Abstract
Hydatid disease (HD) is a parasitic endemic zoononis in Tunisia, caused by the larval stage of Echinococcus Granulosus (EG).
Adrenal glands are an uncommon and rare location for hydatid cysts, even in endemic areas, and primary adrenal cysts are exceptional.
Herein, we report a rare case of 46-year-old man with primary giant adrenal hydatid cyst complicated by inferior vena cava thrombosis. The patient was successfully treated with an open adrenalectomy, with prophylactic albendazole therapy pre and postoperatively.
Keywords: Hydatid cyst, Echinococcus granulosus, Adrenal gland, Adrenalectomy
Introduction
Hydatid disease (HD) is a zoonotic disease caused by Echinococcus Granulosus larva, and is endemic in many countries of the Mediterranean region such as North Africa.1
Primary hydatid cysts are most commonly formed in the liver and the lungs. Even in our country in which Echinococcosis is endemic, adrenal involvement is extremely rare, particularly when it presents the primary site.
We report an unusual clinical presentation of a large primary hydatid cyst of the right adrenal gland complicated by inferior vena cava thrombosis.
Case presentation
A 46-year-old man was referred to our department for nonspecific abdominal pain, radiating to the right lumbar region, for several weeks.
The patient had a 6-month history of occasional right-sided abdominal pain and weight loss.
He denied a history of animal contact.
On clinical examination, his abdomen was tender in the right hypochondrium and his vitals were stable.
Laboratory findings were normal. Hydatid serology was positive.
Abdominal sonography revealed a large heterogeneous mass containing internal cystic component measuring 10,6 × 11,6 × 9,2 cm located in the right adrenal gland (Fig. 1). Furthermore, an inferior vena cava (IVC) thrombosis was detected associated with bilateral lower-extremity deep venous thrombosis.
Fig. 1.
Ultrasound image revealing a giant multicystic lesion located in the right adrenal gland.
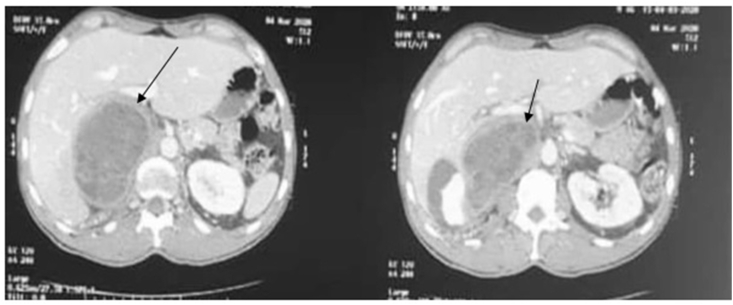
A subsequent abdominal computed tomography (CT) scan showed a giant multi-cystic mass, with thickened and non-enhanced wall, measuring 9,6 × 8,6 × 11,2cm located in the right adrenal gland (Fig. 2) (Fig. 3). Moreover, it confirmed the findings of an extensive IVC thrombosis, with no other abdominal involvement.
Fig. 2.
CT scan-coronal image showing a large adrenal hydatid cyst exerting a mass effect on the upper renal pole.
Fig. 3.
CT scan-axial image demonstrating the adrenal hydatid cyst.
The radiological features were compatible with a hydatid cyst complicated by an IVC thrombus.
Chest CT scan didn't demonstrate any cystic lesion suggesting the primary location of HD in the adrenal gland.
The patient was started on albendazole at a dose of 400 mg twice daily, for two weeks prior to surgery, with therapeutic-dose anticoagulation.
In view of the large sized cyst, he underwent right adrenalectomy through a right subcostal incision while preserving the cyst's integrity. The histopathological examination confirmed the diagnosis of a hydatid adrenal cyst.
The postoperative period was uneventful. The patient underwent albendazole treatment for six weeks. He didn't have any evidence of recurrence during the follow-up period.
