Abstract
Social distancing and ‘stay-at-home’ orders are essential to contain the coronavirus outbreak (COVID-19), but there is concern that these measures will increase feelings of loneliness, particularly in vulnerable groups. The present study examined change in loneliness in response to the social restriction measures taken to control the coronavirus spread. A nation-wide sample of American adults (N = 1,545; 45% women; age 18 to 98, M = 53.68, SD = 15.63) was assessed on three occasions: in late-January/early-February 2020 (before the outbreak), in late-March (during the President’s initial ‘15 Days to Slow the Spread’ campaign), and in late-April (during the ‘stay-at-home’ policies of most states). Contrary to expectations, there were no significant mean-level changes in loneliness across the three assessments (d = .04, p > .05). In fact, respondents perceived increased support from others over the follow-up period (d = .19, p < .01). Older adults reported less loneliness overall compared to younger age groups but had an increase in loneliness during the acute phase of the outbreak (d = .14, p <.05). Their loneliness, however, leveled off after the issuance of stay-at-home orders. Individuals living alone and those with at least one chronic condition reported feeling lonelier at baseline but did not increase in loneliness during the implementation of social distancing measures. Despite some detrimental impact on vulnerable individuals, in the present sample, there was no large increase in loneliness but remarkable resilience in response to COVID-19.
Keywords: COVID-19, loneliness, older adults, perceived support, social distancing
The emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the rapid outbreak of the resulting disease (COVID-19) caused an unprecedented public health crisis in the United States and around the world (Dong et al., 2020). The Centers for Disease Control and Prevention (CDC) recommend physical (social) distancing, self-quarantine and isolation of positive cases to slow the spread of the virus and reduce the burden placed on the healthcare system (Centers for Disease Control and Prevention, 2020a). Despite these measures, there was an increase in the number of cases in the United States (Dong et al., 2020). In March 2020, the President declared a state of emergency and urged Americans to ‘stay home’ (White House, 2020)—particularly, adults age 65 and older and individuals with pre-existing medical conditions, two groups at high risk of complications from COVID-19 (Centers for Disease Control and Prevention, 2020b). By the beginning of April, most states issued varying degrees of ‘stay-at-home’ or ‘shelter-in-place’ orders that mandated closure of schools and non-essential businesses (Lee, 2020). These measures have been critical to slow the rate of infection before a vaccine or effective treatments are developed and widely available. There is, however, concern that limits on social contacts and activities may increase feelings of loneliness, particularly among vulnerable groups (American Psychological Association, 2020; Miller, 2020).1
Even before the coronavirus crisis, loneliness was a public health issue because it is widespread and associated with increased risk of morbidity and mortality (Cacioppo & Cacioppo, 2018; Holt-Lunstad, 2017; National Academies of Sciences, Engineering, and Medicine, 2020). National surveys have found that 35% of adults age 45 and older report feeling lonely (Thayer & Anderson, 2018) and 43% of adults over 60 experience loneliness at least ‘some of the time’ (Perissinotto et al., 2012). Young adults are not immune to loneliness either, and some studies suggest that prevalence rates are highest among young adults (< 30 years) (Hammond et al., 2018; Luhmann & Hawkley, 2016). Thus, loneliness is by no means confined to old age. Higher loneliness is, however, associated consistently with worse health outcomes among older adults. One recent study, for example, found that feeling lonely, particularly perceiving an absence of close relationships, was associated with an 18% increased risk of all-cause mortality in older adults who lived alone (O’Súilleabháin et al., 2019). Others have found that loneliness is associated with chronic disease, including hypertension (Penninx et al., 1999; Stickley & Koyanagi, 2018), cardiovascular disease and stroke (Valtorta et al., 2016, 2018), and cognitive decline and impairment (Lara et al., 2019; Luchetti et al., 2020), that increases risk of premature mortality. Such effects of loneliness on health are comparable to other common behavioral risk factors (e.g., smoking) for poor health outcomes (Holt-Lunstad et al., 2017).
It is not the mere absence of social contacts that has a negative impact on health, but rather the perceived discrepancy between one’s desired and perceived quality of social relationships (Holt-Lunstad et al., 2017; National Academies of Sciences, Engineering, and Medicine, 2020; Shankar et al., 2011). According to the evolutionary theory of loneliness (Cacioppo et al., 2006), transient states of loneliness function as an alarm to motivate individuals to re-connect with others. If the re-connection does not occur, these feelings might persist and lead to further social disruption and distress (Cacioppo et al., 2006; Hawkley & Cacioppo, 2010). In the context of the coronavirus pandemic, it may be particularly difficult to re-connect with others given the restrictions on in-person social gatherings. These even transient feelings of loneliness can have a negative effect on health (Martín-María et al., 2020; Zhong et al., 2016). As such, there could be dangerous unintended consequences if loneliness increases in response to the restrictive measures took in place to contain the spread of SARS-CoV-2.
Specific groups may be at higher risk for increases in loneliness due to the social restriction measures. Older adults are a high-risk group for both COVID-19 and loneliness (American Psychological Association, 2020; Miller, 2020). For COVID-19, it is of note that one of the six points of the March 16 ‘15 Days to slow the spread’ White House guidelines was “If you are an older American, stay home and away from other people”. Individuals of any age who suffer from a chronic illness are another high-risk group. These individuals may have limited social interactions because of their poor health status, which increases risk of distress and loneliness (Barlow et al., 2015). Similar to older adults, this group has also been instructed to isolate from others in response to the pandemic (White House, 2020). The Center for Disease Control indicated that both older adults and individuals with pre-existing medical conditions—specifically, asthma, lung diseases, diabetes, obesity, heart conditions, liver and kidney diseases—are more predisposed to develop serious illness if they contract the coronavirus (Centers for Disease Control and Prevention, 2020b). Because of this risk, it is especially important for these vulnerable groups to practice social distancing. One consequence of limited physical contact with family and friends may be increased feelings of loneliness, in addition to uncertainty and fear due to the pandemic (Nelson et al., 2020). Finally, individuals who live alone may also be at higher risk of increases in loneliness because they do not have the immediate social interactions of living with another person.
In April 2020, in addition to the federal guidelines, the majority of individuals in the United States were under ‘stay-at-home’ or ‘shelter-in-place’ orders from state and local governments. These policies, enacted to contain the health emergency and slow the spread of the virus, resulted in mass restrictions for individuals to stay in their place of residence, except for essential work or travel. Prior studies have found that such measures may increase negative emotionality (Brooks et al., 2020). Quarantine measures undertaken during the 2003 SARS epidemic, for example, led to mental health problems, including increased depression, anxiety and stress symptoms (Brooks et al., 2020; Reynolds et al., 2008). The distress associated with protracted social isolation and quarantine may extend to feelings of loneliness.
