Abstract
Objective
Integrating constructs from three prominent health behavior theories including the extended parallel process model, the health belief model, and the theory of planned behavior, this study seeks to identify sociopsychological factors that influenced American’s intention to receive a COVID-19 vaccine.
Method
An online survey was delivered to a U.S. sample (N = 934), assessing the influences of risk perception and fear associated with COVID-19, beliefs about and attitudes toward COVID-19 vaccines, self-efficacy, social and psychological contexts, and demographic characteristics on people’s intention to get COVID-19 vaccines.
Results
Most respondents intended to get vaccinated. However, they tended to underestimate their risks of contracting COVID-19. Disease exposure led to higher uptake intent via the mediation of fear. Safety concerns negatively influenced vaccination intention, while perceived community benefits were positively associated with vaccination intention. Positive attitudes toward vaccines and recent vaccine history were positively linked to vaccination intent.
Conclusion
This study attests the effectiveness of HBT constructs in predicting people’s intention to receive a COVID-19 vaccine.
Practice Implications
The results point to the importance of fostering confidence in vaccine safety and countering overoptimism of individual susceptibility to the disease in interventions promoting COVID-19 vaccines uptake.
Keywords: COVID-19, COVID-19 vaccine, HBM, TPB, EPPM
1. Introduction
The coronavirus disease-2019 (COVID-19) pandemic has caused catastrophic damages worldwide [1]. As of early 2021, more than 80 million cases of infections and 2 million deaths have been reported worldwide [1]. However, as effective treatment of the disease remains unavailable, societies are relying on preventive measures to curb the pandemic [2,3]. One of the most effective preventive measures to contain the spread of infectious diseases is vaccine [4]. Effective vaccination fosters individual immunity against vaccine preventable diseases (VPD) and protect those unable to get vaccines through “herd immunity” [5]. However, despite its effectiveness in preventing infectious diseases, vaccine hesitancy is on the rise globally, leading to the re-emergence of VPDs such as measles [6,7]. Though public health institutions worldwide have been disseminating vaccines to control the pandemic, polls show that many were reluctant to get vaccinated [8]. To develop effective interventions that promote acceptance of COVID-19 vaccines, it is critical to identify factors that influence people’s intention to get vaccinated.
1.1. Health behavior theories
Decades of research in health psychology have generated multiple health behavior theories (HBT) that identify sociopsychological factors influencing individual’s health behavior [9]. Studies on vaccines uptake ranging from childhood vaccines [10] to HPV vaccines [11] also benefited tremendously from HBTs, such as in predicting parents’ intention to vaccinate their children for VPDs [10] and individuals’ intention to vaccinate themselves against HPV infection [11]. Notably, most HBTs focus on several similar sets of factors that predict the initiation and maintenance of health behaviors [9,12]. Correspondingly, researchers have rallied for the comparative examination, refinement, and integrations of different HBTs [9,11,12]. In the meantime, the novel challenges brought about by the COVID-19 pandemic also necessitate a comprehensive investigation of factors that predict people’s intention to get the COVID-19 vaccines. On the one hand, it aids the strategic design of vaccine promotion campaigns addressing factors that reduce voluntary vaccination. On the other, knowing who are more likely to receive a vaccine helps authorities plan the distribution of COVID-19 vaccines.
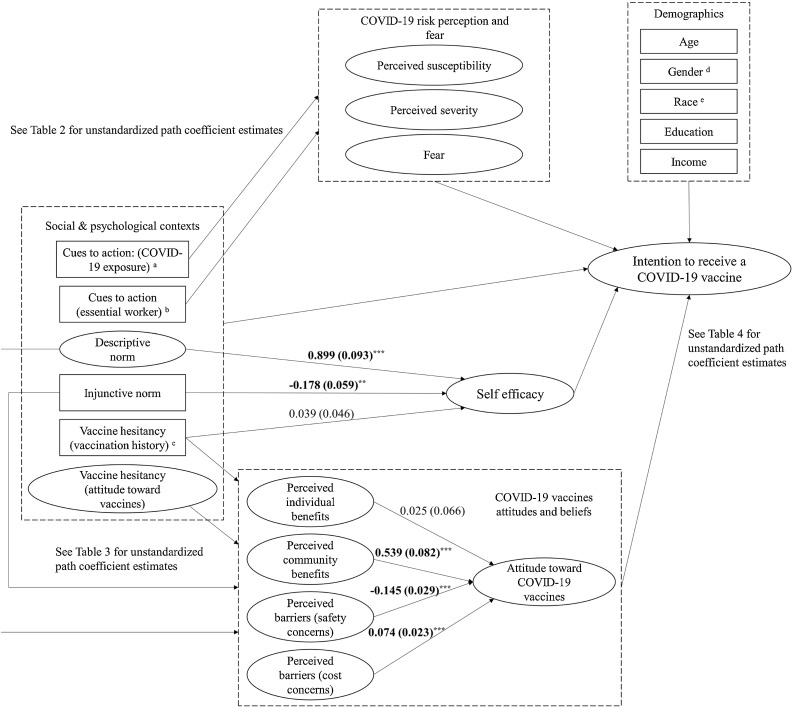
To address such goals, this study examines five sets of HBT constructs and seeks to identify their influences on people’s intention to receive a COVID-19 vaccine. Based on three prominent HBTs including the health belief model (HBM) [13], the theory of planned behavior (TPB) [14], and extended parallel process model (EPPM) [15], we focus on factors including risk perception and fear associated with COVID-19, attitudes and beliefs related to COVID-19 vaccines, self-efficacy, social and psychological contexts, and demographics (Fig. 1 ). Notably, as COVID-19 vaccines were not widely available in the United States when this study was conducted, we focus on the intention to get COVID-19 vaccines due to its strong association with the actual uptake behavior [11,14].
Fig. 1.
Theoretical framework.
1.1.1. COVID-19 risk perception and fear
Vaccination, like many health behaviors, is adopted to prevent negative health consequences such as suffering from VPDs [16]. It is thus arguable that the extent to which people believe a VPD is severe and likely to affect them should predict their intention to get vaccinated [12]. HBM and EPPM measures people’s perception of health risks with similar constructs, including perceived severity of and perceived susceptibility to health threats [9].
