Abstract
Objective
Previous studies have shown increased pain scores to painful stimulation after experimental sleep restriction, but reduced or unchanged magnitude of the event related potentials (ERPs) when averaged in the time-domain. However, some studies found increased response magnitude when averaging in the time-frequency domain. The aim of this study was to determine whether ERP-latency jitter may contribute to this discrepancy.
Methods
Ninety painful electrical stimuli were given to 21 volunteers after two nights of 50% sleep restriction and after two nights of habitual sleep. ERPs were analyzed in the time-domain (N2-and P2-peaks) and time-frequency domain (power spectral density). We quantified latency jitter by the mean consecutive difference (MCD) between single-trial peak latencies and by phase locking value (PLV) across trials.
Results
P2-MCD increased from 20.4 ± 2.1 ms after habitual sleep to 24.3 ± 2.2 ms after sleep restriction (19%, p = 0.038) and PLV decreased from 0.582 ± 0.015 after habitual sleep to 0.536 ± 0.015 after sleep restriction (7.9%, p = 0.009). We found no difference for N2-MCD.
Conclusions
Our results indicate that partial sleep restriction increase latency jitter in cortical responses to experimental pain.
Significance
Latency jitter may contribute to the discrepancies between ERP-responses in the time-frequency domain and time-domain. Latency jitter should be considered when ERPs are analyzed.
Keywords: Sleep, Pain, Jitter, Event related potential, EEG, Cortical response
Sleep, Pain, Jitter, Event related potential, EEG, Cortical response
1. Introduction
Sleep is essential for most animals, and we spend up to one third of our lives sleeping. Adult humans sleep around 7 h a day (Groeger et al., 2004). Sleep length affects pain sensitivity (Edwards et al., 2008; Katsifaraki et al., 2019; Matre et al., 2015; Schrimpf et al., 2015; Schuh-Hofer et al., 2013), and several longitudinal studies have reported that poor sleep increases the risk for chronic pain conditions (e.g. Kaila-Kangas et al., 1976; Odegard et al., 2011, Siivola et al., 1976; Sivertsen et al., 2014). These studies indicate a possible causal relationship between disturbed or short sleep and pain. There may be a reciprocal relationship between sleep and pain, since pain (headache) also predicts insomnia (Ødegård et al., 2013). A recent systematic review concluded that sleep problems seems to be a stronger predictor for future pain, than the reverse (Finan et al., 2013).
Neural correlates of pain may be studied by brief painful stimulation of the skin activating nociceptive Aδ - and/or C-fiber free nerve endings (Bromm and Treede, 1984). Cortical responses to these stimuli can be detected in the human electroencephalogram (EEG) (Inui et al., 2002; Mouraux et al., 2003) as event related potentials (ERPs). In conventional time-domain averaging, EEG segments time-locked to the stimulus onset are averaged across trials. The principle of time-domain averaging is that the background EEG activity is not related to stimulus onset and varies randomly around zero. Thus, background activity will be cancelled out by averaging, increasing the signal-to-noise ratio.
Latencies of the ERPs have some variation across trials, and the ERP timing between trials will therefore differ. This variation in timing, reflecting the degree of synaptic stability, is termed latency jitter (Mouraux and Iannetti, 2008). The more jitter between trials, the more inaccurate the averaged representation will be, resulting in lowered average ERP amplitude (Mouraux and Iannetti, 2008). Thus, if jitter varies across experimental conditions, comparison of averaged ERP amplitudes across experimental conditions may be difficult. Potentially the ERP amplitude will then vary both as a function of the independent (treatment) variable under study and as a function of latency jitter.
Recent studies of experimental sleep restriction and pain-elicited ERPs have shown that while laser-induced pain ratings were unchanged (Odegard et al., 2014) or increased after sleep restriction (Schuh-Hofer et al., 2015; Tiede et al., 2010), the corresponding ERP amplitude was reduced (Odegard et al., 2014; Schuh-Hofer et al., 2015; Tiede et al., 2010). However, for electrical stimuli, sleep restriction increased pain ratings, but did not change the ERP amplitude (Matre et al., 2015; Ree et al., 2019). These seemingly paradoxical differential effects of sleep restriction on psychophysical and neurophysiological outcome measures need attention. In the latter study, ERPs analyzed in the time-frequency domain increased in magnitude after sleep restriction, corresponding to the increased subjective ratings. Since time-frequency domain analysis is less sensitive to latency jitter (Mouraux et al., 2003), we hypothesized that increased jitter contributes to an attenuation of time-domain averaged ERP amplitude after sleep restriction compared to after habitual sleep.
We know that sleep is of great importance to maintain normal and optimal brain function in general (Atienza et al., 2005; Holm et al., 2009; Jones and Harrison, 2001; Miller et al., 2014; Saper et al., 2010; Xie et al., 2013) and specifically for pain processing (Finan et al., 2013). In order to utilize pain-evoked responses as tools for increased understanding of CNS pain processing, it is useful to know why time-locked responses seemingly differ from time-frequency resonses regarding the interaction between sleep time and pain-evoked responses. Sleep-restriction-induced dysfunction in neural coupling may possibly explain reduced memory function after sleep restriction (Atienza et al., 2005), and it is accordingly reasonable to hypothesize that a similar dysfunction may involve pain networks. Jitter, as a measure of synaptic instability and decreased synchronicity, might be a part of the impaired brain function following insufficient sleep. The aim of this cross-over study was to determine whether latency jitter of electrically elicited pain-ERPs is different after partial sleep restriction in healthy adults, compared with after habitual sleep. Latency jitter was measured both in the time domain, by the single trial mean consecutive difference (MCD) value, and in the time-frequency domain, by the phase locking value (PLV).
