Abstract
Introduction
Aripiprazole and olanzapine are atypical antipsychotics. Both drugs can induce metabolic changes; however, the metabolic side effects produced by aripiprazole are more benign. The aim of the study was to evaluate if aripiprazole and olanzapine alter prolactin levels, lipid and glucose metabolism and hepatic, haematological, thyroid and renal function.
Methods
Twenty-four healthy volunteers received a daily oral dose of 10 mg aripiprazole and 5 mg olanzapine tablets for 5 days in a crossover randomised clinical trial and were genotyped for 51 polymorphisms in 18 genes by qPCR. Drug plasma concentrations were measured by LC–MS. The biochemical and haematological analyses were performed by enzymatic methods.
Results
Olanzapine induced hyperprolactinaemia but aripiprazole did not. Dopamine D3 receptor (DRD3) Ser/Gly and ATP binding cassette subfamily B member 1 (ABCB1) rs10280101, rs12720067 and rs11983225 polymorphisms and cytochrome P450 3A (CYP3A) phenotype had an impact on plasma prolactin levels. C-peptide concentrations were higher after aripiprazole administration and were influenced by catechol-O-methyltransferase (COMT) rs4680 and rs13306278 polymorphisms. Olanzapine and the UDP glucuronosyltransferase family 1 member A1 (UGT1A1) rs887829 polymorphism were associated with elevated glucose levels. CYP3A poor metabolizers had increased insulin levels. Volunteers’ weight decreased significantly during aripiprazole treatment and a tendency for weight gain was observed during olanzapine treatment. Triglyceride concentrations decreased as a result of olanzapine and aripiprazole treatment, and varied on the basis of CYP3A phenotypes and the apolipoprotein C-III (APOC3) rs4520 genotype. Cholesterol levels were also decreased and depended on 5-hydroxytryptamine receptor 2A (HTR2A) rs6314 polymorphism. All hepatic enzymes, platelet and albumin levels, and prothrombin time were altered during both treatments. Additionally, olanzapine reduced the leucocyte count, aripiprazole increased free T4 and both decreased uric acid concentrations.
Conclusions
Short-term treatment with aripiprazole and olanzapine had a significant influence on the metabolic parameters. However, it seems that aripiprazole provokes less severe metabolic changes.
Trial Registration
Clinical trial registration number (EUDRA-CT): 2018-000744-26
Graphical Abstract
Electronic Supplementary Material
The online version of this article (10.1007/s12325-020-01566-w) contains supplementary material, which is available to authorized users.
Keywords: Aripiprazole, Metabolism, Olanzapine, Pharmacogenetics, Pharmacokinetics
Key Summary Points
| Why carry out this study? |
| The metabolic side effects of aripiprazole and olanzapine were reported previously in patients and healthy volunteers. Our clinical trial is unique as we administered five doses of both drugs in a crossover design and we additionally associated the metabolic effects with genetic polymorphisms, which is also a novelty. |
| The hypothesis of the study was that genetic biomarkers may predict metabolic side effects induced by aripiprazole and olanzapine. |
| What was learned from the study? |
| Both antipsychotics have significant metabolic effects in acute treatment and several genetic polymorphisms are potential biomarkers to predict these changes. |
| These antipsychotics, especially olanzapine, induce metabolic changes even after five doses. These changes seem to be associated with genetic biomarkers, which ideally can be used to predict them for each individual before treatment initiation. |
Digital Features
This article is published with digital features, including a graphical abstract and summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13200650.
Introduction
Antipsychotic drugs are indicated for the treatment of schizophrenia and other psychotic disorders (schizoaffective disorder, delusional disorder and bipolar affective disorder, among others). They are categorized as first-generation (typical) antipsychotics (FGAs) or second-generation (atypical) antipsychotics (SGAs) [1]. Olanzapine (OLA) acts as an antagonist at dopamine D2 receptors (DRD2) and at serotonin (5-HT) 1A, 2A and 2C receptors similarly to other SGAs [2]. In contrast, aripiprazole (ARI) acts as a partial agonist at DRD2 and dopamine D3 receptors (DRD3) and at 5-HT1A and 5-HT2C receptors, and has antagonistic activity at 5-HT2A receptors. Therefore, ARI possesses a unique mechanism of action compared to other SGAs [3].
ARI is extensively metabolized by cytochrome P450 (CYP) isoforms CYP3A4 and CYP2D6. The main active metabolite—dehydroaripiprazole (DARI)—represents 40% of the parent drug in steady state [4]. OLA is metabolized predominantly by direct glucuronidation via the UDP-glucuronosyltransferase (UGT) enzyme family and CYP1A2, and to a lesser extent by CYP2D6 and CYP3A4 [5].
Several atypical antipsychotics—including OLA—cause plasma prolactin level elevation [6]. Normally, while switching the therapy from OLA to ARI mean prolactin levels decrease significantly even after 1 week of treatment and are maintained thereafter [7]. Nevertheless, ARI can also cause mild prolactin elevation in less than 5% of patients [6]. OLA is a D2 receptor antagonist and induces hyperprolactinaemia via inhibition of dopamine action at D2 receptors in the hypothalamus, where prolactin secretion is regulated [6]. On the contrary, serotonin stimulates prolactin secretion probably via stimulation of prolactin-releasing factors [8]. ARI acts as a functional antagonist under hyperdopaminergic conditions while it acts as a functional agonist under hypodopaminergic conditions at dopamine D2 receptors. D2 receptor stimulation provokes a suppression on prolactin secretion; therefore, ARI’s high D2 receptor occupancy does not induce hyperprolactinaemia in the majority of subjects [9].
DRD2 polymorphisms affected prolactin secretion induced by OLA in healthy volunteers after a single dose administration and in patients with schizophrenia under chronic treatment [10, 11]. Nevertheless, prolactin concentrations were not affected by DRD2 polymorphisms and CYP2D6 phenotype after ARI administration in patients with schizophrenia [12]. On the contrary, an association was found between prolactin levels and CYP2D6 phenotype and HTR2C polymorphisms in healthy volunteers [13].
Previous clinical trials with patients with schizophrenia demonstrated that ARI has a more benign side effect profile—regarding weight gain, blood sugar level and lipid profile—as compared to OLA in short-term treatment. Weight gain was observed more frequently in OLA-treated patients when compared with ARI. Mean serum triglyceride, blood glucose and cholesterol levels in patients treated with OLA were higher than in patients treated with ARI [14, 15]. Additionally, OLA was associated with significantly increased glucose levels compared to placebo and with a significantly greater change in the glucose levels compared to other antipsychotics [16]. In addition, when comparing lean mice and others on a high-fat diet, OLA induced hyperglycaemia and therefore systemic insulin resistance [17].
The aim of the current study was to evaluate the effect of ARI and OLA after multiple dose administration to healthy volunteers on lipid and glucose metabolism, hepatic, haematological and thyroid performance, and prolactin levels and its correlation with various factors including sex, plasma drug concentrations and selected genetic polymorphisms. This study is the first to administer five doses of these atypical antipsychotics to healthy volunteers in a crossover design and to associate the metabolic changes induced by them with genetic polymorphisms.
Methods
Study Population and Design
The study population comprised 24 healthy volunteers (12 men and 12 women) who were enrolled in a phase I, multiple oral doses, open-label, randomised, crossover, two-period, two-sequence, single-centre, comparative clinical trial. This sample size was considered sufficient to detect a clinically important difference in metabolism. Volunteers administered 10 mg/day ARI tablets or 5 mg/day film-coated OLA tablets (Laboratorios Alter, Madrid, Spain). Block randomization was used to assign the treatment to each volunteer on the first day [18]. The whole duration of the hospitalization was 5 days since 1 h before the first dose until 24 h after the administration of the last dose. The drug was administered at 0900 hours each day under fasting conditions. After a washout period of 28 days, each volunteer received the drug that they had not received in the first period. The random allocation sequence, the recruitment of participants and their assignment to interventions were performed by investigators of the clinical trials unit.
The clinical trial was performed at the clinical trials unit of our hospital. The protocol was approved by its research ethics committee (Comité Ético de Investigación Clínica (CEIC) of Hospital de La Princesa, registry number 3411) authorized by the Spanish Drugs Agency and the study was performed under the guidelines of Good Clinical Practice and the Declaration of Helsinki (clinical trial registry name, registration number, URL and date: TREATMENT-HV; EUDRA-CT 2018-000744-26; https://reec.aemps.es/reec/public/detail.html; 23 May 2018). All subjects signed the informed consent before inclusion and were free to withdraw from the study at any time.
The inclusion criteria were the following: male and female volunteers between 18 and 65 years old; free from any known organic or psychiatric conditions; normal vital signs and electrocardiogram (ECG); normal medical records and physical examination; no clinically significant abnormalities in haematology, biochemistry, serology and urine tests.
The exclusion criteria were the following: received prescribed pharmacological treatment in the last 15 days or any kind of medication in the last 48 h prior to receiving the study medication; body mass index (BMI) outside the 18.5–30.0 kg/m2 range; history of drug allergy; having galactose intolerance, lactase deficiency or glucose–galactose malabsorption; suspected consumers of controlled substances; smokers; daily alcohol consumers and/or experienced acute alcohol poisoning the previous week; donated blood last month; pregnant or breastfeeding women; investigational drug study participants in the previous 3 months and subjects unable to follow instructions or collaborate during the study.
