ABSTRACT
Objectives: The purpose of this study was to identify the key constructs associated with symptom description and behavior, natural history of complaints, and previous medical history of cervical arterial dysfunction (CAD) according to a panel of physical therapist (PT) educators.
Methods: An electronic survey was conducted of licensed PT educators currently involved in musculoskeletal physical therapy education within a credentialed program. Survey prompts queried educators to list the subjective and objective items associated with CAD, in open-text format. Responses were coded to identify unique themes (constructs). Principal axis factor analysis with Varimax rotation was performed to identify underlying constructs associated with CAD according to the panel of educators.
Results: Seventy-two educators completed the survey (24.2% response rate) resulting in 50 identified unique items through thematic coding. Factor analysis (Kaiser-Meyer-Olkin measure of sampling adequacy = .679, Bartlett’s test of sphericity (x2(351) = 1129.06. p < .001), resulted in a four-factor solution: ‘5Ds and 3 Ns,’ ‘Other Neurological Findings,’ ‘Signs & Symptoms in Rotation and/or Extension,’ and ‘General Health.’
Discussion: According to the PT educators in this study, the factors associated with CAD appear to reflect the IFOMPT guidelines. The responses and subsequent factor analysis demonstrate the lack of any one clinical finding for the identification of CAD in a patient with neck pain.
Level of Evidence: V.
KEYWORDS: Neck pain, arterial dysfunction, examination
Introduction
Neck pain is a common complaint throughout the world and was the 6th leading cause of disability in the United States (US) as of 2016 [1]. It ranks second to low back pain as the highest cause of musculoskeletal disability in the US with a 54.7% increase in the number of years lived with disability since 1990. Physical therapists (PT) are one of many healthcare providers who routinely manage the care of neck pain complaints. Clinical practice guidelines suggest exercise and cervical manual therapy as interventions to address neck pain with and without headache [2,3]. The frequency of cervical spine manual therapy utilization for neck pain is similar between PTs and chiropractors, however PTs are less likely to employ thrust techniques [4]. Implementation of manual therapy interventions by PTs, including both thrust and non-thrust manipulation, varies based upon the comfort level of the individual practitioner [5].
A recent survey of predominantly orthopedic PTs found 68.9% expressed agreement that cervical thrust manipulation was safe and effective yet < 40% were comfortable performing cervical thrust manipulation and only 33% regularly provide cervical thrust manipulation [5]. The safety and effectiveness along with comfort and use of cervical thrust techniques was reportedly lower than thrust manipulations targeting the thoracic or lumbar regions. Inadequate entry-level or post-graduate training in cervical thrust manipulation, and patient safety concerns were reported as barriers to implementation of cervical thrust manipulation to the cervical spine. The most recent review of US entry-level PT programs found that the instruction of spinal thrust manipulation had increased to 99% [6]. A disparity existed between programs with > 95% including thrust manipulation of the thoracic and lumbar spine with only 65% of programs for the cervical region in their curriculum.
The safety of cervical spine thrust manipulation has been questioned due to possible severe adverse outcomes [7,8]. Clinicians must critically assess the positive therapeutic effects of thrust manipulation against the potential for negative results. The lack of a standard terminology and process for reporting negative patient experiences presents a challenge for PTs who wish to utilize these interventions [9]. Unintended negative outcomes can be divided between adverse events (AE) or side effects (SE) [9,10]. According to Kranenburg et al. [10], AE are ‘medium to long term in duration, with moderate to severe symptoms, and of a nature that was serious, distressing, and unacceptable to the patient and required further treatment,’ while SE are ‘short term, mild in nature, non-serious, transient, and reversible consequences of treatment.’ Concern regarding the implementation of manual therapy has focused on AE which appear to occur rarely, with an incidence of 1 in 50,000 to 1 in 6 million treatments [11]. A variety of AE have been reported with manual therapy intervention in patients with neck pain including dissection or embolism within the internal carotid or vertebral artery, cerebrovascular accident (CVA), disc herniation, spinal cord compression, fracture, and even death [10,12,13]. Arterial dissection is the most common severe AE associated with cervical manipulation accounting for 40–60% of all reported AEs [10,14]. SE are estimated to occur in around 50% of individuals receiving thrust manipulation to the cervical spine often including pain, muscle soreness, stiffness, or headache [12,14]. The resolution of SE complaints is achieved within 24–72 hours after the cervical thrust manipulation and appear to occur at the same frequency in non-thrust manual therapy interventions, exercise, or even sham interventions [12]. Previous literature has suggested that there is an association between arterial dissection and cervical spine thrust manipulation, although there is insufficient evidence to suggest causation [7,10,14].
