ABSTRACT
Objective:
In ICU patients on mechanical ventilation (MV), ventilator-associated pneumonia (VAP) is a common infection. However, such infection can be prevented through oral care protocols. The objective of this study was to compare the efficiency of the use of chlorhexidine and oral hygiene protocols (brushing and clinical procedures) with that of the use of chlorhexidine alone (intervention group and control group, respectively) in decreasing the prevalence of VAP in patients ≥ 18 years of age admitted to the ICU and requiring MV.
Methods:
In this systematic review and meta-analysis, studies were identified through searches of various national and international databases, as well as of the gray literature, and were selected in accordance with eligibility criteria.
Results:
We evaluated six studies, involving a collective total of 1,276 patients. We classified the risk of bias as low in three studies, high in two, and uncertain in one; among the six risk domains evaluated, a low risk of bias was predominant in five. The results for random risks were similar in terms of direction and statistical magnitude-chi-square = 6.34; risk difference: −0.06 (95% CI: −0.11 to −0.02); I2 = 21%; p = 0.007. There was a decrease in the prevalence of VAP in the intervention group (n = 1,276) included in the meta-analysis.
Conclusions:
Protocols that include the mechanical removal of oral biofilm in combination with the use of chlorhexidine can reduce the incidence of VAP among ICU patients requiring MV.
Keywords: Intensive care units; Pneumonia, ventilator-associated; Oral hygiene; Respiration, artificial
RESUMO
Objetivo:
A pneumonia associada à ventilação mecânica (PAVM) é uma infecção frequente em UTI. No entanto, essa infecção pode ser evitada através de protocolos de cuidados orais. O objetivo deste estudo foi comparar a eficiência de protocolos de higiene bucal (escovação e procedimentos clínicos) aliados ao uso de clorexidina (grupo intervenção) com a de protocolos que fazem uso somente de clorexidina (grupo controle) na diminuição da prevalência da PAVM em pacientes adultos (≥ 18 anos) internados em UTI sob VM.
Métodos:
Nesta revisão sistemática e meta-análise, várias bases de dados nacionais e internacionais foram utilizadas para a identificação e seleção de estudos e literatura cinza seguindo critérios de elegibilidade.
Resultados:
Foram incluídos seis estudos, envolvendo 1.276 pacientes. Após a classificação dos estudos, três apresentaram baixo risco de viés, dois apresentaram risco de viés alto, e o risco foi incerto em um; entre os seis domínios avaliados houve predomínio de baixo risco de viés em cinco deles. Os resultados para riscos aleatórios foram semelhantes em direção e magnitude estatística - qui-quadrado = 6,34; diferença de risco: −0,06 (IC95%: −0,11 a −0,02); I2 = 21%; p = 0,007. Houve diminuição na prevalência de PAVM no grupo intervenção (n = 1.276) incluídos na meta-análise.
Conclusões:
Protocolos que incluem a remoção mecânica do biofilme associada ao uso de clorexidina podem reduzir a incidência de PAVM em pacientes internados em UTI sob VM.
Descritores: Unidades de terapia intensiva, Pneumonia associada à ventilação mecânica, Higiene bucal, Respiração artificial
INTRODUCTION
Mechanical ventilation (MV) is a support method for the treatment of patients with severe chronic or acute respiratory insufficiency. 1 Ventilator-associated pneumonia (VAP) is a pulmonary infection that develops ≥ 48 h after hospital admission in patients on MV (via tracheostomy or endotracheal intubation). Among all nosocomial infections, VAP has the greatest negative impact on patient outcomes and health care costs. 2
Prevention strategies for VAP include interventions such as elevating the head of the patient, administering antibiotics prophylactically, limiting the duration of MV, and discontinuing sedation. Oral hygiene has been considered an essential component of VAP prevention and, with standardized application, can significantly reduce the rate of respiratory tract infections due to microbial colonization. 3
Mouthwashes are efficient in reducing oral microbiota, and those that contain chlorhexidine are considered the gold standard, but there are many adverse effects associated with the use of chlorhexidine. Therefore, there is a tendency to search for mouthwashes that are as efficient as those with chlorhexidine, but with fewer adverse effects. 4
Pharmacological control of bacterial plaque through the use of chlorhexidine is practical and is widely accepted among health professionals. 5 However, mechanical cleaning might be the most efficient method to reduce pathogenic agents in the biofilm. 6
The objective of this systematic review and meta-analysis was to determine whether, in ICU patients, protocols involving the use of oral hygiene techniques (mechanical removal of biofilm) together with the use of chlorhexidine are more effective in decreasing the incidence of VAP than are those involving the use of chlorhexidine alone. As a secondary objective, we compared the protocols to determine whether there were differences in terms of the length of the ICU stay or in-hospital mortality.
