Abstract
Objective
From the perspective of percutaneous coronary intervention (PCI) centers, locations of ST‐segment elevation myocardial infarction (STEMI) diagnosis can include a referring facility, emergency medical services (EMS) transporting to a PCI center, or the PCI center's emergency department (ED). This challenges the use of door‐to‐balloon‐time as the primary evaluative measure of STEMI treatment pathways. Our objective was to identify opportunities to improve care by quantifying differences in the timeliness of STEMI treatment mobilization based on the location of the diagnostic ECG.
Methods
This 3‐year, single‐center, retrospective cohort study classified patients by diagnostic ECG location: referring facility, EMS, or PCI center ED. We quantified door‐to‐balloon‐time and diagnosis‐to‐balloon‐time with its care subintervals.
Results
Of 207 ED STEMI patients, 180 (87%) received PCI. Median diagnosis‐to‐balloon‐times were shortest among the ED‐diagnosed (78 minutes [interquartile range (IQR), 61‐92]), followed by EMS‐identified patients (89 minutes [IQR, 78‐122]), and longest among those referred (140 minutes [IQR, 119‐160]), reflecting time for transport to the PCI center. Conversely, referred patients had the shortest median door‐to‐balloon‐times (38 minutes [IQR, 34‐43]), followed by the EMS‐identified (64 minutes [IQR, 47‐77]), whereas ED‐diagnosed patients had the longest (89 minutes [IQR, 70‐114]), reflecting diagnosis and catheterization lab activation frequently occurring before PCI center ED arrival for referred and EMS‐identified patients.
Conclusions
Diagnosis‐to‐balloon‐time and its care subintervals are complementary to the traditional door‐to‐balloon‐times as measures of the STEMI treatment process. Together, they highlight opportunities to improve timely identification among ED‐diagnosed patients, use of out‐of‐hospital cath lab activation for EMS‐identified patients, and encourage pathways for referred patients to bypass PCI center EDs.
Keywords: cardiovascular emergency, diagnosis‐to‐balloon, door‐to‐balloon, emergency care, myocardial infarction, STEMI, STEMI care system, time‐to‐treatment, timely care
1. INTRODUCTION
1.1. Background
ST‐segment elevation myocardial infarction (STEMI) is a life‐threatening disease that can result in irreversible myocardial damage when untreated. Delays in treatment, on the order of minutes are associated with increased mortality and worsening cardiac functional outcomes. 1 This understanding of STEMI pathophysiology has led to the emergency care mantra: “time is myocardium.” 2 To facilitate rapid treatment, international guidelines recommend that out‐of‐hospital clinicians refer patients with symptoms suggestive of STEMI to an emergency department directly or via emergency medical service (EMS) transport. 1 , 3 , 4 , 5 These guidelines recommend the acquisition and diagnostic interpretation of an ECG within 10 minutes of emergency department (ED) arrival. Treatment is rapidly coordinated after diagnosis. The preferred treatment is percutaneous coronary intervention (PCI) provided in a cardiac catheterization (cath) lab by interventional cardiology specialists. 6 The benefits of PCI have been previously shown to outweigh procedural risks when provided within 90 minutes of ED arrival or contact with the emergency care system. 7 In addition, PCI is superior to the alternative therapy of thrombolysis when provided within 120 minutes. 7 As a result, door‐to‐balloon time has become a key process measure for STEMI care, with a target of < 90 minutes. 2 , 3 The diagnosis of STEMI, however, occurs in various locations that may be before or after a patient's "door" time. 3 This challenges the use of door‐to‐balloon time as the most informative temporal measure of STEMI treatment pathways.
1.2. Importance
From the perspective of a PCI center, diagnosis can occur with an ECG acquired either by a referring clinician, 8 the EMS team transporting to a PCI center ED, 9 , 10 , 11 or the PCI center's ED. 12 Because referring clinicians and EMS personnel often initiate communication with the receiving PCI center facility before arrival, 2 , 3 , 10 the location of diagnostic ECG acquisition is associated with varying degrees of engagement with the interdisciplinary emergency STEMI care system, prearrival mobilization of the treatment team, and proximity to treatment resources. 13 Thus, the role of the receiving PCI center ED can differ depending on whether and where the diagnostic ECG is done. Achieving arrival‐to‐PCI treatment (door‐to‐balloon) time within 90 minutes is the traditional measure of timely STEMI care quality and performance. 2 , 3 We posit that diagnosis‐to‐balloon time provides complementary information on patients’ care course relative to the time the need for treatment is identified.
1.3. Goals of this investigation
We examine key process interval differences for ED STEMI patients grouped by the location of their diagnostic ECG. Our objective was to provide a comparison of timely emergency STEMI treatment mobilization and delivery to identify opportunities for STEMI care process improvement that may be masked by door‐to‐balloon time.
2. METHODS
2.1. Study design and setting
This single‐center, retrospective cohort study was conducted in patients with STEMI whose emergency care was facilitated through our urban academic PCI center ED. We received institutional review board approval before study initiation.
