ABSTRACT
Objective: To investigate the effect of the examination process (history taking and physical examination) on pain and function.
Methods: An observational cohort trial of patients presenting to outpatient physical therapy clinics for the first time with low back pain (n = 34, 57.7 ± 18.7 years, 53% female). A blinded investigator measured participants prior to the beginning of the initial evaluation and after each component of evaluation (history taking and physical examination). Another physical therapist provided normal history taking and physical examination as the patient case presented itself. Primary outcome measure was numeric pain rating scale (NPRS) for the low back and leg. Secondary outcomes and time during examination process and connection between PT and patient were also measured as potential confounders.
Results: Participants showed a significant reduction in pain through just the history taking and physical exam for both the back with an NPRS reduction of 1.23 and the leg showing a 0.95 NPRS reduction. The most significant reduction occurs after history taking.
Discussion: The evaluation process produced small, but significant, therapeutic effects related to pain, fear-avoidance, pain catastrophization, and functional measures of mobility and sensitivity. The therapist's report of connection with the patient did not alter the patient outcome.
KEYWORDS: Physical examination, medical history taking, physical therapy, musculoskeletal pain
Introduction
It is well documented that low back pain (LBP) is still the most widely reported musculoskeletal disorder in the world and accounts for significant health-care expenditures [1,2]. In the United States (US), LBP accounts for 25% of outpatient physical therapy (PT) visits and it is estimated over 170,000 people on a daily basis in the US consult a PT for LBP [3–6].
When patients with LBP attend a visit with a health-care provider, they often encounter clinical rituals [7,8]. In general, most initial medical visits contain the clinical ritual of history taking, physical examination, and treatment. This clinical ritual aligns well with current patient expectation studies for LBP that emphasize the importance of doing a thorough history, followed by a physical examination, and then treatment for their primary complaint to reduce pain and disability [9,10]. Patients and health-care providers typically attribute reduction in primary complaint to the treatment provided. In medicine, the treatment delivered is often a medication, which does not provide immediate change in patient status during the initial visit [11]. In physical therapy (PT), however, therapists also perform the clinical ritual of history taking, physical examination, and treatment, but often re-tests are completed following treatment at the conclusion of the initial visit to assess the effectiveness of the treatment. If the patient is better, it is believed the treatment alone was the effective cause of this improvement [12,13]. In this model, outcomes are associated with the chosen treatment [13–15], and little to no thought is given to the influence of the history taking and/or physical examination as a means to influence the outcome [16].
In recent years, with the shift toward the biopsychosocial model, more attention is looking into the therapeutic alliance (TA) and effects it has on outcomes [17,18]. But, research into TA as having an effect on outcomes is still minimal compared to other specific treatments such as exercise, manual therapy, and modalities. TA is defined as the working rapport or positive social connection between the patient and the clinician[19]. TA is a complex blend of clinician technical skill, verbal and non-verbal communication, sense of warmth, collaboration, and trust[19]. Increasing evidence supports the notion that TA, especially trust, is shown to powerfully influence pain and outcomes [8,17,20,21]. During the history taking, strategies such as active listening, being present and in the moment, acknowledging the individual experience of the patient, eye contact, empathy, etc., all have been shown to build trust and foster the TA [22,23]. Even though it can be argued similar virtues of the history taking are displayed during the physical examination, i.e. being present, eye contact, empathy, etc., would influence TA, the actual physicality of touch during the examination may further build trust and foster a TA via the neuropeptide oxytocin and its involvement with pain relief [21,24–27]. In addition, some of the physical tests and measures performed during the physical exam (i.e. repeated movement, joint and soft tissue mobility) may actually serve the function of treatment, before the more formal treatment intervention is applied.
In this study, we explore the idea of history taking and a physical examination potentially influencing the patient’s status. Currently, no study has looked specifically to see if history taking and physical exam alone can alter a patient’s pain and function in the short term. If this is found to be true, then future study should explore elements of the history taking and physical exam to maximize outcomes. The purpose of the study is to investigate if the PT evaluation ritual actually results in a meaningful shift in pain and function for patients with LBP, even before implementing the actual treatment interventions. This study aims to test if there are any therapeutic effects of the history taking and physical examination of patients with LBP attending PT. Secondary aim is to investigate the amount and effect size of change for various outcome measures of pain and function after history taking and physical examination.
Methods
Participants
A sample of convenience of 40 consecutive patients with LBP with/without leg pain attending four different outpatient PT clinics over a 3-month time period were invited to participate in this observational cohort study. One PT at each site did the history taking and physical exam, while another PT did the outcome measurements. The clinicians involved with the history taking and physical exam had an average of 6 years of clinical practice (range 4–8 years). Three of the four clinicians were board certified in orthopedics, and the other had achieved post-professional certifications in manual therapy and pain science. Data sample size was determined by the number of eligible participants collected during the 3-month time period of study. Institutional Review Board approval was obtained. Inclusion criteria were that patients had to: (1) be presenting for treatment of LBP; (2) age greater than 18 years; (3) ability to read and understand English; and (4) be willing to participate in the study. Exclusion criteria included: (1) inability to forward flex the lumbar spine due to some medical complication or contraindication; (2) skin lesions in areas to be tested with pressure pain threshold; or (3) red flag medical condition that indicated PT was not appropriate. As noted in Figure 1, six participants were excluded from the study, thus resulting in a sample total of 34 participants for this study.
Figure 1.
