Abstract
Background:
Despite medicalization and legalization of marijuana use, factors influencing demand for marijuana among persons living with HIV (PLWH) are incompletely understood. This knowledge gap undermines effective clinical management and policies. This study used demand curve simulation methods to address these issues.
Methods:
Marijuana-using PLWH (N=119) completed experimental tasks to simulate amount of marijuana purchasing/use across different costs (money or time), and likelihood of reselling marijuana or marijuana therapeutic-use registration card in relation to profits. Additional simulations assessed purchasing of marijuana relative to other drug and non-drug goods.
Results:
Simulated marijuana use decreased as money and time costs increased. Consumption was greater for participants with more severe Cannabis Use Disorder (CUD) and anxiety, intermediate pain levels, and past 90-day opioid use. Whereas few participants chose to sell their registration card, marijuana resale (diversion) steeply increased with profit. Likelihood of seeking marijuana therapeutic-use certification decreased in relation to registration card money cost, having to visit more physicians to get a signature, and delay to receiving the card, and increased with duration of certification. Participants who reported recent opioid use were more likely to seek certification. Consumption of several commodities assessed was independent of marijuana.
Conclusions:
Simulated marijuana use was related to participants’ clinical profile (CUD, anxiety and pain symptoms, recent opioid use), and unrelated to purchasing other goods. Likelihood of seeking marijuana therapeutic-use registration was affected by several types of costs and recent opioid use. Participants were unlikely to divert registration cards. We discuss clinical and policy implications of these findings.
Keywords: HIV, marijuana, demand curve analysis, cannabis use disorder, pain, opioid
1. Introduction
In U.S. states that have decriminalized marijuana consumption, therapeutic use is allowed for debilitating diseases including HIV/AIDS and related signs/symptoms, e.g., cachexia/wasting, chronic pain, and nausea. Marijuana use is common among persons living with HIV (PLWH), with past-year prevalence of 34% in a nationally representative sample (Shiau et al., 2017) and similar among clinical samples (Hartzler et al., 2017; Parsons et al., 2014). PLWH report various reasons for using marijuana, some not accepted under medicalization including psychiatric symptom relief (Cinti, 2009; Ogborne et al., 2000; Prentiss et al., 2004; Swift et al., 2005; Ware et al., 2003; Woolridge et al., 2005). Heavier marijuana use by PLWH has been associated with less antiretroviral medication adherence (de Jong et al., 2005; Gonzalez et al., 2011; Gross et al., 2016). Thus, obtaining data on price-sensitive marijuana use among PLWH may inform clinical care by balancing therapeutic benefits vs. harms of marijuana use.
Operant behavioral economics (Hantula, 2017) offers a framework (consumer demand theory) and method (demand curve analysis) for evaluating effects of drug prices, concurrent goods, and income on drug demand (Acuff et al., 2020; Bickel et al., 2014). Studies that used hypothetical purchase tasks to simulate marijuana demand in healthy, non-patient samples (Amlung et al., 2019; Aston et al., 2015; Collins et al., 2014; Greenwald, 2008; Strickland et al., 2017; Vincent et al., 2017) observed own price-elastic demand for marijuana, i.e., consumption decreased as marijuana unit price increased. Experimental demand intensity (marijuana consumption at near-zero prices) positively correlated with naturalistic marijuana use (Aston et al., 2015; Collins et al., 20114) and DSM-IV cannabis dependence symptoms (Aston et al., 2015; Strickland et al., 2017). Finally, in a procedure where participants could choose between legal and illegal marijuana, legal marijuana was a superior good to illegal marijuana (Amlung et al., 2019).
Pacula and Lundberg (2014) theorized that marijuana-using subgroups (e.g., initiates, low-level users, heavier users, quitters) should vary in sensitivity to marijuana prices. We posit that, among PLWH, additional individual differences beyond baseline marijuana use (e.g., psychiatric symptoms, pain) could also modulate price-sensitivity and/or intensity of marijuana demand. Thus, we evaluated marijuana demand relative to several factors, including severity of cannabis use disorder (CUD), anxiety, pain, and opioid use, which have not been systematically studied in healthy marijuana users. Our clinically-motivated approach may be useful because demand for marijuana (and other substances) among PLWH - a population with higher prevalence and severity of comorbid conditions, who may use marijuana therapeutically - may differ from the general population.
The present study used hypothetical purchase tasks with marijuana-using PLWH to determine: (1) marijuana demand and relationship to baseline factors (e.g., severity of CUD, severity of pain and psychiatric symptoms); (2) diversion potential of marijuana and marijuana therapeutic-use registration cards, i.e. likelihood of illegally reselling these commodities in relation to monetary profit; (3) likelihood of seeking marijuana therapeutic-use certification; and (4) whether consumption of marijuana and other goods are related. We hypothesized: (1) marijuana demand would be sensitive to price increases, and demand intensity would be higher among PLWH with greater severity of CUD and HIV-related symptoms; (2) marijuana would be diverted more than registration cards; (3) participation in therapeutic-use certification would be price-sensitive; and (4) marijuana and other commodities would be independent goods.
2. Methods
2.1. Study context
The local IRB approved all procedures. The study was conducted according to the Declaration of Helsinki and registered at ClinicalTrials.gov (NCT01536899). Participants provided informed consent. All participants were adult (≥18 years old) PLWH enrolled in a treatment program that provides comprehensive HIV primary and specialty care to an income-poor, inner-city population. Study visits were completed from May 2012 to April 2015, when marijuana therapeutic use, but not recreational use, was legal.
2.2. Participant selection
PLWH in the treatment program were recruited via clinic-based advertisements and contact with clinic staff for a study requiring a baseline visit (this report) and follow-up visits 3, 6, 9 and 12 months later (reported elsewhere).
Participants submitted a urine sample that was tested for cannabinoids, opioids, methadone, cocaine, benzodiazepines, amphetamines, and barbiturates; for inclusion, the sample had to be positive for THC (>50 ng/ml) and negative for methadone, amphetamines and barbiturates (<300 ng/ml). Participants also had to provide an alcohol-free breath sample (<.02%; AlcoSensor Intoximeter).
Volunteers were excluded if they expressed homicidal or suicidal ideation; or were cognitively impaired (IQ < 80) on the Shipley Institute of Living Scale (Zachary, 1991).
2.3. Experimental measures
Hypothetical purchase tasks.
Choice simulations were conducted using a structured interview (Petry and Bickel, 1998). The procedures simulated marijuana purchasing in relation to increasing amounts of money or time required to obtain a unit dose of marijuana (own-price elasticity), likelihood of reselling one’s marijuana or registration card in relation to increasing profit (diversion potential), and demand for non-marijuana goods in relation to monetary cost of marijuana (cross-price elasticity). The ranges of commodity values were obtained from prior studies and preliminary estimates reported by this patient population.
Each purchase task included several unit prices (UPs; typically, 7 values across a 20-fold range) listed on a piece of paper presented to the participant. Demand curves are positively decelerating and we selected a range of UPs with the intent of generating mixed elasticity: This refers to demand for a commodity being inelastic at low UPs (rate of consumption decreases more slowly than rate of UP increases, associated with the flatter left portion of the curve) and elastic at higher UPs (rate of consumption decreases more rapidly than rate of UP increases, associated with the steeper right portion of the curve).
