Abstract
Background
Psychological responses to potentially traumatic events tend to be heterogeneous, with some individuals displaying resilience. Longitudinal associations between resilience and mental distress during the COVID-19 pandemic, however, are poorly understood. The objective of this study was to examine the association between resilience and trajectories of mental distress during the COVID-19 pandemic.
Methods
Participants were 6,008 adults from the Understanding America Study, a probability-based Internet-panel representative of the US adult population. Baseline data were collected between March 10 and March 31, 2020, with nine follow-up waves conducted between April 1 and August 4. Mixed-effects logistic regression was used to examine the association between date and mental distress, stratified by resilience level (low, normal, or high).
Results
In contrast to the high resilience group, participants in the low and normal resilience groups experienced increases in mental distress in the early months of the pandemic (low: OR=2.94, 95% CI=1.93-4.46; normal: OR=1.91, 95% CI=1.55-2.35). Men, middle-aged and older adults, Black adults, and adults with a graduate degree were more likely to report high resilience, whereas adults living below the poverty line were less likely to report high resilience.
Limitations
These associations should not be interpreted as causal, and resilience was measured at only one time-point.
Conclusions
Trajectories of mental distress varied markedly by resilience level during the early months of the COVID-19 pandemic, with low-resilience adults reporting the largest increases in mental distress during this crisis. Activities that foster resilience should be included in broader strategies to support mental health throughout the pandemic.
Keywords: COVID-19, resilience, mental health
1. Introduction
The COVID-19 pandemic has had a deleterious effect on mental health in the US. Compared to before the pandemic, the prevalence of serious psychological distress in the general population has increased approximately three-fold (McGinty et al., 2020). However, despite fears of a “second pandemic” of mental illness, a substantial proportion of the population has continued to report good mental health (Riehm et al., 2020), reflecting possible resilience.
Resilience is a pattern of adaptive functioning that is shaped by interactions between a person, those around them, and their environment (Mancini, 2020; PeConga et al., 2020). The COVID-19 pandemic displays a number of unique qualities, including prolonged social distancing; an uncertain timeframe for resolution; and economic and political instability. Given these unique characteristics, it is plausible that resilience will interact with mental health over time, giving rise to heterogenous trajectories of mental distress among individuals with different levels of resilience (Mancini, 2020; Bendau et al., 2020).
To our knowledge, there are no longitudinal studies that have investigated associations between resilience and mental distress during the COVID-19 pandemic. At best, cross-sectional studies provide a snapshot of functioning during a limited time period; longitudinal investigations are necessary for capturing fluctuations in mental distress over the course of this rapidly evolving pandemic. Additionally, given that resilience can be learned (PeConga et al., 2020), understanding of how resilience interacts with mental distress is essential for supporting population-level mental health. The objectives of this study were to (1) examine the association between resilience and trajectories of mental distress during the COVID-19 pandemic and (2) determine which sociodemographic characteristics are associated with resilience.
2. Methods
2.1. Participants
Participants were drawn from the Understanding America Study (UAS), a probability-based, nationally-representative Internet-panel of adults representing the US. Details regarding the UAS methodology can be found at the UAS website (https://UASdata.usc.edu). The baseline wave of data collection was fielded from March 10 – March 31. Starting on April 1, respondents were then invited to participate in bi-weekly surveys according to a staggered schedule, whereby one fourteenth of the sample was invited every day. Participants who consented completed follow-up surveys biweekly between April 1 and August 4, during which there were nine follow-up surveys administered.
Of the 8,547 eligible panel members, 6,403 completed follow-up survey three (April 29 – May 26), where the resilience measure was administered (response rate of 74.9%). We included the 6,008 (93.8%) participants with complete data on the variables of interest. These participants completed an average of 9.2 out of ten possible surveys (baseline and nine follow-up surveys).
2.2. Measures
2.2.1. Resilience
Resilience was measured with the 6-item Brief Resilience Scale (BRS) (Smith et al., 2008) and responses were recorded on a 5-point Likert scale (“strongly disagree” to “strongly agree”). Total scores were obtained by taking the mean of the item scores; we then categorized participants into low (1.00-2.99), normal (3.00-4.30), and high (4.31-5.00) resilience groups according to previously established cutoffs (Smith et al., 2013). Previous studies have found that the BRS has good internal consistency and correlates with related constructs including coping, social support, and sense of purpose (Cronbach's alpha = 0.87) (Chmitorz et al., 2018; Smith et al., 2008).
