Dear Editor,
airway management is crucial in effective treatment of COVID-19 patients with critical/severe disease. In the literature, the risk of nosocomial SARS-CoV-2 transmission ascribable to increased request for tracheostomy continues to be debated 1,2; in addition, we have to take into account that, once the acute phase passes, we may have to face other problems, such as laryngo-tracheal sequelae following prolonged endotracheal intubation and tracheostomy 3. Now that infectious spreading and contagion has been steadily decreasing in Italy, we observed an escalation in requests for ENT consultation for laryngeal complaints in COVID-19 patients who underwent endotracheal intubation or tracheostomy, independently of age, and were able to overcome the critical stage of disease at our frontline hospital in Milan, located in epicentre of the Italian COVID-19 epidemic.
Several factors could be responsible for a remarkable prevalence of laryngeal dysfunction in post-acute COVID-19 patients:
more time needed for respiratory weaning resulting in prolonged endotracheal intubation/tracheostomy maintenance to continuous positive airway pressure ventilation;
the use of high-pressure ventilation to treat acute respiratory distress syndrome;
Adoption of surgical and anaesthesiologic protocols aimed at reducing dispersal of infected aerosols during/after endotracheal intubation and tracheostomy performance 1,2, such as: the use of non-fenestrated and cuffed tubes with adequate cuff inflation, reduction/avoidance of tracheostomy change 1,2;
poor pulmonary performance and hypoxaemia with increased respiratory rate, negatively affecting the respiration/swallowing balance;
a possible reduced cortical/subcortical laryngeal coordination due to peripheral and/or central SARS-CoV-2 neuroinvasive propensity through a synapse-connected route 4,5, suspected on the grounds of documented neurological complaints and smell impairment 4.
On one hand, this scenario results in perpetuation of mucosal trauma and mechanical lesions/scaring leading to reduced laryngo-tracheal patency. On the other hand, laryngeal/hypopharyngeal sensation as well as airway protection are reduced; muscle weakness and atrophy related to disuse and critical illness myopathy and neuropathy with impairment in coordination of respiration/swallowing pattern may occur and predispose to swallowing disorders 6.
In the post-COVID era, we must be prepared to deal with an increased prevalence of patients with laryngo-tracheal sequelae, and to adequately manage them, also considering that the therapeutic approach can be troublesome and outcomes are not always predictable. In addition, traditional diagnostic and rehabilitative pathways have been reconsidered and applied only to urgent cases 7-9, and optimising non-instrumental swallowing assessment tools as an alternative to fiberoptic endoscopic evaluation is difficult to carry out in a short-time period. All of this may cause further difficulties in management.
A proposed follow-up schedule to be considered by ENT specialists for post-critical assessment of COVID-19 patients with documented or suspected laryngeal sequelae after intensive care management is presented in Figure 1.
Figures and tables
Figure 1.
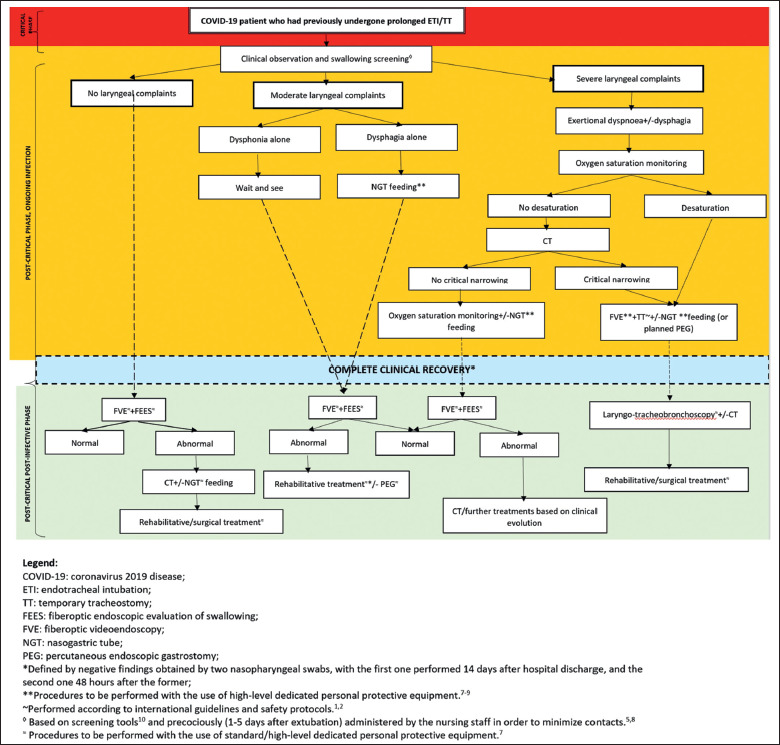
Proposal of a follow-up schedule for post-critical assessment of COVID-19 patients with documented or suspected laryngeal sequelae after intensive care management.
References
- 1.Sommer DD, Engels PT, Weitzel EK, et al. Recommendations from the CSO-HNS taskforce on performance of tracheotomy during the COVID-19 pandemic. J Otolaryngol Head Neck Surg 2020;49:23 https://doi.org/10.1186/s40463-020-00414-9 10.1186/s40463-020-00414-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.David AP, Russell MD, El-Sayed IH, et al. Tracheostomy guidelines developed at a large academic medical center during the COVID-19 pandemic. Head Neck 2020;42:1291-6. https://doi.org/10.1002/hed.26191 10.1002/hed.26191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldsmith T. Evaluation and treatment of swallowing disorders following endotracheal intubation and tracheostomy. Int Anesthesiol Clin 2000;38:219-2. https://doi.10.1097/00004311-200007000-00013 10.1097/00004311-200007000-00013 [DOI] [PubMed] [Google Scholar]
- 4.Yashavantha Rao HC, Jayabaskaran C. The emergence of a novel coronavirus (SARS-CoV-2) disease and their neuroinvasive propensity may affect in COVID-19 patients. J Med Virol 2020;92:786-90. https://doi.org/10.1002/jmv.25918 10.1002/jmv.25918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dziewas R, Warnecke T, Zürcher P, et al. Dysphagia in COVID-19 - multilevel damage to the swallowing network? Eur J Neurol 2020;27:e46-7. https://doi.org/10.1111/ene.14367 10.1111/ene.14367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med 2020;56:323-6. https://doi.org/10.23736/S1973-9087.20.06305-4 10.23736/S1973-9087.20.06305-4 [DOI] [PubMed] [Google Scholar]
- 7.Ku PKM, Holsinger FC, Chan JYK, et al. Management of dysphagia in the patient with head and neck cancer during COVID-19 pandemic: practical strategy. Head Neck 2020;42:1491-6. https://doi.org/10.1002/hed.26224 10.1002/hed.26224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frajkova Z, Tedla M, Tedlova E, et al. Postintubation dysphagia during COVID-19 outbreak-contemporary review. Dysphagia 2020;28:1-9. https://doi.org/10.1007/s00455-020-10139-6 10.1007/s00455-020-10139-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mattei A, Amy de la Bretèque B, Crestani S, et al. Guidelines of clinical practice for the management of swallowing disorders and recent dysphonia in the context of the COVID-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis 2020;137:173-5. https://doi.org/10.1016/j.anorl.2020.04.011 10.1016/j.anorl.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zuercher P, Moret CS, Dziewas R, et al. Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Crit Care 2019;23:103 https://doi.org/10.1186/s13054-019-2400-2 10.1186/s13054-019-2400-2 [DOI] [PMC free article] [PubMed] [Google Scholar]


