Abstract
Introduction
The objective of this study was to assess if the fracture and/or non-union of extended trochanteric osteotomy (ETO) affected the behavior and survival of modular fluted and tapered distal fixation stems in revision total hip arthroplasties (rTHA).
Methods
We retrospectively analyzed 52 rTHA in 52 patients. Preoperative diagnoses were mechanical loosening (42 cases), septic loosening (8), periprosthetic fracture (1), and femoral stem fracture (1). According to the Paprosky classification, femoral bone stock deficiencies were 19 type-II, 26 type IIIA, and 7 type IIIB. We assessed the behavior of the osteotomy (union, fracture, migration) and the survival and behavior (integration and subsidence) of prosthetic femoral stems.
Results
ETO union and non-union rates were 84.61% (44 patients) and 15.38% (8 cases) respectively. There were twelve (23%) intra-operative fractures of the osteotomy fragment and 11 (21.15%) migrations (4.5 mm on average). We observed bone union in 39 (75%) stems and 13 (25%) stable fibrous unions. Nine (17.3%) stems subsided 7 mm (2–15 mm) on average before becoming stable. Stem subsidence and integration was not significantly affected by ETO fracture/no fracture or union/non-union. The postoperative Harris Hip Score (HHS) improved significantly as compared to the pre-operative HHS (38.41 ± 3.54 vs 85.29 ± 3.36; p < 0.01). Patients were followed up for 55 (24–100) months. The overall implant survival at the end of follow-up was 100%.
Conclusions
In this series, neither the non-union nor the intra-operative fracture of the ETO segment affected the behavior or medium-term survival of femoral stems.
Keywords: Extended trochanteric osteotomy (ETO), Fluted tapered modular stem, Revision total hip arthroplasty
1. Introduction
In revision total hip arthroplasties (rTHA), femoral management can be challenging and time consuming.1,2 Surgeons must remove a failed prosthesis, which could be associated with deficient femoral bone stock, and achieve adequate fixation with the new implant.2,4
To remove the prior femoral component, the surgeon must access the bone-implant or bone-cement interface, depending on the type of fixation used in the primary surgery. In the case of mechanical loosening, cemented implants may coexist with a well-bonded cement mantle and a firm cement restrictor or both the cement restrictor and the distal end of the stem may extend beyond the femoral isthmus.3, 4, 5, 6, 7 A proximal approach to remove the cement restrictor and stem may increase bone damage and cause intraoperative fractures or perforations,4, 5, 6 particularly in the case of deficient bone stock or deformities.5, 6, 7
When preparing the distal femur for the implantation of a femoral prosthesis, it is necessary to take a stepwise approach aimed at achieving immediate mechanical stability without causing further damage and preventing perforations which can be difficult because of the frequent presence of a preexisting varus deformity.4,6,8,9
Extended trochanteric osteotomy (ETO), as described by Younger et al.7 is a technique that can facilitate femoral stem removal and reduce both operative time and complications. It consists in opening a window in the posterolateral third of the proximal femur, which should be long enough to remove the failed femoral component while preserving soft tissue attachments.
Abdel et al.8 analyzed 519 rTHAs with distal fixation modular stems., 319 of which were approached with an ETO. They reported an intraoperative fracture rate of 13% and a >5 mm-stem-subsidence rate of 2.4%. Miner et al.9 analyzed 166 ETOs and reported good results, with a reoperation rate of 10.2%, a non-union rate of 1.2%, and a mal-union rate of 0.6%.
The objective of this retrospective study was to assess whether ETO fracture or non-union affected the survival of modular fluted and tapered distal fixation stem in hip revision surgeries. Our hypothesis was that prosthetic survival rates were similar in ETO union and non-union.
2. Methods
According to our department's database, the ETO approach was used in 56 rTHAs between January 2013 and July 2017. This study was conducted after obtaining the approval of our Institutional Ethics Committee.
We included rTHA-ETO patients with modular fluted and tapered distal fixation stems, followed up for a minimum of 24 months.
Three patients were lost to follow-up and another was excluded because a cemented revision stem was used in the reconstruction.
Fifty-two patients with 52 rTHA, 33 women and 19 men, with a mean age of 68.5 ± 7.5 years (range 45–80) were included.
Indications for revisions were 42 cases of mechanical loosening (80.77%), 8 cases of septic loosening (15.38%), 1 (1.9%) fractured stem, and 1 (1.9%) periprosthetic fracture (Vancouver B3).
The mean preoperative Harris Hip Score (HHS)10 was 38.41 ± 3.54 (range 33.6–77.5).