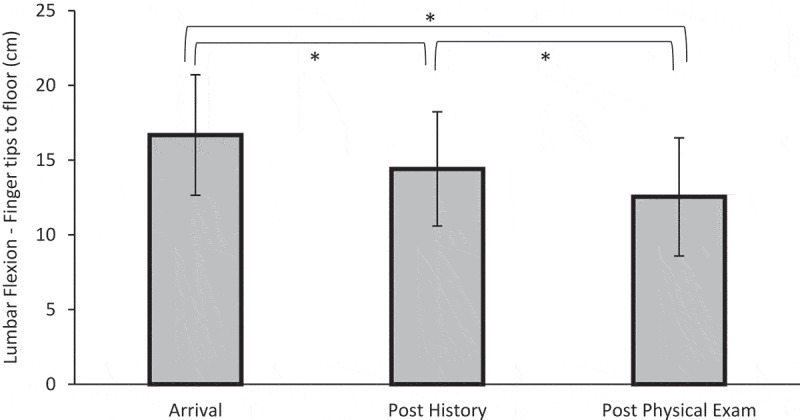
Means of lumbar flexion between each time point with 95% confidence interval bars. *p < 0.05 between arrival and post history, post history and post physical exam, and arrival and post physical exam
Measurements
Upon arrival and prior to history taking and examination, all participating patients completed a demographic survey which included age, gender, ethnicity, socioeconomic status, duration of LBP pain, past LBP, and lumbar surgical history. Prior to the start, participants also completed the Oswestry Disability Index [28–30] to assess their level of disability in order to describe the patient cohort for the study.
Following the demographics, a series of outcome measures were completed before the history as well as immediately after history taking and physical examination:
Pain (low back and leg) (numeric pain rating scale – NPRS)
Low back and leg pain were measured with the use of an NPRS, as has been used in various studies on LBP [31–34]. The minimal clinical important difference (MCID) for the NPRS for acute/subacute LBP is reported to be 2.0 [35] and for chronic pain 1.7 [36].
Fear-avoidance beliefs (fear-avoidance beliefs questionnaire – FABQ)
The FABQ is a 16-item questionnaire with two subscales: (1) physical activity (PA) and (2) work (W). Each item is scored from 0 to 6 with higher scores representing an increase in fear-avoidance beliefs. The FABQ has demonstrated acceptable levels of reliability and validity in previous LBP studies [37–39]. The MCID for the FABQ has been reported as 13.0 [40].
Pain catastrophization (pain catastrophization scale – PCS)
The PCS is a self-report questionnaire that assesses inappropriate coping strategies and catastrophic thinking about pain and injury and demonstrated strong construct validity, reliability and stability [41]. The PCS utilizes a 13-item, 5-point Likert scale with higher scores indicating elevated levels of catastrophizing. Previous studies utilizing the PCS have shown a median score of 18 in healthy individuals and a score over 30 reported as a high level of pain catastrophization [41]. In patients with musculoskeletal pain, the minimal detectable change (MDC) for the PCS is reported to be 9.1 [42], and the MCID has not been established.
Lumbar flexion
Active trunk forward flexion, measured from the longest finger on the dominant hand to the floor in centimeters (cm). The participant is instructed to bend forward at the waist, with knees kept straight, as far as they feel comfortable reaching the fingers toward the floor. The MDC for active trunk forward flexion has been reported as 4.5 cm [43]. Intra- and interrater reliability with fingertip to floor measurement was excellent with ICC of .99 [44].
Nerve sensitivity (pressure pain thresholds – PPT)
To assess the sensitivity of the nervous system, pressure algometry was used. PPT followed standardized protocols [45] and was measured in pounds (lbs/in2) using a digital pressure-pain algometer over the three points on their dominate side: (1) the first and second interosseous web space of the hand; (2) upper trapezius; and (3) adjacent to L3 spinous process. Three consecutive PPT measurements were taken at each point with 20 seconds rest in between each measurement and the mean of the three trials was used for analysis. Various studies have reported a 15% reduction in PPT as a significant clinical change [46–48]. PPT has demonstrated excellent intrarater reliability in both health individuals and those with pain[49].
Intervention
Upon consent and completion of the pre-examination paperwork, patients were escorted to a private treatment room for the physical measurements of active trunk flexion and PPT by non-attending PT. To ensure blinding of attending therapist to the outcome measures, the measurements were conducted by a non-attending PT who was not involved in the patient history taking or examination. After completion of arrival outcomes measures, the attending PT entered the room and performed a pragmatic history taking process guided by the patient’s clinical presentation and clinical reasoning process of attending PT. History taking included gathering information about chief complaint, mechanisms, medical history, functional limitations, prior level of function, social and environmental factors. The attending PT recorded the duration of the history taking episode. Additionally, using a Likert scale, upon completion of the history taking, the attending PT was asked to indicate how well he/she believe they ‘connected’ with the patient (0 = not connected; 10 = very connected). Upon completion of the history taking the non-attending PT collected post history taking outcome measurements (Figure 1). Next, the attending PT conducted a physical examination per his/her discretion. The physical examination was devoid of any treatment interventions during examination process. The physical examination included necessary systems review, functional movement and range of motion assessment, neurologic screening, palpation, joint and soft tissue mobility, and special tests as needed based on the patient presentation to come up with a working hypothesis needed to progress with treatment. Duration of the physical examination was also recorded. Upon completion of the physical examination, all pre-history measurements were once again repeated by the non-attending PT. This concluded the study and the remainder of the session and subsequent plan of care was per attending PT discretion.
Data analysis
Data analysis was performed using IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistics were calculated for means and frequencies for the sample population. A significance level of .05 was set for all analyzes. Changes in non-parametric outcome measures (NPRS-low back, NPRS-leg, FABQ-PA, FABQ-W, PCS) between the three time points were analyzed by using Friedman’s ANOVA with all pairwise for multiple comparisons. Individual mean changes and adjusted significant scores by Bonferroni Correction for multiple tests were calculated for the different time frame comparisons. Generated Z-score was used to determine the effect size (r = Z/√N1+ N2). Interpretation of effect size reported as small 0.1, medium 0.3, and large 0.5 [50].
