Abstract
Objectives:
Central-line associated bloodstream infection (CLABSI) is associated with increased mortality, morbidity, and cost in hospitalized children. An evidence-based bundle of care can decrease CLABSI, but bundle compliance is imperfect. We explored factors impacting bundle performance in the pediatric intensive care unit (PICU) by bedside nurses.
Methods:
Single-center cross sectional electronic survey of PICU bedside nurses in an academic tertiary care center; using the COM-B (capability, opportunity, motivation) and TDF (theoretical domains framework) behavioral models to explore CLABSI bundle performance and identify barriers to compliance.
Results:
We analyzed 160 completed surveys from 226 nurses (71% response rate). CLABSI knowledge was strong (capability). However, challenges related to opportunity were identified: 71% reported that patient care requirements impact bundle completion; 32% described the bundle as stressful; and CLABSI was viewed as the most difficult of all bundles. 75% reported being highly impacted by physician attitude toward the CLABSI bundle (motivation).
Conclusions:
PICU nurses are knowledgeable and motivated to prevent CLABSI, but face challenges from competing clinical tasks, limited resources, and complex family interactions. Physician engagement was specifically noted to impact nurse motivation to complete the bundle. Interventions that address these challenges may improve bundle performance and prevent CLABSI in critically ill children.
Introduction
Preventable patient harm is an epidemic in the United States – a projected 200,000-400,000 Americans experience premature death due to medical error each year.1 Hospitalized children are no less vulnerable, with an estimated adverse event rate in children’s hospitals of 40 per 100 discharges, half of which were deemed preventable in a 2015 investigation.2
Central-line associated bloodstream infection (CLABSI) is the most common hospital acquired condition in children, and is associated with increased mortality, morbidity, prolonged hospital stay, and an expense of approximately $50,000 per infection.3,4 An evidence-based, best-practice “bundle” of care has been recommended by professional societies to prevent CLABSI, and describes specific care practices that should be completed on a regular basis after central line insertion in order to minimize infection risk (Supplement 1). Increased compliance with this CLABSI prevention bundle is associated with up to 43% lower infection rates, with bundle compliance >95% associated with greatest rate reduction and compliance <75% associated with no rate reduction.3,5,6 Despite the effectiveness of CLABSI bundle, achieving and maintaining optimal bundle compliance remains a challenge.7 A study of PICUs in National Healthcare Safety Network hospitals across the country demonstrated that while 73% had policies for central line infection prevention, only 35% reported compliance >95%.8
Previous studies about CLABSI bundle compliance have not sufficiently demonstrated why compliance with this important task can be difficult to achieve. For example, efforts have often been focused on the relationship between knowledge about CLABSI concepts and bundle performance, but knowledge-themed interventions demonstrate inconsistent results.9,10 In addition, sustainability of optimal bundle compliance seems particularly challenging to facilitate, and many interventions may transiently improve performance but ultimately fail because they do not understand the real obstacles to consistent, standardized practice.11 There is growing evidence, however, that understanding barriers to task performance and the context in which these tasks are performed can lead to improved achievement of the ideal or intended practice.12 Little work has attempted to apply principles of implementation science specifically to the challenge of CLABSI bundle performance in the PICU environment, but doing so may allow identification of new and more effective strategies mapped directly onto to identified barriers.
We therefore undertook an exploration of barriers to optimal CLABSI bundle performance in the PICU environment using survey methodology and two specific theory-based tools for understanding behavior: the Capability, Opportunity, Motivation behavioral model (COM-B) and the Theoretical Domains Framework (TDF).