In addition to risk perception, HBTs also suggest that affective response to health risks motivate actions to overcome their adverse effects [15,17]. Fear as a negative emotion was particularly relevant to behavioral change [18]. For instance, research shows that increased fear from reading a narrative message motivated female research participants to receive an HPV vaccine [18]. It is worth noting that too much fear could also prevent action as people may just disregard the threats to avoid feeling overwhelmed [15]. In the context of COVID-19 vaccination, the large number of infections and casualties may have led to heightened risk perception and strong fear [19]. However, the prolonged pandemic and the lower mortality rates among younger populations may also lead to fatigue of practicing preventive measures and overoptimism of one’s susceptibility to the disease. As a consequence, some may hesitate to get a COVID-19 vaccine due to lower risk perception and fear.
1.1.2. COVID-19 vaccines attitudes and beliefs
In addition to risk perception and fear, HBTs argue that attitudes toward and beliefs about the health behaviors also shape people’s intention to adopt them [9,11]. They are often operationalized as perceived benefits and barriers in HBM, response efficacy in EPPM, and positive or negative behavioral beliefs in TPB [9]. These factors can be categorized into two subgroups, respectively capturing the benefits and barriers associated with the health behaviors. In vaccine research, perceived benefits of vaccines (e.g., reduced disease threat) were found to be strong predictors of vaccination intention, while perceived cost or barriers (e.g., monetary cost, effort exertion) of getting vaccinated were negatively associated with uptake intent (e.g., influenza vaccine [20], HPV vaccines [21], Zika Vaccine [22]).
In the context of COVID-19 vaccines, we focus on five interrelated attitudes and beliefs associated with the vaccines, including perceived benefits of getting COVID-19 vaccines for self and communities, perceived barriers of getting COVID-19 vaccines, and attitudes toward to getting COVID-19 vaccines. Notably, perceived benefits and barriers are conceptually similar to positive and negative behavioral beliefs specified in TPB [12]. Such beliefs, according to TPB, shape people’s attitudes toward the behavior, which subsequently influence behavioral intent [9].
1.1.3. Self-efficacy
Knowing that health behaviors such as getting vaccinated prevent negative consequences may not be enough to motivate behavioral adoption [9,12]. HBTs argue that feeling capable of executing such behaviors are also key to behavioral change [23,24]. Such perceived capability is conceptualized as perceived behavioral control in TPB and self-efficacy in EPPM [9]. Recent TPB studies often operationalize perceived behavioral control as self-efficacy due to their similarities [9,25]. Research also shows that self-efficacy is positively related to vaccines uptake [26,27].
1.1.4. Social and psychological context
We extract three sets of contextual factors from HBTs and vaccine research, including subjective norms (TPB [28]), cues to action (HBM [11]), and baseline vaccine hesitancy [6]. Subjective norms include injunctive norms, which are approvals of health behaviors by people important to the health decision-maker, and descriptive norms, which denote important others’ behaviors [29]. TPB research shows that both perceived descriptive and injunctive norms are positively related to vaccines uptake [30,31].
Cues to action specifies motives and hints of actions embedded in one’s surrounding environment such as doctor’s recommendations [11]. Research also shows that disease exposure or knowledge of VPDs are positive predictors of vaccines uptake [27]. In the COVID-19 context, it is possible that exposure to COVID-19 cases such having family or friends tested positive for COVID-19 may function as a behavioral cue [6]. Further, serving as an essential worker during the COVID-19 lockdowns may also be a cue to action. On the one hand, essential workers may be more susceptible to the disease due to the risk of exposure, while on the other, public health officials have called for earlier vaccination for this group [2,3].
The last set of contextual factors include baseline vaccine hesitancy, which describes the attitudes and behaviors surrounding people’s decision to delay and refuse vaccination [6]. Vaccine hesitancy is often operationalized as attitudes toward vaccines or past vaccination behavior [6,7]. Research shows that positive attitudes toward vaccines in general are positively associated with people’s intent to get specific vaccines [6,32], and individuals who have received vaccines recently are more likely to get other vaccines [33].
In addition to their direct effects, risk perception, fear, self-efficacy, and beliefs about COVID-19 vaccines may also mediate contextual factors’ influence on vaccination intention. First, social cognitive theory suggests that people learn not only by directly interacting with the environment, but also by vicariously observing other’s actions [34]. Therefore, socially important others’ beliefs and behaviors may influence people’s evaluation of the vaccine and their confidence in getting vaccinated [11,35]. In terms of COVID-19 vaccines, it is likely that subjective norms may influence self-efficacy, which would subsequently influence uptake intent. Second, people’s perception of the vaccines may also be influenced by their existing attitudes toward other vaccines [6,7]. Thus, attitudes toward COVID-19 vaccines may mediate baseline vaccine-hesitancy’s influences on intention to receive a COVID-19 vaccine. Third, as exposure to COVID-19 cases and serving as essential workers may lead to higher contraction risk and elevated risk perception, severity and susceptibility perception may also mediate its impacts on uptake intent. Lastly, recent vaccination history may boost self-efficacy which would lead to increased uptake intent, as successful past experiences are often positively related to self-efficacy [34].
1.1.5. Demographic factors
Lastly, demographic factors are also associated with vaccines uptake intent. Due to historical and cultural reasons, minorities in the United States are often reluctant to receive novel medical treatment [36,37]. Gender difference in vaccination behavior was also observed in some studies, but the patterns of such difference vary across contexts [38]. Older adults and individuals with higher education and income often show higher vaccination intention [[39], [40], [41]].
1.2. Hypotheses and research questions
To address the challenges of the COVID-19 pandemic and aid the strategic promotion and distribution of COVID-19 vaccines, we utilize three HBTs to identify sociopsychological factors that influence American’s intention to receive a COVID-19 vaccine. Based on HBM and EPPM, we hypothesize that perceived susceptibility to and severity of COVID-19 and fear will be positively associated with people’s intention to get a COVID-19 vaccine (H1). According to TPB and EPPM, we hypothesize that self-efficacy is positively related to vaccination intention (H2). Synthesizing HBM, EPPM, and TPB, we ask three research questions. First, are perceived benefits and barriers of COVID-19 vaccination associated with uptake intent directly or indirectly via the mediation of attitudes toward COVID-19 vaccines (RQ1)? Second, are contextual factors (i.e., subjective norms, cues to action, and vaccine hesitancy) directly and indirectly associated with people’s intention to receive a COVID-19 vaccine (RQ2)? Lastly, how are demographic characteristics associated with vaccination intention (RQ3)?