2.2.2. Mental Distress
Mental distress was measured with the 4-item Patient Health Questionnaire (PHQ-4). The PHQ-4 has adequate construct validity and is reliable in the general population (Kroenke et al., 2009). Participants were asked for the frequency over the past two weeks with which they had been bothered by two symptoms of anxiety (items drawn from the 7-item Generalized Anxiety Disorder scale) and two symptoms of depression (items drawn from the PHQ-9). Scores were obtained by summing the four items (range 0-12), which were classified into categories indicating distress severity based on validated cut-points (normal [0-2], mild [3-5], moderate [6-8], or severe [9-12]) (Kroenke et al., 2009). We dichotomized these categories into a binary outcome (normal versus mild/moderate/severe mental distress).
2.2.3. Survey Date
We used survey date as the time scale to assess changes over time. Survey date was entered into each model as a continuous variable representing the number of days since March 10, ending on August 4. We modelled survey date with restricted cubic splines, which capture features that may be missed by traditional techniques such as linear models or categorization into bins. We generated splines with five knots using percentiles (5, 27.5, 50, 72.5, and 95) corresponding to the following dates: March 12, April 26, May 27, June 29, and July 29.
2.2.4. Sociodemographic Characteristics
Sociodemographic characteristics of interest included age, sex, race/ethnicity, Federal Poverty Line, household structure, and education.
2.3. Statistical Analysis
First, we examined changes over time in mental distress within each category of resilience. We used mixed-effects logistic regression models with a random effect for participant to accommodate repeated measures. To determine whether trajectories of mental distress over time differed between resilience groups, we estimated a model with interactions between the splines for days since March 10 and an indicator variable for resilience group. The margins and the xbrcspline commands in Stata were used to generate predicted probabilities of mental distress and to estimate odds ratios for mental distress on given survey dates compared to March 11, respectively, in each resilience group. March 11 was used as the reference date instead of March 10 due to a higher number of observations (2,127 versus 384, respectively). Second, we estimated a single logistic regression model with covariates for each sociodemographic characteristic and resilience level as the outcome (high versus normal/low).
2.3.1. Inference
All analyses incorporated survey weights that account for probabilities of sample selection and survey non-response and are aligned with Current Population Survey benchmarks. Missing observations due to survey non-response were handled with full information maximum likelihood estimation. Statistical significance was assessed at the p<.05 level. Analyses were conducted using Stata version 16 (StataCorp Inc., College Station, TX) and R (R studio version 1.2.5042; R version 4.0.0).
3. Results
Of 6,008 respondents, 1,037 (16.6%) reported low resilience, 3,944 (66.2%) reported normal resilience, and 1,027 (17.2%) reported high resilience (Table 1 ).
Table 1.
Sociodemographic characteristics and associations with resilience among US adults in the UAS Panel, 2020 (n=6,008).
| Sociodemographic Characteristic | N (%) | Association with High Resilience (OR, 95% CI) |
|---|---|---|
| Sex | ||
| Female | 3,500 (51.0) | ref. |
| Male | 2,508 (49.0) | 1.61 (1.33, 1.95) |
| Age Group | ||
| 18-29 | 646 (12.3) | ref. |
| 30-49 | 2,181 (39.5) | 1.29 (0.86, 1.92) |
| 50-64 | 1,814 (27.2) | 1.56 (1.05, 2.33) |
| 65+ | 1,367 (20.9) | 1.69 (1.12, 2.55) |
| Race/Ethnicity | ||
| White | 4,043 (64.1) | ref. |
| Black | 450 (11.6) | 1.72 (1.25, 2.35) |
| Hispanic/Latino | 911 (15.5) | 0.92 (0.65, 1.31) |
| Other | 604 (8.8) | 0.95 (0.65, 1.38) |
| Household Structure | ||
| With Partner Only | 1,827 (29.1) | ref. |
| Alone | 1,025 (16.1) | 0.83 (0.62, 1.10) |
| With Partner and Children | 1,424 (24.5) | 1.08 (0.82, 1.40) |
| With Children Only | 269 (4.5) | 0.62 (0.37, 1.02) |
| Other | 1,463 (25.8) | 0.88 (0.67, 1.17) |
| Federal Poverty Line | ||
| Above | 5,273 (85.1) | ref. |
| Below | 735 (14.7) | 0.47 (0.33, 0.67) |
| Education | ||
| High School or Less | 1,276 (37.4) | ref. |
| Some College | 2,224 (27.9) | 1.19 (0.93, 1.52) |
| Bachelor's Degree | 1,478 (19.4) | 1.10 (0.84, 1.44) |
| Graduate Degree | 1,030 (15.4) | 1.60 (1.21, 2.13) |
Notes: Percentages are weighted.