Pharmacokinetic Analysis
Twenty-two blood samples were collected until 10 days after the last dose in EDTA K2 tubes for pharmacokinetic assessments during each period of the study. Samples were centrifuged at 3500 rpm (1900×g) for 10 min and then the plasma was collected and stored at − 80 °C until the determination of plasma concentrations. Plasma concentrations of ARI, DARI and OLA were quantified by a high-performance liquid chromatography tandem mass spectrometry (HPLC–MS/MS) method developed and validated in our laboratory [19].
The pharmacokinetic parameters were calculated by noncompartmental analysis by Phoenix® WinNonlin® (version 8, Pharsight, Mountain View, CA, USA). The peak concentration (Cmax) was obtained directly from the original data. The area under the plasma concentration–time curve from time zero to the last observed time point (AUClast) was calculated using the trapezoidal rule. The AUC from time zero to infinity (AUCinf) was determined as the sum of the AUClast and the extrapolated area beyond the last plasma concentration. The terminal rate constant (ke) used for the extrapolation was determined by regression analysis of the log-linear part of the concentration–time curve. The AUC and Cmax were adjusted for dose and weight (AUC/dW and Cmax/dW, respectively) and were logarithmically transformed for statistical analysis [20].
Biochemical and Haematological Analyses
The biochemical and haematological analyses were carried out by Eurofins Megalab S.A. (Madrid, Spain). All subjects underwent the oral glucose tolerance test (GTT) on days 1 and 6 with 75 g of oral anhydrous glucose dissolved in 250 mL water. Glucose, triglyceride, bilirubin, glutamate-oxaloacetate transaminase (GOT), glutamate-pyruvate transaminase (GPT), gamma-glutamyl transferase (GGT), albumin, alkaline phosphatase (ALP), uric acid, urea and creatinine concentrations were measured spectrophotometrically and the samples were collected at screening and on days 3, 6 and 15. Cholesterol levels were analysed by enzymatic colorimetric method at screening and days 3, 6 and 15. Prolactin levels were analysed on days 1, 3 and 5 before and after dosing and days 6 and 15, and C-peptide, insulin, thyroid stimulating hormone (TSH) and free thyroxine (T4) concentrations were quantified on days 1 and 6 by enzyme-linked immunosorbent assay (ELISA). Haemoglobin A1c (HbA1c) was measured on days 1 and 6. Haematocrit, platelet, leucocyte, haemoglobin and red blood cell (RBC) counts were measured by flow cytometry at screening and on days 3, 6 and 15. Finally, prothrombin time was determined by coagulometry at screening and on days 3, 6 and 15.
Genotyping
DNA was extracted from 1 mL of peripheral blood samples using a MagNA Pure LC DNA Isolation Kit in an automatic DNA extractor (MagNa Pure® System, Roche Applied Science, Indianapolis, Indiana). It was then quantified spectrophotometrically in a NanoDrop® ND-1000 Spectrophotometer (Nanodrop Technologies, Wilmington, Delaware, USA) and the purity of the samples was measured by the A260/280 absorbance ratio.
The samples were genotyped with TaqMan assays using the OpenArray platform on a QuantStudio 12K Flex instrument (Thermo Fisher Scientific, Waltham, Massachusetts, USA). The genotyping array included 120 single nucleotide polymorphism (SNPs), of which the following 51 were analysed in 18 genes because of their importance in the metabolism and the mechanism of action of ARI and OLA: CYP1A2*1C (rs2069514), *1F (rs762551), *1B 5347T>C (rs2470890), CYP2D6*3 (rs35742686), *4 (rs3892097), *6 (rs5030655), *7 (rs5030867), *8 (rs5030865), *9 (rs5030656), *10 (rs1065852), *14 (rs5030865), *17 (rs28371706), *41 (rs28371725), CYP3A4*22 (rs35599367), rs55785340, rs4646438, CYP3A5*3 (rs776746), *6 (rs10264272), ATP binding cassette subfamily B member 1 (ABCB1) C3435T (rs1045642), G2677 T/A (rs2032582), C1236T (rs1128503), rs3842, 1000-44G>T (rs10276036), 2895 + 3559C>T (rs7787082), 330-3208C>T (rs4728709), 2481 + 788T>C (rs10248420), 2686-3393T>G (rs10280101), 2320-695G A (rs12720067), 2482-707A>G (rs11983225), 2212-372A>G (rs4148737), ADRA2A rs1800544, APOC3 rs5128, rs4520, APOA5 rs662799, brain-derived neurotrophic factor (BDNF) Val66Met (rs6265), COMT rs4680, rs13306278, DRD2 TaqIA (rs1800497), 957C>T (rs6277), − 141 Ins/Del (rs1799732), DRD3 Ser9Gly (rs6280), HTR2A T102C (rs6313), C1354T (rs6314), rs7997012, HTR2C − 759C/T (rs3813929), − 697G/C (rs518147), rs1414334, leptin (LEP) rs7799039, leptin receptor (LEPR) rs1137101, opioid receptor mu 1 (OPRM1) rs1799971 and UGT1A1 rs887829 [20].
Results were analysed within both the QuantStudio™ 12K Flex and Thermo Fisher Cloud softwares (Thermo Fisher Scientific, Waltham, Massachusetts, USA). Finally, a matrix of genotypic calls was exported for each polymorphism.
The copy number variations (CNVs) in the CYP2D6 gene were determined with the TaqMan® Copy Number Assay (Assay ID: Hs00010001_cn; Thermo Fisher Scientific, Waltham, Massachusetts, USA) which detects a specific sequence on exon 9. The samples were run in the same instrument.
Whereas the CYP2D6*29 (rs16947) polymorphism was not included in the array, it was genotyped with the same instrument using individual TaqMan® probes. Additionally, the CYP3A4*20 (rs67666821) polymorphism was genotyped by the KASPar SNP Genotyping System (LGC Genomics, Herts, UK). The ABI PRISM 7900HT Sequence Detection System (Thermo Fisher Scientific, Waltham, Massachusetts, USA) was used for fluorescence detection and allele assignment [21].
Statistical Analysis
The statistical analysis was performed with the SPSS 24.0 software (SPSS Inc., Chicago, Illinois, USA). P values lower than 0.05 were considered statistically significant. The Hardy–Weinberg equilibrium was estimated for all genetic variants. Deviations from the equilibrium were detected by comparing the observed and expected frequencies using a Fisher exact test based on the De Finetti program (available at http://ihg.gsf.de/cgi-bin/hw/hwa1.pl). The metabolic parameters were analysed by repeated measures analysis of variance (ANOVA). Pharmacokinetic parameters and polymorphisms were analysed as covariates. Multivariate analysis of variance (MANOVA) was used to study factors related to all metabolic data and pharmacokinetic variables. Estimate of effect size (partial eta squared, ηp2), i.e. the proportion of the total variance that is attributed to an effect, is reported for each ANOVA test to avoid type II errors. The larger this value is, the more significant the effect is. The Bonferroni post hoc test for multiple comparisons was applied for each analysis to avoid type I errors.
CYP2D6*3, *4, *5, *6, *7, *8, *9, *10, *14, *17, *29 and *41 were classified in phenotypes based on the functionality of the alleles [22, 23]. CYP3A4*2, *20, *22, and CYP3A5*3 and *6 genotypes were merged into a CYP3A phenotype based on Sanchez Spitman et al. [24]. CYP1A2*1C, *1F and *1B variants were also merged into a phenotype as previously reported [25]. ABCB1 variants were merged into haplotypes: 0–8 mutated alleles were assigned to group 1, 9–12 mutated alleles were assigned to group 2 and 13–17 mutated alleles were assigned to group 3. Another ABCB1 haplotype was assembled by only considering C3435T, G2677T/A and C1236T polymorphisms owing to their greater impact on the transporter’s activity or expression levels [26]. Zero or one mutated allele carriers were assigned to group 1, carriers of 2 or 3 mutated alleles were assigned to group 2 and carriers bearing 4, 5 or 6 mutated alleles were assigned to group 3. COMT rs13306278 and rs4680 polymorphisms were merged into a haplotype: carrying no mutant allele was assigned as wild type, carrying one mutant allele was considered as heterozygous while bearing more than one mutant allele was considered as mutant.
Results
Demographic Characteristics
The study was performed between June 2018 and April 2019 including recruitment and follow-up visits. Demographic data are shown in Table S1 in the electronic supplementary material. Ten subjects were Caucasian and 14 were Latino. Average age was similar between men and women (p = 0.204). Men had greater weight and height than women (p < 0.001); however, the BMI values did not differ significantly (p = 0.798).
Genotype Frequencies
The genotype frequencies of the analysed genes are shown in Table S2. HTR2C rs3813929 and rs518147, ABCB1 rs4728709 and COMT rs13306278 were not in Hardy–Weinberg equilibrium (p ≤ 0.05). The rest of the polymorphisms were in Hardy–Weinberg equilibrium (p ≥ 0.05).
Genotype frequencies of ABCB1 C1236T, G2677T/A, 10276036 and rs4148737 and HTR2C rs518147 polymorphisms were significantly different between men and women (Table S2).
Pharmacokinetic Analysis
Mean and standard deviation (SD) of ARI, DARI and OLA pharmacokinetic parameters are shown in Table 1. Women had lower DARI/ARI ratio than men (p = 0.046). The remaining pharmacokinetic parameters were not statistically different between the two sexes. Associations between pharmacokinetic parameters and polymorphisms were reported previously [20].