2. Method
Upon IRB approval at the lead author’s institution, data collection was completed during early September 2020. A sample of participants with demographics similar to the United States population was recruited on Prolific.co. 1043 Individuals opened the survey, and 1027 continued with informed consent. Among them, 1001 participants completed the survey and were rewarded 2.00 U.S. dollars. Response from 54 participants who failed one or two attention check questions were removed. Responses from 13 participants who indicated that they were tested positive for COVID-19 and/or COVID-19 antibody were dropped, resulting in a final sample of 934 participants.
2.1. Instruments
HBT and vaccine research constructs including perceived severity of and susceptibility to COVID-19, fear of COVID-19 [18,27], perceived individual benefits of COVID-19 vaccines [11,42], perceived community benefits of COVID-19 vaccines, perceived barriers to getting COVID-19 vaccines including safety concerns and cost concerns [21], subjective norms, baseline vaccine hesitancy including attitudes toward vaccines in general and recent vaccination history, cues to actions, and demographics were measured in the survey. Measurement items, reliability indices, means, and standard deviations of the measurement instruments are presented in Table 1 . Scales were adopted from existing research if available.
Table 1.
Descriptive statistics and composite reliability of survey measures.
| M | SD | Reliability | |
|---|---|---|---|
| COVID-19 risk perception and fear | |||
| Perceived susceptibility to COVID-19 | 3.35 | .78 | α = .74 |
| It is likely that I will get COVID-19. (1 “strongly disagree” to 5 “strongly agree”) | 2.77 | .88 | |
| I am at risk of getting COVID-19. | 3.54 | 1.04 | |
| It is possible that I will get COVID-19. | 3.75 | .94 | |
| Perceived severity of COVID-19 | 4.21 | .89 | α = .92 |
| I believe that COVID-19 is a severe health problem. (1 “strongly disagree” to 5 “strongly agree”) | 4.24 | .99 | |
| I believe that COVID-19 has serious negative consequences. | 4.29 | .87 | |
| I believe that COVID-19 is extremely harmful. | 4.12 | 1.00 | |
| Fear | 2.68 | 1.33 | α = 0.96 |
| On a scale of 1 (not at all) to 5 (very much), please indicate how you feel when you think about COVID-19: Fear | 2.71 | 1.37 | |
| … Afraid | 2.66 | 1.41 | |
| … Scared. | 2.67 | 1.395 | |
| COVID-19 vaccines attitudes and beliefs | |||
| Attitude toward COVID-19 vaccines | 4.16 | 1.19 | α = 0.98 |
| Using the following adjective scales, please indicate how much you feel that getting vaccinated for COVID-19 is: 1 "Negative" to 5 "Positive" | 4.40 | 1.04 | |
| … 1 "Unfavorable" to 5 "Favorable" | 4.38 | 1.08 | |
| … 1 "Bad" to 5 "Good" | 4.44 | 1.01 | |
| … 1 "Harmful" to 5 "Beneficial" | 4.41 | 1.02 | |
| … 1 "Foolish" to 5 "Wise" | 4.45 | 1 | |
| Perceived individual benefits of COVID-19 vaccines | 3.75 | 0.86 | α = 0.91 |
| COVID-19 vaccines will work in preventing the disease. (1 “strongly disagree” to 5 “strongly agree”) | 3.71 | 0.92 | |
| COVID-19 vaccines will be effective in preventing COVID-19. | 3.64 | 0.89 | |
| If I get the vaccines, I will be less likely to get COVID-19. | 3.89 | 0.99 | |
| Perceived community benefits of COVID-19 vaccines | 4.10 | 0.94 | r = 0.85 |
| Having myself vaccinated against COVID-19 is beneficial for the health of others in my community. (1 “strongly disagree” to 5 “strongly agree”) | 4.13 | 1.01 | |
| COVID-19 vaccines protect the health of my community. | 4.08 | 0.96 | |
| Perceived barriers of getting COVID-19 vaccines (safety concerns) | 3.31 | 1.23 | α = 0.88 |
| How much would the following factors prevent you from getting vaccinated for COVID-19: Concerns about whether COVID-19 vaccines are safe (1 = not at all, 5 = a great deal) | 3.39 | 1.38 | |
| Not enough research done on COVID-19 vaccines | 3.36 | 1.36 | |
| I have concerns about possible side effects of COVID-19 vaccines | 3.18 | 1.37 | |
| Perceived barriers of getting COVID-19 vaccines (cost concerns) | 2.01 | 1.07 | α = 0.80 |
| How much would the following factors prevent you from getting vaccinated for COVID-19: Vaccine cost (it's too expensive) (1 "not at all" to 5 "a great deal") | 2.32 | 1.38 | |
| I'm not sure how to file the insurance claim to get reimbursed | 1.72 | 1.11 | |
| My insurance may not cover COVID-19 vaccine | 1.98 | 1.28 | |
| Self-efficacy | 3.5 | 0.76 | α = 0.77 |
| I will be able to get the vaccines to prevent contracting COVID-19. (1 “strongly disagree” to 5 “strongly agree”) | 3.67 | 0.85 | |
| It will be easy for me to get the vaccines to protect myself from COVID-19. | 3.42 | 0.86 | |
| Getting vaccinated to prevent COVID-19 is convenient. | 3.43 | 1.02 | |
| Social and psychological contexts | |||
| Cues to action (COVID-19 exposure) | |||
| Have you experienced any of the following in the past 9 months? Tested positive for COVID-19 (excluded from final sample) | n = 10 | ||
| Tested positive for COVID-19 antibody (excluded from final sample) | n = 3 | ||
| Hospitalized due to COVID-19 (excluded from final sample) | n = 1 | ||
| Family or close friend tested positive for COVID-19 | 0.21 (n = 197) | ||
| Someone you knew tested positive for COVID-19 | 0.37 (n = 342) | ||
| Exposed to people who have got COVID-19 | 0.08 (n = 73) | ||
| Treating patients with COVID-19 | 0.01 (n = 12) | ||
| Taking care of someone with COVID-19 | 0.01 (n = 9) | ||
| Family or close friend passed away due to COVID-19 | 0.05 (n = 46) | ||
