥2 weeks | ||
| Size of cluster | <30 cases | Type I | Type II |
| 30–99 cases | NA | Type III | |
| ≥100 cases | NA | Type IV |
Table 2.
Characteristics of types of COVID-19 clusters with 5 or more cases from January to September 2020 in the Seoul metropolitan area.
| Phase 1 (23 Jan–11 Aug) |
Phase 2 (12 Aug–24 Sep) |
|||||
|---|---|---|---|---|---|---|
| No. cases (%)a | No. clusters | Cases per cluster (range) | No. cases (%)a | No. clusters | Cases per cluster (range) | |
| Total | 1154 (35.2) | 43 | 27 (5–163) | 2879 (46.6) | 91 | 32 (5–1010) |
| Type I | 178 | 21 | 8 (5-17) | 465 | 49 | 9 (5–22) |
| Type II | 212 | 13 | 16 (9–30) | 484 | 28 | 17 (5–35) |
| Type III | 301 | 6 | 50 (36–87) | 466 | 11 | 42 (29–75) |
| Type IV | 456 | 3 | 152 (116–163) | 1464 | 3 | 488 (205–1010) |
Cases from ≥5 case clusters as a percentage of total cases reported in the Seoul metropolitan area in the given time period.
Over both phases, type I clusters included 21 workplaces, 15 church activities, 13 family/friends gatherings and several other circumstances (Table 3 ). Type II included 14 church activities, 10 workplaces and 4 family/friends gathering. Club activities such as trekking, book and volunteering were unique to type II. Type III clusters included 7 church activities, 4 workplaces, 1 family/friends gathering, 1 restaurant and 1 shop. Type IV clusters included outbreaks at a customer service call center, the Itaewon night clubs, a network marketing service company, an outbreak at a church involving at least 1010 cases, and the National Liberation Day rally.
Table 3.
Number of COVID-19 clusters (with case numbers range) by type from January to September 2020 in the Seoul metropolitan area. Types of clusters: type I – small size <30 cases, short duration <2 weeks; type II – small size <30 cases, long duration ≥ 2 weeks; type III – medium size 30–99 cases, long duration ≥2 weeks; and type IV – large size ≥100 cases, long duration ≥2 weeks.
| Type I | Type II | Type III | Type IV | |
|---|---|---|---|---|
| Church | 15 (5–17) | 14 (5–30) | 7 (34–51) | 2 (205–1010) |
| Workplace | 21 (5–20) | 10 (8–31) | 4 (36–87) | 1 (163) |
| Protest | NA | NA | NA | 1 (249) |
| Night clubs | NA | NA | NA | 1 (177) |
| Network marketing services | 2 (10–12) | NA | NA | 1 (163) |
| Family/friends | 13 (5–16) | 4 (6–21) | 1 (29) | NA |
| Health training center | 3 (8–16) | 1 (12) | 1 (49) | NA |
| Apartment | 1 (6) | 2 (13–19) | 1 (36) | NA |
| Restaurant | 2 (8–9) | NA | 2 (30–58) | NA |
| Shop | 1 (6) | NA | 1 (75) | NA |
| Club activities | NA | 3 (15–26) | NA | NA |
| School | 1 (5) | 2 (15–32) | NA | NA |
| Public/private academy | 1 (10) | 2 (22–35) | NA | NA |
| Meeting | 1 (8) | 2 (23–25) | NA | NA |
| Hair salon | NA | 1 (11) | NA | NA |
| Buddhist conference | 1 (22) | NA | NA | NA |
| Guest house | 1 (6) | NA | NA | NA |
| Military unit | 1 (16) | NA | NA | NA |
| Nursery center | 4 (6–17) | NA | NA | NA |
| Police station | 1 (7) | NA | NA | NA |
| Sauna | 1 (19) | NA | NA | NA |
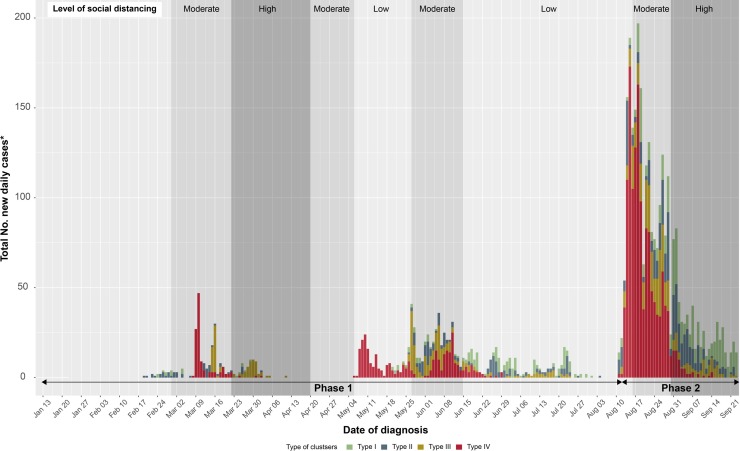
Figure 3 shows new reported daily cases belonging to clusters of ≥5 cases according to types designated by K-means clustering along with the social distancing level. Increased levels of social distancing followed a surge in daily cases in late March and late August, 2020. Peaks in daily cases in early May, 2020 (Itaewon clubs outbreak) and early August, 2020 (National Liberation Day rally and churches outbreak) were preceded by an easing of social distancing. From mid-June to early August, 2020, small clusters such as type I and II predominated; thus, the government maintained a low social distancing level. During phase 2, large clusters (type IV) decreased as a high level of social distancing was administered; however, type I and II clusters persisted with a gradual increase in the number of cases in these clusters.
