Abstract
Objective
To optimize the ability of hospitalized patients isolated because of coronavirus disease 2019 (COVID-19) to participate in physical therapy (PT).
Design
This was a prospective quality improvement trial of the feasibility and acceptability of a “hybrid” in-person and telerehabilitation platform to deliver PT to hospitalized adults.
Setting
Inpatient wards of a tertiary care, multispecialty academic medical center in the greater New York City metropolitan area.
Participants
A convenience sample of 39 COVID-19–positive adults (mean age, 57.3y; 69% male) all previously community dwelling agreed to participate in a combination of in-person and telerehabilitation sessions (N=39).
Interventions
Initial in-person evaluation by physical therapist followed by twice daily PT sessions, 1 in-person and 1 via a telehealth platform meeting Health Insurance Portability and Accountability Act confidentiality requirements. The communication platform was downloaded to each participant's personal smart device to establish audiovisual contact with the physical therapist.
Main Outcome Measures
We used the 6-clicks Activity Measure of Post-Acute Care (AM-PAC) to score self-reported functional status premorbidly and by the therapist at baseline and discharge.
Results
Functional status measured by AM-PAC 6-clicks demonstrated improvement from admission to discharge. Barriers to participation were identified and strategies were planned to facilitate use of the platform in the future.
Conclusions
A consistent and structured protocol for engaging patient participation in PT delivered via a telehealth platform was successfully developed. A process was put in place to allow for further development, recruitment, and testing in a randomized trial.
KEYWORDS: Coronavirus, COVID-19, Pandemics, Physical therapy modalities, Rehabilitation, Telemedicine
List of abbreviations: AM-PAC, Activity Measure of Post-Acute Care; COVID-19, coronavirus disease 2019; PT, physical therapy; TR, telerehabilitation
New York City and the greater metropolitan area rapidly became 1 of the nation's first coronavirus disease 2019 (COVID-19) pandemic epicenters in the spring of 2020.1,2 One of the largest health systems in the state became the “epicenter of the epicenter,” caring for over 13,000 patients with COVID-19 between March and May 2020. Standard hospital protocol required that patients with COVID-19 be placed in strict contact and airborne isolation.3 This translated to social isolation, with room doors closed and limited interaction with hospital staff. In-room visits were kept to essential tasks, and the duration of each visit was encouraged to be reduced to conserve critically needed personal protective equipment and limit virus exposure. This resulted in a significant decrease in case load for the physical therapy (PT) team and marked decrease in the duration of contact between therapists and the isolated COVID-19–positive patients they served on the wards.
Telerehabilitation (TR), the delivery of PT and other rehabilitation services via a natural interface (eg, computer, tablet, smartphone) connecting patients and therapists, has been successfully used in the community, clinic, and home settings. Randomized controlled trials of TR have demonstrated success in populations such as advanced stage cancers, cerebrovascular accidents, and orthopedic conditions. In the community, home-based TR vs in-clinic therapy in people with osteoarthritis and cerebrovascular accidents demonstrated improvement in function4,5 In patients with advanced cancer, TR has also demonstrated health cost savings and decreased hospitalizations.6 A home-based TR program for veterans living in rural areas showed improvement in functional status, patient satisfaction, and quality of life.7 We found only 1 report on the use of TR in the hospital setting for patients with advanced cancer, which demonstrated improved function and decreased length of stay.8
In an effort to provide more effective PT during the first surge of COVID-19 hospitalizations and based on these encouraging reports, the Departments of Medicine and Physical Therapy initiated a TR feasibility and pilot study.9, 10, 11 The overall goal was to optimize frequency of inpatient PT for isolated patients, prevent hospital-acquired debility, and minimize length of stay.
Methods
First-time evaluations by a PT were conducted in person, and the quality improvement initiative was described to those with access to their own smart device (eg, phone or tablet). Potential barriers and challenges to participation were explored for all, and those who agreed were then oriented to the tele-PT process (described below).
Ethical considerations
This quality improvement feasibility initiative received a determination of “Not Research” from the Institutional Review Board. All participants were fully informed of the purpose of the project, were informed of the process to be followed, and gave verbal consent to participate.
Role of the funding source
The tablet devices the PT team used were iPadsa acquired through a philanthropic gift. The funders played no role in the design, conduct, or reporting of this study.