| Someone you knew passed away due to COVID-19 | 0.12 (n = 115) | ||
| None of above | 0.50 (n = 464) | ||
| Cues to action (served as essential worker) | |||
| Were you an essential worker during the COVID-19 lockdown? (1 "yes", 0″no") | 0.18 (n = 170) | ||
| Subjective norm (descriptive norm) | 3.69 | 0.9 | r = 0.66 |
| Most people who are like me will get vaccinated for COVID-19. (1 "strongly disagree", 5 "strongly agree") | 3.66 | 0.99 | |
| Most people who are important to me will get vaccinated for COVID-19. | 3.71 | 0.98 | |
| Subjective norm (injunctive norm) Most people who are important to me think that I should get COVID-19 vaccines (1 "strongly disagree", 5 "strongly agree") | 3.67 | 1.07 | |
| Baseline vaccine hesitancy (attitude toward vaccines in general) | 4.42 | 0.99 | α = 0.98 |
| Using the following adjective scales, please indicate how much you feel that getting vaccines is: 1 "Negative" to 5 "Positive" | 4.40 | 1.04 | |
| … 1 "Unfavorable" to 5 "Favorable" | 4.38 | 1.08 | |
| … 1 "Bad" to 5 "Good" | 4.44 | 1.01 | |
| … 1 "Harmful" to 5 "Beneficial" | 4.41 | 1.02 | |
| … 1 "Foolish" to 5 "Wise" | 4.45 | 1 | |
| Baseline vaccine hesitancy (vaccination history). Have you received any vaccine such as flu shot in the past 18 months? - Yes | 0.51 (n = 480) | ||
| No | 0.47 (n = 441) | ||
| Not sure | 0.02 (n = 13) | ||
| Intention to receive a COVID-19 vaccine | 3.98 | 1.25 | α = 0.98 |
| One the scale of 1 (very unlikely) to 5 (very likely), please indicate the likelihood that you will: Consider getting COVID-19 vaccines. | 4.15 | 1.25 | |
| … Try to get COVID-19 vaccines. | 3.88 | 1.32 | |
| … Actually get vaccinated for COVID-19. | 3.86 | 1.31 | |
| … Get vaccinated if a physician offered you COVID-19 vaccines. | 4.02 | 1.29 | |
2.2. Analysis
Q-Q plot was generated in R to assess multivariate normality of the measurement items [43]. Upon inspection, the data failed to achieve multivariate normality. To account for non-normality, all measurement and path models were analyzed with maximum likelihood estimation with robust standard errors [44]. Indirect effect models were estimated with maximum likelihood estimation with bootstrapped sub-samples (N = 5000).
We first inspected the measurement model [45]. The model has achieved satisfactory fit based on conventional criteria (Adjusted χ² (df = 636) = 1207.693, CFI = 0.981, TLI = 0.977, RMSEA = 0.031, 95% confidence interval of RMSEA = [0.028, 0.034], SRMR = 0.039) [45,46].
A path model based on the theoretical framework illustrated in Fig. 1 was then estimated. Latent HBT constructs without directional effects specified between each other were allowed to covary to account for common method and conceptual covariances. The path model also fits the data well (Adjusted χ² (df = 1127) = 2314.812, CFI = 0.965, TLI = 0.962, RMSEA = 0.034, 95% confidence interval of RMSEA = [0.032, 0.036], SRMR = 0.054) [45,46].
3. Results
Path coefficient estimates are reported in Fig. 2 and Table 2, Table 3, Table 4 . Indirect effects are reported in Table 5 . The path model was able to predict 82.1% of variance in participants’ COVID-19 vaccines uptake intent (R 2 = .821).
Fig. 2.
Unstandardized path coefficient estimates (B(SE)).
Note.a Dummy-coded variable (1 = knowing someone who was tested positive for or died due to COVID-19, 0 = not having such experience).
bdummy-coded variable (1 = served as an essential worker during COVID-19 lockdowns; 0 = did not serve as an essential worker during COVID-19 lockdowns).
cdummy-coded variable (1 = received vaccines in the past 18 months, 0 = did not receive vaccine in the past 18 months or not sure).
ddummy-coded variable with male as reference group.
edummy-coded variable with non-Hispanic White or Caucasian as reference group.
*p < .05; **p < .01; ***p < .001.
Table 2.
Unstandardized coefficients estimate for paths predicting perceived susceptibility to, perceived severity and fear of COVID-19.
| Perceived susceptibility | Perceived severity | Fear | |
|---|---|---|---|
| B (SE) | B (SE) | B (SE) | |
| Cues to action (exposure) | 0.218 (0.041) *** | 0.257 (0.063) *** | 0.376 (0.085) *** |
| Cues to action (essential worker) | 0.134 (0.051) ** | −0.046 (0.08) | −0.216 (0.107) * |
Note. *p< .05; **p< .01; ***p< .001; significant path estimates are in boldface; outcome variables are specified in the first row.
Table 3.
Unstandardized coefficient estimates for paths predicting perceived individual and community benefits and perceived safety and const concerns of COVID-19 vaccines and attitudes toward COVID-19 vaccines.
| Perceived individual benefit | Perceived community benefits | Perceived barriers (safety concerns) | Perceived barriers (cost concerns) | Attitude toward COVID-19 vaccines | |
|---|---|---|---|---|---|
| B (SE) | B (SE) | B (SE) | B (SE) | B (SE) | |
| Vaccine hesitancy (attitude toward vaccines) | 0.273 (0.041) *** | 0.423 (0.044) *** | −0.129 (0.062) * | 0.143 (0.059) * | 0.471 (0.056) *** |
| Vaccine hesitancy (vaccination history) | −0.093 (0.043) * | −0.079 (0.04) * | −0.179 (0.081) * | −0.319 (0.088) *** | −0.019 (0.048) |
| Injunctive norm | −0.079 (0.051) | 0.03 (0.05) | −0.003 (0.08) | 0.016 (0.089) | 0.07 (0.045) |
| Descriptive norm | 0.709 (0.098) *** | 0.609 (0.094) *** | −0.663 (0.141) *** | −0.347 (0.152) * | −0.047 (0.097) |
Note. *p< .05; **p< .01; ***p< .001; significant path estimates are in boldface; outcome variables are specified in the first row.
Table 4.