Recent evidence has demonstrated a decrease in neck pain and disability for patients with neck pain who receive PT services within the first 4 weeks of symptoms, suggesting that early intervention is beneficial [15]. Individuals with neck pain are likely to continue seeking healthcare from PTs who may consider manual therapy interventions. The indications for employing thrust manipulation to the cervical region have been reported to include neck pain, neck stiffness, headache, and dizziness [10]. Unfortunately, occult sinister pathologies may present with similar signs and symptoms. This presents a challenge in identifying individuals likely to have a beneficial response to manual therapies in comparison to those more likely to experience an AE. Church et al. [16] suggested that many AE related to cervical thrust manipulation may have resulted from a patient seeking care for symptoms of an ongoing arterial dissection mimicking a benign musculoskeletal condition. The association between manipulation and AE may in fact be a result of ineffective screening or clinical reasoning [7,14]. Given the potential for overlapping patient signs and symptoms, PTs should critically evaluate our knowledge, beliefs, and decision-making regarding patients with neck pain.
Cervical arterial dysfunction (CAD) is a term that encompasses the broad anatomical and pathological spectrum of events, including dissection and other conditions, affecting arterial structures of the cervical region and potentially the blood supply to the brain [17]. This includes a wide range of dysfunctions that result in vascular changes from arterial dissection, embolism, transient ischemic attack (TIA), and CVA which likely to produce signs and symptoms of ischemia [17,18]. In the early stages, CAD may mimic normal musculoskeletal complaints, presenting a challenge for clinicians not conducting a comprehensive subjective and objective examination focused on non-ischemic signs and symptoms. Non-ischemic symptoms of CAD may be neck pain and headache prior to progressing to ischemic signs and symptoms over a period of days to weeks [17–19]. Additional signs of CAD that may present prior to brain ischemia with ptosis, miosis, and lower cranial nerve (XIII-VII) dysfunctions [19]. The clinical manifestation of CAD further along the natural history more clearly signify ischemic findings as non-normal musculoskeletal complaints. Ischemic changes associated with late stage CAD may present consistent with CVA or TIA. The classic cardinal signs of cervical ischemia, colloquially referred to as the ‘5Ds and 3 Ns,’ also present in the late stage of CAD: diplopia, dizziness, drop attacks, dysarthria, dysphagia, ataxia, nausea, numbness, and nystagmus [19,20].
The International Federation of Orthopedic Manipulative Physical Therapists (IFOMPT) created best practice guidelines aimed at assisting PTs in identifying patients at risk for CAD and associated AE [19]. The IFOMPT guidelines acknowledge the difficulty in identifying CAD while providing general recommendations to perform an individualized patient history aimed at identifying likelihood of CAD, prioritize physical examination procedures understanding that diagnostic utility is limited for ruling in or out CAD, and utilize a simple risk to benefit model to guide patient care [18]. These recommendations have been supported by the Orthopedic Section of the American Physical Therapy Association, in their neck pain guidelines [2]. In the absence of valid screening protocols, these guidelines recommend a high index of suspicion for patients with headache and neck pain and entertain the possibility of a vascular cause of neck pain using a focused subjective interview prior to relying upon objective measures of questionable utility [11,19].
Clinical practice guidelines, like those developed by IFOMPT, are intended to compile recent advances in evidence with historical practices in a manner to facilitate current best practice. Unfortunately, guidelines are not routinely applied throughout the clinical world. The implementation of guidelines can be limited by clinician knowledge, attitude, or behavioral barriers [21]. Effective dissemination requires the participation of various stakeholders to actively target the knowledge and attitude of clinicians prior to realization of behavioral change embodied by guideline use in practice. Guideline-informed educational programs have been strongly associated with evidence-based decision making by PTs [22]. A strong majority of PTs reported original educational training, post-licensure coursework, and previous experience as most influential in guiding decision making. Given the potential impact of formalized training programs, examining the beliefs of PT educators may provide insight into the penetration of guidelines in the profession.
