Abstract
Background:
Platelet gene polymorphisms are associated with variable on-treatment platelet reactivity and vary by race. Whether differences in platelet reactivity and aspirin or ticagrelor exist between African-American and European-Americans remains poorly understood.
Methods:
Biological samples from three prior prospective antiplatelet challenge studies at the Duke Clinical Research Unit were used to compare platelet reactivity between African-American and European-American subjects. Platelet reactivity at baseline, on-aspirin, on-ticagrelor, and the treatment effect of aspirin or ticagrelor were compared between groups using an adjusted mixed effects model.
Results:
Compared with European-Americans (n=282; 50% female; mean±standard deviation age, 50±16), African-Americans (n=209; 67% female; age 48±12) had lower baseline platelet reactivity with platelet function analyzer-100 (PFA-100) (p<0.01) and with light transmission aggregometry (LTA) in response to arachidonic acid (AA), adenosine diphosphate (ADP), and epinephrine agonists (p<0.05). African-Americans had lower platelet reactivity on aspirin in response to ADP, epinephrine, and collagen (p<0.05) and on ticagrelor in response to AA, ADP, and collagen (p<0.05). The treatment effect of aspirin was greater in European-Americans with an AA agonist (p=0.002). Between-race differences with in vitro aspirin mirrored those seen in vivo. The treatment effect of ticagrelor was greater in European-Americans in response to ADP (p<0.05) but with collagen, the treatment effect was greater for African-Americans (p<0.05).
Conclusions:
Platelet reactivity was overall lower in African-Americans off-treatment, on aspirin, and on ticagrelor. European-Americans experienced greater platelet suppression on aspirin and on ticagrelor. The aspirin response difference in vivo and in vitro suggests a mechanism intrinsic to the platelet. Whether the absolute level of platelet reactivity or the degree of platelet suppression after treatment is more important for clinical outcomes is uncertain.
Keywords: antiplatelets, platelet reactivity, platelet aggregation, aspirin, ticagrelor, race, light transmission aggregometry, platelet function analyzer, African-American, European-American
INTRODUCTION
Antiplatelet therapy is a key component of acute coronary syndrome (ACS) treatment and secondary prevention of ischemic arterial diseases like myocardial infarction (MI) or stroke.1,2,3 There is a strong association between high on-treatment platelet reactivity (HTPR) and recurrent thrombotic events,4,5,6,7 and a link between low on-treatment platelet reactivity (LTPR) and increased bleeding events.8,9,10 Platelet signaling pathways independent of or partially dependent on antiplatelet drug targets allow residual on-treatment platelet aggregation.11,12,13,14A heightened aggregatory response to physiologic platelet agonists is reproducible,15 heritable,16,17 and heritability is greater among individuals of African than of European ancestry.18 Polymorphisms in platelet-related genes, which differ in prevalence by race, also influence response to therapy.19,20,21,22,23
Aspirin and ticagrelor are widely prescribed for patients of all races despite data based on trials including overwhelmingly men of European ancestry. In the Platelet Inhibition and Patient Outcomes (PLATO) trial, which demonstrated clinical superiority of ticagrelor over clopidogrel after ACS, the ticagrelor arm was comprised of 8,566 (91.8%) patients of European ancestry and just 115 (1.2%) patients of African ancestry.24 Despite more consistent and potent effects than earlier P2Y12-inhibitors, inter-individual variation in platelet reactivity exists after both loading25,26,27 and maintenance13,14 dosing of ticagrelor. In platelet function studies, response to ticagrelor varies after stimulation with collagen or epinephrine platelet agonists.28,29 Aspirin prevents platelet aggregation via cyclooxygenase-1 (COX-1) inhibition, however, COX-1-independent pathways of platelet aggregation–those stimulated by adenosine diphosphate (ADP), collagen, and epinephrine–can lead to HTPR despite aspirin compliance.12,17 Racial breakdown is not specified in landmark aspirin trials and thus representation is unknown.1,2,30,31
In the United States, although overall cardiovascular-related mortality has declined in recent decades, the rate for African-Americans has remained flat.32 The risk of recurrent thrombotic events is higher among individuals of African ancestry than among those of European ancestry.33,34 While reasons for this are likely multifactorial, the potential for differential response to antiplatelet medications by race has not been well studied. The goals of this study were to determine whether off- and on-treatment platelet reactivity differs between African-Americans and European-Americans and to assess whether the treatment response to aspirin or ticagrelor differs between these groups.
METHODS
Study Sample
This study analyzed whole blood and platelet rich plasma (PRP) samples from three prior prospective antiplatelet challenge studies conducted between 2009 and 2013 at the Duke Clinical Research Unit (Durham, NC, USA). Clinical and demographic data collected at the time of enrollment was compiled within each study. All subjects were studied under similar experimental protocols. Studies 1 and 3 have been previously described.35 The detailed design, methods, and inclusion/exclusion criteria from each original study are outlined in the Supplement. Study cohorts included patients with specific disease profiles: healthy volunteers, patients with known coronary artery disease (CAD), and patients with diabetes mellitus (DM). From the three original antiplatelet challenge studies, only self-reported African-American and European-American subjects were included in our analysis. This study was approved by the Duke University Health System Institutional Review Board.
Sample collection and antiplatelet medication adherence
PRP and whole blood samples were collected at each study visit. Subjects were asked to fast and to refrain from alcohol and intensive exercise on the day of testing and from tobacco during the preceding 24 hours. Study drug adherence was assured and verified through telephone calls, patient diaries recording the date and time of each medication dose, and a pill count at study visits.
Platelet function testing protocols
The protocols for platelet function testing using light transmission aggregometry (LTA) area under the curve (AUC) (Supplement Figure 2) including the addition of in vitro aspirin35 and the protocol for the platelet function analyzer-100 (PFA-100) (Siemens Healthineers, Erlangen, Germany)36 have been previously described and are detailed in the Supplement. For LTA AUC using PRP, the percent aggregation units were plotted over time in minutes (AU*min). Higher AUC values, in AU*min, reflect higher maximal and residual platelet aggregation. Agonists used in our study included: epinephrine 0.5, 1, and 10 micromoles/liter (μmol/L), collagen 2 and 5 microgram/milliliter (μg/ml), ADP 1, 5, and 10 μmol/L, and arachidonic acid (AA) 0.5 millimoles/liter (mmol/L). To normalize pharmacokinetic differences, baseline samples from study 3 were tested using LTA after the addition of in vitro aspirin at a concentration of 53 μmol/L, which exceeds the concentration achieved in vivo with a 325 mg aspirin dose. Whole blood samples were tested using PFA-100. Shorter closure time reflects greater platelet aggregation.