2. Methods
2.1. Subjects
Healthy adults were enlisted to the study by means of a post on the webpage of the National Institute of Occupational Health, Norway, and by flyers and advertisement posted at the colleges and university in Oslo. Previous history of psychiatric or neurological disease, pain or use of prescription drugs, except contraceptives in females, were used as exclusion criteria.
Twenty-one adults participated in the study. Their age ranged between 18 and 31 years, with a mean age of 23.4 ± 3.7 years, and 13 were female. For the last 24 h before the experiment subjects were instructed not to use any over-the-counter analgesics or drink alcohol. Participants were blinded for the study's hypothesis. The Norwegian Regional Committee for Medical Research Ethics accepted the study (approval number 2012/199), and all subjects gave informed consent.
2.2. Design
Each subject underwent the experimental procedure twice after two different interventions in a paired crossover design: two nights with 50 % sleep restriction, and at least two nights with habitual sleep. The following is the instruction, translated from Norwegian, the subjects got before sleep restriction: “The 2 nights before the lab-experiment you should sleep half your normal sleep length, i.e. _ hours. We ask you to get up at 7:00 AM tomorrow and the day of the lab-experiment. You should therefore go to bed at _ AM, both tonight and tomorrow night. We ask you not to sleep at other times.” The times were specified based on self-reported sleep and wake up time from the Pittsburgh sleep quality index. Lab tests started the morning after the second night of intervention, between 08 and 09 AM. The subjects were randomized for which intervention they would receive first. There was at least one week between the two interventions. Two days before the first test day, a pretest to familiarize the subjects with the procedures was performed.
2.2.1. Measurements of sleepiness, alertness, sleep latency and sleep length
Sleep diaries and triaxial wrist accelerometers (ActiSleep, ActiGraph, Maribo Medico A/S, Maribo, Denmark) were used to find time in bed and total sleep time for the two nights of habitual sleep and sleep restriction. The Karolinska sleepiness scale (KSS) (Akerstedt and Gillberg, 1990) were used to calculate subjective sleepiness. Before pain testing began, a psychomotor vigilance test (PVT) (Basner and Dinges, 2011) (custom written C++ program, National Institute of Occupational Health, Norway) lasting 10 min, was used to assess behavioral alertness by measuring reaction time. After the other tests were completed, EEG + electrooculography (EOG) was used to assess sleep latency. The lighting was reduced to below 1 lux and the subject was asked to try to fall asleep, while sitting in a reclined chair for 20 min.
2.2.2. Painful electrical test stimuli
An electrode revised from Inui et al. (2002) and Klein et al. (2004) was used to give electrical stimulation. The electrode projected 0.2 mm from a polyoxymethylene frame (custom made at the National Institute of Occupational Health, Oslo, Norway), with a 0.2 mm diameter and material of platinum. The stimulation point was 1 cm medial to the halfway distance between the distal end of ulna and the insertion of the biceps brachii tendon. A Velcro strap (Alpine Biomed ApS, Skovlunde, Denmark) drenched in isotonic NaCl water was used as anode. The strap band was placed 5 cm proximal to the ipsilateral cubital fossa. A constant current stimulator (DS7A and DG2A, Digitimer, Hertfordshire, England) delivered the electrical stimuli, and each of the stimuli consisted of two unipolar pulses with 0.5 ms duration and 10 ms inter-pulse interval. Test arm was chosen at random, 8 subjects received stimuli on the left arm. It was confirmed that the stimulation gave activation of Aδ-fibers in an experiment comparing reaction time when stimulating the proximal and distal arm. Based on the differences in reaction time from the two stimulus sites, the conduction velocity was calculated to 8 m/s.
During the pretest, individual pain thresholds were determined. Stimuli started at 0 mA and were increased by 0.1 mA until the test subject rated a stimulation as painful. This procedure was repeated twice, and the pain threshold was set as the mean of the stimulations rated as painful from the two procedures.
2.2.3. Pain ratings
The instruction given to participants before stimulation is translated from Norwegian: “You will now receive 30 electrical stimulations. The stimulations will come with a few seconds interval and will vary in strength. After each stimulation, please rate the pain from 0 (‘not painful’) and 10 (‘most intense pain imaginable’), as we have rehearsed earlier. While stimulation is ongoing, you should keep your eyes open and focus on the marking on the wall ahead of you. If you can avoid blinking, especially in the period directly following stimulation, that would be nice.” Subjects could use decimals when rating pain.
2.2.4. EEG registration
EEG was obtained by a 32 active electrode setup in agreement to the 10–20 system. A soft electrode cap adjusted to the subjects’ head size were used for holding the electrodes in place (actiCAP, BrainProducts GmbH, Gilching, Germany). An impedance of 20 kΩ were used. The EEG signal was then filtered (0.53–100 Hz) and sampled at 2 kHz (QuickAmp 40 channel amplifier; Brain Vision Recorder software, BrainProducts). FCz was used as common reference electrode. Two surface electrodes, placed at the lower right and at the upper left side of the eye, were used to detect eye blinks and ocular movements.