2.2. Selection of participants
Our study population included all patients receiving a final hospital International Classification of Diseases (ICD) diagnosis code consistent with STEMI 14 who presented to the ED from January 1, 2014 to December 31, 2016. The cohort was obtained via data extraction from the hospital electronic health record (EHR) data repository, 15 , 16 including medical record number, name, date of service, date of birth, and ICD‐coded final diagnoses. To best describe care delivered for those who ultimately needed PCI intervention, we subsequently excluded patients without evidence of an acute STEMI presentation, as well as those with evidence of an alternative primary diagnosis whose cath findings were inconsistent with STEMI. A detailed description of the methodology to identify our patient population is included in Supplement I, which was adapted from an approach used in previously published work. 15 , 16
2.3. Comparison groups
We stratified patients based on the location of the diagnostic ECG. The diagnostic ECG was defined as the one used to activate the cath lab. Those diagnosed with STEMI by a referring facility are described as referred. Examples of referral sources included a referring ED, urgent care clinic, clinic‐based cardiologist, or primary care setting. Those whose diagnostic ECG was acquired by an EMS team are the EMS identified, and those diagnosed within the PCI center ED are the ED diagnosed.
2.4. STEMI care intervals
Our primary measure was the diagnosis‐to‐PCI balloon inflation time, complementary to the more traditional door‐to‐balloon time. Our time‐0 was the completion of the diagnostic ECG as the point when data were available to identify the patient as potentially eligible for treatment.
We defined balloon time as the time of first balloon inflation during PCI. When documentation of this event time was absent, we used the time the balloon guidewire crossed the coronary lesion. 10 Because the diagnostic team has a limited ability to influence the interventional cardiologist's case start and balloon inflation times, 13 we added the time to cath lab arrival as a diagnostic team‐centric performance measure. In addition, we looked at subintervals of care including the times from (1) the diagnostic ECG to cath lab activation, (2) cath lab activation to cath lab arrival, and (3) cath lab arrival to balloon inflation. These measures follow an event sequence from diagnosis (diagnostic ECG) to request for intervention (cath lab activation), to transition of care from the diagnostic to intervention team (cath lab arrival), and intervention (balloon inflation).
2.5. Other variables
We abstracted age, sex, race, ethnicity, time of presentation, 17 and the arrival chief complaint. The arrival chief complaint included the first or second complaint documented during arrival registration or triage. The shortest driving distance from the patient's home to the hospital was calculated using google.com/maps.com as a proxy measure for variation in proximity to PCI‐care access. We also compared the proportion of patients diagnosed during cath lab business hours (when a full interventional team is within the hospital) versus off hours (when the interventional team is outside of the hospital but on call).
The Bottom Line
The speed of ST‐segment elevation myocardial infarction (STEMI) door‐to‐balloon care may be influenced by the timeliness of its recognition and notification. In this retrospective analysis of 207 cases at a university hospital, STEMI door‐to‐balloon time was shorter for cases referred by community hospitals (median 38 minutes) or identified by EMS (64 minutes), compared with cases diagnosed in the local emergency department (89 minutes). These findings underscore the importance of early STEMI recognition in accelerating STEMI care.
2.6. Data collection
Study data were obtained for patients in the identified cohort via manual chart review by 3 data abstractors (OOO, JLW, VDA), who each received 2 hours of standardized training that involved a 90‐minute training module with practice data collection and data collection accuracy verified by the study team. The training process and content have been previously published. 14 Data from each patient's medical record was abstracted using the data collection instrument included in Supplement I. We managed anticipated coding misclassification by requesting data abstractors flag cases for potential exclusion when care was not facilitated by the ED, there was no ED or final hospital diagnosis of STEMI (reflecting coding misclassification), or coronary angiography found no evidence of STEMI and an alternative hospital diagnosis was identified for which in‐hospital care was most consistent. Flagged cases underwent additional review by the principal investigator who determined whether the case should be included or excluded based on the prespecified eligibility criteria. Additional data checks were implemented to minimize missingness and to ensure STEMI care event timestamps were temporally consistent (eg, date of birth occurring before ED arrival, which is before balloon time; see Supplement II for detail).
2.7. Defining the occurrence of STEMI care events
With advancement through the STEMI Chain of Survival, 18 population attrition is expected as non‐PCI treatment is elected for some patients. Alternative treatment options may include thrombolysis, medical management, hospice/comfort care, or no care. The absence of data, however, can be the result of an event not occurring or missing data. To quantify attrition from the first ECG through PCI, we identified the occurrence of STEMI care events (ie, first ECG, diagnostic ECG, cath lab activation, cath lab arrival, and balloon inflation) from available data even when documentation of the event's timestamp was not available in the medical record. The specific logic used to derive evidence of each STEMI care event is included in Supplement III.
2.8. Analysis
Descriptive statistics were calculated using medians with interquartile ranges for continuous variables and proportions for categorical variables. Group comparisons were conducted using Kruskal‐Wallis test for continuous variables, chi‐square test for categorical variables, and the Fisher's exact test when categorical outcomes included < 5 patients. Significance was set a priori at P < 0.05. Statistical analyses were performed using the R statistical software, Version 3.4.2.