Statistical Analysis
Differences in baseline characteristics between African-American and European-American subjects were calculated using Fisher’s exact test for categorical variables and an unpaired t-test for continuous variables.
To determine whether platelet function varied by race, platelet reactivity was modeled as a function of race and the interaction of treatment and race. This linear mixed-effects model was fit using the maximum likelihood within each study cohort. Modeling was performed for each platelet agonist and concentration (including PFA-100). Additional subgroup analyses were performed to compare platelet reactivity at baseline versus in vitro aspirin-treated samples. The models controlled for age, hypertension, hyperlipidemia, coronary artery disease, diabetes, peripheral artery disease, sex (fixed effects) and patient (random effect) for each agonist.
The estimates from the linear mixed-effects model were used to calculate the pairwise differences of the least squares means for each study using the difflsmeans function in the lmerTest package for R version 3.3.2. The function metagen from the package meta was then used to return the fixed effects meta-analysis with inverse variance weights. All statistical testing was two-sided with α=0.05 and performed using R version 3.3.2.
RESULTS
Baseline Characteristics
Baseline characteristics are compared between European-American and African-American subjects in Table 1. African-American subjects were more likely to be female and to have diabetes. European-Americans were more likely to have coronary artery disease. Patients were adherent to the aspirin regimen: 6.2% of patients missed a single dose during the study, and no patients reported missing more than one dose.
Table 1.
Baseline Patient Characteristics
| European-American | African-American | p-value | |
|---|---|---|---|
| Age (years), mean ± SD | 50.2 (16.1) | 48.1 (11.8) | 0.11 |
| Female (n, %) | 140 (49.7%) | 140 (67%) | <0.01 |
| Coronary artery disease (n, %) | 41 (14.5%) | 6 (2.8%) | <0.01 |
| Diabetes (n, %) | 65 (23.0%) | 97 (46.1%) | <0.01 |
| Hypertension (n, %) | 69 (24.4%) | 68 (32.5%) | 0.05 |
| Hyperlipidemia (n, %) | 71 (25.2%) | 53 (25.4%) | 1.00 |
| Study 1 | 31 (10.9%) | 9 (4.3%) | <0.01 |
| Study 2 | 106 (37.6%) | 112 (53.5%) | 0.67 |
| Study 3 | 145 (51.4%) | 88 (42.1%) | 0.05 |
Continuous variables are displayed as mean ± standard deviation. Categorical variables are displayed as number of participants ‘n’ (percentage of group).
Abbreviations: SD, standard deviation
Platelet reactivity by race
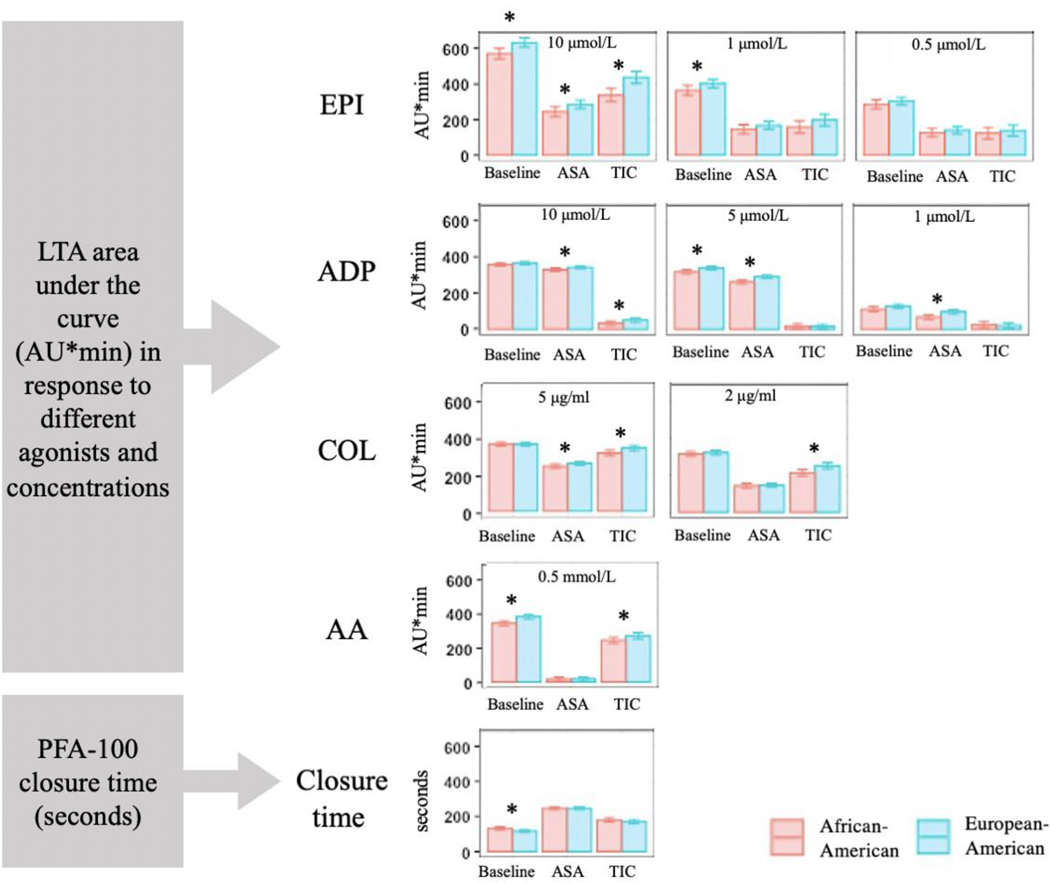
Platelet reactivity by race at baseline
Off-treatment, African-Americans had lower platelet reactivity compared with European-Americans in response to epinephrine, ADP, and AA with LTA and based on PFA-100 closure time (Figure 1, Supplement Table 1). Compared with European-Americans, platelet reactivity in African-American subjects was lower in response to epinephrine 1 μmol/L (95% confidence interval [CI]: −74.9, −2.1; p=0.03) and epinephrine 10 μmol/L (95% CI: −101.0, −23.6; p<0.01). African-American subjects also had lower platelet reactivity in response to ADP 5 μmol/L (95% CI: −34.5, −5.9; p<0.01) and AA 0.5 mmol/L (95% CI: −56.5, −18.0; p<0.01). There was a non-statistically significant trend towards lower platelet reactivity across remaining epinephrine, collagen, and ADP concentrations for African-American subjects compared with European-Americans. Correspondingly, PFA closure time was significantly longer, signifying lower platelet reactivity, in African-American compared with European-American subjects (95% CI: 4.0, 25.9; p<0.01).