Figure 3.
The number of reported daily COVID-19 cases belonging to clusters ≥5 cases and the government-administered social distancing level in 2020. Cases are categorized into 4 types of clusters: type I – small size <30 cases, short duration <2 weeks; type II – small size <30 cases, long duration ≥ 2 weeks; type III – medium size 30-99 cases, long duration ≥ 2 weeks; and type IV – large size ≥100 cases, long duration ≥ 2 weeks).
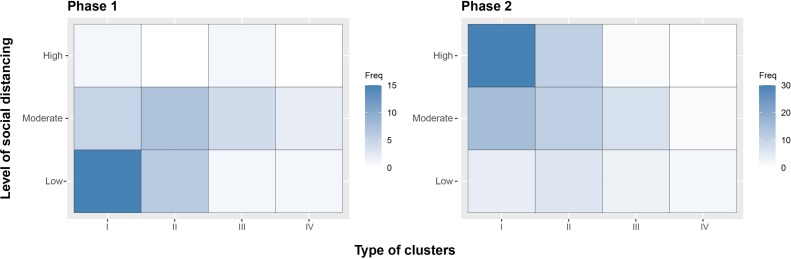
The distribution of the types of clusters was mapped against the government’s social distancing levels. Spearman’s rank correlation coefficients between the type of cluster and the social distancing level showed a statistically significant positive correlation in phase 1 and a negative correlation in phase 2 (Figure 4 and Supplementary Table 3), i.e. smaller clusters correlated with low social distancing levels in phase 1 and high social distancing levels in phase 2.
Figure 4.
The correlation between the type of clusters and the level of social distancing in phase 1 (January 23 to August 11, 2020) and phase 2 (August 11 to September 24, 2020). During phase 1, the smaller the clusters (type I and II), the lower the social distancing level. During phase 2, the smaller the clusters, the higher the social distancing level.
Discussion
We categorized 43 clusters from phase 1 and 91 clusters from phase 2 into 4 types depending on cluster size and duration. We then investigated the correlation between the types of clusters and the levels of social distancing.
Large clusters (type IV) mainly occurred on occasions where several hundred people were concentrated in a single area, such as call centers, dance clubs, network marketing service companies, and protests. The details of the characteristics of clusters are provided in the Supplementary Material. Type III clusters tended to occur during gatherings with several dozen people and included eating at a cafeteria, playing table tennis, or worshiping and singing in close proximity without wearing masks. Type I and II clusters occurred at small-sized workplaces, church, and family and neighborhood gatherings, which often involved dining together. The reasons why type II clusters showed longer durations than type I clusters were not clear but may be associated with the nature of activities that are distinct to type II, such as club activities including book club and trekking club, school, public/private academy, and meetings including business meetings and auctions. These circumstances could involve many people, but their intimacy may be less than in type I gatherings. For example, 13 family/friends’ gatherings were identified in type I, but only 4 were found in type II. It is possible that type II clusters could have occurred at larger sizes with longer duration but were effectively controlled to a lower number of cases since social distancing was more easily applied due to limited intimacy among the people in those circumstances.
