Abstract
Objective:
Evaluate racial/ethnic differences in maternal resilience and its associations with low birthweight (LBW).
Study Design:
Retrospective cohort study of 3244 women surveyed in the Longitudinal Study of Adolescent to Adult Health. The Add Health Resilience Instrument assessed resilience. Logistic regression models explored associations between women’s resilience and risk of LBW.
Result:
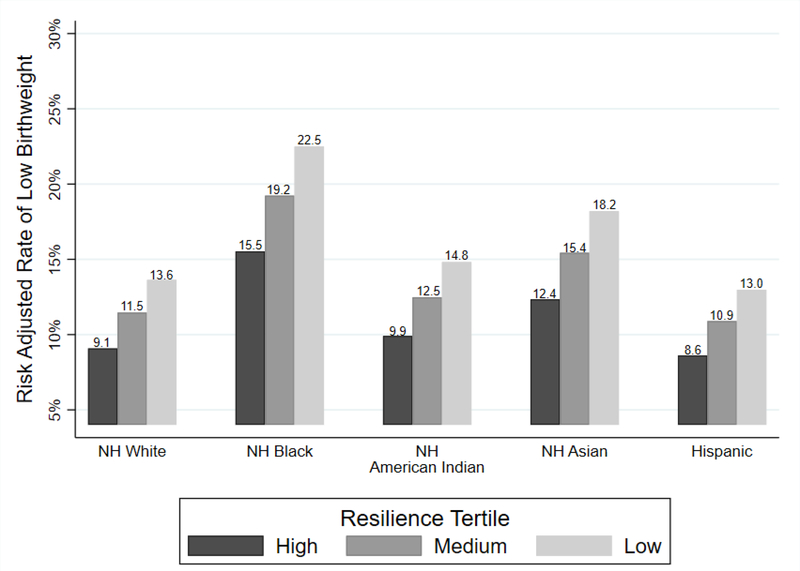
Resilience scores were lowest in American Indian women. Women with the lowest resilience scores were more likely to deliver a LBW infant than highly resilient women, after adjusting for demographic and health-related factors (aOR 1.58 95% CI 1.05–2.38). The risk- adjusted rate of LBW among highly resilient Black women (15.6%) was significantly higher than the risk-adjusted rate of LBW among highly resilient white women (9.1%, p = 0.01) and highly resilient Hispanic women (8.6%, p=0.04).
Conclusion:
Resilience scores differ significantly among women of different race and ethnicity but do not appear to entirely account for racial/ethnic disparities in LBW.
Introduction
Low birthweight (LBW) represents an important measure of population health given its relationship to infant mortality, adult cardiovascular morbidity and mortality, insulin resistance and potentially adult reproductive fertility.[1–4] LBW most often occurs in the context of preterm birth and/or intrauterine growth restriction.[5] Significant racial/ethnic disparities in LBW exist in the United States, with non-Hispanic Black (NHB) women having a LBW rate twice that of non-Hispanic white (NHW) women.[6] Hispanic women also have a higher LBW rate than NHW women, although the overall gap is smaller.[6] Furthermore, racial/ethnic disparities in LBW persist after controlling for patient-level socioeconomic variables such as income, education, and health behaviors.[7]
One important driver of LBW may be social determinants of health.[7,8] Social determinants of health are thought to lead to LBW either directly, such as through lack of access to reproductive health care or indirectly, such as through increased stress associated with personal and structural racism.[9,10] The importance of stress as a driver of poor birth outcomes has been bolstered by the observation that the psychosocial stress burden appears greatest in NHB women,[11,12] and may be associated with physiologic dysfunction. The term “allostatic load” refers to these measurable stress-related pathologic changes in the body,[13] and there is evidence that allostatic load is higher in those who are NHB, older and have lower socioeconomic status.[14]
Resilience can be defined as the many factors that allow individuals to maintain good health despite experiencing stress or adversity in their lives.[15] In addition, racial disparities with respect to resilience appear to exist among pregnant women.[11] However, the literature on maternal resilience during pregnancy and its relationship with birth outcomes is limited and contradictory. Some groups have found resilience to be protective against adverse birth outcomes,[9,16,17] while others have not.[18] Because resilience often has been defined using scales that are neither comprehensive nor validated, study populations have often been small, and neonatal outcome definitions have varied, the true relationship between maternal resilience and birth weight remains uncertain.