METHODS
Protocol and registration
The present systematic review was conducted in accordance with the criteria from Preferred Reporting Items for Systematic Review and Meta-Analysis 7 and registered with the International Prospective Register of Systematic Reviews (Registration no. CRD42018083932).
Research information and search strategy
The descriptors were selected in accordance with the DeCS and MeSH lists of descriptors, and the questions were defined in accordance with the strategy known as PICO: Population-adult ICU patients (≥ 18 years of age) on MV; Intervention-different protocols involving oral hygiene combined with the use of chlorhexidine; Comparison-protocols involving the use of chlorhexidine alone; and Outcome-efficacy in reducing the incidence of VAP.
We performed searches of the following databases: PubMed (MedLine), the Brazilian Library of Dentistry, LILACS, the Nursing Database of the Brazilian Virtual Library of Health, SciELO, and the Cochrane Library (Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials); for the gray literature, we used the Brazilian Institute of Information in Science and Technology Digital Library of Theses and Dissertations. The search terms included the following descriptors, as well as their plural forms and synonyms-“Intensive Care Unit”, “Oral Hygiene”, “Ventilator Associated Pneumonia”, and “Randomized Clinical Trial”-in conjunction with Boolean operators (AND/OR). Searches were adapted in accordance with the particularities of each database. The following search strategy was used: “intensive care units”[All Fields] OR “ITU”[All Fields] OR “ITC”[All Fields] OR “intensive care centers”[All Fields] OR “intensive care center”[All Fields] AND “dentistry”[All Fields] OR “oral hygiene”[All Fields] OR “oral health”[All Fields] OR “care oral”[All Fields] OR “dental”[All Fields] AND “ventilator associated pneumonia”[All Fields] AND (“trial”[All Fields] OR “study trial”[All Fields] OR “clinical study”[All Fields] OR “randomized clinical study”[All Fields] OR “randomized clinical trial”[All Fields]). For the gray literature, in addition to the aforementioned database, manual search was also considered. There were no restrictions regarding the language or year of publication.
Eligibility criteria
The inclusion criteria were as follows: design-randomized clinical trials (RCTs); population-adult ICU patients (≥ 18 years of age) on MV; intervention-oral hygiene protocols (mechanical removal of biofilm) combined with the use of chlorhexidine; control-use of chlorhexidine only; and outcome measure-efficacy in reducing the incidence of VAP. Studies that evaluated patients already diagnosed with VAP, edentulous patients, or pregnant patients were excluded.
Study selection and collection
The studies identified in the databases were transferred to the reference manager EndNote Web (Clarivate, Philadelphia, PA, USA) for storage and exclusion of duplicates. Two reviewers, working independently, evaluated the titles and abstracts of the studies, applying the eligibility criteria, and a third reviewer evaluated any discrepant results. The potentially eligible studies (articles and theses) were then included in the second phase for a full-text reading, especially if the title and abstract did not provide enough information to include the study out of hand. Any disagreements were resolved through discussion with the third reviewer. Only the studies in which there were complete data on primary and secondary outcome measures were included in the meta-analysis.