During phase 1, there was a positive correlation between cluster size and social distancing level, but it was negative during phase 2. The government’s administration of social distancing measures followed the trend of daily confirmed cases, and the level of social distancing implemented impacted the spread of infection. From March, large outbreaks (type IV) occurred and were followed by the implementation of higher levels of social distancing, hence a positive correlation between cluster size and social distancing level in phase 1. A high level of social distancing suppresses the spread of COVID-19 so that only small clusters (type I) occur in September, resulting in a negative correlation between the 2 variables in phase 2 (Supplementary Figure 3). The relationship between social distancing and the number of COVID-19 cases is supported by previous studies, which show that an early mitigation strategy is associated with a smaller number of cases, while the relaxation of social distancing is linked with increased cases (Duque et al., 2020, Kaur et al., 2020). Therefore, precautions should be taken when making decisions to ease social distancing, and the duration should be carefully considered.
Considering the types of clusters helps to discern the pattern of disease propagation and its relationship with social distancing. For example, raising the level of social distancing succeeded in suppressing the daily number of cases but changed the cluster types, shifting from large to small clusters, as seen from August to September, 2020 (Figure 3). Although the number of daily reported cases are both approximately 25 in early May and mid-September, in early May, the cases are all from large clusters (type IV), while in mid-September, the cases are mostly from small clusters (type I). Different strategies are required for different types of clusters. For example, the duration of type IV clusters is almost always >4 weeks (Figure 2); therefore, a prolonged investigation is anticipated once type IV clusters are identified, and resources should be allocated accordingly.
An increase in the proportion of smaller clusters (type I and II) is observed over time. At the beginning of a pandemic, citizens might have been more alert to social distancing at an individual level, which prevented small clusters, but as time passes, the cases from small clusters increased, probably due to personal social distancing fatigue. Of total cases, including non-cluster cases, from January to September (Supplementary Figure 3), a substantial proportion are “other community infections” that are not otherwise grouped, occurring after the level of social distancing was increased during phase 2. This pattern suggests that a strategy should be adopted to control small and sporadic clusters, as well as targeting large-scale events.
During phase 2, the diagnosis-based epidemic curve of type IV clusters was already down-sloping before the high social distancing level was initiated in mid-August; one interpretation for this is as follows although it requires further investigation. Firstly, the downward slope of the peak of type IV clusters may have been achieved by epidemiological investigation and mass screening, contributing to early detection and isolation of cases. Secondly, people may have changed behaviors ahead of increased social distancing levels when the media reports that the government is considering raising the level of social distancing about a week before the actual implementation. Lastly, the timing of raising the level of social distancing appears relatively late because, at the time of elevating the level of social distancing, the curve was already down-sloping from the peak.
We inspected all the reported cases during the study period to identify clusters; thus, the cluster distribution reflects the whole COVID-19 cluster situation in the Seoul metropolitan area. However, this study has a few limitations. Firstly, since detailed information on epidemiological factors was not open to the public, further analyses of each cluster in terms of case characteristics, environment and circumstances were not possible; this should be pursued in further studies. Information on specific conditions for each cluster event could be used to develop a model to predict the type of cluster in the early phases, e.g. data on the number of people gathered in one place, the size of the area, whether the place was adequately ventilated, whether people were wearing masks, whether people had meals or sang together. If the type of cluster can be predicted, non-pharmaceutical interventions could be staged preemptively according to the cluster type. Secondly, there could have been misclassification of transmission routes during contact tracing since investigators’ capacity and training level may vary across municipal offices in different districts. More systematic information gathering is required during contact tracing to improve the quality of contact tracing data. Thirdly, as the data are based on the patients’ residential addresses, patients who share a transmission route but reside outside Seoul or Gyeonggi were excluded from the cluster. Further resources are needed from the municipal offices nationwide to include all infected individuals in a cluster. Lastly, the duration of a cluster may be affected by generation time from infector to infectee; however, data on this relationship was not available. Further studies are warranted to understand the relationship between generation time and the duration of clusters.
Conclusions
We categorized all clusters in the Seoul metropolitan area, showing the temporal distribution of clusters by type. Cluster categorization provides an opportunity to understand the pattern of disease propagation better. Temporal distribution of the different types of cluster and their relationship with the level of social distancing implies the need for different containment strategies for specific periods.
Funding Source
None
Ethical approval
For this article, ethical approval was not required.