Explanation of COM-B and TDF
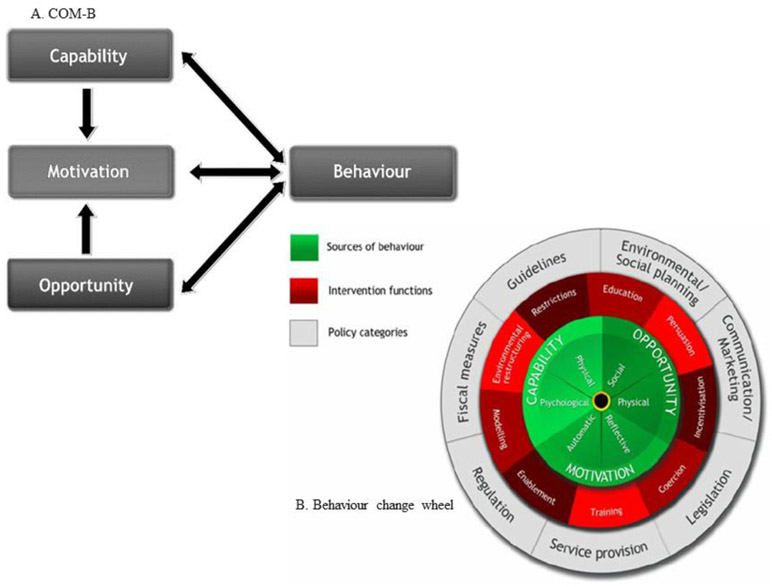
The COM-B model allows for systematic evaluation of capabilities, opportunities, and motivations as the fundamental elements that must be understood prior to the development of interventions that effectively change human behavior.13 Capability can be conceived of as skills and knowledge; opportunities are the external social or environmental factors that facilitate behavior change; and motivation refers to reflective or emotional processes that direct behavior.14 The COM-B model is the center of the Behavior Change Wheel framework, in which nine categories of interventions (such as training, education, and incentivizing) address gaps in capability, opportunity, and motivation in order to lead to sustained behavior change (Figure 1).13 Related to the COM-B, the Theoretical Domains Framework (TDF) synthesizes 84 theoretical constructs of behavior into 14 core domains. The TDF is an established approach to understand behaviors theoretically in order to effectively target processes for change, and has been used in a wide variety of health care settings. 15,16 Each component of the COM-B maps onto TDF domains, and the COM-B can thus be thought of as being grounded in the larger TDF model, though simpler, and offering its own approach to analyzing and understanding behavior change (Supplement 2).12,13,17
Figure 1. The Capability, Opportunity, Motivation Behavioral Model (COM-B) (A) and the Behavior Change Wheel (B).
Adapted from: Michie S, van Stralen MM, West R. The behavior change wheel: a new method for characterizing and designing behavior change interventions. Implementation Science: IS. 2011; 6;42.
Our primary aims were to survey PICU nurses using the COM-B model and TDF to understand for the first time how issues of capability, opportunity, and motivation around performing CLABSI bundle tasks may interact to influence successful bundle performance in the pediatric intensive care unit, and to identify barriers to optimal bundle compliance within each of these domains to guide future development of new interventions to improve performance.
Methods
Overview
We conducted a cross-sectional electronic survey of the 226 full-time bedside nurses in the 60-bed PICU of The Children's Hospital of Philadelphia (CHOP), an urban, academic referral center from October 2018 to January 2019. Nurses were targeted given their direct role in performing the tasks of the CLABSI bundle at patient bedsides during every clinical shift.
Survey development
There are few validated COM-B measures, and none to our knowledge that focus on a harm-prevention task as complex as the CLABSI bundle. Thus, our multidisciplinary study team of pediatric critical care physicians, nurses, patient safety experts, quality improvement leaders, and content experts in mixed methods health services research developed a novel instrument specific to this investigation. We used examples of existing COM-B measures to create the structure and general content of this survey (eg, including questions about adequacy of training for the task, or time allowed to complete the task).18 We then used existing CLABSI literature, established guidelines on CLABSI bundle elements, and principles of infection prevention to tailor the survey items to the specific topic of CLABSI bundle tasks.2-8 The questions were pilot tested by 5 PICU nurses and revised based on this feedback. The final survey instrument consisted of 28 questions which were focused on evaluating the domains of capability, opportunity, and motivation around CLABSI bundle tasks according to the COM-B behavioral model. Approximately 1/3 of the survey was devoted to each of these three domains (Figure 2 and Supplement 3). In addition, two questions solicited free-text comments from respondents about which element of the CLABSI bundle is the most difficult to complete and why. We then performed an exploratory thematic analysis of this qualitative data.