Context: screening and recruiting of patients
We screened and recruited a convenience sample of hospitalized patients using the following inclusion criteria: age ≥18 years, confirmed COVID-19 diagnosis, smart device at bedside and patient ability to use device independently, ability to follow verbal commands of therapist, and ability to actively perform exercises in bed or chair.
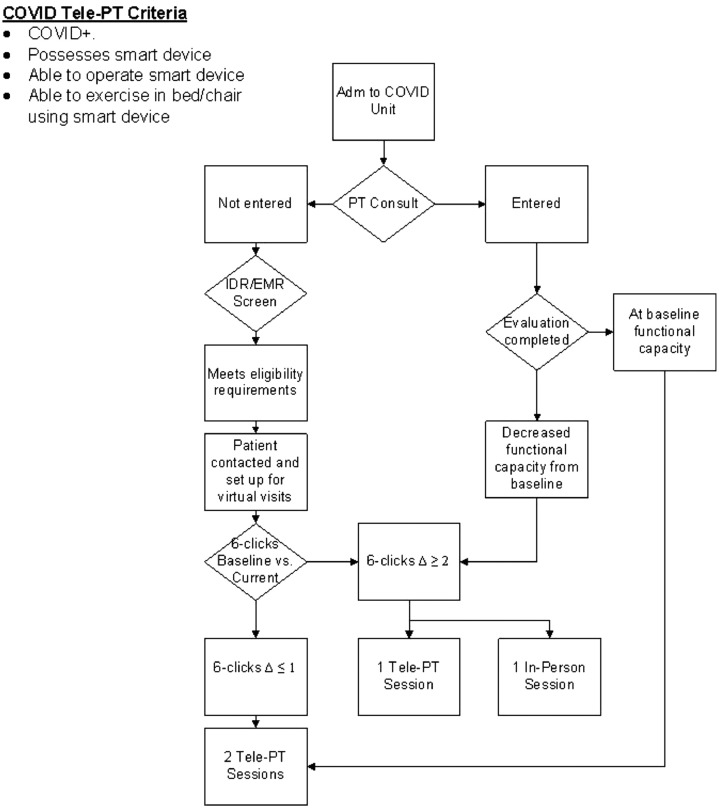
Potential participants were identified in several ways. PT staff reviewed patient census on medical wards daily (fig 1) between April 1, 2020 and June 1, 2020. Participants were also identified during in-person initial PT evaluations where a formal consult was requested. Finally, physical therapists participating in unit huddles and interdisciplinary rounds used these opportunities to identify patients who met inclusion criteria. Once identified, a dedicated telehealth physical therapist vetted each potential participant via phone or in person to ascertain interest and ability to participate in the project. If interested in participating, the patient needed to own a smart device with video capability and be able to independently operate the device when on the telehealth call.
Fig 1.
Enrollment protocol and procedure.
Intervention: PT sessions and telehealth setup
This quality improvement project used a hybrid approach to deliver PT, with a combination of in-person and TR visits. Standard practice for inpatient PT may vary significantly between facilities. Our frequency of follow-up PT sessions can vary from 3-7 in-person sessions per week depending on diagnosis and patient need. All sessions take place within the patient room, and the activities performed are aligned with patient ability. For example, a patient poststroke who is unable to move extremities may receive active, active-assisted, or passive range-of-motion exercises of the affected limbs, depending on muscle strength. Patients admitted for different medical conditions may participate in functional-based sessions; activities performed at the bedside may include movement in bed, transferring from sit to stand, ambulating, or stair climbing to maximize functional capacity and endurance. Although this is the standard approach, many hospitalized patients do not receive the full complement of PT sessions. Patients may be taken off the floor or detained in a testing location (eg, radiology) at the time of a planned PT session. Alternately, a patient may decline to participate if feeling too tired.
Because of isolation precautions imposed by the pandemic, all sessions reported here were conducted in patient rooms (in-person and TR). All PT sessions were conducted with the patient physically in their hospital room; in-person sessions were conducted with patient and therapist in the hospital room and wearing the required personal protective equipment. In-person evaluations and sessions were individualized to each patient's functional baseline, focusing on activities of daily living, bed mobility, transfers, and ambulation. Physical therapists took into consideration the mode of oxygen delivery and possible need for home oxygen at time of discharge. Tentative plans for safe and appropriate discharge measures were formulated after the initial evaluation.