There is an apparent discrepancy in the clinical utilization of cervical spine thrust manipulation when compared to other spinal regions for PTs in the US. PTs expressing less comfort with these techniques have reported safety considerations and a lack of training as impediments. Further training, at entry-level or post-graduate programs, related to the safety and skill associated with cervical manual therapy would be a reasonable remedy. Unfortunately, we are currently unaware of PT educators’ beliefs related to the examination of patients with neck pain. The purpose of this study was to identify the underlying constructs related to CAD according to a panel of PT educators and compare these constructs to the IFOMPT guidelines.
Methods
This study was approved by the Institutional Review Board at the University of Illinois at Chicago. The participants targeted for this investigation included PTs involved in providing musculoskeletal content within physical therapy educational programs in the US.
Survey design and recruitment
A list of potential respondents was created by contacting the director of each physical therapy entry-level and post-professional Doctor of Physical Therapy (DPT) degree program along with each credentialed orthopedic and sports physical therapy residency and fellowship program credentialed by the American Board of Physical Therapy Residency and Fellowship Education as of 1 July 2016. The director of each program was asked to identify all individuals meeting the following inclusion criteria: (1) PT and (2) currently involved in musculoskeletal physical therapy education within the credentialed program. PT educators identified by the director of the educational program were then invited to participate in the study via e-mail containing a link to the informed consent document and the electronic survey.
Survey administration
Data collection was conducted using Qualtrics Electronic Survey Software (Provo, Utah, USA). The survey instrument included two open-ended questions about CAD. Participants were asked to report all potential items or factors within the patient subjective report or history that may be related to CAD. Items within this category were considered but not limited to symptom description and behavior, natural history of complaints, and previous medical history. The second prompt targeted all potential factors or items within an objective physical examination that may be related to CAD. Items within this category were considered but not limited to activities, motions, signs and special tests.
Upon completion of the survey instrument, two researchers pooled all responses, subjective and objective, and independently reviewed the responses to identify qualitative themes. The researchers then met to compare identified themes and reach agreement on the themes. If agreement between the two researchers was not achieved a third researcher was intended as a tie break. The third researcher was not required in this study as agreement was achieved after short discussion focusing primarily on the specific naming of each identified theme. Once the researchers agreed upon the themes represented, the responses were analyzed for the frequency of each item in the educators’ responses.
Data analysis
Frequency analysis was performed for each item followed by exploratory principal axis factor analysis. While novel to many clinicians, factor analysis is frequently employed in situations where a multitude of seemingly independent variables may represent an underlying concept or ‘factor’ which may be more easily understood [23]. In this study the accumulation of subjective and objective findings was large leading to difficulty in interpretation. Factor analysis was utilized to cluster items based upon shared variance and identify latent factors within the responses provided by the PT educators. Statistical significance (p < .05) on Bartlett’s Test of Sphericity was used to determine if patterned relationships existed, potentially representing underlying constructs [23]. A threshold of Kaiser-Meyer-Olkin Measure of Sampling Adequacy (KMO) of .5 was used to establish suitability for factor analysis. Items with < .500 measures of sampling adequacy in anti-image correlation were excluded from subsequent factor analysis to achieve further data reduction. The number of factors was determined using initial eigenvalues >1.0 and visually via the scree plot of initial eigenvalues. A statistical process called rotation is used during factor analysis to ensure that the identified latent factors represent distinct concepts [23,24]. While numerous rotation methods exist, Varimax rotation was selected to produce the simplest factor structure where individual factors are uncorrelated therefor representing distinct concepts [24]. After Varimax rotation, any item with <.3 factor loading was suppressed due to the low correlation with that given factor [23,25]. After the completion of statistical analysis, the resultant factors were analyzed for qualitative themes that would best describe or explain the cluster of individual items represented. Each factor was then labeled with language familiar to PT practice.
Results
A total of 451 educational program directors were contacted (217 entry-level, 41 post-professional, 107 orthopedic residency, 46 sports residency, and 40 fellowship programs) with 92 responses received (20.4% response rate) yielding 297 individual PT educators as potential respondents. The 297 potential respondents identified by the respective program directors were then contacted via e-mail with an invitation to participate in this study. Ninety-two PT educators agreed to participate (31.0% response rate), however 72 educators completed the survey (24.2% response rate).