The current study examines change in loneliness across the response to the coronavirus pandemic in the United States. This study makes use of data from a relatively large sample of Americans who were assessed in late-January and early-February 2020, prior to the outbreak. The sample was re-assessed twice, once in March 2020 during the President’s ‘15 Days to Slow the Spread’ guidelines, which recommended social distancing (White House, 2020), and again in late-April after formal restrictions had been in place for nearly a month in most states (Kates et al., 2020; Lee, 2020). This study design allows examining acute changes in loneliness during a period of social distancing measures: first as part of health care recommendations and then as a critical component of stay-at-home policies enacted by most states. The study also tests whether changes in loneliness varied by high-risk groups, specifically by age (younger, middle-aged and older adults), health status (presence/absence of pre-existing health conditions), and living arrangements (living alone versus living with others). There are two possible scenarios. The first scenario is an increase in loneliness, particularly among adults aged over 65, those with chronic conditions, and those who live alone. This increase might be more evident after protracted social distancing. There is, however, also anecdotal evidence that the pandemic has led to greater connection in this phase because of more frequent virtual contact with family and friends (Klein, 2020; McCammon, 2020). As such, a second scenario hypothesizes an increase in perceived support from others and no increase in loneliness.
Methods
Study design
Data were from an online Qualtrics survey distributed through Dynata (formerly Survey Sampling International), a panel company that provides recruitment services for researchers (www.dynata.com). As illustrated in Figure 1, the study included an initial baseline assessment and two follow-up assessments. The first assessment (Wave 1) was completed between January 31 and February 10, 2020. This first survey was originally distributed as a cross-sectional survey to examine loneliness, personality and health. At that time, the coronavirus was known but not yet a major concern for the public in the United States. In March, when the coronavirus spread was declared a national emergency, the original study was leveraged and reconceptualized as longitudinal by re-contacting participants through Dynata to complete a second assessment on responses to COVID-19. This second assessment (Wave 2) was completed between March 18 and 29, 2020 during the President’s initial ‘15 Days To Slow the Spread’ campaign (White House, 2020), which recommended social distancing measures. The campaign also advised older adults and persons with pre-existing conditions to isolate themselves and avoid contact with others. At the end of March, the White House extended these recommendations for an additional 30-day period. By early April, most state and local governments had issued stay-at-home orders that closed schools and non-essential businesses and advised residents to stay home and limit social contact. The third assessment (Wave 3) occurred between April 23 and April 29, when most state and local governments had such policies in place for nearly a month (see Survey Timeline, Figure 1). Pre-registration of data collection can be found at https://osf.io/vqnh8 (the analyses in this paper and the Wave 3 assessment were not part of the original pre-registration).
Figure 1. Survey Timeline.
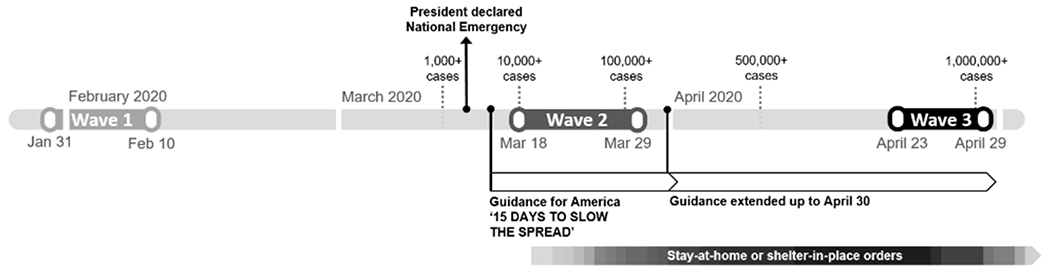
Note. Most states and local governments issued varying degrees of ‘stay-at-home’ or ‘shelter-in-place’ orders at the end of March becoming effective at the beginning of April. Arkansas, Iowa, Nebraska, North and South Dakota did not enact stay-at home orders but enacted other type of policies (e.g., closing schools).
Data collection and participants
Dynata contacted potential participants from their online panels to participate in the study. Participants had to be 18 years or older and living in the United States. The original target sample was n = 3,500. The sample was stratified to be about 50% female, 20% African American, and to have an equal number of participants (n = 500) across seven age bands: 18-19, 20-29, 30-39, 40-49, 50-59, 60-69, and 70 and older. The stratification did not to go as intended. There was an oversample of participants between 30 and 59 years of age and few participants who were 18 or 19 years old. More participants in the 18–19 age ban were tested to improve representation in this age group. This resulted in an overall sample size that was larger than originally planned. Of the 5,103 individuals who clicked on the link provided by Dynata, 4,078 consented to participate in the study and completed at least part of the survey at Wave 1; 3,767 participants had valid data on loneliness and perceived support. Of these, 2,230 consented to participate and started the survey at Wave 2; 2,088 (55% of Wave 1 respondents) had valid data on loneliness and/or support. At Wave 3, 1,595 respondents started the survey and 1,545 (74% of Wave 2 respondents) had valid data on loneliness and/or support. Table 1 reports descriptive statistics for participants with data at Wave 1 and Wave 2 and those with data across all three waves. The following cases were excluded: speeders (i.e., respondents that took less than 5 minutes to complete the survey), cases with evidence of careless responding (e.g., demographics did not match across assessments), straight-lining (i.e., giving the same answers across questionnaires) or missing data on loneliness (>20% of missing items) and/or perceived support (see Figure S1, Supplementary Material). Compared to those with a follow-up assessment, participants without a follow-up assessment reported higher loneliness (Cohen’s d = .32) and lower support (d = −.11). They were also younger (d = −.98), had less education (33% of non-respondents vs. 17.9% of respondents completed high school or less), were more likely female (58.5% of non-respondents vs. 48.2% of respondents were females) and living alone (32.1% of non-respondents vs. 22.6% of respondents lived alone). There were no differences in the number of pre-existing health conditions between respondents and non-respondents.
Table 1.
Demographic Characteristics of the Longitudinal Sample
| Participants with data at Wave 1 and Wave 2 | Participants with data across all three waves | |
|---|---|---|
| N | 2,088 | 1,545 |
| Age in years | 51.17 (16.53) | 53.68 (15.63) |
| Age groups | ||
| Young adults | 26.9% (n = 562) | 21.2% (n = 328) |
| Middle-aged adults | 47.9% (n = 1,000) | 50.0% (n = 772) |
| Older adults | 25.2% (n = 526) | 28.8% (n = 445) |
| Females | 48.2% (n= 1,007) | 45% (n = 695) |
| African American | 15.0% (n = 313) | 12.8% (n = 198) |
| Hispanic ethnicity | 10.7% (n = 223) | 9.6% (n = 149) |
| Education | 4.17 (1.50) | 4.25 (1.47) |
| Living alone | 22.6% (n = 471) | 21.7% (n = 336) |
| Number of pre-existing health conditions (range 0-7) | 0.74 (0.98) | 0.72 (0.94) |
| One or more pre-existing health conditions | 47.7% (n = 997) | 47.2% (n = 729) |
Note. Means (and standard deviations) are reported if not otherwise specified. Education is on a scale from 1 (less than high school) to 7 (PhD or equivalent).