Table 1.
Pharmacokinetic parameters of aripiprazole, dehydroaripiprazole and olanzapine after administration of five multiple doses
| All (n = 24) | Men (n = 12) | Women (n = 12) | |
|---|---|---|---|
| Aripiprazole | |||
| AUCinf (ng·h/mL) | 11,102.4 ± 8234.0 | 7789.1 ± 4071.5 | 14,415.7 ± 10,061.4 |
| Cmax (ng/mL) | 137.94 ± 45.92 | 129.6 ± 47.4 | 146.3 ± 44.9 |
| Dehydroaripiprazole | |||
| AUC24h (ng·h/mL) | 5149.8 ± 1628.6 | 4721.3 ± 1670.3 | 5578.3 ± 1534.8 |
| Cmax (ng/mL) | 34.88 ± 8.45 | 35.62 ± 9.62 | 34.13 ± 7.45 |
| Aripiprazole + dehydroaripiprazole | |||
| AUC24h (ng·h/mL) | 14,596.1 ± 6639.1 | 11,883.5 ± 4788.9 | 17,308.6 ± 7292.2 |
| Cmax (ng/mL) | 172.82 ± 48.74 | 165.27 ± 53.98 | 180.38 ± 43.93 |
| Dehydroaripiprazole/aripiprazole | |||
| AUC ratio | 0.64 ± 0.25 | 0.74 ± 0.27 | 0.54 ± 0.20* |
| Cmax ratio | 0.27 ± 0.08 | 0.29 ± 0.07 | 0.25 ± 0.09 |
| Olanzapine | |||
| AUCinf (ng·h/mL) | 1289.4 ± 370.1 | 1142.7 ± 291.2 | 1436.2 ± 393.1 |
| Cmax (ng/mL) | 19.10 ± 4.77 | 18.35 ± 4.04 | 19.85 ± 5.48 |
Values are shown as mean ± SD
Cmax maximum plasma concentration, AUCinf area under the curve from zero to infinity, AUC24h area under the curve over 24 h, AUC ratio dehydroaripiprazole/aripiprazole AUC ratio, Cmax ratio dehydroaripiprazole/aripiprazole Cmax ratio
*P ≤ 0.05 versus men
Prolactin Concentrations and Their Relationship with Pharmacogenetics
OLA caused a significant elevation in prolactin levels (p < 0.001, ηp2 = 0.474) (Fig. 1; men and women are shown separately because of the known differences of prolactin levels between the two sexes). Men had lower prolactin levels than women; however, the extent of the increment did not differ between them. Additionally, a significant interaction was found between OLA Cmax and prolactin levels (p = 0.006, ηp2 = 0.168). Moreover, DRD3 Gly carriers had significantly higher prolactin concentrations than volunteers with the Ser/Ser genotype (p = 0.036, ηp2 = 0.121).
Fig. 1.
Prolactin concentrations during the administration of a daily oral dose of aripiprazole 10 mg and olanzapine 5 mg tablets for 5 days in a men and b women. Results are shown as mean ± SD
Compared to OLA, ARI did not elevate prolactin levels. On the contrary, a tendency for decrease was observed but it did not reach significance (p = 0.052) (Fig. 1). Additionally, CYP3A poor metabolizers (PMs) had higher prolactin concentrations during ARI treatment compared to intermediate metabolizers (IMs) and extensive metabolizers (EMs) (p = 0.001, ηp2 = 0.226). ABCB1 rs10280101 A/A, rs12720067 C/C and rs11983225 T/T subjects had significantly higher prolactin concentrations compared to C, T and C allele carriers (p = 0.037, ηp2 = 0.123). However, when analysing ABCB1 haplotypes, this association could not be detected.
The same genetic associations were found in men and women. Prolactin levels were significantly higher during OLA treatment compared to ARI (p < 0.0001, ηp2 = 0.356). Prolactin levels were outside of the recommended range (men, 2–18 ng/mL; women, 3–30 ng/mL) during OLA treatment in 9 (75%) men and 9 (75%) women [27].
Glucose Metabolism and Its Relationship with Pharmacogenetics
C-peptide concentrations were significantly higher after completing ARI treatment compared to its initial levels (p = 0.030, ηp2 = 0.205) (Table 2). Additionally, the increase of C-peptide levels was greater in COMT rs4680 G/G subjects and rs13306278 T carriers compared to A carriers and C/C homozygotes, respectively (p = 0.010, ηp2 = 0.289; p < 0.001, ηp2 = 0.535, respectively). This association could not be detected when analysing the COMT phenotype. Moreover, although the insulin levels only tended to increase after ARI administration (p = 0.073), BDNF rs6265 C/C subjects had greater increment compared to the other genotypes (p = 0.040, ηp2 = 0.237). Likewise, DARI AUClast was indirectly proportional to the changes in insulin levels (p = 0.045, ηp2 = 0.228).
Table 2.
C-peptide, insulin, haemoglobin A1c and glucose levels during aripiprazole and olanzapine multiple dose treatment
| Aripiprazole | ||||||||
|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 6 | |||||||
| C-peptide (ng/mL)* | 1.60 ± 0.35 | 3.50 ± 3.85 | ||||||
| Insulin (mcU/mL) | 7.84 ± 2.37 | 9.61 ± 4.37 | ||||||
| C-peptide/insulin ratio | 0.22 ± 0.06 | 0.24 ± 0.09 | ||||||
| HbA1c (%) | 5.30 ± 0.22 | 5.28 ± 0.21 | ||||||
| Screening | Day 3 | Day 6 | Day 15 | |||||
| Glucose (mg/dL) | 80.33 ± 6.64 | 79.71 ± 6.49 | 80.87 ± 9.01 | 79.17 ± 5.84 | ||||
| Day 1 | Day 6 | |||||||
| 0 h | 60 min | 120 min | 0 h | 60 min | 120 min | |||
| GTT (mg/dL) | 81.79 ± 7.79 | 103.38 ± 35.63 | 76.00 ± 13.40 | 84.54 ± 8.82 | 122.04 ± 31.80 | 97.38 ± 21.56 | ||
| Olanzapine | ||||||||
|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 6 | |||||||
| C-peptide (ng/mL) | 1.69 ± 0.51 | 2.60 ± 2.29 | ||||||
| Insulin (mcU/mL) | 8.19 ± 2.31 | 10.40 ± 12.76 | ||||||
| C-peptide/insulin ratio* | 0.21 ± 0.03 | 0.25 ± 0.08 | ||||||
| HbA1c (%) | 5.36 ± 0.23 | 5.07 ± 1.09 | ||||||
| Screening | Day 3 | Day 6 | Day 15 | |||||
| Glucose (mg/dL) | 79.96 ± 7.52 | 79.38 ± 6.50 | 79.14 ± 8.05 | 80.71 ± 6.22 | ||||
| Day 1 | Day 6 | |||||||
| 0 h | 60 min | 120 min | 0 h | 60 min | 120 min | |||
| GTT (mg/dL)* | 81.88 ± 6.73 | 104.08 ± 33.81 | 89.38 ± 20.98# | 79.71 ± 8.65 | 124.21 ± 38.07 | 101.96 ± 28.51 | ||
*P ≤ 0.05. #p ≤ 0.05 compared to aripiprazole. Values are shown as mean ± SD
HbA1c haemoglobin A1c, GTT glucose tolerance test
After completing OLA treatment, the 1 and 2 h glucose levels after performing GTT were higher compared to the measurements on the first day (p = 0.007, ηp2 = 0.213) (Table 2). In addition, these changes were dependent on the UGT1A1 rs887829 genotype: C/C homozygote subjects had significantly higher glucose concentrations in GTT both after 1 h and 2 h than the T allele carriers (p = 0.014, ηp2 = 0.186). Moreover, this polymorphism was additionally related to a higher increase in glucose levels in C/C subjects compared to the T allele carriers (p = 0.013, ηp2 = 0.258). Additionally, the insulin levels of CYP3A PMs incremented more compared to EMs and IMs (p = 0.029, ηp2 = 0.217). Moreover, OLA administration increased the C-peptide/insulin ratio (p = 0.044, ηp2 = 0.196).
Glucose levels in the first day’s GTT test were higher in OLA-treated subjects compared to ARI-treated subjects (p = 0.011, ηp2 = 0.131); however, ARI showed the same tendency. The increment in glucose levels after GTT and the increment of C-peptide levels did not differ between ARI and OLA (Table 2). No changes were detected in HbA1c.
No differences were found between men and women, nor in C-peptide, insulin, glucose and GTT levels, and nor in the genetic associations. No levels were outside of the normal range.
Weight and Lipid Metabolism and Their Relationship with Pharmacogenetics
During ARI treatment, volunteers’ weight decreased significantly (p < 0.0001, ηp2 = 0.301). On the contrary, a tendency for weight gain was observed during OLA treatment, but it did not reach significance (p = 0.120) (Fig. 2). Additionally, a significant difference was found when comparing weight changes between ARI and OLA treatment (p < 0.001, ηp2 = 0.301). Moreover, HTR2C rs1414334 C/C subjects gained significantly more weight compared to T carriers (p = 0.002; ηp2 = 0.196).
Fig. 2.