Repeated measures ANOVA was used to analyze for time point changes for trunk flexion and PPT at the three different measurement points. Mauchly’s test was used to look for sphericity and the Geenhouse–Geisser correction was used to correct for violation of sphericity.
Differences between participant outcomes for each of the clinicians were evaluated through one-way ANOVA for initial status (age, duration of symptoms, ethnicity, gender, ODI, and baseline outcome measurements) and changes after history taking and physical exam for the outcome variables of interest. For any significant findings, a post hoc Bonferroni correction for multiple tests was calculated to determine significance.
Pearson correlations were calculated to determine if there were associations between the differences of outcome measures at baseline and values following either the history or physical examination based on the duration of the patient’s pain, duration of the history, duration of the physical examination, and the perceived connection with the physical therapist providing the care.
Results
Sample description
A total of 34 patients consented to participate and complete all data collection in this single cohort study. Six participants were excluded during the consent process due to age (n = 3), lack of consent (n = 2), and a skin lesion over the testing site (n = 1). Table 1 shows demographic information for the participants. The cohort consisted of patients with mean duration of LBP of 113.7 months (range 1–360 months) and mean disability (ODI) of 28.2% indicating moderate disability. Subjects presented to each treating therapist with no significant differences in age, gender, ethnicity, duration of symptoms, FABQ-PA, FABQ-W, PCS, low back and leg pain, and PPT at initial intake. The only significant difference was one set of clinicians had patients with significant differences for their ODI score, F(3,30) = 4.37, p = .011.
Table 1.
Demographics and clinical characteristics of patient population
| Population sample (n = 34) | |
|---|---|
| Mean age (years) ± SD | 57.7 ± 18.7 |
| Gender, female (%) | 18 (52.9) |
| Race, n (%) | |
| African-American | 2 (5.9) |
| Asian American | 1 (2.9) |
| Hispanic | 1 (2.9) |
| Caucasian | 29 (85.3) |
| Other | 1 (2.9) |
| Educational level, n (%) | |
| High school | 15 (44.1) |
| College graduate | 10 (29.4) |
| Postgraduate education | 9 (26.5) |
| Currently employed, n (%) | 22 (64.7) |
| Previous history of LBP, n (%) | 27 (79.4) |
| Previous history of back surgery, n (%) | 8 (23.5) |
| Duration of LBP (months) ± SD | 113.7 ± 101.1 |
| Oswestry disability index ± SD | 28.2 ± 14.8 |
SD, standard deviation; LBP, low back pain.
LBP and leg pain
Mean scores with standard deviation for LBP and leg pain are reported for each test point (Table 2). NPRS for LBP significantly decreased following the conclusion of the physical exam from intake measurements and showed a moderate effect size, yet mean improvements did not meet or exceed MCID. Leg pain showed a significant change after history taking at a moderate effect size but did not reach MCID levels (Table 3). There was no difference found between the changes after history taking or physical exam with each individual clinician and their patients with these outcome measurements. Immediate following the history, eight patient’s (23.5%) LBP decreased ≥2 points exceeding MCID, while nine patient’s (26.5%) leg pain reduced ≥2 points. Four patient’s (11.7%) LBP decreased ≥2 points from after the history taking to after the physical examination and no patient’s leg pain eased with addition of the physical examination.
Table 2.
Mean outcome measurement scores at each time point
| Arrival | Post history | Post physical examination | |
|---|---|---|---|
| NPRS – low back | 3.97 ± 2.25 | 3.02 ± 2.14 | 2.74 ± 2.43 |
| NPRS – leg | 2.69 ± 2.67 | 1.65 ± 2.45 | 1.74 ± 2.57 |
| FABQ – PA | 12.97 ± 4.54 | 11.35 ± 5.36 | 10.29 ± 5.89 |
| FABQ – W | 14.06 ± 11.37 | 12.50 ± 11.03 | 11.59 ± 9.85 |
| PCS | 25.47 ± 9.19 | 22.76 ± 8.39 | 22.28 ± 8.76 |
| Lumbar flexion | 16.68 ± 11.56 | 14.41 ± 10.95 | 12.54 ± 11.33 |
| PPT – hand | 8.39 ± 4.20 | 9.57 ± 5.58 | 9.87 ± 6.09 |
| PPT – upper trapezius | 9.83 ± 5.51 | 11.36 ± 6.51 | 12.26 ± 7.06 |
| PPT – low back | 10.61 ± 6.37 | 13.05 ± 8.14 | 14.56 ± 9.12 |
Values are mean ± standard deviation.
NPRS, numeric pain rating scale; FABQ-PA, fear-avoidance belief questionnaire-physical activity subscale; FABQ-W, fear-avoidance belief questionnaire-work subscale; PCS, pain catastrophizing scale; PPT, pain pressure threshold.
Table 3.
Mean change score between each time point for pain, fear-avoidance, and catastrophization with significance values and effect sizes
| Friedman’s ANOVA |
Change between arrival and post history |
Change between post history and post physical examination |
Change between arrival and post physical examination |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | Mean change | p-Value | Effect size (r) | Mean change | p-Value | Effect size (r) | Mean change | p-Value | Effect size (r) | |
| NPRS – low back | 0.003 | 0.95 | 0.345 | 0.19 | 0.28 | 0.489 | 0.17 | 1.23 | 0.009 | 0.36 |
| NPRS – leg | <0.001 | 1.04 | 0.033 | 0.31 | −0.09 | 1.00 | −0.02 | 0.95 | 0.054 | 0.29 |
| FABQ – PA | 0.041 | 1.62 | 0.825 | 0.13 | 1.06 | .609 | 0.15 | 2.68 | .054 | 0.29 |
| FABQ – W | 0.097 | 1.56 | n/a | 0.18 | 0.91 | n/a | 0.13 | 2.47 | n/a | 0.29 |
| PCS | <0.001 | 2.71 | .003 | 0.40 | 0.48 | 1.00 | 0.09 | 3.19 | <0.001 | 0.49 |
NPRS, numeric pain rating scale; FABQ-PA, fear-avoidance belief questionnaire-physical activity subscale; FABQ-W, fear-avoidance belief questionnaire-work subscale; PCS, pain catastrophizing scale.