Figure 2. Proposed COM-B Model for CLABSI.
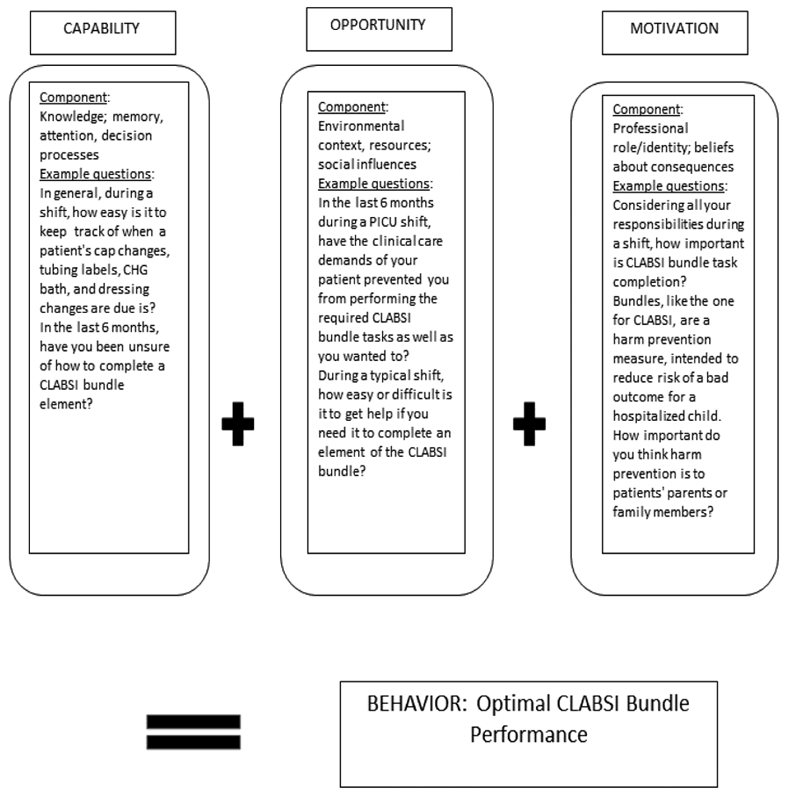
Adapted from: Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, “Psychological Theory” Group. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 14(1):26-33, 2005; and Michie S. The Behaviour Change Wheel, Theoretical Domains Framework, Behaviour Change Techniques. KT Terminology Meeting. 2012, Ottawa, Canada: Conference proceedings
Survey completion
Participation in the survey was entirely voluntary. The survey was distributed via email invitation to all currently employed PICU bedside nurses (REDCap 9.0.3). An email with consent, instructions, and a link to the survey was drafted by the lead physician and nurse members of the study team, but the original survey request and subsequent bi-monthly reminder emails were only distributed by the study team nurses. Limited demographic information without identifying information was collected about each respondent. It took approximately 20-30 minutes to complete. A survey was considered complete if all items including demographics were answered.
Regulatory oversight
This investigation was deemed to be exempt by the Institutional Review Board of The Children's Hospital of Philadelphia.
Analysis
Data were analyzed using descriptive statistics (percent of respondents, means, and medians to summarize demographics as appropriate), using REDCap (9.0.3) and Excel (2016). We examined if responses to items were different based on median respondent age in years, and median years of PICU nursing experience both within our institution and total (<1 year, 1-3 years, 3-5 years, 5-10 years, or >10 years) using the Mann-Whitney test (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). We analyzed only completed surveys; missing data were not imputed.
Results
We analyzed 160 completed surveys for a response rate of 71%. Three incomplete surveys were not included in analysis. Respondent demographics are displayed in Table 1. The majority of respondents (96%) were female, and the majority (59%) had between 0 and 3 years of experience working as a bedside nurse in the CHOP PICU. A minority of those surveyed (13.1%) had any experience working in the PICUs of other institutions, and a minority (8.8%) had more than 10 years of clinical nursing experience. Survey respondents included a mix of those who work primarily day shifts (28.8%), primarily night shifts (22.5%), and a mix of day and night shifts (48.8%). Most respondents had previous experience taking care of a patient with a CLABSI (88.8%).