Standard purchase prices for drugs represented local values: marijuana $10.00 per 1/10th oz., alcohol $3.00 per standard drink, cigarettes $0.30 each, hydrocodone $5.00 per 7.5-mg pill, alprazolam $1.50 per 0.5-mg pill, and dronabinol $5.00 per 2.5-mg pill. Provider services were $60 for 1-hr massage and $120 for 1-hr acupuncture. Supplements were $10 for 1-hr herbal therapy and $2 for daily vitamins.
To constrain choices, participants were instructed that they (1) had no access to experimental goods except those purchased; (2) could only purchase goods within the income allocated, (3) could not give or sell goods (except for assessment of diversion potential), (4) had to consume all goods within 24-hr; and (5) would not experience adverse consequences from consuming the good.
Marijuana own-price elasticity
Marijuana own-price elasticity was measured in two parallel simulations as the number of 0.1-oz marijuana units purchased in relation to its: (1) money cost ($5, $15, $30, $45, $60, $75 and $100 per ¼ oz); and (2) round-trip time to obtain ¼-oz marijuana (3, 10, 30, 45, 60, 90, 120 min). We did not stipulate whether purchasing was for recreational or therapeutic use.
Diversion (commodity misuse) potential
Diversion (commodity misuse) potential was evaluated in two simulations by measuring effects of different income gains ($10, $25, $40, $50, $70, $90, $100) on choice to sell his/her (a) marijuana supply (0.1-oz.) or (b) registration card. Whereas some therapeutic users may resell their marijuana (Martins et al., 2016; Nussbaum et al., 2015), the registration card served as a comparator commodity that, because of its ability to reduce legal risks (price) of marijuana possession/use, should have a lower likelihood of diversion/misuse.
Marijuana therapeutic-use certification demand
Marijuana therapeutic-use certification demand was measured as choice to seek certification in relation to five UP factors (parallel simulations): (1) number of physicians the patient must solicit to obtain certification (1, 2, 4, 6, 8, 10, 15); (2) cost of registration card ($10, $25, $50, $75, $100, $150, $250); (3) delay from mailing application to receiving registration card (0.5, 1, 2, 4, 8, 12, 26 weeks); (4) duration of certification (0.5, 1, 2, 3, 4, 5, 10 years); and (5) cost to renew registration after initial one-year period ($5, $15, $25, $35, $50, $75, $100).
Marijuana cross-price elasticity
Marijuana cross-price elasticity was evaluated by measuring the effect of marijuana UP variation on purchasing legal substances (cigarettes, alcohol), controlled substances (hydrocodone, alprazolam, cocaine/crack), HIV-symptom medications (ondansetron, dronabinol), and alternatives (massage, acupuncture, vitamins, herbals). These commodity options reflect different complementary/alternative medicine (CAM) practices among PLWH (Littlewood and Vanable, 2008; Lorenc and Robinson, 2013; Mills et al., 2005; Owen-Smith et al., 2011; Power et al., 2002) and CAM approaches and provider services sought by patients in this clinic (Greenwald et al., under review). On each trial, price of the non-marijuana option was held constant. We repeated purchasing opportunities on separate trials, varying prices for these goods.
Clinical assessments.
The Cannabis Abuse/Dependence module of the Structured Clinical Interview for DSM-IV (First et al., 1996) was edited to determine CUD presence/absence and severity according to DSM-5 criteria.
Participants rated past 90-day severity of 24 symptoms, using a 0–3 scale (0=not at all, 1=slightly, 2=somewhat, 3=severe): pain, depression, anxiety, poor appetite, weight change, poor sleep, fatigue/lack of energy, memory loss, cough, shortness of breath, fever, night sweats, nausea, vomiting, constipation, diarrhea, tingling in extremities, numbness in extremities, muscle weakness, tremor, headache, not interested in sex, slurred speech, and vision problem.
Participants reported the number of past 90-days they used each substance, and percentage of time they “used marijuana for symptom relief” (0 [entirely recreational use]–100 [entirely therapeutic use]).
2.4. Data analysis
Distributions for all measures were reviewed for normality. Measures with non-normal distributions were log10 transformed before analysis.
Demand curve analysis was used to estimate the amount of marijuana consumed across increasing UPs. We measured each participant’s demand intensity and elasticity for marijuana (number of 0.1-oz units purchased/consumed at a fixed daily income of $120), in relation to marijuana money cost (UP: $2.50–20.00) and round-trip time cost to purchase each 0.1-oz (UP: 3–120 min). To maximize demand curve fit (in log/log space) when including zero consumption values and to use all UP/consumption pairwise data, a fixed value of 10 was added to all raw consumption data (Koffarnus et al., 2015) so log10 of zero values would equal 1. Demand curves were fit for each subject in GraphPad Prism v.6 using the formula (Winger and Hursh, 1995): Y = log(L) * exp (−a*X); where L=intensity, a=elasticity, X=unit price, and Y=consumption. Effects of naturalistic marijuana- and symptom-related factors on marijuana demand were analyzed separately for intensity and elasticity. Analyses are presented using transformed data (Table 2 and Supplemental Table 1), whereas results are illustrated (Figure 1) using raw consumption data.
Table 2.
Marijuana demand intensity (left) and elasticity (right) as a function of monetary cost and individual differences
| Mean (SD) demand intensity (L) for absence and presence/severity of sign/symptom | Univariate ANOVA results | Mean (SD) elasticity (a) for absence and presence/severity of sign/symptom | Univariate ANOVA results | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Absent | Mild | Mod. | Severe | Absent | Mild | Mod. | Severe | ||||
| CUD severity | 12.72 (2.96) | 12.46 (1.71) | 13.33 (2.62) | 14.17 (2.66) | F(3,109)= 2.78, p=.045 | .002983 (.003041) | .002314 (.002293) | .002892 (.002627) | .003554 (.003502) | F(3,109)= 1.01, p=.393 | |
| Anxiety severity | 12.50 (1.52) | 13.49 (2.56) | 13.26 (2.36) | 14.58 (3.79) | F(3,109)= 3.80, p=.012 | .002458 (.002156) | .0033134 (.003591) | .002777 (.002736) | .003662 (.003532) | F(3,109)= 1.06, p=.367 | |
| Pain severity | 12.43 (1.66) | 13.70 (2.25) | 14.11 (3.29) | 12.59 (1.70) | F(3,109)= 3.69, p=.014 | .002343 (.002072) | .003805 (.002935) | .003471 (.003639) | .0023779 (.002113) | F(3,109)= 1.70, p=.172 | |
| Absent | Present | Absent | Present | ||||||||
| Past 3-month opioid use | 12.71 (2.05) | 13.66 (2.80) | ------ | ------ | F(1,111)= 4.19, p=.043 | .002585 (.002373) | .003174 (.003201) | ------ | ------ | F(1,111)= 1.24, p=.268 | |
Figure 1.

Simulated marijuana demand in relation to money cost for different univariate predictors. Marijuana demand intensity (mean consumption at low unit prices) was significantly positively related to current severity of cannabis use disorder (CUD; upper left); past 3-month anxiety severity (upper right); past 3-month pain severity (higher for slight or moderate pain severity; lower left); and any past 3-month opioid use (lower right). These factors did not significantly alter marijuana price-elasticity.
In two parallel, generalized estimating equations (GEE) repeated-measures logistic regression analyses, we evaluated likelihood of diversion in relation to income gains (repeated-measures factor) for willingness to sell 0.1-oz marijuana ($10–250) or his/her hypothetically-existing marijuana therapeutic-use registration card ($5–100).