Synthesis and presentation of data
The studies included were examined independently, and the relevant information was extracted to evaluate the quality of each study and synthesize the data. The details of the studies are shown in Table 1. Only the information available in the articles was considered. The data were presented as follows: author/year; country; sample size; intervention; control; and outcome measures (primary and secondary). We evaluated the incidence of VAP, as the primary outcome measure, by calculating absolute and relative frequencies. We also evaluated the secondary outcome measures length of ICU stay, by calculating the mean and standard deviation, and in-hospital mortality, by calculating the absolute frequency.
Table 1. Organization and presentation of data taken from the studies included in the qualitative and quantitative analyses.
| Study/country | Sample | Groups | Outcome measures | ||
|---|---|---|---|---|---|
| N | Intervention | Control | Primary | Secondary | |
| Bellíssimo-Rodrigues et al. 9 /Brazil | 254 | Tooth brushing, tongue scraping, calculus removal, atraumatic restorative treatment, tooth extraction, and irrigation with chlorhexidine at 0.12% or 2.0%, depending on the level of patient consciousness, 3 times a day (n = 127) |
Cleaning with gauze wrapped onto a tongue depressor, followed by rinsing with chlorhexidine at 0.12% or 2.0%, 3 times a day (n = 127) |
Prevalence of VAP Absolute frequency: IG: 18/127; CG: 8/127 Relative frequency: IG: 8.%; CG 18.% (RR = 0.38; 95% CI: 0.16-0.93; p = 0.030) |
Length of ICU stay, days: IG: 10.7 ± 10.6; CG: 11.3 ± 9.0 (p = 0.225) Mortality associated with lower respiratory tract infection: IG: 5/127; CG 8/127 (RR = 0.61; 95% CI: 0.19-1.92; p = 0.393) |
| The IG had more favorable results in reducing VAP than did the CG (p < 0.05). There were no significant differences between the groups in terms of the length of ICU stay on MV and in-hospital mortality. | |||||
| Félix et al. 10 /Brazil | 58 | Tooth brushing with a toothbrush soaked in 0.12% chlorhexidine, 3 times a day (n = 30) |
Cleaning with gauze soaked in 0.12% chlorhexidine, 3 times a day (n = 28) |
Prevalence of VAP Absolute frequency: IG: 1/30; CG: 3/28 Relative frequency: IG: 3.3%; CG: 10.7% (p = 0.344) |
NR |
| Neither protocol resulted in a significant decrease in the prevalence of VAP | |||||
| de Lacerda Vidal et al. 11 /Brazil | 213 | Tooth brushing with chlorhexidine gel at 0.12%, 2 times a day (n = 105) |
Irrigation with and suction extraction of chlorhexidine at 0.12%, 2 times a day (n = 108) |
Prevalence of VAP Absolute frequency: IG: 88/105; CG: 80/108 Relative frequency: IG: 37.8%; CG: 62.2% (RR = 1.81; 95% CI: 0.93-3.57; p = 0.084) |
Length of ICU stay, days IG = 8.7± 9.0; CG = 11.1 ± 7.6 (p = 0.018) In-hospital mortality: IG: 20/105 (42.5%); CG: 27/108 (57.5%) (RR = 1.41; 95% CI: 0.73-2.70; p = 0.2) |
| The IG showed a significant reduction in the length of ICU stay on MV (p < 0.05), although there were no statistical differences between the groups in terms of the decrease of VAP prevalence or in-hospital mortality | |||||
| Lorente et al. 12 /Spain | 436 | Brushing teeth and tongue for 90 s + gauze soaked in 20 mL of 0.12% chlorhexidine + irrigation of 10 mL of 0.12% chlorhexidine in the oral cavity for 30 s, 3 times a day (n = 217) |
Cleaning with gauze soaked in 20 mL of 0.12% chlorhexidine + irrigation of 10 mL of 0.12% chlorhexidine in the oral cavity for 30 s, 3 times a day (n = 219) |