Psychosocial: FABQ and PCS
FABQ-PA improved at each time point but fell short of significance after applying the Bonferroni correction (Table 3). There were no differences found for FABQ scores between clinicians with their specific patients. Prior to the history, 13 patients (38.2%) exceeded the cutoff score of >14 points for increased disability, whereas the number of patients exceeding the cutoff was nine (26.5%) after the history and seven after the physical examination (20.6%). FABQ-WS also showed minimal improvements at each time point, but did not reach significance levels (Table 3). Only two patients exceeded the cutoff score >34 points at the initial evaluation, of which one dropped below the cutoff after the history and physical examination. PCS improved significantly with a moderate effect size from arrival to after history taking, but did not show a significant change between history taking and physical exam (Table 3). One significant difference was found between two therapists in patient improvements in PCS score after objective exam, F(3,30) = 3.14, p = .040. Prior to the history, 12 patients were classified as high on the PCS (score >30 points), whereas only 6 exceeded the cutoff after the history as well as the physical examination.
Physical tests: flexion and PPT
With each of the outcome measures of lumbar flexion and the three different PPT measures sphericity assumption was violated, so the Greenhouse–Geisser adjustment was used. Figure 1 showcases the differences in flexion during the examination process. Active lumbar flexion significantly improved following the history by 2.27 cm (p < 0.001), it improved another 1.86 cm following the physical examination (p < 0.001) for an overall increase of 4.14 cm (p < 0.001). None of the changes met or exceeded MCID and there were no differences between therapists for patient changes with lumbar flexion.
PPT change for the hand, upper trapezius, and low back from initial measurement to immediately after the history and following physical examination all exceeded MCID of 15% (Figures 2–4). But overlap in 95% confidence intervals between changes was evident. Some differences were found when comparing individual therapist’s changes after history taking or physical exam for the different PPT measurements, but none were consistent across all three measures or between specific therapists.
Figure 2.
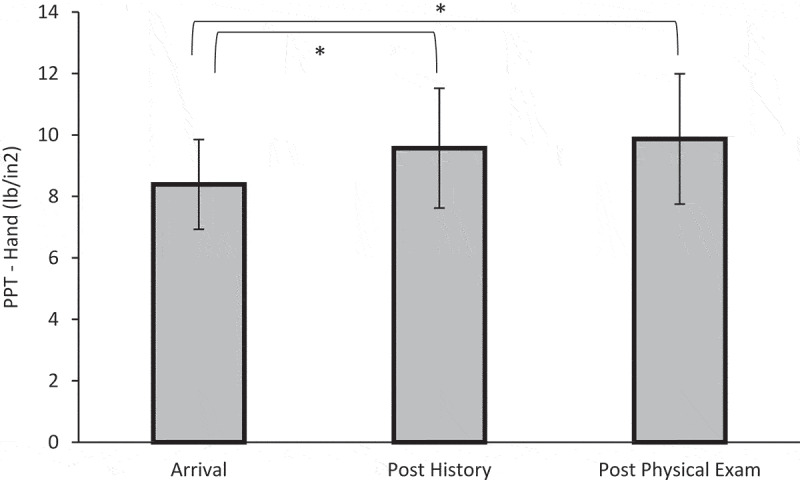
Means of pain pressure threshold (PPT) between each time point for the web space of the dominant hand in pounds per square inch (lb/in2) with 95% confidence interval bars. *p < 0.05 between arrival and post history and arrival and post physical exam
Figure 3.
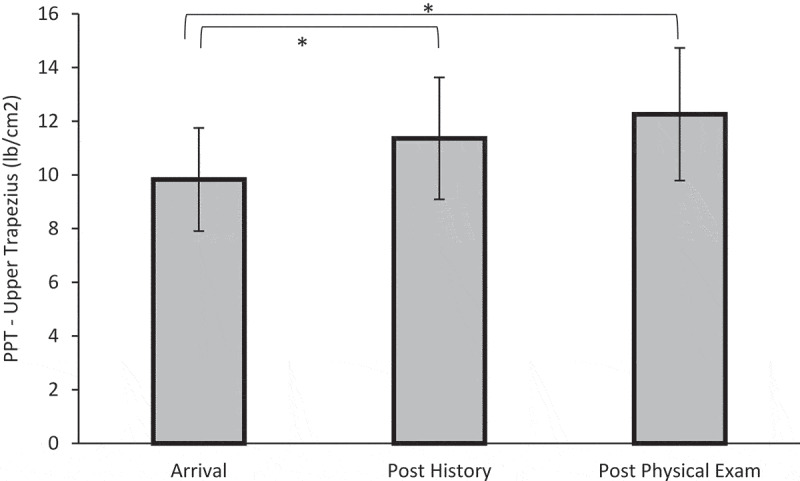
Means of pain pressure threshold (PPT) between each time point for the upper trapezius on their dominant side in pounds per square inch (lb/in2) with 95% confidence interval bars. *p < 0.05 between arrival and post history and arrival and post physical exam
Figure 4.