Conflict of interest
None.
Acknowledgments
We thank epidemiological investigators and contact tracers in Seoul Metropolitan Government and Gyeonggi-do Provincial Office who devoted themselves to contain the outbreaks. We also acknowledge Prof. Sung-il Cho for his valuable advice on this paper.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.ijid.2021.02.058.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Duque D., Morton D.P., Singh B., Du Z., Pasco R., Meyers L.A. Timing social distancing to avert unmanageable COVID-19 hospital surges. Proc Natl Acad Sci. 2020;117:19873–19878. doi: 10.1073/pnas.2009033117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuse Y., Sando E., Tsuchiya N., Miyahara R., Yasuda I., Ko Y.K. Clusters of Coronavirus Disease in Communities, Japan, January-April 2020. Emerg Infect Dis. 2020;26(9):2176–2179. doi: 10.3201/eid2609.202272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung J., Noh J.Y., Cheong H.J., Kim W.J., Song J.Y. Coronavirus disease 2019 outbreak at nightclubs and distribution centers after easing social distancing: vulnerable points of infection. J Korean Med Sci. 2020;35:e247. doi: 10.3346/jkms.2020.35.e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur S., Bherwani H., Gulia S., Vijay R., Kumar R. Understanding COVID-19 transmission, health impacts and mitigation: timely social distancing is the key. Environ Dev Sustain. 2020;1–17 doi: 10.1007/s10668-020-00884-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Disease Control and Prevention Agency . 2020. Updates on COVID-19 in Republic of Korea. Available: https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030. [Google Scholar]
- Liu T., Gong D., Xiao J., Hu J., He G., Rong Z. Cluster infections play important roles in the rapid evolution of COVID-19 transmission: a systematic review. Int J Infect Dis. 2020;99:374–380. doi: 10.1016/j.ijid.2020.07.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Government Legislation . 2020. Infectious Disease Control and Prevention Act. Korea Law Translation Center. Available: https://elaw.klri.re.kr/kor_service/lawView.do?hseq=53530&lang=ENG. [Accessed 27 October 2020] [Google Scholar]
- Ministry of Health and Welfare . Central Disease Control Headquarters. Central Disaster Management Headquarters; 2020. COVID-19 response guideline for municipal officials (9th-2nd Edition) [in Korean] Available: http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=28. [Accessed 27 October 2020] [Google Scholar]
- Ministry of Health and Welfare . 3rd Edition. Central Disease Control Headquarters. Central Disaster Management Headquarters; 2020. Guidelines on temporary living/testing facilities for inbound travelers. Available: http://ncov.mohw.go.kr/en/guidelineView.do?brdId=18&brdGubun=181&dataGubun=&ncvContSeq=2615&contSeq=2615&board_id=&gubun=. [Accessed 27 October 2020] [Google Scholar]
- Ministry of Health and Welfare . Central Disaster and Safety Countermeasure Headquarters; 2020. Basic guidelines for distancing in daily life. Available: http://ncov.mohw.go.kr/en/guidelineView.do?brdId=18&brdGubun=181&dataGubun=&ncvContSeq=2763&contSeq=2763&board_id=&gubun=. [Accessed 27 October 2020] [Google Scholar]
- Park S.Y., Kim Y.M., Yi S., Lee S., Na B.J., Kim C.B. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020;26:1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.C., Clapham H.E. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–1046. doi: 10.1016/s0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seoul Metropolitan Government . 2020. (Seoul & Gyeonggi) Raising the social distancing and disinfection responding system to level 2. Available: http://english.seoul.go.kr/seoul-gyeonggi-raising-the-social-distancing-and-disinfection-responding-system-to-level-2/. [Accessed 27 October 2020] [Google Scholar]
- Son H., Lee H., Lee M., Eun Y., Park K., Kim S. Epidemiological characteristics of and containment measures for COVID-19 in Busan, Korea. Epidemiol Health. 2020;42 doi: 10.4178/epih.e2020035. e2020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. COVID-19 weekly epidemiological update. Available: https://www.who.int/publications/m/item/weekly-epidemiological-update---27-october-2020. [Accessed 2 November 2020] [Google Scholar]
- Workman J. The proportion of COVID-19 cases that are asymptomatic in South Korea: Comment on Nishiura et al. Int J Infect Dis. 2020;96:398. doi: 10.1016/j.ijid.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.