Therefore, in this study, we used a validated scale in a large population to investigate the relationship between maternal resilience, race/ethnicity, and LBW specifically. We hypothesized that racial/ethnic disparities might exist with respect to resilience to stress and that racial differences in resilience may be associated with the racial/ethnic disparities in LBW.
Methods
Study Participants
Data were drawn from an existing prospective longitudinal cohort, the National Longitudinal Study of Adolescent to Adult Health (Add Health), which is a nationally-representative longitudinal cohort that followed middle and high school students in the United States into adulthood. Students were initially recruited to the study in grades 7–12 during the 1994–95 school year, and thereafter followed into adulthood with in-school and in-home surveys collected over five waves of data collection spanning 24 years, making the Add Health study one of the broadest data sets on the social, economic, academic, psychological and physical health status of adolescents transitioning into adulthood.[19] For this analysis, we specifically used data from the fourth wave of Add Health data collection in order to maximize information on participants’ birth outcomes. Conducted in 2008, this wave consisted of in-home interviews of 15,701 young adults ages 24–32 years. Given the interest in the association between maternal resilience and LBW, the cohort for our analysis was restricted to female participants who had experienced at least one pregnancy at the time of the 2008 wave four interviews. Exclusion criteria were primarily not having a liveborn infant at the conclusion of the pregnancy and not answering questions related to resilience.
Although some Add Health data are publicly available via the Add Health website (https://www.cpc.unc.edu/projects/addhealth/documentation/publicdata), this study utilized the extensive restricted-use data available by contractual agreement. Written consent was obtained from participants by the original investigators. This study was deemed exempt by our local institutional review board due to the de-identified nature of the data.
Key Variables
Resilience is examined alternately as an exposure and an outcome in this study. We measured resilience using the Add Health Resilience Instrument (AHRI).[20] No resilience instruments were used during any of the Add Health interviews, but many of the questions participants were asked during the fourth wave of data collection are related to themes common to resilience instruments. As such, our team created a resilience instrument specific to Add Health using the fourth wave of Add Health data and the Connor Davidson Resilience Scale (CD RISC) as a model.[20] We modeled the AHRI after the CD RISC because the CD RISC has strong psychometric properties[21] and has been validated in diverse populations of many ages.[22–24] In our previous work, we showed that the AHRI exhibited appropriate internal consistency and discriminant validity. The AHRI consists of 13 items grouped into 3 factors: personal competence, feeling supported vs. overwhelmed, and optimism (See Table 1 for the full instrument). The maximum possible score on the AHRI is 29, with higher scores indicating higher resilience. AHRI scores are normally distributed, and for some aspects of our analyses, were stratified into tertiles in this study population of Add Health participants, with low scores defined as < 10, medium as 10–19 and high as 20–29.[20]
Table 1.
Add Health Resilience Instrument
| Factors | Items from Add Health |
|---|---|
| Personal Competence/Agency | I can’t change the important things in my life.* |
| I avoid having to deal with problems in my life.* | |
| Other people determine what I can and cannot do.* | |
| Many things interfere with what I want to do.* | |
| I feel confident in my ability to handle my problems. | |
| I hardly ever expect things to go my way.* | |
| I have no way to solve the problems I have.* | |
| Support / Feeling Overwhelmed | I often feel isolated.* |
| Difficulties pile up so high that I can’t overcome them.* | |
| I feel I can’t control the important things in my life.* | |
| Optimism | I’m always optimistic about my future. |
| I am not easily bothered. | |
| I expect more good things to happen to me than bad. | |
These items are reverse coded in order for higher scores to indicate higher resilience.
For our aim of looking for racial/ethnic differences in resilience, self-reported race and ethnicity were considered as the relevant exposure. Six mutually exclusive racial/ethnic categories were created from self-reported Add Health data: NHW, NHB, American Indian, Asian, Hispanic and other. For the second aim of exploring the association between maternal resilience and low birthweight (i.e. weight <2500 grams at birth), resilience was the exposure variable. In Add Health, birthweight was self-reported by parents. LBW was considered to have occurred if a given participant had at least one LBW delivery prior to the 2008 interview.