Prevalence of VAP Absolute frequency: IG: 21/217; CG: 24/219 Relative frequency: IG: 9.7%; CG: 11.0% (p = 0.75) |
Length of ICU stay, days: IG: 12.07 ± 15.55; CG: 13.04 ± 17.27 (p = 0.54) In-hospital mortality: IG: 62/217 (28.6%); CG: 69/219 (31.5%) (p = 0.53) |
| There were no significant differences between the IG and CG in terms of the decrease in VAP prevalence, length of ICU stay, or in-hospital mortality. | |||||
| Nasiriani et al. 13 /Iran | 168 | Tooth brushing with a soft toothbrush with distilled water plus application of a cotton swab saturated in 0.12% chlorhexidine on the tongue, 2 times a day (n = 84) |
Use of saline solution and application of chlorhexidine on the tongue with a cotton swab soaked in the solution, 2 times a day (n = 84) |
Prevalence of VAP Absolute frequency: IG: 25/84; CG: 40/84 Relative frequency: IG: 29.8%; CG: 47.6% (p = 0.02) |
NR |
| The prevalence of VAP in intubated ICU patients was lower in the IG (p < 0.05). | |||||
| Pobo et al. 14 /USA | 147 | Electric toothbrush + use of 0.12% chlorhexidine, 3 times a day (n = 74) |
Use of 0.12% chlorhexidine, 3 times a day (n = 73) |
Prevalence of VAP Absolute frequency: IG: 15/74; CG: 18/73 Relative frequency: IG: 20.3%; CG: 24.7% (OR: 0.78; 95% CI: 0.36-1.65; p = 0.56) |
Length of ICU stay, days: IG: 8.9 ± 5.8; CG: 9.8 ± 6.1 (p = 0.45) In-hospital mortality General: 39/147 (26.5%) IG: 21.6%; CG: 31.5% (p = 0.19) |
| There were no significant differences between the IG and CG in terms of the decrease in VAP prevalence, length of ICU stay, or in-hospital mortality. | |||||
IG: intervention group; CG: control group; VAP: ventilator-associated pneumonia; MV: mechanical ventilation; NR: not reported; and RR: relative risk.
We extracted data on the study design, patient population, intervention, comparison, and clinical results. The main result of interest was prevention of VAP. Other results of interest were length of ICU stay and in-hospital mortality.
Evaluations of risk of bias and summarization
Although RCTs are the type of clinical study with the highest level of evidence, they are quite prone to biases, whether due to the arbitrariness of investigators in the selection of the sample and gauging of the variables analyzed or to the difficulty in controlling other factors that could influence the clinical outcome. Although there are several tools to evaluate the susceptibility to biases in RCTs, we used the Review Manager program, version 5.1 (RevMan 5; Cochrane Collaboration, Oxford, UK).
Quantitative analysis
The values for the frequency of VAP in ICU patients on MV were obtained from the studies selected. The results were divided into two groups: the intervention group-those obtained with protocols involving oral hygiene (brushing or clinical procedures) in combination with chlorhexidine; and the positive control group-those obtained with protocols involving the use of chlorhexidine only. For the meta-analysis, we chose the Review Manager program, version 5.3, with a significance level of 5%. In the comparison of the groups, the effect size defined was the difference between the absolute prevalences (difference between risks). 8 Fixed- and random-effects models were used in order to analyze the heterogeneity in the two models. The heterogeneity was evaluated with the chi-square method, and the I2 value was calculated. The I2 statistic (range, 0-100) was used in order to analyze the variations of heterogeneity: an I2 > 75 indicates significant heterogeneity.
