Abstract
Background: The mobile cloud electrocardiography (C-ECG) system is useful for reducing door-to-balloon (DTB) time in patients with acute coronary syndrome (ACS), but few studies have reported the usefulness of the C-ECG system across a wide provincial prefecture, such as Oita, in Japan.
Methods and Results: On 17 April 2017, the C-ECG system was integrated into the Oita remote image transmission system, in 10 ambulances of 10 respective fire departments in Oita Prefecture. During 6 months, 162 ECG indicating suspected ACS were transmitted to 18 hospitals using the C-ECG system. Of 162 patients, 17 who received emergency percutaneous coronary intervention (PCI) were assigned to the cloud group (mean age, 71±11 years). The control group consisted of 29 consecutive ACS patients who were transported to Oita University Hospital without using the C-ECG system (mean age, 66±12 years). Another 40 consecutive patients were diagnosed with ACS before transportation to Oita University Hospital, and were assigned to the diagnosed group (mean age, 70±14 years). DTB time (70±26 min vs. 96±24 min, P<0.005) and door-to-catheterization laboratory time (33±20 min vs. 53±22 min, P<0.0001) were shorter in the cloud group than in the control group, respectively.
Conclusions: C-ECG system integration in Oita Prefecture was useful to appropriately transfer ACS patients to hospital and to facilitate earlier PCI than in the conventional diagnostic system.
Key Words: Acute coronary syndrome, Door-to-balloon time, Mobile cloud ECG system, Oita, Prehospital
A 12-lead electrocardiogram (ECG) should be recorded for a diagnosis of ST-segment elevation myocardial infarction (STEMI). The recorded ECG should be interpreted by cardiologists as soon as possible for early diagnosis and triage. In the European guidelines, it is recommended that a regional reperfusion strategy should be established to maximize the efficiency of treatment.1 An automated wireless network sends 12-lead ECG to the emergency hospital and cardiologists who are away from the patient can decrease door-to-intervention times to <90 min, and has been broadly applied in clinical practice.2 The mobile cloud electrocardiography (C-ECG) system has been shown to be useful for reducing door-to-balloon (DTB) time in patients with acute coronary syndrome (ACS).3,4
In the previous studies, a single medical center in town individually introduced the C-ECG system.3,5 Few studies, however, have reported the usefulness of C-ECG system across a wide area in a provincial prefecture, as Oita, in Japan. The specific aim of this study was to evaluate the impact of the C-ECG system on DTB time in patients with ACS who require percutaneous coronary intervention (PCI) in Oita Prefecture.
Methods
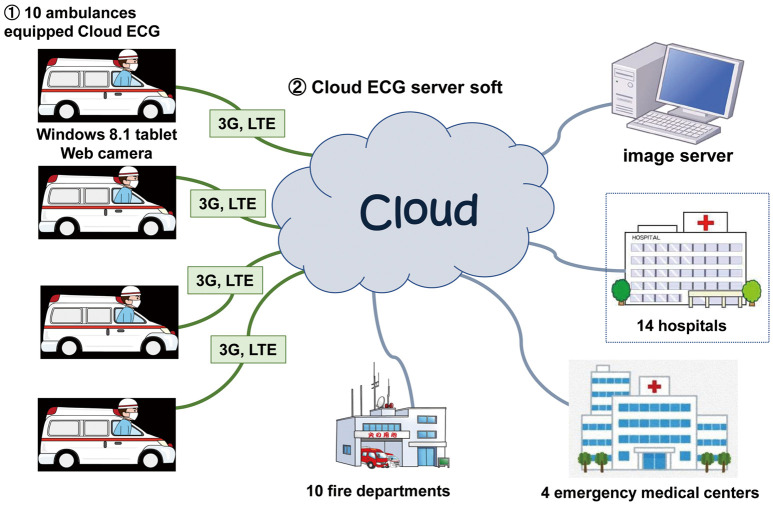
C-ECG in Oita
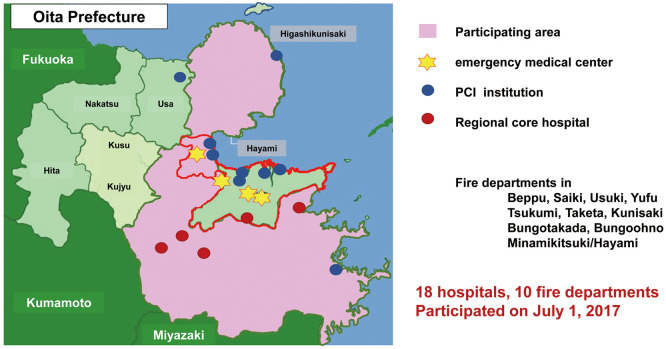