2.2.5. Experimental procedure
Before the stimulation electrode and the EEG electrodes were set up, the subjects completed the KSS and the PVT test. Ninety electrical stimuli divided in 3 separate blocks of 30 stimuli were given. The stimuli were of three different intensities; 2, 3 and 4 times the individual pain threshold. Each block contained 10 stimuli of all three intensities. Inter-stimulus interval was 10–15 s and inter-block interval was 2 min. Each block had a predetermined random order of which stimulus intensity was given. Subject focused on a marking on the wall to reduce eye movements during EEG-recording. A verbal grading of the pain intensity was given 3–4 s after each stimulus.
2.3. EEG preprocessing
In the Analyzer 2 software (BrainProducts GmbH), the following steps were performed; down-sampling to 512 Hz, band pass filtering [1–100 Hz], notch filtering at 50 Hz, ocular correction with independent component analysis, re-referencing to linked mastoid and segmentation into epochs relative to stimulus onset [-1, 2 s]. Artifacts, e.g. due to ocular movements, were detected by visual review of the segments, 15.3 % of segments were removed due to artifacts. We pulled data from two electrodes (C3 and C4) contralateral to the stimulated side. Finally, segmented single trial data were exported to Matlab format (Matlab R2012, The Mathworks, Massachusetts, USA) for further processing.
2.4. Data analysis
Analysis of latency jitter requires single-trial data and a high signal-to-noise ratio. For this purpose, only data from the first block and the highest stimulus intensity was analyzed, since this block/intensity combination had the best signal-to-noise ratio. The data analyzed was a subset of the data published in Matre et al. (2015).
2.4.1. Latency jitter
Latency jitter was measured by different methods. The MCD of inter-potential intervals is a method for evaluating latency variability between action potentials from two muscle fibers from the same motor unit (Ekstedt et al., 1974) and is routinely calculated in single fiber electromyography studies in patients with suspected neuromuscular transmission defects (Stalberg et al., 1974). We calculated a modified MCD for ERP as the average of the absolute time-differences between consecutive single-trial peak latencies. The procedure is illustrated in Figure 1. A larger MCD represents more jitter.
Figure 1.
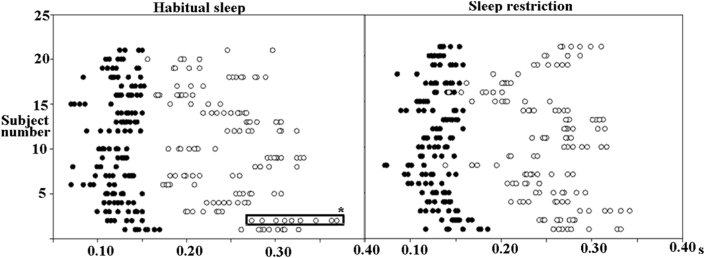
N2 (black) and P2 (white) peak latencies in consecutive single trials for all subjects (each horizontal “line” on the y-axis represents one subject). Habitual sleep on the left and sleep restriction on the right. Data from the first block and highest stimulus intensity were included in this analysis. ∗: Peaks used for example of calculation of mean consecutive difference in Figure 2.
Another measure of latency jitter is the phase locking value (PLV) (Mouraux and Iannetti, 2008). Phase locking occurs when an event resets the phase of ongoing EEG oscillations and transiently locks to the onset of the event. PLV is a measure of phase locking across trials in the time-frequency domain, as detailed below (Mouraux and Iannetti, 2008). A lower value represents more jitter.
2.4.1.1. Time-domain analysis
After removal of segments with artifacts (15.3%), 3202 epochs were analyzed in STEP (Single Trial detection toolbox for Evoked Potentials), an open source toolbox running under the Matlab environment, for single trial peak detection (Hu et al., 2010, 2011a, 2011b). STEP was run with wavelet filtering and multiple linear regression with dispersion term. Search intervals were [50–200 ms] for the maximum negative peak (N2) and [150–500 ms] for the maximum positive peak (P2). No peaks were found in 2.6 % of the single trial epochs. Figure 1 shows the distribution of N2P2-peak latencies in single trials for each subject divided by habitual sleep and sleep restriction.
MCD was calculated for both N2 and P2 peak latency. If the STEP analysis was unable to find a peak (N2 or P2) in a given epoch, the corresponding epoch and the preceding epoch were removed. Statistically defined outliers exceeding ±3 standard deviations were removed, including the epoch preceding the epoch with the outlier. After removal of outliers, the N2 peak dataset consisted of 2988 peak values, and the P2 peak dataset consisted of 3003 peak values. For the first block and the highest stimulus intensity, 287 consecutive N2 peaks and 284 consecutive P2-peaks were used for the final MCD calculation.
2.4.1.2. Time-frequency domain analysis
Single trial responses were processed in the time frequency domain using custom written scripts (Hu et al., 2014; Zhang et al., 2012). Briefly, the power spectral density of each epoch was calculated with the Short-Time Windowed Fourier Transform (200 ms Hanning window). The average post-stimulus changes of EEG oscillation were found by averaging across trials. A percentage change in power for each time frequency point after stimulus (0–800 ms relative to stimulus onset) was calculated from a pre-stimulus reference interval [-900, -100 ms] in order to find the magnitude of event-related changes in oscillation amplitude (ER%). By combining bootstrapping (1000 times) and a paired t-test, a statistical map of p-values (threshold: p < 0.01, uncorrected) was produced, comparing each ER% time frequency point to the reference interval (Durka et al., 2004). The null hypothesis of this test would be no difference between the ER% time frequency point and the reference interval. A large cluster of significant p-values, corresponding to the N2- and P2-peaks in the time-domain average, were found in the [1–400 ms] and [1–25 Hz] range. Within this region of interest, the phase locking of the signal was estimated as the PLV (Mouraux and Iannetti, 2008; Zhang et al., 2012) using custom written Matlab scripts on the averaged waveforms. PLV for each time-frequency point (t, f) was calculated by the formula below (Eq. 1), where N is the number of trials and F is the phase information. Vertical bars indicate absolute values.
| (1) |
PLV will range from 0 to 1, where 1 means a constant phase between trials, and 0 means random phase between trials (Aydore et al., 2013). The mean within this region of interest was used as the dependent variable in a mixed model analysis. For a more thorough description of the PLV measure, see e.g (Lachaux et al., 1999; Mouraux and Iannetti, 2008; Zhang et al., 2012).