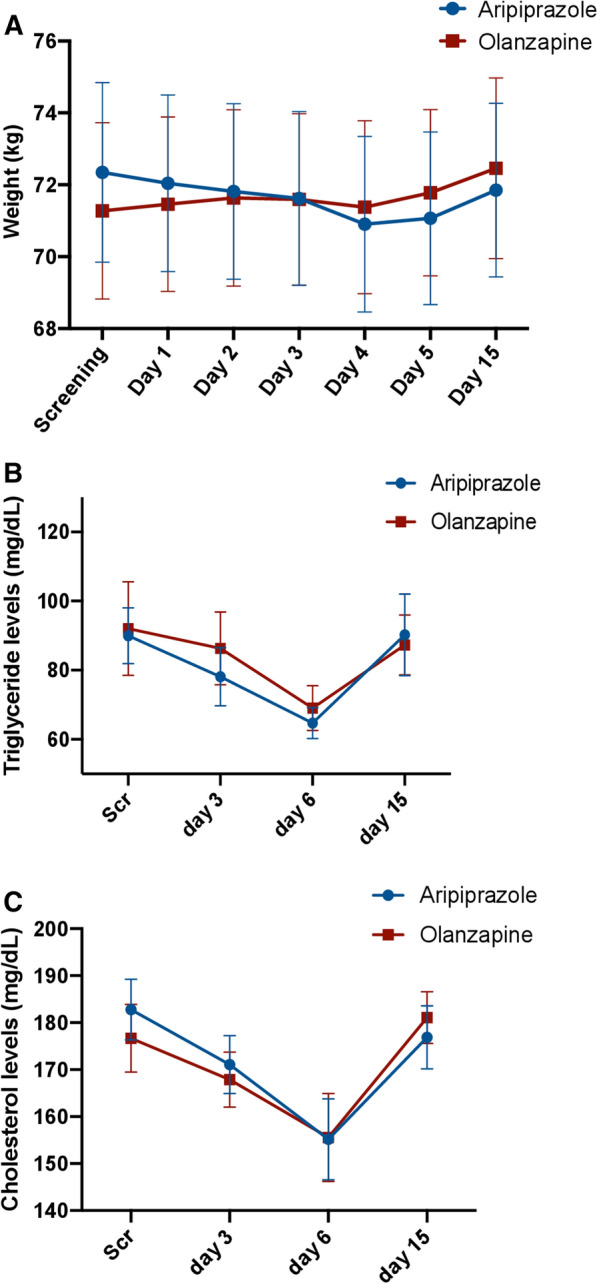
a Weight and b triglyceride and c cholesterol concentrations during the administration of a daily oral dose of aripiprazole 10 mg and olanzapine 5 mg tablets for 5 days. Values are shown as mean ± SD.
Triglyceride levels linearly decreased as a result of ARI and OLA administration (p = 0.009, ηp2 = 0.177; p = 0.047, ηp2 = 0.125, respectively) (Fig. 2). No significant difference was found in the extent of this decrease between ARI and OLA (p = 0.593). Additionally, ARI Cmax, DARI Cmax and ARI + DARI Cmax were inversely proportional to triglyceride levels (p = 0.003, ηp2 = 0.203; p < 0.001, ηp2 = 0.327; p < 0.001, ηp2 = 0.258, respectively). Moreover, CYP3A PMs had a significantly greater decrease in triglyceride levels during ARI treatment compared to the other phenotypes (p < 0.001, ηp2 = 0.296). Furthermore, APOC3 rs4520 C/C homozygotes had a lesser decrease in triglyceride concentrations after OLA administration than T allele carriers (p = 0.018, ηp2 = 0.162).
Likewise, total cholesterol levels diminished significantly during ARI and OLA treatment (p = 0.002, ηp2 = 0.250; p = 0.004, ηp2 = 0.209, respectively) (Fig. 2). No significant difference was found between ARI and OLA in the extent of this reduction (p = 0.241). Moreover, HTR2A rs6314 C/C subjects had higher cholesterol concentrations during ARI treatment compared to T allele carriers (p = 0.037, ηp2 = 0.141).
No differences were found between men and women in terms of changes of weight and triglyceride and cholesterol levels. No levels were outside of the normal range.
Hepatic Performance
GOT, GPT, GGT, ALP and albumin levels significantly decreased during ARI treatment (p = 0.001, ηp2 = 0.249; p = 0.004, ηp2 = 0.209; p = 0.001, ηp2 = 0.224; p < 0.001, ηp2 = 0.312; p < 0.001, ηp2 = 0.307, respectively) (Table S3). Additionally, GGT levels were inversely proportional to DARI and ARI + DARI Cmax (p = 0.050, ηp2 = 0.116; p = 0.043, ηp2 = 0.121). Likewise, ALP levels were dependent on ARI and ARI + DARI Cmax (p = 0.042, ηp2 = 0.121; p = 0.048, ηp2 = 0.117).
OLA treatment produced a decline in GGT, bilirubin, ALP and albumin levels (p < 0.001, ηp2 = 0.281; p = 0.045, ηp2 = 0.123; p = 0.007, ηp2 = 0.215; p = 0.004, ηp2 = 0.285, respectively). All GOT, GPT, GGT, bilirubin and ALP levels normalized after discontinuing ARI or OLA treatment (Table S3).
No differences were found between men and women in GOT, GPT, GGT, ALP, bilirubin and albumin levels. Additionally, the changes in albumin levels differed between ARI and OLA treatment (p = 0.009, ηp2 = 0.183). The changes in the rest of the parameters were not dependent on the treatment (ARI versus OLA). No levels were outside of the normal range.
Haematological Parameters
Platelet count significantly decreased during ARI treatment (p < 0.001, ηp2 = 0.361). Additionally, the prothrombin time increased and the prothrombin index decreased over time (p < 0.001, ηp2 = 0.360; p < 0.001, ηp2 = 0.410, respectively) (Table S4).
On the contrary, the leucocyte and platelet count decreased during OLA treatment (p = 0.004, ηp2 = 0.217; p = 0.007, ηp2 = 0.199, respectively). Similarly to ARI, the prothrombin index decreased over time (p = 0.006, ηp2 = 0.237) (Table S4).
No differences were found between men and women in leucocyte, platelet, haemoglobin, red blood cell and haematocrit count, and prothrombin time and index. No levels were outside of the normal range.
Thyroid Function
Free T4 levels significantly increased after ARI treatment (p = 0.035, ηp2 = 0.180). On the contrary, after OLA treatment, decreased levels were observed. However, this association did not reach significance (p = 0.230). Neither ARI nor OLA had a significant effect on TSH levels (Fig. 3). Nonetheless, a significant difference was found between ARI and OLA treatment in both free T4 and TSH levels (p = 0.010, ηp2 = 0.267; p = 0.022, ηp2 = 0.216). No differences were found between men and women in free T4 and TSH levels. No levels were outside of the normal range.
Fig. 3.
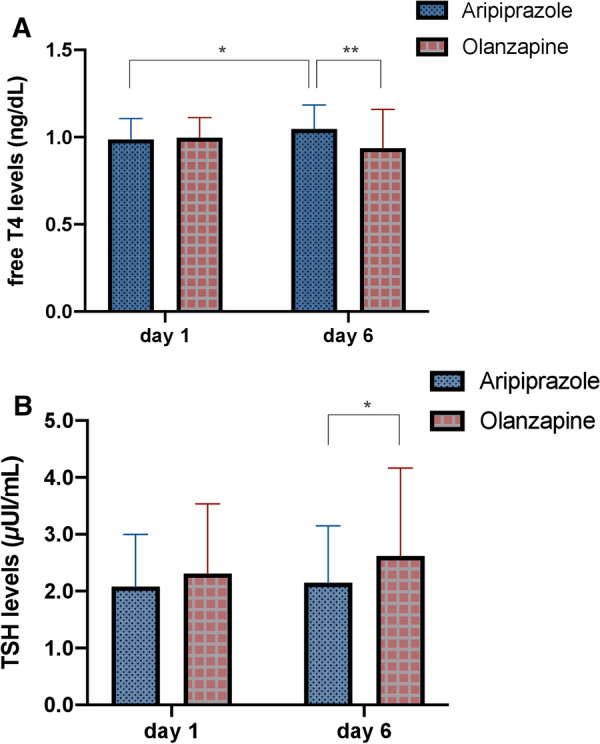
a Free T4 and b TSH concentrations after multiple dose administration of aripiprazole 10 mg and olanzapine 5 mg tablets. Values are shown as mean ± SD. *p < 0.05, **p < 0.01.
Renal Function
Uric acid levels significantly decreased during ARI and OLA treatment (p < 0.001, ηp2 = 0.324; p = 0.045, ηp2 = 0.116) (Table S5). No differences were found between men and women in urea, creatinine and uric acid levels. Additionally, the changes in their levels were not dependent on the treatment (ARI versus OLA). The uric acid levels were not outside of the normal range.
A summary of the effects of ARI and OLA on all metabolic parameters is shown in Table 3.
Table 3.