3. RESULTS
3.1. Characteristics of study subjects
There were 147 ED‐diagnosed, 56 EMS‐identified, and 4 referred patients for a total of 207. There were no statistically significant demographic differences observed between patient groups. The ED‐diagnosed patients, however, had a lower proportion of patient presenting with chest pain (Table 1). The flow of patients through the STEMI care pathway are shown for each group in Figure 1. Overall, the first ECG was the diagnostic ECG for 85% (175/207), the cath lab was activated for 93% (192/207), 90% (187/207) arrived in the cath lab and had cardiac catheterization performed, and 87% (180/207) received PCI. Of those receiving PCI, 69% (126/180) were ED‐diagnosed patients, 28% (51/180) were EMS‐identified and 2% (3/180) were referred patients. The median door‐to‐diagnostic ECG time varied significantly between the 3 patient groups. The median time was ‐101 (interquartile range [IQR], −204 to −46) minutes among referred patients, −32 (IQR, −50 to −15) minutes for EMS‐identified patients, and 7 (IQR, 5 to 17) minutes for ED‐diagnosed patients (P < 0.001). Negative time is reflective of diagnosis occurring before PCI center ED arrival in the referred and EMS‐identified groups.
TABLE 1.
Emergency department ST‐segment elevation myocardial infarction (STEMI) patients demographics by location of the diagnostic ECG
| Available data patient sample (N) | Total population N = 207 | ED‐diagnosed (diagnosis after arrival) N = 147 | EMS‐diagnosed (diagnosed en route to PCI center ED) N = 56 | Referred (diagnosed before transport ED arrival) N = 4 | P * | |
|---|---|---|---|---|---|---|
|
Age (years)† < 65 ≥65 |
207 |
55 62 70 62% (128) 38% (79) |
55 61 69 64% (94) 36% (53) |
55 62 73 57% (32) 43% (24) |
55 62 70 50% (2) 50% (2) |
0.84 |
|
Sex Female |
207 |
27% (55) |
27% (39) |
29% (16) |
0% (0) |
0.46 |
|
Race White Black Other |
205 |
88% (180) 11% (22) 1% (3) |
87% (127) 11% (16) 2% (3) |
89% (49) 11% (6) 0% (0) |
100% (4) 0% (0) 0% (0) |
0.90 |
|
Ethnicity Hispanic Non‐Hispanic Unknown |
207 |
1% (3) 92% (190) 7% (14) |
< 1% (2) 93% (136) 6% (9) |
2% (1) 89% (50) 9% (5) |
0% (0) 100% (4) 0% (0) |
0.92 |
|
Insurance status Private Medicare Self‐pay/unknown Other Medicaid |
206 |
45% (92) 19% (40) 34% (69) 2% (4) 0% (1) |
48% (70) 18% (26) 32% (47) 2% (3) < 1% (1) |
35% (19) 24% (13) 39% (22) 2% (1) 0% (0) |
75% (3) 25% (1) 0% (0) 0% (0) 0% (0) |
0.45 |
| Established primary care Yes | 148 | 80% (118) | 79% (84) | 82% (31) | 100% (3) | 0.90 |
|
Distance from the hospital† Miles from home address |
202 | 11 25 65 | 9.2 25 60 | 12 20 69 | 57 79 87 | 0.33 |
|
Arrival chief complaints‡ Chest pain Shortness of breath Shoulder/neck pain Abdominal pain |
207 |
74% (153) 25% (51) 9% (18) 2% (4) |
69% (101) 29% (42) 8% (12) 2% (3) |
86% (48) 16% (9) 9% (5) 0% (0) |
100% (4) 0% (0) 25% (1) 25% (1) |
0.02 0.12 0.42 0.05 |
| Door to diagnostic ECG† | 207 | ‐12 5 10 | 5 7 17 | ‐50 ‐32 ‐15 | ‐204 ‐101 ‐46 | <0.001 |
|
Cases occurring during cath lab Business hours After hours |
185 |
44% (82) 56% (103) |
44% (55) 56% (71) |
45% (25) 55% (31) |
67% (2) 33% (1) |
0.73 |
Cath, catheterization; ED, emergency department; EMS, emergency medical services; PCI, percutaneous coronary intervention.
P values calculated using the Pearson chi‐square test for continuous and categorical outcomes, and Fisher's exact test when categorical outcomes includes < 5 patients. †a b c where a represent the lower quartile, b the median, and c the upper quartile for continuous variables. Numbers after proportions are frequencies. ‡Presented are the chief complaints reported during ED intake. Arrival chief complaints are not mutually exclusive.
FIGURE 1.
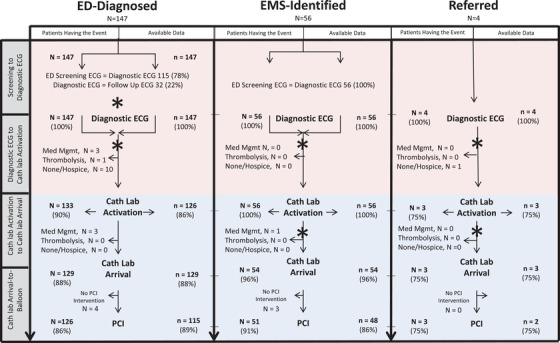
ST‐segment elevation myocardial infarction (STEMI) patients’ care course and treatment intervals by location of diagnosis. Within the 3 emergency department STEMI patient subcohorts, *denotes when a patient's PCI center ED arrival time may occur at varying points along the STEMI care pathway. Within each subcohort panel sample sizes (N) on the left represent patients whose medical course included evidence they had the STEMI care event: (1) first or screening ECG, (2) diagnostic ECG (which may also be the screening ECG), (3) cath lab activation, 4) cath lab arrival, (5) PCI; sample sizes (n) on the right represent patients with documented timestamps for the beginning and end of each care interval, thus permitting the measure of (1) screening‐ECG‐to‐diagnostic‐ECG, (2) diagnostic‐ECG‐to‐cath lab activation, (3) cath‐lab‐activation to cath‐lab‐arrival, and (4) cath‐lab‐arrival‐to‐balloon‐times. EMS, emergency medical services; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction
3.2. Door versus diagnosis to treatment times
Of the 165 ED STEMI PCI patients, who had complete STEMI event timestamp data (92% of the 180 PCI patients), median diagnosis‐to‐balloon times were shortest among the ED‐diagnosed (78 minutes [IQR, 61‐92]), followed by EMS‐identified patients (89 minutes [IQR, 78‐122]), and longest in the referred patients (140 minutes, [IQR, 119‐160]). The percentage of PCI patients receiving treatment within 90 minutes of diagnosis was 73% (84/115) of the ED‐diagnosed, 52% (25/48) of the EMS‐identified, and 0% (0/2) of the referred patients (Figure 2).