2.4.2. Statistical analysis
Data was analyzed by linear mixed models with maximum likelihood estimation. The independent fixed factor was sleep condition (sleep restriction vs. habitual sleep). Dependent variables were PLV, MCD for N2 peak latency (N2-MCD), and MCD for P2 peak latency (P2-MCD). Since PLV depends on ER%, the analysis of PLV included ER% as a covariate if it improved the model fit (Mouraux and Iannetti, 2008), based on the Akaike Information Criterion. Also, stimulus number (exact occurrence in the stimulus sequence) was included as a covariate to adjust for potential habituation or sensitization. The intercept was allowed to vary randomly in all models (random intercept). Random slope for sleep was added if it improved the model fit. Individual variation was accounted for by including participant as a random factor in the models.
Paired comparisons of sleepiness, sleep latency, response speed and number of hours slept were performed by Student's t-test or by the non-parametric Wilcoxon test, if data were non-normally distributed. Statistical analyzes were performed with IBM SPSS version 21 (IBM, Chicago, Illinois, USA). The significance level was set to 0.05.
3. Results
3.1. Effects of sleep restriction on sleep and sleepiness measures
The dot-distributions of N2 and P2 peak latencies for each subject, before and after sleep restriction, is shown in Figure 2 (data from the first block and highest stimulus intensity). Average time in bed and total sleep time was significantly shorter in the sleep restriction condition vs. in the habitual sleep condition. Also, PVT reaction time was significantly longer, and subjects were significantly sleepier (KSS) after sleep restriction vs. after habitual sleep. Sleep measures are summarized in Table 1.
Figure 2.
Example of P2-MCD calculation. Data are from one subject. MCD is calculated as the mean of the differences between the peak latencies of single trial subsequent ERPs. Red dots are individual P2 peaks.
Table 1.
Sleep and sleepiness measures after habitual sleep and sleep restriction.
| Habitual sleep | Sleep restriction | Z | p-value | |
|---|---|---|---|---|
| Time in bed, hrs | 7.36 ± 0.68 | 3.77 ± 0.28 | 3.90 | <0.001 |
| Total sleep time, hrs | 6.67 ± 0.70 | 3.45 ± 0.40 | 3.90 | <0.001 |
| Response speed, s−1 | 3.01 ± 0.30 | 2.89 ± 0.26 | 2.50 | <0.001 |
| Subjective sleepiness (KSS) | 4.0 ± 1.4 | 6.8 ± 1.3 | 3.90 | <0.001 |
| Sleep latency, min | 8.8 ± 7.4 | 6.3 ± 5.5 | 1.60 | 0.12 |
Mean ± standard deviation. Time in bed was taken from the sleep diary. Total sleep time was based on actigraphy measurements (Cole-Kripke algorithm) adjusted with In-bed and Out-bed times from the diary. KSS: Karolinska sleepiness scale (1–9). Measures were tested by Wilcoxon signed rank test; Z: Test statistic. Response speed was measured by the 10-min psychomotor vigilance test (PVT).
3.2. Effect of sleep restriction on jitter
Table 2 shows mean values and SDs for the three main variables PLV, N2-MCD and P2-MCD, after habitual sleep and after sleep restriction. Slightly different estimates emerge from mixed model estimation (Table 3). The time-domain based MCD show that latency jitter was increased after sleep restriction, but only for the P2 peak. P2-MCD increased from 20.4 ± 2.1 ms after habitual sleep to 24.3 ± 2.2 ms after sleep restriction (19% increase) (p = 0.038) (Table 3). Neither stimulus number (the exact occurrence in the stimulus sequence) nor ER% had a significant effect on N2-MCD or P2-MCD.
Table 2.
Mean jitter measures in evoked EEG-responses to electrical pain stimulation after habitual sleep and sleep restriction.
| Habitual sleep |
Sleep restriction |
|||
|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | |
| PLV | 21 | 0.582 (0.08) | 21 | 0.536 (0.08) |
| N2-MCD | 145 | 15.1 (11.9) | 142 | 14.9 (11.5) |
| P2-MCD | 143 | 19.5 (15.7) | 141 | 23.3 (16.1) |
PLV = Phase locking value, MCD = Mean consecutive difference (ms), N = number of consecutive single-trial peaks for MCD-analysis, and number of subjects for PLV-analysis, SD = Standard deviation.
Table 3.