In five parallel GEE mixed-model logistic regression analyses, we evaluated likelihood of seeking marijuana therapeutic-use certification relative to number of physicians the participant needed to visit to obtain certification (1–15), yearly cost for initial certification ($10–150) and renewal of certification ($5–100), time between submitting the application and receiving the certification card (0.5–26 weeks), and duration of certification (0.5–10 years). The foregoing factors were repeated-measures factors, and covariates included several clinical factors from Table 1.
Table 1.
Participant characteristics
| Cannabis Use Disorder (CUD) Severity | |||||||
|---|---|---|---|---|---|---|---|
| Absent n = 14 | Mild n = 38 | Moderate n = 38 | Severe n = 29 | Mean (SD) N = 119 | F/χ2 | p | |
| Demographics | |||||||
| Sex | 2.56 | .861 | |||||
| Male | 8 | 25 | 23 | 19 | |||
| Female | 6 | 13 | 14 | 10 | |||
| Transgender | 0 | 0 | 1 | 0 | |||
| Race | 15.94 | .386 | |||||
| African American | 10 | 37 | 32 | 27 | |||
| White | 1 | 0 | 2 | 0 | |||
| Native American | 0 | 0 | 1 | 0 | |||
| Biracial | 1 | 0 | 1 | 0 | |||
| Multiracial | 1 | 1 | 1 | 2 | |||
| Other | 1 | 0 | 1 | 0 | |||
| Age (years) | 45.6 (9.7) | 43.9 (10.1) | 44.8 (10.3) | 45.6 (8.7) | 44.8 (9.7) | 0.20 | .897 |
| HIV status | |||||||
| Years since diagnosis | 10.3 (5.7) | 12.5 (8.6) | 10.4 (6.8) | 11.9 (7.0) | 11.4 (7.3) | 0.66 | .576 |
| Substance Use (past 90 days) | |||||||
| Marijuana frequency (# use episodes) | 180.0 (274.6) | 205.6 (202.7) | 368.6 (288.9) | 419.0 (365.4) | 306.6 (297.6) | 4.62 | .004 |
| Daily alcohol use, n (%) | 0 (0) | 5 (13.2) | 7 (18.4) | 6 (20.7) | 18 (15.1) | 3.63 | .304 |
| Any opioid use, n (%) | 8 (57.1) | 22 (57.9) | 16 (42.1) | 16 (55.2) | 62 (52.1) | 2.29 | .515 |
| Any cocaine use, n (%) | 2 (14.3) | 12 (31.6) | 5 (13.2) | 9 (31.0) | 28 (23.5) | 5.21 | .157 |
| Any sedative use, n (%) | 0 (0) | 2 (5.3) | 2 (5.3) | 3 (10.3) | 7 (5.9) | 1.97 | .579 |
| Symptoms (past 90 days) | |||||||
| STAI Y-2 | 40.4 (11.2) | 39.5 (11.5) | 41.8 (10.8) | 45.2 (12.8) | 41.7 (11.6) | 1.42 | .242 |
| BDI-II | 13.9 (7.8) | 13.7 (10.3) | 15.9 (11.1) | 16.2 (9.8) | 15.0 (10.2) | 0.50 | .685 |
| Anxiety (0–3) | 1.36 (1.28) | 0.82 (1.06) | 1.16 (1.13) | 1.28 (1.28) | 1.10 (1.17) | 1.24 | .300 |
| Depression (0–3) | 1.71 (1.14) | 1.29 (1.27) | 1.32 (1.14) | 1.17 (1.17) | 1.32 (1.19) | 0.67 | .573 |
| Pain (0–3) | 2.29 (0.99) | 1.71 (1.18) | 1.97 (1.10) | 1.62 (1.15) | 1.84 (1.14) | 1.44 | .236 |
| Poor sleep (0–3) | 1.79 (1.12) | 1.13 (1.12) | 1.76 (1.32) | 1.31 (1.23) | 1.45 (1.23) | 2.20 | .092 |
| Poor appetite (0–3) | 1.36 (1.22) | 1.13 (1.21) | 1.24 (1.15) | 1.24 (0.95) | 1.22 (1.12) | 0.15 | .928 |
| Nausea (0–3) | 0.79 (1.19) | 0.55 (0.89) | 0.76 (1.00) | 0.66 (0.90) | 0.67 (0.96) | 0.37 | .772 |
| Fatigue (0–3) | 1.57 (1.28) | 1.37 (1.17) | 1.21 (1.09) | 1.28 (1.13) | 1.32 (1.14) | 0.37 | .772 |
| Tingling in extremities (0–3) | 1.07 (1.14) | 0.89 (1.13) | 0.82 (0.98) | 1.14 (1.16) | 0.95 (1.09) | 0.57 | .639 |
| Numbness in extremities (0–3) | 0.64 (1.01) | 0.84 (1.08) | 0.92 (1.08) | 0.93 (1.07) | 0.87 (1.06) | 0.28 | .840 |
3. Results
3.1. Participant characteristics
Data were collected from 119 marijuana-using PLWH. The average (±SD) participant was a 44.8±9.7 year-old African American (89.1%) male (63.0%). Average time since HIV diagnosis was 11.4±7.3 years. The sample was divided into four CUD severity groups: absent (n=14), mild (n=38), moderate (n=38), and severe (n=29). Table 1 displays participant characteristics stratified on this factor. Participants with higher-severity CUD used marijuana more frequently than those with lower-severity CUD, but there were no other significant differences.
3.2. Simulations
3.2.1. Marijuana demand in relation to monetary price
Marijuana demand was first evaluated in relation to money prices for a 1/10th-oz. unit amount. Figure 1 shows effects of symptom severity group on marijuana demand using money prices; Table 2 presents findings from ANOVAs of demand-curve intensity and elasticity. Demand intensity was significantly related to: increasing CUD severity and past 3-month anxiety severity; past 3-month pain severity such that purchasing was higher among participants reporting mild and moderate pain, and lower for participants reporting no pain and severe pain; and any past 3-month opioid use versus no opioid use. In contrast, there were no significant group effects on marijuana money-price elasticity (Table 2). Similar results were obtained for marijuana demand intensity and elasticity in relation to purchase-time cost (Supplemental Table 1).
Multiple linear regression analysis was used to predict marijuana demand intensity (L), controlling for age, which had a bivariate association with the outcome (r=−.204, p=.03). Table 3 presents results of this analysis. Past 3-month anxiety, current CUD severity, younger age, and past 3-month opioid use, significantly predicted marijuana demand intensity, F(4,108)=7.25, p<.001, accounting for 18.2% of variance in demand intensity.
Table 3.
Multiple linear regression analysis predicting marijuana money-price demand intensity
| Predictors | R2 | Adj. R2 | B (SE) | β | t | p |
|---|---|---|---|---|---|---|
| Model | .212 | .182 | ||||
| (Constant) | 13.921 (1.06) | 13.14 | .000 | |||
| Anxiety severity | 0.553 (0.18) | .260 | 3.03 | .003 | ||
| CUD severity | 0.533 (0.22) | .210 | 2.44 | .016 | ||
| Current age | −0.061 (0.02) | −.240 | −2.78 | .006 | ||
| Past 3-mo. opioid | 0.972 (0.43) | .197 | 2.27 | .025 |
3.2.2. Diversion potential
Diversion potential was independently evaluated for marijuana and marijuana therapeutic-use registration card according to resale profit. Figure 2 shows findings of GEE mixed-model logistic regression analyses, represented as growth curves. Diversion likelihood was minimal (≤13% of participants) for the registration card up to a profit of $150 (highest amount assessed). In contrast, for income prospects ≥$15, most participants would sell their marijuana, Wald χ2(6)=95.41, p=.000. No group factors above were significantly related to marijuana diversion potential.
