Abstract
Background
Transvenous lead extraction of cardiovascular implantable electronic device (CIED) has been proven safe in the general patient population with the advances in extraction techniques. Octogenarians present a unique challenge given their comorbidities and the perceived increase in morbidity and mortality.
Objective
To assess the safety and outcomes of CIED extraction in octogenarians to younger patients.
Methods
We performed an extensive literature search and systematic review of studies that compared CIED extraction in octogenarians versus non-octogenarians. We separately assessed the rate of complete procedure success, clinical success, procedural mortality, major and minor complications. Risk ratio (RR) 95% confidence intervals were measured using the Mantel-Haenszel method. The random effects model was used due to heterogeneity across study cohorts.
Results
Seven studies with a total of 4,182 patients were included. There was no difference between octogenarians and non-octogenarians in complete procedure success (RR 1.01, 95% CI 1.00 – 1.02, p = 0.19) and clinical success (RR 1.01, 95% CI 1.00 – 1.01, p = 0.13). There was also no difference in procedural mortality (RR 1.43, 95% CI 0.46 – 4.39, p = 0.54), major complication (RR 1.40, 95% CI 0.68 – 2.88, p = 0.36), and minor complication (RR 1.43, 95% CI 0.90 – 2.29, p = 0.13).
Conclusion
In this study, there was no evidence to suggest a difference in procedural success and complication rates between octogenarians and younger patients. Transvenous lead extraction can be performed safely and effectively in the elderly population.
Keywords: Cardiovascular implantable electronic device, Implantable cardioverter-defibrillator, Octogenarian, Pacemaker, Transvenous lead extraction
Key Findings.
-
▪
The rates of complete procedural success and clinical success were similar between octogenarians and younger patients.
-
▪
Procedural mortality was low in both octogenarians and younger patients. There was no statistically significant difference between the 2 groups.
-
▪
There was no statistically significant difference in major and minor complications between the octogenarians and younger patients.
Introduction
The use of cardiovascular implantable electronic devices (CIED) such as implantable cardioverter-defibrillators (ICD), permanent pacemakers, and cardiac resynchronization therapy has become increasingly prevalent as an important aspect in the management of chronic heart disease. Inevitably, the increase in CIED implantation has paralleled the rise in need for CIED extraction, driven mainly by systems failure or device infection.1 Historically, the perceived risk of complications and lack of specialists has limited the performance of lead extractions. However, with growing physician experience and the improvement of extraction techniques,2, 3, 4 CIED extraction is now considered a relatively safe procedure.5 Prior studies have reported major complication rates of 0.7%–1.9% and minor complication rates of 1.4%–7.2% to be associated with transvenous CIED extraction.2, 3, 4,6,7
A unique population worth separate consideration is the octogenarians. Given their higher number of comorbidities and likely longer duration of device implantation, CIED extraction may be delayed in favor of conservative treatment owing to the perceived risk of procedural morbidity and mortality. The issue of CIED extraction in octogenarians is of particular concern given the growing number of elderly patients living with CIEDs.8,9 While some studies have reported old age as a risk factor for worse outcomes in lead extraction,10 others have shown varying results.11, 12, 13, 14, 15, 16, 17 The purpose of our current study was to perform a systematic review of literature and meta-analysis to assess the safety and success rate of CIED extraction in octogenarians compared to younger patients.
Methods
Literature search
We performed a systematic review of PubMed, Medline, Google scholar, and the Cochrane Library. This was assessed up to January 2020. Restriction to humans was applied. The reference list of all eligible studies was also reviewed. Search terms included (octogenarian or elderly) and (implantable cardioverter-defibrillator or pacemaker or cardiovascular implantable electronic device) and extraction.
Study selection
Studies were selected by 2 independent reviewers. The PRISMA statement for reporting systemic reviews and meta-analyses was applied to the methods for this study.18 The studies had to fulfill the following criteria to be considered in the analysis: (1) Studies must have reported the safety and efficacy of CIED extraction in an elderly patient group vs a younger control group. (2) Elderly patient group must have a mean age of 80 years or greater. (3) Definition for lead extraction must be consistent with the Heart Rhythm Society expert consensus document.19 (4) Studies must have been published in a peer-reviewed scientific journal.