FIGURE 2.
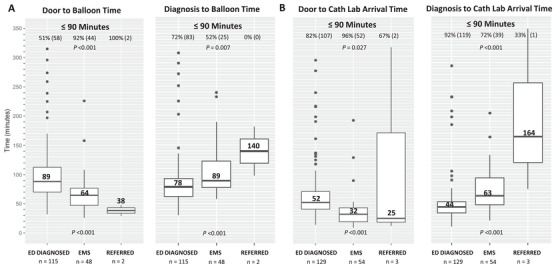
Door versus diagnosis to treatment times for emergency department ST‐segment elevation myocardial infarction (STEMI) patients. Panel A provides side‐by‐side comparisons of door‐to‐balloon and diagnosis‐to‐balloon times for the acute STEMI patients who received percutaneous coronary intervention (PCI) whose care was facilitated by the emergency department in the form of box‐and‐whisker plots. The central dark line within each box is the median, top, and bottom of the box are the 75th and 25th percentiles, and the whiskers represent the tails of the width of the data distribution with outlier cases presented as black circles. Each measure is separated by location of diagnosis cohorts including those diagnosed with STEMI via an electrocardiogram (ECG) acquired in the PCI center ED (ED‐diagnosed), emergency medical services (EMS), or a referring facility (referred). Panel B presents an analogous, but diagnostic‐team‐centric comparison for door‐to‐cathlab‐arrival and diagnosis‐to‐cathlab‐arrival times. Sample sizes (n) include patients with available data. See Supplement IV eTable 1 for additional data detail
Conversely, referred patients had the shortest door‐to‐balloon times (38 minutes [IQR, 34‐43]), followed by the EMS‐identified (64 minutes [IQR, 48‐77]), whereas ED‐diagnosed patients had the longest (89 minutes [IQR, 70‐114]). The percentage of patients receiving treatment within 90 minutes of documented door time was 100% (2/2) of the referred patients, 92% (44/48) of the EMS‐identified patients, and 51% (59/115) of the ED‐diagnosed patients (Figure 2).
Time from the door to cath lab arrival and from diagnosis to cath lab arrival illustrated similar patterns across groups (Figure 2).
3.3. Diagnosis to treatment care subintervals
Referred patients had the longest median time from diagnosis to cath lab activation (140 minutes, [IQR, 87‐195] and from cath lab activation to cath lab arrival (41 minutes [IQR, 32‐69]). The shortest median times were seen among the ED‐diagnosed patients where we observed a median of 8 minutes [IQR, 5‐15] from diagnosis to cath lab activation and 31 minutes [IQR, 21‐40] from cath lab activation to cath lab arrival (Figure 3A and 3B). We observed the inverse pattern with time from cath lab arrival to balloon (Figure 3C) where referred patients had the shortest median time (20 minutes [IQR, 18‐22]), followed by EMS‐identified patients (median 30 minutes [IQR, 24‐36] and ED‐diagnosed patients, who had the longest interval (median 31 minutes [IQR, 24‐43]).
FIGURE 3.
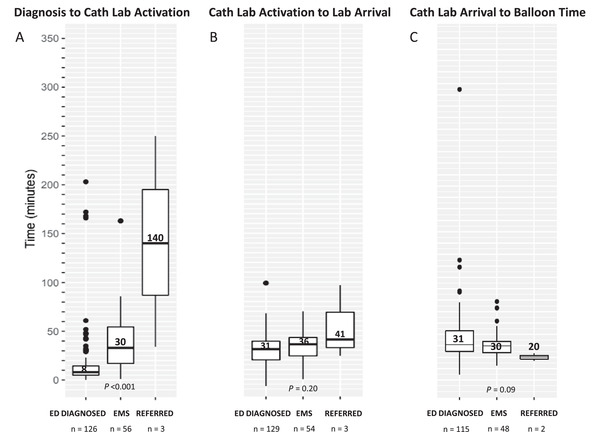
Diagnosis to percutaneous coronary intervention balloon time subintervals. Presented are side‐by‐side presentations of ST‐segment elevation myocardial infarction (STEMI) care intervals from diagnosis to percutaneous coronary intervention (PCI) balloon inflation in the form of box and whisker plots. The central dark line within each box is the median, top, and bottom of the box are the 75th and 25th percentiles, and the whiskers represent the tails of the width of the data distribution with outlier cases presented as black circles. Each measure is separated by location of diagnosis cohorts including those diagnosed with STEMI via an ECG acquired in the PCI center emergency department (ED‐diagnosed), emergency medical services (EMS), or a referring facility (referred). Panel A presents diagnosis‐to‐cathlab‐activation times, Panel B presents cathlab‐activation‐to‐lab‐arrival times, and Panel C presents cathlab‐arrival‐to‐balloon time. Sample sizes (n) include patients with available data. See Supplement II Table e1 for data detail
4. LIMITATIONS
Studying emergency STEMI care from the perspective of a PCI center afforded several benefits that were not without limitations. It reduced variation in the diagnosis‐to‐treatment interval associated with different intervention targets for PCI (within 90 minutes) versus thrombolysis (within 30 minutes). In addition, colocation of the ED and cath lab within one hospital facility enhanced our access to patient data despite a care transition from emergency medicine to cardiology. Having PCI as the primary form of treatment provided a unified target for timely intervention but resulted in the exclusion of those who did not receive PCI as their intervention (13%, 27/207) from our door and diagnosis to balloon measures (Figure 1). This limits the generalizability of our findings to ED STEMI patients who receive other forms of treatment. We have, however, provided care process measures of STEMI care subintervals and represented the expected attrition that occurs as alternative treatment plans are established (Figure 1). In addition, referencing the perspective of a PCI center does not include all patients diagnosed with STEMI in the referring facilities, as many referring facilities will transfer patients to > 1 center, and the majority of referred patients bypass the PCI center ED for direct transportation to the cath lab. Those patients were not part of this study.