All material and procedures were reviewed and approved by the Institutional Review Board of the Florida State University. Participant compensation was distributed through Dynata. A bonus of 50% and 75% was provided at Wave 2 and Wave 3, respectively, to heighten retention. Dynata uses an incentive point system and panelists can redeem the incentives for a range of gift cards, charitable contributions, and other products or services upon completion of a survey.
Measures
Outcome variables
Loneliness.
Participants completed the 11-item University of California Los Angeles (UCLA) Loneliness Scale (Lee & Cagle, 2017). This scale provided both a score for overall loneliness and two distinct aspects of loneliness, namely feeling isolated (“How much of the time do you feel… lack companionship? …left out? …isolated from others? …alone?”) and unavailable social connections (“How much of the time do you feel… that you are “in tune” with the people? …that there are people you can talk to? …that there are people you can turn to? …that there are people that really understand you? …that there are people you feel close to? … part of a group of friends? …That you have a lot in common with the people around you?” All reverse scored). Each item was rated on a three-point scale that ranged from hardly ever or never (1) to often (3). Respondents were asked to rate the items referring to the last two weeks. Items were reverse scored in the direction of loneliness when necessary and the mean taken across items; higher scores indicated higher loneliness. Across assessments, alpha reliability was excellent (>.85) for overall loneliness and the two facets.
Perceived support.
Participants responded to a single question on perceived support at each assessment. Specifically, they were asked how much they agreed with the statement, “I receive the social and emotional support that I need” on a scale that ranged from strongly disagree (1) to strongly agree (5).
Moderators
Age Groups.
Participants were categorized into three groups based on their self-reported age at baseline: young adults (between 18 and 39 years of age), middle-aged adults (between 40 and 64 years of age) and older adults (65 years or older). This categorization aligns with other studies on age differences in loneliness (Luhmann & Hawkley, 2016) and the guidelines that identify adults over 65 as a group at higher risk for COVID-19 (Centers for Disease Control and Prevention, 2020b).
Health Status.
At Wave 1, participants reported on the presence/absence of pre-existing health conditions, including asthma (yes/no), chronic respiratory disease (yes/no), diabetes (yes/no), heart conditions (yes/no), kidney disease (yes/no), liver disease (yes/no), and obesity (Body Mass Index ≥ 30 based on reported height and weight). According to the CDC, having one or more of these conditions at any age increases risk for severe illness from COVID-19 (Centers for Disease Control and Prevention, 2020b). Those with 1+ condition(s) were compared to those with no conditions.
Living Arrangements.
At Wave 2, participants reported on the number of individuals living in their household, including themselves. Those who reported one individual in the household were classified as living alone, whereas those reporting two or more individuals per household were classified as living with others.
Analytic Strategy
Mean-level changes across waves were examined separately for loneliness and perceived support. Differences between Wave 1 and Wave 2 were first tested to identify change in loneliness in response to the President’s initial guidelines and implementation of social distancing measures. Specifically, a repeated measures analysis of variance (ANOVA) was performed with time (Wave 1 and Wave 2) as the independent (within-subject) variable and loneliness and support as the dependent variables. Exploratory analyses also examined mean-level changes for the two facets of the loneliness scale: feeling isolated and unavailable social connections. The analyses were then repeated to include Wave 3 to examine changes in response to the protracted social distancing measures and stay-at-home orders. Time was specified as a 3-level (within-subject) factor: Wave 1, Wave 2 and Wave 3. Further, moderation analyses were conducted to test whether mean-level changes across the three waves varied by age group, health status or living arrangements. Each moderator was entered as an independent (between-subject) factor in the repeated measures ANOVAs. Significance was set to p < .05 (two-tailed). Significant main effects and interactions (e.g., time (3-level) × age groups (3-level)) were followed up using pairwise comparisons and effect sizes were calculated (ds); d values of 0.2, 0.5, and 0.8 are considered small, medium and large effect sizes, respectively (Cohen, 1988).
Results
The repeated measures ANOVA indicated no significant mean-level change in loneliness between Wave 1 and Wave 2 (see Figure 2). When examining the two facets of loneliness, there was an effect of time. Specifically, there was a slight decrease in feeling isolated and an increase in unavailable social connections between the first two waves. That is, participants did not feel more isolated in response of the implementation of social distancing measures but did perceive an increased absence of social contacts during this initial stage of the outbreak. Perceived support also increased between the two assessments. These differences were small in size (ds ~ .10). For individuals who completed Wave 3 (N =1,545), there were no significant changes in loneliness or support between the March (Wave 2) and April (Wave 3) assessments (see Figure 2).
Figure 2. Differences in Loneliness and Perceived Support across Waves.
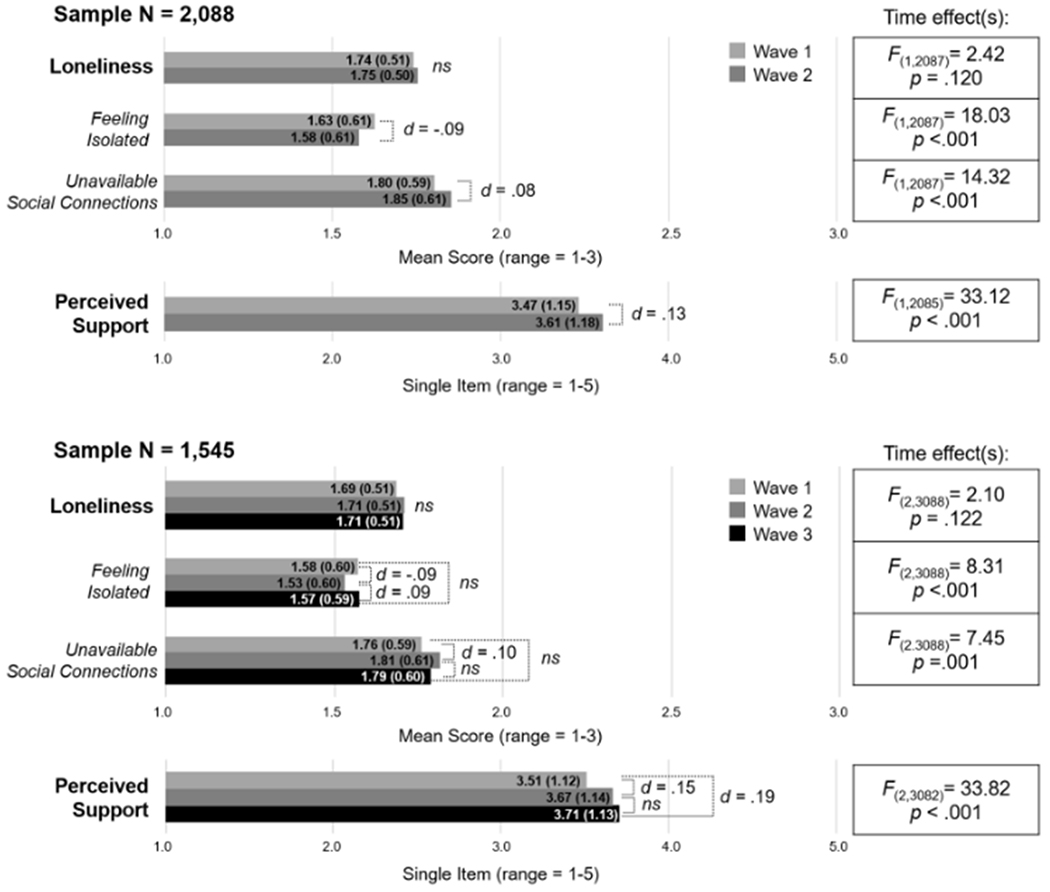
Note. N = 2,088 participants had valid data at Wave 1 and Wave 2; N = 1,545 had valid data across all three waves. Means (and standard deviations) are reported for each measure. Effect sizes (Cohen’s ds) were computed for significant differences across waves (all ps were < .01); ns = non-significant difference.