RESULTS
Research and selection of studies
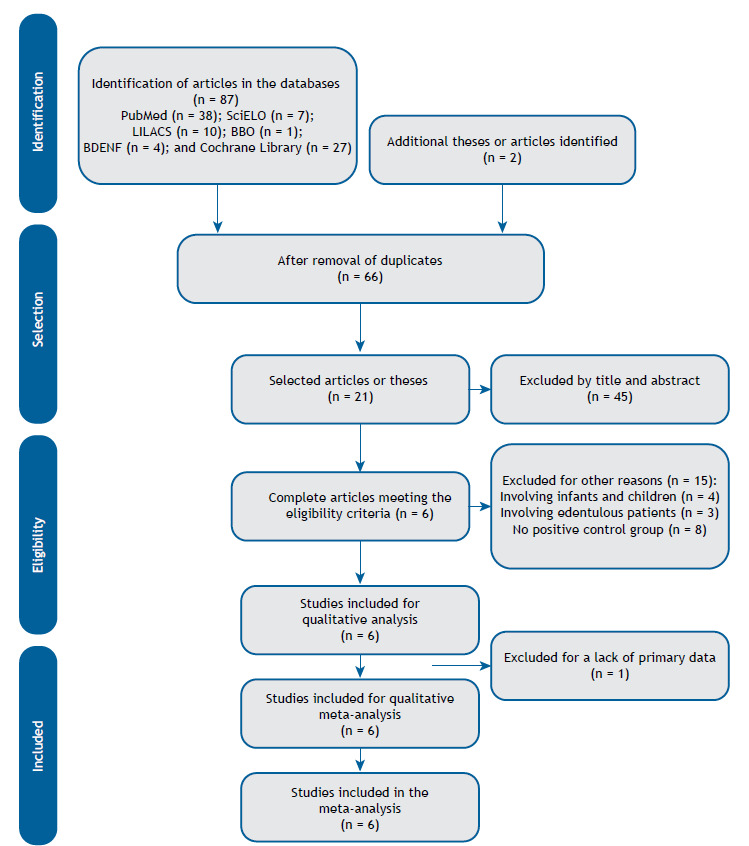
In total, 89 articles were identified and inserted into the reference manager. After the removal of duplicates, 66 studies remained. Of those, 21 were selected for the first phase of title and abstract reading. On the basis of the eligibility criteria, 15 articles were excluded: 4 because they included infants and children, 3 because they included edentulous patients, and 8 because they did not have a positive CG. Therefore, we included 6 studies in the qualitative review, including those same 6 studies in the meta-analysis (Figure 1). All of the studies included were published between 2009 and 2017.
Figure 1. Flow chart of the study selection process.BBO: Biblioteca Brasileira de Odontologia (Brazilian Library of Dentistry); and BDENF: Base de Dados de Enfermagem (Nursing Database [of the Brazilian Virtual Library of Health]).
Characteristics of the patient sample
The studies included in the present systematic review evaluated a collective total of 1,276 adult ICU patients on MV and comprised 3 studies conducted in Brazil, 9 - 11 1 conducted in Spain, 12 1 conducted in Iran, 13 and 1 conducted in the USA. 14 The participants included 770 males and 506 females. All of the participants were ≥ 18 years of age, and the mean age varied between 45 and 63 years. The main reasons for admitting the patients to the ICU were coronary diseases, diabetes, respiratory diseases, neurological diseases, and neoplasms.
Types of intervention and gauging scale
In the 6 studies included, oral hygiene routines were performed (Table 1): three times a day in 4 of the studies 9 , 10 , 12 , 14 ; and twice a day in 2. 11 , 13
Chlorhexidine was used in all of the studies included, although the concentration varied. The concentration used was 0.12% for all patients in 4 studies, 10 - 12 , 14 whereas the authors of 1 study adjusted the concentration from 0.12% in conscious patients to 0.2% in unconscious patients 9 and those of another study did not report the concentration. 13
In the intervention group, various tooth brushing techniques were employed: brushing with an electric toothbrush 14 ; brushing with distilled water 13 ; brushing with a toothbrush saturated in chlorhexidine 10 ; and brushing before the application of chlorhexidine. 11 Bellíssimo-Rodrigues et al. 9 employed a protocol involving tooth brushing, tongue scraping, removal of calculi, atraumatic restorative treatment, dental extraction, and rinsing with chlorhexidine. Lorente et al. 12 evaluated an oral hygiene protocol involving tooth brushing and cleaning with gauze soaked in 20 mL of 0.12% chlorhexidine, followed by 30-s irrigation of the oral and oropharyngeal area with 10 mL of 0.12% chlorhexidine, which was then extracted by suction.