We present data for referred patients’ diagnosis‐to‐treatment course. Our measures, however, should be interpreted with caution given the small cohort sample. The ability of a referring facility to initiate activation of a PCI center's cath lab has been a major focus of efforts to improve timely care by reducing delays associated with the interfacility care transition. 25 , 32 , 33 , 36 The resultant structured communication and information transfer removes the need for all transferred patients to be reevaluated in the receiving PCI center's ED. Thus, referred patients whose care course is stable can bypass the PCI center's ED. As a result, the majority of referred patients were not part of this ED‐focused study. This limited the need to focus on their care in this study. However, the ED is available as a safety net when those transporting patients are unable to navigate to the cath lab or need emergent resuscitation. As a result, our sample included an appropriately small number of referred patients.
Lastly, the proportion of patients in each cohort is influenced by the preexisting EMS network and interfacility relationships that can facilitate or hinder referrals. We observed that all referred patients were male, non‐Hispanic, and had chest pain, established primary care, and insurance. These findings were not statistically significantly different, but this may be an artifact of the small sample size. A multicentered study may be helpful to understand variation associated with different referral facility and EMS environments. Despite these limitations, our methodology presents a framework to better examine the contemporary emergency STEMI care system.
5. DISCUSSION
Our data suggest door‐to‐balloon time may mask differences in the timeliness of care among patients diagnosed in different locations, which can be uncovered by also examining diagnosis‐to‐balloon time and its care subintervals.
5.1. Importance of findings
Referred patients had the shortest median PCI center door‐to‐balloon time with 38 minutes, yet their median diagnosis‐to‐balloon time was nearly 3.7 times longer at 140 minutes. This places them outside the timely PCI target of 90 minutes and the extended target of 120 minutes. 19 Cath lab activation for referred patients frequently occurs before PCI center ED arrival. Although this may result in a reduction in door‐to‐balloon time, it may not expedite overall care because of transportation time and other delays. The long diagnosis‐to‐balloon time illustrates existing concerns over differential care quality from delayed intervention in this cohort. 20 Although there were only 4 patients in this group, timely care may be improved by having referred patients with a preceding ED visit bypass the PCI center ED to go directly to the cath lab. 21
Conversely, ED‐diagnosed patients had the longest door‐to‐balloon times with a median of 89 minutes, yet the shortest diagnosis‐to‐balloon times with a median of 78 minutes. The median difference represents the time between the “door” and “diagnosis,” which is 11 minutes. Guidelines advise a target of 10 minutes. Noting that a median is the 50th percentile; this reflects a large proportion of ED‐diagnosed patients experiencing untimely identification. Once diagnosed, however, they benefit from cath lab transportation efficiencies owing to proximity. Prior work has noted timely identification of STEMI patients is a persistent care performance issue made challenging by a notable number of patients presenting with atypical presentations in tandem with a declining STEMI prevalence. 22 , 23 , 24
The timeliness of care for the EMS‐identified patient group, whose diagnostic ECG is often acquired just before ED arrival, fell consistently between that of the referred and ED‐diagnosed patients. EMS‐identified patients had a marked difference between median door‐to‐balloon time and diagnosis‐to‐balloon time (64 vs 89 minutes). This 25‐minute difference reflects prearrival time that could be used more effectively to expedite the patient's movement to treatment. The STEMI care best‐practice consortium, Mission Life Line, recommends using EMS ECGs to activate the cath lab to reduce this source of care delay. 25 This is often done by EMS directly activating the cath lab before arrival 26 or via facilitated activation by a physician after transmission of the ECG for interpretation. 27 In a post hoc analysis, we separated the EMS‐identified group into cases where the EMS agency routinely used prearrival cath lab activation compared to those who did not. We found that agencies using prearrival cath lab activation saved ≈ 12 minutes given the median diagnosis‐to‐cath‐lab‐activation time of 27 minutes (IQR, 10‐39) compared to 39 minutes for EMS agencies that did not use prearrival cath lab activation (IQR, 21‐57). We also saw differences in median door‐to‐balloon time between those that awaited ED arrival for activation (69 minutes [IQR, 63‐80]) and those with activation in the ED (50 minutes [IQR, 43‐65]). This is consistent with prior work suggesting EMS‐initiated cath lab activation may improve timely care for patients with a diagnostic ECG acquired en route to a PCI center. 8 , 9 , 10 , 11 , 12 , 16 , 21 , 26 , 27
Earlier literature described marked variation in cath lab‐arrival‐to‐balloon inflation time. 28 We found no significant differences among the median time of this care interval for ED‐diagnosed (31 minutes) and EMS‐identified patients (30 minutes). However, among the 2 referred patients the median time was shorter (20 minutes) (Figure 3). This may be because of the extended transport time for referred patients providing the cath team more lead time to prepare but requires further investigation in a larger patient sample. The cath lab‐arrival‐to‐balloon times observed among our location‐of‐diagnosis comparison groups are shorter than those previously reported. 28 This may be because of the uptake of guidelines that advise the use of focused diagnostic angiography on the suspected culprit lesion and intervention that precedes exploration of other coronary arteries. 2 , 29 The shift in practice resulting from these guidelines may also account for us observing less variation.