The moderation analysis indicated an interaction between time and age (see Table 2). Specifically, loneliness increased between Wave 1 and Wave 2 among individuals over 65 (d = .14) and remained relatively stable for this age group at Wave 3. For the facet unavailable social connections, the increase between the first two assessments was observed for middle-aged (d = .12) and older (d = .17) adults but not younger adults (d = −.05). For the facet feeling isolated, the decrease at Wave 2 was observed for middle-aged adults (d = −.14) but not for the other age groups. In addition, there was a significant overall effect of age on loneliness (Table 2): Older adults in general tended to report lower levels of loneliness compared to middle-aged (d = −.40) and younger adults (d = −.82). For perceived support, there was no interaction between age and time: The increase across waves was apparent across all age groups. However, there was a main effect of age: Older adults tended to report higher perceived support than middle-aged (d = −.34) and younger adults (d = −.47).
Table 2.
Mean-level changes by Age Groups, Health Status, and Living Arrangements
| ANOVAs | Means Comparison | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measures | Time | Group | Time × Group | Group(s) | Wave 1 | Wave 2 | Wave 3 | M (SD) by Group | Summary | |||||
| M | SD | M | SD | M | SD | |||||||||
| Age Groups | ||||||||||||||
| Loneliness |
F(2,3084)=0.94 p =.391 |
F(2,1542)=63.64 p <.001 |
F(4,3084)=3.34 p =.010 |
Young | 1.92 | 0.49 | 1.89 | 0.49 | 1.87 | 0.49 | 1.89 | 0.43 | W2 > W1, W2 = W3 in older adults Young > middle-aged > older adults |
|
| Middle-aged | 1.70 | 0.49 | 1.72 | 0.49 | 1.73 | 0.49 | 1.71 | 0.43 | ||||||
| Older | 1.51 | 0.49 | 1.56 | 0.49 | 1.55 | 0.49 | 1.54 | 0.43 | ||||||
| M (SD) by Wave | 1.71 | 0.52 | 1.72 | 0.53 | 1.72 | 0.53 | ||||||||
| Feeling Isolated |
F(2,3084)=4.89 p =.008 |
F(2,1542)=50.09 p <.001 |
F(4,3084)=2.60 p =.034 |
Young | 1.82 | 0.58 | 1.78 | 0.59 | 1.77 | 0.58 | 1.79 | 0.52 | W1 > W2 < W3 in middle-aged adults Young > middle-aged > older adults |
|
| Middle-aged | 1.56 | 0.58 | 1.50 | 0.59 | 1.57 | 0.58 | 1.54 | 0.52 | ||||||
| Older | 1.41 | 0.58 | 1.40 | 0.59 | 1.43 | 0.58 | 1.42 | 0.52 | ||||||
| M (SD) by Wave | 1.60 | 0.62 | 1.56 | 0.62 | 1.59 | 0.62 | ||||||||
| Unavailable social connections |
F(2,3084)=4.34 p =.013 |
F(2,1542)=49.00 p <.001 |
F(4,3084)=2.83 p =.034 |
Young | 1.98 | 0.57 | 1.95 | 0.60 | 1.94 | 0.59 | 1.95 | 0.49 | W2 > W1, W2 = W3 in middle-aged and older Young > middle-aged > older adults |
|
| Middle-aged | 1.78 | 0.57 | 1.85 | 0.60 | 1.82 | 0.59 | 1.81 | 0.49 | ||||||
| Older | 1.56 | 0.57 | 1.66 | 0.60 | 1.62 | 0.59 | 1.61 | 0.49 | ||||||
| M (SD) by Wave | 1.77 | 0.61 | 1.82 | 0.64 | 1.79 | 0.63 | ||||||||
| Support |
F(2,3078)=29.89 p <.001 |
F(2,1539)=24.37 p <.001 |
F(4,3078)=0.66 p =.621 |
Young | 3.30 | 1.11 | 3.50 | 1.14 | 3.50 | 1.12 | 3.44 | 0.96 | Older > middle-aged = young adults No interaction with time |
|
| Middle-aged | 3.45 | 1.11 | 4.58 | 1.14 | 3.66 | 1.12 | 3.56 | 0.96 | ||||||
| Older | 3.77 | 1.11 | 3.94 | 1.14 | 3.95 | 1.12 | 3.89 | 0.96 | ||||||
| M (SD) by Wave | 3.51 | 1.19 | 3.67 | 1.21 | 3.70 | 1.20 | ||||||||
| Health Status | ||||||||||||||
| Loneliness |
F(2,3086)=1.99 p =.136 |
F(1,1543)=11.66 p =.001 |
F(2,3086)=0.48 p =.618 |
No condition | 1.65 | 0.51 | 1.68 | 0.51 | 1.67 | 0.51 | 1.67 | 0.45 | With 1+ condition > with no condition No interaction with time |
|
| 1+ condition | 1.74 | 0.51 | 1.75 | 0.51 | 1.75 | 0.51 | 1.74 | 0.45 | ||||||
| M (SD) by Wave | 1.69 | 0.51 | 1.71 | 0.51 | 1.71 | 0.51 | ||||||||
| Feeling Isolated |
F(2,3086)=8.79 p <.001 |
F(1,1543)=19.04 p <.001 |
F(2,3086)=2.62 p =.073 |
No condition | 1.51 | 0.60 | 1.49 | 0.60 | 1.51 | 0.59 | 1.50 | 0.53 | With 1+ condition > with no condition No interaction with time |
|
| 1+ condition | 1.65 | 0.60 | 1.58 | 0.60 | 1.63 | 0.59 | 1.62 | 0.53 | ||||||
| M (SD) by Wave | 1.58 | 0.60 | 1.53 | 0.60 | 157 | 0.59 | ||||||||
| Unavailable social connections |
F(2,3086)=7.41 p =.001 |
F(1,1543)=4.64 p =.031 |
F(2,3086)=0.01 p =.999 |
No condition | 1.73 | 0.59 | 1.79 | 0.61 | 1.76 | 0.60 | 1.76 | 0.50 | With 1+ condition > with no condition No interaction with time |
|
| 1+ condition | 1.79 | 0.59 | 1.84 | 0.61 | 1.82 | 0.60 | 1.81 | 0.50 | ||||||
| M (SD) by Wave | 1.76 | 0.59 | 1.81 | 0.61 | 1.79 | 0.60 | ||||||||
| Support |
F(2,3080)=33.75 p <.001 |
F(1,1540)=6.25 p =.013 |
F(2,3080)=0.05 p =.955 |
No condition | 3.57 | 1.12 | 3.73 | 1.15 | 3.76 | 1.13 | 3.69 | 0.97 | With 1+ condition < with no condition No interaction with time |
|
| 1+ condition | 3.44 | 1.12 | 3.60 | 1.15 | 3.65 | 1.13 | 3.56 | 0.97 | ||||||
| M (SD) by Wave | 3.51 | 1.13 | 3.66 | 1.15 | 3.71 | 1.14 | ||||||||
| Living Arrangements | ||||||||||||||
| Loneliness |
F(2,3086)=3.07 p =.046 |
F(1,1543)=34.95 p <.001 |
F(2,3086)=2.63 p =.072 |