The oral hygiene conditions were evaluated by different methods. In one study, 13 the Quigley-Hein plaque index, as modified by Turesky, 15 was used. In the remaining studies, 9 , 10 , 11 , 14 the evaluation method was not clearly described, the exception being the study conducted by Lorente et al., 12 who specifically stated that no such evaluation was performed.
Incidence of VAP
One study 13 showed that the incidence of VAP in was significantly lower in the intervention group than in the control group; in another study, 9 it was concluded that the dental care protocol evaluated was safe and effective in preventing VAP. Two studies 10 , 11 showed that the incidence of VAP was low after the application of the two oral hygiene techniques evaluated, with no significant differences between the two groups. However, another two studies 12 , 14 showed that other oral hygiene methods involving the use of chlorhexidine were not effective in preventing VAP.
In-hospital mortality
In relation to the reduction of in-hospital mortality, no significant difference between the groups was found in the study conducted by Belíssimo-Rodrigues et al. 9 However, the number of patients who died from VAP was 38.1% lower in the intervention group than in the control group. In another study, 11 in-hospital mortality was significantly lower in the intervention group than in the control group. Nevertheless, in three studies, 12 - 14 no significant differences were found in terms of in-hospital mortality, whereas in one study, 10 the difference in mortality between the groups was not mentioned.
Length of ICU stay
In relation to the length of ICU stay, one study 11 showed that it was shorter among the intervention group patients, although the difference was not statistically significant. Three studies 12 - 14 showed no significant differences related to the length of ICU stay between the intervention group and control group, whereas the length of ICU stay was not mentioned in two other studies. 9 , 10
Publication bias
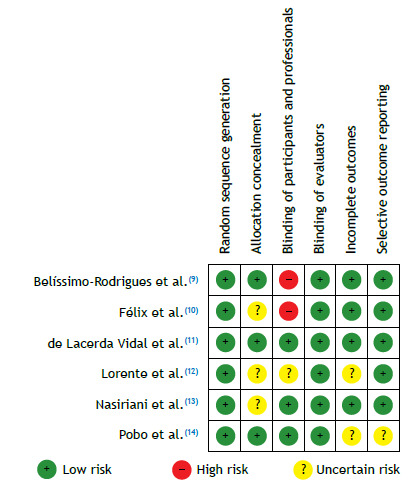
All of the studies were included in the evaluation of risk of bias. 16 This evaluation generally showed a predominantly low risk of bias in five domains; a high risk of bias was predominant in only one domain (blinding between patients and professionals; Figure 2). In the classification of individual risk of bias, three studies showed a low risk of bias, 9 , 10 , 13 and two other studies were considered to have a high risk of bias 12 , 14 ; only one study was classified as having an uncertain risk of bias, 11 as shown in Figure 3.
Figure 2. Risks of bias.
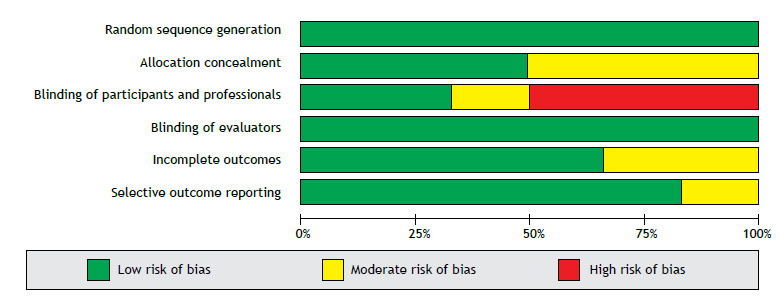
Figure 3. Summary of the risks of bias.