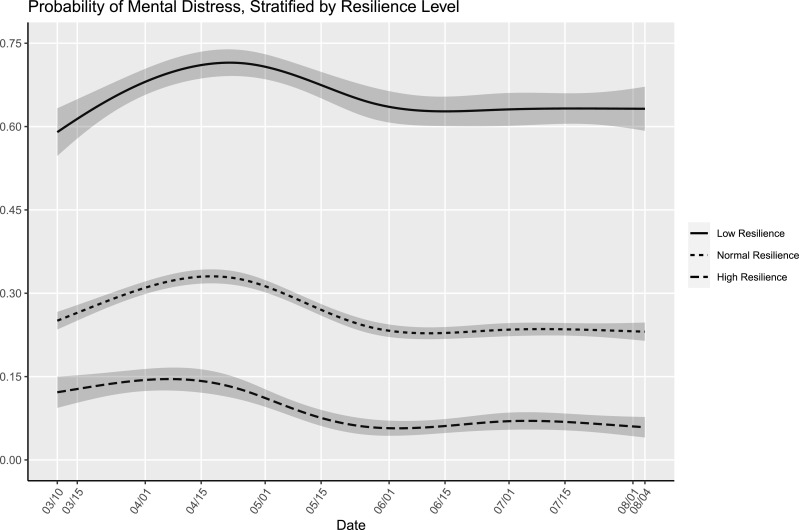
Fig. 1 displays the probability of reporting mild, moderate, or severe mental distress by survey date, stratified by level of resilience. The interaction between the spline terms and level of resilience was significant (p<0.001), indicating that trajectories of mental distress over time differed between resilience groups. Between March 11 and May 1, participants in the low and normal resilience groups experienced increases in mental distress (low: OR=2.94, 95% CI=1.93-4.46; normal: OR=1.91, 95% CI=1.55-2.35), whereas those in the high resilience group did not (OR=0.83, 95% CI=0.51-1.37). By August 1, levels of mental distress in the low and normal resilience groups were comparable to March 11 (low: OR=1.38, 95% CI=0.91-2.10; normal: OR=0.77, 95% CI=0.61-0.98); among those in the high resilience group, mental distress was significantly lower than on March 11 (OR=0.28, 95% CI=0.15-0.54). In supplementary analyses, resilience level had similar associations with the anxiety and depressive symptom subscales of the PHQ-4 (see Supplementary Figs. 1 and 2).
Fig. 1.
Predicted probabilities (bold lines) of mild, moderate, or severe mental distress with 95% confidence intervals (shaded areas) by date of survey completion, stratified by resilience level, among US adults in the UAS Panel, 2020 (n=6,008).
In regression analyses (Table 1), the odds of high resilience were higher among male compared to female participants (OR=1.61, 95% CI=1.33-1.95); older age groups compared to adults ages 18-29 (50-64: OR=1.56, 95% CI=1.05-2.33; 65+: OR=1.69, 95% CI=1.12-2.55); Black compared to White participants (OR=1.72, 95% CI=1.25-2.35); and adults with a graduate degree compared to those with a high school education or less (OR=1.60, 95% CI=1.21-2.13). Adults living below the FPL were less likely to report high resilience, compared to those above the FPL (OR=0.47, 95% CI=0.33-0.67).
4. Discussion
In this longitudinal study, we observed marked differences in trajectories of mental distress over time by self-reported resilience level among US adults during the COVID-19 pandemic. Between March 10 and August 4, 2020, adults reporting low or normal levels of resilience experienced approximately a twofold increase in the odds of mental distress, whereas adults reporting high resilience reported no change in mental distress. Males, Black adults, adults over age 50, and adults with a graduate degree had a higher likelihood of reporting high resilience, whereas adults living below the FPL were less likely to report high resilience.