The Oita remote image transmission system consists of a remote image transmission system and a high-definition global positioning system vehicle tracking system. The system has been loaded into 34 ambulances of 10 respective fire departments in Oita Prefecture and was established utilizing administrative funds in 2013. The image in the ambulance and its location are sent to a tablet personal computer via a Bluetooth connection in the field, and transmitted to 4 emergency medical centers using LTE or the 3G cellular network. On 17 April 2017, the C-ECG system (Cloud Cardiology®; Labtech, Debrecen, Hungary) was integrated into the Oita remote image transmission system in 10 ambulances of 10 respective fire departments in Oita Prefecture. Ambulance crews obtain 12-lead ECG and transmit to a secure cloud server (Sucuna®; Mehergen, Japan), using the network of the existing image transmission system. The ECG in the cloud server could be browsed simultaneously from personal computers, smartphones, and tablets from anywhere after access key authentication (Figure 1). Immediately after the diagnosis of suspected ACS, the cardiologists in 18 hospitals participating in the C-ECG system, can decide on emergency cardiac catheterization before patient arrival at hospital. The locality of the 10 fire departments and 18 hospitals participating in the C-ECG system in Oita is shown in Figure 2 (pink area). Four emergency medical centers and 9 PCI institutions can carry out PCI, while the other 5 regional core hospitals cannot. In Oita Prefecture, the population in the 2 largest cities, that is, Oita City and Beppu City, comprises 50% of the total population, and PCI facilities are common in these 2 cities (Figure 2, area surrounded by red line).
Figure 1.
Schematic diagram of the integration of the cloud electrocardiogram (ECG) system into the Oita remote image transmission system.
Figure 2.
Location of the mobile cloud electrocardiogram (ECG) system in Oita. PCI, percutaneous coronary intervention.
Patient Selection
During 17 months, 162 ECG with suspected ACS were transmitted to hospitals by ambulances equipped with a C-ECG system. Of 162 patients, 17 received emergency PCI using the C-ECG system, and thus were assigned to the cloud group (5 women; mean age, 71±11 years), while 29 consecutive suspected ACS patients were transported to Oita University Hospital directly by a conventional ambulance, and thus were assigned to the control group (8 women; mean age, 66±12 years). A total of 40 consecutive patients were diagnosed with ACS before transportation to Oita University Hospital, and thus were assigned to the diagnosed group (10 women; mean age, 70±14 years).
Statistical Analysis
Data are presented as mean±SD. Chi-squared test was used for categorical variables, and analysis of variance (ANOVA) was used for continuous variables. The differences between groups were analyzed using Student’s t-test. P<0.05 was considered significant. All analysis was performed with JMP (version 13.2.0; SAS, Cary, NC, USA) running under Windows 10 (Microsoft, Redmond, WA, USA).
Results
Transmission Status
The transmission of ECG by the C-ECG system was successfully achieved in 96% of cases. In 7 cases, ECG transmission was not achieved successfully. This was due to human error in 4 cases, failure of Bluetooth connection due to insufficient battery charge in 2 cases, and malfunction of the application software in 1.