Study outcomes
We aimed to compare the rates of complete procedure success, clinical success, procedural mortality, and major and minor complications between the octogenarian and the nonoctogenarian groups. Term definitions were taken from the Heart Rhythm Society expert consensus document.19
Data extraction
Two authors (A.L. and F.L.) independently performed the literature search and extracted data from eligible studies. Outcomes were extracted from original manuscripts. Information was gathered using standardized protocol and reporting forms. Discrepancies were resolved by consensus. Two reviewers (A.L. and F.L.) independently assessed the quality items and differences were resolved by consensus.
Individual study quality appraisal
Two authors (A.L. and F.L.) independently assessed the quality and reporting of the studies with the Newcastle-Ottawa scale.20 Three categories were included in the analysis. Study quality was then classified into 1 of 3 categories: (1) high quality (7–9 points), (2) satisfactory quality (4–6 points), or (3) unsatisfactory quality (0–3 points).
Statistical analysis
Data were summarized across comparison arms using the Mantel-Haenszel risk ratio (RR). Random-effects models for analyses were used owing to heterogeneity across study cohorts. Funnel plot analysis was used to address publication bias.21 Statistical analysis was performed using Review Manager (RevMan) Version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. Continuous variables are presented as means with standard deviations (SD) and categorical or dichotomous variables are presented as numbers with percentage (%).
Results
Study selection and patient characteristics
The initial search resulted in 2188 abstracts, of which 1312 were duplications and 864 were excluded based on titles and abstracts (Figure 1). We included 7 studies in our final analysis with a total of 4182 patients (17% octogenarians). Baseline characteristics are summarized in Table 1. Patients were mostly male with multiple medical comorbidities. More octogenarians underwent lead extraction for the indication of infection than nonoctogenarians (71% vs 56%, P < .01), and octogenarians had a lower proportion of ICDs extracted relative to other types of CIEDs (19% vs 44%, P < .01). Study characteristics are shown in Table 2. All 7 studies were retrospective in nature; 6 were single-center studies. Year of CIED extraction ranged from 2001 to 2018.
Figure 1.
Selection of studies.
Table 1.
Patient demographics and characteristics
| Study | Rodriguez et al |
Williams et al |
Pelargonio et al |
Kempa et al |
Kutarski et al |
El-Chami et al |
Yagishita et al |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | |
| Patients | 118 | 388 | 72 | 334 | 150 | 699 | 26 | 134 | 192 | 1060 | 100 | 674 | 51 | 184 |