Figure 1. Differences in platelet aggregation by race at baseline, after treatment with aspirin, and after treatment with ticagrelor.
Light transmission aggregometry values are expressed as mean area under the curve of light transmission aggregometry in percent aggregation units per minute minute (AU*min) with standard error bars. PFA-100 closure time is expressed in seconds. Significant differences are noted by an asterisk (*). Agonist concentrations are denoted above each frame and expressed as μmol/liter for epinephrine and adenosine diphosphate, as mmol/liter for arachidonic acid, and as μg/ml for collagen.
Abbreviations: AA, arachidonic acid; ADP, adenosine diphosphate; AU*min, percent aggregation units per minute; COL, collagen; EPI, epinephrine; LTA, light transmission aggregometry; μg/ml, microgram/milliliter; μmol/L, micromole/liter; mmol/L, millimole/liter; PFA-100, platelet function analyzer-100
Platelet reactivity by race on aspirin
Aspirin resulted in significant platelet suppression across all subjects assessed by both LTA and PFA-100 (Figure 1, Supplement Table 1).
On aspirin, African-American subjects had significantly lower platelet reactivity by LTA in response to all ADP concentrations and higher concentrations of epinephrine and collagen compared with European-Americans. Platelet reactivity was lower for African-American subjects on aspirin in response to ADP 1 μmol/L (95% CI: −46.8,−12.8; p<0.01), ADP 5 μmol/L (95% CI: −41.7, −15.0; p< 0.01), and ADP 10 μmol/L (95% CI: −25.1, −1.6; p=0.02). Platelet reactivity was also lower in African-Americans on aspirin in response to epinephrine 10 μmol/L (95% CI: −77.5, −4.9; p=0.02) and collagen 5 mg/ml (95% CI: −28.4, −1.1; p=0.03). There was no difference between groups on aspirin with respect to PFA-100 closure time.
Platelet reactivity by race on ticagrelor
Ticagrelor resulted in significant platelet suppression across all subjects assessed by both LTA and PFA-100 (Figure 1, Supplement Table 1).
On ticagrelor, African-American subjects had lower platelet reactivity by LTA in response to both collagen concentrations, AA, and higher concentrations of ADP and epinephrine compared with European-Americans. Platelet reactivity in African-Americans was significantly lower in response to collagen 2μg/ml (95% CI: −61.0, −14.7; p<0.01) and 5μg/ml (95% CI: −46.9, −6.1; p=0.01). Platelet reactivity was also lower for African-Americans in response to ADP 10 μmol/L (95% CI: −33.3, −2.4; p=0.02), epinephrine 10 μmol/L (95% CI: −151.1, −49.0; p<0.01), and in response to AA 0.5 μmol/L (95% CI: −50.4, −0.1; p=0.04). There was no difference between groups on ticagrelor with respect to PFA-100 closure time.
Platelet aggregation by race: treatment effect
Treatment effect of aspirin by race
The treatment effect of aspirin, or suppression of platelet reactivity from baseline, was greater in European-American subjects than African-American subjects (Figure 2, Supplement Table 2) with LTA in response to AA 0.5 mmol/L (95% CI: −53.5,−12.1; p<0.01). Compared with baseline, the change in PFA closure time on aspirin was significantly longer for European-Americans—indicating greater treatment effect—than for African-Americans (95% CI: 5.7, 28.3; p<0.01). The treatment effect of aspirin did not differ between African-American and European-American subjects with LTA in response to ADP, epinephrine, or collagen.
Figure 2. Treatment effect of aspirin and ticagrelor by race using light transmission aggregometry and standardized in comparison to baseline platelet aggregation for each agonist, which is set at 0.
Values are expressed as the change in area under the curve of light transmission aggregometry in percent aggregation units per minute (AU*min) from baseline. Standard error bars are displayed, and significant differences in treatment effect are noted by an asterisk (*). Agonist concentrations are denoted on the left and are expressed as μmol/liter for epinephrine and adenosine diphosphate, as mmol/liter for arachidonic acid, and as μg/ml for collagen.
Abbreviations: AA, arachidonic acid; ADP, adenosine diphosphate; AU*min, percent aggregation units per minute; COL, collagen; EPI, epinephrine; μg/ml, microgram/milliliter; μmol/L, micromole/liter; mmol/L, millimole/liter
Treatment effect of ticagrelor by race
The treatment effect of ticagrelor differed between African-American and European-American subjects with LTA in response to ADP and collagen (Figure 2, Supplement Table 2). The degree of platelet suppression on ticagrelor was greater in European-American compared with African-American subjects in response to ADP 1 μmol/L (95% CI: −42.0, −5.8; p<0.01) and 5 μmol/L (95% CI: −46.8, −5.0; p=0.01). The opposite treatment effect was seen with collagen. There was a greater degree of platelet suppression on ticagrelor in African-American compared with European-American subjects in response to collagen 2μg/ml (95% CI: −55.3, −2.0; p=0.03) and 5μg/ml (95% CI: −52.6, −4.4; p=0.02). There was no difference between groups on ticagrelor with respect to PFA-100 closure time change from baseline.
Intrinsic platelet response to aspirin
In vitro aspirin resulted in significant suppression of platelet aggregation compared with baseline platelet reactivity for both African-American and European-American subjects in response to all agonists (p<0.01). Following in vitro addition of aspirin, platelet reactivity was lower in response to epinephrine 0.5 μmol/L (95% CI: −24.9, −5.0; p<0.01), ADP 5 μmol/L (95% CI: −44.0, −9.4; p<0.01), and collagen 2 μg/ml (95% CI: −39.3, −1.3; p=0.03) in African-American subjects (n=88) compared with European-American subjects (n=145), mirroring the main effect seen in vivo (Figure 3, Supplement Table 3). The treatment effect of in vitro aspirin was greater in European-Americans compared with African-Americans in response to AA 0.5mmol/L (95% CI: −55.9, −17.1; p<0.01), mirroring the between-race treatment effect with in vivo aspirin.
