Abstract
Background
Knowledge of women's experience of childbirth in the outbreak of the coronavirus (COVID-19) pandemic and associated maternal health outcomes is scarce.
Methods
A sample of primarily American women who gave birth around the height of COVID-19 (n = 1,611) and matched controls, i.e., women who gave birth before COVID-19 (n = 640), completed an anonymous Internet survey about recent childbirth, birth-related traumatic stress (peritraumatic distress inventory; PTSD-checklist), maternal bonding (maternal attachment inventory; mother-to-infant bonding scale) and breastfeeding status. Groups (n = 637 in each) were matched on demographics, prior mental health/trauma and childbirth factors to determine the unique contribution of COVID-19 to the psychological experience of childbirth.
Results
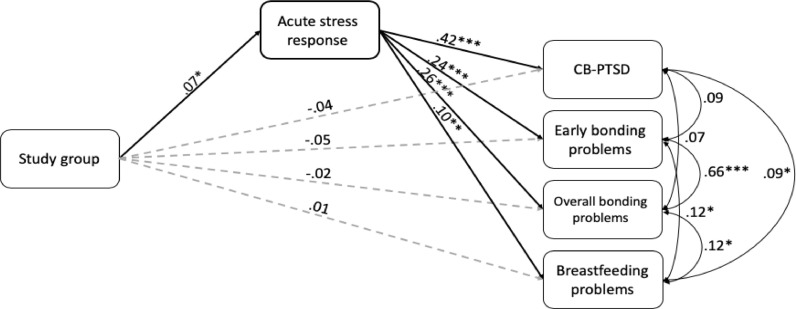
Mothers in COVID-19-exposed communities endorsed more clinically acute stress response to childbirth than matched controls (Z = 2.65, p = .008, OR= 1.38). A path mediation model revealed that acute stress mediated the relationship between study group and postpartum outcomes. Specifically, higher acute stress response in birth was associated with more childbirth-related posttraumatic stress disorder symptoms (β = .42, p < .001) and less bonding with the infant (β = .26, p < .001), including breastfeeding problems (β = .10, p < .01).
Limitations
Use of a convenient internet sample introduces bias towards more educated women and reliance on retrospective self-report assessments may entail recall bias.
Conclusions
COVID-19 is a major stressor for delivering women. It can heighten traumatic childbirth experiences and interfere with successful postpartum adjustment. Clinical attention to traumatic stress in childbirth and problems with caring for the young during this pandemic is important.
Keywords: Traumatic childbirth, Posttraumatic stress disorder, Postpartum, Coronavirus (COVID-19) pandemic, Maternal bonding, Breastfeeding
The known physical and mental health toll of the novel 2019 Coronavirus (COVID-19) pandemic is already vast (Pfefferbaum and North, 2020). As researchers consider the potential long-term, generational impacts of this global and ongoing stressor on communities, it is critical to examine its impact on postpartum women. New mothers must now cope with not only the known stressors of the postpartum period but also the burden of the pandemic during a critical time of care for their children (Dekel et al., 2019). Not surprisingly, elevated depression and anxiety symptoms have been documented in postpartum women since the outbreak of COVID-19 (Cameron et al., 2020; Davenport et al., 2020; Davis-Floyd et al., 2020).
One factor to consider in discussing maternal mental health outcomes is the impact of the pandemic on women's experiences of childbirth. As the pandemic spread, hospitals deferred non-urgent care in many cases, leaving patients with COVID-19, Intensive Care Unit (ICU) patients, and women giving birth as the main populations receiving hospital care. Women being admitted for childbirth were one of the only healthy populations to be treated in medical settings as drastic changes were made in visitor and other polices to stem the spread of the virus, including leaving patients without a support person during critical decisions and life events (Ecker and Minkoff, 2020).