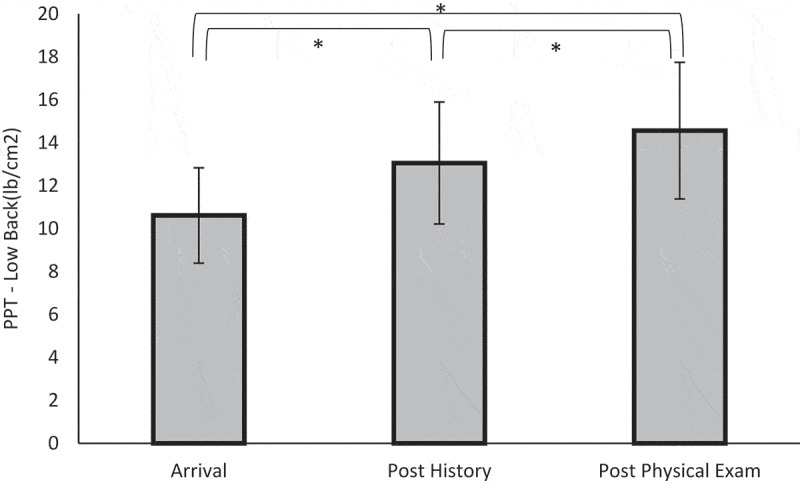
Means of pain pressure threshold (PPT) between each time point for the adjacent to L3 spinous process on their dominant side in pounds per square inch (lb/in2) with 95% confidence interval bars. *p < 0.05 between arrival and post history, post history and post physical exam, and arrival and post physical exam
Duration of evaluations
The mean duration of the history was 20.5 minutes (range 11–35 minutes) and physical examination was 18.4 minutes (range 8–41 minutes). There were no statistically significant correlations between the duration of the subjective examination and the pre-to-post changes of any of the outcome measures taken. There was significant differences, F(3,30) = 9.16, p < .001, between one clinician and two of the other three clinicians for longer duration of history taking portion of the exam. Mean duration of the history taking between each clinician was 13.67, 18.62, 21.63, and 28.57 minutes. The same clinician also had significant difference for a longer time for the physical exam, F(3,30) = 11.91, p < .001, between the other three clinicians. Physical exam mean duration of time for each clinician was 15.12, 15.17, 17.5, and 28.14 minutes. In contrast, the duration of the physical examination yielded a few positive correlations in regards to PPT at the low back (r = 0.366; p = 0.033) and hand (r = 0.345; p = 0.046). Interestingly, the duration of the objective examination also resulted in a negative correlation for the PCS (r = −.578; p < 0.001).
Connection with the patient
The mean score for perceived connection by the therapist during their history taking was 7.15 (range 3–10). There was no difference in connection score with all but one patient outcome scores between clinicians. PPT for the upper trapezius at intake was positively correlated to the perceived connection the PT felt during the examination process (r = 0.371; p = 0.031).
Discussion
In patients presenting with LBP to PT, the evaluation process of history taking and conducting a physical examination yields a significant therapeutic effect in regards to pain, fear-avoidance, pain catastrophization, movement, and sensitivity of the nervous system. Some changes met or exceeded clinical significant differences but they did not correlate to the duration of the examination and perceived connection by the PT.
Following the history taking, the NPRS leg pain, PCS, trunk flexion, and PPT measurements showed significant improvements from initial intake. With the completion of the combination of the history and physical examination, all these measures with the addition of NPRS for LBP improved significantly. In contrast, only two measures (active trunk flexion and PPT for the low back) were significantly improved with the addition of the physical examination when compared to the measurements after history taking. In all, the history taking yielded most of the significant changes seen in the evaluation process. It could be argued that the history, as first contact, versus the physical examination allowed for an immediate opportunity to connect, alleviate fears, and establish a TA. This assumption is supported by the current literature on TA that implies therapist characteristics such as strong communication and listening skills (verbal and non-verbal) [22,23,51–54], demonstrating empathy [23,55–59], being respectful and validating the patient [22,52,56,58], and developing rapport/connection [23,52,55,58,59]. Within the history taking, the display and use of the various bonding elements of TA fosters trust, which in many ways set up the remainder of the clinical encounter.
In this study, the physical examination also yielded a therapeutic effect by itself as well as enhancing various post-history measures. Physical tests are a cornerstone of a PT examination to rule in or out potential problems are a key element of patient expectations [9,10,]. The physical tests within the physical examination likely enhance confidence and alleviate fears of movement as seen in the immediate changes in ROM. The reduction in PPT for the low back may be due to potential changes in psychological variables related to the reduction of fear of movement after going through the physical examination process [60]. These results concur with studies showcasing the power of movement-based tests on movement [61,62]. The physical examination, however, cannot and should not be disconnected from the history and the results from this study may imply that the physical examination yielded such positive changes since the history taking set up the various parameters (TA and trust), which is essential for outcomes [8,17,20,21].
An interesting finding regarding the inverse correlation with time during the evaluation and the PCS was produced during this study. More time during the evaluation did show an increase in PCS, which may be due to the patient becoming more worried during the extended examination time. A quick yet thorough examination may reflect to the patient that everything is okay and more ‘normal’ than a longer examination. The longer examination time may create some increase magnification and rumination within the patient that the therapist is spending lots of time, thus finding more problems due to their negative outlook. Further study into this potential phenomena would be needed to confirm findings. There potentially could be middle range that is optimal for the examination process in regards to time. There most likely needs to be adequate time to develop the TA and gather needed information for the examination process, but not too long that TA gains neutralize or become a negative [23,52,55,58,59]. In essence, ‘being present’ and focused on the task at hand (examination and getting to know the patient) may be more important than just time alone [63].
The other surprising finding is that connecting with the patient did not correlate with the changes in pain or function. The fact that connection did not correlate may be due to the question only being asked from the PT-perspective and not the patient. Additionally, the field of ‘connection’ – be it from provider to patient or vice-versa is poorly understood, especially if they are different or similar when surveying clinician and patient. Future studies should explore this thought.