Table 1.
Demographics of survey respondents
| Demographic | N, % |
|---|---|
| Gender | Female (153, 96%); Male (7, 4%) |
| Years of experience in the CHOP PICU | <1 year, 25, 16%; 1-3 years, 69, 43%; 4-5 years, 17, 10% 5-10 years, 35, 22 %; >10 years, 14, 9% |
| Experience working in another PICU | No (109, 68%); Yes (51, 32%) |
| Primarily work day vs night shifts | Day (46, 29%); Night (36, 22%); Both (78, 49%) |
| Have cared for a patient with a CLABSI | No (18, 11%); Yes (142, 89%) |
| Experience on a harm prevention team | No (100, 62%); Yes (60, 38%) |
| Have received feedback that personal CLABSI bundle compliance needed improvement | No (132, 83%); Yes (28, 17%) |
Capability (knowledge, memory, attention, decision processes)
A majority of nurses, 88.5%, reported that keeping track of when elements of the bundle were due to be performed was either very easy or fairly easy (142/160) (Figure 3, A). A smaller proportion of respondents (35%, 56/160) reported having forgotten to complete an element or elements of the CLABSI bundle during a shift in the last 6 months (Figure 3, A). A majority of our sample (65%, 104/160) reported that they have never been unsure of how to complete any element of the CLABSI bundle, while 35% (56/160) reported being unsure (Figure 3, A).
Figure 3.
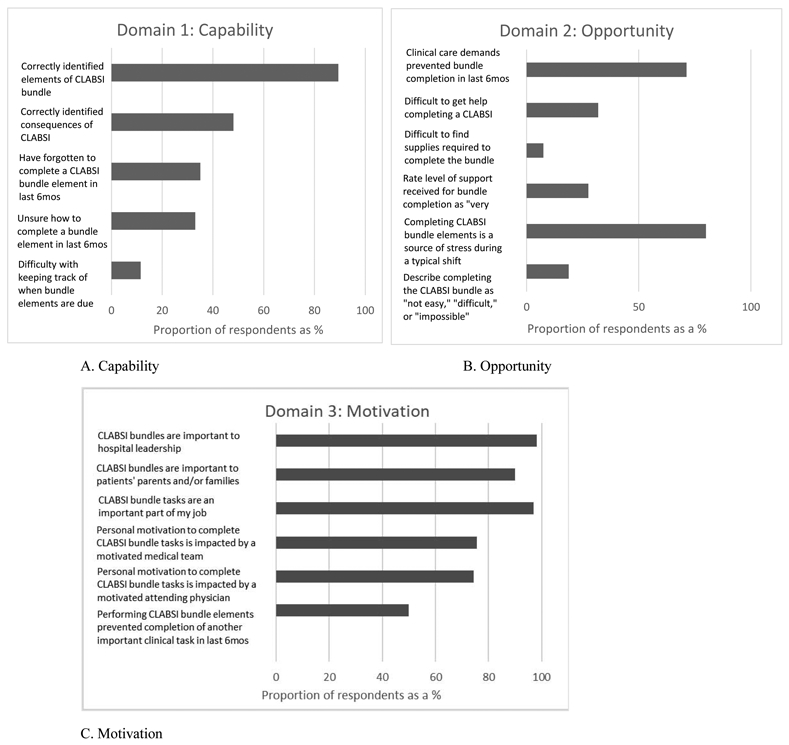
Results of survey questions about A) Capability, B) Opportunity, and C) Motivation
Those who indicated they had been unsure about how to complete a bundle task and those who had forgotten to complete a CLABSI bundle task were slightly younger and less experienced than nurses who reported “never” having been unsure or forgotten to complete a bundle task, but this did not reach statistical significance (median ages 28 years vs 31 years, p = 0.07; median years of experience 2.2 vs 2.7, p = 0.08).