5.2. Utility of diagnosis‐to‐balloon time and STEMI care intervals
When door‐to‐balloon time emerged as an important quality measure for timely STEMI care, the only clinician able to confirm the suspected diagnosis and activate the cath lab was a bedside consulting cardiologist at the hospital of a PCI‐capable facility. 30 , 31 , 32 Early efforts to reduce door‐to‐balloon time focused on shortening the time from ED arrival to cath lab activation. 31 , 32 , 33 This included permitting emergency physicians to activate the cath lab, structured pathways for referring hospitals to bypass routine reevaluation in the PCI‐capable facility's ED, and having EMS agencies activate the cath lab directly or via prearrival facilitation by an emergency physician. As a result, there are now multiple clinicians to move patients from diagnosis to treatment.
Referred and EMS‐identified patient populations have the potential for diagnosis and cath lab activation to occur before PCI‐facility ED arrival. Consequently, PCI center ED arrival or “door” time is no longer always the first step in the sequence of emergency STEMI care events. Most facilities diagnosing patients with STEMI are not PCI capable, 34 so connecting a STEMI patient with PCI involves interfacility transfer. 35 Consequently, ensuring STEMI patients receive care within the recommended 90 minutes requires understanding and measuring the full trajectory from diagnosis to treatment. Door‐in‐door‐out time was developed for referring facilities, who are unable to directly influence a patient's journey to balloon intervention after ED departure. 36 , 37 This measures activity within the referring facility's locus of control. However, the efficiency of the sometimes complex coordination of emergent treatment at another facility is better informed with a measure of the diagnosis‐to‐treatment process.
Similarly, we lack strong metrics for EMS's specific influence on the timeliness of STEMI treatment. The EMS‐identified cohort may include patients transferred from an outside hospital ED to a receiving facility whose clinical state changed en route and prompted an ECG. It also includes patients whose first medical contact is with EMS after a 911 emergency response call. Prearrival activation affords patients the opportunity to potentially bypass the ED or have the cath lab team mobilize while a patient is simultaneously stabilized or medically optimized. First medical contact (FMC) is a time‐0 for measures that capture STEMI screening, diagnosis, and treatment. However, it lacks a common time 0 with other ED STEMI patients for treatment pathway comparison and the inclusion of EMS documentation within hospital records is still maturing. 36 Examining the diagnostic ECG‐to‐balloon time and subintervals provides more comparable treatment measures.
Because of changing clinical practice, the true opportunity for a STEMI patient to engage the emergency treatment pathway is after the diagnostic ECG is acquired rather than ED arrival. In addition, examination of the subintervals of the emergency STEMI care pathway is needed to uncover intervention and process improvement opportunities. Figure 3 separates the diagnosis‐to‐treatment pathway into 3 component intervals. Despite many clinical disciplines involved in moving a patient through these steps, few care clinicians can directly influence > 2 intervals of this pathway. Care teams need to have tools to measure processes within their locus of control and to understand how performance within subintervals affects overall performance. As a result, timely care performance measures need to account for (1) variation in patients’ experience by location of diagnosis, and (2) the clinicians primarily responsible for progression to the next phase of care.
In conclusion, diagnosis‐to‐balloon time and its care subintervals are complementary to traditional door‐to‐balloon times as measures of the STEMI treatment process. Together, they highlight opportunities to improve timely emergency STEMI treatment. Efforts to improve door‐to‐balloon time have diversified the pool of involved clinicians and pathways to PCI and increased the number of STEMI treatment activities occurring before ED arrival. Examining care subintervals among patients by location of diagnosis can uncover process improvement opportunities that are otherwise masked. Our results suggest persistent opportunity may lie in improving the timelines of diagnosis among the ED‐diagnosed patients by recognizing the first ECG is not always the diagnostic ECG, increasing the use of out‐of‐hospital cath lab activation in the referred and EMS‐diagnosed patients, and encouraging pathways for referred patients to bypass the PCI center ED.
AUTHOR CONTRIBUTIONS
OOO lead the study design, data collection and cleaning, and drafting of the manuscript. MYABY conceptualized the study, design, and the interpretation of results, and drafting of the manuscript. CA performed the statistical analysis. DL and CJL provided design and statistical analysis oversight. KFM developed the study database and clarified study variables and assisted with the process of data collection. JLW and VDA performed study data collection and data cleaning with OOO. ABS provides senior scientific guidance for the course of the study. All authors contributed to and edited the final form of the manuscript.