Unstandardized coefficient estimates for paths predicting intention to receive a COVID-19 vaccine.
| B (SE) | |
|---|---|
| Contextual cues and baseline vaccine hesitancy | |
| Vaccine hesitancy (attitude toward vaccine) | 0.113 (0.043)** |
| Vaccine hesitancy (vaccination history) | 0.144 (0.044)*** |
| Injunctive norm | 0.046 (0.058) |
| Descriptive norm | 0.410 (0.174)* |
| Cues to action (exposure) | 0.048 (0.039) |
| Cues to action (essential worker) | 0.030 (0.051) |
| Risk perception and fear | |
| Perceive susceptibility | 0.114 (0.062) |
| Perceived severity | 0.002 (0.040) |
| Fear | 0.050 (0.018)** |
| Beliefs about COVID-19 vaccines | |
| Perceived individual benefits | 0.044 (0.085) |
| Perceived community benefits | 0.228 (0.089)** |
| Perceived barriers (safety concerns) | −0.118 (0.027)*** |
| Perceived barriers (cost concerns) | 0.009 (0.026) |
| Attitudes toward COVID-19 vaccines | 0.276 (0.044)*** |
| Self-efficacy | |
| Self-efficacy | −0.158 (0.120) |
| Demographics | |
| Age | 0.001 (0.001) |
| Female 1 | −0.071 (0.037) |
| Other gender 1 | 0.001 (0.128) |
| Black or African American 2 | −0.116 (0.061) |
| Hispanic or Latino 2 | −0.099 (0.082) |
| Asian, Pacific Islander, and Native American 2 | 0.088 (0.061) |
| Other racial groups 2 | 0.017 (0.135) |
| Education | 0.009 (0.013) |
| Income | −0.004 (0.01) |
Note. 1 dummy-coded variable with male as reference group; 2 dummy-coded variable with non-Hispanic White or Caucasian as reference group; *p< .05; **p< .01; ***p< .001; significant path estimates are in boldface.
Table 5.
Total direct and indirect effects of contextual factors and COVID-19 vaccines attitudes and beliefs on intention to receive COVID-19 vaccines.
| Total effect |
Total indirect effect |
Direct effect |
||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI 1 | Estimate | 95% CI 1 | Estimate | 95% CI 1 | |
| COVID-19 vaccines attitudes and beliefs | ||||||
| Cues to action 3 (COVID-19 exposure) | 0.092 | [0.013, 0.170] | 0.044 | [0.013, 0.075] | 0.048 | [-0.033, 0.128] |
| Cues to action 4 (essential worker) | 0.034 | [-0.074, 0.142] | 0.005 | [-0.024, 0.033] | 0.030 | [-0.079, 0.138] |
| Vaccine hesitancy (vaccination history) | 0.117 | [0.018, 0.216] | −0.027 | [-0.084, 0.03] | 0.144 | [0.054, 0.234] |
| Vaccine hesitancy (attitude toward vaccines) | 0.440 | [0.340, 0.539] | 0.327 | [0.235, 0.42] | 0.113 | [0.024, 0.201] |
| Social and psychological contexts | ||||||
| Descriptive norm | 0.614 | [0.385, 0.844] | 0.205 | [-0.106, 0.515] | 0.410 | [-0.038, 0.858] |
| Injunctive norm | 0.102 | [-0.022, 0.225] | 0.056 | [-0.027, 0.138] | 0.046 | [-0.097, 0.189] |
| Perceived individual benefits | 0.051 | [-0.136, 0.238] | 0.007 | [-0.031, 0.045] | 0.044 | [-0.138, 0.226] |
| Perceived community benefits | 0.376 | [0.180, 0.572] | 0.149 | [0.078, 0.219] | 0.228 | [0.032, 0.424] |
| Perceived barriers (safety concerns) | −0.158 | [-0.215, -0.101] | −0.040 | [-0.061, -0.019] | −0.118 | [-0.174, -0.062] |
| Perceived barriers (cost concerns) | 0.029 | [-0.025, 0.084] | 0.020 | [0.007, 0.034] | 0.009 | [-0.045, 0.063] |
Note. 1 bootstrapped 95% confidence interval (N = 5000); 2 dummy-coded variable (1 = knowing someone tested positive or died due to COVID-19, 0 = not having such experience); 3 dummy-coded variable (1 = served as an essential worker during the COVID-19 lockdowns, 0 = not having such experience); statistically significant effects are in boldface.
3.1. Demographics
The average age of participants was 46.01 years (SD = 16.17). The majority of participants identified as female (n = 468, 50.1%), followed by male (n = 455, 48.7%) and other gender (n = 11, 1.2%). Approximately three quarters of participants identified as non-Hispanic White or Caucasian (n = 698, 74.7%), followed by Black or African American (n = 114, 12.2%), Hispanic or Latino (n = 34, 3.6%), Asian, Pacific Islander or Native American (n = 68, 7.3%), and other racial groups (n = 20, 2.1%). The median education level was 4-year college degree, and the median household income was between US$ 50,000 and 74,999. RQ3 asks about demographic factors’ association with COVID-19 vaccines uptake intent. No significant effect of the demographic variables was identified after controlling for the HBT constructs.
3.2. COVID-19 risk perception and fear
In general, participants perceived COVID-19 as a severe health risk. However, mean perceived susceptibility was significantly lower than perceived severity (paired-sample t(933) = 28.70, p < .001). The average rating for fear was below the scale mid-point, suggesting that participants were not very fearful of the disease. H1 was partially supported as only fear was positively associated with intention to receive a COVID-19 vaccine. However, perceived susceptibility’s association with vaccination intention was approaching statistical significance (B = 0.114, SE = 0.062, p = 0.064).
3.3. COVID-19 vaccines attitudes and beliefs
Participants showed positive attitudes toward COVID-19 vaccines. They also perceived COVID-19 vaccines as beneficial to both themselves and their communities. Participants reported that concerns about vaccine safety were more likely to prevent vaccination than concerns about cost (paired-samplet(933) = 28.36, p < .001). In response to RQ1, we found that perceived community benefits of and positive attitudes toward COVID-19 vaccines were positively associated with intention to get the vaccines. However, stronger safety concerns were related to lower vaccination intention. In addition to their direct effects, beliefs about COVID-19 vaccines’ benefits and barriers also indirectly influenced intention to receive a COVID-19 vaccine (RQ1b). Attitudes toward COVID-19 vaccines mediated perceived community benefits and safety concerns’ association with uptake intent, but the former was positive while the latter was negative. Interestingly, attitudes toward COVID-19 vaccines also mediated cost concerns’ positive relationship with vaccines uptake.
