TO THE EDITOR:
COVID-19 has become a pandemic and a major challenge for health professionals, the health care system, and the population itself. Most COVID-19 patients present with mild symptoms, including self-limited flu-like symptoms. However, approximately 20% present with moderate to severe disease, characterized by pneumonia. In addition, 5% can progress to severe respiratory failure, usually in the second week after symptom onset. 1 Chest CT findings include peripheral/bilateral ground-glass opacities or multifocal/rounded ground-glass opacities, with or without consolidation or crazy-paving pattern. 2 Other CT findings include the reversed halo sign and the target sign, as well as findings consistent with pulmonary embolism. 3 - 6 To our knowledge, this is the second reported case of a patient with COVID-19 and migratory pulmonary infiltrates consistent with organizing pneumonia (OP), the patient having responded well and rapidly to corticosteroid therapy. 7
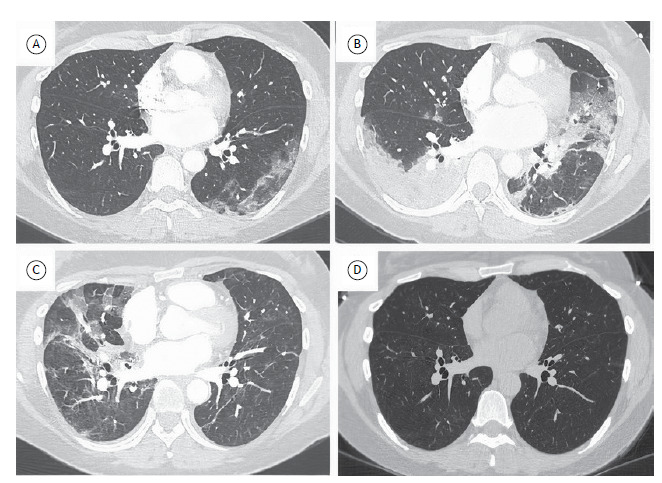
A 47-year-old female patient with follicular lymphoma was re-evaluated 33 days after the onset of COVID-19 symptoms. The patient was RT-PCR-positive for COVID-19 and reported progressive worsening of dyspnea, requiring supplemental oxygen at 2 L/min to reverse hypoxemia. Her laboratory test results were as follows: lymphocyte count, 1,040 cells/mm3; D-dimer level, 6,106 ng/mL; negative serum galactomannan; negative for cytomegalovirus by real-time serum PCR; normal procalcitonin; elevated C-reactive protein (15 mg/dL); and normal lactate. The chest CT scans were reviewed, showing migratory pulmonary infiltrates without signs of pulmonary thromboembolism (Figure 1). A presumptive diagnosis of OP was made on the basis of prolonged clinical progression and CT findings, and the patient was started on methylprednisolone at 80 mg/day. At 7 days after treatment initiation, the patient showed significant improvement, with a C-reactive protein level of 1.3 mg/dL and an SpO2 of 95% on room air, being discharged from the hospital. At 92 days after the onset of COVID-19 symptoms, a chest CT scan showed resolution of the pulmonary infiltrates and the patient had an SpO2 of 97% on room air and a C-reactive protein level of 1.0 mg/dL. Prednisone was tapered and discontinued after three months of treatment. At five months after the onset of COVID-19 symptoms, the patient remained asymptomatic, with an SpO2 of 97% on room air and a C-reactive protein level of 0.1 mg/dL.
Figure 1. HRCT scans taken 14 days, 24 days, and 33 days after the onset of COVID-19 symptoms (in A, B, and C, respectively) and showing progressive migratory pulmonary infiltrates consistent with organizing pneumonia. In D, HRCT scan showing resolution of the pulmonary infiltrates 92 days after the onset of COVID-19 symptoms.
The present case report adds to the literature on COVID-19. COVID-19 should be included in the differential diagnosis of migratory pulmonary infiltrates along with cryptogenic OP and secondary OP (associated with drugs such as amiodarone, bleomycin, cyclophosphamide, mesalazine, anticonvulsants, and cocaine; with diseases such as rheumatic diseases, leukemia, and lymphoma; and with radiation therapy, among other causes), as well as with eosinophilic pneumonia. 8
It should be noted that the patient was evaluated at a time when corticosteroid use was not standard therapy for patients with COVID-19 and hypoxemia. 9 , 10 In addition, there was a concern that the use of corticosteroids might worsen the prognosis of COVID-19, based on the literature on Middle Eastern respiratory syndrome, SARS, and even influenza. 10 Therefore, it was a challenge to decide whether or not to use corticosteroids in the present case. Prolonged duration of symptoms, as well as late clinical worsening, together with migratory pulmonary infiltrates, raised the hypothesis of OP secondary to infection (COVID-19), which was confirmed by the exuberant response to corticosteroids in our patient. In addition, our patient had a lymphoma, which can also cause migratory pulmonary infiltrates (consistent with OP). However, she had received six cycles of chemotherapy with rituximab, cyclophosphamide, vincristine, and prednisone for grade 3A follicular lymphoma, followed by maintenance therapy with rituximab every two months. A PET-CT scan taken after 11 cycles of maintenance therapy showed that the patient had achieved complete remission. Therefore, a neoplastic cause was thought to be less likely given the temporal relationship between RT-PCR positivity for SARS-CoV-2 and clinical and laboratory findings of COVID-19, as well as the fact that the symptoms did not recur after corticosteroid discontinuation. It is of note that the first reported case of COVID-19 and migratory pulmonary infiltrates (consistent with OP) was that of a leukemia patient who responded well to treatment with corticosteroids, clinical and CT findings of OP therefore being attributed to COVID-19. 7 In addition, our patient presented with chronic myeloid leukemia after the lymphoma and responded to treatment.
In conclusion, COVID-19 should de included in the differential diagnosis of migratory pulmonary infiltrates along with OP and eosinophilic pneumonia.
REFERENCES
- 1.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China Summary of a Report of 72?314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19 Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020;35(4):219–227. doi: 10.1097/RTI.0000000000000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martins RR, Santana VG, Souza DL, Reinaux JCF. New CT finding (the target sign) in three patients with COVID-19 pneumonia. J Bras Pneumol. 2020;46(6):e20200413. doi: 10.36416/1806-3756/e20200413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Müller CIS, Müller NL. Chest CT target sign in a couple with COVID-19 pneumonia. Radiol Bras. 2020;53(4):252–254. doi: 10.1590/0100-3984.2020.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jasinowodolinski D, Filisbino MM, Baldi BG. COVID-19 pneumonia a risk factor for pulmonary thromboembolism?. J Bras. Pneumol. 2020;46(4):e20200168. doi: 10.36416/1806-3756/e20200168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farias LPG, Strabelli DG, Sawamura MVY. COVID-19 pneumonia and the reversed halo sign. J Bras Pneumol. 2020;46(2):e20200131. doi: 10.36416/1806-3756/e20200131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.John TM, Malek AE, Mulanovich VE, Adachi JA, Raad II, Hamilton AR. Migratory Pulmonary Infiltrates in a Patient With COVID-19 Infection and the Role of Corticosteroids. Mayo Clin Proc. 2020;95(9):2038–2040. doi: 10.1016/j.mayocp.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cordier JF. Bronchiolitis obliterans organizing pneumonia. Semin Respir Crit Care Med. 2000;21(2):135–146. doi: 10.1055/s-2000-9840. [DOI] [PubMed] [Google Scholar]
- 9.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. Geneva: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/331446 [Google Scholar]