Meta-analysis
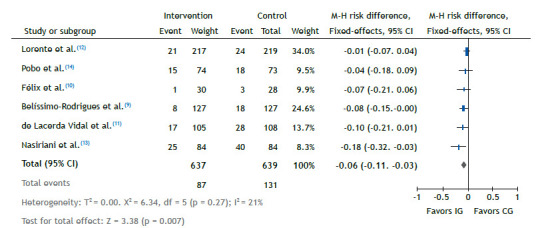
All of the studies were included in the meta-analysis, 9 - 14 comprising a collective sample of 1,276 patients. In the comparison between the intervention group and control group in relation to the prevalence of VAP, the synthesis of the analysis showed that the incidence of VAP was lower in the intervention group than in the control group (p = 0.007). Random-effects models (Figure 4) and fixed-effects models (Figure 5) were employed in the meta-analysis. The results for random risks were similar in direction and statistical magnitude-chi-square = 6.34; risk difference: −0.06 (95% CI: −0.11 to −0.02); I2 = 21%; p = 0.007-the analysis favoring the intervention group over the control group in terms of the decrease in VAP prevalence among ICU patients on MV.
Figure 4. Comparison between the intervention and control groups in relation to the decrease in the prevalence of ventilator-associated pneumonia, fixed-effects model. M-H: Mantel-Haenszel (method); df: degrees of freedom; IG: intervention group; and CG: control group.
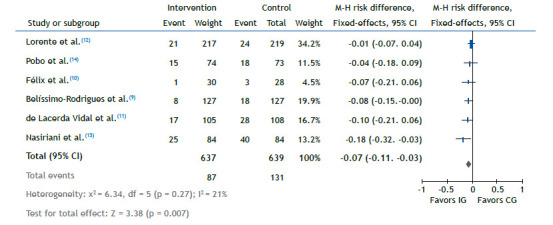
Figure 5. Comparison between the intervention and control groups in relation to the decrease in the prevalence of ventilator-associated pneumonia, random-effects model. M-H: Mantel-Haenszel (method); df: degrees of freedom; IG: intervention group; and CG: control group.
DISCUSSION
The results of the present meta-analysis allow us to state that mechanical removal of biofilm combined with the use of chlorhexidine was more effective in reducing the incidence of VAP than were other oral hygiene protocols. All of the studies showed a decrease in the incidence of VAP, although only two studies 9 , 13 showed significant differences between the intervention group and control group. The four other studies 10 - 12 , 14 showed no statistically significant differences.
There is scientific evidence that the use of chlorhexidine in different formulations (solution or gel) reduces the incidence of VAP from 25% to approximately 19%. 14 However, there is insufficient evidence regarding the impact that mechanical removal of biofilm (with manual brushing, brushing with an electric toothbrush, or gauze) has on that incidence. 12
Regarding in-hospital mortality, five studies 9 , 11 - 14 showed no statistically significant differences. However, two of those studies 9 , 11 reported reductions in the mortality rate related to VAP. In relation to the length of ICU stay, four studies 9 , 12 - 14 showed no significant differences between the groups. Only one study 11 showed such a difference, the length of stay being significantly shorter in the intervention group.
There is no convincing evidence that the use of chlorhexidine is associated with differences in in-hospital mortality, duration of MV, or length of ICU stay. 14 The mechanical removal of microorganisms can increase the efficacy of the effects of chlorhexidine on the remaining bacteria or diminish bacterial growth. 11 The meta-analysis showed that additional methods of hygiene (mechanical removal of biofilm) combined with the use of chlorhexidine are more effective in preventing VAP than is the use of chlorhexidine alone.
Our study has some limitations. There were differences across studies in terms of the proposed methods of oral hygiene, such as use of manual or electric toothbrushes, as well as the use of gauze, immersion of the toothbrush in distilled water, tongue scraping, and single versus multiple daily cleanings. The microbiological data to determine the relationship between VAP and the in-hospital mortality rate were not analyzed in the studies included in our meta-analysis. That limitation raises questions about the potential use of antibiotics, with the appearance of resistance, unnecessary adverse effects, and toxicity of those medications. There were no data regarding the oral microbiota and its contribution to the occurrence of VAP. In addition, strategies such as optimizing the time of intervention and personalizing the intensity of the individualization of risk should be adopted. Future studies adopting the same protocol for RCTs could be conducted in such a way that those adverse effects are minimized.