Figure 3. Platelet response to in vitro aspirin exposure.
Values are expressed as mean area under the curve of light transmission aggregometry with standard error bars. Significant differences in aggregation between African-American and European-American subjects after the addition of in vitro aspirin are noted by an asterisk.
Abbreviations: AA, arachidonic acid; ADP, adenosine diphosphate; COL, collagen; EPI, epinephrine; μmol/L, micromole/liter; μg/ml, microgram/milliliter; mmol/L, millimole/liter.
DISCUSSION
The major findings of this study were that platelet reactivity in African-Americans was lower at baseline (off-treatment) and remained lower on-treatment with aspirin or ticagrelor compared with European-Americans. Whether overall platelet reactivity or the degree of platelet suppression is more important for thrombotic and bleeding events is not clear. For patients on P2Y12-receptor inhibitor therapy, elevated platelet reactivity in response to ADP has been consistently associated with adverse outcomes,9,10,37 however, clinical outcomes associated with a diminished treatment response to ticagrelor have not yet been studied. We demonstrated differences in epinephrine, collagen, arachidonic acid (AA), and ADP-induced platelet aggregation between African-American and European-American subjects, which to our knowledge have not been previously shown. A prior study evaluating platelet reactivity in subjects of African and European ancestry did not find differences in response to ADP, AA, and collagen-related peptide, however, only a single concentration of each agonist was used.19 In our study, differences in platelet reactivity between groups were agonist concentration-dependent; this may explain why between-race differences were not seen in prior studies using limited agonist concentrations.
Comparing our results to prior platelet studies in individuals of African and European ancestry
In our study, African-Americans had lower baseline platelet reactivity than European-Americans and this was consistent across two metrics: light transmission aggregometry (LTA) using platelet rich plasma (PRP) and platelet function analyzer-100 (PFA-100) using whole blood. This corroborates prior studies demonstrating lower off-treatment platelet aggregation in individuals of African ancestry compared with of European ancestry.18,38 Whether lower baseline platelet reactivity indicates an inherent protection from thrombotic events among individuals of African ancestry is unclear. Higher off-treatment levels of spontaneous aggregation (absence of agonist) and aggregation stimulated by AA, ADP, epinephrine, collagen, and thrombin were predictive of thrombotic events in some studies39,40,41 but not predictive in others.42,43
African-American subjects in our study exhibited lower overall platelet reactivity on aspirin or ticagrelor in response to the majority of agonists. On aspirin, African-Americans had lower platelet reactivity in response to all concentrations of ADP and the higher concentrations of epinephrine and collagen, but notably not in response to AA. On ticagrelor, African-Americans had lower overall platelet reactivity in response to the highest dose of ADP 10 μmol/L and in response to both collagen doses, AA, and epinephrine. A recent ticagrelor pharmacodynamics study corroborated this finding. In response to ADP 20 μmol/L, African-American patients with ACS exhibited lower maximal platelet aggregation measured by LTA at 4 and 8 hours after a ticagrelor loading dose and after 30 days of ticagrelor maintenance dosing compared with a historical cohort of patients of European ancestry.44 The treatment effect of ticagrelor, or the difference between off- and on-treatment platelet reactivity, was not reported.
Following treatment with aspirin or ticagrelor, respectively, absolute PFA-100 closure times no longer differed between African-Americans and European-Americans, likely due to the greater relative treatment response to aspirin and ticagrelor in European-Americans. Aspirin response was greater in European-Americans measured with both PFA-100 closure time and LTA in response to AA, the latter perhaps suggesting differences in baseline COX-1 activity between European-Americans and African-Americans. Bray et al. previously demonstrated lack of heritability for AA-induced platelet aggregation in whole blood and PRP in African-Americans,18 which may indicate a less predictable response to aspirin. In our study, the between-race differences in on-treatment platelet reactivity and treatment response with in vitro aspirin mirrored those seen in vivo, suggesting a mechanism intrinsic to the platelet.
The treatment effect of ticagrelor differed by race in a way that was agonist-dependent. Treatment response to ticagrelor was greater in African-Americans compared with European-Americans with both concentrations of collagen. Bray et al. previously showed heritability of collagen-induced platelet aggregation in PRP among African-American but not European-American subjects.18 With the two higher concentrations of ADP, however, ticagrelor’s antiplatelet effect was greater in European-Americans than African-Americans. This is somewhat surprising given that ticagrelor is an allosteric non-competitive inhibitor of the ADP-P2Y12-receptor and theoretically ADP at any concentration should not significantly alter its effect.28,29,45 Platelet suppression by ticagrelor does, however, depend on intact association with receptors and a sufficient concentration of ticagrelor to occupy receptors; deficiencies in either area could lead to variable effects.47 The ability of ADP to influence P2Y12-independent pathways is possible as is the potential for biased signaling affecting downstream G-protein coupled receptors (GPCR).46,47
Differences in clinical outcomes between African-Americans and European-Americans
The risk of recurrent thrombotic events, such as myocardial infarction or stroke are higher among patients of African ancestry than European ancestry.33,34 Despite controlling for demographic, socioeconomic, neighborhood, and clinical factors, African-American race is an independent predictor of increased mortality in patients with CAD,48 suggesting that additional factors–including genetic influences on disease progression or response to therapies–may account for this difference. In a recent epidemiologic study, low-dose aspirin use was associated with decreased risk of ischemic cardiac death among patients of European ancestry but not in those of African ancestry.49 Another study showed that, despite higher rates of compliance with dual antiplatelet medications among African-American patients after drug eluting stent placement, African-American race was strongly associated with stent thrombosis after adjusting for comorbid conditions and socioeconomic status.50 Large-scale studies assessing cardiovascular outcomes in patients of different racial ancestry on ticagrelor have not been done. While there is evidence for increased bleeding risk in patients of Asian ancestry on standard doses of antiplatelet medications, the data on bleeding risk in other racial groups, including African-American patients, is lacking.51 Further research in this area is warranted.