Figure 2.

Simulated diversion (commodity misuse) potential. At income prospects (i.e. simulated profit from selling) ≥ $15, high proportions (means ± 1 SEMs) of the sample were likely to divert 1/10th oz. marijuana (asterisks indicate significant increase relative to the $5 profit condition), whereas participants were unlikely to divert their (hypothetical) personal, state-issued registration card at any income prospect up to $150 (highest amount assessed).
3.2.3. Marijuana therapeutic-use certification
The percent of the sample willing to obtain marijuana therapeutic-use certification was evaluated in relation to: amount of ‘doctor shopping’ to obtain a physician’s signature on the application form; initial and renewal cost of registration card; delay from submitting the application to receiving the card; and duration of certification. Figure 3 presents results from GEE mixed-model logistic regression analyses.
Figure 3.
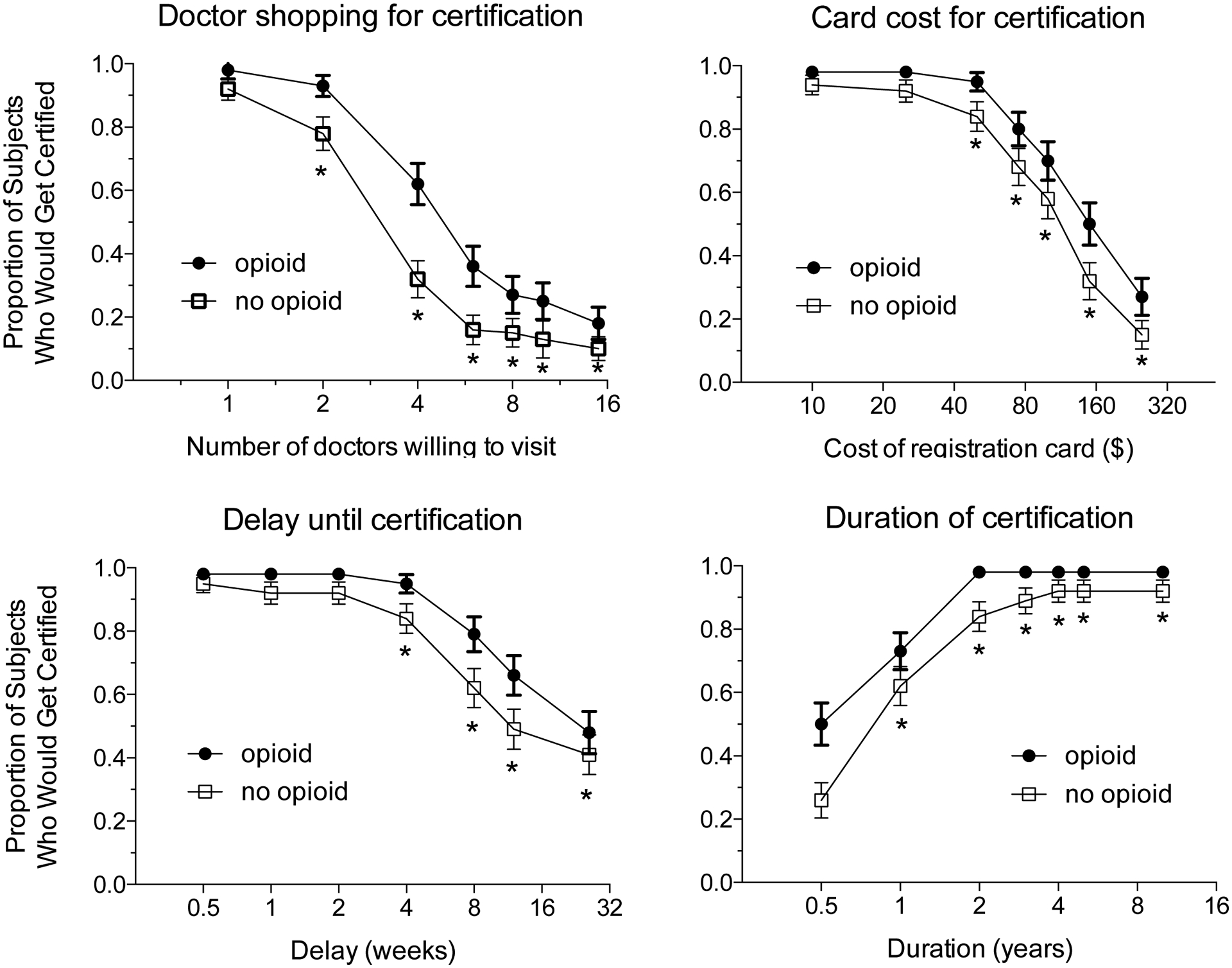
Simulated rates of marijuana therapeutic-use certification (i.e. willingness to obtain a state-issued registration card) in relation to several price factors (different panels) and prior 3-month opioid use (within each panel). Participation rate (mean ± 1 SEM proportion of participants who would seek certification) significantly decreased in relation to increasing: number of doctors they would have to visit to obtain certification signoff (‘doctor shopping’; upper left), money cost of the state-issued registration card for certification (upper right), delay in weeks from the participant submitting the application to receipt of registration card (lower left); and participation rate increased as duration of certification increased (lower right). Asterisks indicate that the value at the unit price was significantly lower than the value at the lowest unit price. For all price factors, past 3-month opioid use was associated with statistically higher participation rates (doctor shopping, card price, duration of certification) or numerically higher rates (delay to certification).
Likelihood of certification significantly decreased when participants had to visit more physicians, Wald χ2(6)=71.80, p<.001, and was higher for individuals with past 3-month opioid use, Wald χ2(1)=7.42, p=.006. There was no significant interaction.
Likelihood of certification significantly decreased as registration cost increased, Wald χ2(6)=113.64, p<.001, and was higher for individuals with past 3-month opioid use, Wald χ2(1)=4.14, p=.042. There was no significant interaction. Likelihood of renewing certification (not shown) also decreased as registration cost increased, Wald χ2(5)=39.95, p<.001, yielding a curve that closely tracked initial certification rate, indicating reliable price-sensitivity.
Likelihood of certification significantly decreased with longer delay from mailing the application to receiving the card, Wald χ2(5)=68.35, p<.001, and was numerically higher overall among those with past 3-month opioid use, Wald χ2(1)=2.96, p=.085. There was no significant interaction.
Likelihood of certification significantly increased as expected duration of certification increased, Wald χ2(4)=68.73, p<.001, and was marginally higher for those with past 3-month opioid use, Wald χ2(1)=3.57, p=.059. A significant interaction was found, Wald χ2(4)=10.25, p=.036, such that opioid-use group differences were greater at shorter certification durations.
3.2.4. Cross-price elasticity
To evaluate cross-price elasticity, price-dependent consumption of non-marijuana commodities was separately tested at different marijuana UPs. Supplemental Table 2 presents numbers of participants who purchased at least some units of these alternative commodities. Figure 4 shows representative examples of these simulations. Among participants who purchased cigarettes (n=84), alcoholic drinks (n=73), hydrocodone 7.5-mg tablets (n=17), and 1-hr massage (n=76), all goods were own-price sensitive but were not sensitive to marijuana UP.