Statistical Analyses
Sampling weights were used per guidelines provided by the Add Health research team for all multivariable analyses and to report summary statistics for each racial/ethnic group or resiliency tertile.[25] In order to estimate the association between self-reported race/ethnicity and AHRI resilience scores, bivariable analyses were conducted using ANOVA tests. Adjusted Wald tests with Bonferroni corrected p-values were conducted for all pairwise comparisons of resilience scores amongst different race/ethnicity categories. Poisson regression multivariable regression models were then employed to estimate the relative change in resilience scores for each racial/ethnic category compared to the reference group (non-Hispanic white women). These models were sequentially adjusted for education and household income, as these variables have been documented to be associated with resilience in the literature.[26,27]
We then turned our attention to the outcome of LBW and estimated risk of LBW in this cohort by race/ethnicity. In order to examine the association between resilience and LBW, resilience score tertiles were used as the exposure. Logistic regression models with LBW as the outcome adjusted for factors previously associated with LBW: age, race/ethnicity, education, body mass index (BMI), smoking/alcohol use, prenatal care and household income, where each covariate was obtained from specific questions in waves 1 and 4 of the Add Health survey. All Poisson and logistic regression models were clustered by the high school where participants were initially recruited and surveyed. Finally, we conducted a series of prespecified interaction analyses to assess whether the strength of the association between resilience and LBW differed for women of different races/ethnicities. This was done by interacting our race/ethnicity variables with resilience tertile in the regression models that used LBW as the outcome. Finally, we calculated the predicted probability of LBW by both race/ethnicity and resilience tertile using the margins command in STATA. This methodology allows for the prediction of the probability of an outcome based on varying levels of an exposure variable.[28] In our case, the predicted probabilities we generated correspond to a covariate risk-adjusted rate of LBW in each race/ethnicity and resilience grouping. We then performed pairwise comparisons of these predicted probabilities of LBW using Bonferroni corrected p-values to assess significance.
Code Availability
We used STATA version 15 (StataCorp LLC, College Station, TX) for all analyses. Codes used for analyses are available upon request.
Results
Of the 15,701 participants sampled in wave 4, 53% were women (n=8352). Of these women, 58% (n= 4813) reported on 5985 pregnancies that ended with a live born infant. Less than 0.5% of these women failed to answer the questions on the AHRI resilience instrument we constructed, thus we felt this was a negligible source of bias. 583 of the infants reported on during this wave of data collection were LBW. In order to not overrepresent multiparous women’s resilience, we collapsed women’s pregnancy outcomes to a binary variable indicating whether she had ever had a LBW infant or not. This left an analytic sample of 3244 women and infants.
Table 2 summarizes descriptive statistics for this analytic sample. Two thirds of the cohort identified as white, 15% as non-Hispanic Black and 12% as Hispanic. 13.1% of the cohort had completed college and over half of the cohort reported a household income of less than $100,000/year. The median resilience score was 14 (interquartile range, IQR 11–18). American Indian (AI) participants had the lowest scores (median 12, IQR 7–15) and participants in the “other” race/ethnicity category had the highest resilience scores (median 15, IQR 12–19) (Table 3). In pairwise comparisons, AI scores were significantly lower than resilience scores among NHW women (p=0.008), NHB women (p=0.013), Hispanic women (p=0.014) and participants in the “other” racial/ethnic category (p=0.028). After adjusting for household income and education in the multivariable Poisson regression models, AI women had an 11% lower resilience score than NHW women (aRR 0.89, 95% CI 0.81–0.98) and Asian women had a 10% lower resilience score than NHW women (aRR 0.90, 95% CI 0.84–0.96). None of the other relative differences in resilience scores were statistically significant (Table 3).
Table 2.