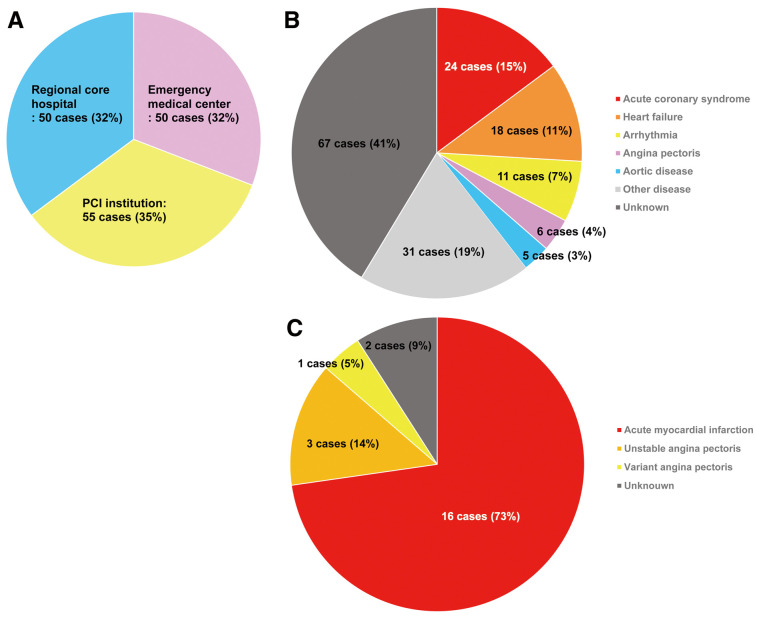
The institutions to which the 162 ECG were transmitted are shown in Figure 3A. Fifty ECG (32%) were transmitted to an emergency medical center, while 55 ECG (35%) were sent to a PCI institution. Fifty ECG (32%) were transmitted to a regional core hospital. The other 7, however, were excluded from analysis because the ECG were not successfully transmitted. Final diagnosis of the transferred patients is shown in Figure 3B. Cardiovascular disease other than ACS was more frequent. Although 24 cases were diagnosed as ACS using the C-ECG system, emergency coronary angiography (CAG) was performed in 19 cases (acute myocardial infarction [AMI], n=16; unstable angina pectoris [UAP], n=3; Figure 3C), and emergency PCI was performed in 17 cases (AMI, n=15; UAP, n=2). Of the 24 ACS patients, 7 did not receive emergency PCI (4 were judged not to need emergency PCI, 2 were transferred to regional core hospital because of bad systemic condition, and 1 did not agree to invasive treatment).
Figure 3.
(A) Institutions to where the cloud electrocardiogram was transmitted; (B) final diagnosis of the transferred patients; and (C) final diagnosis of patients who received emergency coronary angiography in Oita Prefecture. PCI, percutaneous coronary intervention.
Table 1 lists the number of patients finally diagnosed with or without ACS, according to where they were transferred. As shown, 58 patients were transferred to the regional core hospital. Fifty-six of 58 patients (96.6%) were finally diagnosed without AMI, and emergency CAG was unnecessary.
Table 1.
Diagnosis of ACS vs. Transfer Destination
| Transfer to emergency medical center/PCI institution (n=104) |
Transfer to regional core hospital (n=58) |
|
|---|---|---|
| Finally diagnosed with ACS | 22 | 2 |
| Finally diagnosed without ACS | 82 | 56 |
ACS, acute coronary syndrome; PCI, percutaneous coronary intervention.
Baseline Characteristics and Treatment
The baseline characteristics of the cloud group (n=17; mean age, 71±11 years), control group (n=29; mean age, 66±12 years), and diagnosed group (n=42; mean age, 70±13 years) are listed in Table 2. No significant difference was observed in age, gender, culprit vessel, number of diseased vessels, successful PCI, maximum creatine kinase, ejection fraction, or mortality between the 3 groups. Ejection fraction data were not available for 4 patients in the cloud group because of early death after PCI or for unknown reasons.
Table 2.