The notion that childbirth can be traumatic for as much as a third of women and result in acute stress response surrounding cildbirth has been documented in pre-COVID-19 samples (Ayers et al., 2016; Dekel et al., 2017). These initial traumatic symptoms are strong markers of full-blown childbirth-related posttraumatic stress (CB-PTSD), which is the more chronic manifestation of trauma and has an expected prevlance of 6 to 19% (Dekel et al., 2017). The association between maternal traumatic stress and problems with bonding with the infant and breastfeeding failure, has also been noted (Chan et al., 2020; Dekel et al., 2019). However, the unique added adversities of COVID-19 on childbirth-evoked maternal traumatic stress and subsequent maternal morbidity remain unknown.
We studied a large sample of women who gave birth during the first peaks of COVID-19 and compared them to women who gave birth before the pandemic. We asked whether COVID-19 is associated with stressful childbirth and whether acute stress in birth mediates the association between COVID-19ʼs presence in communities and enduring posttraumatic stress and maternal bonding problems.
1. Methods
1.1. Participants
This study commenced on April 2nd, 2020, during the outbreak of COVID-19 in the US. Women who gave birth to a live baby within the past 6 months were recruited via social media, professional organizations, and hospital announcements. They were asked to complete an anonymous survey concerning their recent childbirth, mental health, and related factors. Partners (Mass General) Human Research Committee granted exemption for this study.
The COVID-19 outbreak was declared a global pandemic by the World Health Organization on March 11, 2020 (Cucinotta and Vanelli, 2020). The sample comprised of 1611 women who gave birth since COVID-19 outbreak in their communities (primarily March and April 2020) and an additional 640 women who gave birth before the pandemic (on average earlier in 2020). We included women who provided the childbirth date and responded “no” to suspected/confirmed COVID-19, thereby excluding women positive for COVID-19. The final sample following the group-matching procedure was 637 women, the majority giving birth during the initial outbreak of COVID-19 and an additional 637 who gave birth before a COVID-19 outbreak in their communities. Participants were on average two months postpartum and 32 years old, married (91%), at least middle class (60%), employed (77%), and had a college degree (79%). The majority resided in the US (86%) (the most represented states were Massachusetts, California, Texas, and New York), and the rest of the sample resided in Oceania (5%), Europe (4%), Central/South America (1%) and less than 1% in Asia, the Caribbean, Africa, and the Middle East. The majority (85%) delivered a healthy baby at-term and had a vaginal delivery (72%). Close to two-thirds (59%) were primiparas.
1.2. Measures
Acute stress response to childbirth was assessed with the commonly used Peritraumatic Distress Inventory (PDI) (Brunet et al., 2001). It is a 13-item self-report with good psychometric properties assessing negative emotional response during or immediately after a specified trauma. We used the suggested clinical cutoff of 17 to define clinically significant acute stress response (Nishi et al., 2010) (α was .86).
Posttraumatic stress disorder related to recent childbirth (CB-PTSD) symptoms were measured with the Posttraumatic Checklist for DSM-5 (PCL-5). The PCL-5 has 20 items in accordance with the DSM-5 PTSD symptoms and is the most commonly used symptom severity. The PCL-5 has strong correspondence with clinician assessments (Bovin et al., 2016) (α was .90). Prior life time exposure to traumatic events (experienced or witnessed) was assessed with the Life Events Checklist for DSM-5 (LEC-5) (Weathers et al., 2013) (α was .93).
Maternal bonding problems were assessed with the Mother-to-Infant Bonding Scale (MIBS) (Taylor et al., 2005) and the Maternal Attachment Inventory (MAI) (Müller, 1994). The MIBS is an 8-item to measure feelings towards the infant in the first postpartum days and weeks following childbirth. The MAI is a 26-item assessing maternal perception and feelings and is a robust tool to measure problems in mother-infant relationship (Perrelli et al., 2014). Both measures show good correspondence with observational assessments (Müller, 1994; Taylor et al., 2005) (α was .78 and .93, for MIBS and MAI, respectively). Additionally, breastfeeding habits were assessed by a single item (exclusive breastfeeding, partial breastfeeding, currently not but in past, breastfeeding never offered).