Effects of aripiprazole and olanzapine on all measured metabolic parameters
| Aripiprazole | Olanzapine | |
|---|---|---|
| Prolactin (ng/mL)* | ⇑ | |
| C-peptide (ng/mL) | ⇑ | ⇑ ns |
| Insulin (μU/mL) | ⇑ ns | ⇑ ns |
| C-peptide/insulin ratio | ⇑ | |
| HbA1c (%) | ||
| Glucose (ng/mL) | ||
| GTT (mg/dL)* | ⇑ ns | ⇑ |
| Weight (kg)* | ⇓ ns | ⇑ ns |
| Triglyceride (mg/dL) | ⇓ | ⇓ |
| Cholesterol (mg/dL) | ⇓ | ⇓ |
| GOT (U/L) | ⇓ | |
| GPT (U/L) | ⇓ | |
| GGT (U/L) | ⇓ | ⇓ |
| Total bilirubin (mg/dL) | ⇓ | |
| ALP (U/L) | ⇓ | ⇓ |
| Leucocytes (/µL (103)) | ⇓ ns | ⇓ |
| Platelets (/µL (103)) | ⇓ | ⇓ |
| Haemoglobin (mg/dL) | ⇓ ns | ⇓ ns |
| Red blood cells (/µL (106)) | ⇓ ns | ⇓ ns |
| Haematocrit (vol%) | ⇓ ns | ⇓ ns |
| Prothrombin time (s) | ⇑ | |
| Prothrombin index (%) | ⇓ | ⇓ |
| Albumin (g/dL)* | ⇓ | ⇓ |
| Free T4 (ng/dL)* | ⇑ | |
| TSH (µUI/mL)* | ⇑ ns | |
| Urea (mg/dL) | ||
| Creatinine (mg/dL) | ||
| Uric acid (mg/dL) | ⇓ | ⇓ |
HbA1c haemoglobin A1c, GTT glucose tolerance test, GOT glutamate-oxaloacetate transaminase, GPT glutamate-pyruvate transaminase, GGT gamma-glutamyl transferase, ALP alkaline phosphatase, free T4 free thyroxine, TSH thyroid stimulating hormone, ns non-significant
*P ≤ 0.05 aripiprazole compared to olanzapine
Discussion
The present study is the first to associate genetic polymorphisms with metabolic changes induced by ARI and OLA after 5 days of drug administration to healthy volunteers in a crossover design. Although metabolic side effects were reported in both patients and healthy volunteers, the same design was not followed previously [14, 28]. Furthermore, our study administered both drugs to all individuals; therefore, the presence of several confounding factors can be ruled out.
Hyperprolactinaemia is known to cause galactorrhoea, abnormal menstruation, infertility and osteoporosis in women. Likewise, it can cause galactorrhoea, impotence and infertility in men. Therefore, both sexes are affected and prolactin levels of patients taking SGAs, especially OLA, should be monitored frequently [29]. In the current study, OLA caused prolactin elevation instantly after administering the first dose. Hyperprolactinaemia is produced by DRD2 blockage. Therefore, it causes loss of the dopaminergic prolactin inhibitory factor in the lactotroph cells in the anterior pituitary. Hence, antipsychotics with a greater D2 occupation index produce significant prolactin elevation [30]. Our previous study revealed that prolactin levels significantly increase after administering a single dose of OLA [31]. Our current study confirms that five multiple doses of OLA treatment also cause prolactin elevation.
Prolactin levels decreased after changing the therapy from other SGAs—including OLA—to ARI [32]. Our previous study showed that a single dose of ARI mildly increases prolactin levels compared to the controls [13]. However, compared to OLA, no change was observed in prolactin levels after administration in the present study. Our study is the first to report a comparison between prolactin elevation induced by ARI and OLA in the same subjects. Therefore, the results can be considered reliable as intraindividual variability is avoided. Patients with schizophrenia usually receive several SGA agents before ARI and therefore they are almost never drug-naïve [32]. Our healthy subjects had not received any SGA medication previously; hence, no prior drug treatment could cause prolactin elevation. The current clinical practice recommends switching to ARI monotherapy in case of having high prolactin levels and if it does not appear to be normalized after 4 weeks of treatment, it should be discontinued [33].
Sex has a clear effect on prolactin concentrations, as was confirmed in several studies [12, 34]. Prolactin levels tend to be higher in women than in men [34]. Therefore, effects of ARI and OLA on prolactin secretion were analysed both jointly and separately.
HTR2C rs17326429 and rs3813929, COMT rs4680, DRD2 rs1800497, DRD3 rs6280 and ABCB1 rs1045642, rs1128503, rs2032582 and rs2235048 polymorphisms and CYP2D6 phenotypes were previously associated with prolactin levels after risperidone, quetiapine, clozapine, ARI or OLA treatment [10, 13, 35, 36]. We expected similar results as ARI is a partial agonist at DRD2 and at 5-HT1A receptors, and an antagonist at 5-HT2A receptors while OLA is an antagonist at DRD2 and at 5-HT2A and 5-HT2C receptors [37, 38]. In addition, ARI is metabolized by CYP2D6 and CYP3A4. However, ARI usually does not induce hyperprolactinaemia [6]; therefore, a clear difference in prolactin levels would not be expected among phenotype groups. However, CYP3A PM subjects had significantly higher prolactin concentrations compared to the other phenotypes during ARI treatment. These subjects were under prolonged ARI exposure which could cause mild prolactin increase. Regarding ABCB1, subjects with rs10280101, rs12720067 and rs11983225 A-C-T haplotype had higher prolactin concentrations compared to those carrying the mutated alleles. This confirms the hypothesis that ABCB1 polymorphisms and haplotypes might affect P-glycoprotein activity and therefore ARI brain availability and prolactin levels [36]. Regarding OLA, DRD3 rs6280 Ser/Ser subjects had lower prolactin levels compared to those carrying the Gly allele. Consequently, they may show higher DRD3 occupancy and thus dopamine can inhibit prolactin release [6]. Previous findings imply that DRD3 does not play a major role in OLA-induced prolactin secretion [39]. Nevertheless, we did not expect these results considering that none of the DRD2 polymorphisms affected prolactin levels. More studies are needed to resolve the ambiguity.
C-peptide levels were significantly higher after ARI treatment. However, these levels were not significantly different between ARI and OLA. Clozapine, OLA, risperidone and sulpiride were associated with an increase in C-peptide levels in patients with schizophrenia [40]. In our study, OLA tended to increase C-peptide levels without reaching statistical significance; however, the C-peptide/insulin ratio was higher after the 5 days of treatment. This ratio is an indirect index of hepatic insulin clearance [41]. The observed increase in the ratio may be due to the increase in hepatic insulin clearance and therefore decreased insulin secretion [42]. A similar study design used by Teff et al.—3 days of OLA treatment in healthy volunteers—found the contrary: a decrease was observed in the ratio which may imply an increase in insulin secretion [43]. In the latter study, ARI did not cause elevation in C-peptide levels [43]; this was the opposite result to ours. High C-peptide levels can imply insulin resistance and finally can lead to type 2 diabetes, atherosclerosis and metabolic syndrome. Thus, it may serve as a biomarker to identify the risk of developing these diseases [44].
COMT rs4680 G/G and rs1330678 T carriers had a higher increase in C-peptide levels after ARI treatment. COMT polymorphisms were previously associated with glycaemic function and type 2 diabetes, which can alter catecholamine production [45]. COMT rs4680 A carriers achieved a significantly lower change in C-peptide levels compared to subjects with G/G genotype, which is consistent with a previous study [46]. Thus, A may be the protective allele against changes in glucose metabolism. ARI and OLA seem to have an effect on C-peptide levels; however, more studies are needed both in patients and healthy volunteers to confirm these findings.
OLA is associated with glucoregulatory abnormalities. The 5-HT1 antagonism may decrease the responsiveness of the pancreatic beta cells, thus reducing the secretion of insulin and causing hyperglycaemia [47]. In our study, basal glucose levels did not change during acute treatment; however, the GTT performed after treatment showed higher 1 and 2 h glucose levels compared to the first day. These levels were significantly higher than during ARI treatment. Previous findings show the same association in patients undergoing chronic treatment and healthy volunteers with acute treatment [28, 48]. UGT1A1 rs887829 C/C homozygotes had higher basal glucose levels and also higher glucose levels in GTT after 1 h and 2 h on day 6 compared to the first day. OLA is metabolized predominantly by the UGT enzyme family, but clear evidence was found only for UGT1A4 [49]. On the basis of our results, T allele carriers may be under prolonged OLA exposure and therefore show higher glucose concentrations. This result is confirmed by our previous study as this polymorphism affected OLA pharmacokinetics [20].
ARI and OLA tended to increase insulin levels. In addition, BDNF rs6265 C/C subjects showed higher insulin levels compared to the other genotypes after ARI administration and in CYP3A PMs compared to the other phenotypes after OLA administration. In a previous study the BDNF rs6265 polymorphism did not affect insulin levels during chronic risperidone and OLA treatment [50]. To the best of our knowledge, our study is the first to report this relationship with ARI. C/C subjects may be more predisposed to develop high insulin levels and finally insulin resistance during ARI treatment.
It is not completely understood how SGAs cause weight gain, but 5-HT2C and 5-HT1A receptors, histamine H1 receptor and DRD2 presumably play a role [51]. However, OLA pharmacology is not the only factor to affect weight gain; diet and activity level may also play a role. Weight increases rapidly within the first 6 weeks of OLA treatment and patients continue to gain weight [52]. To the best of our knowledge, our study is the first to report OLA-related weight gain during only 5 days of treatment. ARI did not induce weight gain in the same volunteers, which strengthens our results as we can discard the effect of diet. HTR2C polymorphisms are clearly linked to susceptibility to gain weight with antipsychotics [53]. The HTR2C rs1414334 polymorphism was widely analysed and the C allele was associated with OLA-, clozapine- and risperidone-induced weight gain and metabolic syndrome [54], which we confirm in our study.