Subject Baseline Characteristics
| Cloud group (n=17) |
Control group (n=29) |
Diagnosed group (n=40) |
P-value | |
|---|---|---|---|---|
| Age (years) | 71±11 | 66±12 | 70±14 | NS |
| Female | 5 (29) | 8 (28) | 10 (25) | NS |
| Culprit vessel | NS | |||
| LMT | 3 (18) | 1 (3) | 3 (8) | |
| LAD | 8 (47) | 13 (45) | 12 (30) | |
| LCX | 1 (6) | 5 (19) | 8 (20) | |
| RCA | 5 (29) | 10 (34) | 17 (43) | |
| No. diseased vessels | NS | |||
| 1 | 9 (53) | 19 (66) | 14 (35) | |
| 2 | 5 (29) | 6 (21) | 17 (43) | |
| 3 | 3 (18) | 4 (14) | 9 (23) | |
| Successful PCI | 17 (100) | 29 (100) | 38 (95) | NS |
| Killip class | NS | |||
| 1 | 10 (59) | 18 (62) | 31 (78) | |
| 2 | 3 (18) | 5 (17) | 6 (15) | |
| 3 | 3 (18) | 3 (10) | 2 (5) | |
| 4 | 1 (6) | 3 (10) | 1 (3) | |
| Max CK (U/L) | 2,968±2,657 | 2,787±2,611 | 2,452±1,908 | NS |
| EF (%) | 50±11 (n=13) | 52±11 | 55±12 | NS |
| Mortality | 11.8 | 10.3 | 2.5 | NS |
Data given as mean±SD or n (%). CK, creatine kinase; EF, ejection fraction; LAD, left anterior descending artery; LCX, left circumflex coronary artery; LMT, left main trunk; PCI, percutaneous coronary intervention; RCA, right coronary artery.
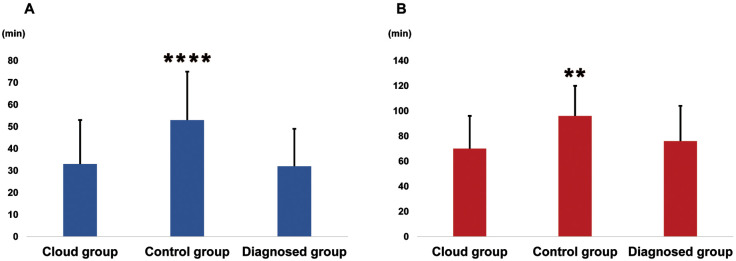
Time Intervals
DTB time ≤90 min was achieved in 82% in the cloud group and in 45% in the control group (P<0.005). DTB time (70±26 min vs. 96±24 min, P<0.005) and door-to-catheterization laboratory time (33±20 min vs. 53±22 min, P<0.0001) were shorter in the cloud group than in the control group, respectively. No significant difference was observed in DTB time or in door-to-catheterization laboratory time between the cloud group and the diagnosed group (Figure 4).
Figure 4.
(A) Door-to-balloon time and (B) door-to-catheterization laboratory time in patients with acute coronary syndrome in Oita Prefecture. **P<0.01, ****P<0.0001 vs. all other groups.
Discussion
The core findings of the present study are as follows: (1) this is the first report demonstrating the usefulness of C-ECG across a wide area of a provincial prefecture, Oita, in Japan; (2) the transmission of ECG was successfully achieved in 96%; and (3) DTB time (70±26 min vs. 96±24 min, P<0.005) and door-to-catheterization laboratory time (33±20 min vs. 53±22 min, P<0.0001) were shorter in the cloud group than in the control group, respectively.