All the femoral stems extracted were cemented. Septic cases were treated with a two-stage revision using an antibiotic-loaded cement spacer. The osteotomy was always performed in the first stage. The median time between stages was 12 (range 8–24) weeks.
Femoral bone deficiencies were classified using the Della Valle and Paprosky classification.11 There were 19 (36.53%) type II, 26 (50%) type IIIA, and 7 (13,46%) type IIIB defects.
Indication and length of the osteotomy were defined during preoperative planning using anteroposterior (AP) and lateral (L) radiographs of both hips and the femur to be operated on. The length of the osteotomy was determined according to the size of the stem to be removed, the cement mantle and/or the restrictor plug, if any. In periprosthetic infections, the indication also facilitated surgical cleaning.
In 35 cases (67.3%), the osteotomy was performed before dislocating and removing the femoral component. In the remaining 17 cases, where stem removal was easier, the osteotomy was performed after dislocation and removal of the prosthetic component.
All osteotomies were fixed using double-looped cerclage wires. In 36 (69.23%) cases, surgeons placed one or two prophylactic cerclage wires on the diaphyseal femur, depending on the case, to prevent vertical fracture of the distal femur.
Prostheses used were: 21 MP® (Waldemar Link®, Hamburg, Germany), 13 Restoration® (Stryker®, NJ. USA), 13 ZMR® (Zimmer® Ind. USA), and 5 MGS® (Samo®, Bologna, Italy).
In 34 cases, the acetabular component was also revised, and in 14 of them only the polyethylene liner was replaced.
In two cases, surgeons used cortical strut allografts to treat bone stock deficiency or poor bone quality.
In 22 (42.30%) cases, the osteotomy was fixed after placing the distal segment of the stem, and in other 30 (57.69%) after placing the entire final femoral component without preparing the proximal femur with trial segments, depending on the surgeon's preference.
All surgeries were performed by the same surgical team in a laminar airflow operating room, from a posterolateral approach under hypotensive spinal anesthesia. Three doses of 1 g-Cefazolin were used for antibiotic prophylaxis, except in septic revisions where antibiotics were indicated by the Infectology Department. Low-molecular-weight heparin was used as antithrombotic prophylaxis for 4 weeks.
Post-surgery rehabilitation included sitting at the bedside during the first 24 h and mobilizing using a frame or stick after postoperative day 2.
Clinical and radiological outcomes were assessed at weeks 3 and 6, months 6 and 9, and then on an annual basis. In the case of septic loosening, serial laboratory testing was also indicated.
The radiological examination included AP view of the pelvis and AP and lateral view of the affected hip. Radiographs were digitally calibrated according to the diameter of the femoral head, as recorded in the operative report. When applicable, the operative report also included the time of osteotomy fracture.
Radiological measurements and analyses were performed digitally by two independent observers. Differences, if any, were settled by the senior author.
The length of the osteotomy was measured in the immediate postoperative radiograph from the tip of the greater trochanter to its distal end.
During postoperative radiological follow-up examinations assessed the behavior of the osteotomy in terms of union and migration. Union was described as bony callus formation in both projections (AP-L view).
Non-union of the ETO fragment is defined as the absence of signs of union 9 months after surgery.
ETO migration was analyzed by comparing the distance between the teardrop line and the tip of the greater trochanter recorded at each radiological follow-up visit.
The relationship between the different types of pre-operative femoral defects and osteotomy union/non-union was assessed.
The behavior of femoral stems was assessed on the basis of integration-fixation and classified as bone union, stable fibrous union, or unstable fibrous union, according to Engh's criteria 12.
Stem subsidence was determined using Loudon and Charnley method by measuring the distance between a selected variable point in the femoral prosthetic component to a fixed point in the bone.13 This method was used to compare the immediate postoperative radiograph with the subsequent follow-up radiographs. Subsidence was defined as a measurement of ≥2 mm and radiological failure as subsidence >10 mm with no need for a revision procedure. Finally, the behavior (integration and subsidence) of these stems was compared between the group that achieved osteotomy union and the group that did not and the groups with fracture/no fracture of the osteotomy. To objectify clinical results, we used each patient's last annual HHS.
The survival of prostheses was determined by stem replacement for any reason.
2.1. Statistical analysis
Quantitative data were expressed as mean and standard deviation and non-continuous variables were expressed as absolute values and percentages. Fischer's non-parametric test was used for categorical variables and t-student test for numerical variables. A p < 0.05 was considered statistically significant. Statistical analysis was performed using Graph Pad PRISM-7.4.