Our findings are consistent with prior studies that show higher resilience among males and with increased age (Chmitorz et al., 2018). Moreover, we found that Black participants were 72% more likely than White participants to report high resilience, whereas Hispanic/Latino adults and adults of another race/ethnicity reported comparable levels of resilience to White participants. This finding is positioned in the midst of mixed evidence related to the relationship between exposure to disasters and psychological outcomes among racial/ethnic minorities (Lowe et al., 2015). This finding may also relate to a longstanding paradox in psychiatric epidemiology, namely the observation that despite exposure to higher levels of adversity than their white counterparts, racial/ethnic minorities tend to report equal or better mental health (McGuire & Miranda, 2008). In the context of the COVID-19 pandemic, one study found that Hispanic/Latino adults were especially likely to report psychological distress compared to other racial/ethnic groups (McGinty et al., 2020); this contradicts this paradox, and suggests that the pandemic may have presented systemic challenges that overwhelm the capacity for individual resilience. With regards to higher resilience among Black participants, (Egede & Walker, 2020), our study period covered a time of significant stress for Black Americans, given the disproportionate COVID-19 mortality and systemic racism experienced by this population. A potential explanation for this finding is that Black respondents may be more likely to endorse trait-level (e.g. personality) resilience. Researchers argue that resilience is dynamic, and trait-level measures may omit context-specific aspects that are salient for longitudinal studies (Aburn et al., 2016). Forthcoming research should consider including dynamic measures of resilience in measuring mental health trajectories, particularly among racially diverse populations.
Adults living below the FPL were less likely to report high resilience. The Coronavirus Aid, Relief, and Economic Security (CARES) Act includes provisions intended to support low-income adults. However, programs such as Medicaid and the Supplemental Nutrition Assistance Program remain areas where greater attention is needed to protect low-income families (Karpman et al., 2020; Parrott et al., 2020). Alleviation of economic deprivation will afford low-income adults the ability to engage in protective behaviors and adapt to changing circumstances – key processes for resilience.
Resilience can be learned (PeConga et al., 2020), and therefore, universal interventions to foster resilience should be considered for supporting mental health throughout the pandemic. Another study found that keeping a routine and staying physically active were associated with lower mental distress (Shanahan et al., 2020); public health campaigns could highlight these behaviors. Phone apps focusing on mental well-being could promote cognitive processes such as “meaning-making,” which involves making sense of challenging events in a way that promotes growth (Walsh, 2020). Given that social support is a strong predictor of resilience (PeConga et al., 2020), regular engagement with others in a safe capacity (i.e., distanced if in-person) should be encouraged. Finally, advocates and researchers posit that enhancing personal resilience among historically marginalized populations is not enough, and must be coupled with systemic efforts to eradicate oppressive systems (Allen et al., 2019; Anderson, 2019). These longer-term efforts to address structural racism could include reinvesting in neighborhoods and partnering with community-based services, among others (Egede & Walker, 2020).
Some limitations of our study were that resilience was measured at a single time point, and we opted to categorize resilience scores, which may have led to loss of information. In addition, we measured resilience partway through the study period and did not collect longitudinal data to investigate changes in resilience over time, which does not capture the dynamic nature of resilience. That said, a previous study on mental distress during the pandemic found that resilience did not significantly vary between three samples collected at different time-points in March and April 2020 (Gilan et al., 2020). Regardless, our results should not be used to draw conclusions about a causal relationship between resilience and mental health. Our study is strengthened by the use of nationally-representative, longitudinal data spanning critical months of the COVID-19 pandemic, and the administration of widely used and validated measures of resilience (Smith et al., 2013) and mental distress (Kroenke et al., 2009).
Funding
The Understanding America Study is funded from several sources, including the Social Security Administration and the National Institute on Aging under grant 5U01AG054580. The survey that collected the mental health and COVID-19 related data used in this paper was funded by the Center for Economic and Social Research at USC and received substantial support from the Bill & Melinda Gates Foundation. This work was also supported by a RAPID grant from the National Science Foundation (grant number 2028683) and by a Capital Group COVID-19 Response Fund Grant. Ms. Riehm was supported by the National Institute of Mental Health (NIMH) Mental Health Services and Systems Training Program (5T32MH109436-03) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research.
Role of Funding Sources
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. For any questions or more information about the UAS, contact Tania Gutsche, Project and Panel Manager, Center for Economic and Social Research, University of Southern California, at tgutsche@usc.edu.
Author Contributions
Ms. Riehm conceptualized and designed the study, carried out data analyses, drafted the initial manuscript, and revised the manuscript. Dr. Thrul conceptualized and designed the study, assisted with interpreting results, and reviewed the manuscript. Ms. Brenneke assisted with the literature review, assisted with interpreting results, and reviewed the manuscript. Dr. Adams, Dr. Gilan, Dr. Kunzler, Dr. Lieb, Ms. Smail, Dr. Holingue, Dr. Stuart, and Dr. Kalb assisted with interpreting results and reviewing the manuscript. All authors approved the final manuscript as submitted.
Declaration of Competing Interests
The authors have no conflicts of interest to declare.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.12.071.