On the basis of current knowledge, OLA, but not ARI, increments triglyceride and cholesterol levels in chronic treatment [55]. Moreover, in a previous study, after three daily doses of OLA were administered to healthy volunteers, the cholesterol and the triglyceride levels were higher [28]. These results suggest that OLA may have acute adverse effects on lipid profiles as well. However, in our study, both triglyceride and cholesterol levels decreased during ARI and OLA treatment. The observed decrease could be due to the participants’ low carbohydrate diet during their stay [56]. It could explain why triglyceride and cholesterol levels recovered by the safety visit (10 days after discontinuing the treatment).
CYP3A PMs showed a greater decrease in triglyceride levels during ARI treatment compared to the other phenotypes. PMs could have a prolonged ARI exposure and therefore higher effect on the triglyceride levels as ARI is metabolized by CYP3A [5]. Furthermore, APOC3 rs4520 C/C homozygotes had higher triglyceride concentrations after OLA administration than T allele carriers, which is consistent with a previous study [57]. Polymorphisms in this gene influence serum or plasma triglyceride levels as the APOC3 protein raises plasma triglyceride levels by the inhibition of lipoprotein lipase, stimulates low-density lipoprotein secretion and intestinal triglyceride trafficking modulation [58]. The HTR2A rs6314 C/C homozygotes had greater cholesterol levels during ARI therapy. In a previous study the contrary was found: T carriers had higher cholesterol levels. However, Koreans have a lower frequency of HTR2A C allele (approximately 0.515) when compared to Caucasians; therefore, the frequency variation among different ethnic groups could cause this variation [59]. Our study is the first to report differences between HTR2A rs6314 alleles in cholesterol level changes during antipsychotic therapy.
In a previous study, ARI elevated transaminase levels (e.g. GOT and GPT) mildly, while OLA elevated them greatly [60]. The effects of ARI on GGT and ALP levels were not reported previously. However, OLA was reported to increase GGT, ALP and bilirubin levels [60]. To the best of our knowledge, our study is the first to report changes in hepatic enzyme and bilirubin levels during short-term antipsychotic treatment in healthy volunteers. In our study, GOT, GPT, GGT and ALP levels significantly decreased during ARI treatment while GGT, bilirubin and ALP levels significantly decreased during OLA treatment. The observed decrease could be explained by the participants’ low carbohydrate diet during their stay [56]. Additionally, the albumin levels also decreased during ARI and OLA treatment as with risperidone and clozapine, which suggests that these drugs have a negative impact on serum antioxidant protection [61]. In addition, none of these levels were outside of the reference range.
OLA may cause leukopenia [62], thrombocytopenia [63] and thromboembolism [64]. ARI only causes these conditions when co-administered with other CYP2D6 substrates [65]. Our study confirms that both antipsychotics cause significant decrease in platelet count and OLA additionally induces a decrease in leucocyte count. The current study is the first to report that these alterations start immediately after starting treatment, although none of these levels were outside of the reference range.
The free T4 levels significantly increased after ARI treatment. The ARI drug label states that it can induce both hypo- and hyperthyroidism. Nevertheless, the underlying mechanism is currently unknown [4]. In studies with quetiapine, only free T4 changes were detected, and not TSH [66], similar to our results. Additionally, compared to the ARI group, the OLA group had higher TSH and lower free T4 levels after treatment. OLA was associated with lower free T4 and higher TSH levels in patients compared to healthy controls in a previous study [67]. Our study is the first to report increase in free T4 levels after ARI treatment in healthy volunteers.
SGAs can increase the risk of developing chronic kidney diseases through the elevation of urea and creatinine levels [68, 69]. After the acute treatment with ARI and OLA we could not see this effect. Uric acid levels decreased during haloperidol [70], but not risperidone or clozapine treatment [61]. In the current study, we observed that both ARI and OLA reduced uric acid levels during treatment, but the levels were normalized after discontinuing the drugs. Uric acid is one of the principal antioxidants in human plasma and therefore its low levels may cause oxidative stress [61]. To the best of our knowledge, this is the first study to analyse uric acid alterations in acute ARI and OLA treatment.
Study Limitations
Our study should be repeated in healthy volunteers to increase the sample size as well as in patients with schizophrenia to demonstrate its clinical utility. Despite application of the Bonferroni post hoc test to each analysis, some of our results could be false positives due to the high number of analysed variables. Moreover, neither ARI nor OLA reached steady state during 5 days of treatment. Both could have had a greater effect on metabolism if they had reached steady state. However, the ethics committee would rarely authorize more than 5 days of treatment with antipsychotics in healthy volunteers. Nevertheless, we had very well controlled conditions which can reduce the influence of other factors, e.g. comorbidity, smoking and nutrition, and we administered both drugs to each volunteer.
Conclusions
OLA caused significant prolactin elevation, but ARI did not. CYP3A phenotype and ABCB1 and DRD3 genes affected prolactin levels. ARI caused C-peptide elevation and was dependent on COMT genotypes while the C-peptide/insulin ratio was higher after OLA treatment. Glucose levels in GTT were higher after five doses of OLA and were influenced by UGT1A1 genotypes. Insulin levels did not change but were dependent on BDNF genotypes and CYP3A phenotypes. ARI caused weight loss and OLA caused weight gain, and the latter was influenced by HTR2C alleles. Triglyceride and cholesterol levels decreased during ARI and OLA treatment, and varied on the basis of CYP3A phenotypes and APOC3 genotypes. Cholesterol levels were dependent on HTR2A genotypes. ARI induced an increase in free T4 levels. Both ARI and OLA reduced uric acid levels. In conclusion, both antipsychotics have significant metabolic effects in acute treatment. However, it seems that aripiprazole provokes less severe metabolic changes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful to the volunteers as well as the effort of the staff of the Clinical Trials Unit of Hospital de La Princesa, especially to Samuel Martín and Alejandro de Miguel-Cáceres for sample processing and to Daniel Romero-Palacián and María J. Hernández for safety evaluations.
Funding
The study and DK were financed by the H2020 Marie Sklodowska-Curie Innovative Training Network 721236 grant. MN is co-financed by “Consejería de Educación, Juventud y Deporte” PEJ-2018-TL/BMD-11080 grant from “Comunidad de Madrid” and “Fondo Social Europeo”. No Rapid Service Fee was received by the journal for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Wrote Manuscript: DK, MSR, PZ, SA, FAS; Designed Research: DK, FAS, MSR, GM, MR, DO; Performed Research: DK, MR, GM, FAS, MN; Analysed Data: DK, SA, ESM, EPS.
Prior Presentation
This was published previously as a preprint https://doi.org/10.1101/2020.07.29.226209.
Disclosures
FAS and DO have been consultants or investigators in clinical trials sponsored by the following pharmaceutical companies: Abbott, Alter, Aptatargets, Chemo, Cinfa, FAES, Farmalíder, Ferrer, Galenicum, GlaxoSmithKline, Gilead, Italfarmaco, Janssen-Cilag, Kern, Normon, Novartis, Servier, Silverpharma, Teva and Zambon. DK, MSR, PZ, SA, GM, MR, MN, ESM and EPS declare no conflict of interest. DK changed affiliation since the completion of the study to Department of Psychiatry, School of Medicine, Yale University, New Haven, Connecticut, USA.
Compliance with Ethics Guidelines
The protocol was approved by its research ethics committee (Comité Ético de Investigación Clínica (CEIC) of Hospital de La Princesa, registry number 3411) authorized by the Spanish Drugs Agency and the study was performed under the guidelines of Good Clinical Practice and the Declaration of Helsinki. All subjects signed the informed consent before inclusion and were free to withdraw from the study at any time.
Data Availability
All data generated or analysed during this study are included in this published article (and its supplementary material files). Clinical trial registry name, URL and registration number: TREATMENT-HV; EUDRA-CT 2018-000744-26; https://eudract.ema.europa.eu/.
References
- 1.Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114:169–179. doi: 10.1093/bmb/ldv017. [DOI] [PubMed] [Google Scholar]
- 2.Moore NA, Leander JD, Benvenga MJ, Gleason SD, Shannon H. Behavioral pharmacology of olanzapine: a novel antipsychotic drug. J Clin Psychiatry. 1997;58(Suppl 10):37–44. [PubMed] [Google Scholar]
- 3.Stip E, Tourjman V. Aripiprazole in schizophrenia and schizoaffective disorder: a review. Clin Ther. 2010;32(Suppl 1):S3–20. doi: 10.1016/j.clinthera.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Food and Drug Administration. ABILIFY (aripiprazole) label. Otsuka Pharmaceutical. http://www.https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021436s038,021713s030,021729s022,021866s023lbl.pdf. Accessed 1 Jul 2014.