3.4. Self-efficacy
Our respondents generally believed that they will be able to get COVID-19 vaccines to prevent contracting COVID-19. Different from existing research findings, no significant relationship was identified between self-efficacy and intention to get vaccinated for COVID-19, rejecting H2.
3.5. Contextual cues and baseline vaccine hesitancy
More than half of our sample had some experiences with COVID-19. Particularly, more than one third of participants knew someone who was tested positive for COVID-19 and more than 20% of participants reported having family or close friends tested positive for COVID-19. Further, more than one hundred respondents indicated that someone they knew died due to COVID-19, again showing the dire situation of the pandemic. About 20% of our respondents indicated that they worked as an essential worker during COVID-19 lockdowns. As for subjective norms, participants in general believed people similar to them or important to them would get a COVID-19 vaccine (i.e., descriptive norms) and would want them to get vaccinated against COVID-19 (i.e., injunctive norms). In terms of baseline vaccine hesitancy, our participants largely thought of vaccines positively and more than half of them reported that they had received at least one vaccine in the past 18 months prior to completing the survey.
In response to RQ2, we found that having positive baseline attitudes toward vaccines in general and received some vaccines recently were positive predictors of intention to receive a COVID-19 vaccine. Further, descriptive norms were also positively associated with vaccination intentions. Though exposure to COVID-19 cases was not directly linked to uptake intent, fear mediated its positive relationship with vaccination intention. Additionally, the relationship between attitudes to vaccines in general and intention to receive a COVID-19 vaccine was mediated by perceived benefits and attitudes toward COVID-19 vaccines specifically.
4. Discussion and conclusion
The current study integrates factors from three prominent HBTs including EPPM, HBM, and TPB to investigate sociopsychological factors associated with American’s intentions to get COVID-19 vaccines. In general, participants indicated that they were likely to get vaccinated for COVID-19 once the vaccines are available. This finding is encouraging as massive vaccination is key to controlling the spread of COVID-19 [3]. However, approximately 20% of participants reported some extent of unwillingness to get the vaccines (average uptake intent score below the scale mid-point). Considering that herd immunity against VPDs sometimes require an immunization rate of 70%–90% and the immunity against COVID-19 developed by vaccination may not last as long as immunity for other diseases [2], efforts are needed to design and implement interventions that effectively promote vaccination, especially among populations reluctant to get the vaccines.
4.1. COVID-19 risk perception and fear
Participants in general perceived COVID-19 as a severe health risk. However, they tend not to feel very vulnerable to and afraid of the disease. Such findings show that people were generally optimistic about their own risks of suffering from COVID-19, which is consistent with the optimistic bias observed in earlier research [3,19].
There are two possible explanations for the finding that fear was positively associated with intention to receive a vaccine. First, fear as emotional response may arise from cognitive appraisals of COVID-19 and served as a more immediate predictor of vaccination intention than susceptibility perception [47]. Second, we may fail to capture any effect of severity perception due to its limited variance (i.e., ceiling effect). In summary, the general public may have recognized the severity of COVID-19, but the underestimation of their risks of contracting and suffering from the disease may prevent them from getting vaccinated. Campaigns to promote COVID-19 vaccines should consider highlighting personal risks to the disease and using fear appeal messages when communicating to populations that are less susceptible to COVID-19 (e.g., younger population).
4.2. COVID-19 vaccines attitudes and beliefs
Our findings indicate that Americans held a generally positive view toward COVID-19 vaccines. They considered the vaccines as beneficial to both themselves and their communities. However, the accelerated development of the vaccines, especially in comparison to earlier vaccines, may have led to heightened safety concerns [3]. Cost concerns, on the other hand, was not a serious barrier to people’s vaccination intentions.
More importantly, we found that perceived community benefit of COVID-19 vaccines was positively associated with vaccination intention both directly and indirectly through the mediation of attitudes toward the COVID-19 vaccines. Differently, concerns about the safety of COVID-19 vaccines were negatively associated with uptake intent, directly and indirectly through the mediation of attitudes toward the COVID-19 vaccines. Therefore, public health campaigns aiming at increasing the vaccination rate should address the community benefits of COVID-19 vaccines, while also maintain high level of transparency regarding the vaccines’ safety and effectiveness. Notably, we also found that cost concerns were positively associated with intention to get vaccinated for COVID-19, and the relationship was mediated by attitudes toward the COVID-19 vaccines. Such pattern is consistent with earlier finding where practical concerns were positively linked to behavioral intention [21]. Therefore, providing the vaccines at a reasonable cost or for free may help increase vaccination rates, especially among people who intend to get vaccinated.
4.3. Self-efficacy
We found that participants were confident in their ability to get the COVID-19 vaccines. However, self-efficacy was not significantly associated with vaccination intention. The absence of a significant relationship may be attributable to the fact that vaccines were still not available. As the transtheoretical model (TTM) of behavioral change suggests, difference in self-efficacy tend to develop at later stages of people’s health decision-making [48]. Limited variance in self-efficacy may thus prevent us from identifying its relationship with vaccination intention. Notably, injunctive and descriptive norms were differently associated with self-efficacy. Believing that important others will get the vaccines (i.e., descriptive norms) was positively related to self-efficacy, whereas the relationships was negative between beliefs that important others would want oneself to get vaccinated (i.e., injunctive norms) and self-efficacy. Such difference may emerge as people learn from others’ behaviors [34], but too much preaching may also lead to psychological reactance.
4.4. Contextual cues and baseline vaccine hesitancy
Our findings confirm the widespread of COVID-19 cases and mortalities reported elsewhere [1,19]. First-hand experience with the disease was related to heightened fear and increased intention to get vaccinated. Such finding may indicate that exposure to COVID-19 countered the negative influences of overoptimism on vaccination intention. Therefore, campaigns encouraging vaccination against COVID-19 may stress the personal relevance of COVID-19 as a means to overcome overoptimism and stipulate vaccination intention. It is also encouraging to see that most participants held positive views toward vaccines and considered getting COVID-19 vaccines a socially sanctioned behavior. Baseline attitudes toward vaccines and the vaccine-friendly norms were also conducive to vaccination intention. Therefore, promotion of COVID-19 vaccines should be considered as an integral part of the long-term efforts to reduce vaccine hesitancy [6]. It is necessary to not only foster acceptance of the COVID-19 vaccines, but also cultivate an enduring trust in vaccines and other health measures.