TR sessions were conducted with the therapist located in the office of the PT department and via the audio-video “natural interface” created by the link between the patient's smart device and the therapist's iPad. The TR sessions focused on and reinforced therapeutic exercises in supine, sitting, and/or standing positions (depending on the patient's functional ability determined during the in-person sessions). Exercises focused on deep breathing, balance, and strengthening and were tailored to the patient's current abilities. Oxygen saturation as measured by pulse oximetry levels were monitored remotely to ensure maintenance of appropriate oxygenation during exertion.
The telehealth software used was Avizia,b which was downloaded onto an iPad controlled by the therapist. The patient had to download the complementary AmWell Touchpoint applicationc onto their smart device and open the application once the PT started the remote session. PT staff were available for the initial installation of the application onto the patient's smart device if needed.
Measures: baseline and follow-up assessments
Baseline assessment included premorbid function, social history, and assessment of living environment/situation. Total number of in-person PT and tele-PT sessions was recorded along with dates of each visit and any barriers or issues to participation at each time point. Function was captured using the 6-clicks Activity Measure of Post-Acute Care (AM-PAC) inpatient basic mobility form.12 The AM-PAC is a therapist-scored standardized assessment of basic mobility and daily activity measure rating an individual's functional status on 6 items: turning over in bed, sitting down/standing up from a chair with arms, moving from lying on back in bed to sitting on the edge, moving between bed and chair, walking in the room, and climbing 3-5 steps with a railing. Each item is scored on a 4-point scale, the first 3 items based on how much difficulty the patient has and the last 3 items on how much assistance is needed from another—unable, a lot, a little, or none.
A total AM-PAC score was calculated for premorbid function (based on self-report) and admission function for all participants. Although the goal was to obtain a final AM-PAC score at discharge, this was not possible for all participants (eg, patient discharged prior to therapist knowledge, patient died, etc).
Statistical analysis
Descriptive statistics and analysis of variance were run using SPSS.d Analysis of variance was used to compare change in AM-PAC scores from preillness baseline, admission, and discharge.
Results
Participants, PT sessions, and functional performance
A total of 48 patients were invited to join the program and 39 accepted. Approximately half of those enrolled were men; demographic information for all approached patients is shown in table 1. The average age of enrolled participants was 57.3 years (range, 31-87y), and the average age of those who declined was 70.6 years (range, 56-86y).
Table 1.
Demographic description of patients approached to participate in tele-PT
| Variables | Refused | Enrolled | Comments |
|---|---|---|---|
| Patients approached (n) | 9 | 39 | |
| Age (y), mean ± SD (range) | 70.6±9.1 (56-86) | 57.3±12.2 (31-87) | |
| Male, n (%) | 4 (44.4) | 20 (51.4) | |
| Reasons | |||
| Refused (security concern) | 3 (1) | 3 | 3 initial refusals or deferred |
| Tech issue | 3 | 1 | Flip phones, forgot access |
| Motor skills issue | 2 | - | Poor fine motor skills |
| Health literacy/language | 1 | 1 | Unable to read or write; English difficulty |
Of the 39 individuals who initially agreed to participate, 32 ultimately completed at least 1 tele-PT session. Seven withdrew for a variety of reasons, including technical difficulties, fine motor difficulty, unavailability when the therapist visited, preference for only in-person sessions, and discharge or death. Results and numbers of participants at each timepoint are reported in table 2.
Table 2.
Therapy sessions and function among participants
| Variables | Total n=32 | Men n=22 (68.8%) | Women n=10 (31.2%) |
|---|---|---|---|
| Age (y), mean ± SD (range) | 57.3±12.4 (31-87) | 55.8±11.1 | 56.3±16.3 |
| No. of PT sessions (n=32), mean ± SD | |||
| In-person | 2.5±1.7 | 2.3±1.4 | 2.9±2.2 |
| Tele-PT | 2.8±2.1 | 2.7±2.2 | 2.9±2.2 |
| AM-PAC (6-clicks function), mean ± SD | |||
| Preadmission (n=32; range, 23-24) | 23.9±0.5 | 24±0 | 23.9±0.6 |
| Admission (n=32; range, 8-24) | 19.0±4.8 | 19.0±4.7 | 19.0±5.2 |
| Discharge (n=19; range, 14-24) | 21.8±3.3 | 21.3±4.1 | 22.0±3.1 |
| Change Preadmission-admission | −4.9±4.8 | −4.8±4.7 | −5.0±5.2 |
| Change admission to discharge* | 2.5±3.2 | 2.4±3.1 | 2.8±3.8 |
| Change predischarge† | −2.1±3.2 | −1.8±2.9 | −2.7±4.1 |
Quadratic effect, F=13.2, P=.002, repeated measures analysis of variance, no effect of sex.