Figure 4.
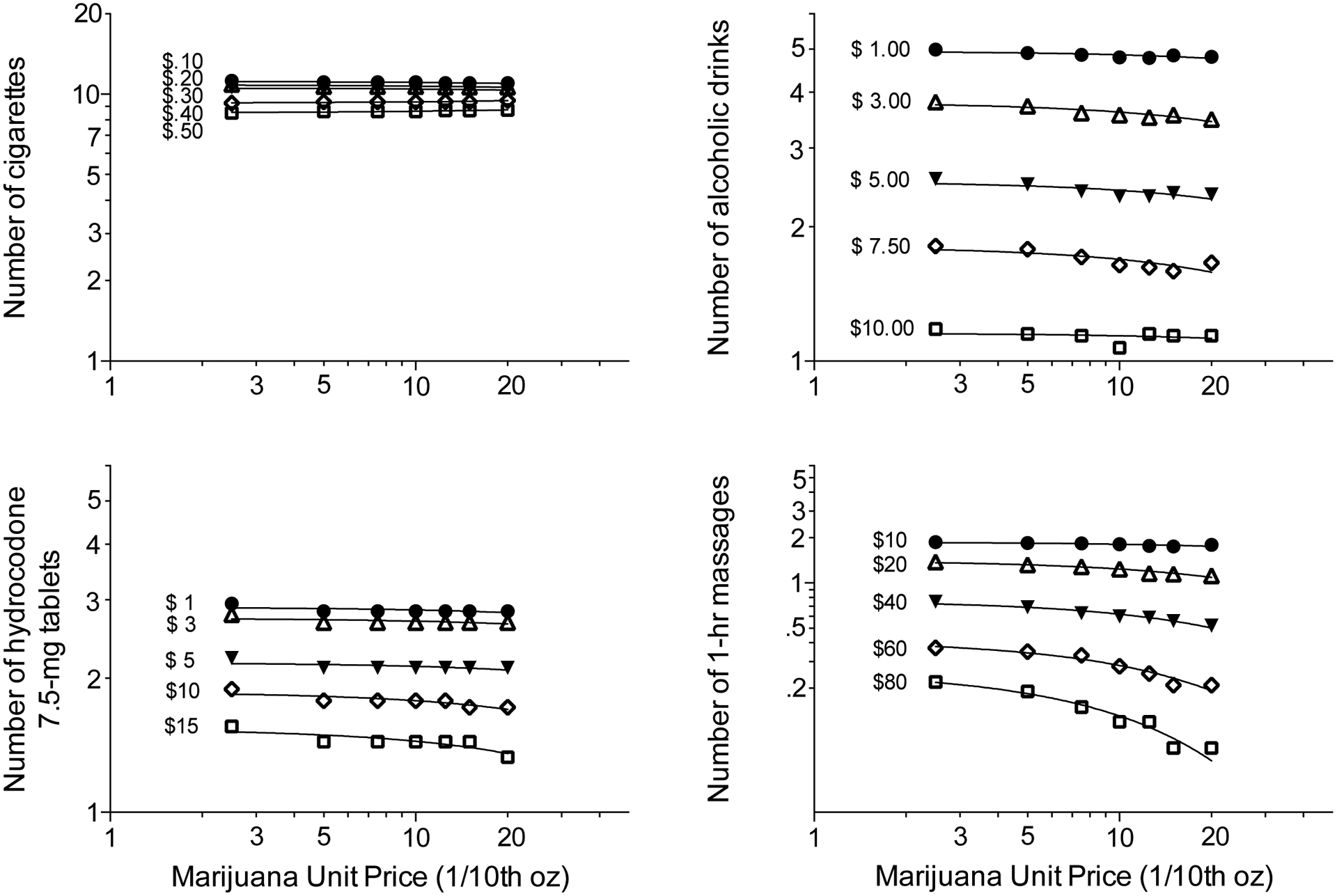
Simulated cross-price elasticity, demonstrating that marijuana and other commodities tested were independent goods. Among participants who reported they would purchase/consume cigarettes in addition to marijuana (n=84), cigarettes were own-price sensitive (downward curve shift) but not sensitive to marijuana unit price (UP) (upper left). Among participants who reported they would purchase/consume alcohol in addition to marijuana (n=73), alcohol was own-price sensitive but not sensitive to marijuana UP (upper right). Among participants who reported they would purchase/consume hydrocodone (Vicodin 7.5-mg tablets) in addition to marijuana (n=17), hydrocodone was own-price sensitive but not sensitive to marijuana UP (lower left). Among participants who reported they would purchase/consume massage therapy in addition to marijuana (n=73), massage therapy was own-price sensitive but not sensitive to marijuana UP (upper right). The marijuana demand curve is shown in each panel (heavy dashed line). See text for explanation of methods.
4. Discussion
This is the first study to demonstrate in PLWH that (1) marijuana demand intensity was related to clinical symptom severity, (2) diversion potential was related to resale profit for marijuana but not registration card, (3) likelihood of seeking marijuana therapeutic-use certification was related to various unit-cost factors, and (4) marijuana demand was independent of other goods.
4.1. Overall purchasing and individual differences
One primary result was that PLWH diagnosed with more severe CUD purchased/consumed more marijuana across UPs tested (higher demand intensity, but no difference in elasticity). Our findings in PLWH are concordant with studies of healthy participants that found relationships between naturalistic marijuana consumption and experimental marijuana demand intensity and/or elasticity on purchase tasks (Aston et al., 2015; Collins et al., 2014; Strickland et al., 2017; Vincent et al., 2017). We also obtained similar findings when marijuana UP was defined either by money or time, indicating these results are reliable and valid. Our results partly agree with Pacula and Lundberg (2014) who proposed that marijuana-using subgroups may be differentially sensitive to marijuana prices. The observation that CUD severity specifically related to marijuana demand intensity but not elasticity has implications for policy, namely, that naturalistic price controls on marijuana consumption may work equally well across levels of CUD severity, but overall demand will remain greater among those with more severe CUD compared to those with mild CUD.
Past 90-day anxiety symptom severity was also positively related to marijuana demand intensity but not price-elasticity. Previous studies have found associations between anxiety and marijuana use in both healthy participants (Comeau et al., 2001; Buckner et al., 2007; Bonn-Miller et al., 2007) and PLWH (Prentiss et al., 2004; Woolridge et al., 2005). Our study, however, is the first to examine anxiety levels in relation to experimental marijuana purchasing by PLWH. As anxiety severity was positively related to marjuana demand intensity, our findings again imply price controls on marijuana should be effective across anxiety severity levels although demand would remain greater among highly anxious patients.
Whereas severity of CUD and anxiety were linearly related to marijuana demand intensity, past 90-day pain severity had an inverted-U relationship to demand intensity: participants reporting mild and moderate pain purchased/consumed more marijuana than those reporting no pain or severe pain. These findings suggest marijuana has greater reinforcing effects among PLWH with intermediate pain levels, but we cannot establish whether this utility is due to an effect of marijuana on pain relief (negative reinforcement), recreational motives (positive reinforcement), or both. Cross-sectional surveys (Prentiss et al., 2004; Swift et al., 2005; Woolridge et al., 2005) and randomized placebo-controlled clinical trials (Abrams et al., 2007; Ellis et al., 2009) have identified an analgesic effect of marijuana use among PLWH. In contrast, a longitudinal observational study found that marijuana use and pain were unrelated over a 1-year period (Merlin et al., 2019) and an experimental purchase task study of past-year non-medical prescription opioid-using adults (without regard to HIV status) found no relationship between pain levels and marijuana purhasing (Strickland et al., 2019). Given these mixed findings, future studies should stratify analysis on pain and CUD severity to characterize the relationship between pain and marijuana demand/use.