Study limitations
The study contained various limitations with the most pressing being the study design of a cohort observational study that cannot provide direct causal relationships occurred between the changes found in the outcome measures. The pragmatic design of the study with no specific controls put on history taking and physical examination process are uncontrolled variables in the study design that could affect the findings. Each therapist provided their history taking and examination in their usual fashion. This is demonstrated in the difference in time to deliver history taking and physical exam between each therapist, with one therapist taking significantly longer than the others. Even though this individual took longer, they did not see any improvements in any of the outcome measures compared to other clinicians. In fact, the few measurements that showed some significant differences between the different therapists, the clinician taking longer had lower improvements in their scores. Caution needs to be applied when looking at the individual therapist comparisons as the study design was not powered for this type of analysis, so false positive or negative results may be present. We look forward to future research questions with study designs developed and powered accordingly to further investigate the potential for history taking and physical examination process can have on outcomes.
History taking was done first on every patient followed by physical examination because of the pragmatic design of the study. The larger changes in outcome measures following the history portion may have been because it came first and if the order of delivery during the evaluation process was reversed with the physical examination taking place prior to subjective history taking the results may be reversed as well. Connection ratings were only asked of the clinician, not the patient and validation of the connection question has not been studied. The patient sample only contained patients with LBP, so it may be difficult to generalize findings to other patient populations. The short duration of the follow-up with the design being pre-post does not lead to indication of changes in outcome measures are sustained over time or if only maintained for only short time frame.
Another cause for the changes found could be due to the Hawthorne-effect. The patients may have demonstrated improvements purely from the fact of knowing they were being assessed during the study. The potential Hawthorne-effect actually plays into all clinical encounters as patients may alter their behavior due to the awareness of being observed and evaluated.
Post hoc power analysis showed that the sample size may have been too small based on effect sizes found at the α = 0.05 level. Because of the smaller sample size, there is more likely higher variability in the results, so they should be interpreted with caution as bias may be present. Small sample size increases the risk for Type II error for any of the differences between testing points and clinicians.
Conclusion
The examination process of history taking and physical examination lead to positive therapeutic effects of short-term decreases in pain, catastrophization, improved functional mobility, and decreased sensitivity to pressure in patients being seen for LBP by a PT. The most significant reduction was found after the initial history taking process. The examination process and ritual that occurs may be a vital component of the development of the therapeutic alliance and overall patient outcomes.
Biographies
Adriaan Louw, PT, PhD is a licensed physical therapist with a doctoral degree from Stellenbosch University. He is the owner of International Spine and Pain Institute, now affiliated with Evidence in Motion and teaches within the residency program as St. Ambrose University. He can be contacted at Adriaan@eimpt.com.
Steve Goldrick, PT, DPT is a licensed physical therapist with a clinical doctorate in physical therapy. He is board certified in orthopedics and provides patient care at Kitsap Physical Therapy in Silverdale, WA. He can be contacted at goldricksteve@gmail.com.
Andrew Bernstetter, PT, DPT is a licensed physical therapist with a clinical doctorate in physical therapy. He is board certified in orthopedics and provides patient care at Outpatient Physical Therapy in Kent, WA. He can be contacted at ABernstetter@outpatientpt.com.
Leonard H. Van Gelder, PT, DPT, ATC is a license physical therapist and athletic trainer with a clinical doctorate in physical therapy. He provides patient care at his clinic, Dynamic Principles L.L.C. in Grand Rapids, MI. He can be contacted at Leonard@dynamicprinciples.com.
Aaron Parr, PT, DPT is a licensed physical therapist with board certification in orthopedics and a clinical doctorate in physical therapy. He provides patient care at ProActive Physical Therapy in Tucson, AZ. He can be contacted at AParrqsi@gmail.com.
Kory Zimney, PT, DPT is a licensed physical therapist with a post professional clinical doctorate from Des Moines University. He is an associate professor at the University of South Dakota in the Department of Physical Therapy. He can be contacted at kory.zimney@usd.edu.
Terry Cox, PT, DPT is a licensed physical therapist with a clinical doctorate in physical therapy. He is a professor in the physical therapy doctoral program at Southwest Baptist University. He can be contacted at tcox@sbuniv.edu.
Funding Statement
The authors affirm that they have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
Highlights
This study shows that the evaluation process by itself plays a big role in the improvement of patients with low back pain at the initial consultation, not just the treatment.
The history taking portion showed to have a larger effect over the physical exam on reducing pain and function during the initial evaluation.