Time delay in reperfusion therapy is an important issue in the management of STEMI. Detailed recommendations on timelines, logistics, and pre-hospital management have been described in the European Society of Cardiology (ESC) guidelines on STEMI.6 A recent Feedback Intervention and Treatment Times in ST-Elevation Myocardial Infarction (FITT-STEMI) trial emphasized the strong impact of time delay on mortality, particularly in STEMI patients with cardiogenic shock or out-of-hospital cardiac arrest.7 ESC guidelines on STEMI state that delay ≤60 min from first medical contact to PCI is desirable, and that a delay of 90 min should be considered as the upper limit.8 In STEMI patients, any delay in treatment increases the risk of major adverse cardiovascular events. Efforts should focus on improving patient awareness along with minimizing in-hospital transfer to the catheterization laboratory.9 In a previous study, the systematic implementation of a communication technology that allowed paramedics an instantaneous ECG image and voice consultation with a cardiologist reduced the total ischemic interval from 241 to 181 min.10
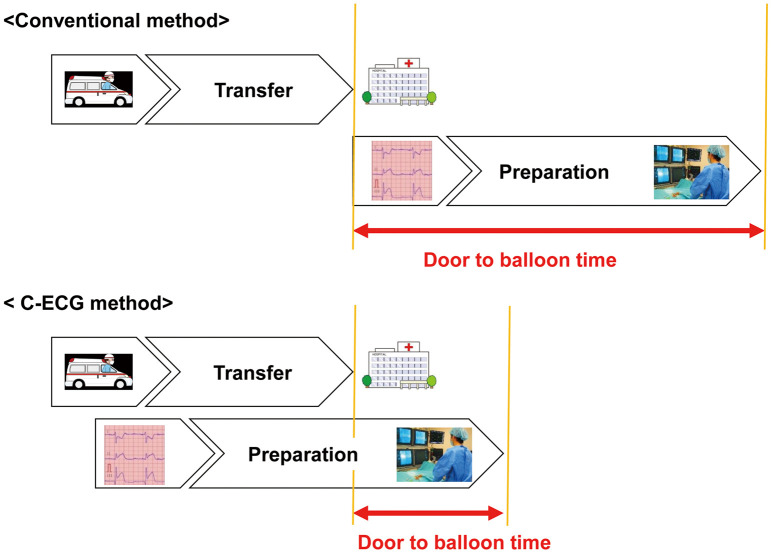
The biggest advantage of the C-ECG system is that cardiologists can simultaneously read the ECG waveforms and can decide whether emergency PCI is necessary or not. Therefore, preparation for emergency catheterization can be completed before the ambulance arrives at the hospital, and the patient can undergo PCI immediately in the catheterization room (Figure 5). In the present study, DTB time and door-to-catheterization laboratory time were shorter in the cloud group than in the control group. As shown in Figure 2, most of the PCI facilities are located in the 2 largest cities, that is, Oita City and Beppu City. These 2 cities occupy only 10% of the area of Oita Prefecture. Accordingly, ACS patients in the remaining 90% of Oita Prefecture have to be transported to PCI facilities at a very long distance away. Thus, the present study is important to demonstrate the usefulness of the mobile C-ECG system to shorten the DTB time in patients with AMI in remote areas.
Figure 5.
Shortening of transport time using the cloud electrocardiogram (C-ECG) system.
Another advantage of the C-ECG system is that it avoids transport of non-ACS patients to PCI institutions in remote regions. In this study, 58 patients (36% of the total patients) diagnosed as not having ACS on ECG were transferred not to a PCI institution but to the regional core hospitals. This shows that the C-ECG system could be helpful to transport true ACS patients appropriately to PCI institutions, with reduction of unnecessary ambulance transport.
The C-ECG system has been introduced across some prefectures in Japan,3 but the system in Oita Prefecture presented here has distinct features, in that many hospitals and fire department headquarters participate across the whole prefecture compared with other regions.3,11 The Oita remote image transmission system, which became the foundation of the C-ECG system, was established utilizing administrative funds in 2013. Fujita et al had proposed that the C-ECG system could be a powerful solution for cardiology emergency services, along with its significant clinical outcome.12 A demonstration of the C-ECG system was conducted between the advanced trauma emergency and critical care centers in Oita University Hospital and in Taketa City, in cooperation with the Department of Ubiquitous Health Informatics, University of Tokyo in 2012. One of the reasons for the success of the C-ECG system in Oita Prefecture might be the fact that the public Oita University Hospital encouraged many hospitals to participate in C-ECG system. In addition, another important feature of the Oita Prefecture system is the participation of the regional core hospitals that did not have PCI facilities.
In a previous study, DTB time >90 min did not influence the short-term outcome or first admission cost but did increase the 1-year cardiovascular readmission rate and the 1-year cardiovascular-related cost.13 Unfortunately, we could not obtain detailed data on cost effectiveness in the present study. The avoidance of emergency transportation to PCI facilities, however, might reduce the cost.