Function at discharge remained significantly less than premorbid, t=28.7, P<.001.
The average number of total PT sessions (in-person+TR) per participant was 5.25±3.6 (range, 2-16). The average number of in-person sessions was 2.5±1.7, and the average number of TR sessions was 2.75±2.1. Average number of daily sessions was 1.9±0.41 (based on the total number of days each patient was seen by PT).
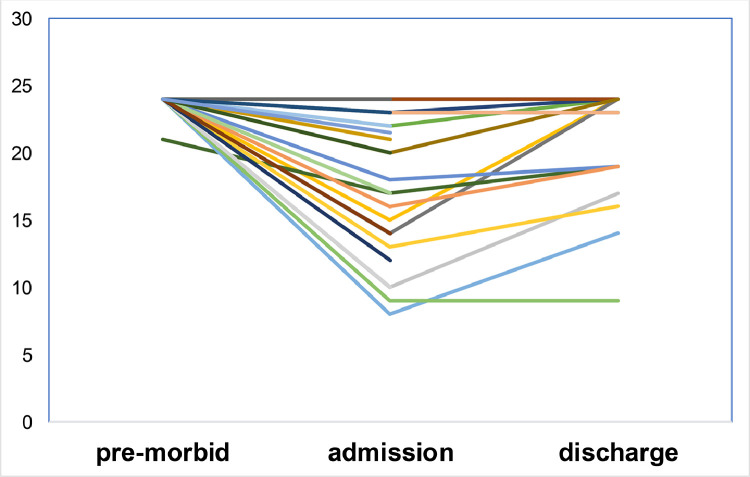
Self-reported premorbid function based on AM-PAC showed a highly functional group with a score of 23.9 of 24 maximum possible (see table 2). Mean AM-PAC function on admission was almost 5 points lower than self-reported baseline, 18.5±5.1 vs 23.9±0.5 (range, 8-24 vs 21-24). For the 19 participants for whom a discharge AM-PAC measure was available, there was significant improvement compared with admission (mean 2.5 points [range, 1-10 points]) but still less than premorbid function, repeated measures analysis of variance quadratic effect, F=13.2, P=.002 (see table 2) (fig 2). Final AM-PAC measures were missing on 13 participants who were discharged prior to a final PT session. These 13 participants were not significantly different in demographic characteristics (eg, age, sex, data not shown), self-reported preillness AM-PAC function (24.0±0 vs 23.85±0.5, t=0.97, P=.34), and admission AM-PAC (18.72±4.4 vs 18.55±5.49, t=0.106, P=.92).
Fig 2.
Change in 6-clicks AM-PAC.
Discussion
This brief quality improvement report describes the process for implementation and demonstrates the feasibility of delivering PT via a telehealth platform to individuals hospitalized and isolated because of COVID-19. Over 80% of the potentially eligible patients identified by a physical therapist out of a convenience sample agreed to participate; 67% of the total eventually engaged in tele-PT sessions. Participants had an average of 2 PT sessions per day and demonstrated improvement in function from admission to discharge.
Noting barriers to participation will help guide the team in planning for additional trials. For example, more easily manipulated devices (iPads or tablets) that can be sterilized and used by successive participants who lack their own smart devices. Use of “in-house” encrypted devices will also address concerns around security of health information. Additional strategies to assist those with impaired fine motor skills include tablets with larger surface areas and application of textured acetate covers that improve touch sensitivity. Other barriers that occur across the spectrum of health care in this country, such as English language proficiency and health literacy, pose more difficult challenges and will require additional resources.
Study limitations
Because this was a feasibility pilot, we did not control for demographic variables such as sex and age. The sample size was small, and data capture was incomplete; demographic information was limited to age and sex, there was not a standardized protocol for attempting to capture missing data points, and we were unable to contact participants postdischarge. We were also limited when determining severity of illness, which could significantly affect the ability to participate in PT. Future trials of this approach will take these variables into account and inform Intention to Treat design. Additional patient-centered outcome measures such as the Borg Perceived Exertion Scale13 will be needed to demonstrate improved effectiveness of this hybrid approach to conducting PT vs standard in-person only PT.