- 5.Callaghan JT, Bergstrom RF, Ptak LR, Beasley CM. Olanzapine pharmacokinetic and pharmacodynamic profile. Clin Pharmacokinet. 1999;37:177–193. doi: 10.2165/00003088-199937030-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bargiota SI, Bonotis KS, Messinis IE, Angelopoulos NV. The effects of antipsychotics on prolactin levels and women’s menstruation. Schizophr Res Treat. 2013;2013:502697. doi: 10.1155/2013/502697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casey DE, Carson WH, Saha AR, et al. Switching patients to aripiprazole from other antipsychotic agents: a multicenter randomized study. Psychopharmacology. 2003;166:391–399. doi: 10.1007/s00213-002-1344-3. [DOI] [PubMed] [Google Scholar]
- 8.Hall TR, Harvey S, Chadwick A. Mechanism of serotonin effects on prolactin and growth hormone secretion in domestic fowl. Acta Endocrinol (Copenh) 1983;104:266–271. doi: 10.1530/acta.0.1040266. [DOI] [PubMed] [Google Scholar]
- 9.Di Sciascio G, Riva MA. Aripiprazole: from pharmacological profile to clinical use. Neuropsychiatr Dis Treat. 2015;11:2635–2647. doi: 10.2147/NDT.S88117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.López-Rodríguez R, Román M, Novalbos J, Pelegrina ML, Ochoa D, Abad-Santos F. DRD2 Taq1A polymorphism modulates prolactin secretion induced by atypical antipsychotics in healthy volunteers. J Clin Psychopharmacol. 2011;31:555–562. doi: 10.1097/JCP.0b013e31822cfff2. [DOI] [PubMed] [Google Scholar]
- 11.Miura I, Zhang J-P, Hagi K, et al. Variants in the DRD2 locus and antipsychotic-related prolactin levels: a meta-analysis. Psychoneuroendocrinology. 2016;72:1–10. doi: 10.1016/j.psyneuen.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagai G, Mihara K, Nakamura A, et al. Prolactin concentrations during aripiprazole treatment in relation to sex, plasma drugs concentrations and genetic polymorphisms of dopamine D2 receptor and cytochrome P450 2D6 in Japanese patients with schizophrenia: prolactin response to aripiprazole. Psychiatry Clin Neurosci. 2012;66:518–524. doi: 10.1111/j.1440-1819.2012.02391.x. [DOI] [PubMed] [Google Scholar]
- 13.Koller D, Belmonte C, Saiz-Rodríguez M, et al. Effects of aripiprazole on circadian prolactin secretion related to pharmacogenetics in healthy volunteers. Basic Clin Pharmacol Toxicol. 2020;126:236–246. doi: 10.1111/bcpt.13323. [DOI] [PubMed] [Google Scholar]
- 14.Kane JM, Osuntokun O, Kryzhanovskaya LA, et al. A 28-week, randomized, double-blind study of olanzapine versus aripiprazole in the treatment of schizophrenia. J Clin Psychiatry. 2009;70:572–581. doi: 10.4088/JCP.08m04421. [DOI] [PubMed] [Google Scholar]
- 15.Rummel-Kluge C, Komossa K, Schwarz S, et al. Head-to-head comparisons of metabolic side effects of second generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophr Res. 2010;123:225–233. doi: 10.1016/j.schres.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y, Liu Y, Su Y, et al. The metabolic side effects of 12 antipsychotic drugs used for the treatment of schizophrenia on glucose: a network meta-analysis. BMC Psychiatry. 2017;17:373. doi: 10.1186/s12888-017-1539-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Townsend LK, Peppler WT, Bush ND, Wright DC. Obesity exacerbates the acute metabolic side effects of olanzapine. Psychoneuroendocrinology. 2018;88:121–128. doi: 10.1016/j.psyneuen.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Kim J, Shin W. How to do random allocation (randomization) Clin Orthop Surg. 2014;6:103–109. doi: 10.4055/cios.2014.6.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koller D, Zubiaur P, Saiz-Rodríguez M, Abad-Santos F, Wojnicz A. Simultaneous determination of six antipsychotics, two of their metabolites and caffeine in human plasma by LC-MS/MS using a phospholipid-removal microelution-solid phase extraction method for sample preparation. Talanta. 2019;198:159–168. doi: 10.1016/j.talanta.2019.01.112. [DOI] [PubMed] [Google Scholar]
- 20.Koller D, Saiz-Rodríguez M, Zubiaur P, et al. The effects of aripiprazole and olanzapine on pupillary light reflex and its relationship with pharmacogenetics in a randomized multiple-dose trial. Br J Clin Pharmacol. 2020;86:2051–2062. doi: 10.1111/bcp.14300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Apellániz-Ruiz M, Inglada-Pérez L, Naranjo MEG, et al. High frequency and founder effect of the CYP3A4*20 loss-of-function allele in the Spanish population classifies CYP3A4 as a polymorphic enzyme. Pharmacogenomics J. 2015;15:288–292. doi: 10.1038/tpj.2014.67. [DOI] [PubMed] [Google Scholar]
- 22.Gaedigk A, Simon SD, Pearce RE, Bradford LD, Kennedy MJ, Leeder JS. The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther. 2008;83:234–242. doi: 10.1038/sj.clpt.6100406. [DOI] [PubMed] [Google Scholar]
- 23.Caudle KE, Dunnenberger HM, Freimuth RR, et al. Standardizing terms for clinical pharmacogenetic test results: consensus terms from the Clinical Pharmacogenetics Implementation Consortium (CPIC) Genet Med. 2017;19:215–223. doi: 10.1038/gim.2016.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanchez Spitman AB, Moes DJAR, Gelderblom H, Dezentje VO, Swen JJ, Guchelaar HJ. Effect of CYP3A4*22, CYP3A5*3, and CYP3A combined genotypes on tamoxifen metabolism. Eur J Clin Pharmacol. 2017;73:1589–1598. doi: 10.1007/s00228-017-2323-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saiz-Rodríguez M, Ochoa D, Belmonte C, et al. Polymorphisms in CYP1A2, CYP2C9 and ABCB1 affect agomelatine pharmacokinetics. J Psychopharmacol. 2019;33:522–531. doi: 10.1177/0269881119827959. [DOI] [PubMed] [Google Scholar]
- 26.Vivona D, Lima LT, Rodrigues AC, et al. ABCB1 haplotypes are associated with P-gp activity and affect a major molecular response in chronic myeloid leukemia patients treated with a standard dose of imatinib. Oncol Lett. 2014;7:1313–1319. doi: 10.3892/ol.2014.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Einarson TR, Hemels ME, Nuamah I, Gopal S, Coppola D, Hough D. An analysis of potentially prolactin-related adverse events and abnormal prolactin values in randomized clinical trials with paliperidone palmitate. Ann Pharmacother. 2012;46:1322–1330. doi: 10.1345/aph.1R123. [DOI] [PubMed] [Google Scholar]
- 28.Albaugh VL, Singareddy R, Mauger D, Lynch CJ. A double blind, placebo-controlled, randomized crossover study of the acute metabolic effects of olanzapine in healthy volunteers. PLoS One. 2011;6:e22662. doi: 10.1371/journal.pone.0022662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bushe C, Shaw M, Peveler RC. A review of the association between antipsychotic use and hyperprolactinaemia. J Psychopharmacol. 2008;22:46–55. doi: 10.1177/0269881107088435. [DOI] [PubMed] [Google Scholar]
- 30.Montejo ÁL, Arango C, Bernardo M, et al. Multidisciplinary consensus on the therapeutic recommendations for iatrogenic hyperprolactinemia secondary to antipsychotics. Front Neuroendocrinol. 2017;45:25–34. doi: 10.1016/j.yfrne.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Cabaleiro T, López-Rodríguez R, Ochoa D, Román M, Novalbos J, Abad-Santos F. Polymorphisms influencing olanzapine metabolism and adverse effects in healthy subjects. Hum Psychopharmacol. 2013;28:205–214. doi: 10.1002/hup.2308. [DOI] [PubMed] [Google Scholar]
- 32.Torre DL, Falorni A. Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag. 2007;3:929–951. [PMC free article] [PubMed] [Google Scholar]
- 33.Miyamoto BE, Galecki M, Francois D. Guidelines for antipsychotic-induced hyperprolactinemia. Psychiatr Ann. 2015;45:266–272. doi: 10.3928/00485713-20150501-09. [DOI] [Google Scholar]
- 34.Yamaji T, Shimamoto K, Ishibashi M, Kosaka K, Orimo H. Effect of age and sex on circulating and pituitary prolactin levels in human. Acta Endocrinol (Copenh) 1976;83:711–719. doi: 10.1530/acta.0.0830711. [DOI] [PubMed] [Google Scholar]
- 35.Yoshida K, Müller DJ. Pharmacogenetics of antipsychotic drug treatment: update and clinical implications. Mol Neuropsychiatry. 2018;5(Suppl 1):1–26. 10.1159/000492332. [DOI] [PMC free article] [PubMed]
- 36.Hattori S, Suda A, Kishida I, et al. Effects of ABCB1 gene polymorphisms on autonomic nervous system activity during atypical antipsychotic treatment in schizophrenia. BMC Psychiatry. 2018;18:231. doi: 10.1186/s12888-018-1817-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conley RR, Kelly DL. Second-generation antipsychotics for schizophrenia: a review of clinical pharmacology and medication-associated side effects. Isr J Psychiatry Relat Sci. 2005;42:51–60. [PubMed] [Google Scholar]