Demographic characteristics of women with at least one completed pregnancy at time of 2008 interview (N= 3244)
| Variable | Mean (SD) or % of Cohort |
|---|---|
| Mean Age in years (SD) | 28.6 (1.9) |
| Race/Ethnicity | |
| Non-Hispanic White | 66.5% |
| Non-Hispanic Black | 15.2% |
| Non-Hispanic American Indian | 2.4% |
| Non-Hispanic Asian | 2.9% |
| Other Non-Hispanic | 1.0% |
| Hispanic | 12.0% |
| Foreign Born | 7.4% |
| Highest Level of Education Achieved | |
| Less than High School | 12.1% |
| Less than College | 68.1% |
| College Degree | 13.1% |
| More than College | 6.7% |
| Household Income | |
| <$20,000 | 13.1% |
| $20–49,999 | 34.5% |
| $50–99,999 | 40.7% |
| $100–149,999 | 8.1% |
| >$150,000 | 3.6% |
| Missing | 0% |
| BMI | |
| Underweight | 2.4% |
| Normal | 29.3% |
| Overweight | 25.0% |
| Obese | 43.4% |
| Mean Resilience Score (SD) | 13.8 (5.2) |
| Low Birth Weight (% of all births) | 13.5% |
Table 3.
Differences in Resilience by Race/Ethnicity
| Race/Ethnicity Category | Median AHRI score (Interquartile Range) | Unadjusted Relative Change in Resilience Score* | P-value | Adjusted Relative Change in Resilience Score** | P-value |
|---|---|---|---|---|---|
| Non-Hispanic White | 14 (11–18) | Ref | – | Ref | – |
| Non-Hispanic Black | 14 (11–17) | 0.98 (0.94–1.03) | 0.455 | 1.04 (0.99–1.09) | 0.122 |
| Non-Hispanic American Indian | 12 (7–15) | 0.81 (0.72–0.91) | <0.001 | 0.89 (0.81–0.98) | 0.020 |
| Non-Hispanic Asian | 13 (10–16) | 0.90 (0.83–0.97) | 0.006 | 0.90 (0.84–0.96) | 0.003 |
| Other Non- Hispanic | 15 (12–19) | 1.11 (0.98–1.25) | 0.088 | 1.08 (0.96–1.22) | 0.215 |
| Hispanic | 14 (11–18) | 0.99 (0.94–1.04) | 0.568 | 1.04 (0.97–1.10) | 0.249 |
Adjusted for education and household income
In this cohort, 13.5% of births were LBW, which is higher than the LBW rate of 8.2% reported by the CDC in the United States in 2008.[29] NHB women had the highest rates of LBW (20.1%), which was nearly double that seen among NHW women (11.4%) (Supplementary Table 1). The next highest LBW rates were seen among Asian (15.4%) and AI women (13.6%). Among Hispanic women, 10.8% in our cohort had delivered a LBW infant. In multivariable analyses adjusted for maternal demographics, BMI and smoking, NHB women had a 1.9 times higher risk of delivering a LBW infant compared to White women (95% CI 1.3–2.8). Women from other racial/ethnic categories had similar risk of LBW compared to NHW women (Supplementary Table 1).
Table 4 reports on the association between resilience and LBW in our cohort. We found that compared to women with a resilience score that fell into the highest tertile, women with a resilience score in the lowest tertile were 1.6 times more likely to have had a LBW infant (95% CI 1.05–2.38), after adjusting for covariates. Although the direction of the association between medium resilience and LBW was similar to the association between low resilience and LBW, this association did not reach statistical significance (aOR 1.3, 95% CI 0.89–1.89).
Table 4.