The following points, however, should be noted with regard to use of the C-ECG system. ACS is difficult to diagnose on ECG in the early stage. Other serious cardiovascular diseases such as acute aortic dissection, impending rupture of aortic aneurysm, and valvular disease, have no significant ECG change in general. These patients, however, should be transferred to hospitals where emergency surgical treatment can be performed. Although ECG is an important tool for emergency triage, it is dangerous to judge emergency cases using only the C-ECG system.
Currently, there is only 1 ambulance equipped with the C-ECG system for each fire department in Oita Prefecture. It is therefore impossible to cover the whole area of each fire department depending on the state of deployment. Since 20 March 2019, 8 more ambulances equipped with the C-ECG system have been provided in Oita Prefecture. In the future, we should further increase the number of participating hospitals, fire departments, ambulances equipped with the C-ECG system and network area. With such a network extension, more regional ACS patients will be able to benefit from the C-ECG system.
Conclusions
The C-ECG system integrated to Oita Prefecture was useful to appropriately transfer ACS patients to hospital, and to facilitate PCI earlier than the conventional diagnostic system.
Disclosures
There was no financial support for the present study.
References
- 1. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al.. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019; 40: 87–165.30165437 [Google Scholar]
- 2. Dhruva VN, Abdelhadi SI, Anis A, Gluckman W, Hom D, Dougan W, et al.. ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction (STAT-MI) trial. J Am Coll Cardiol 2007; 50: 509–513. [DOI] [PubMed] [Google Scholar]
- 3. Takeuchi I, Fujita H, Yanagisawa T, Sato N, Mizutani T, Hattori J, et al.. Impact of doctor car with mobile cloud ECG in reducing door-to-balloon time of Japanese ST-elevation myocardial infarction patients. Int Heart J 2015; 56: 170–173. [DOI] [PubMed] [Google Scholar]
- 4. Diercks DB, Kontos MC, Chen AY, Pollack CV Jr, Wiviott SD, Rumsfeld JS, et al.. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: Data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol 2009; 53: 161–166. [DOI] [PubMed] [Google Scholar]
- 5. Zhang XS, Leu FY, Yang CW, Lai LS.. Healthcare-based on cloud electrocardiogram system: A medical center experience in middle Taiwan. J Med Syst 2018; 42: 39. [DOI] [PubMed] [Google Scholar]
- 6. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al.. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018; 39: 119–177. [DOI] [PubMed] [Google Scholar]
- 7. Scholz KH, Maier SKG, Maier LS, Lengenfelder B, Jacobshagen C, Jung J, et al.. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: Results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J 2018; 39: 1065–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al.. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33: 2569–2619. [DOI] [PubMed] [Google Scholar]
- 9. Shahin M, Obeid S, Hamed L, Templin C, Gamperli O, Nietlispach F, et al.. Occurrence and impact of time delay to primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction. Cardiol Res 2017; 8: 190–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Studencan M, Alusik D, Plachy L, Bajerovska L, Ilavsky M, Karas J, et al.. Significant benefits of new communication technology for time delay management in STEMI patients. PLoS One 2018; 13: e0205832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ho CK, Chen FC, Chen YL, Wang HT, Lee CH, Chung WJ, et al.. using a cloud computing system to reduce door-to-balloon time in acute ST-elevation myocardial infarction patients transferred for percutaneous coronary intervention. Biomed Res Int 2017; 2017: 2963172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fujita H, Uchimura Y, Waki K, Omae K, Takeuchi I, Ohe K.. Development and clinical study of mobile 12-lead electrocardiography based on cloud computing for cardiac emergency. Stud Health Technol Inform 2013; 192: 1077. [PubMed] [Google Scholar]
- 13. Fan CM, Lai CL, Li AH, Chung KP, Yang MC.. Shorter door-to-balloon time in ST-elevation myocardial infarction saves insurance payments: A single hospital experience in Taiwan. Acta Cardiol Sin 2015; 31: 127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]