4.5. Limitations
This study also has some limitations. First, the online sample may limit the generalizability of our findings. Future research should consider recruiting a more diverse sample and re-examine the relationships reported here. Second, as the COVID-19 vaccines were yet to be widely available when this study was conducted, actual vaccines uptake was not measured. Though behavioral intention and actual behaviors tend to correlate highly [14], we recommend future research to test the current framework at later stage of the pandemic or with other vaccines and health behaviors.
4.6. Conclusion
Integrating findings from prominent HBTs, this study offers a timely overview of sociopsychological factors that are related to American’s intention to get vaccinated for COVID-19. We found that despite recognizing the severity of the disease, people felt less susceptible to and afraid of its negative consequences. Such overoptimism may prevent wide acceptance of COVID-19 vaccines. Further, safety concerns are negatively associated with vaccination intention. Lastly, public acceptance of COVID-19 vaccines was largely influenced by their perceptions of vaccines in general, which confirms the importance of sustained efforts in cultivating vaccine acceptance.
4.7. Practice implications
Findings from the current study has several implications for health campaigns and education aiming at promoting COVID-19 vaccination. First and foremost, the prolonged struggle caused by the pandemic may have led to fatigue of practicing preventive measures and overoptimism in people’s (in)vulnerability to the disease. Therefore, it is important for health communicators to emphasize the personal relevance of the disease and foster adequate amount of fear among the public. Second, campaigns need to address the safety concerns associated with COVID-19 vaccines. It is imperative to remain transparent and truthful in communications about the vaccines, as public confidence in the vaccines’ safety and effectiveness are closely associated with their intention to receive a COVID-19 vaccine. Third, the vaccines’ community benefits need to be highlighted in campaigns and education materials. This is especially true considering that some populations such as young people may think of themselves as less susceptible to the disease and less in need of a vaccine. Informing this group about the collective benefits of COVID-19 vaccines may encourage them to actually get vaccinated. Lastly, as the results indicate, COVID-19 vaccine promotion needs to be considered as an integral part of the prolonged effort to cultivate vaccine acceptance in our societies. Long-term investment in the education of vaccines and other health measures needs to be sustained to maximize the effectiveness of preventive medicines.
CRediT authorship contribution statement
Haoran Chu: Conceptualization, Methodology, Formal analysis, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization. Sixiao Liu: Conceptualization, Methodology, Validation, Formal analysis, Writing - original draft, Writing - review & editing.
References
- 1.World Health Organization . World Health Organization; 2020. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. [Google Scholar]
- 2.Bloom B.R., Nowak G.J., Orenstein W. “When will we have a vaccine?”—understanding questions and answers about Covid-19 vaccination. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2025331. [DOI] [PubMed] [Google Scholar]
- 3.Schoch-Spana M., Brunson E., Long R., Ravi S., Ruth A., Trotochaud M. Johns Hopkins Center for Health Security; Baltimore: 2020. The Public’s Role in Covid-19 Vaccination: Planning Recommendations Informed by Design Thinking and the Social, Behavioral, and Communication Sciences. [Google Scholar]
- 4.Centers for Disease Control and Prevention Ten great public health achievements--United States, 2001-2010. MMWR Morb. Mortal. Wkly. Rep. 2011;60(19):619. [PubMed] [Google Scholar]
- 5.Betsch C., Böhm R., Korn L., Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat. Hum. Behav. 2017;1(3):1–6. [Google Scholar]
- 6.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J.A. Vaccine hesitancy: an overview. Hum. Vaccin. Immunother. 2013;9(8):1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quinn S.C., Jamison A.M., An J., Hancock G.R., Freimuth V.S. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine. 2019;37(9):1168–1173. doi: 10.1016/j.vaccine.2019.01.033. [DOI] [PubMed] [Google Scholar]
- 8.PEW Research Center . 2020. U.S. Public Now Divided Over Whether to Get COVID-19 Vaccine: Concerns About the Safety and Effectiveness of Possible Vaccine, Pace of Approval Process. [Google Scholar]
- 9.Noar S.M., Zimmerman R.S. Health behavior theory and cumulative knowledge regarding health behaviors: are we moving in the right direction? Health Educ. Res. 2005;20(3):275–290. doi: 10.1093/her/cyg113. [DOI] [PubMed] [Google Scholar]
- 10.Chen M.-F., Wang R.-H., Schneider J.K., Tsai C.-T., Jiang D.D.-S., Hung M.-N., Lin L.-J. Using the health belief model to understand caregiver factors influencing childhood influenza vaccinations. J. Commun. Health Nurs. 2011;28(1):29–40. doi: 10.1080/07370016.2011.539087. [DOI] [PubMed] [Google Scholar]
- 11.Gerend M.A., Shepherd J.E. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann. Behav. Med. 2012;44(2):171–180. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein N.D. Testing four competing theories of health-protective behavior. Health Psychol. 1993;12(4):324. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]
- 13.Becker M.H. The health belief model and sick role behavior. Health Educ. Monogr. 1974;2(4):409–419. [Google Scholar]
- 14.Azjen I. Englewood Cliffs; 1980. Understanding Attitudes and Predicting Social Behavior. [Google Scholar]
- 15.Witte K. Fear control and danger control: a test of the extended parallel process model (EPPM) Commun. Monographs. 1994;61(2):113–134. [Google Scholar]
- 16.Brien S., Kwong J.C., Buckeridge D.L. The determinants of 2009 pandemic A/H1N1 influenza vaccination: a systematic review. Vaccine. 2012;30(7):1255–1264. doi: 10.1016/j.vaccine.2011.12.089. [DOI] [PubMed] [Google Scholar]
- 17.Abril E.P., Szczypka G., Emery S.L. LMFAO! Humor as a response to fear: decomposing fear control within the extended parallel process model. J. Broadcast. Electron. Media. 2017;61(1):126–143. doi: 10.1080/08838151.2016.1273921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu S., Yang J.Z., Chu H. When we increase fear, do we dampen hope? Using narrative persuasion to promote human papillomavirus vaccination in China. J. Health Psychol. 2019 doi: 10.1177/1359105319894626. [DOI] [PubMed] [Google Scholar]