Associations Between Resilience and Risk of Low Birthweight
| Resilience Category | Unadjusted Odds of LBW (95% CI) | P-value | Adjusted Odds of LBW* (95% CI) | P-value |
|---|---|---|---|---|
| High Resilience | Ref | – | Ref | – |
| Medium Resilience | 1.25 (0.89–1.78) | 0.212 | 1.29 (0.88–1.89) | 0.191 |
| Low Resilience | 1.59 (1.07–2.38) | 0.023 | 1.58 (1.05–2.38) | 0.030 |
Adjusted for maternal age, race/ethnicity, education, household income, BMI, prenatal care and nicotine/alcohol use during pregnancy
We found no significant interaction between race/ethnicity and resilience tertile for the outcome of LBW (p-values for interactions all > 0.05). Figure 1 summarizes the predicted probability of LBW within each combined race/ethnicity and resilience tertile grouping. We found that NHB women in the highest resilience category had a higher predicted probability of LBW (15.5%) than highly resilient NHW women (9.1%, p=0.010) and highly resilient Hispanic women (8.6%, p = 0.038) (Figure 1), after adjusting for covariates. Similarly, the risk-adjusted rate of LBW among NHB women in the lowest resilience tertile (22.5%) was significantly higher than the risk-adjusted rate of LBW for both NHW women (13.6%, p=0.010) and Hispanic women (13.0%, p=0.038) in the lowest resilience tertile.
Figure 1. Differences in the risk adjusted rate of LBW by race/ethnicity and resilience tertile grouping.
These rates were adjusted for maternal age, education, household income, BMI and nicotine use during pregnancy.
Discussion
In this large cohort of US women of childbearing age, we found that there were racial/ethnic differences in resilience as determined on the Adolescent to Adult Health Resilience Instrument, with AI and Asian participants having the lowest resilience scores. In addition, we demonstrated an association between resilience and risk of LBW: mothers with the overall lowest resilience scores exhibited a higher risk of having a LBW infant than mothers with the highest resilience scores.
Our study results differ from prior literature primarily because of the instrument we used to assess resilience. The Add Health Resilience Instrument our group developed and used in this study was modeled off the CD-RISC (Table 1),[20] which in a recent systematic review of existing resilience measures was found to have one of the top psychometric ratings of all validated resilience scales.[21] It is also considered one of the most comprehensive scales because it assesses both internal personal assets and external resources that together might comprise an individuals’ ability to tolerate and respond positively in the face of stress.[21,30] The AHRI was developed to be able to apply the strengths of the CD RISC to the existing Add Health dataset, but it has not been used by others to assess perinatal resilience.
Despite differences in how we defined and measured resilience, several studies have found similar associations between maternal resilience and adverse birth outcomes. For instance, one group reported lower rates of LBW among women who were most optimistic on the Life Orientation Test during the second trimester of pregnancy.[17] In a much larger cohort, Bhatia et al. examined rates of preterm birth amongst a large cohort in Los Angeles and found that women who perceived themselves to have low resilience had significantly more preterm births than those who perceived themselves to have high resilience.[16] In this study, resilience was measured postnatally using five questions pulled from the Rosenberg self-esteem scale and the Pearlin Mastery scale.[16]
The largest study which has assessed the relationship between resilience and perinatal outcomes using the CD-RISC was conducted by Grobman et al. using the nuMoM2b cohort of over 9,000 women across the United States. In this study, researchers reported no significant association between CD-RISC resilience scores measured during the second trimester of pregnancy and preterm birth or small-for-gestational age (SGA) size at birth.[11] They did however find that lower reported social support was associated with a marginally increased risk in preterm birth and SGA.[11] It is unclear why we found a relationship between resilience and LBW in our cohort while this association was not found in the nuMom2b cohort, though it may be related to the fact that our group looked at associations between resilience and LBW, not preterm birth or SGA, two clinically distinct populations which do not always overlap with LBW. SGA in particular, encompasses all infants affected fetal growth restriction and adjusts for gestational age; as such the term includes infants born both preterm and term.[31] In addition, resilience was measured prenatally in the nuMom2b study while in the present analysis it was measured in the months to years after the infant in question was born, similar to the design used by Bhatia et al.[16] Additionally, our group used tertiles to define low resilience score cutoffs, while Grobman et al used quartiles, thereby defining their low resilience population more stringently than our group did.
These inconsistent findings in the literature coupled with the various time points when resilience was measured bring up unanswered questions about whether pregnancy changes a woman’s resilience profile such that her answers on a defined resilience scale become negatively associated with her risk of a poor birth outcome only when measured outside of the actual pregnancy period. To our knowledge, no studies have examined the relationship between women’s birth outcomes and their resilience either before conception or shortly thereafter, nor examined resilience longitudinally before and after pregnancy. It is thus unclear whether resilience is changed by the psychosocial and physical load of pregnancy and birth.