Statistical comparison of jitter measure from mixed models analysis comparing habitual sleep and sleep restriction. Estimated mean values are also tabulated.
| Habitual sleep |
Sleep restriction |
F (df) | p-value | |
|---|---|---|---|---|
| Estimates (SE) | Estimates (SE) | |||
| PLV | .582 (.015) | .536 (.015) | 8.81 (1,15.6) | .009 |
| N2-MCD | 15.8 (1.7) | 15.3 (1.8) | 0.001 (1,277) | .976 |
| P2-MCD | 20.4 (2.2) | 24.3 (2.2) | 4.35 (1,280) | .038 |
PLV = Phase locking value (range 0–1), MCD = Mean consecutive difference in ms, SE = Standard error, df = adjusted degrees of freedom, F = test statistic.
Figure 3 shows grand average PLV for habitual sleep and sleep deprivation. The largest PLV values (red in Figure 3) corresponded to the N2- and P2-peaks detected in the time-domain (mean latencies for both groups combined: N2 peak: 136 ± 21 ms; P2 peak 214 ± 42 ms). PLV values were decreased after sleep restriction, compared with after habitual sleep. This was manifested as a 7.9% decrease in PLV from 0.582 ± 0.015 after habitual sleep to 0.536 ± 0.015 after sleep restriction (p = 0.009) (Table 3, Figure 3).
Figure 3.
Phase locking value (PLV) for the different frequencies and latencies across all trials and subjects. Habitual sleep (left) and sleep restriction (right). The highlighted area around [0–0.5s] s roughly corresponds to the N2- and P2-peaks in the time-domain.
4. Discussion
4.1. Summary of results
Our findings indicate that experimental sleep restriction may increase latency jitter of electrically elicited nociceptive ERPs. This was shown both as increased MCD of the P2 latencies and as decreased PLV after experimental sleep restriction, compared to habitual sleep in the same subjects.
4.2. Relevance to previous research
Previous studies have reported increased or unchanged pain ratings, combined with lowered or unchanged time-domain ERPs after sleep restriction compared to habitual sleep (Matre et al., 2015; Odegard et al., 2014; Ree et al., 2019; Schuh-Hofer et al., 2015; Tiede et al., 2010). Our results indicate that increased latency jitter after sleep restriction may contribute to the attenuation of averaged ERPs after sleep restriction. However, alternative explanations to reduced ERP amplitude after sleep restriction exist. A recent study (Schuh-Hofer et al., 2015) suggests that increased (attention-dependent) habituation to repeated noxious laser stimuli could explain an observed laser evoked potential-amplitude decline after sleep restriction. We could not confirm the reported effect of sleep restriction on habituation in a similar study without the attention component (Matre et al., 2015). Also, a study by Odegard et al. (2014) did not find differences in laser evoked potential-habituation after sleep restriction. The latter studies applied conventional averaging and did not consider the effect on single trial responses. The importance of habituation as the cause of amplitude reduction after sleep restriction is therefore unclear, and it is tempting to speculate that increased jitter is a more probable cause. If so, it is possible that the information lost during time-domain averaging could lead to misguided conclusions, information that to some extent is kept in time-frequency domain analysis (Mouraux and Iannetti, 2008).
Increased latency jitter could be an expression of altered cortical processing of pain stimuli following sleep restriction. A study performed on rats (Barnes and Cheetham, 2015) suggests that diminished temporal precision (jitter) is a signature of impending loss of cortical connections. Although the present 4 ms increase in latency variability may seem small, it represents a 20% difference between sleep conditions. Increased latency jitter of cortical evoked responses may be both a result and/or a cause of changes in brain function after sleep restriction. Another study (Franz et al., 2015) found that attention to noxious laser stimuli have various effects on single trial amplitudes and latency jitter (measured by standard deviation), and this result may possibly be explained by similar mechanisms as our findings on jitter after sleep restriction.
4.2.1. Jitter and event related desynchronization
Matre et al. (2015) found that event-related desynchronization in the alfa frequency band was reduced after sleep restriction, which may indicate reduced event-related processing in cortical neural networks during painful stimulation (because the alpha rhythms reflect a cortical resting state). This could hypothetically also cause less intra-cortical (non-alpha) synchronization of the cortical cells involved in the evoked response, with more jitter as the result. One could speculate that increased latency jitter, i.e. less accuracy in response-timing, may be essential for the larger affective component of the painful stimulation after sleep restriction (Schuh-Hofer et al., 2015). The fact that we find increased jitter only for the P2 component, which corresponds more with cognitive and affective components of pain (Bromm and Lorenz, 1998), strengthens this assumption. The P2 component seems to be generated in deeper brain structures, especially gyrus cinguli, and is considered to be related to cognitive and affective components of pain (Bentley et al., 2002; Bromm and Lorenz, 1998). P2 depends accordingly on more diversified afferents and synaptic connections than the mainly SII-dependent N2-component. This could make the P2 component more sensitive than N2 to the sleep restriction-induced modulations of several brain processes.
Desensitization of serotonin receptors might be relevant to the changes in pain perception and processing after sleep restriction. A recent study (Martikainen et al., 2018) found that high availability of a serotonin (5-HT1A) receptor in the cortex is associated with low pain intensity in response to experimental nociceptive stimulation, while high dopamine receptor availability is associated with high pain intensity. Another study on rats found that this serotonin receptor system is desensitized after sleep restriction (Roman et al., 2005). Desensitization of the serotonin receptor system might partially explain links found between decreased sleep and increased pain, both experimental pain and epidemiological associations with chronic pain conditions. Another study (Satterfield et al., 2017) found that decreased PVT performance due to sleep restriction varied for different dopamine transporter genotypes, suggesting a possible genetic vulnerability regarding performance or health issues related to sleep deprivation.