- 38.Kern RS, Green MF, Cornblatt BA, et al. The neurocognitive effects of aripiprazole: an open-label comparison with olanzapine. Psychopharmacology. 2006;187:312–320. doi: 10.1007/s00213-006-0428-x. [DOI] [PubMed] [Google Scholar]
- 39.López-Rodríguez R, Román M, Novalbos J, Pelegrina ML, Ochoa D, Abad-Santos F. DRD2 Taq1A polymorphism modulates prolactin secretion induced by atypical antipsychotics in healthy volunteers. J Clin Psychopharmacol. 2011;31:555–562. doi: 10.1097/JCP.0b013e31822cfff2. [DOI] [PubMed] [Google Scholar]
- 40.Wu R-R, Zhao J-P, Liu Z-N, et al. Effects of typical and atypical antipsychotics on glucose-insulin homeostasis and lipid metabolism in first-episode schizophrenia. Psychopharmacology. 2006;186:572–578. doi: 10.1007/s00213-006-0384-5. [DOI] [PubMed] [Google Scholar]
- 41.Polonsky KS, Rubenstein AH. C-peptide as a measure of the secretion and hepatic extraction of insulin: pitfalls and limitations. Diabetes. 1984;33:486–494. doi: 10.2337/diab.33.5.486. [DOI] [PubMed] [Google Scholar]
- 42.Najjar SM, Perdomo G. Hepatic insulin clearance: mechanism and physiology. Physiology (Bethesda) 2019;34:198–215. doi: 10.1152/physiol.00048.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teff KL, Rickels MR, Grudziak J, Fuller C, Nguyen H-L, Rickels K. Antipsychotic-induced insulin resistance and postprandial hormonal dysregulation independent of weight gain or psychiatric disease. Diabetes. 2013;62:3232–3240. doi: 10.2337/db13-0430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khan HA, Sobki SH, Ekhzaimy A, Khan I, Almusawi MA. Biomarker potential of C-peptide for screening of insulin resistance in diabetic and non-diabetic individuals. Saudi J Biol Sci. 2018;25:1729–1732. doi: 10.1016/j.sjbs.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marco GSD, Colucci JA, Fernandes FB, Vio CP, Schor N, Casarini DE. Diabetes induces changes of catecholamines in primary mesangial cells. Int J Biochem Cell Biol. 2008;40:747–754. doi: 10.1016/j.biocel.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 46.Bozek T, Blazekovic A, Perkovic MN, et al. The influence of dopamine-beta-hydroxylase and catechol O-methyltransferase gene polymorphism on the efficacy of insulin detemir therapy in patients with type 2 diabetes mellitus. Diabetol Metab Syndr. 2017;9:97. doi: 10.1186/s13098-017-0295-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bettinger TL, Mendelson SC, Dorson PG, Crismon ML. Olanzapine-induced glucose dysregulation. Ann Pharmacother. 2000;34:865–867. doi: 10.1345/aph.19327. [DOI] [PubMed] [Google Scholar]
- 48.Haupt DW, Fahnestock PA, Flavin KA, et al. Adiposity and insulin sensitivity derived from intravenous glucose tolerance tests in antipsychotic-treated patients. Neuropsychopharmacology. 2007;32:2561–2569. doi: 10.1038/sj.npp.1301392. [DOI] [PubMed] [Google Scholar]
- 49.Linnet K. Glucuronidation of olanzapine by cDNA-expressed human UDP-glucuronosyltransferases and human liver microsomes. Hum Psychopharmacol Clin Exp. 2002;17:233–238. doi: 10.1002/hup.403. [DOI] [PubMed] [Google Scholar]
- 50.Bonaccorso S, Sodhi M, Li J, et al. The brain-derived neurotrophic factor (BDNF) Val66Met polymorphism is associated with increased body mass index and insulin resistance measures in bipolar disorder and schizophrenia. Bipolar Disord. 2015;17:528–535. doi: 10.1111/bdi.12294. [DOI] [PubMed] [Google Scholar]
- 51.Reynolds GP, Hill MJ, Kirk SL. The 5-HT2C receptor and antipsychoticinduced weight gain—mechanisms and genetics. J Psychopharmacol. 2006;20:15–18. doi: 10.1177/1359786806066040. [DOI] [PubMed] [Google Scholar]
- 52.Dayabandara M, Hanwella R, Ratnatunga S, Seneviratne S, Suraweera C, de Silva VA. Antipsychotic-associated weight gain: management strategies and impact on treatment adherence. Neuropsychiatr Dis Treat. 2017;13:2231–2241. doi: 10.2147/NDT.S113099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wallace TJ, Zai CC, Brandl EJ, Müller DJ. Role of 5-HT(2C) receptor gene variants in antipsychotic-induced weight gain. Pharmacogenomics Pers Med. 2011;4:83–93. doi: 10.2147/PGPM.S11866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ma X, Maimaitirexiati T, Zhang R, et al. HTR2C polymorphisms, olanzapine-induced weight gain and antipsychotic-induced metabolic syndrome in schizophrenia patients: a meta-analysis. Int J Psychiatry Clin Pract. 2014;18:229–242. doi: 10.3109/13651501.2014.957705. [DOI] [PubMed] [Google Scholar]
- 55.Olfson M, Marcus SC, Corey-Lisle P, Tuomari AV, Hines P, L’Italien GJ. Hyperlipidemia following treatment with antipsychotic medications. Am J Psychiatry. 2006;163:1821–1825. doi: 10.1176/ajp.2006.163.10.1821. [DOI] [PubMed] [Google Scholar]
- 56.Purkins L, Love ER, Eve MD, et al. The influence of diet upon liver function tests and serum lipids in healthy male volunteers resident in a phase I unit: effect of diet upon liver function tests and serum lipids. Br J Clin Pharmacol. 2003;57:199–208. doi: 10.1046/j.1365-2125.2003.01969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith RC, Segman RH, Golcer-Dubner T, Pavlov V, Lerer B. Allelic variation in ApoC3, ApoA5 and LPL genes and first and second generation antipsychotic effects on serum lipids in patients with schizophrenia. Pharmacogenomics J. 2008;8:228–236. doi: 10.1038/sj.tpj.6500474. [DOI] [PubMed] [Google Scholar]
- 58.Kohan AB. Apolipoprotein C-III: a potent modulator of hypertriglyceridemia and cardiovascular disease. Curr Opin Endocrinol Diabetes Obes. 2015;22:119–125. doi: 10.1097/MED.0000000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choi J-H, Zhang S-Y, Park K-W, et al. The association between the T102C polymorphism of the HTR2A serotonin receptor gene and HDL cholesterol level in Koreans. BMB Rep. 2005;38:238–242. doi: 10.5483/BMBRep.2005.38.2.238. [DOI] [PubMed] [Google Scholar]
- 60.Marwick KFM, Taylor M, Walker SW. Antipsychotics and abnormal liver function tests: systematic review. Clin Neuropharmacol. 2012;35:244–253. doi: 10.1097/WNF.0b013e31826818b6. [DOI] [PubMed] [Google Scholar]
- 61.Gilca M, Piriu G, Gaman L, et al. A study of antioxidant activity in patients with schizophrenia taking atypical antipsychotics. Psychopharmacology. 2014;231:4703–4710. doi: 10.1007/s00213-014-3624-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Buchman N, Strous RD, Ulman A-M, Lerner M, Kotler M. Olanzapine-induced leukopenia with human leukocyte antigen profiling. Int Clin Psychopharmacol. 2001;16:55–57. doi: 10.1097/00004850-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Malik YK, Sahoo S, Avasthi A. Olanzapine-induced leucopaenia and thrombocytopaenia in an elderly patient: a case report and review of the evidence. Gen Psychiatry. 2018;31:e000013. doi: 10.1136/gpsych-2018-000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hägg S, Tätting P, Spigset O. Olanzapine and venous thromboembolism. Int Clin Psychopharmacol. 2003;18:299–300. doi: 10.1097/01.yic.0000085241.99018.30. [DOI] [PubMed] [Google Scholar]
- 65.Mendhekar D, Duggal H, Andrade C. Leukopenia and thrombocytopenia on adding aripiprazole to phenytoin. World J Biol Psychiatry. 2009;10:1043–1044. doi: 10.1080/15622970802032292. [DOI] [PubMed] [Google Scholar]
- 66.Lambert CG, Mazurie AJ, Lauve NR, et al. Hypothyroidism risk compared among nine common bipolar disorder therapies in a large US cohort. Bipolar Disord. 2016;18:247–260. doi: 10.1111/bdi.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Iversen T, Steen NE, Birkeland KI, et al. T229. Antipsychotic drug use and thyroid function in patients with severe mental disorders. Schizophr Bull. 2018;44:S205–S206. doi: 10.1093/schbul/sby016.505. [DOI] [Google Scholar]
- 68.Lozano Ortiz R. Influence of drug treatment with antidepressants and antipsychotics on plasma urea levels. Neuropsychiatr Dis Treat. 2012;8:245–6. [DOI] [PMC free article] [PubMed]
- 69.Wang H-Y, Huang CL-C, Feng IJ, Tsuang H-C. Second-generation antipsychotic medications and risk of chronic kidney disease in schizophrenia: population-based nested case-control study. BMJ Open. 2018;8:e019868. doi: 10.1136/bmjopen-2017-019868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yao JK, Reddy R, van Kammen DP. Reduced level of plasma antioxidant uric acid in schizophrenia. Psychiatry Res. 1998;80:29–39. doi: 10.1016/S0165-1781(98)00051-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its supplementary material files). Clinical trial registry name, URL and registration number: TREATMENT-HV; EUDRA-CT 2018-000744-26; https://eudract.ema.europa.eu/.