Another important area of future exploration that our study highlights is the relationship between stress, resilience to stress and birth weight among NHB women in particular. There is evidence that pregnant NHB women experience increased stress compared to women of other racial/ethnic groups.[32,33] In the setting of these known stress disparities, our findings that even the most highly resilient NHB women in our cohort had higher rates of LBW than NHW and Hispanic women with similarly high resilience scores, raises questions about whether the impact of stress on birth weight is particularly magnified among Black women. Although resilience did appear to improve risk of LBW in our cohort, it did not overcome baseline racial differences in risk of LBW. Given that race is a social construct which likely serves as a proxy measure for sociopolitical and environmental risk factors related to structural racism,[34,35], our findings indicate that solely focusing on individual resilience may be insufficient to fully address birth outcomes disparities for Black women if not accompanied by attention to the structural roots of maternal stress.
Limitations of our study include the small sample size within some of the racial/ethnic categories. In particular, the two groups who demonstrated the lowest resilience scores in our cohort, American Indian and Asian women, were among the smallest. Given that only 12 American Indian women and 25 Asian women, respectively, reported a LBW pregnancy, our limited sample size likely affected our power to detect a significant interaction between low resilience and LBW. However, resilience effects in this study were noted to be consistent across all racial/ethnic groups, with all groups showing progressively higher rates of LBW as resilience decreased, which indicates a trend that merits future study. Interestingly, resilience scores were highest among women in the “Other” racial/ethnic category. Although this category could include multi-racial women, we have no way of confirming who self-identified in this way. As such, this highlights the need for improved racial/ethnic categorizations in administrative and research datasets.[36] Another limitation of our study is that, since resilience instruments were not employed by the original Add Health investigators, the AHRI we created retrospectively only captures resilience data at one point in time (wave 4 of Add Health data collection). Thus, although there is evidence that resilience is dynamic and can change in response to stressors,[37] we had no way to assess whether resilience changed in participants over the course of the multiple pregnancies assessed during the wave 4 data collection. In general, this is a gap in the literature: there is no published data on the trajectory of resilience over the course of a pregnancy or across different pregnancies in the same woman. Finally, the necessary cross-sectional nature of the AHRI led us to collapse the outcome of LBW into a single binary variable for women interviewed during this wave of data collection. This meant we could not include risk factors for LBW related to prior pregnancy history, such as interpregnancy interval or previous history of a LBW or preterm infant, in our models.[38] We also could also not explore the risk of LBW across pregnancies in multiparous women. These all represent areas worthy of future investigation.
In this study of Add Health participants, we found evidence that postnatal maternal resilience may be associated with low birthweight. Future research is needed to assess whether resilience plays a modifying role in the known relationship between stress and adverse birth outcomes and if such an effect is present, whether it varies for women of different racial/ethnic background.
Supplementary Material
Acknowledgements
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. No direct support was received from grant P01-HD31921 for this study, however we would like to acknowledge the Division of Neonatology at the Children’s Hospital of Philadelphia for administrative support and Ms. Ali Chandler for her assistance in preparing this manuscript.
Funding: This research uses data from Add Health, which was originally funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. The authors of this paper received no additional funding to complete this study.
Footnotes
Conflicts of interest/Competing interests: The authors declare that they have no conflicts of interest.
Ethics approval: This study was deemed exempt by the local Institutional Review Board as it uses de-identified, publicly available data. This study was performed in accordance with the Declarations of Helsinki.
Consent to participate: All original participants provided written, informed consent to participate
Consent for publication: The written consent informed participants that results, in aggregate, would be published.
Availability of data and material: This study utilized both the public use and restricted use data provided by the original Add Health investigative team. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth).
Code availability: The codes used for the analyses in this paper are available upon request.