We conclude that ICU patients on MV get more benefit when various protocols for mechanical removal of biofilm (brushing or scraping) are combined with the concomitant use of chlorhexidine to reduce the incidence of VAP.
Footnotes
Study carried out at the Faculdade de Odontologia de Bauru, Universidade de São Paulo, Bauru (SP) Brasil.
REFERENCES
- 1.Carvalho CR, Toufen C, Jr, Franca SA. Mechanical ventilation principles, graphic analysis and ventilatory modalities [Article in Portuguese]. J Bras. Pneumol. 2007;33(2S):S54–S70. doi: 10.1590/S1806-37132007000800002. [DOI] [PubMed] [Google Scholar]
- 2.Bassi GL, Ferrer M, Marti JD, Comaru T, Torres A. Ventilator-associated pneumonia. Semin Respir Crit Care Med. 2014;35(4):469–481. doi: 10.1055/s-0034-1384752. [DOI] [PubMed] [Google Scholar]
- 3.Chacko R, Rajan A, Lionel P, Thilagavathi M, Yadav B, Premkumar J. Oral decontamination techniques and ventilator-associated pneumonia. Br J Nurs. 2017;26(11):594–599. doi: 10.12968/bjon.2017.26.11.594. [DOI] [PubMed] [Google Scholar]
- 4.ten Cate JM. Biofilms, a new approach to the microbiology of dental plaque. Odontology. 2006;94(1):1–9. doi: 10.1007/s10266-006-0063-3. [DOI] [PubMed] [Google Scholar]
- 5.Scannapieco FA. Role of oral bacteria in respiratory infection. J Periodontol. 1999;70(7):793–802. doi: 10.1902/jop.1999.70.7.793. [DOI] [PubMed] [Google Scholar]
- 6.Institute for Healthcare Improvement (HIH) Boston, MA: HIH; 2012. http://www.ihi.org [Google Scholar]
- 7.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellissimo-Rodrigues WT, Menegueti MG, Gaspar GG, Nicolini EA, Auxiliadora-Martins M, Basile-Filho A. Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients a randomized clinical trial. Infect Control Hosp Epidemiol. 2014;35(11):1342–1348. doi: 10.1086/678427. [DOI] [PubMed] [Google Scholar]
- 10.Félix LC. Two methods of oral hygiene with chlorhexidine in preventing of ventilator-associated pneumonia. Fortaleza: Faculdade de Farmácia, Odontologia e Enfermagem, Universidade Federal do Ceará; 2016. [Google Scholar]
- 11.de Lacerda Vidal CF, Vidal AK, Monteiro JG, Jr, Cavalcanti A, Henriques APC, Oliveira M, et al. Impact of oral hygiene involving toothbrushing versus chlorhexidine in the prevention of ventilator-associated pneumonia a randomized study [published correction appears in BMC Infect. Dis. 2017;17(1):173–173. doi: 10.1186/s12879-017-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorente L, Lecuona M, Jiménez A, Palmero S, Pastor E, Lafuente N. Ventilator-associated pneumonia with or without toothbrushing a randomized controlled trial. Eur J Clin Microbiol Infect Dis. 2012;31(10):2621–2629. doi: 10.1007/s10096-012-1605-y. [DOI] [PubMed] [Google Scholar]
- 13.Nasiriani K, Torki F, Jarahzadeh MH, Rashidi Maybodi F. The Effect of Brushing with a Soft Toothbrush and Distilled Water on the Incidence of Ventilator-Associated Pneumonia in the Intensive Care Unit. Tanaffos. 2016;15(2):101–107. [PMC free article] [PubMed] [Google Scholar]
- 14.Pobo A, Lisboa T, Rodriguez A, Sole R, Magret M, Trefler S. A randomized trial of dental brushing for preventing ventilator-associated pneumonia. Chest. 2009;136(2):433–439. doi: 10.1378/chest.09-0706. [DOI] [PubMed] [Google Scholar]
- 15.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41(1):41–43. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928–d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]