Discussion
Most common sites of hydatid cysts are the liver (more than 65%) followed by lungs (20%). Adrenal location is very rare,occurring in less than 1% of all hydatid disease, even in endemic areas.2 It is usually due to a disseminated echinococcosis and primary adrenal hydatid cyst is exceptional.2
Adrenal hydatid cyst disease is most commonly asymptomatic and rarely complicated.3 The majority of adrenal cysts are underrecognized and incidentally identified during radiological studies indicated for other pathological conditions. Nevertheless, symptoms can occasionally occur, resulting from local compression or complicated cysts (rupture, infection, etc.).4 The most common symptoms are lumbar or hypochondrium pain and gastrointestinal complaints (anorexia, nausea, vomiting).3,4
Moreover, clinical presentation may include arterial hypertension, resulting from compression of renal artery, particularly in giant cysts, due to the pressure exerted by the cyst on the glandular parenchyma.
The radiological findings play a key role in the diagnosis of adrenal cystic lesions. Ultrasound is still the first exam performed to orient their location. The CT scan presents currently the modality of choice to identify the accurate location of the cyst and its relationships with surrounding organs. Its diagnostic sensitivity is near to 100%.2 Indeed, hydatid cyst must be differentiated from other cystic lesions such as adrenal pseudocyst, endothelial or epithelial cyst and cystic adrenal neoplasm.
The treatment of choice for adrenal hydatid cyst is surgical and should be as conservative as possible. It consists, ideally, of a simple cystectomy preserving the adrenal gland, except in the case where the adrenal parenchyma is damaged by the cyst.2
Both laparoscopic resection and laparotomy can be performed, depending on the size of the cyst and the presence of complications.
Laparoscopic approach should be avoided in the cases where the cyst is giant or complicated.4
For the open approach, access to the adrenal gland could be either anterior transperitoneal via a subcostal incision, or retroperitoneal through a posterior approach. Furthermore, the open surgery allows the surgeon to ensure a better exploration of the peritoneal cavity. In our case, as the mass was giant, an open adrenalectomy was carried out.
Antiseptic precautions, using hypertonic saline solution, are highly recommended to avoid larvae dissemination and anaphylactic shock in the case of a ruptured cyst during surgery.5 Adjuvant albendazole therapy pre-and postoperatively allows to reduce cystic pressure and the risk of anaphylaxis associated with a decreased recurrence rate(2,5).
Conclusion
Hydatid adrenal cysts remain extremely rare. However, they must be included in the differential diagnosis of adrenal cystic lesions, especially in endemic areas. Clinical features are variable and non-specific. Ultrasonography and CT scan guide clinicians and surgeons in the management of this uncommon adrenal disease. Surgical removal of the cyst remains the recommended treatment.
Finally, the prevention of hydatid contamination remains an imperative step to avoid HD wherever it is located.
Consent
Consent of the patient for publishing was obtained.
Declaration of competing interest
No conflict of interest to be noted.
References
- 1.Borhani M., Fathi S., Lahmar S., Ahmed H., Abdulhameed M.F., Fasihi Harandi M. Cystic echinococcosis in the eastern mediterranean region: neglected and prevailing! PLoS Negl Trop Dis. mai. 2020;14(5) doi: 10.1371/journal.pntd.0008114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geramizadeh B., Maghbou M., Ziyaian B. Primary hydatid cyst of the adrenal gland: a case report and review of the literature. Iran Red Crescent Med J. mai. 2011;13(5):346–347. [PMC free article] [PubMed] [Google Scholar]
- 3.Akbulut S. Incidentally detected hydatid cyst of the adrenal gland: a case report. World J Clin Cases. 16 sept 2016;4(9):269–272. doi: 10.12998/wjcc.v4.i9.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aprea G., Aloia S., Quarto G. Uncommon primary hydatid cyst occupying the adrenal gland space, treated with laparoscopic surgical approach in an old patient. Open Med Wars Pol. 2016;11(1):413–417. doi: 10.1515/med-2016-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spahn S., Helmchen B., Zingg U. Alveolar echinococcosis of the right adrenal gland: a case report and review of the literature. J Med Case Rep. 15 nov 2016;10(1):325. doi: 10.1186/s13256-016-1115-0. [DOI] [PMC free article] [PubMed] [Google Scholar]