Living with others | 1.66 | 0.51 | 1.68 | 0.50 | 1.67 | 0.50 | 1.67 | 0.44 | Living alone > living with others No interaction with time |
|
| Living alone | 1.80 | 0.51 | 1.82 | 0.50 | 1.86 | 0.50 | 1.83 | 0.44 | ||||||
| M (SD) by Wave | 1.73 | 0.61 | 1.75 | 0.61 | 1.76 | 0.61 | ||||||||
| Feeling Isolated |
F(2,3086)=8.29 p <.001 |
F(1,1543)=60.05 p <.001 |
F(2,3086)=2.69 p =.068 |
Living with others | 1.52 | 0.59 | 1.48 | 0.60 | 1.51 | 0.58 | 1.50 | 0.52 | Living alone > living with others No interaction with time |
|
| Living alone | 1.76 | 0.59 | 1.71 | 0.60 | 1.80 | 0.58 | 1.75 | 0.52 | ||||||
| M (SD) by Wave | 1.64 | 0.72 | 1.60 | 0.71 | 1.65 | 0.71 | ||||||||
| Unavailable social connections |
F(2,3086)=5.38 p =.005 |
F(1,1543)=13.15 p <.001 |
F(2,3086)=1.12 p =.325 |
Living with others | 1.74 | 0.59 | 1.79 | 0.61 | 1.76 | 0.60 | 1.76 | 0.50 | Living alone > living with others No interaction with time |
|
| Living alone | 1.83 | 0.59 | 1.89 | 0.61 | 1.90 | 0.60 | 1.87 | 0.50 | ||||||
| M (SD) by Wave | 1.78 | 0.71 | 1.84 | 0.74 | 1.83 | 0.72 | ||||||||
| Support |
F(2,3080)=22.20 p <.001 |
F(1,1540)=24.05 p <.001 |
F(2,3080)=0.44 p =.645 |
Living with others | 3.57 | 1.12 | 3.74 | 1.14 | 3.77 | 1.13 | 3.69 | 0.97 | Living alone < living with others No interaction with time |
|
| Living alone | 3.29 | 1.12 | 3.41 | 1.14 | 3.50 | 1.13 | 3.40 | 0.97 | ||||||
| M (SD) by Wave | 3.43 | 1.36 | 3.57 | 1.38 | 3.63 | 1.37 | ||||||||
Note. Total N = 1,545. Ns vary across measures due to missing data on dependent and moderator variables. F statistics (and degree of freedom) are reported for the main effect of time (3-level: Wave 1, Wave 2 and 3), group effects, and interactions (time × group).We also reported estimated marginal means (and standard deviations) across waves by age groups, health status and living arrangements. In the last column, results are summarized noting significant differences (p <.05) across groups.
There was no significant interaction between time and health status nor between time and living arrangements (Table 2), which indicated loneliness did not increase for these two high-risk groups. 2 Similar to age, there were overall differences in loneliness between high and low risk groups: Individuals either with a chronic disease or who lived alone reported more loneliness (d 1+ conditions = .17; d Living alone = .36) and lower support (d 1+ conditions = −.13; d Living alone = −.30) compared to those without a chronic disease or those who lived with others.
Discussion
This study examined change in loneliness and perceived support in response to social distancing and restriction measures undertaken to contain the outbreak of the SARS-CoV-2 in the United States. Since the beginning of the outbreak, there have been significant concerns that social distancing would lead to increases in loneliness, as highlighted in both popular press articles (Aten, 2020; Shihipar, 2020) and scientific publications (Berg-Weger & Morley, 2020; Fiorillo & Gorwood, 2020; Miller, 2020; see also American Psychological Association, 2020). Contrary to expectations, there were no significant mean-level changes in loneliness across the three assessments. In fact, respondents perceived more support from others over the study period. These results support the anecdotal evidence for increases in social connections, even if those connections are happening in ways other than in person (Klein, 2020; McCammon, 2020). Individuals, families and communities can still come together and feel emotionally close despite the physical distancing.
Attention should still be directed to groups that may be more vulnerable to the effects of social distancing (American Psychological Association, 2020). In the current sample, for example, older adults, as a group, reported lower average levels of loneliness relative to younger adults (as found in prior studies, e.g., Bruce et al., 2019; Hammond et al., 2018). Older adults, however, were the only group that showed a slight increase in loneliness, on average, after social distancing measures were initiated in March. This increase was particularly evident for the facet of unavailable social connections. That is, older adults perceived an increased absence of social contacts in the initial phase of the social distancing measures. This increase leveled off after the protraction of social distancing and the issuance of stay-at-home orders in April. This modest effect size is important to note: Even a small increase in loneliness may pose greater risk for poor health and well-being outcomes (Hawkley & Cacioppo, 2010). Further, this increase may have cumulative effects over time. Loneliness in older adulthood, for example, increases risk of depression and anxiety (Santini et al., 2020), physical health problems (Penninx et al., 1999; Stickley & Koyanagi, 2018), and ultimately leads to premature mortality (O’Súilleabháin et al., 2019; Pantell et al., 2013).