When asked to identify elements of the bundle, overall 89.4% of respondents answered correctly (143/160) (Figure 3, A). When asked to identify potential negative consequences for a patient who experiences a CLABSI, 95-98.8% of respondents correctly chose increased mortality, morbidity, and longer/costlier hospital stay; but 40.6% (65/160) incorrectly chose “need for a blood transfusion” and “increased likelihood of needing total parenteral nutrition” as well; for an overall correct response rate of 48.1% (77/160) (Figure 3, A).
Opportunity (environmental context, resources, social influences)
A majority of nurses (76.9%, 123/160) described completing the CLABSI bundle as “very easy” or “easy,” (Figure 3, B). Finding required supplies to complete the bundle was “very easy” or “fairly easy” for 92.5% of nurses (148/160), and getting help if needed to complete a bundle element was “very easy” or “fairly easy” for 68.1% (109/160) (Figure 3, B). A majority of nurses at 71.3% (114/160) reported that the clinical care demands of their patient prevented them from completing an element or elements of the CLABSI bundle during at least one shift in the last 6 months (Figure 3, B). Four in five (128/160, 80%) reported that it is stressful to complete the CLABSI bundle elements during a typical PICU shift, (Figure 3, B). Most nurses indicated that they currently receive “a fair amount of support” to complete the CLABSI bundle (85/160, 53.1%), but with over a quarter reporting they receive “very little support” (44/160, 27.5%) (Figure 3, B). When stratifying responses by age and experience level, we did not note any significant differences.
Compared to harm-prevention bundles, CLABSI was most frequently identified as both the most difficult (61/160, 38.1%) and the most time-consuming (92/160, 57.5%) bundle to complete. We received 137 free-text comments from respondents describing why this is the case. Four main themes emerged: the time required to complete the bundle, the need for additional personnel in order to complete the bundle, process or workflow challenges, and patient or family refusal of the bundle (Table 2).
Table 2.
Qualitative insights about the challenges of completing the CLABSI bundle in a PICU setting
| Theme or concept identified by respondents | Example |
|---|---|
| Time required to complete the CLABSI bundle elements | “It is the most time consuming and most protested (by patients). Line changes, cap changes, sheet changes take more time than things like oral care or foley care” “Cap/line changes can be difficult and time consuming if the patient has many infusions” “If there are line changes on critically ill children who are requiring a lot of support via IV medication, it does take a long time to set-up and organize” |
| Additional personnel resources required | “You have to find a second person for dressing changes.” “Need second trained RN to help perform tasks” “[Chlorhexidine] bathing on a larger patient requires additional support which is not always available in a timely fashion” “It often requires additional help which can be difficult to come by during times of high census and high acuity” |
| Physical process or workflow challenges | “The [chlorhexidine] bathing is due when there is a lot of transferring/discharging/admitting on the unit, so the support staff if busy doing those and there is very little help getting the baths done on time” “A patient may be heavier than our backs can handle.” “The CLABSI bundle includes the [chlorhexidine] bath. Often a patient may be unstable for turning” |
| Patient or family refusal of a bundle element | “Parents often also would refuse nightly [chlorhexidine] baths and make it difficult for nurses to get them done” “[Chlorhexidine] bathing can take a long time on some patients who are total care or critically ill, and the task often receives push back from family members” |
Motivation (professional role/identify, beliefs about consequences)
The majority of respondents reported that the CLABSI bundle tasks were either a “very important” or “important” part of their job (155/160, 96.9%) (Figure 3, C). Half of nurses reported that performing the required CLABSI bundle element tasks had prevented them from doing another important clinical care task for a patient in the last 6 months (80/160) (Figure 3, C). The majority of respondents (75.6%, 121/160) reported that their personal motivation for completing the CLABSI bundle tasks is impacted when the medical team (such physicians and nurse practitioners) is highly motivated to prevent CLABSIs, (Figure 3, C). When asked specifically about the impact of the attending physician being highly motivated to prevent CLABSIs, 35.6% (57/160) of nurses are impacted “a great deal,” (Figure 3, C). The majority of nurses surveyed believe that CLABSI bundles are important both to patients’ parents or family members (145/160, 90%) and to hospital leadership (157/160, 98.1%) (Figure 3, C). When stratifying responses by age and experience level, we did not note any significant differences.