Any potential association between marijuana use and pain severity is complicated by concomitant use of opioids, and how the analgesic and reinforcing efficacies of marijuana and opioids interact. In our study, PLWH who endorsed any past 90-day opioid use (52% of sample) exhibited higher marijuana demand intensity and reported higher pain severity, but did not differ in marijuana price-sensitivity or CUD severity, compared to non-users of opioids. This positive association between pre-experimental opioid use and experimental marijuana demand agrees with Strickland et al. (2019), who found non-medical prescription opioid users had higher marijuana demand intensity on a purchasing task. In contrast, among online respondents (without regard to HIV status) who endorsed pain and past-month use of marijuana and prescribed opioid analgesics, concurrent opioid availability decreased marijuana demand intensity and increased elasticity on experimental purchasing tasks (Bergeria et al., 2020). The similar findings from our study and Strickland et al. (2019) may diverge from Bergeria et al. (2020) due to methodological differences. Notably, there could be asymmetrical effects between pre-existing marijuana or opioid use on demand for the other commodity, which our study does not address; thus, further research is needed to investigate these relationships.
4.2. Cross-price purchasing
In cross-price simulations, marijuana and hydrocodone were independent goods (i.e., increasing marijuana UP did not alter hydrocodone price-sensitivity). There was similar independence between marijuana and other goods (e.g., alcohol, cigarettes, massage, vitamins, acupuncture). There are few studies of marijuana cross-price elasticity to which our data can be compared. Our sample of marijuana-using PLWH, half of whom reported recent naturalistic opioid use, mostly did not purchase opioids experimentally (only 14%) but when they did, hydrocodone purchasing was independent of marijuana purchasing. In contrast, participants in the Bergeria et al. (2020) study were current users of opioids for pain relief and marijuana; different subgroups were found to treat marijuana and opioids as either complements, substitutes, or independent goods (i.e., there was not a consistent pattern). Thus, sample characteristics (PLWH or other clinical population [e.g., pain], pre-experimental concomitant use of specific goods) and experimental procedures (e.g., online vs. in-person, range of UPs) may co-determine cross-price elasticity between marijuana and other commodities.
4.3. Diversion potential
Our study identifed a striking difference between diversion potential of marijuana and a marijuana therapeutic-use registration card. Probability of diverting marijuana steeply increased with expected profit (>75% of participants would sell 0.1-oz marijuana if they could earn ≥$30), wherease probability of diverting their registration card remained low (<15%) at profits up to $150. These results regarding marijuana resale are consistent with studies that found higher marijuana diversion rates in states with marijuana therapeutic-use laws (Martins et al., 2016; Nussbaum et al., 2015). Our study is the first to probe marijuana and registration card diversion potential among PLWH. These findings suggest PLWH view the registration card as a longer-term investment, because it is a tool with flexible utility to obtain marijuana for therapeutic use (as legally intended) or recreational use and, among a small minority of individuals, for possible diversion.
4.4. Certification demand
Our study assessed willingness to choose marijuana therapeutic-use certification in relation to several cost factors. Certification demand decreased with greater ‘doctor shopping’ requirements (to certify the user), money-cost and wait-time to receive the card, and increased with the duration of registration card validity. Certification rate dropped to ≈50% (ED50) when participants had to: (1) visit 4 physicians to obtain a signature, (2) pay $140 for the registration card, (3) wait 16 weeks to receive the card, and (4) renew certification after 8 months (0.75 years). As there are no comparable data, these estimates offer benchmarks for setting administrative policies related to ease of certification and, thus, willingness of patients to participate.
For each experimental cost factor, past 90-day opioid use was associated with higher marijuana therapeutic-use certification rates. Whereas other studies of non-PLWH patients found prior substance use may affect certification and use (Ilgen et al., 2013), the present study offers the first demonstration that opioid users may be more willing to seek certification. This may be related to higher marijuana demand exhibited by recent opioid users in our study. Yet, there is a complex relationship between opioid and marijuana use that this study cannot fully address. Some population-level studies observed that state marijuana therapeutic-use laws correlate with lower rates of opioid prescribing (McMichael et al., 2020; Wen and Hockenberry, 2018), use (Flexon et al., 2019; Shah et al., 2019), and overdose mortality (Bachhuber et al., 2014; Chihuri and Li, 2019). However, confounds between marijuana laws and opioid use have not been controlled (Campbell et al., 2018; Shover et al., 2019; Smart and Pacula, 2019), and epidemiological and ecological data cannot predict individual-level use patterns (Caputi and Sabet, 2018; Hall et al., 2018). Thus, prospective longitudinal research is needed to examine whether the effect of opioid use on demand for marijuana and/or certification is independent of pain severity and illicit/sanctioned use; and whether enabling use of marijuana through legalization/medicalization might mediate reductions in opioid analgesic use.
4.5. Limitations
This study has several limitations. First, we used hypothetical purchase tasks, which are intended to simulate (under controlled conditions) purchasing/consumption that might occur in the user’s natural environment. It is possible that perception of values in the experimental and naturalistic settings may vary. The resulting data therefore are indirect estimates, and we have not established the predictive validity of our findings. Other studies have found greater hypothetical marijuana demand is associated with driving under the influence (Patel and Amlung, 2019) and CUD (Strickland et al., 2017), which supports the concurrent validity of purchase tasks, but we are unaware of studies that have demonstrated the predictive validity of marijuana purchase task data in any study population. Second, we may not have included a sufficient range of UPs (or profits) in our simulations, which could affect results for marijuana price-elasticity (which may explain lack of group differences in elasticity) or diversion potential (which could explain low rates of selling the registration card); yet, including more UPs would have lengthened assessments and decreased study feasibility. Second, some measures lacked precision. For instance, endorsing past 90-day opioid use could reflect legitimate therapeutic use of prescribed opioids, misuse of analgesics, or use of illegal opioids; we lacked data to differentiate these possibilities. Likewise, past 90-day symptom severity ratings are broad indices that may not correlate with daily use; however, these easily-assessed factors were examined in relation to experimental marijuana choices rather than naturalistic use. Third, this study took place when only marijuana therapeutic use was legal; with many states legalizing recreational use, further examination of these contextual issues will be useful. Fourth, our economically-disadvantaged, urban participant sample may respond differently to prices compared to other populations; thus, our findings may not generalize.
4.6. Conclusion
We found that UPs and clinical factors (CUD, anxiety and pain severity, as well as recent opioid use) modulated marijuana demand, diversion potential and certification demand among PLWH. Marijuana and other commodities were independent goods. Our findings have implications for clinicians and policymakers. Clinicians may expect changes in marijuana use resulting from these variables. In the absence of significant individual differences in price-sensitivity, policymakers should consider that moderate price controls may have limited impact on use of marijuana and other goods. Also, state-issued certification cards are price-sensitive and appear unlikely to be diverted. Future studies should focus on therapeutic vs. recreational marijuana use among PLWH given growing legalization of recreational marijuana use, and comorbidities in this population.
Supplementary Material
Highlights.