Possible mechanisms for differences in platelet reactivity and response to therapy
The differential response to aspirin or ticagrelor between African-Americans and European-Americans may be due to underlying genetic differences. Different allele frequencies and linkage disequilibrium patterns between populations of African and European ancestry have been identified and genetic variations specifically affecting platelet function have also been described.39,52,53, A single nucleotide polymorphism in the protease-activated receptor 4 (PAR4), for example, which is more prevalent among individuals of African ancestry54 results in a relative resistance to antiplatelet therapies targeting COX-1 and the P2Y12 receptor.50 Single nucleotide polymorphisms in the platelet endothelial aggregation receptor 1 (PEAR1) gene were associated with altered platelet aggregation stimulated by epinephrine, collagen, and ADP, suggesting that PEAR1 may be a common downstream signaling pathway for all three agonists.38,55,56 Prior studies have demonstrated heritability of epinephrine-induced,16,18,57 collagen-induced,18 and ADP-induced18 platelet aggregation. Although several specific genetic polymorphisms, such as those involving PAR4 and PEAR1, have been identified, genetic variants discovered to date account for only a small proportion of this heritability difference.39
We demonstrated agonist-specific differences in epinephrine, collagen, AA, and ADP-induced platelet aggregation between African-Americans and European-Americans. Platelet surface receptors and key components of intracellular signaling pathways stimulated by these agonists could be examined as potential sources of platelet function variation in future studies. The G protein beta3 subunit 825T allele, which is more prevalent in individuals of African ancestry,58 is associated with a hyperreactive response to agonists acting through GPCR, including ADP and epinephrine.59,60,61 Polymorphisms of genes involved in collagen-mediated platelet activation, GP1BA and ITGA2, are associated with increased thrombotic risk and differ in prevalence by race.62 Elevated levels of von Willebrand factor (vWF), which aids in collagen-platelet binding, is an independent risk factor for arterial thrombotic events63 and individuals of African ancestry exhibit higher levels of circulating vWF antigen than individuals of European ancestry.64 Individuals of African ancestry also possess a higher number of platelet activation markers as measured by flow cytometry65 and have greater platelet-fibrin clot strength than those of European ancestry.66 Thus it is plausible that genetic or pathophysiologic differences in platelet function, response to antiplatelet therapies, and other hematologic variables affecting thrombosis may, at least in part, contribute to clinical outcome disparities.
Benefits and pitfalls of evaluating racial subgroups
We acknowledge that “race” is a non-precise term referring to a group of people sharing common social and phenotypic characteristics. Commonly used racial classifications such as African-American and European-American are insufficient descriptions of human genetic structure and do not effectively summarize genetic variation between and within subgroups of the population.67 However, many genetic markers including pharmacogenetic polymorphisms are strongly associated with ancestral continent of origin and self-identified racial groups.68,69 Differences in treatment response by self-identified race has resulted in tailored cardiovascular pharmacotherapies for African-Americans with hypertension and with heart failure.70,71 One-fifth of new pharmaceuticals approved between 2008 and 2013, including ticagrelor, demonstrated racial differences in pharmacokinetics, efficacy, dosing, safety, or pharmacogenetics.72,73 Ignoring the existence of racial differences in allele frequencies, some of which contribute to disease or treatment response, may reduce treatment benefits for non-European populations.
Future directions
There remains much to be understood about the nuances of aspirin or ticagrelor response in specific subgroups of patients. A better understanding of the genetic, heritable factors, and social determinants influencing platelet function is important for personalization of antiplatelet therapies. Our hope is that the identification of agonist-specific differences in platelet reactivity between African-American and European-American subjects will contribute to the broader goal of precision-based practice of medicine in several ways. First, our study could serve as a starting point for future mechanistic studies focusing on candidate genes or gene expression profiles specific to these platelet activation and aggregation pathways. Agonist-dependent differences in treatment effects, particularly when present across multiple concentrations of an agonist, may point to race-specific variation in pathways of platelet activation and aggregation stimulated by these agonists. Key components of these pathways such as transmembrane receptors and intracellular enzymes could be targeted as future areas of investigation. In addition, racial diversity in genome-wide association studies and other large-scale genomics data sets and biorepositories are critical.
Second, we highlight current gaps in knowledge regarding the clinical impact of differential response to aspirin or ticagrelor in African-American and European-American subjects, as shown in our analyses. These knowledge gaps could be addressed by clinical and epidemiological studies focusing on bleeding and thrombotic risks among African-American and European-American individuals taking aspirin or ticagrelor. Finally, our findings of between-race differences in response to aspirin or ticagrelor in an experimental setting support the need for increased racial diversity in clinical trials of anti-platelet therapies to better understand the safety and efficacy of these drugs in all patients. Continued attention to between-race differences in pharmacokinetics and pharmacodynamics will be essential to advancing our understanding of cardiovascular disease treatment and achieving the goal of personalized medical therapy in patients of different racial backgrounds.
Limitations
We acknowledge several limitations with respect to this study. We combined data from three prior antiplatelet challenge studies comprised of patient cohorts with different comorbidity profiles. Although centrally developed protocols were used, each study was analyzed individually, and results were combined using meta-analysis our approach may have increased heterogeneity in results. Race, ancestry, and lineage are complex constructs in humans and gene pooling can be quite different within self-identified racial groups. While the observed between-race differences seen in this study may have been underestimated or diluted, on the other hand heterogeneity may have been compounded by combining three distinct studies. In our primary analysis, we did not account for menstrual cycles or whether female patients were taking hormonal contraception, which may influence the pharmacokinetics of aspirin and ticagrelor. While patients typically take antiplatelet agents for months or years, we evaluated aspirin and ticagrelor for two to four weeks. We do not know the extent to which the between-race differences identified in our study could change over time. Additionally, more than half of the aspirin exposures were at a dose of 325mg/day while the rest of the exposures were 81mg/day. Therefore, the extent to which our findings extend to low-dose aspirin are not known. Although we evaluated and adjusted for potential confounding variables in our analyses, we could not exclude residual confounding by imperfectly measured and unmeasured factors.