| Age, y | 85±4 | 64±12 | 84±3 | 62±14 | 84±3 | 61±10 | 84±3 | 60±14 | 83±3 | 63±13 | 85±4 | 60±15 | 86±5 | 67±15 |
| Male | 78 (66) | 301 (78) | 53 (74) | 258 (77) | 96 (64) | 556 (80) | 16 (62) | 97 (72) | 105 (55) | 669 (63) | 63 (63) | 446 (66) | 34 (68) | 133 (73) |
| Lead age, mo | 60±53 | 39±44 | 71 | 74 | 42 | 29 | 55 | 40 | 76 | 84 | 71 | 67 | 110 | 88 |
| EF | 42±17 | 35±19 | 42±14 | 45±13 | 49±13 | 42±14 | 44±10 | 40±15 | NR | NR | 43±15 | 36±17 | 57±15 | 54±16 |
| Device type | ||||||||||||||
| PPM | 68 (56) | 141 (36) | 46 (64) | 172 (51) | 126 (84) | 385 (55) | 24 (92) | 67 (50) | 147 (77) | 593 (56) | 36 (36) | 70 (10) | 42 (82) | 93 (51) |
| ICD | 35 (28) | 181 (47) | 11 (15) | 96 (29) | 24 (16) | 314 (45) | 2 (8) | 63 (47) | 14 (7) | 305 (29) | 48 (48) | 496 (74) | 3 (6) | 63 (34) |
| CRT-P | 2 (3) | 1 (1) | 1 (1) | 20 (6) | Bi-V: | Bi-V: | Bi-V: | Bi-V: | Bi-V: | Bi-V: | Bi-V | Bi-V: | 3 (6) | 4 (2) |
| CRT-D | 13 (13) | 65 (16) | 14 (19) | 46 (14) | 38 | 170 | 0 (0) | 4 (3) | 31 (16) | 162 (15) | 16 (16) | 108 (16) | 3 (6) | 24 (13) |
| Indications | ||||||||||||||
| Infection | 99 (84) | 296 (76) | 58 (80) | 207 (62) | 133 (89) | 573 (82) | 15 (58) | 64 (48) | 102 (53) | 448 (42) | 47 (47) | 225 (33) | 50 (98) | 116 (63) |
| Lead failure | 17 (14) | 84 (21) | 9 (13) | 96 (29) | NR | NR | 6 (23) | 56 (42) | NR | NR | 39 (39) | 339 (50) | 1 (2) | 49 (27) |
| Device upgrade | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 7 (7) | 64 (10) | 0 (0) | 9 (5) |
| SVC syndrome | NR | NR | 1 (1) | 3 (1) | NR | NR | 0 (0) | 2 (1) | NR | NR | NR | NR | 0 (0) | 2 (1) |
| Chronic pain | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 0 (0) | 2 (1) |
| Other | NR | NR | 4 (6) | 28 (8) | NR | NR | 5 (19) | 12 (9) | NR | NR | 7 (7) | 46 (7) | 0 (0) | 6 (3) |
| Comorbidities | ||||||||||||||
| HTN | 104 (88) | 324 (84) | 25 (41) | 89 (30) | 122 (81) | 502 (72) | 16 (62) | 61 (46) | NR | NR | 77 (77) | 411 (61) | 27 (53) | 70 (38) |
| DM | 45 (38) | 190 (49) | 6 (10) | 30 (10) | 60 (40) | 222 (32) | 11 (42) | 37 (28) | NR | NR | 19 (19) | 206 (31) | 13 (26) | 40 (22) |
| CAD | 72 (61) | 261 (67) | 35 (57) | 117 (38) | 41 (27) | 264 (38) | 12 (47) | 60 (45) | NR | NR | 50 (50) | 265 (39) | 10 (20) | 31 (17) |
| CKD | 26 (22) | 84 (22) | 12 (18) | 44 (14) | 83 (55) | 182 (26) | 4 (15) | 21 (16) | NR | NR | 25 (25) | 131 (19) | 3 (6) | 7 (4) |
| CVA | NR | NR | 8 (13) | 18 (6) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| COPD | NR | NR | 7 (12) | 28 (9) | 69 (46) | 133 (19) | NR | NR | NR | NR | NR | NR | NR | NR |
Values presented as mean ± standard deviation for continuous variables and number (percentage) for categorical variables.