Persons living with HIV (PLWH) often use marijuana (MJ); drivers poorly understood
119 MJ-using PLWH completed simulated commodity purchasing and selling tasks
Cannabis use disorder, anxiety, pain, and opioid use altered MJ demand intensity
More PLWH sold MJ as simulated profit increased, but few sold the registration card
Several cost factors influenced likelihood of medical marijuana certification
Acknowledgements
The authors thank Christina DeAngelis, Elorie Eggleston, Katie Mattison, and Lisa Sulkowski for data collection and management.
Role of Funding Sources
NIH grant R01 DA032678 (to MKG) from the National Institute on Drug Abuse, the Gertrude Levin Endowed Chair in Addiction and Pain Biology (MKG), a research grant (Joe Young, Sr./Helene Lycaki Funds) from the Michigan Department of Health and Human Services, and the Detroit Wayne Integrated Health Network, supported this research. These funding sources had no role in study design, data collection, analysis or interpretation of the data, writing of the report, or the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare no conflict of interest with respect to the conduct or content of this work.
References
- Abrams DI, Jay CA, Shade SB, Vizoso H, Reda H, Press S, et al. , 2007. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology 68, 515–521. [DOI] [PubMed] [Google Scholar]
- Acuff SF, Amlung M, Dennhardt AA, MacKillop J, Murphy J, 2020. Experimental manipulations of behavioral economic demand for addictive commodities: a meta-analysis. Addiction 115, 817–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, Reed DD, Morris V, Aston ER, Metrik J, MacKillop J, 2019. Price elasticity of illegal versus legal cannabis: a behavioral economic substitutability analysis. Addiction 114, 112–118. [DOI] [PubMed] [Google Scholar]
- Andreyeva E, Ukert B, 2019. (Oct 16 [Epub ahead of print]) The impact of medical marijuana laws and dispensaries on self-reported health. Forum Health Econ. Policy [DOI] [PubMed] [Google Scholar]
- Aston ER, Metrik J, MacKillop J, 2015. Further validation of a marijuana purchase task. Drug Alcohol Depend. 152, 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Saloner B, Cunningham CO, Barry CL, 2014. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern. Med 174, 1668–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates BR, Kissinger P, Bessinger RE, 1996. Complementary therapy use among HIV-infected patients. AIDS Patient Care STDs 10, 32–36. [DOI] [PubMed] [Google Scholar]
- Belle-Isle L, Hathaway A, 2007. Barriers to access to medical cannabis for Canadians living with HIV/AIDS. AIDS Care 19, 500–506. [DOI] [PubMed] [Google Scholar]
- Bergeria CL, Dolan SB, Johnson MW, Campbell CM, Dunn KE, 2020. Evaluating the co-use of opioids and cannabis for pain among current users using hypothetical purchase tasks. J. Psychopharmacol 0269881120914211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, DeGrandpre RJ, 1996. Modeling drug abuse policy in the behavioral economics laboratory In Green L and Kagel JH (Eds), Advances in Behavioral Economics. Vol. 3: Substance Use and Abuse, pp. 69–95. Ablex: Norwood, NJ. [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG, 2014. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu. Rev. Clin. Psychol 10, 641–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A, 2007. Marijuana use motives: concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addict. Behav 32, 49–62. [DOI] [PubMed] [Google Scholar]
- Braitstein P, Kendall T, Chan K, Wood E, Montaner JS, O’Shaughnessy MV, Hogg RS, 2001. Mary-Jane and her patients: sociodemographic and clinical characteristics of HIV-positive individuals using medicinal marijuana and antiretroviral agents. AIDS 15, 532–533. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Bonn-Miller MO, Zvolensky MJ, Schmidt NB, 2007. Marijuana use motives and social anxiety among marijuana-using young adults. Addict. Behav 32, 2238–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell G, Hall W, Nielsen S, 2018. What does the ecological and epidemiological evidence indicate about the potential for cannabinoids to reduce opioid use and harms? A comprehensive review. Int. Rev. Psychiatry 30, 91–106. [DOI] [PubMed] [Google Scholar]
- Caputi TL, Sabet KA, 2018. Population-level analyses cannot tell us anything about individual-level marijuana-opioid substitution. Am. J. Public Health 108, e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulkins J, Reuter P, 1996. The meaning and utility of drug prices. Addiction 91, 1261–1264. [PubMed] [Google Scholar]
- Chihuri S, Li G, 2019. State marijuana laws and opioid overdose mortality. Inj. Epidemiol 6, 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinti S, 2009. Medical marijuana in HIV-positive patients: what do we know? J. Intl. Assoc. Physicians AIDS Care 8, 342–346. [DOI] [PubMed] [Google Scholar]
- Collins RL, Vincent PC, Yu J, Liu K, Epstein LH, 2014. A behavioral economic approach to assessing demand for marijuana. Exp. Clin. Psychopharmacol 22, 211–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comeau N, Stewart SH, Loba P, 2001. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addict. Behav 26, 803–825. [DOI] [PubMed] [Google Scholar]
- Costiniuk CT, Saneei Z, Salahuddin S, Cox J, Routy J-P, Rueda S, et al. , 2019. Cannabis consumption in people living with HIV: reasons for use, secondary effects, and opportunities for health education. Cannabis Cannabinoid Res. 4, 204–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong BC, Prentiss D, McFarland W, Machekano R, Israelski DM, 2005. Marijuana use and its association with adherence to antiretroviral therapy among HIV-infected persons with moderate to severe nausea. J. Acquir. Immune Defic. Syndr 38, 43–46. [DOI] [PubMed] [Google Scholar]
- Duggan J, Peterson WS, Schutz M, Khuder S, Charkraborty J, 2001. Use of complementary and alternative therapies in HIV-infected patients. AIDS Patient Care STDs 15, 159–167. [DOI] [PubMed] [Google Scholar]
- Ellis RJ, Toperoff W, Vaida F, Van Den Brande G, Gonzales J, Gouaux B, et al. , 2009. Smoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trial. Neuropsychopharmacology 34, 672–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, 1996. Structured Clinical Interview for DSM-IV Axis Disorders - Patient Edition (SCID-I/P, Version 2.0) Biometrics Research Dept., NY State Psychiatric Institute: New York. [Google Scholar]
- Flexon JL, Stolzenberg L, D’Alessio SJ, 2019. The effect of cannabis laws on opioid use. Int. J. Drug Policy 74, 152–159. [DOI] [PubMed] [Google Scholar]
- Fogelman I, Lim L, Bassett R, Volberding P, Fischl MA, Stanley K, Cotton DJ, 1994. Prevalence and patterns of use of concomitant medications among participants in three multicenter human immunodeficiency virus type I clinical trials. J. Acquir. Immune Defic. Syndr 7, 1057–1063. [PubMed] [Google Scholar]
- Gonzalez A, Barinas J, O’Cleirigh C, 2011. Substance use: impact on adherence and HIV medical treatment. Curr HIV/AIDS Rep. 8, 223–224. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Akcasu N, Baal P, Outlaw AY, Cohn JA, Lundahl LH, under review. Marijuana and complementary/alternative self-treatment approaches for symptom management among African American persons living with HIV. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald MK, Steinmiller CL, 2014. Cocaine behavioral economics: from the naturalistic environment to the controlled laboratory setting. Drug Alcohol Depend. 141, 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross IM, Hosek S, Richards MH, Fernandez MI, 2016. Predictors and profiles of antiretroviral therapy adherence among African American adolescents and young adult makes living with HIV. AIDS Patient Care STDs 30, 324–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, West R, Marsden J, Humphreys K, Neale J, Petry N, 2018. It is premature to expand access to medicinal cannabis in hopes of solving the US opioid crisis. Addiction 113, 987–988. [DOI] [PubMed] [Google Scholar]