4.3. Jitter's potential impact on other areas of brain research
Our findings may have relevance for other areas of brain research. Increased jitter could be a manifestation of, but also causing, the impaired brain function that has been observed with less sleep, i.e. changes in reward-related brain function, impaired memory and executive function measured by planning skills, less verbal fluency and creativity (Holm et al., 2009; Jones and Harrison, 2001; Miller et al., 2014; Saper et al., 2010). Another study (Atienza et al., 2005) supporting this concept found worse performance in an oddball auditory experiment in a group of subjects with restricted sleep compared to the group with normal sleep. The consolidation of learned skills was decreased when sleep restricted the night after the training session. The mismatch negativity ERP was attenuated due to increased jitter after sleep restriction, and this could explain the lack of consolidation of the trained skill (Atienza et al., 2005).
One possible explanation for the link between sleep restriction and decreased brain function might be decreased waste clearance (Xie et al., 2013). Although speculative, this may possibly alter synaptic accuracy and/or plasticity, apparent as increased jitter in our study. Aberrant pain processing could also be viewed as a manifestation of the generally impaired brain function described above after sleep restriction.
4.4. Methodological considerations
Jitter-estimates may be influenced by biological and technical noise, and successful valid calculations depend on a low-noise EEG-recording. More noise may cause an apparent increase in jitter besides the effect of sleep restriction. However, the paired design will partly control for noise-differences between conditions and, from inspection of our recordings, we have no reason to believe that noise was systematically changed by sleep restriction.
One possible way of avoiding the problem with jitter when comparing ERPs before and after sleep restriction may be to use other response measures than amplitude, e.g. the area under the curve, for time-domain analysis. However, this involves added uncertainty in response-duration-estimates and unresolved phase-cancellation issues.
We have assumed that both MCD and PLV represent measures of jitter. However, some differences should be considered, since MCD depends on the peaks of the waveform, while PLV represents the whole time-frequency region of interest for the ERP. MCD could be a more precise estimator for temporal jitter in the main components of the ERP, while PLV could be viewed as a more general estimator of jitter for the pain response across spectral components. However, it is reassuring that results by both methods were consistent.
The sample size is not large, but it is sufficient for a paired design. Our study had 81% power to detect a medium-sized effect equal to 0.65 × SD, with two-sided alfa = 0.05 (Lachin 1981). The sample size is too small to investigate e.g. gender differences within this group. However, this was not an aim of the present study.
5. Conclusions
The present study indicates that latency jitter of electrically elicited pain evoked responses increases after sleep restriction, suggesting; 1) Synaptic instability in pain-processing networks seems to be increased after sleep deprivation, and 2) Synaptic instability reflected by increased latency jitter could explain why the averaged pain evoked response is not always increased in parallel with the time-frequency response after various interventions. Techniques for single trial response analysis should be further developed and simplified for future ERP studies. As mentioned, jitter should also be useful outcome measure for synaptic stability in electrophysiological brain research.
Declarations
Author contribution statement
J.O. Hansen, P.M. Omland & T. Sand: Analyzed and interpreted the data; Wrote the paper.
K.B. Nilsen: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
D. Matre: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
Jorid Thrane Stuenæs is acknowledged for performing the experimental procedure and Monica Wigemyr for running the data through the STEP-analysis.
References
- Akerstedt T., Gillberg M. Subjective and objective sleepiness in the active individual. Int. J. Neurosci. 1990;52(1-2):29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- Atienza M., Cantero J.L., Quian Quiroga R. Precise timing accounts for posttraining sleep-dependent enhancements of the auditory mismatch negativity. Neuroimage. 2005;26(2):628–634. doi: 10.1016/j.neuroimage.2005.02.014. [DOI] [PubMed] [Google Scholar]
- Aydore S., Pantazis D., Leahy R.M. A note on the phase locking value and its properties. Neuroimage. 2013;74:231–244. doi: 10.1016/j.neuroimage.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes S.J., Cheetham C.E. Delayed and temporally imprecise neurotransmission in reorganizing cortical microcircuits. 2015;35(24):9024–9037. doi: 10.1523/JNEUROSCI.4583-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basner M., Dinges D.F. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011;34(5):581–591. doi: 10.1093/sleep/34.5.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley D.E., Youell P.D., Jones A.K. Anatomical localization and intra-subject reproducibility of laser evoked potential source in cingulate cortex, using a realistic head model. Clin. Neurophysiol. 2002;113(8):1351–1356. doi: 10.1016/s1388-2457(02)00149-9. [DOI] [PubMed] [Google Scholar]