Conclusion
In conclusion, we have identified agonist-specific differences in platelet response to aspirin and ticagrelor between African-Americans and European-Americans. Although absolute platelet reactivity levels were lower before and after treatment with aspirin and with ticagrelor in African-Americans compared with European-Americans, the treatment effect of both aspirin and ticagrelor was more profound in European-American subjects. While this may suggest that aspirin and ticagrelor provide less antithrombotic protection in African-Americans, it is uncertain whether the absolute level of platelet reactivity or the treatment response is more important in terms of clinical outcomes. In addition, the race-treatment interactions seen with different agonists in our study could point to genetic or pathophysiologic differences related to the agonist and its associated signaling pathways. Identifying where in the platelet signaling cascade racial differences emerge will further aid in understanding why individuals of different racial ancestry respond differently to antiplatelet therapies. Clinically relevant differences in on-treatment platelet reactivity and treatment response with respect to thrombosis and bleeding warrants further study.
Supplementary Material
KEY POINTS:
Platelet aggregation at baseline and in response to aspirin and ticagrelor differ between African-American and European-American subjects.
Whether the absolute level of platelet aggregation or the change in platelet aggregation in response to treatment is more important for drug response and clinical outcomes is uncertain.
Agonist-dependent differences in treatment effects may point to race-specific variation in pathways of platelet activation and aggregation stimulated by these agonists.
Clinical and epidemiological studies evaluating racial differences in bleeding and thrombotic outcomes on ticagrelor or aspirin are lacking.
Potential mechanisms underlying the differences between African-American and European-American subjects in off- and on-treatment platelet reactivity and in the treatment response to aspirin or ticagrelor warrant further study.
Acknowledgements:
No other persons besides the authors have made substantial contributions to this manuscript.
Funding: This research was supported by the National Institutes of Health R01HL118049 and National Center for Research Resources, a component of the NIH 5UL1RR024128 grant (Dr. Voora); the National Institutes of General Medical Sciences 5RC1GM091083 grant (Dr. Ginsburg); the Centers for Disease Control and Prevention grant 5U01DD000014 (Dr. Ortel), and the 2012/0003R grant from Duke-National University Singapore (Dr. Ru San)
ABBREVIATIONS:
- AA
arachidonic acid
- AUC
area under the curve
- AU*min
percent aggregation units per minute
- ADP
adenosine diphosphate
- CAD
coronary artery disease
- COL
collagen
- COX-1
cyclooxygenase-1
- DM
diabetes mellitus
- EPI
epinephrine
- HTPR
high on-treatment platelet reactivity
- LTA
light transmission aggregometry
- LTPR
low on-treatment platelet reactivity
- PFA
platelet function analyzer
- PLATO
Platelet Inhibition and Patient Outcomes trial
- PRP
platelet rich plasma
- vWF
von Willebrand factor
Footnotes
Disclosures: The authors have no relevant disclosures.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Patrono C, Morais J, Baigent C, et al. Antiplatelet Agents for the Treatment and Prevention of Coronary Atherothrombosis. J Am Coll Cardiol. 2017;70(14):1760–1776. [DOI] [PubMed] [Google Scholar]
- 2.Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet. 1988;2(8607):349–360. [PubMed] [Google Scholar]
- 3.Antithrombotic Trialists C. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013;382(9892):614–623. [DOI] [PubMed] [Google Scholar]
- 5.Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ. A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol. 2003;41(6):961–965. [DOI] [PubMed] [Google Scholar]
- 6.Wenaweser P, Dorffler-Melly J, Imboden K, et al. Stent thrombosis is associated with an impaired response to antiplatelet therapy. J Am Coll Cardiol. 2005;45(11):1748–1752. [DOI] [PubMed] [Google Scholar]
- 7.Snoep JD, Hovens MM, Eikenboom JC, van der Bom JG, Huisman MV. Association of laboratory-defined aspirin resistance with a higher risk of recurrent cardiovascular events: a systematic review and meta-analysis. Arch Intern Med. 2007;167(15):1593–1599. [DOI] [PubMed] [Google Scholar]
- 8.Cuisset T, Cayla G, Frere C, et al. Predictive value of post-treatment platelet reactivity for occurrence of post-discharge bleeding after non-ST elevation acute coronary syndrome. Shifting from antiplatelet resistance to bleeding risk assessment? EuroIntervention. 2009;5(3):325–329. [DOI] [PubMed] [Google Scholar]
- 9.Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013;62(24):2261–2273 [DOI] [PubMed] [Google Scholar]
- 10.Aradi D, Kirtane A, Bonello L, et al. Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J. 2015;36(27):1762–1771. [DOI] [PubMed] [Google Scholar]
- 11.Faraday N, Yanek LR, Mathias R, et al. Heritability of platelet responsiveness to aspirin in activation pathways directly and indirectly related to cyclooxygenase-1. Circulation. 2007;115(19):2490–2496. [DOI] [PubMed] [Google Scholar]
- 12.Frelinger AL 3rd, Furman MI, Linden MD, et al. Residual arachidonic acid-induced platelet activation via an adenosine diphosphate-dependent but cyclooxygenase-1- and cyclooxygenase-2-independent pathway: a 700-patient study of aspirin resistance. Circulation. 2006;113(25):2888–2896. [DOI] [PubMed] [Google Scholar]
- 13.Verdoia M, Sartori C, Pergolini P, et al. Prevalence and predictors of high-on treatment platelet reactivity with ticagrelor in ACS patients undergoing stent implantation. Vascul Pharmacol. 2016;77:48–53. [DOI] [PubMed] [Google Scholar]
- 14.Siller-Matula JM, Akca B, Neunteufl T, et al. Inter-patient variability of platelet reactivity in patients treated with prasugrel and ticagrelor. Platelets. 2016;27(4):373–377. [DOI] [PubMed] [Google Scholar]
- 15.Yee DL, Sun CW, Bergeron AL, Dong JF, Bray PF. Aggregometry detects platelet hyperreactivity in healthy individuals. Blood. 2005;106(8):2723–2729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaxiola B, Friedl W, Propping P. Epinephrine-induced platelet aggregation. A twin study. Clin Genet. 1984;26(6):543–548. [DOI] [PubMed] [Google Scholar]