Bi-V = biventricular; CAD = coronary artery disease; CKD = chronic kidney disease; COPD = chronic obstructive pulmonary disease; CRT-D = cardiac resynchronization therapy defibrillator; CRT-P = cardiac resynchronization therapy pacemaker; CVA = cerebrovascular accident; DM = diabetes mellitus; EF = ejection fraction; HTN = hypertension; ICD = implantable cardioverter-defibrillator; NR = not reported; PPM = permanent pacemaker; SVC = superior vena cava.
Table 2.
Study characteristics
| Study | Rodriguez et al | Williams et al | Pelargonio et al | Kempa et al | Kutarski et al | El-Chami et al | Yagishita et al |
|---|---|---|---|---|---|---|---|
| Study design | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective | Retrospective |
| Years of extraction | 2004–2009 | 2001–2011 | 2005–2011 | 2003–2011 | 2006–2013 | 2007–2016 | 2013–2018 |
| Year of publication | 2011 | 2012 | 2012 | 2012 | 2013 | 2017 | 2019 |
| Study site | Single center | Single center | Multicenter | Single center | Single center | Single center | Single center |
| Single operator | Yes | No | No | Not reported | Yes | No | Not reported |
| Follow-up | 30 days | At least 30 days | Not reported | Not reported | Not reported | 3 years | Not reported |
Study endpoints
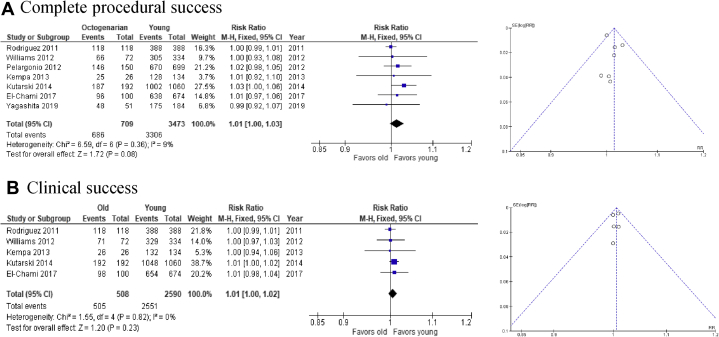
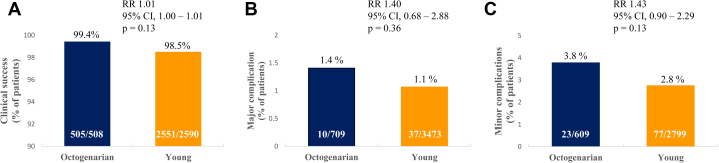
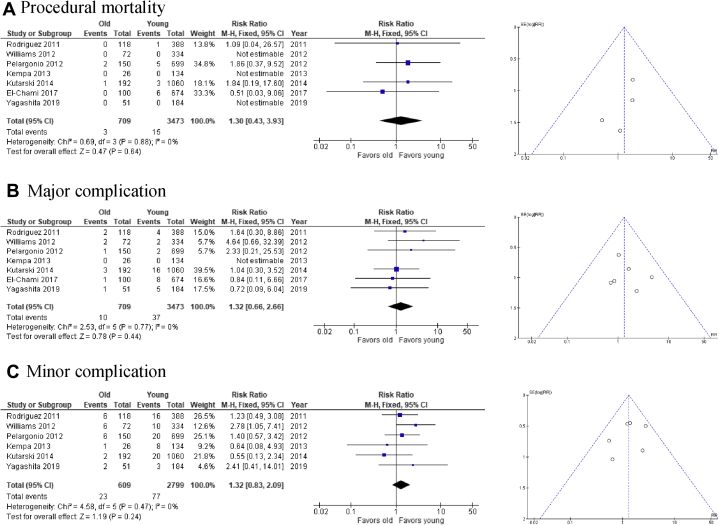
There was no difference in complete procedural success (RR 1.01, 95% confidence interval [CI] 1.00–1.02, P = .19) and clinical success (RR 1.01, 95% CI 1.00–1.01, P = .13) between octogenarians and nonoctogenarians (Figure 2). There was also no statistically significant difference in procedural mortality (RR 1.43, 95% CI 0.46–4.39, P = .54), major complications (RR 1.40, 95% CI 0.68–2.88, P = .36), and minor complications (RR 1.43, 95% CI 0.90–2.29, P = .13) (Figures 3 and 4). Thirty-day mortality was comparable between the 2 groups (RR 1.14, 95% CI 0.41–3.15, P = .80).
Figure 2.
Forest plot and funnel plot of efficacy outcomes of cardiovascular implantable electronic device extraction in octogenarians vs younger patients. A: Complete procedural success. B: Clinical success.
Figure 3.
Comparative analysis of A: clinical success, B: major complication, and C: minor complication of device extraction in octogenarians vs younger control group.
Figure 4.
Forest plot and funnel plot of safety outcomes of cardiovascular implantable electronic device extraction in octogenarians vs younger patients. A: Procedural mortality. B: Major complication. C: Minor complication.
Procedural characteristics
Procedural characteristics are summarized in Table 3. More than 7000 leads were extracted in the included studies. Most lead extractions were performed via the subclavian approach using manual traction or laser sheaths. Two studies reported no difference in procedure time between octogenarians and younger patients.
Table 3.