The therapist reported level of connection did not alter the improvements in pain in function following the evaluation process.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rivero-Arias O, Gray A, Frost H, et al. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine (Phila Pa 1976). 2006;31(12):1381–1387. [DOI] [PubMed] [Google Scholar]
- [3].Jette DU, Jette AM.. Physical therapy and health outcomes in patients with spinal impairments. Phys Ther. 1996;76(9): 930–941. discussion 942–935. [DOI] [PubMed] [Google Scholar]
- [4].Jette AM, Delitto A. Physical therapy treatment choices for musculoskeletal impairments. Phys Ther. 1997;77(2):145–154. [DOI] [PubMed] [Google Scholar]
- [5].Carey TS, Freburger JK, Holmes GM, et al. A long way to go: practice patterns and evidence in chronic low back pain care. Spine (Phila Pa 1976). 2009;34(7):718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zheng P, Kao MC, Karayannis NV, et al. Stagnant physical therapy referral rates alongside rising opioid prescription rates in patients with low back pain in the United States 1997–2010. Spine (Phila Pa 1976). 2017;42(9):670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Verghese A, Brady E, Kapur CC, et al. The bedside evaluation: ritual and reason. Ann Intern Med. 2011;155(8):550–553. [DOI] [PubMed] [Google Scholar]
- [8].Benedetti F, Amanzio M. The placebo response: how words and rituals change the patient’s brain. Patient Educ Couns. 2011;84(3):413–419. [DOI] [PubMed] [Google Scholar]
- [9].Verbeek J, Sengers MJ, Riemens L, et al. Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine (Phila Pa 1976). 2004;29(20):2309–2318. [DOI] [PubMed] [Google Scholar]
- [10].McRae M, Hancock MJ. Adults attending private physiotherapy practices seek diagnosis, pain relief, improved function, education and prevention: a survey. J Physiother. 2017;63(4):250–256. [DOI] [PubMed] [Google Scholar]
- [11].Hopayian K, Notley C. A systematic review of low back pain and sciatica patients’ expectations and experiences of health care. Spine J. 2014;14(8):1769–1780. [DOI] [PubMed] [Google Scholar]
- [12].Flynn TW, Fritz JM, Wainner RS, et al. The audible pop is not necessary for successful spinal high-velocity thrust manipulation in individuals with low back pain. Arch Phys Med Rehabil. 2003;84(7):1057–1060. [DOI] [PubMed] [Google Scholar]
- [13].Puentedura EJ, Landers MR, Hurt K, et al. Immediate effects of lumbar spine manipulation on the resting and contraction thickness of transversus abdominis in asymptomatic individuals. J Orthop Sports Phys Ther. 2011;41(1):13–21. [DOI] [PubMed] [Google Scholar]
- [14].Fernandez-de-Las-Penas C, Downey C, Miangolarra-Page JC. Immediate changes in radiographically determined lateral flexion range of motion following a single HVLA manipulation in patients presenting with mechanical neck pain: A case series. Int J Osteopathic Med. 2005;8:139–145. [Google Scholar]
- [15].Tsao H, Hodges PW. Immediate changes in feedforward postural adjustments following voluntary motor training. Exp Brain Res. 2007;181(4):537–546. [DOI] [PubMed] [Google Scholar]
- [16].Diener I, Kargela M, Louw A. Listening is therapy: patient interviewing from a pain science perspective. Physiother Theory Pract. 2016;32(5):356–367. [DOI] [PubMed] [Google Scholar]
- [17].Fuentes J, Armijo-Olivo S, Funabashi M, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2014;94(4):477–489. [DOI] [PubMed] [Google Scholar]
- [18].Joyce AS, Ogrodniczuk JS, Piper WE, et al. The alliance as mediator of expectancy effects in short-term individual therapy. J Consult Clin Psychol. 2003;71(4):672–679. [DOI] [PubMed] [Google Scholar]
- [19].Crepeau EB, Garren KR. I looked to her as a guide: the therapeutic relationship in hand therapy. Disabil Rehabil. 2011;33(10):872–881. [DOI] [PubMed] [Google Scholar]
- [20].Hall AM, Ferreira PH, Maher CG, et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90(8):1099–1110. [DOI] [PubMed] [Google Scholar]
- [21].Rash JA, Aguirre-Camacho A, Campbell TS. Oxytocin and pain: a systematic review and synthesis of findings. Clin J Pain. 2014;30(5):453–462. [DOI] [PubMed] [Google Scholar]
- [22].Grant S. Are there blueprints for building a strong patient-physician relationship? Am Med Assoc J Ethics. 2009;11:3. [DOI] [PubMed] [Google Scholar]
- [23].O’Keeffe M, Cullinane P, Hurley J, et al. What influences patient-therapist interactions in musculoskeletal physical therapy? Qualitative systematic review and meta-synthesis. Phys Ther. 2016;96(5). [DOI] [PubMed] [Google Scholar]
- [24].Kosfeld M, Heinrichs M, Zak PJ, et al. Oxytocin increases trust in humans. Nature. 2005;435(7042):673–676. [DOI] [PubMed] [Google Scholar]
- [25].Zak PJ, Kurzban R, Matzner WT. The neurobiology of trust. Ann N Y Acad Sci. 2004;1032:224–227. [DOI] [PubMed] [Google Scholar]
- [26].Walker SC, Trotter PD, Swaney WT, et al. C-tactile afferents: cutaneous mediators of oxytocin release during affiliative tactile interactions? Neuropeptides. 2017;64:27–38. [DOI] [PubMed] [Google Scholar]
- [27].Morhenn V, Beavin LE, Zak PJ. Massage increases oxytocin and reduces adrenocorticotropin hormone in humans. Altern Ther Health Med. 2012;18(6):11. [PubMed] [Google Scholar]
- [28].Deyo RA, Battie M, Beurskens AJ, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976). 1998;23(18):2003–2013. [DOI] [PubMed] [Google Scholar]
- [29].Fritz JM, Irrgang JJ. A comparison of a modified oswestry low back pain disability questionnaire and the quebec back pain disability scale. Phys Ther. 2001;81(2):776–788. [DOI] [PubMed] [Google Scholar]
- [30].Hakkinen A, Kautiainen H, Jarvenpaa S, et al. Changes in the total Oswestry index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J. 2007;16(3):347–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Moseley GL. Joining forces - combining cognition-targeted motor control training with group or individual pain physiology education: a successful treatment for chronic low back pain. J Man Manip Therap. 2003;11(2):88–94. [Google Scholar]