- 19.Dryhurst S., Schneider C.R., Kerr J., Freeman A.L., Recchia G., Van Der Bles A.M., Spiegelhalter D., van der Linden S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020:1–13. [Google Scholar]
- 20.Shahrabani S., Benzion U. How experience shapes health beliefs: the case of influenza vaccination. Health Educ. Behav. 2012;39(5):612–619. doi: 10.1177/1090198111427411. [DOI] [PubMed] [Google Scholar]
- 21.Gerend M.A., Shepherd M.A., Shepherd J.E. The multidimensional nature of perceived barriers: global versus practical barriers to HPV vaccination. Health Psychol. 2013;32(4):361. doi: 10.1037/a0026248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guidry J.P., Carlyle K.E., Perrin P.B., LaRose J.G., Ryan M., Messner M. A path model of psychosocial constructs predicting future Zika vaccine uptake intent. Vaccine. 2019;37(36):5233–5241. doi: 10.1016/j.vaccine.2019.07.064. [DOI] [PubMed] [Google Scholar]
- 23.Maloney E.K., Lapinski M.K., Witte K. Fear appeals and persuasion: a review and update of the extended parallel process model. Soc. Personal. Psychol. Compass. 2011;5(4):206–219. [Google Scholar]
- 24.Petrovic K., Burney S., Fletcher J. The relationship of knowledge, health value and health self-efficacy with men’s intentions to receive the human papillomavirus (HPV) vaccine. J. Health Psychol. 2011;16(8):1198–1207. doi: 10.1177/1359105311402861. [DOI] [PubMed] [Google Scholar]
- 25.Ajzen I. Perceived behavioral control, self‐efficacy, locus of control, and the theory of planned behavior 1. J. Appl. Soc. Psychol. 2002;32(4):665–683. [Google Scholar]
- 26.Gargano L.M., Painter J.E., Sales J.M., Morfaw C., Jones L.M., Murray D., Wingood G.M., DiClemente R.J., Hughes J.M. Seasonal and 2009 H1N1 influenza vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination among secondary school teachers and staff. Hum. Vaccin. 2011;7(1):89–95. doi: 10.4161/hv.7.1.13460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brewer N.T., Fazekas K.I. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev. Med. 2007;45(2–3):107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 28.Catalano H.P., Knowlden A.P., Birch D.A., Leeper J.D., Paschal A.M., Usdan S.L. Using the theory of planned behavior to predict HPV vaccination intentions of college men. J. Am. Coll. Health. 2017;65(3):197–207. doi: 10.1080/07448481.2016.1269771. [DOI] [PubMed] [Google Scholar]
- 29.Fishbein M., Ajzen I. Taylor & Francis; 2011. Predicting and Changing Behavior: the Reasoned Action Approach. [Google Scholar]
- 30.Visser O., Hulscher M.E., Antonise-Kamp L., Akkermans R., van der Velden K., Ruiter R.A., Hautvast J.L. Assessing determinants of the intention to accept a pertussis cocooning vaccination: a survey among healthcare workers in maternity and paediatric care. Vaccine. 2018;36(5):736–743. doi: 10.1016/j.vaccine.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 31.Xiao X., Borah P. Do norms matter? Examining norm-based messages in HPV vaccination promotion. Health Commun. 2020:1–9. doi: 10.1080/10410236.2020.1770506. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 33.Marlow L.A., Waller J., Wardle J. Trust and experience as predictors of HPV vaccine acceptance. Hum. Vaccin. 2007;3(5):171–175. doi: 10.4161/hv.3.5.4310. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A., Walters R.H. Prentice-hall Englewood; Cliffs, NJ: 1977. Social Learning Theory. [Google Scholar]
- 35.Stout M.E., Christy S.M., Winger J.G., Vadaparampil S.T., Mosher C.E. Self-efficacy and HPV vaccine attitudes mediate the relationship between social norms and intentions to receive the HPV vaccine among college students. J. Commun. Health. 2020 doi: 10.1007/s10900-020-00837-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cates J.R., Brewer N.T., Fazekas K.I., Mitchell C.E., Smith J.S. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. J. Rural. Health. 2009;25(1):93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- 37.Quinn S.C., Jamison A., Freimuth V.S., An J., Hancock G.R., Musa D. Exploring racial influences on flu vaccine attitudes and behavior: results of a national survey of White and African American adults. Vaccine. 2017;35(8):1167–1174. doi: 10.1016/j.vaccine.2016.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nan X. Communicating to young adults about HPV vaccination: consideration of message framing, motivation, and gender. Health Commun. 2012;27(1):10–18. doi: 10.1080/10410236.2011.567447. [DOI] [PubMed] [Google Scholar]
- 39.Chapman G.B., Coups E.J. Predictors of influenza vaccine acceptance among healthy adults. Prev. Med. 1999;29(4):249–262. doi: 10.1006/pmed.1999.0535. [DOI] [PubMed] [Google Scholar]
- 40.Kumar S., Quinn S.C., Kim K.H., Musa D., Hilyard K.M., Freimuth V.S. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ. Behav. 2012;39(2):229–243. doi: 10.1177/1090198111415105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Larson H.J., Jarrett C., Eckersberger E., Smith D.M., Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32(19):2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 42.Brabin L., Roberts S.A., Farzaneh F., Kitchener H.C. Future acceptance of adolescent human papillomavirus vaccination: a survey of parental attitudes. Vaccine. 2006;24(16):3087–3094. doi: 10.1016/j.vaccine.2006.01.048. [DOI] [PubMed] [Google Scholar]
- 43.Korkmaz S., Goksuluk D., Zararsiz G. MVN: An R package for assessing multivariate normality. R J. 2014;6(2):151–162. [Google Scholar]
- 44.Muthén L., Muthén B. 2018. Mplus, the Comprehensive Modelling Program for Applied Researchers: User’s Guide 5. [Google Scholar]
- 45.Kline R.B. Guilford publications; 2015. Principles and Practice of Structural Equation Modeling. [Google Scholar]
- 46.Hu L.t., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. A. 1999;6(1):1–55. [Google Scholar]
- 47.Slovic P., Finucane M.L., Peters E., MacGregor D.G. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 48.Lipschitz J.M., Fernandez A.C., Larson H.E., Blaney C.L., Meier K.S., Redding C.A., Prochaska J.O., Paiva A.L. Validation of decisional balance and self-efficacy measures for HPV vaccination in college women. Am. J. Health Promot. 2013;27(5):299–307. doi: 10.4278/ajhp.110606-QUAN-240. [DOI] [PubMed] [Google Scholar]