Socio-demographics, mental health and childbirth history, and recent childbirth information (i.e., gestational age and mode of delivery) were collected using single item self-report by the participants. Due to the anonymous internet survey methodology, medical records were not available for review.
2. Results
Matched COVID-19 (i.e., women giving birth during the pandemic) and non-COVID-19 (i.e., women giving birth before the pandemic) groups on similar background characteristics (e.g., maternal age, marital status, employment, education, ethnicity, trauma and mental health history, prior birth stressors, primiparity, delivery mode, gestational age, and weeks postpartum) were created using a propensity score matching procedure with SPSS PS module (Thoemmes, 2012) with estimiation algorithm as logistic regresstion and the matching algorithm as the nearest matching with caplier of 0.2. An overall balance test (Hansen and Bowers, 2008) indicated that the balance of the matching groups was high, χ2 (45) = 29.95, p = .96.
Kolmogorov-Smirnov and Shapiro-Wilk tests revealed that the acute stress responses to childbirth (PDI scores) were significantly positively skewed (p < .001). To estimate differences between COVID-19 and non-COVID-19 groups in acute stress response to childbirth Mann-Whitney U test was performed. The test showed that women delivering during COVID-19 had significantly higher stress response to childbirth; (M rank = 582.19) than matched controls (M rank = 531.21), Z = 2.65, p = .008, r = .07, 95% CI = .02, .13 (CI are based on bootstrapping of 1000 resampling cycles). Odds ratio analysis indicated higher prevalence of clinically significant acute stress level in the COVID-19 group in comparison to controls (OR = 1.38, 95% CI = 1.01–1.89).
To examine whether acute stress response to childbirth mediated the effects of study groups on CB-PTSD, bonding, and breastfeeding problems, we estimated a multi-path mediation model using observed measures in Structural Equation Modeling (SEM) and a saturated model. Significance was estimated by bias-corrected bootstrap analysis with 5000 sampling cycles. Missing data were handled with the Full Information Maximum Likelihood (FIML) procedure. The study group (0 = before COVID-19, 1 = since COVID-19) served as the predictor, acute stress response as the mediator, and CB-PTSD symptoms, maternal bonding and breastfeeding problems as the outcome measures.
Results of the mediation model are depicted in Fig. 1 . Tolerance scores of all measures ranged between .49–.96 indicating no multicollinearity between measures. The model revealed that acute stress response to childbirth significantly mediated the paths between study group and CB-PTSD, maternal bonding, and breastfeeding [bias-corrected 95% confidence interval, (95% CIBC) .003, .03 for CB-PTSD symptoms .08, .56 for initial maternal bonding problems, .03, .22 for general bonding problems, and .003, .03 for breastfeeding problems]. The COVID-19 group had higher acute stress response to childbirth; higher acute stress response in turn was associated with more CB-PTSD symptoms (β = .42, p < .001) and more problems with maternal bonding (β = .24, p < .001; β = .26, p < .001) and breastfeeding (β = .10, p < .01).
Fig. 1.
Multi-path mediation model linking study group to childbirth-related PTSD (CB-PTSD) symptoms, maternal bonding and breastfeeding via acute stress response to childbirth. Solid lines represent significant paths; gray dashed lines represent non-significant paths. Values are standardized scores. To figure legend: ***p<.001, **p<.01, *p<.05.
3. Discussion
This study provides new insights regarding the psychological impact of COVID-19 on postpartum women from traumatic stress and maternal attachment perspectives. We found that when comparing women who are similar on various important background information such as demographics, prior trauma history, and even delivery mode and gestational age, women who gave birth when COVID-19 was prevalent in their communities, with the majority giving birth in the heights of the pandemic had more clinically significant acute stress responses to childbirth than women who gave birth in communities not experiencing COVID-19. Moreover, having a stress response to childbirth via COVID-19 presence in the mother's community was in turn associated with posttraumatic stress symptoms and problems with bonding and breastfeeding of the infant in the very early postpartum period. These conditions may result in enduring mental health morbidity in the mother and undermine child development.