- 17.O’Donnell CJ, Larson MG, Feng D, et al. Genetic and environmental contributions to platelet aggregation: the Framingham heart study. Circulation. 2001;103(25):3051–3056. [DOI] [PubMed] [Google Scholar]
- 18.Bray PF, Mathias RA, Faraday N, et al. Heritability of platelet function in families with premature coronary artery disease. J Thromb Haemost. 2007;5(8):1617–1623. [DOI] [PubMed] [Google Scholar]
- 19.Edelstein LC, Simon LM, Montoya RT, et al. Racial differences in human platelet PAR4 reactivity reflect expression of PCTP and miR-376c. Nat Med. 2013;19(12):1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim HO, Jin Y, Kickler TS, Blakemore K, Kwon OH, Bray PF. Gene frequencies of the five major human platelet antigens in African-American, white, and Korean populations. Transfusion. 1995;35(10):863–867. [DOI] [PubMed] [Google Scholar]
- 21.Ramsey G, Salamon DJ. Frequency of PLA1 in blacks. Transfusion. 1986;26(6):531–532. [DOI] [PubMed] [Google Scholar]
- 22.Ulrich CM, Carlson CS, Sibert J, et al. Thromboxane synthase (TBXAS1) polymorphisms in African-American and Caucasian populations: evidence for selective pressure. Hum Mutat. 2005;26(4):394–395. [DOI] [PubMed] [Google Scholar]
- 23.Weng Z, Li X, Li Y, Lin J, Peng F, Niu W. The association of four common polymorphisms from four candidate genes (COX-1, COX-2, ITGA2B, ITGA2) with aspirin insensitivity: a meta-analysis. PLoS One. 2013;8(11):e78093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–1057. [DOI] [PubMed] [Google Scholar]
- 25.Alexopoulos D, Xanthopoulou I, Gkizas V, et al. Randomized assessment of ticagrelor versus prasugrel antiplatelet effects in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2012;5(6):797–804. [DOI] [PubMed] [Google Scholar]
- 26.Parodi G, Valenti R, Bellandi B, et al. Comparison of prasugrel and ticagrelor loading doses in ST-segment elevation myocardial infarction patients: RAPID (Rapid Activity of Platelet Inhibitor Drugs) primary PCI study. J Am Coll Cardiol. 2013;61(15):1601–1606. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim K, Christoph M, Schmeinck S, et al. High rates of prasugrel and ticagrelor non-responder in patients treated with therapeutic hypothermia after cardiac arrest. Resuscitation. 2014;85(5):649–656. [DOI] [PubMed] [Google Scholar]
- 28.VANG JJ, Nilsson L, Berntsson P, et al. Ticagrelor binds to human P2Y(12) independently from ADP but antagonizes ADP-induced receptor signaling and platelet aggregation. J Thromb Haemost. 2009;7(9):1556–1565. [DOI] [PubMed] [Google Scholar]
- 29.Wadowski PP, Eichelberger B, Kopp CW, et al. Disaggregation Following Agonist-Induced Platelet Activation in Patients on Dual Antiplatelet Therapy. J Cardiovasc Transl Res. 2017;10(4):359–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elwood PC, Cochrane AL, Burr ML, et al. A randomized controlled trial of acetyl salicylic acid in the secondary prevention of mortality from myocardial infarction. Br Med J. 1974;1(5905):436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. The RISC Group. Lancet. 1990;336(8719):827–830. [PubMed] [Google Scholar]
- 32.Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61(22):2249–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics−−2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. [DOI] [PubMed] [Google Scholar]
- 34.Albright KC, Huang L, Blackburn J, et al. Racial differences in recurrent ischemic stroke risk and recurrent stroke case fatality. Neurology. 2018;91(19):e1741–e1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voora D, Ortel TL, Lucas JE, et al. Time-dependent changes in non-COX-1-dependent platelet function with daily aspirin therapy. J Thromb Thrombolysis. 2012;33(3):246–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ortel TL, James AH, Thames EH, et al. Assessment of primary hemostasis by PFA-100 analysis in a tertiary care center. Thromb Haemost. 2000;84(1):93–97. [PubMed] [Google Scholar]
- 37.Valenti R, Cantini G, Marcucci R, et al. Prognostic impact of high residual platelet reactivity after chronic total occlusion percutaneous coronary intervention in patients with diabetes mellitus. Int J Cardiol. 2015; 201: 561–567. [DOI] [PubMed] [Google Scholar]
- 38.Meade TW, Vickers MV, Thompson SG, Stirling Y, Haines AP, Miller GJ. Epidemiological characteristics of platelet aggregability. Br Med J (Clin Res Ed). 1985;290(6466):428–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trip MD, Cats VM, van Capelle FJ, Vreeken J. Platelet hyperreactivity and prognosis in survivors of myocardial infarction. N Engl J Med. 1990;322(22):1549–1554. [DOI] [PubMed] [Google Scholar]
- 40.Thaulow E, Erikssen J, Sandvik L, Stormorken H, Cohn PF. Blood platelet count and function are related to total and cardiovascular death in apparently healthy men. Circulation. 1991;84(2):613–617. [DOI] [PubMed] [Google Scholar]
- 41.Terres W, Lund GK, Hubner A, Ehlert A, Reuter H, Hamm CW. Endogenous tissue plasminogen activator and platelet reactivity as risk factors for reocclusion after recanalization of chronic total coronary occlusions. Am Heart J. 1995;130(4):711–716. [DOI] [PubMed] [Google Scholar]
- 42.Elwood PC, Renaud S, Beswick AD, O’Brien JR, Sweetnam PM. Platelet aggregation and incident ischaemic heart disease in the Caerphilly cohort. Heart. 1998;80(6):578–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Meade TW, Cooper JA, Miller GJ. Platelet counts and aggregation measures in the incidence of ischaemic heart disease (IHD). Thromb Haemost. 1997;78(2):926–929. [PubMed] [Google Scholar]
- 44.Gaglia MA Jr., Lipinski MJ, Lhermusier T, et al. Comparison of Platelet Reactivity in Black Versus White Patients With Acute Coronary Syndromes After Treatment With Ticagrelor. Am J Cardiol. 2017;119(8):1135–1140. [DOI] [PubMed] [Google Scholar]