In addition to older adults, individuals with chronic conditions (Penninx et al., 1999) and those who live alone (Sundström et al., 2009; Victor et al., 2000) are also at higher risk of loneliness. Indeed, both of these at-risk groups reported higher loneliness and lower perceived support at the baseline assessment. Loneliness may increase over time as a function of poor health status and perceptions of health-related threats (Barlow et al., 2015). In the context of the coronavirus crisis, individuals with underlying health conditions that put them at greater risk of complications from COVID-19 may be particularly sensitive to this threat and may take increased precautions that include isolation from other people to reduce the threat. Such distancing may increase loneliness. Likewise, stay-at-home orders may have been particularly difficult for those who live alone because such living arrangements severely limit any in-person interactions. In the current sample, however, there was no evidence of an increase in loneliness over the follow-up period based on either health status or living arrangements. Many people have felt part of community-wide efforts to slow the spread of the virus. The feeling of increased social support and of being in this together may increase resilience to loneliness, even among at risk groups.
In the present sample, there was no evidence of a large increase in loneliness either in the initial phase of the social distancing guidelines or after the extension of these measures and issuance of the stay-at-home orders that were in effect across most of the United States for much of April 2020. Concerns and anxiety related to the virus spread may have been highest in mid-March when there was more uncertainty and a great need to take measures to ‘flatten the curve’ (Nelson et al., 2020). The stricter measures taken across much of the country in late-March and April were effective at slowing the spread of the virus.
The results of the present study are consistent with an emerging literature on the social connection implications of COVID-19 (Folk et al., 2020; Jacobson et al., 2020; Tull et al., 2020). In a pre-published study, for example, Folk and colleagues assessed loneliness and social connection prior (mid-February 2020) and during (early-April 2020) the COVID-19 pandemic in a sample of Canadian undergraduates (mean age ~ 20) and a community sample primarily from the United States and United Kingdom (mean age ~30). Across the two samples (ns < 500), the authors noted no substantial change in social connection, but a small and significant decrease in loneliness between baseline and follow-up. Tull and colleagues (2020) conducted an MTurk cross-sectional survey across the United States from March 27 to April 5, 2020. The authors found that even though living under a stay-at-home order was associated with feeling lonely, a higher perceived impact of COVID-19 on participants’ daily life was associated with higher perceived social support and lower loneliness. Other studies that examined Google searches reported a rise in searches for loneliness, worry and depression during the spread of the virus (Brodeur et al., 2020; Jacobson et al., 2020) but the rapid rise in mental health searches in mid-March flattened after stay-at-home orders were issued (Jacobson et al., 2020). In the current study, the trajectory of loneliness observed for older adults followed a similar trend.
In addition to social distancing measures put in place across the country, the current findings need to be interpreted in the context of the devastating impact of the pandemic. By the end of April 2020, at least 1 million Americans have tested positive for the coronavirus and tens of thousands have been hospitalized or died (Dong et al., 2020). Social isolation, fear of contagion and loss of family members have been compounded by the distress caused by loss of income and growing unemployment. In the United States, there have been at least 30 million new jobless claims from mid-March to late April (corresponding to the second and third assessment in the present study; Tappe, 2020). For these reasons, the World Health Organization recently urged an increase in mental health services to avoid a potential unprecedented crisis (World Health Organization, 2020). Some international studies conducted in the midst of the pandemic (March-April 2020) have noted that individuals who felt lonely and isolated reported more severe psychological symptoms (i.e., anxiety and depression; González-Sanguino et al., 2020; Losada-Baltar et al., 2020; Newby et al., 2020; Okruszek et al., 2020). Nonetheless, within the context of this pandemic, it is remarkable that loneliness, on average, may be less reactive to the effects of social isolation and other sources of stress.
It is important to note that although there was little evidence of mean-level change in loneliness over time across the sample, there still could be significant individual differences in change. That is, some individuals may increase substantially in loneliness and others may decrease substantially in loneliness, and thus overall there was no change at the sample level. Even within vulnerable groups, there is likely to be variability in loneliness responses to COVID-19. As highlighted by the American Psychological Association Committee on Aging (CONA), older adults may vary in their needs and their coping strategies to the current crisis (American Psychological Association Committee on Aging, 2020) and two older adults may not respond in the same way. Therefore, it is critical to identify factors that put specific individuals at risk (not merely based on age) to help identify who would benefit most from intervention.
The current study had several strengths, including the study design and the assessment of loneliness just prior to the COVID-19 outbreak in the United States and again following social distancing and stay-at-home orders across much of the country. There are also a few limitations to note. First, as with all longitudinal studies, there were non-random patterns of attrition across the waves. That is, participants with higher loneliness at baseline tended to dropout at the follow-ups. It is possible that these individuals were the most at-risk of increased loneliness in response to the pandemic. Individuals high in loneliness prior to the pandemic were already an at-risk group. The attrition limited the generalizability of the current results. Second, this study was limited to the United States. The trajectory of loneliness in response to the pandemic could vary across cultures, but in many countries, there have been evocative reports of people coming together while maintaining social distancing (e.g., applause and singing from windows in hard-hit Italy and Spain; BBC NEWS, 2020). Third, loneliness might vary day-by-day in response to availability of social contacts and interactions. It would be interesting to examine such variation in relation to the social restrictions imposed due to the coronavirus spread (see for example a pre-published study, Fried et al., 2020). Lastly, the magnitude of change observed for loneliness among older adults was relatively small. This suggested more stability than changes across assessments. However, even small effects are meaningful from a public health perspective. As noted by Holt-Lunstad (2017), social factors (including loneliness) merit attention when designing public health policies and interventions. The effects of such factors on health are comparable to many leading behavioral determinants of health that receive significant public health resources.
Of the two hypothesized scenarios, there was more evidence in support of the second: There was no large increase in loneliness in the acute phase of the outbreak, which may be due, in part, to increases in perceived support. It should be noted, however, the necessity to monitor loneliness over time as the current situation evolves. According to a recent report, intermittent social distancing may be necessary into 2022 to control resurgence of waves of contagion (Kissler et al., 2020). For groups at risk, such as older adults, it may be useful to have preventive programs in place that offer support and promote online social interactions (Fakoya et al., 2020; Morris et al., 2014).
The definition of loneliness is the disconnection between desired social connection with perceived quality of social connections (Hawkley & Cacioppo, 2010; Perlman & Peplau, 1981). An important aspect of this definition is that it is possible to feel lonely in a crowd of family and friends and it is possible to feel connected when physically alone. It is this feeling of connection rather than the number of social contacts that tends to promote better health outcomes (Holt-Lunstad et al., 2017; Shankar et al., 2011). Within the context of a pandemic that requires social distancing for the greater good, people are able to feel that everyone is in this together. This feeling, even when physically isolated, may help to keep feelings of loneliness in check.