- Hartzler B, Dombrowski JC, Crane HM, Eron JJ, Geng EH, Mathews WC, et al. , 2017. Prevalence and predictors of substance use disorders among HIV care enrollees in the United States. AIDS Behav. 21, 1138–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A, 2008. Economic demand and essential value. Psychol. Rev 115, 186–198. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Bohnert K, Kleinberg F, Jannausch M, Bohnert ASB, Walton M, Blow FC, 2013. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 132, 654–659. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM 1999; Joy JE, Watson SJ, Benson JA Jr, Eds.) Marijuana and medicine: assessing the science base. National Academy Press, Washington, DC. [PubMed] [Google Scholar]
- Koffarnus MN, Franck CT, Stein HS, Bickel WK, 2015. A modified exponential behavioral economic demand model to better describe consumption data. Exp. Clin. Psychopharmacol 23, 504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlewood RA, Vanable PA, 2008. Complementary and alternative medicine use among HIV-positive people: research synthesis and implications for HIV care. AIDS Care 20, 1002–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenc A, Robinson N, 2013. A review of the use of complementary and alternative medicine and HIV: issues for patient care. AIDS Patient Care STDs 27, 503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, et al. 2016. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general US population. Drug Alcohol Depend. 169, 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael BJ, Van Horn RL, Viscusi WK, 2020. The impact of cannabis access laws on opioid prescribing. J. Health Econ 69, 102273. doi: 10.1016/j.healeco.2019.102273 [DOI] [PubMed] [Google Scholar]
- Merlin JS, Long D, Becker WC, Cachay ER, Christopolous KA, Claborn KR, et al. , 2019. Marijuana use is not associated with changes in opioid prescriptions or pain severity among people living with HIV and chronic pain. JAIDS 81, 231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum AM, Thurstone C, McGarry L, Walker B, Sabel AL, 2015. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. Am. J. Drug Alcohol Abuse 41, 166–172. [DOI] [PubMed] [Google Scholar]
- Ogborne AC, Smart RG, Weber T, Birchmore-Timney C, 2000. Who is using cannabis as a medicine and why: an exploratory study. J. Psychoactive Drugs 32, 435–443. [DOI] [PubMed] [Google Scholar]
- Owen-Smith A, DePadilla L, DiClemente R, 2011. The assessment of complementary and alternative medicine use among individuals with HIV: a systematic review and recommendations for future research. J Altern Compl Med 17, 789–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Chriqui JF, Reichmann DA, Terry-McElrath YM, 2002. State medical marijuana laws: understanding the laws and their limitations. J. Public Health Policy 23, 413–439. [PubMed] [Google Scholar]
- Pacula RL, Kilmer B, Grossman M, Chaloupka FJ, 2007. Risks and prices: the role of user sanctions in marijuana markets Working Paper No. 13415 Cambridge, MA: National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Lundberg R, 2014. Why changes in price matter when thinking about marijuana policy: a review of the literature on the elasticity of demand. Public Health Rev. 35, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Starks TJ, Millar BM, Boonrai K, Marcotte D, 2014. Patterns of substance use among HIV-positive adults over 50: implications for treatment and medication adherence. Drug Alcohol Depend. 139, 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel H, Amlung M, 2019. Elevated cannabis demand is associated with driving after cannabis use in a crowd-sourced sample of adults. Exp Clin Psychopharmacol. 27, 109–114. [DOI] [PubMed] [Google Scholar]
- Petry NM, Bickel WK, 1998. Polydrug abuse in heroin addicts: a behavioral economic analysis. Addiction 93, 321–335. [DOI] [PubMed] [Google Scholar]
- Power R, Gore-Felton C, Vosvick M, Israelski DM, Spiegel D, 2002. HIV: effectiveness of complementary and alternative medicine. Primary Care 29, 361–378. [DOI] [PubMed] [Google Scholar]
- Prentiss D, Power R, Balmas G, Tzuang G, Israelski DM, 2004. Patterns of marijuana use among patients with HIV/AIDS followed in a public health care setting. JAIDS 35, 38–45. [DOI] [PubMed] [Google Scholar]
- Roddy JK, Greenwald MK, 2009. An economic analysis of income and expenditures in heroin abusing research volunteers. Substance Use Misuse 44, 1503–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roddy JK, Steinmiller CL, Greenwald MK, 2011. Heroin purchasing is income- and price-sensitive. Psychol. Addict. Behav 25, 358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagy I, Peleg-Sagy T, Barski L, Zeller L, Jotkowitz A, 2018. Ethical issues in medical cannabis use. Eur. J. Intern. Med 49, 20–22. [DOI] [PubMed] [Google Scholar]
- Shah A, Hayes CJ, Lakkad M, Martin BC, 2019. Impact of medical marijuana legalization on opioid use, chronic opioid use, and high-risk opioid use. J. Gen. Intern. Med 34, 1419–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Davis CS, Gordon SC, Humphreys K, 2019. Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proc Natl Acad Sci USA 116, 12624–12626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, Pacula RL, 2019. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am. J. Drug Alcohol Abuse 45, 644–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stogner JM, Sanders A, Miller BL, 2014. Deception for drugs: self-reported “doctor shopping” among young adults. J. Am. Bd. Family Med 27, 583–593. [DOI] [PubMed] [Google Scholar]
- Strickland JC, Lile JA, Stoops WW, 2017. Unique prediction of cannabis use severity and behaviors by delay discounting and behavioral economic demand. Behav. Processes 140, 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, Lile JA, Stoops WW, 2019. Evaluating non-medical prescription opioid demand using commodity purchasing tasks: test-retest reliability and incremental validity. Psychopharmacology (Berl.) 236, 2641–2652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift W, Gates P, Dillon P, 2005. Survey of Australians using cannabis for medical purposes. Harm Reduct. J 2, 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent PC, Collins RL, Liu L, Yu J, De Leo JA, Earleywine M, 2017. The effects of perceived quality on behavioral economic demand for marijuana: a web-based experiment. Drug Alcohol Depend. 170, 174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware M, Rueda S, Singer J, Kilby D, 2003. Cannabis use by persons living with HIV/AIDS: Patterns and prevalence of use. J. Cannabis Ther 2, 3–15. [Google Scholar]
- Wen H, Hockenberry JM, 2018. Association of medical and adult-use marijuana laws with opioid prescribing for Medicaid enrollees. JAMA Intern. Med 178, 673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesner B, 1996. The medicinal marijuana issue among PWAS: Reports of therapeutic use and attitudes towards legal reform Working Paper No.3, Working Paper Series. Drug Research Unit, Social Science Institute, University of Hawaii, Manoa. [Google Scholar]
- Wilkinson ST, Yarnell S, Radhakrishnan R, Ball SA, D’Souza DC, 2016. Marijuana legalization: impact on physicians and public health. Annu. Rev. Med 67, 453–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, Holdcroft A, 2005. Cannabis use in HIV for pain and other medical symptoms. J. Pain Symptom Manag 29, 358–367. [DOI] [PubMed] [Google Scholar]
- Zachary RA, 1991. The Manual of the Shipley Institute of Living Scale, 120th ed Western Psychological Services, Los Angeles, CA. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