- [32].Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. [DOI] [PubMed] [Google Scholar]
- [33].Moseley GL. Widespread brain activity during an abdominal task markedly reduced after pain physiology education: fMRI evaluation of a single patient with chronic low back pain. Aust J Physiother. 2005;51(1):49–52. [DOI] [PubMed] [Google Scholar]
- [34].Cleland JA, Childs JD, Whitman JM. Psychometric properties of the neck disability index and numeric pain rating scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89(1):69–74. [DOI] [PubMed] [Google Scholar]
- [35].Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005;30(11):1331–1334. [DOI] [PubMed] [Google Scholar]
- [36].Farrar JT, Young JP Jr., LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. [DOI] [PubMed] [Google Scholar]
- [37].Cleland JA, Fritz JM, Childs JD. Psychometric properties of the fear-avoidance beliefs questionnaire and tampa scale of kinesiophobia in patients with neck pain. Am J Phys Med Rehabil. 2008;87(2):109–117. [DOI] [PubMed] [Google Scholar]
- [38].Grotle M, Vollestad NK, Brox JI. Clinical course and impact of fear-avoidance beliefs in low back pain: prospective cohort study of acute and chronic low back pain: II. Spine (Phila Pa 1976). 2006;31(9):1038–1046. [DOI] [PubMed] [Google Scholar]
- [39].Poiraudeau S, Rannou F, Baron G, et al. Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 2006;124(3):305–311. [DOI] [PubMed] [Google Scholar]
- [40].George SZ, Fritz JM, McNeil DW. Fear-avoidance beliefs as measured by the fear-avoidance beliefs questionnaire: change in fear-avoidance beliefs questionnaire is predictive of change in self-report of disability and pain intensity for patients with acute low back pain. Clin J Pain. 2006;22(2):197–203. [DOI] [PubMed] [Google Scholar]
- [41].Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–532. [Google Scholar]
- [42].George SZ, Valencia C, Beneciuk JM. A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. J Orthop Sports Phys Ther. 2010;40(4):197–205. [DOI] [PubMed] [Google Scholar]
- [43].Ekedahl H, Jonsson B, Frobell RB. Fingertip-to-floor test and straight leg raising test: validity, responsiveness, and predictive value in patients with acute/subacute low back pain. Arch Phys Med Rehabil. 2012;93(12):2210–2215. [DOI] [PubMed] [Google Scholar]
- [44].Perret C, Poiraudeau S, Fermanian J, et al. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil. 2001;82(11):1566–1570. [DOI] [PubMed] [Google Scholar]
- [45].Fernandez-de-Las-Penas C, Madeleine P, Caminero A, et al. Generalized neck-shoulder hyperalgesia in chronic tension-type headache and unilateral migraine assessed by pressure pain sensitivity topographical maps of the trapezius muscle. Cephalalgia. 2010;30(1):77-86. [DOI] [PubMed] [Google Scholar]
- [46].Moss P, Sluka K, Wright A. The initial effects of knee joint mobilization on osteoarthritic hyperalgesia. Manual Ther. 2007;12(2):109–118. [DOI] [PubMed] [Google Scholar]
- [47].Vicenzino B, Collins D, Benson H, et al. An investigation of the interrelationship between manipulative therapy-induced hypoalgesia and sympathoexcitation. J Manipulative Physiol Ther. 1998;21(7):448–453. [PubMed] [Google Scholar]
- [48].Sterling M, Jull G, Wright A. Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity. Manual Ther. 2001;6(2):72–81. [DOI] [PubMed] [Google Scholar]
- [49].Walton D, MacDermid J, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644–650. [DOI] [PubMed] [Google Scholar]
- [50].Portney LG, Watkins MP. Foundations of clinical research: applications to practice. Vol. 2. Upper Saddle River, NJ: Prentice Hall; 2000. [Google Scholar]
- [51].Ambady N, Koo J, Rosenthal R, et al. Physical therapists’ nonverbal communication predicts geriatric patients’ health outcomes. Psychol Aging. 2002;17(3):443. [DOI] [PubMed] [Google Scholar]
- [52].Bedi RP, Duff CT. Client as expert: a Delphi poll of clients’ subjective experience of therapeutic alliance formation variables. Counselling Psychol Q. 2014;27(1):1–18. [Google Scholar]
- [53].Fiscella K, Meldrum S, Franks P, et al. Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care. 2004;42(11):1049–1055. [DOI] [PubMed] [Google Scholar]
- [54].Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423. [PMC free article] [PubMed] [Google Scholar]
- [55].Bachelor A. Clients’ perception of the therapeutic alliance: a qualitative analysis. J Couns Psychol. 1995;42(3):323. [Google Scholar]
- [56].Goold SD, Lipkin M. The doctor–patient relationship. J Gen Intern Med. 1999;14(S1):26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Halpern J. What is clinical empathy? J Gen Intern Med. 2003;18:670–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Miciak M. Bedside matters: a conceptual framework of the therapeutic relationship in physiotherapy. University of Alberta; 2015. [Google Scholar]
- [59].Raue PJ, Goldfried MR, Barkham M. The therapeutic alliance in psychodynamic-interpersonal and cognitive-behavioral therapy. J Consult Clin Psychol. 1997;65(4):582. [DOI] [PubMed] [Google Scholar]
- [60].Walton DM, Levesque L, Payne M, et al. Clinical pressure pain threshold testing in neck pain: comparing protocols, responsiveness, and association with psychological variables. Phys Ther. 2014;94(6):827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Shapiro LM, Harris AHS, Eppler SL, et al. Can the QuickDASH PROM be altered by first completing the tasks on the instrument? Clin Orthop Relat Res. 2019;477:2062–2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Coppieters MW, Ryan L, Chan KP, et al. Do patients’ beliefs based on widespread medical information hinder accurate diagnosis? Paper presented at: 11th World Congress on Pain; 2005; Sydney. [Google Scholar]
- [63].Merel SE, McKinney CM, Ufkes P, et al. Sitting at patients’ bedsides may improve patients’ perceptions of physician communication skills. J Hosp Med. 2016;11(12):865–868. [DOI] [PubMed] [Google Scholar]