Supplementary Material
Public Significance Statement.
This study tests for change in loneliness prior and during the outbreak of the coronavirus in the United States. While continued attention should be directed to vulnerable groups, the study did not find a large increase in loneliness despite the social distancing measures undertaken to contain the outbreak. Even when physically isolated, the feeling of increased social support and of being in this together may help limit increases in loneliness.
Acknowledgments
Authors received support from the National Institute on Aging (NIA) of the National Institutes of Health, Award Numbers R01AG053297 and R56AG064952. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
We have no known conflict of interest to disclose.
It is important to note that within any defined group, there are significant individual differences. Any individual within a group has his/her own risks, resources, and needs that make him/her unique. The groups examined here are considered at high risk of complications from COVID-19 and/or loneliness (American Psychological Association, 2020; Centers for Disease Control and Prevention, 2020b). Any specific individual, however, may or may not be at risk depending on their own profile of risk, resources, and needs.
Exploratory analyses were performed to test for possible interactions between age group, health status and living arrangements, and between these factors and time. These analyses revealed no significant interaction of age group with living arrangements or health status in predicting loneliness nor support changes. The only exception was an interaction between time, age group and health status in predicting perceived support (F(4,3060) = 2.41, p = .047). An examination of the means indicated that support increased across assessments among young adults with health problems, while this increase was more apparent among individuals without health condition at older ages. Of note, interpretation and generalizability of such high-order interactions need to be approached with caution.
References
- American Psychological Association. (2020, March 18). COVID-19 isn’t just a danger to older people’s physical health. https://www.apa.org/news/apa/2020/03/covid-19-danger-physical-health
- American Psychological Association Committee on Aging. (2020). Key points on COVID-19 and older adults. https://ahcpsychologists.org/wp-content/uploads/2020/03/APA-Committee-on-Aging-Key-Points-on-COVID-19.pdf
- Aten JD (2020, April 3). How to help older adults fight loneliness during COVID-19. Psychology Today. https://www.psychologytoday.com/us/blog/hope-resilience/202004/how-help-older-adults-fight-loneliness-during-covid-19 [Google Scholar]
- Barlow MA, Liu SY, & Wrosch C (2015). Chronic illness and loneliness in older adulthood: The role of self-protective control strategies. Health Psychology, 34(8), 870–879. 10.1037/hea0000182 [DOI] [PubMed] [Google Scholar]
- BBC NEWS. (2020, March 15). Coronavirus: Spain and Italy applaud health workers. https://www.bbc.com/news/av/world-europe-51895386/coronavirus-spain-and-italy-applaud-health-workers
- Berg-Weger M, & Morley JE (2020). Loneliness and social isolation in older adults during the Covid-19 pandemic: Implications for gerontological social work. The Journal of Nutrition, Health & Aging, s12603-020-1366-1368 10.1007/s12603-020-1366-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur A, Clark AE, Fleche S, & Powdthavee N (2020). Assessing the impact of the coronavirus lockdown on unhappiness, loneliness, and boredom using Google Trends. ArXiv: 2004.12129 [Physics]. http://arxiv.org/abs/2004.12129 [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce LD, Wu JS, Lustig SL, Russell DW, & Nemecek DA (2019). Loneliness in the United States: A 2018 National Panel Survey of demographic, structural, cognitive, and behavioral characteristics. American Journal of Health Promotion, 33(8), 1123–1133. 10.1177/0890117119856551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Cacioppo S (2018). The growing problem of loneliness. The Lancet, 391(10119), 426 10.1016/S0140-6736(18)30142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, & Spiegel D (2006). Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality, 40(6), 1054–1085. 10.1016/j.jrp.2005.11.007 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. (2020a, April 8). Coronavirus Disease 2019 (COVID-19): How to prepare. https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html
- Centers for Disease Control and Prevention. (2020b, April 17). Coronavirus Disease 2019 (COVID-19): Groups at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html [PubMed]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates. [Google Scholar]
- Dong E, Du H, & Gardner L (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases, S1473309920301201 10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakoya OA, McCorry NK, & Donnelly M (2020). Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health, 20(1), 129 10.1186/s12889-020-8251-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A, & Gorwood P (2020). The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. European Psychiatry, 63(1), e32 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folk DP, Okabe-Miyamoto K, Dunn EW, & Lyubomirsky S (2020). Have introverts or extraverts declined in social connection during the first wave of COVID-19? [Preprint]. PsyArXiv. 10.31234/osf.io/tkr2b [DOI] [Google Scholar]
- Fried EI, PapanikolaouLekkas F, & Epskamp S (2020). Mental health and social contact during the COVID-19 Pandemic: An ecological momentary assessment study [Preprint]. https://osf.io/mvdpe
- González-Sanguino C, Ausín B, ÁngelCastellanos M, Saiz J, López-Gómez A, Ugidos C, & Muñoz M (2020). Mental health consequences during the initial stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, S0889159120308126 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond C, Qualter P, Victor C, & Barretto M (2018). Who feels lonely? The results of the world’s largest loneliness study. BBC Radio 4 website. https://www.bbc.co.uk/programmes/articles/2yzhfv4DvqVp5nZyxBD8G23/who-feels-lonely-the-results-of-the-world-s-largest-loneliness-study. [Google Scholar]
- Hawkley LC, & Cacioppo JT (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J (2017). The potential public health relevance of social isolation and loneliness: Prevalence, epidemiology, and risk factors. Public Policy & Aging Report, 27(4), 127–130. 10.1093/ppar/prx030 [DOI] [Google Scholar]
- Holt-Lunstad J, Robles TF, & Sbarra DA (2017). Advancing social connection as a public health priority in the United States. American Psychologist, 72(6), 517–530. 10.1037/amp0000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NC, Lekkas D, Price G, Heinz MV, Song M, O’Malley AJ, & Barr PJ (2020). Flattening the mental health curve: COVID-19 stay-at-home orders result in alterations in mental health search behavior in the United States [Preprint]. PsyArXiv. 10.31234/osf.io/24v5b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kates J, Michaud J, & Tolbert J (2020, April 6). Stay-at-home orders to fight COVID-19 in the United States: The risks of a scattershot approach. https://www.kff.org/coronavirus-policy-watch/stay-at-home-orders-to-fight-covid19/
- Kissler SM, Tedijanto C, Goldstein E, Grad YH, & Lipsitch M (2020). Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science, eabb5793 10.1126/science.abb5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein N (2020, April 4). Social distancing should not equal social isolation—Preventing one public health crisis should not create another one. https://www.npr.org/2020/03/17/816691923/how-to-be-alone-but-not-lonely-despite-the-coronavirus