Finally, respondents indicated which current resources or strategies are most helpful in achieving optimal CLABSI bundle performance, and which potential new resources or strategies may best improve CLABSI bundle performance. Respondents indicated that a lower PICU census/acuity and more help from nursing colleagues would most likely help to consistently achieve 100% CLABSI bundle compliance (Supplement 4).
Discussion
In this single-center study of pediatric critical care bedside nurses, we found that nurses were highly knowledgeable about the CLABSI bundle (capability), and driven to complete the bundle tasks (motivation), but several factors emerged that prevent optimal adherence to the bundle elements: competing clinical priorities, time constraints, reliance on additional personnel, and patient or family refusal (opportunity). To our knowledge, this is the first time these three specific domains have been assessed in relationship to PICU CLABSI bundle performance. Two main lessons emerge from our findings: 1) using an implementation science framework such as COM-B can be useful in diagnosing incomplete adherence to evidence-based practices, and 2) strategies that address the domain of opportunity, rather than just capability or motivation, may have a strong positive impact on CLABSI bundle performance.
Capability (knowledge, memory, attention, decision processes)
Overall, PICU nurses in this sample are highly knowledgeable about what the CLABSI bundle entails, how to complete those elements, and the consequences of CLABSI. This suggests that interventions focused primarily on ensuring that nurses simply have adequate knowledge about the CLABSI bundle may not be sufficient to increase compliance to target levels. This realization is important considering the limited resources available in many hospitals for harm-prevention work. Continued education or reminders perhaps should be targeted to newer or less experienced members vs the entire team, freeing up resources to investigate non-educational strategies that may have a synergistic or larger impact.
Opportunity (environmental context, resources, social influences)
The domain of opportunity may contain the greatest insights into barriers to CLABSI bundle compliance. Completing the CLABSI bundle tasks can both interfere with clinical care demands of PICU patients and be prevented by clinical care demands of PICU patients. For a majority of nurses in this cohort, completing the CLABSI bundle is a source of stress during a typical PICU shift. CLABSI was identified as the most difficult of the required harm-prevention bundles in place at the CHOP PICU. The length of time required to complete the CLABSI bundle, the need for help from another nurse/colleague, challenges related to busy unit workflow and operations, and resistance from family members emerged as important contributors to the difficulty of these bundle tasks. These findings represent clear potential targets for new interventions to improve bundle compliance. For example, units could consider adjusting the 24-hour time window for completing chlorhexidine bathing to a time of day that is less predictably busy with admissions and discharges; expanding the numbers of nursing technicians or support staff available to assist the bedside nurse in completing the bundle tasks successfully; and partnering with the physician/provider to address family resistance to the bundle tasks and reframing those tasks as essential for good outcomes of the patient.
Survey respondents themselves also provided direct insight on potential strategies to improve bundle performance, though these admittedly may be challenging to realize: a lower PICU census/acuity and more help from nursing colleagues were singled out as most likely help to consistently achieve 100% CLABSI bundle compliance. In our sample, options like feedback about individual performance or reminders in the electronic medical record were chosen less often as potentially useful interventions.
In addition, just over one-quarter of nurses surveyed reported receiving inadequate support to complete the CLABSI bundle elements. Completing stressful tasks in the challenging critical care environment without adequate support can contribute to job dissatisfaction and burnout.19 Unit leadership should take note of how their staff may inadvertently be negatively impacted by the current infrastructure for hospital-acquired harm prevention in their institutions, and proactively strategize how best to mitigate this impact.