Most respondents had ≥ 11 years since initial licensure as a PT (78.6%), ≤ 10 years as a PT educator (57.2%), and were Board Certified Specialists (84.3%) through the American Board of Physical Therapy Specialties. Initial PT degree was evenly distributed amongst baccalaureate (32.9%), entry-level master’s (31.4%), and entry-level doctorate (DPT) (35.7%). Post professional training was prevalent with transitional DPT (24.3%) or other doctoral degree (35.7%), and 38.6% of respondents achieving fellowship status in the American Academy of Orthopedic Manual PTs. The program affiliation of the respondents was 74.3% DPT, 24.3% transitional DPT, 55.7% residency, and 15.7% fellowship with many educators participating in multiple programs.
The work group identified fifty individual items proposed by the educator panel. The items represented a wide response frequency; only six items were reflected in >70% and eight items in >50% of total responses, Figure 1. Initial principal axis factor analysis identified 27 items demonstrating >.500 measure of sampling adequacy in anti-image correlation. The 27 items produced a Kaiser-Meyer-Olkin measure of sampling adequacy of .679, with a significant Bartlett’s test of sphericity (x2(351) = 1129.06. p < .001). Initial analyses yielded 9 factors with > 1.0 initial eigenvalue, although the slope of the scree plot leveled-off after four factors, Figure 2. A four-factor solution was selected and confirmed through analysis of the items grouped in each factor being easily categorized as similar or related in clinical practice. The four-factor solution explained 50.7% of total variance (20.6; 12.6; 9.9; and 7.5% respectively).
Figure 1.
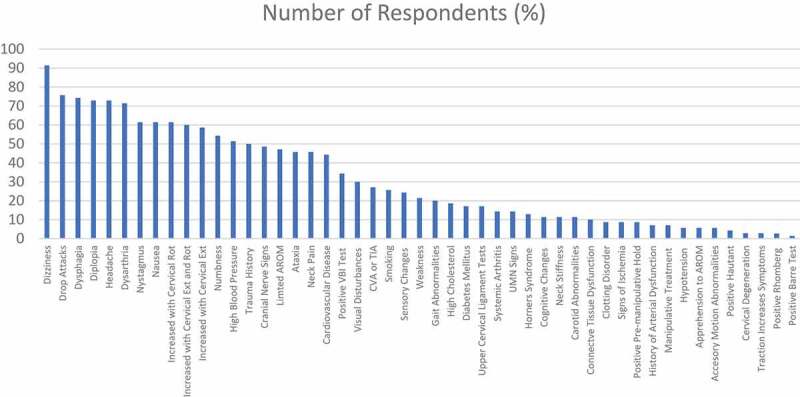
The qualitative themes identified through the survey and subsequent work group are displayed with the corresponding frequency of responses from the educator panel
Figure 2.
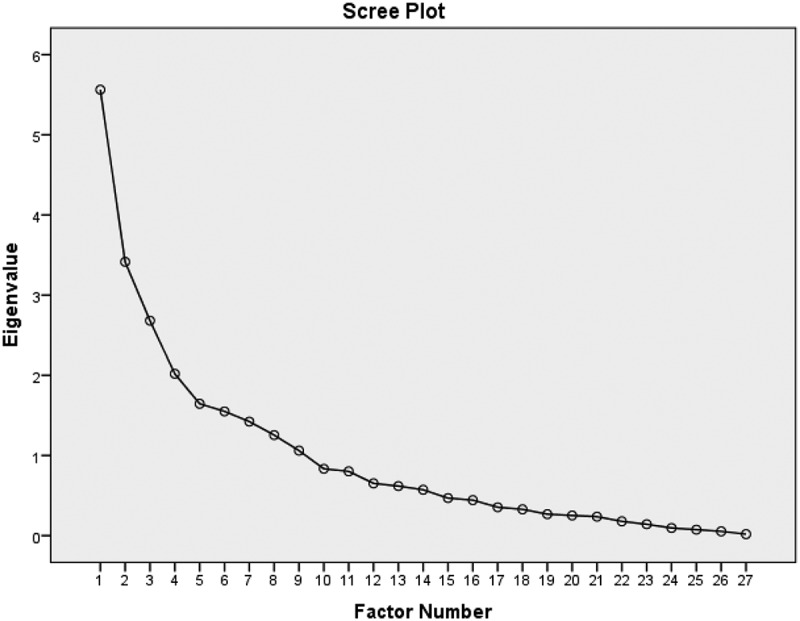
Scree plot of initial Eigen values and number of factors
After Varimax rotation, five items were eliminated from the factor analysis for failing to achieve a primary factor loading of .3 or above suggesting that these items were not directly correlated with the corresponding factor [23]. The five items eliminated were: headache, carotid abnormalities, positive VBI test, positive UCI tests, and limited AROM. The four-factors were labeled with language common in PT practice: Factor 1, ‘5Ds and 3 Ns,’ Factor 2, ‘Other Neurological Findings,’ Factor 3, ‘Signs & Symptoms in Rotation and/or Extension,’ and Factor 4, ‘General Health’ factor loadings for each item are shown in Table 1. This analysis suggests that four underlying constructs are represented in the items reported by the panel of educators.