Supporting information
Supporting Information
ACKNOWLEDGMENT
We extend thanks to the Emergency Care Health Services Research Data Coordinating Center (HSR‐DCC) support staff, Brittney Jackson, Kelsea Hadley, and Christina Kampe, for their administrative support of this study; and to Dr. Stephan Russ and the Vanderbilt Institute of Clinical and Translational Research's Research Derivative for extracting core patient cohort data from the Vanderbilt electronic medical record data warehouse.
Biography
Maame Yaa A. B. Yiadom, MD, MPH, is an Assistant Professor of Emergency Medicine at Vanderbilt University.

Yiadom MYAB, Olubowale OO, Jenkins CA, et al. Understanding timely STEMI treatment performance: A 3‐Year retrospective cohort study using diagnosis‐to‐balloon‐time and care subintervals. JACEP Open. 2021;2:e12379 10.1002/emp2.12379
Disclosures: Dr. Storrow has received grant funding from Abbott Diagnostics and Roche Diagnostics. He is a consultant for Quidel. Dr. Bernard is a clinical trials data safety monitoring consultant for Bayer AG. All other authors have no disclosures.
Funding and support: Research reported in this publication was supported by the National Institutes of Health's (NIH) National Heart Lung and Blood Institute's (NHLBI) award numbers 5K12HL109019, 1K23HL133477, Bethesda, Maryland; and the National Center for Advancing Translational Sciences (NCATS) award number UL1TR000445, Bethesda, Maryland. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the design, conduct, collection, analysis, or interpretation of the data; nor were they involved in the preparation, review, or approval of the manuscript.
Supervising Editor: Henry Wang, MD, MS.
REFERENCES
- 1. Shiomi H, Nakagawa Y, Morimoto T, et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;344:e3257. [DOI] [PubMed] [Google Scholar]
- 2. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. JACC. 2013;61(4):e78‐140. [DOI] [PubMed] [Google Scholar]
- 3. Bradley EH, Roumanis SA, Radford MJ, et al. Achieving door‐to‐balloon times that meet quality guidelines: how do successful hospitals do it?. J Am Coll Cardiol. 2005;46(7):1236‐1241. [DOI] [PubMed] [Google Scholar]
- 4. Steg PG, James SK, Gersh BJ. 2012 ESC STEMI guidelines and reperfusion therapy: evidence‐based recommendations, ensuring optimal patient management. Heart. 2013;99(16):1156‐1157. [DOI] [PubMed] [Google Scholar]
- 5. Wessler JD, Stant J, Duru S, Rabbani L, Kirtane AJ. Updates to the ACCF/AHA and ESC STEMI and NSTEMI guidelines: putting guidelines into clinical practice. Am J Cardiol. 2015;115(5):23A. [DOI] [PubMed] [Google Scholar]
- 6. Vermeer F, Oude Ophuis AJM, van den Berg EJ, et al. Prospective randomized comparison between thrombolysis, rescue PTCA, and primary PTCA in patients with extensive myocardial infarction admitted to a hospital without PTCA facilities: a safety and feasibility study. Heart. 1999;82:426‐431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grines CL, Westerhausen DR Jr, Grines LL, et al. A randomized trial of transfer for primary angioplasty versus on‐site thrombolysis in patients with high‐risk myocardial infarction: the air primary angioplasty in myocardial infarction study. JACC. 2002;39:1713‐1719. [DOI] [PubMed] [Google Scholar]
- 8. Moyer P, Ornato JP. Development of systems of care for ST‐elevation myocardial infarction patients: the emergency medical services and emergency department perspective. Circulation. 2007;116:e43‐e48. [DOI] [PubMed] [Google Scholar]
- 9. Swor R, Hegerberg S, McHugh‐McNally A, Goldstein M, McEachin CC. Prehospital 12‐lead ECG: efficacy or effectiveness?. Prehosp Emerg Care. 2006;10(3):374‐377. [DOI] [PubMed] [Google Scholar]
- 10. Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre‐hospital electrocardiograms for patients with acute ST‐segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. JACC. 2009;53(2):161‐166. [DOI] [PubMed] [Google Scholar]
- 11. Rokos IC, French WJ, Koenig WJ, et al. Integration of pre‐hospital electrocardiograms and ST‐elevation myocardial infarction receiving center (SRC) networks: impact on door‐to‐balloon times across 10 independent regions. JACC Cardiovasc Interv. 2009;2(4):339‐346. [DOI] [PubMed] [Google Scholar]
- 12. Committee NationalHeartAttackAlertProgramCoordinating, Group 60MinutestoTreatmentWorking . Emergency department: rapid identification and treatment of patients with acute myocardial infarction. Ann Emerg Med. 1994;23:311‐329. [PubMed] [Google Scholar]
- 13. Krumholz HM, Anderson JL, Bachelder BL, et al. ACC/AHA 2008 performance measures for adults with ST‐elevation and non‐ST‐elevation myocardial infarction: a report of the ACC/AHA task force on performance measures. Circulation. 2008;118:2596‐2648. [DOI] [PubMed] [Google Scholar]