Motivation (professional role/identify, beliefs about consequences)
Despite the completion of the CLABSI bundle being a source of stress and one that can make a PICU shift more challenging, nurses demonstrated a high level of motivation for completing this bundle: the overwhelming majority believe it is an important part of their job, and important to both patients/patients’ families, as well as to hospital leadership. Contrary to the existing dogma that tasks like the CLABSI bundle are “nursing jobs” that do not require physician participation, the majority of nurses surveyed here expressed that their motivation to complete the CLABSI bundle is impacted when the medical team, including specifically the attending physician, is also motivated to reduce these infections. This finding represents a prime opportunity to harness multidisciplinary collaboration for the shared goal of improving patient outcomes. Physician involvement in CLABSI prevention can take many forms. One model which has been effective locally in The Children's Hospital of Philadelphia is dedicated central venous line rounds led jointly by a PICU nurse specialist and PICU attending physician, with structured bedside discussions designed to identify barriers to CLABSI bundle completion in real time on a weekly basis.20
Considering our findings in total, it is clear that the entire multidisciplinary team of the pediatric ICU must recognize the challenges the bedside nurse faces in completing a time-intensive series of harm-prevention tasks while providing clinical care to a critically ill child. PICU nurses are highly motivated to complete this harm-prevention task but can face real barriers in the form of patient care demands, inadequate support from colleagues in a busy environment, and family resistance (illustrating a tension between motivation vs opportunity). Addressing these barriers may be difficult in practice, but unit leadership should strongly consider how to mitigate some of them as suggested above to both improve patient outcomes and to promote wellness among their nursing staff. Physician partnership in CLABSI prevention is a strong motivator for individual nurse performance of the CLABSI bundle and dedicated effort should be made to collaborate more intentionally about bedside harm prevention practices.
Additional work is needed to evaluate drivers of CLABSI bundle performance in other institutions, as well as to develop and implement opportunity-targeted strategies to improve performance based on survey results. Such work is currently underway, with the ultimate goal of preventing these infections and improving patient outcomes.
Limitations
The single-center nature of this work limits generalizability, but constrained staff resources and a busy clinical environment are certainly common across many pediatric ICUs nationwide. Our data reflect self-reported practices owing to the survey methodology, without secondary validation of responses. We did not assess every possible construct within the 3 COM-B domains, but a select few in each domain chosen a priori based on investigator expertise and review of the literature. This may have resulted in bias, but to limit survey length, a limited set of constructs was necessary. Finally, our investigator-developed survey items were not validated using psychometric tests and we did not specify themes or domains for our qualitative analysis a priori, owing to the exploratory, pilot nature of this work.
Conclusion
Pediatric critical care nurses are highly knowledgeable and motivated to prevent harmful hospital-acquired bloodstream infections in their patients, but report facing significant challenges to optimal bundle compliance in the form of competing clinical tasks, limited time and personnel resources, and complex interactions with families. Clear potential targets that may improve bundle performance have emerged from this COM-B guided exploration of bundle performance, demonstrating that implementation science frameworks are a powerful tool to optimize the provision of safe, high quality clinical care.
Supplementary Material
Highlights.
Central-line associated bloodstream infections (CLABSIs) have serious negative impact on critically ill children
Compliance by bedside nurses to a best-practice bundle to prevent these infections in the pediatric intensive care unit is suboptimal
Research that harnesses implementation and behavioral science offers new insights into why bundle compliance is challenging in the pediatric intensive care unit
Strategies that facilitate opportunity and optimize motivation, rather than knowledge or capability, may significantly improve CLABSI bundle performance by pediatric intensive care unit nurses
Acknowledgments
Funding source. There were no direct sources of funding for this work. Dr. Woods-Hill received support from a National Institute of Health Ruth L. Kirschstein National Research Service Award (T32HL098054-55) and receives support from The Agency for Healthcare Research and Quality (1R18HS025642). Dr. Lane-Fall receives support from the Robert Wood Johnson Foundation, the NIA, and NHLBI.