Procedural characteristics
| Study | Rodriguez et al |
Williams et al |
Pelargonio et al |
Kempa et al |
Kutarski et al |
El-Chami et al |
Yagishita et al |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | Old | Young | |
| Patients, n | 118 | 388 | 72 | 334 | 150 | 699 | 26 | 134 | 192 | 1060 | 100 | 674 | 51 | 184 |
| Procedure time | NR | NR | 88±53 | 92±52 | NR | NR | NR | NR | 104±46 | 111±48 | NR | NR | NR | NR |
| Technique | ||||||||||||||
| MT | 0 (0) | 0 (0) | 35 (49) | 168 (50) | 26 (17) | 109 (15) | NR | NR | NR | NR | 42 (42) | 277 (41) | 0 (0) | 0 (0) |
| LS | 118 (100) | 388 (100) | 37 (51) | 166 50) | 124 (83) | 578 (83) | NR | NR | NR | NR | 41 (41) | 304 (45) | 44 (86) | 165 (90) |
| MS | 0 (0) | 0 (0) | 0 (0) | 0 (0 0 | 0 (0) | 12 (2) | NR | NR | NR | NR | 17 (17) | 93 (14) | 7 (14) | 19 (10) |
| Leads extracted | ||||||||||||||
| Total | 253 | 814 | 141 | 657 | 301 | 1410 | 35 | 185 | 2137 | 1078 | 170 | NR | NR | |
| Atrial | 99 (39) | 295 (36) | 57 (40) | 254 (39) | 97 (32) | 484 (34) | 12 (34) | 65 (35) | 914 (43) | NR | NR | NR | NR | |
| Ventricular | 145 (57) | 442 (54) | 70 (50) | 344 (52) | 166 (55) | 753 (53) | 23 (66) | 116 (63) | 1145 (54) | NR | NR | NR | NR | |
| CS | 9 (4) | 77 (10) | 14 (10) | 59 (9) | 38 (13) | 173 (13) | 0 (0) | 4 (2) | 78 (3) | NR | NR | NR | NR | |
| Approach | ||||||||||||||
| Subclavian | 116 (98) | 379 (98) | 70 (97) | 331 (97) | NR | NR | 25 (96) | 131 (98) | NR | NR | 96 (96) | 640 (95) | NR | NR |
| Femoral | 2 (2) | 9 (2) | 2 (3) | 11 (3) | NR | NR | 1 (4) | 3 (2) | NR | NR | 4 (4) | 34 (5) | NR | NR |
Values presented as mean ± standard deviation for continuous variables and number (percentage) for categorical variables.
CS = coronary sinus; LS = laser sheath; MS = mechanical sheath; MT = manual traction; NR = not reported.
Quality assessment and publication bias
Based on the Newcastle-Ottawa scale, 5 of the 7 studies were of high quality, 2 were satisfactory quality, and none were unsatisfactory quality (Table 4). Funnel plots did not reveal publication bias for any of the reported outcomes (Figures 2 and 4).
Table 4.
Newcastle-Ottawa scale of the included studies
| Study | Selection† | Comparability‡ | Outcome§ |
|---|---|---|---|
| Rodriguez et al | 3 | 1 | 2 |
| Williams et al | 3 | 1 | 3 |
| Pelargonio et al | 3 | 1 | 3 |
| Kempa et al | 3 | 1 | 2 |
| Kutarski et al | 3 | 2 | 3 |
| El-Chami et al | 3 | 1 | 3 |
| Yagishita et al | 3 | 1 | 3 |
Maximum 4 stars.
Maximum 2 stars.
Maximum 3 stars.
Discussion
To the best of our knowledge, this is the first meta-analysis and systematic review of studies that have compared the safety and clinical outcomes of CIED extraction in octogenarians vs younger patients. The results of this meta-analysis show similar rates of clinical success and complete procedural success in elderly patients without an increase in procedural death or in major or minor complications.
The proportion of elderly adults in the United States is rising and they account for a large portion of health care consumers, with an estimated annual increase of 5.4%–7.2%.22 More than 70% of pacemakers implanted in the United States are in patients aged >70 years, and up to two-thirds of ICDs are implanted in patients aged >65 years.23 Other large registries have shown 12%–20% of ICD implantations are in patients aged >80 years.24,25 The aging of patients living with CIED is a global phenomenon, as similar findings have been described in areas outside the United States, including Canada,26 Italy,27 and Korea.28 It is therefore important to expand the literature on the safety and efficacy of CIED extraction in elderly patients.
A survey of 38 high-volume medical centers in Europe showed increasing age as a factor for hesitancy of clinicians in proceeding with lead extraction,29 likely owing to higher perceived risk for adverse events. Since then, several studies have evaluated age as a predictor of perioperative complications in transvenous lead extractions. In a multicenter study using data from the National Cardiovascular Data Registry Implantable Cardioverter-Defibrillator Registry involving 11,304 extraction procedures, age was not found to be associated with major complications on univariate analysis, with an odds ratio of 1.00.30 In a separate registry study involving 91,890 transvenous lead extractions, more elderly patients experienced procedural complications, but the results were not statistically significant when adjusted with multivariate analysis.31 Contrary to the above, Maytin and colleagues32 reported increasing age at time of lead extraction as a correlate with increased mortality risk. Similarly, a meta-analysis involving 62 studies suggested increasing age as a risk factor for major complications or death in patients who undergo laser lead extraction.10 The ambiguity in literature on safety of lead extractions in elderly patients may be due to the overall low complication rate, making accurate risk analysis difficult.