Table 1.
Latent factors associated with cervical arterial dysfunction
| Factors | Factor Loading |
|---|---|
| Factor 1: ‘5Ds and 3Ns’ Dysphagia Drop Attacks Dysarthria Diplopia Numbness Nausea Nystagmus Dizziness |
.928 .831 .830 .775 .549 .529 .497 .382 |
| Factor 2: ‘Other Neurological Findings’ Deep Tendon Reflex Changes Upper Motor Neuron Signs Weakness Sensory Changes Gait Abnormalities Ataxia Cranial Nerve Signs Signs of Horner’s Syndrome |
.800 .734 .673 .547 .517 .514 .499 .476 |
| Factor 3: ‘Symptoms Increased with Extension and/or Rotation’ Increased with Extension Increased with Rotation Increased with Extension and Rotation |
.956 .956 .924 |
| Factor 4: ‘General Health’ Smoking History Diabetes Mellitus Systemic Arthritis |
.593 .512 .354 |
| Factor loadings <.30 suppressed | |
Discussion
The purpose of this study was to identify the underlying constructs related to CAD according to a panel of PT educators. Fourteen items were identified by ≥ 50% of the PT educators as having an association with CAD. Most of these (dizziness, drop attacks, dysphagia, diplopia, headache, dysarthria, nausea, increased symptoms with cervical extension/rotation or both, numbness, and trauma history) can be assessed at least in part through patient history and subjective examination; the remaining items can be assessed through mild objective measures (nystagmus, and high blood pressure). The items with high response frequency and the four-factor solution presented in this study appear to reflect the general focus of the IFOMPT guidelines with respect to the broad collection of patient subjective information and lack of reliance upon and single test or measure.
Cervical manual treatment will continue to be included in the management of neck-related musculoskeletal pain even though the actual risk of AE resulting from manual therapy techniques, while likely extremely low, is unknown and likely under reported [12,26]. Clinicians must use the best available evidence to identify patients at risk for AE prior to manual therapy intervention in the management of neck pain. The results of this study suggest, through factor analysis, that the participating PT educators agree with the most current best available evidence in the IFOMPT guidelines.
Historically PTs have utilized positional testing of the cervical spine in extension, rotation or a combination of both to identify patients with potential vertebrobasilar artery insufficiency (VBI) indicating a patient is inappropriate for manual therapy and requires appropriate referral for additional medical evaluation [27,28]. VBI positional testing was reported by < 40% of respondents in the current study, failing to reach the threshold for inclusion in the four-factor solution. However, the results of this study did find the third factor, representing approximately 60% of respondents, reported increased symptoms with extension, rotation, and combined extension with rotation as an important clinical finding in patients with CAD. The discrepancy between respondents specifically reporting ‘positive VBI’ test or merely describing the pattern of provocative movement may reflect the current uncertainty in the utility of these procedures. Multiple authors have questioned the clinical utility of the VBI testing due to unconvincing evidence that the procedure can identify altered blood flow in the presence of apparent or latent arterial symptomology [18,27,29,30]. It is unlikely that this test can reliably identify patients with CAD or VBI and may provide a false negative finding and sense of security if negative in patients with nonischemic CAD, leading to inappropriate manual therapy intervention. It is possible that positional testing may have a role in the identification of patients presenting with CAD [28], although consistent with the IFOMPT guidelines, the clinical usefulness seems unknown.