- Bromm B., Lorenz J. Neurophysiological evaluation of pain. Electroencephalogr. Clin. Neurophysiol. 1998;107(4):227–253. doi: 10.1016/s0013-4694(98)00075-3. [DOI] [PubMed] [Google Scholar]
- Bromm B., Treede R.D. Nerve fibre discharges, cerebral potentials and sensations induced by CO2 laser stimulation. Hum. Neurobiol. 1984;3(1):33–40. [PubMed] [Google Scholar]
- Durka P.J., Zygierewicz J., Klekowicz H., Ginter J., Blinowska K.J. On the statistical significance of event-related EEG desynchronization and synchronization in the time-frequency plane. IEEE Trans. Biomed. Eng. 2004;51(7):1167–1175. doi: 10.1109/TBME.2004.827341. [DOI] [PubMed] [Google Scholar]
- Edwards R.R., Almeida D.M., Klick B., Haythornthwaite J.A., Smith M.T. Duration of sleep contributes to next-day pain report in the general population. Pain. 2008;137(1):202–207. doi: 10.1016/j.pain.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekstedt J., Nilsson G., Stalberg E. Calculation of the electromyographic jitter. J. Neurol. Neurosurg. Psychiatry. 1974;37(5):526–539. doi: 10.1136/jnnp.37.5.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finan P.H., Goodin B.R., Smith M.T. The association of sleep and pain: an update and a path forward. J. Pain. 2013;14(12):1539–1552. doi: 10.1016/j.jpain.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franz M., Nickel M.M., Ritter A., Miltner W.H., Weiss T. Somatosensory spatial attention modulates amplitudes, latencies, and latency jitter of laser-evoked brain potentials. J. Neurophysiol. 2015;113(7):2760–2768. doi: 10.1152/jn.00070.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeger J.A., Zijlstra F.R., Dijk D.J. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J. Sleep Res. 2004;13(4):359–371. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- Holm S.M., Forbes E.E., Ryan N.D., Phillips M.L., Tarr J.A., Dahl R.E. Reward-related brain function and sleep in pre/early pubertal and mid/late pubertal adolescents. J. Adolesc. Health. 2009;45(4):326–334. doi: 10.1016/j.jadohealth.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Liang M., Mouraux A., Wise R.G., Hu Y., Iannetti G.D. Taking into account latency, amplitude, and morphology: improved estimation of single-trial ERPs by wavelet filtering and multiple linear regression. J. Neurophysiol. 2011;106(6):3216–3229. doi: 10.1152/jn.00220.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L., Mouraux A., Hu Y., Iannetti G.D. A novel approach for enhancing the signal-to-noise ratio and detecting automatically event-related potentials (ERPs) in single trials. Neuroimage. 2010;50(1):99–111. doi: 10.1016/j.neuroimage.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Hu L., Xiao P., Zhang Z.G., Mouraux A., Iannetti G.D. Single-trial time-frequency analysis of electrocortical signals: baseline correction and beyond. Neuroimage. 2014;84:876–887. doi: 10.1016/j.neuroimage.2013.09.055. [DOI] [PubMed] [Google Scholar]
- Hu L., Zhang Z.G., Hung Y.S., Luk K.D., Iannetti G.D., Hu Y. Single-trial detection of somatosensory evoked potentials by probabilistic independent component analysis and wavelet filtering. Clin. Neurophysiol. 2011;122(7):1429–1439. doi: 10.1016/j.clinph.2010.12.052. [DOI] [PubMed] [Google Scholar]
- Inui K., Tran T.D., Hoshiyama M., Kakigi R. Preferential stimulation of Adelta fibers by intra-epidermal needle electrode in humans. Pain. 2002;96(3):247–252. doi: 10.1016/S0304-3959(01)00453-5. [DOI] [PubMed] [Google Scholar]
- Jones K., Harrison Y. Frontal lobe function, sleep loss and fragmented sleep. Sleep Med. Rev. 2001;5(6):463–475. doi: 10.1053/smrv.2001.0203. [DOI] [PubMed] [Google Scholar]
- Kaila-Kangas L., Kivimaki M., Harma M., Riihimaki H., Luukkonen R., Kirjonen J. Sleep disturbances as predictors of hospitalization for back disorders-a 28-year follow-up of industrial employees. Spine (Phila Pa 1976) 2006;31(1):51–56. doi: 10.1097/01.brs.0000193902.45315.e5. [DOI] [PubMed] [Google Scholar]
- Katsifaraki M., Nilsen K.B., Christensen J.O., Waersted M., Knardahl S., Bjorvatn B. Sleep duration mediates abdominal and lower-extremity pain after night work in nurses. Int. Arch. Occup. Environ. Health. 2019;92(3):415–422. doi: 10.1007/s00420-018-1373-9. [DOI] [PubMed] [Google Scholar]
- Klein T., Magerl W., Hopf H.C., Sandkuhler J., Treede R.D. Perceptual correlates of nociceptive long-term potentiation and long-term depression in humans. J. Neurosci. 2004;24(4):964–971. doi: 10.1523/JNEUROSCI.1222-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachaux J.P., Rodriguez E., Martinerie J., Varela F.J. Measuring phase synchrony in brain signals. Hum. Brain Mapp. 1999;8(4):194–208. doi: 10.1002/(SICI)1097-0193(1999)8:4<194::AID-HBM4>3.0.CO;2-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachin J.M. Introduction to sample size determination and power analysis for clincal trials. Contr. Clin. Trials. 1981;2:93–113. doi: 10.1016/0197-2456(81)90001-5. [DOI] [PubMed] [Google Scholar]
- Martikainen I.K., Hagelberg N., Jaaskelainen S.K., Hietala J., Pertovaara A. Dopaminergic and serotonergic mechanisms in the modulation of pain: in vivo studies in human brain. Eur. J. Pharmacol. 2018;834:337–345. doi: 10.1016/j.ejphar.2018.07.038. [DOI] [PubMed] [Google Scholar]