One of the concerns for increased periprocedural complications for octogenarians arises from the assumption that older patients are frailer and have more comorbidities. However, it is important to note that this was not consistently observed in the studies included in this meta-analysis. In a study by Rodriguez and colleagues,11 the majority of patients had 3 or more comorbidities but there was no statistically significant difference between the octogenarians and the younger cohort. In a separate study by Williams and colleagues,12 octogenarians had more comorbidities than nonoctogenarians but only the difference in ischemic heart disease was statistically significant when the prevalence of each comorbidity is compared individually. In other studies, octogenarians actually had lower prevalence of coronary artery disease and diabetes, and higher ejection fraction, compared to nonoctogenarians.13,17 This finding may be attributed to the fact that older patients with higher numbers of comorbidities may not receive CIED implantation in the first place. Although previous landmark trials have shown decreased mortality with ICD and cardiac resynchronization therapy in certain patient populations, this benefit is less well defined in octogenarians, given their lower ratio of arrhythmic to nonarrhythmic deaths.
Prior works have reported 30-day mortality in patients undergoing lead extraction to be 2%–3%.33,34 However, this was not more commonly observed in octogenarians based on this current meta-analysis. One of the included studies assessed mortality up to 3 years after lead extraction between octogenarians and the younger cohort.17 Although there was a slight divergence of Kaplan-Meier survival curve after 1.5 years favoring younger patients, this was not statistically significant (P = .203). This finding suggests long-term outcomes of lead extraction in octogenarians are excellent and comparable to younger patients.
Notably, more patients in the octogenarian group underwent lead extraction for the indication of CIED infection compared to the nonoctogenarian group. This is consistent with clinical practice, as the decision to proceed with CIED extraction is a result of shared decision-making considering the risks vs potential benefits of the procedure. Although extraction of an infected CIED is a class I indication, other common indications listed in the included studies (ie, lead failure, device upgrade) are more often performed in younger patients, as they are expected to live long enough to derive the long-term benefits. Although this may introduce selection bias, in the context that extraction of infected CIEDs has previously been associated with an increased risk for procedural complications,30,35 octogenarians did not experience more adverse outcomes despite having more infected lead extractions. Another notable difference is the lower proportion of defibrillating leads extracted in octogenarians, which can be more difficult to extract and may be associated with a higher risk of adverse outcomes.19
The current meta-analysis has several limitations that should be acknowledged. First, most of the studies included were single-center experiences and, in some cases, single-operator outcomes, which limits the generalizability of our findings. This is especially important, as procedural success has been associated with proceduralist experience. Next, there was notable heterogeneity on lead characteristics and indications for extraction in the studies. Multiple risk factors reported in literature to be associated with increased complications were not addressed in this study, as the lack of data available precludes the performance of sensitivity analysis. Third, all included studies were retrospective and our findings are limited by the nature of retrospective designs.
Conclusion
In patients undergoing CIED extraction, there is no evidence to suggest a difference in procedural success and complication rates between octogenarians and younger patients. Based on our meta-analysis, clinicians may consider CIED extraction in elderly patients as a safe and effective management option.
Funding Sources
This research was partially funded by the American Heart Association (United States, AHA 19CDA34760021) and National Institutes of Health (United States, NIH 1KL2TR001444) to GH.
Disclosures
Dr Ho receives grant support from the American Heart Association (AHA 19CDA34760021) and National Institutes of Health (NIH 1KL2TR001444). He also reports equity in Vektor Medical Inc unrelated to this work. Dr Birgersdotter-Green has received grant support from Abbott Laboratories and honoraria from Medtronic, Abbott, and Boston Scientific. The rest of the authors have no conflicts of interest.