Examination and intervention of the cervical region continues to be difficult requiring PTs to maintain reflective practice regarding their individual knowledge, experience, and skill. Each clinician should ensure that their individual practice is consistent with the IFOMPT guidelines and address any noted deficiencies. Participation in formal educational programs employing didactic, hands-on, and clinical mentorship may be beneficial to improve confidence and competence in the management of patients with neck pain. PTs should consider programs where curriculum content is supported by evidence-based guidelines. These courses may include manual therapy certification, post-graduate residency or fellowship, or self-study. The findings of this study suggest that the PT educators in accredited programs in the US beliefs are consistent with the IFOMPT guidelines.
This study is limited by the relatively small sample of PT educators, predominantly associated with DPT programs, making inferences about the population of PT educators uncertain. Respondents were identified as instructors within the musculoskeletal curriculum of an accredited program but were not queried as to their participation in teaching cervical examination or intervention, nor were they asked to report their knowledge of the IFOMPT guidelines. Additionally, the open-ended format of the survey instrument required coding of participant responses which may have resulted in inappropriate coding, which is a common limitation in qualitative research. As new evidence emerges further study of the impact it has on clinicians and educators is warranted.
Conclusion
According to the PT educators in this study, the factors associated with CAD appear to reflect the IFOMPT guidelines. The responses and subsequent factor analysis demonstrate the lack of any one clinical finding for the identification of CAD in a patient with neck pain. It is essential that the PT profession continue to discuss the limitation of clinicals skills in the context of patient risk. Increasing the uniformity and standardization of clinical practice among PT educators for the use of thrust manipulation and the application of consistency in the utilization of the IFOMPT guidelines within educational programs is vital to reduce patient risk of AE.
Biographies
Bradley J. Myers is a physical therapist and educator within the Campbell University Doctor of Physical Therapy Program. His clinical and research interests include the appropriate application of manual therapy techniques with exercise interventions within orthopedic dysfunctions, and the identification of motor control dysfunctions as a precursor/result of musculoskeletal impairments.
Deborah Davey Davey is a physical therapist and educator within the University of Illinois at Chicago Doctor of Physical Therapy and Orthopedic Physical Therapy Residency Programs. Her clinical and research interests include musculoskeletal conditions, chronic pain management, and health disparities.
Chad E. Cook is a clinical researcher, physical therapist and academic program director of Doctor of Physical Therapy Program at Duke University. His passions include refining and improving the patient examination process and validating tools used in day-to-day physical therapist practice.
Funding Statement
No funding source was included in this project.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Mokdad AH, Ballestros K, Echko M, et al.; US Burden of Disease Collaborators . The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 2018;319(14):1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1–A83. [DOI] [PubMed] [Google Scholar]
- [3].Cohen SP, Hooten WM.. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221. [DOI] [PubMed] [Google Scholar]
- [4].Carlesso LC, Macdermid JC, Gross AR, et al. Treatment preferences amongst physical therapists and chiropractors for the management of neck pain: results of an international survey. Chiropr Man Therap. 2014;22(1):11-709X-22-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Puentedura EJ, Slaughter R, Reilly S, et al. Thrust joint manipulation utilization by U.S. physical therapists. J Man Manip Ther. 2017;25(2):74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Noteboom JT, Little C, Boissonnault W. Thrust joint manipulation curricula in first-professional physical therapy education: 2012 update. J Orthop Sports Phys Ther. 2015;45(6):471–476. [DOI] [PubMed] [Google Scholar]
- [7].Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(10):3155–3174. [DOI] [PubMed] [Google Scholar]
- [8].Miley ML, Wellik KE, Wingerchuk DM, et al. Does cervical manipulative therapy cause vertebral artery dissection and stroke? Neurologist. 2008;14(1):66–73. [DOI] [PubMed] [Google Scholar]