References
- 1.Hughes MM, Black RE, Katz J. 2500-g Low Birth Weight Cutoff: History and Implications for Future Research and Policy. Matern Child Health J. 2017. February;21(2):283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Visentin S, Grumolato F, Nardelli GB, Di Camillo B, Grisan E, Cosmi E. Early origins of adult disease: low birth weight and vascular remodeling. Atherosclerosis. 2014. December;237(2):391–9. [DOI] [PubMed] [Google Scholar]
- 3.Boeri L, Ventimiglia E, Capogrosso P, Ippolito S, Pecoraro A, Paciotti M, et al. Low Birth Weight Is Associated with a Decreased Overall Adult Health Status and Reproductive Capability - Results of a Cross-Sectional Study in Primary Infertile Patients. PLoS One. 2016. November 28;11(11):e0166728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hovi P, Andersson S, Eriksson JG, Järvenpää A-L, Strang-Karlsson S, Mäkitie O, et al. Glucose regulation in young adults with very low birth weight. N Engl J Med. 2007. May 17;356(20):2053– 63. [DOI] [PubMed] [Google Scholar]
- 5.Institute of Medicine (US) Committee on Improving Birth Outcomes, Bale JR, Stoll BJ, Lucas AO. Improving Birth Outcomes: Meeting the Challenge in the Developing World. National Academies Press (US); 2003. [PubMed] [Google Scholar]
- 6.Hamilton Brady E., Martin Joyce A., Osterman Michelle J.K., Rossen Lauren M. Births: Provisional Data for 2018. National Vital Statistics Rapid Release. 2019. May;(007):1–25. [Google Scholar]
- 7.Burris HH, Hacker MR. Birth outcome racial disparities: A result of intersecting social and environmental factors. Semin Perinatol. 2017. October;41(6):360–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorch SA, Enlow E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Pediatr Res. 2015. October;(April):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDonald SW, Kingston D, Bayrampour H, Dolan SM, Tough SC. Cumulative psychosocial stress, coping resources, and preterm birth. Arch Womens Ment Health. 2014. December;17(6):559–68. [DOI] [PubMed] [Google Scholar]
- 10.Wainstock T, Anteby E, Glasser S, Shoham-Vardi I, Lerner-Geva L. The association between prenatal maternal objective stress, perceived stress, preterm birth and low birthweight [Internet]. Vol. 26, The Journal of Maternal-Fetal & Neonatal Medicine. 2013. p. 973–7. Available from: 10.3109/14767058.2013.766696 [DOI] [PubMed] [Google Scholar]
- 11.Grobman WA, Parker C, Wadhwa PD, Willinger M, Simhan H, Silver B, et al. Racial/Ethnic Disparities in Measures of Self-reported Psychosocial States and Traits during Pregnancy. Am J Perinatol. 2016. December;33(14):1426–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenthal L, Lobel M. Explaining racial disparities in adverse birth outcomes: unique sources of stress for Black American women. Soc Sci Med. 2011. March;72(6):977–83. [DOI] [PubMed] [Google Scholar]
- 13.Olson DM, Severson EM, Verstraeten BSE, Ng JWY, McCreary JK, Metz GAS. Allostatic Load and Preterm Birth. Int J Mol Sci. 2015. December 15;16(12):29856–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hux VJ, Catov JM, Roberts JM. Allostatic load in women with a history of low birth weight infants: the national health and nutrition examination survey. J Womens Health . 2014. December;23(12):1039–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Solivan AE, Wallace ME, Kaplan KC, Harville EW. Use of a resiliency framework to examine pregnancy and birth outcomes among adolescents: A qualitative study. Fam Syst Health. 2015. December;33(4):349–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhatia N, Chao SM, Higgins C, Patel S, Crespi CM. Association of Mothers’ Perception of Neighborhood Quality and Maternal Resilience with Risk of Preterm Birth . Int J Environ Res Public Health. 2015. August 12;12(8):9427–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lobel M, DeVincent CJ, Kaminer A, Meyer BA. The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol. 2000. November;19(6):544–53. [DOI] [PubMed] [Google Scholar]