References
- 1.Greenspon A.J., Patel J.D., Lau E. 16-year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States 1993 to 2008. J Am Coll Cardiol. 2011;58:1001–1006. doi: 10.1016/j.jacc.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 2.Wazni O., Epstein L.M., Carrillo R.G. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J Am Coll Cardiol. 2010;55:579–586. doi: 10.1016/j.jacc.2009.08.070. [DOI] [PubMed] [Google Scholar]
- 3.Bongiorni M.G., Soldati E., Zucchelli G. Transvenous removal of pacing and implantable cardiac defibrillating leads using single sheath mechanical dilatation and multiple venous approaches: high success rate and safety in more than 2000 leads. Eur Heart J. 2008;29:2886–2893. doi: 10.1093/eurheartj/ehn461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma S., Ekeruo I.A., Nand N.P. Safety and efficacy of transvenous lead extraction utilizing the evolution mechanical lead extraction system: A single-center experience. JACC Clin Electrophysiol. 2018;4:212–220. doi: 10.1016/j.jacep.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 5.Maus T.M., Shurter J., Nguyen L., Birgersdotter-Green U., Pretorius V. Multidisciplinary approach to transvenous lead extraction: a single center's experience. J Cardiothorac Vasc Anesth. 2015;29:265–270. doi: 10.1053/j.jvca.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Bongiorni M.G., Kennergren C., Butter C. The European Lead Extraction ConTRolled (ELECTRa) study: a European Heart Rhythm Association (EHRA) registry of transvenous lead extraction outcomes. Eur Heart J. 2017;38:2995–3005. doi: 10.1093/eurheartj/ehx080. [DOI] [PubMed] [Google Scholar]
- 7.Byrd C.L., Wilkoff B.L., Love C.J., Sellers T.D., Reiser C. Clinical study of the laser sheath for lead extraction: the total experience in the United States. Pacing Clin Electrophysiol. 2002;25:804–808. doi: 10.1046/j.1460-9592.2002.t01-1-00804.x. [DOI] [PubMed] [Google Scholar]
- 8.Kurtz S.M., Ochoa J.A., Lau E. Implantation trends and patient profiles for pacemakers and implantable cardioverter defibrillators in the United States: 1993-2006. Pacing Clin Electrophysiol. 2010;33:705–711. doi: 10.1111/j.1540-8159.2009.02670.x. [DOI] [PubMed] [Google Scholar]
- 9.Barra S., Providencia R., Paiva L., Heck P., Agarwal S. Implantable cardioverter-defibrillators in the elderly: rationale and specific age-related considerations. Europace. 2015;17:174–186. doi: 10.1093/europace/euu296. [DOI] [PubMed] [Google Scholar]
- 10.Diemberger I., Mazzotti A., Giulia M.B. From lead management to implanted patient management: systematic review and meta-analysis of the last 15 years of experience in lead extraction. Expert Rev Med Devices. 2013;10:551–573. doi: 10.1586/17434440.2013.811837. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez Y., Garisto J.D., Carrillo R.G. Laser lead extraction in the octogenarian patient. Circ Arrhythm Electrophysiol. 2011;4:719–723. doi: 10.1161/CIRCEP.111.964270. [DOI] [PubMed] [Google Scholar]
- 12.Williams S.E., Arujuna A., Whitaker J. Percutaneous extraction of cardiac implantable electronic devices (CIEDs) in octogenarians. Pacing Clin Electrophysiol. 2012;35:841–849. doi: 10.1111/j.1540-8159.2012.03400.x. [DOI] [PubMed] [Google Scholar]
- 13.Pelargonio G., Narducci M.L., Russo E. Safety and effectiveness of transvenous lead extraction in octogenarians. J Cardiovasc Electrophysiol. 2012;23:1103–1108. doi: 10.1111/j.1540-8167.2012.02372.x. [DOI] [PubMed] [Google Scholar]
- 14.Kempa M., Budrejko S., Piepiorka M., Rogowski J., Raczak G., Kozlowski D. Safety and effectiveness of transvenous extraction of pacemaker and implantable cardioverter-defibrillator leads in patients under or over 80 years of age. Kardiol Pol. 2013;71:130–135. doi: 10.5603/KP.2013.0005. [DOI] [PubMed] [Google Scholar]
- 15.Kutarski A., Polewczyk A., Boczar K., Zabek A., Polewczyk M. Safety and effectiveness of transvenous lead extraction in elderly patients. Cardiol J. 2014;21:47–52. doi: 10.5603/CJ.a2013.0084. [DOI] [PubMed] [Google Scholar]
- 16.Yagishita A., Goya M., Sekigawa M. Transvenous excimer laser-assisted lead extraction of cardiac implantable electrical devices in the Japanese elderly population. J Cardiol. 2020;75:410–414. doi: 10.1016/j.jjcc.2019.09.005. [DOI] [PubMed] [Google Scholar]
- 17.El-Chami M.F., Sayegh M.N., Patel A. Procedural outcomes and long-term survival following lead extraction in octogenarians. Pacing Clin Electrophysiol. 2017;40:868–872. doi: 10.1111/pace.13113. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 19.Kusumoto F.M., Schoenfeld M.H., Wilkoff B.L. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–e551. doi: 10.1016/j.hrthm.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Wells G.A., Shea B., O'Connell D. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Available at.