- 14. Ward MJ, Kripalani S, Zhu Y, et al. Incidence of emergency department visits for ST‐elevation myocardial infarction in a recent six‐year period in the United States. Am J Cardiol. 2015;115:167‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yiadom MYAB, Mumma BE, Baugh CW, et al. Measuring outcome differences associated with STEMI screening and diagnostic performance: a multi‐centred retrospective cohort study protocol. BMJ Open. 2018;8:e022453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA. 2005;294(7):803‐812. [DOI] [PubMed] [Google Scholar]
- 18. Ornato JP. The ST‐segment‐elevation myocardial infarction chain of survival. Circulation. 2007;116(1):6‐9. [DOI] [PubMed] [Google Scholar]
- 19. Bates ER, Jacobs AK. Time to treatment in patients with STEMI. NEJM. 2013;369(10):889. [DOI] [PubMed] [Google Scholar]
- 20. Nestler DM, White RD, Rihal CS, et al. Impact of prehospital electrocardiogram protocol and immediate catheterization team activation for patients with ST‐elevation–myocardial infarction. Circ Cardiovas Qual Outcomes. 2011;4(6):640‐646. [DOI] [PubMed] [Google Scholar]
- 21. Dauerman HL, Bates ER, Kontos MC, et al. Nationwide analysis of patients with ST‐segment elevation myocardial infarction transferred for primary percutaneous intervention: findings from the American heart association mission lifeline program. Circ Cardiovasc Interv. 2015:8e002450. [DOI] [PubMed] [Google Scholar]
- 22. El‐Menyar A, Zubaid M, Sulaiman K, et al. Atypical presentation of acute coronary syndrome: a significant independent predictor of in‐hospital mortality. J Cardiol. 2011;57(2):165‐171. [DOI] [PubMed] [Google Scholar]
- 23. Yiadom MY, Baugh CW, McWade CM, et al. Performance of emergency department screening criteria for an early ECG to identify ST‐Segment elevation myocardial infarction. JAHA. 2017;6(3):e003528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American Heart Association. Mission: Lifeline. Chicago, IL: American Heart Association; 2019. Available at: https://www.heart.org/en/professional/quality-improvement/mission-lifeline. Accessed January 7, 2019. [Google Scholar]
- 25. Cone DC, Lee CH, Van Gelder C. EMS activation of the cardiac catheterization laboratory is associated with process improvements in the care of myocardial infarction patients. Prehosp Emerg Care. 2013;17(3):293‐298. [DOI] [PubMed] [Google Scholar]
- 26. Davis DP, Graydon C, Stein R, et al. The positive predictive value of paramedic versus emergency physician interpretation of the prehospital 12‐lead electrocardiogram. Prehosp Emerg Care. 2007;11(4):399‐402. [DOI] [PubMed] [Google Scholar]
- 27. Chiang A, Gada H, Kodali SK, et al. Procedural variation in the performance of primary percutaneous coronary intervention for ST‐elevation myocardial infarction: a SCAI‐based survey study of US interventional cardiologists. Catheter Cardiovasc Interv. 2014;83(5):721‐726. [DOI] [PubMed] [Google Scholar]
- 28. Kornowski R, Mehran R, Dangas G, et al. Prognostic impact of staged versus “one‐time” multivessel percutaneous intervention in acute myocardial infarction: analysis from the HORIZONS‐AMI (Harmonizing Outcomes With Revascularization and Stents In Acute Myocardial Infarction) trial. JACC. 2011;58(7):704‐711. [DOI] [PubMed] [Google Scholar]
- 29. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941‐2947. [DOI] [PubMed] [Google Scholar]
- 30. Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door‐to‐balloon time in acute myocardial infarction. NEJM. 2006;355(22):2308‐2320. [DOI] [PubMed] [Google Scholar]
- 31. Bradley EH, Nallamothu BK, Herrin J, et al. National efforts to improve door‐to‐balloon time: results from the door‐to‐balloon alliance. JACC. 2009;54(25):2423‐2429. [DOI] [PubMed] [Google Scholar]
- 32. Wang TY, Nallamothu BK, Krumholz HM, et al. Association of door‐in to door‐out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA. 2011;305(24):2540‐2547. [DOI] [PubMed] [Google Scholar]
- 33. Langabeer JR, Henry TD, Kereiakes DJ, et al. Growth in percutaneous coronary intervention capacity relative to population and disease prevalence. JAHA. 2013;2(6):e000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hsia RY, Shen YC. Percutaneous coronary intervention in the United States: risk factors for untimely access. Health Serv Res. 2015;51(2):592‐609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bagai A, HR Al‐Khalidi, Muñoz D, et al. Bypassing the emergency department and time to reperfusion in patients with prehospital ST‐segment–elevation: findings from the reperfusion in acute myocardial infarction in carolina emergency departments project. Circulation. 2013;6(4):399‐406. [DOI] [PubMed] [Google Scholar]
- 36. Aguirre FV, Varghese JJ, Kelley MP, et al. Rural interhospital transfer of ST‐elevation myocardial infarction patients for percutaneous coronary revascularization: the STAT heart program. Circulation. 2008;117(9):1145‐1152. [DOI] [PubMed] [Google Scholar]
- 37. Wang TY, Nallamothu BK, Krumholz HM, et al. Association of door‐in to door‐out time with reperfusion delays and outcomes among patients transferred for primary percutaneous coronary intervention. JAMA. 2011;305(24):2540‐2547. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