- 18.Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, et al. Racial Disparities in Adverse Pregnancy Outcomes and Psychosocial Stress. Obstet Gynecol. 2018. February;131(2):328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris KM, Halpern CT, Whitsel E, Hussey J, Tabor J, Entzel P, and Udry JR The National Longitudinal Study of Adolescent to Adult Health: Research Design [Internet]. 2009. [cited 2019 Mar 4]. Available from: http://www.cpc.unc.edu/projects/addhealth/design
- 20.Montoya-Williams D, Passarella M, Lorch SA. Retrospective Development of a Novel Resilience Scale using Existing Cohort Data: The Adolescent to Adult Health Resilience Instrument Under Review. [DOI] [PMC free article] [PubMed]
- 21.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health Qual Life Outcomes. 2011. February 4;9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blanco V, Guisande MA, Sánchez MT, Otero P, Vázquez FL. Spanish validation of the 10-item Connor-Davidson Resilience Scale (CD-RISC 10) with non-professional caregivers. Aging Ment Health. 2017. November 8;1–6. [DOI] [PubMed] [Google Scholar]
- 23.Green KT, Hayward LC, Williams AM, Dennis PA, Bryan BC, Taber KH, et al. Examining the factor structure of the Connor-Davidson Resilience Scale (CD-RISC) in a post-9/11 U.S. military veteran sample. Assessment. 2014. August;21(4):443–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Notario-Pacheco B, Solera-Martínez M, Serrano-Parra MD, Bartolomé-Gutiérrez R, García- Campayo J, Martínez-Vizcaíno V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health Qual Life Outcomes. 2011. August 5;9:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen P, Chantala K. Guidelines for Analyzing Add Health Data [Internet]. Carolina Digital Repository; 2014. Available from: 10.17615/C6BW8W [DOI] [Google Scholar]
- 26.Oliveira ACP de Miss, Machado APG Mr, Aranha RN Miss. Identification of factors associated with resilience in medical students through a cross-sectional census. BMJ Open. 2017. November 12;7(11):e017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Z, Liu Y, Li X, Li X. Resilience and Associated Factors among Mainland Chinese Women Newly Diagnosed with Breast Cancer. PLoS One. 2016. December 9;11(12):e0167976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014. June;43(3):962–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Osterman MJK. Births: final data for 2008. Natl Vital Stat Rep. 2010. December 8;59(1):1, 3–71. [PubMed] [Google Scholar]
- 30.Rutter M Resilience as a dynamic concept. Dev Psychopathol. 2012. May;24(2):335–44. [DOI] [PubMed] [Google Scholar]
- 31.Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle- income countries in 2010. Lancet Glob Health. 2013. July;1(1):e26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hogue CJR, Bremner JD. Stress model for research into preterm delivery among black women. Am J Obstet Gynecol. 2005. May;192(5 Suppl):S47–55. [DOI] [PubMed] [Google Scholar]
- 33.Borders AEB, Wolfe K, Qadir S, Kim K-Y, Holl J, Grobman W. Racial/ethnic differences in self- reported and biologic measures of chronic stress in pregnancy. J Perinatol. 2015. August;35(8):580–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boyd RW, Lindo EG, Weeks LD, Lemore MR. On Racism: A New Standard For Publishing On Racial Health Inequities [Internet]. Health Affairs Blog. 2020. [cited 2020 Jul 6]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20200630.939347/full/ [Google Scholar]
- 35.Vyas DA, Eisenstein LG, Jones DS. Hidden in Plain Sight — Reconsidering the Use of Race Correction in Clinical Algorithms. N Engl J Med [Internet]. 2020. June 17; Available from: 10.1056/NEJMms2004740 [DOI] [PubMed] [Google Scholar]
- 36.Ashok S The Rise of the American “Others.” The Atlantic [Internet]. 2016. August 27 [cited 2020 Jul 3]; Available from: https://www.theatlantic.com/politics/archive/2016/08/the-rise-of-the-others/497690/ [Google Scholar]
- 37.Helmreich I, Kunzler A, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst Rev [Internet]. 2017. February [cited 2020 Jul 3];2017(2). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464102/ [Google Scholar]
- 38.Liauw J, Jacobsen GW, Larose TL, Hutcheon JA. Short interpregnancy interval and poor fetal growth: Evaluating the role of pregnancy intention. Paediatr Perinat Epidemiol. 2019. January;33(1):O73–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.