- Lara E, Martín-María N, De la Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, & Miret M (2019). Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Research Reviews, 52, 7–16. 10.1016/j.arr.2019.03.002 [DOI] [PubMed] [Google Scholar]
- Lee A (2020). These states have implemented stay-at-home orders. Here’s what that means for you. https://www.cnn.com/2020/03/23/us/coronavirus-which-states-stay-at-home-order-trnd/index.html [Google Scholar]
- Lee J, & Cagle JG (2017). Validating the 11-Item Revised University of California Los Angeles Scale to assess loneliness among older adults: An evaluation of factor structure and other measurement properties. The American Journal of Geriatric Psychiatry, 25(11), 1173–1183. 10.1016/j.jagp.2017.06.004 [DOI] [PubMed] [Google Scholar]
- Losada-Baltar A, Jiménez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro M, del S, Fernandes-Pires J, & Márquez-González M (2020). “We Are Staying at Home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. The Journals of Gerontology: Series B, gbaa048 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M, Terracciano A, Aschwanden D, Lee JH, Stephan Y, & Sutin AR (2020). Loneliness is associated with risk of cognitive impairment in the Survey of Health, Ageing and Retirement in Europe. International Journal of Geriatric Psychiatry. 10.1002/gps.5304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhmann M, & Hawkley LC (2016). Age differences in loneliness from late adolescence to oldest old age. Developmental Psychology, 52(6), 943–959. 10.1037/dev0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-María N, Caballero FF, Miret M, Tyrovolas S, Haro JM, Ayuso-Mateos JL, & Chatterji S (2020). Differential impact of transient and chronic loneliness on health status. A longitudinal study. Psychology & Health, 35(2), 177–195. 10.1080/08870446.2019.1632312 [DOI] [PubMed] [Google Scholar]
- McCammon S (2020, March 17). How to be alone, but not lonely, despite the coronavirus. Npr News. https://www.npr.org/2020/03/17/816691923/how-to-be-alone-but-not-lonely-despite-the-coronavirus [Google Scholar]
- Miller G (2020). Social distancing prevents infections, but it can have unintended consequences. Science. 10.1126/science.abb7506 [DOI] [Google Scholar]
- Morris ME, Adair B, Ozanne E, Kurowski W, Miller KJ, Pearce AJ, Santamaria N, Long M, Ventura C, & Said CM (2014). Smart technologies to enhance social connectedness in older people who live at home: Smart technology and social connectedness. Australasian Journal on Ageing, 33(3), 142–152. 10.1111/ajag.12154 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2020). Social isolation and loneliness in older adults Opportunities for the health care system. The National Academies Press. [PubMed] [Google Scholar]
- Nelson BW, Pettitt AK, Flannery J, & Allen NB (2020). Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample [Preprint]. PsyArXiv. 10.31234/osf.io/jftze [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby J, O’Moore K, Tang S, Christensen H, & Faasse K (2020). Acute mental health responses during the COVID-19 pandemic in Australia [Preprint]. 10.1101/2020.05.03.20089961 [DOI] [PMC free article] [PubMed]
- Okruszek L, Aniszewska-Stańczuk A, Piejka A, Wiśniewska M, & Żurek K (2020). Safe but lonely? Loneliness, mental health symptoms and COVID-19 [Preprint]. PsyArXiv. 10.31234/osf.io/9njps [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Súilleabháin PS, Gallagher S, & Steptoe A (2019). Loneliness, living alone, and all-cause mortality: The role of emotional and social loneliness in the elderly during 19 years of follow-up. Psychosomatic Medicine, 81(6), 521–526. 10.1097/PSY.0000000000000710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, & Adler N (2013). Social Isolation: A predictor of mortality comparable to traditional clinical risk factors. American Journal of Public Health, 103(11), 2056–2062. 10.2105/AJPH.2013.301261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx BWJH, van Tilburg T, Kriegsman DMW, Boeke AJP, Deeg DJH, & van Eijk J, Th M (1999). Social network, social support, and loneliness in older persons with different chronic diseases. Journal of Aging and Health, 11(2), 151–168. 10.1177/089826439901100202 [DOI] [PubMed] [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, & Covinsky KE (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14). 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman D, & Peplau LA (1981). Toward a social psychology of loneliness In Personal relationships (pp. 33–56). [Google Scholar]
- Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, & Styra R (2008). Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiology and Infection, 136(7), 997–1007. 10.1017/S0950268807009156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, Meilstrup C, Madsen KR, & Koushede V (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet Public Health, 5(1), e62–e70. 10.1016/S2468-2667(19)30230-0 [DOI] [PubMed] [Google Scholar]
- Shankar A, McMunn A, Banks J, & Steptoe A (2011). Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology, 30(4), 377–385. 10.1037/a0022826 [DOI] [PubMed] [Google Scholar]
- Shihipar A (2020, March 13). Opinion: Coronavirus and the Isolation Paradox: “Social distancing” is required to prevent infection. But loneliness can make us sick. https://www.nytimes.com/2020/03/13/opinion/coronavirus-social-distancing.html [Google Scholar]
- Stickley A, & Koyanagi A (2018). Physical multimorbidity and loneliness: A population-based study. PLOS ONE, 13(1), e0191651 10.1371/journal.pone.0191651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundström G, Fransson E, Malmberg B, & Davey A (2009). Loneliness among older Europeans. European Journal of Ageing, 6(4), 267–275. 10.1007/s10433-009-0134-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tappe A (2020, April 30). 30 million Americans have filed initial unemployment claims since mid-March. CNN Business. https://www.cnn.com/2020/04/30/economy/unemployment-benefits-coronavirus/index.html [Google Scholar]
- Thayer C, & Anderson GO (2018). Loneliness and social connections: A national survey of adults 45 and older. AARP Research. 10.26419/res.00246.001 [DOI] [Google Scholar]
- Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, & Gratz KL (2020). Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Research, 289, 113098 10.1016/j.psychres.2020.113098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, & Hanratty B (2018). Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. European Journal of Preventive Cardiology, 25(13), 1387–1396. 10.1177/2047487318792696 [DOI] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, Ronzi S, & Hanratty B (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart, 102(13), 1009–1016. 10.1136/heartjnl-2015-308790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor C, Scambler S, Bond J, & Bowling A (2000). Being alone in later life: Loneliness, social isolation and living alone. Reviews in Clinical Gerontology, 10(4), 407–417. 10.1017/S0959259800104101 [DOI] [Google Scholar]
- White House. (2020, March 16). THE PRESIDENT’S CORONAVIRUS GUIDELINES FOR AMERICA: 15 DAYS TO SLOW THE SPREAD. https://www.justice.gov/doj/page/file/1258511/download
- World Health Organization. (2020, May 14). News release: Substantial investment needed to avert mental health crisis. https://www.who.int/news-room/detail/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis
- Zhong B-L, Chen S-L, & Conwell Y (2016). Effects of Transient Versus Chronic Loneliness on Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. The American Journal of Geriatric Psychiatry, 24(5), 389–398. 10.1016/j.jagp.2015.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