Appendix. Supplementary materials
References
- Aburn G., Gott M., Hoare K. What is resilience? An integrative review of the empirical literature. Journal of Advanced Nursing. 2016;72(5):980–1000. doi: 10.1111/jan.12888. [DOI] [PubMed] [Google Scholar]
- Allen A.M., Wang Y., Chae D.H., Price M.M., Powell W., Steed T.C., Rose Black A., Dhabhar F.S., Marquez-Magaña L., Woods-Giscombe C.L. Racial discrimination, the superwoman schema, and allostatic load: exploring an integrative stress-coping model among African American women. Annals of the New York Academy of Sciences. 2019;1457(1):104–127. doi: 10.1111/nyas.14188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson L.A. Rethinking Resilience Theory in African American Families: Fostering Positive Adaptations and Transformative Social Justice. Journal of Family Theory & Review. 2019;11(3):385–397. [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain and Behavior. 2020:e01964. doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmitorz A., Wenzel M., Stieglitz R.-D., Kunzler A., Bagusat C., Helmreich I., Gerlicher A., Kampa M., Kubiak T., Kalisch R., Lieb K., Tüscher O. Population-based validation of a German version of the Brief Resilience Scale. PloS one. 2018;13(2) doi: 10.1371/journal.pone.0192761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede L.E., Walker R.J. Structural Racism, Social Risk Factors, and Covid-19 — A Dangerous Convergence for Black Americans. New England Journal of Medicine. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilan D., Röthke N., Blessin M., Kunzler A., Stoffers-Winterling J., Müssig M., Yuen K.S.L., Tüscher O., Thrul J., Kreuter F., Sprengholz P., Betsch C., Stieglitz R.D., Lieb K. Psychomorbidity, resilience, and exacerbating and protective factors during the SARS-CoV-2-pandemic. Dtsch Arztebl International. 2020;117(38):625–632. doi: 10.3238/arztebl.2020.0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpman, M., Zuckerman, S., Gonzalez, D., & Kenney, G.M. (2020). The COVID-19 Pandemic is Straining Families’ Abilities to Afford Basic Needs. Urban Institute. https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_2.pdf.
- Kroenke K., Spitzer R.L., Williams J.B.W., Löwe B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Lowe S.R., Rhodes J.E., Waters M.C. Understanding Resilience and Other Trajectories of Psychological Distress: a Mixed-Methods Study of Low-Income Mothers Who Survived Hurricane Katrina. Current Psychology. 2015;34(3):537–550. doi: 10.1007/s12144-015-9362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini A.D. Heterogeneous mental health consequences of COVID-19: Costs and benefits. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S15–S16. doi: 10.1037/tra0000894. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire T.G., Miranda J. New Evidence Regarding Racial And Ethnic Disparities In Mental Health: Policy Implications. Health Affairs. 2008;27(2):393–403. doi: 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott S., Stone C., Huang C.-C., Leachman M., Bailey P., Aron-Dine A., Dean S., Pavetti L. CARES Act Includes Essential Measures to Respond to Public Health, Economic Crises, But More Will Be Needed. Center on Budget and Policy Priorities. 2020 https://www.jstor.org/stable/pdf/resrep23736.pdf [Google Scholar]
- PeConga E.K., Gauthier G.M., Holloway A., Walker R.S.W., Rosencrans P.L., Zoellner L.A., Bedard-Gilligan M. Resilience is spreading: Mental health within the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S47–S48. doi: 10.1037/tra0000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehm K.E., Holingue C., Kalb L.G., Bennett D., Kapteyn A., Jiang Q., Veldhuis C., Johnson R.M., Fallin M.D., Kreuter F., Stuart E.A., Thrul J. Associations Between Media Exposure and Mental Distress Among U.S. Adults at the Beginning of the COVID-19 Pandemic. American Journal of Preventive Medicine. 2020 doi: 10.1016/j.amepre.2020.06.008. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Ribeaud D., Eisner M. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine. 2020:1–10. doi: 10.1017/S003329172000241X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. International Journal of Behavioral Medicine. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Smith B.W., Epstein E.M., Ortiz J.A., Christopher P.J., Tooley E.M. Resilience in Children, Adolescents, and Adults. Springer; 2013. The foundations of resilience: what are the critical resources for bouncing back from stress? pp. 167–187. [Google Scholar]
- Walsh F. Loss and Resilience in the Time of COVID-19: Meaning Making, Hope, and Transcendence. Family Process. 2020;59(3):898–911. doi: 10.1111/famp.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.