Our findings shift attention to the adverse effect of traumatic childbirth experiences on maternal postpartum adjustment in women giving birth during the recent pandemic. The increase acute stress response to childbirth, as noted here, was evident in healthy women who did not carry the novel coronavirus. It has been shown that the subjective acute emotional response to a traumatic event is more important than the magnitude of the objective stressor in determining successful post-trauma coping or the manifestation of PTSD (Chan et al., 2020; Ozer et al., 2003). Factors such as fear of virus exposure of mother or newborn during hospital stay, sense of reduced social support surrounding childbirth when giving birth during visitor restrictions, and discrepancy between pre-pandemic birth expectations and the actual experience of giving birth during the pandemic may have all contributed to a stressful childbirth in COVID-19. Taken as a whole, the pandemic may involve a more stressful climate in labor and delivery than during normalcy.
Childbirth offers a unique opportunity to screen women for acute stress following childbirth because the event is predictable, and women stay in the hospital following birth. Immediate screening for traumatic stress is almost impossible in other forms of trauma. Although depressive reactions are routinely assessed during peripartum obstetric care, currently there are no screenings for acute stress in postpartum units. It could be important to expand mental health screening in hospitals and birthing centers during the pandemic to identify women early on who are at high risk for negative mental health outcomes. Premature weaning of breastfeeding may also lead to worse long-term health outcomes for women and children; enhancing breastfeeding support is called for during the pandemic in vulnerable dyads.
Shortcomings of this study include a cross-sectional design, a internet-based sample, and the use of self-reports which could be influenced by memory effects. The employment of a within-sample group comparison may in part overcome these limitations. We did not include clinician assessment of maternal stress or maternal attachment impairment. The chosen stress measures are commonly used and well validated in trauma survivors and accord with clinician assessments (Brunet et al., 2001; Weathers et al., 1993) and the maternal attachment measures correspond with observational assessments (Taylor et al., 2005). Future prospective studies can provide more insight by examining the underlying factors contributing to stressful childbirth during the pandemic among COVID-19 positive and negative women.
In summary, our findings indicate that the novel coronavirus pandemic adds a significant amount of stress to childbirth. This additional childbirth-related stress may in turn interfere with successful maternal postpartum adjustment with potential long-term health consequences for mother and child. Attention to the special needs of delivering women is warranted to reduce stress surrounding childbirth and improve peripartum care during an international health crisis.
Declaration of Competing Interest
Gus Mayopoulos, Tsachi Ein-Dor PhD, Gabriella Dishy, Rasvitha Nandru, Sabrina Chan, Lauren Hanley, MD, Anjali Kaimal MD, and Sharon Dekel PhD declare that they have no conflict of interest.
Acknowledgments
Contributors
Gus Mayopoulos: Contributed significantly to the writing of the manuscript. Tsachi Ein-Dor: PhD. Took the lead in developing and performing the statistical analysis model, and wrote the results. Gabriella Dishy: Assisted in developing the internet study survey. Rasvitha Nandru: Contributed to recruitment activities. Sabrina Chan: Contributed to the manuscript preparation and recruitment activities. Lauren Hanley, MD: Assisted with manuscript development including the breastfeeding measurement in the model and manuscript revisions. Anjali Kaimal, MD: Contributed to the manuscript preparation and the final editing. Sharon Dekel, PhD: Is the principal investigator of the study. She developed the study conceptualization and the study survey and supervised the manuscript writing and preparation. All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript.
Role of funding source
Dr. Dekel was supported by a grant from the National Institute of Child Health and Human Development (R21HD100817) and an award (ISF) from the MGH Executive Committee on Research.