Footnotes
Financial Disclosure and Conflicts Statement: Dr. Beidas receives royalties from Oxford University Press and has provided consultation to Merck and Camden Coalition of Healthcare Providers. The authors have no other financial relationships or conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013; 9(3):122–128. [DOI] [PubMed] [Google Scholar]
- 2.Lyren A, Brilli RJ, Zieker K, Marino M, Muething S, Sharek PJ. Children’s hospitals’ solutions for patient safety collaborative impact on hospital-acquired harm. Pediatrics. 2017; 140(3). [DOI] [PubMed] [Google Scholar]
- 3.Ziegler MJ, Pellegrini DC, Safdar N. Attributable mortality of central-line associated bloodstream infection: systematic review and meta-analysis. Infection. 2015; 43: 29–36. [DOI] [PubMed] [Google Scholar]
- 4.Goudie A, Dynan L, Brady PW, Rettiganti M. Attributable cost and length of stay for central line associated bloodstream infections. Pediatrics. 2014; 133 (6): e1525–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller MR, et al. Decreasing PICU Catheter-Associated Bloodstream Infections: NACHRI's Quality Transformation Efforts. Pediatrics. 2010; 125 (2): 206–213. [DOI] [PubMed] [Google Scholar]
- 6.Pronovost P Interventions to decrease catheter-related bloodstream infections in the ICU: the Keystone intensive care unit project. Am J Inf Control. 2008; 36, S171.e1–S171.e5. [DOI] [PubMed] [Google Scholar]
- 7.Ista E, van der Hoven B, Kornelisse R, et al. Effectiveness of insertion and maintenance bundles to prevent central-line associated bloodstream infections in critically ill patients of all ages: a systematic review and meta-analysis. Lancet Infect Dis. 2016; 16: 724–734. [DOI] [PubMed] [Google Scholar]
- 8.Edwards JD, Herzig CT, Liu H, et al. Central-line associated bloodstream infections in pediatric intensive care units: longitudinal trends and compliance with bundle strategies. Am J Infect Control. 2015; 43: 489–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Labeau S, Vereecke A, Vandijck D, Claes B, Blot S. Critical care nurses’ knowledge of evidence based guidelines for preventing infections associated with central venous catheters: an evaluation questionnaire. Am J Crit Care. 2008; 17: 65–71. [PubMed] [Google Scholar]
- 10.Ullman A, Long DA, Rickard CM. Prevention of central venous catheter infections: a survey of pediatric ICU nurses’ knowledge and practice. Nurse Educ Today. 2014; 34: 202–207. [DOI] [PubMed] [Google Scholar]
- 11.Gurses AP, Murphy DJ, Martinez EA, et al. A practical tool to identify and eliminate barriers to compliance with evidence-based practices. Jt Comm J Qual Patient Saf. 2009; 35(10):526–32. [DOI] [PubMed] [Google Scholar]
- 12.Dixon-Woods M, Leslie M, Tarrant C, Bion J. Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci. 2013; 8:70: 167–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michie S, van Stralen MM, West R The behaviour change wheel: a new method for characterising and designing behaviour change interventions Implement Sci, 6 (2011), p. 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson LM, Diaz-Artiga A, Weinstein JR, et al. Designing a behavioral intervention using the COM-B model and the theoretical domains framework to promote gas stove use in rural Guatemala: a formative research study. BMC Public Health. 2018; 18: 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, “Psychological Theory” Group. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005; 14(1):26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Michie S The Behaviour Change Wheel, Theoretical Domains Framework, Behaviour Change Techniques. KT Terminology Meeting. 2012, Ottawa, Canada: Conference proceedings. [Google Scholar]
- 17.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012; 24;7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lydon S, Greally C, Tujjar O, et al. Psychometric evaluation of a measure of factors influencing hand hygiene behaviour to inform intervention. J Hosp Infect. 2019; 102 (4): 407–412. [DOI] [PubMed] [Google Scholar]
- 19.Pastores S, Kvetan V, Coopersmith C, et al. Workforce, Workload, and Burnout Among Intensivists and Advanced Practice Providers: A Narrative Review. Crit Care Med. 2019. April;47(4):550–557. [DOI] [PubMed] [Google Scholar]
- 20.Woods-Hill CZ, Papili K, Nelson E, et al. Improving ICU physician engagement reduces pediatric central-line associated bloodstream infections. Crit Care Med. 2018; 46(1): 636. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.