Conclusions
This pilot quality improvement project has demonstrated the feasibility of conducting PT with a hybrid combination of in-person and virtual sessions for hospitalized patients isolated with COVID-19. The team will continue to use this approach and is developing plans for a pragmatic trial. This hybrid model may also have broader applicability in hospitalized and homebound populations. Improvements for future studies would include providing each participant with a smart device during their hospital stay and easing use for those with limited fine motor skills. Participants regularly commented that they greatly appreciated the value of the extra PT session each day and the effort of the therapist in providing the service.
Suppliers
-
a
iPad; Apple Inc.
-
b
Avizia Connect Solution; American Well Corporation.
-
c
AmWell Touchpoint, version 20.05.0; American Well Corporation.
-
d
SPSS, version 26; IBM Corp.
Acknowledgments
We thank Greg Galdi, BS, and Custom Computer Specialists for their generous support, Kenneth McMillan, BA, for support and encouragement, and Jennifer Itty, MPH, for assistance with proofreading, formatting, and submitting the manuscript.
Footnotes
Part of this material was presented to an internal meeting sponsored by the Center for Health Innovations and Outcomes Research, Northwell Health, September 16, 2020, Manhasset, NY.
Supported by the National Institutes of Health (grant no. UG3AG060626), National Institute of Aging (grant no. R21 AG061307), National Institute of Aging (grant no. T35 AG029793-11), and National Institute of Aging/National Institute of Nursing Research (grant no. 5R21NR018500-02).
Disclosures: none
References
- 1.Centers for Disease Control and Prevention Severe outcomes among patients with coronavirus disease (COVID-19) – United States, February 12-March 16, 2020. MMWR Morb Motal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Preliminary estimate of excess mortality during the COVID-19 outbreak – New York City, March 11-May 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:603–605. doi: 10.15585/mmwr.mm6919e5. [DOI] [PubMed] [Google Scholar]
- 3.Palmore T, Sexton D, Mitty J. Coronavirus disease 2019 (COVID-19): infection control in health care and home settings. Available at:https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19-infection-control-in-health-care-and-home-settings#H969410871. Accessed August 14, 2020.
- 4.Azma K, RezaSoltani Z, Rezaeimoghaddam F, Dadarkhah A, Mohsenolhosseini S. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: a randomized clinical trial. J Telemed Telecare. 2018;24:560–565. doi: 10.1177/1357633X17723368. [DOI] [PubMed] [Google Scholar]
- 5.Cramer SC, Dodakian L, Le V. Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. 2019;76:1079–1087. doi: 10.1001/jamaneurol.2019.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Longacre CF, Nyman JA, Visscher SL, Borah BJ, Cheville AL. Cost-effectiveness of the Collaborative Care to Preserve Performance in Cancer (COPE) trial tele-rehabilitation interventions for patients with advanced cancers. Cancer Med. 2020;9:2723–2731. doi: 10.1002/cam4.2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy CE, Silverman E, Jia H, Geiss M, Omura D. Effects of physical therapy delivery via home video telerehabilitation on functional and health-related quality of life outcomes. J Rehabil Res Dev. 2015;52:361–370. doi: 10.1682/JRRD.2014.10.0239. [DOI] [PubMed] [Google Scholar]
- 8.Cheville AL, Moynihan T, Herrin J, Loprinzi C, Kroenke K. Effect of collaborative telerehabilitation on functional impairment and pain among patients with advanced-stage cancer: a randomized clinical trial. JAMA Oncol. 2019;5:644–652. doi: 10.1001/jamaoncol.2019.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Falvey JR, Mangione KK, Stevens-Lapsley JE. Rethinking hospital-associated deconditioning: proposed paradigm shift. Phys Ther. 2015;95:1307–1315. doi: 10.2522/ptj.20140511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoyer EH, Needham DM, Atanelov L, Knox B, Friedman M, Brotman DJ. Association of impaired functional status at hospital discharge and subsequent rehospitalization. J Hosp Med. 2014;9:277–282. doi: 10.1002/jhm.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kortebein P. Rehabilitation for hospital-associated deconditioning. Am J Phys Med Rehabil. 2009;88:66–77. doi: 10.1097/PHM.0b013e3181838f70. [DOI] [PubMed] [Google Scholar]
- 12.Pfoh ER, Hamilton A, Hu B, Stilphen M, Rothberg MB. The six-clicks mobility measure: a useful tool for predicting discharge disposition. Arch Phys Med Rehabil. 2020;101:1199–1203. doi: 10.1016/j.apmr.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]