References
- Ayers S., Bond R., Bertullies S., Wijma K. The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol. Med. 2016;46:1121–1134. doi: 10.1017/S0033291715002706. [DOI] [PubMed] [Google Scholar]
- Bovin M.J., Marx B.P., Weathers F.W., Gallagher M.W., Rodriguez P., Schnurr P.P., Keane T.M. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. J. Psychol. Assess. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Brunet A., Weiss D.S., Metzler T.J., Best S.R., Neylan T.C., Rogers C., Fagan J., Marmar C.R. The peritraumatic distress inventory: a proposed measure of PTSD criterion A2. Am. J. Psychiatry. 2001;158:1480–1485. doi: 10.1176/appi.ajp.158.9.1480. [DOI] [PubMed] [Google Scholar]
- Cameron E., Joyce K., Delaquis C., Reynolds K., Protudjer J., Roos L.E. Maternal psychological distress & mental health services use during the COVID-19 pandemic. J. Affect Disord. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S., Ein-Dor T., Mayopoulos P., Mesa M., Sunda R., McCarthy B., Kaimal A., Dekel S. Risk factors for developing posttraumatic stress disorder following childbirth. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113090. [DOI] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta bio-Medica. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davenport M.H., Meyer S., Meah V.L., Strynadka M.C., Khurana R. Moms are not ok: COVID-19 and maternal mental health. Front. Global Women’s Health. 2020;1:1. doi: 10.3389/fgwh.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis-Floyd R., Gutschow K., Schwartz D.A. Pregnancy, Birth and the COVID-19 Pandemic in the United States. Med. Anthropol. 2020:1–15. doi: 10.1080/01459740.2020.1761804. [DOI] [PubMed] [Google Scholar]
- Dekel S., Stuebe C.M., Dishy G.A. Childbirth induced posttraumatic stress syndrome: A systematic review of prevalence and risk factors. Front Psychol. 2017;8:560. doi: 10.3389/fpsyg.2017.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel S., Thiel F., Dishy G., Ashenfarb A.L. Is childbirth-induced PTSD associated with low maternal attachment? Arch. Womens Ment. Health. 2019;22:119–122. doi: 10.1007/s00737-018-0853-y. [DOI] [PubMed] [Google Scholar]
- Ecker J.L., Minkoff H.L. Laboring alone? Brief thoughts on ethics and practical answers during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. MFM. 2020;2 doi: 10.1016/j.ajogmf.2020.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen B.B., Bowers J. Covariate balance in simple, stratified and clustered comparative studies. Stat. Sci. 2008;23:219–236. [Google Scholar]
- Müller M.E. A questionnaire to measure mother-to-infant attachment. J. Nurs. Meas. 1994;2:129–141. [PubMed] [Google Scholar]
- Nishi D., Matsuoka Y., Yonemoto N., Noguchi H., Kim Y., Kanba S. Peritraumatic distress inventory as a predictor of post-traumatic stress disorder after a severe motor vehicle accident. Psychiatry Clin. Neurosci. 2010;64:149–156. doi: 10.1111/j.1440-1819.2010.02065.x. [DOI] [PubMed] [Google Scholar]
- Ozer E.J., Best S.R., Lipsey T.L., Weiss D.S. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol. Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Perrelli J.G.A., Zambaldi C.F., Cantilino A., Sougey E.B. Mother-child bonding assessment tools. Revista Paulista de Pediatria. 2014;32:257–265. doi: 10.1590/0103-0582201432318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. New Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Taylor A., Atkins R., Kumar R., Adams D., Glover V. A new Mother-to-Infant Bonding Scale: links with early maternal mood. Arch. Women’s Mental Health. 2005;8:45–51. doi: 10.1007/s00737-005-0074-z. [DOI] [PubMed] [Google Scholar]
- Thoemmes F. arXiv preprint; 2012. Propensity Score Matching in SPSS. arXiv:1201.6385. [Google Scholar]
- Weathers F.W., Litz B.T., Herman D.S., Huska J.A., Keane T.M. Annual Convention of the International Society For Traumatic Stress Studies, San Antonio, TX. San Antonio, TX; 1993. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. [Google Scholar]
- Weathers F.W., Blake D.D., Schnurr P.P., Kaloupek D.G., Marx B.P., Keane T.M. Instrument available from the National Center for PTSD at www.ptsd.va.gov. 2013. The life events checklist for DSM-5 (LEC-5) [Google Scholar]