- [9].Carlesso LC, MacDermid JC, Santaguida LP. Standardization of adverse event terminology and reporting in orthopaedic physical therapy: application to the cervical spine. J Orthop Sports Phys Ther. 2010;40(8):455–463. [DOI] [PubMed] [Google Scholar]
- [10].Kranenburg HA, Schmitt MA, Puentedura EJ, et al. Adverse events associated with the use of cervical spine manipulation or mobilization and patient characteristics: a systematic review. Musculoskelet Sci Pract. 2017;28:32–38. [DOI] [PubMed] [Google Scholar]
- [11].Hutting N, Kerry R, Coppieters MW, et al. Considerations to improve the safety of cervical spine manual therapy. Musculoskelet Sci Pract. 2018;33:41–45. [DOI] [PubMed] [Google Scholar]
- [12].Carnes D, Mars TS, Mullinger B, et al. Adverse events and manual therapy: a systematic review. Man Ther. 2010;15(4):355–363. [DOI] [PubMed] [Google Scholar]
- [13].Haynes MJ, Vincent K, Fischhoff C, et al. Assessing the risk of stroke from neck manipulation: a systematic review. Int J Clin Pract. 2012;66(10):940–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Puentedura EJ, March J, Anders J, et al. Safety of cervical spine manipulation: are adverse events preventable and are manipulations being performed appropriately? A review of 134 case reports. J Man Manip Ther. 2012;20(2):66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Horn ME, Brennan GP, George SZ, et al. A value proposition for early physical therapist management of neck pain: A retrospective cohort analysis. BMC Health Serv Res. 2016;16:253-016-1504-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Church EW, Sieg EP, Zalatimo O, et al. Systematic review and meta-analysis of chiropractic care and cervical artery dissection: no evidence for causation. Cureus. 2016;8(2):e498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kerry R, Taylor AJ. Cervical arterial dysfunction: knowledge and reasoning for manual physical therapists. J Orthop Sports Phys Ther. 2009;39(5):378–387. [DOI] [PubMed] [Google Scholar]
- [18].Kerry R, Taylor AJ, Mitchell J, et al. Cervical arterial dysfunction and manual therapy: a critical literature review to inform professional practice. Man Ther. 2008;13(4):278–288. [DOI] [PubMed] [Google Scholar]
- [19].Rushton A, Rivett D, Carlesso L, et al. International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention. Man Ther. 2014;19(3):222–228. [DOI] [PubMed] [Google Scholar]
- [20].Kerry R, Taylor AJ, Mitchell J, et al. Manual therapy and cervical arterial dysfunction, directions for the future: a clinical perspective. J Man Manip Ther. 2008;16(1):39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Fischer F, Lange K, Klose K, et al. Barriers and strategies in guideline implementation: a scoping review. Healthcare. 2016;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Turner P, Whitfield TWA. Physiotherapists’ use of evidence based practice: A cross-national study. Physiother Res Int. 1997;2(1):17–29. [DOI] [PubMed] [Google Scholar]
- [23].Yong AG, Pearce S. A beginner’s guide to factor analysis: focusing on exploratory factor analysis. Tutorials Quant Methods Psychol. 2013;9(2):79–94. [Google Scholar]
- [24].Schmitt TA, Sass DA. Rotation criteria and hypothesis testing for exploratory factor analysis: implications for factor pattern loadings and interfactor correlations. Educ Psychol Meas. 2011;71(1):95–113. [Google Scholar]
- [25].Salkind NJ. Encyclopedia of research design. Thousand Oaks, Calif: SAGE Publications, Inc; 2010. [Google Scholar]
- [26].Carlesso LC, Gross AR, Santaguida PL, et al. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: A systematic review. Man Ther. 2010;15(5):434–444. [DOI] [PubMed] [Google Scholar]
- [27].Richter RR, Reinking MF. Evidence in practice. how does evidence on the diagnostic accuracy of the vertebral artery test influence teaching of the test in a professional physical therapist education program? Phys Ther. 2005;85(6):589–599. [PubMed] [Google Scholar]
- [28].Thomas L, Treleaven J. Should we abandon positional testing for vertebrobasilar insufficiency?. Musculoskeletal Sci Pract. 2019;102095. https://www.sciencedirect.com/science/article/pii/S2468781219301274 [DOI] [PubMed] [Google Scholar]
- [29].Thiel H, Rix G. Is it time to stop functional pre-manipulation testing of the cervical spine? Man Ther. 2005;10(2):154–158. [DOI] [PubMed] [Google Scholar]
- [30].Hutting N, Verhagen AP, Vijverman V, et al. Diagnostic accuracy of premanipulative vertebrobasilar insufficiency tests: A systematic review. Manual Ther. 2013;18(3):177–182. [DOI] [PubMed] [Google Scholar]