- 45.Husted S, van Giezen JJ. Ticagrelor: the first reversibly binding oral P2Y1P2Y12 receptor antagonist. Cardiovasc Ther. 2009;27(4):259–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao P, Metcalf M, Bunnett NW. Biased signaling of protease-activated receptors. Front Endocrinol (Lausanne). 2014;5:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tourdot BE, Conaway S, Niisuke K, Edelstein LC, Bray PF, Holinstat M. Mechanism of race-dependent platelet activation through the protease-activated receptor-4 and Gq signaling axis. Arterioscler Thromb Vasc Biol. 2014;34(12):2644–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas KL, Honeycutt E, Shaw LK, Peterson ED. Racial differences in long-term survival among patients with coronary artery disease. Am Heart J. 2010;160(4):744–751. [DOI] [PubMed] [Google Scholar]
- 49.Fernandez-Jimenez R, Wang TJ, Fuster V, Blot WJ. Low-Dose Aspirin for Primary Prevention of Cardiovascular Disease: Use Patterns and Impact Across Race and Ethnicity in the Southern Community Cohort Study. J Am Heart Assoc. 2019;8(24):e013404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Collins SD, Torguson R, Gaglia MA Jr., et al. Does black ethnicity influence the development of stent thrombosis in the drug-eluting stent era? Circulation. 2010;122(11):1085–1090. [DOI] [PubMed] [Google Scholar]
- 51.Urban P, Mehran R, Colleran R, et al. Defining High Bleeding Risk in Patients Undergoing Percutaneous Coronary Intervention. Circulation. 2019;140(3):240–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Casto AM, Feldman MW. Genome-wide association study SNPs in the human genome diversity project populations: does selection affect unlinked SNPs with shared trait associations? PLoS Genet. 2011;7(1):e1001266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tourdot BE, Stoveken H, Trumbo D, et al. Genetic Variant in Human PAR (Protease-Activated Receptor) 4 Enhances Thrombus Formation Resulting in Resistance to Antiplatelet Therapeutics. Arterioscler Thromb Vasc Biol. 2018;38(7):1632–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Edelstein LC, Simon LM, Lindsay CR, et al. Common variants in the human platelet PAR4 thrombin receptor alter platelet function and differ by race. Blood. 2014;124(23):3450–3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Faraday N, Yanek LR, Yang XP, et al. Identification of a specific intronic PEAR1 gene variant associated with greater platelet aggregability and protein expression. Blood. 2011;118(12):3367–3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Qayyum R, Becker LC, Becker DM, et al. Genome-wide association study of platelet aggregation in African-Americans. BMC Genet. 2015;16:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kambayashi J, Shinoki N, Nakamura T, et al. Prevalence of impaired responsiveness to epinephrine in platelets among Japanese. Thromb Res. 1996;81(1):85–90. [DOI] [PubMed] [Google Scholar]
- 58.Siffert W, Forster P, Jockel KH, et al. Worldwide ethnic distribution of the G protein beta3 subunit 825T allele and its association with obesity in European-American, Chinese, and Black African individuals. J Am Soc Nephrol. 1999;10(9):1921–1930. [DOI] [PubMed] [Google Scholar]
- 59.Dusse F, Frey UH, Bilalic A, et al. The GNB3 C825T polymorphism influences platelet aggregation in human whole blood. Pharmacogenet Genomics. 2012;22(1):43–49. [DOI] [PubMed] [Google Scholar]
- 60.Yee DL, Bergeron AL, Sun CW, Dong JF, Bray PF. Platelet hyperreactivity generalizes to multiple forms of stimulation. J Thromb Haemost. 2006;4(9):2043–2050. [DOI] [PubMed] [Google Scholar]
- 61.Naber C, Hermann BL, Vietzke D, et al. Enhanced epinephrine-induced platelet aggregation in individuals carrying the G protein beta3 subunit 825T allele. FEBS Lett. 2000;484(3):199–201. [DOI] [PubMed] [Google Scholar]
- 62.Strisciuglio T, Franco D, Di Gioia G, et al. Impact of genetic polymorphisms on platelet function and response to anti platelet drugs. Cardiovasc Diagn Ther. 2018;8(5):610–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morange PE, Simon C, Alessi MC, et al. Endothelial cell markers and the risk of coronary heart disease: the Prospective Epidemiological Study of Myocardial Infarction (PRIME) study. Circulation. 2004;109(11):1343–1348. [DOI] [PubMed] [Google Scholar]
- 64.Conlan MG, Folsom AR, Finch A, et al. Associations of factor VIII and von Willebrand factor with age, race, sex, and risk factors for atherosclerosis. The Atherosclerosis Risk in Communities (ARIC) Study. Thromb Haemost. 1993;70(3):380–385. [PubMed] [Google Scholar]
- 65.Folsom AR, Aleksic N, Sanhueza A, Boerwinkle E. Risk factor correlates of platelet and leukocyte markers assessed by flow cytometry in a population-based sample. Atherosclerosis. 2009;205(1):272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lev EI, Bliden KP, Jeong YH, et al. Influence of race and sex on thrombogenicity in a large cohort of coronary artery disease patients. J Am Heart Assoc. 2014;3(5):e001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wilson JF, Weale ME, Smith AC, et al. Population genetic structure of variable drug response. Nat Genet. 2001;29(3):265–269. [DOI] [PubMed] [Google Scholar]
- 68.Rosenberg NA, Pritchard JK, Weber JL, et al. Genetic structure of human populations. Science. 2002;298(5602):2381–2385. [DOI] [PubMed] [Google Scholar]
- 69.Tang H, Quertermous T, Rodriguez B, et al. Genetic structure, self-identified race/ethnicity, and confounding in case-control association studies. Am J Hum Genet. 2005;76(2):268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Carson P, Ziesche S, Johnson G, Cohn JN. Racial differences in response to therapy for heart failure: analysis of the vasodilator-heart failure trials. Vasodilator-Heart Failure Trial Study Group. J Card Fail. 1999;5(3):178–187. [DOI] [PubMed] [Google Scholar]
- 71.Jamerson K, DeQuattro V. The impact of ethnicity on response to antihypertensive therapy. Am J Med. 1996;101(3A):22S–32S. [DOI] [PubMed] [Google Scholar]
- 72.Ramamoorthy A, Pacanowski MA, Bull J, Zhang L. Racial/ethnic differences in drug disposition and response: review of recently approved drugs. Clin Pharmacol Ther. 2015;97(3):263–273. [DOI] [PubMed] [Google Scholar]
- 73.Teng R, Butler K. Pharmacokinetics, pharmacodynamics, and tolerability of single and multiple doses of ticagrelor in Japanese and European-American volunteers. Int J Clin Pharmacol Ther. 2014;52(6):478–491. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.