- 21.Sterne J.A., Sutton A.J., Ioannidis J.P. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 22.Lassman D., Hartman M., Washington B., Andrews K., Catlin A. US health spending trends by age and gender: selected years 2002-10. Health Aff (Millwood) 2014;33:815–822. doi: 10.1377/hlthaff.2013.1224. [DOI] [PubMed] [Google Scholar]
- 23.Bailey S.M., Wilkoff B.L. Complications of pacemakers and defibrillators in the elderly. Am J Geriatr Cardiol. 2006;15:102–107. doi: 10.1111/j.1076-7460.2006.04815.x. [DOI] [PubMed] [Google Scholar]
- 24.Kremers M.S., Hammill S.C., Berul C.I. The National ICD Registry Report: version 2.1 including leads and pediatrics for years 2010 and 2011. Heart Rhythm. 2013;10:e59–e65. doi: 10.1016/j.hrthm.2013.01.035. [DOI] [PubMed] [Google Scholar]
- 25.Epstein A.E., Kay G.N., Plumb V.J. Implantable cardioverter-defibrillator prescription in the elderly. Heart Rhythm. 2009;6:1136–1143. doi: 10.1016/j.hrthm.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Yung D., Birnie D., Dorian P. Survival after implantable cardioverter-defibrillator implantation in the elderly. Circulation. 2013;127:2383–2392. doi: 10.1161/CIRCULATIONAHA.113.001442. [DOI] [PubMed] [Google Scholar]
- 27.Proclemer A., Ghidina M., Gregori D. Impact of the main implantable cardioverter-defibrillator trials in clinical practice: data from the Italian ICD Registry for the years 2005-07. Europace. 2009;11:465–475. doi: 10.1093/europace/eun370. [DOI] [PubMed] [Google Scholar]
- 28.Lee J.H., Lee S.R., Choi E.K. Temporal trends of cardiac implantable electronic device implantations: a nationwide population-based study. Korean Circ J. 2019;49:841–852. doi: 10.4070/kcj.2018.0444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Erven L., Morgan J.M. Attitude towards redundant leads and the practice of lead extractions: a European survey. Europace. 2010;12:275–276. doi: 10.1093/europace/eup443. [DOI] [PubMed] [Google Scholar]
- 30.Sood N., Martin D.T., Lampert R., Curtis J.P., Parzynski C., Clancy J. Incidence and predictors of perioperative complications with transvenous lead extractions: real-world experience with national cardiovascular data registry. Circ Arrhythm Electrophysiol. 2018;11 doi: 10.1161/CIRCEP.116.004768. [DOI] [PubMed] [Google Scholar]
- 31.Deshmukh A., Patel N., Noseworthy P.A. Trends in use and adverse outcomes associated with transvenous lead removal in the United States. Circulation. 2015;132:2363–2371. doi: 10.1161/CIRCULATIONAHA.114.013801. [DOI] [PubMed] [Google Scholar]
- 32.Maytin M., Jones S.O., Epstein L.M. Long-term mortality after transvenous lead extraction. Circ Arrhythm Electrophysiol. 2012;5:252–257. doi: 10.1161/CIRCEP.111.965277. [DOI] [PubMed] [Google Scholar]
- 33.Brunner M.P., Yu C., Hussein A.A. Nomogram for predicting 30-day all-cause mortality after transvenous pacemaker and defibrillator lead extraction. Heart Rhythm. 2015;12:2381–2386. doi: 10.1016/j.hrthm.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 34.Deckx S., Marynissen T., Rega F. Predictors of 30-day and 1-year mortality after transvenous lead extraction: a single-centre experience. Europace. 2014;16:1218–1225. doi: 10.1093/europace/eut410. [DOI] [PubMed] [Google Scholar]
- 35.Hosseini S.M., Rozen G., Kaadan M.I., Galvin J., Ruskin J.N. Safety and in-hospital outcomes of transvenous lead extraction for cardiac implantable device-related infections: Analysis of 13 years of inpatient data in the United States. JACC Clin Electrophysiol. 2019;5:1450–1458. doi: 10.1016/j.jacep.2019.08.020. [DOI] [PubMed] [Google Scholar]