- Matre D., Hu L., Viken L.A., Hjelle I.B., Wigemyr M., Knardahl S. Experimental sleep restriction facilitates pain and electrically induced cortical responses. Sleep. 2015 doi: 10.5665/sleep.5058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M.A., Wright H., Ji C., Cappuccio F.P. Cross-sectional study of sleep quantity and quality and amnestic and non-amnestic cognitive function in an ageing population: the English Longitudinal Study of Ageing (ELSA) PloS One. 2014;9(6) doi: 10.1371/journal.pone.0100991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouraux A., Guerit J.M., Plaghki L. Non-phase locked electroencephalogram (EEG) responses to CO(2) laser skin stimulations may reflect central interactions between A partial differential - and C-fibre afferent volleys. Clin. Neurophysiol. 2003;114(4):710–722. doi: 10.1016/s1388-2457(03)00027-0. [DOI] [PubMed] [Google Scholar]
- Mouraux A., Iannetti G.D. Across-trial averaging of event-related EEG responses and beyond. Magn. Reson. Imaging. 2008;26(7):1041–1054. doi: 10.1016/j.mri.2008.01.011. [DOI] [PubMed] [Google Scholar]
- Odegard S.S., Omland P.M., Nilsen K.B., Stjern M., Gravdahl G.B., Sand T. The effect of sleep restriction on laser evoked potentials, thermal sensory and pain thresholds and suprathreshold pain in healthy subjects. Clin. Neurophysiol. 2014 doi: 10.1016/j.clinph.2014.12.011. [DOI] [PubMed] [Google Scholar]
- Odegard S.S., Sand T., Engstrom M., Stovner L.J., Zwart J.A., Hagen K. The long-term effect of insomnia on primary headaches: a prospective population-based cohort study (HUNT-2 and HUNT-3) Headache. 2011;51(4):570–580. doi: 10.1111/j.1526-4610.2011.01859.x. [DOI] [PubMed] [Google Scholar]
- Ødegård S.S., Sand T., Engstrom M., Zwart J.A., Hagen A. The impact of headache and chronic musculoskeletal complaints on the risk of insomnia: longitudinal data from the Nord-Trøndelag Health Study. J. Headache Pain. 2013;14(24) doi: 10.1186/1129-2377-14-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ree A., Nilsen K.B., Knardahl S., Sand T., Matre D. Sleep restriction does not potentiate nocebo-induced changes in pain and cortical potentials. Eur. J. Pain. 2019 doi: 10.1002/ejp.1466. [DOI] [PubMed] [Google Scholar]
- Roman V., Walstra I., Luiten P.G., Meerlo P. Too little sleep gradually desensitizes the serotonin 1A receptor system. Sleep. 2005;28(12):1505–1510. [PubMed] [Google Scholar]
- Saper C.B., Fuller P.M., Pedersen N.P., Lu J., Scammell T.E. Sleep state switching. Neuron. 2010;68(6):1023–1042. doi: 10.1016/j.neuron.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterfield B.C., Wisor J.P., Schmidt M.A., Van Dongen H.P.A. Time-on-Task effect during sleep deprivation in healthy young adults is modulated by dopamine transporter genotype. Sleep. 2017;40(12) doi: 10.1093/sleep/zsx167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrimpf M., Liegl G., Boeckle M., Leitner A., Geisler P., Pieh C. The effect of sleep deprivation on pain perception in healthy subjects: a meta-analysis. Sleep Med. 2015;16(11):1313–1320. doi: 10.1016/j.sleep.2015.07.022. [DOI] [PubMed] [Google Scholar]
- Schuh-Hofer S., Baumgartner U., Treede R.D. Effect of sleep deprivation on the electrophysiological signature of habituation to noxious laser stimuli. Eur. J. Pain. 2015;19(8):1197–1209. doi: 10.1002/ejp.698. [DOI] [PubMed] [Google Scholar]
- Schuh-Hofer S., Wodarski R., Pfau D.B., Caspani O., Magerl W., Kennedy J.D. One night of total sleep deprivation promotes a state of generalized hyperalgesia: a surrogate pain model to study the relationship of insomnia and pain. Pain. 2013 doi: 10.1016/j.pain.2013.04.046. [DOI] [PubMed] [Google Scholar]
- Siivola S.M., Levoska S., Latvala K., Hoskio E., Vanharanta H., Keinanen-Kiukaanniemi S. Predictive factors for neck and shoulder pain: a longitudinal study in young adults. Spine (Phila Pa 1976) 2004;29(15):1662–1669. doi: 10.1097/01.brs.0000133644.29390.43. [DOI] [PubMed] [Google Scholar]
- Sivertsen B., Lallukka T., Salo P., Pallesen S., Hysing M., Krokstad S. Insomnia as a risk factor for ill health: results from the large population-based prospective HUNT Study in Norway. J. Sleep Res. 2014;23(2):124–132. doi: 10.1111/jsr.12102. [DOI] [PubMed] [Google Scholar]
- Stalberg E., Ekstedt J., Broman A. Neuromuscular transmission in myasthenia gravis studied with single fibre electromyography. J. Neurol. Neurosurg. Psychiatry. 1974;37(5):540–547. doi: 10.1136/jnnp.37.5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiede W., Magerl W., Baumgartner U., Durrer B., Ehlert U., Treede R.D. Sleep restriction attenuates amplitudes and attentional modulation of pain-related evoked potentials, but augments pain ratings in healthy volunteers. Pain. 2010;148(1):36–42. doi: 10.1016/j.pain.2009.08.029. [DOI] [PubMed] [Google Scholar]
- Xie L., Kang H., Xu Q., Chen M.J., Liao Y., Thiyagarajan M. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z.G., Hu L., Hung Y.S., Mouraux A., Iannetti G.D. Gamma-band oscillations in the primary somatosensory cortex--a direct and obligatory correlate of subjective pain intensity. J. Neurosci. 2012;32(22):7429–7438. doi: 10.1523/JNEUROSCI.5877-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.