3. Results
The mean length of the osteotomy was 14.27 cm ± 2.067 (range, 12–24).
The average number of cerclage wires used to close the osteotomy was 2.42 (2–5).
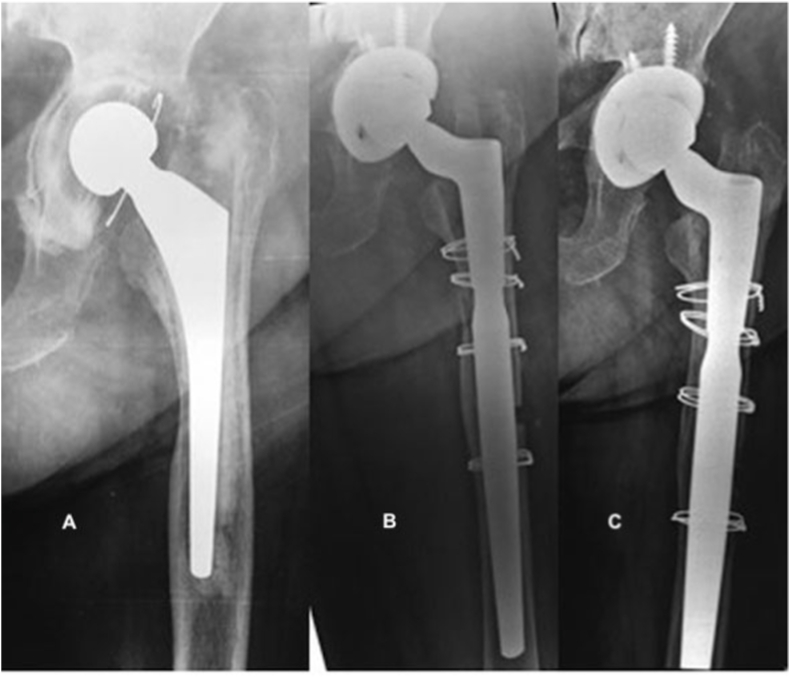
There were twelve (23.07%) fractures of the osteotomy segment [Fig. 1], seven (13.46%) occurred when opening the osteotomy and five (9.61%) during wire-tightening, 9 (75%) of which achieved union. There were no reamer fractures or stem perforations distal to the osteotomy.
Fig. 1.
(A): Preoperative radiograph 12 years after cemented total hip arthroplasty with loose stem. (B): Inmediate postoperative radiograph reveals osteotomy fracture. (C): four years follow-up with healing and remodeling of the osteotomy.
The rate of ETO union was 84.61% (44 hips), over an average time of 9.18 (range, 7–24) weeks. There were 8 (15.38%) cases of non-union [Fig. 2].
Fig. 2.
(A): Preoperative AP radiograph 9 years after hybrid Total Hip Arthroplasty with failed cemented stem. (B): Inmediate postoperative radiograph reveals osteotomy fracture and non-anatomic reduction of the ETO. (C): Seven years follow-up with ETO non-union, bone remodeling and no stem subsidence.
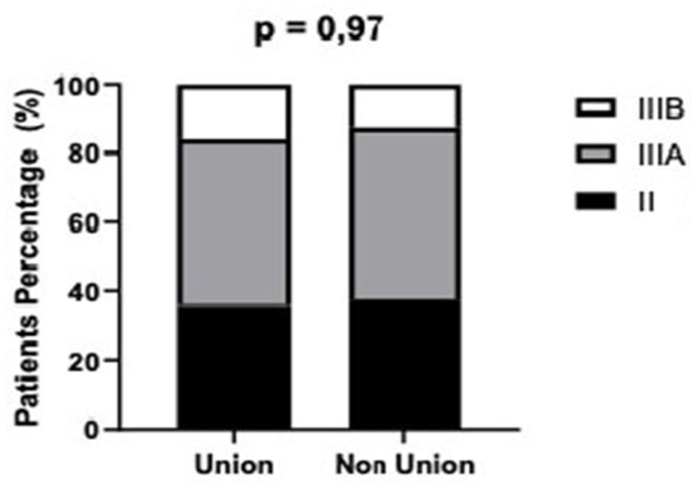
The analysis conducted to determine if preoperative bone stock deficiency exerted an influence on ETO union showed no statistically significant differences [Fig. 3].
Fig. 3.
Comparative analysis of union versus non-union of the ETO depending on previous bone stock deficiency: no statistically significant difference observed.
On average 4.5 mm (range 2–7) osteotomy migration was observed in 11 cases (21.15%). The remaining cases showed no movement.
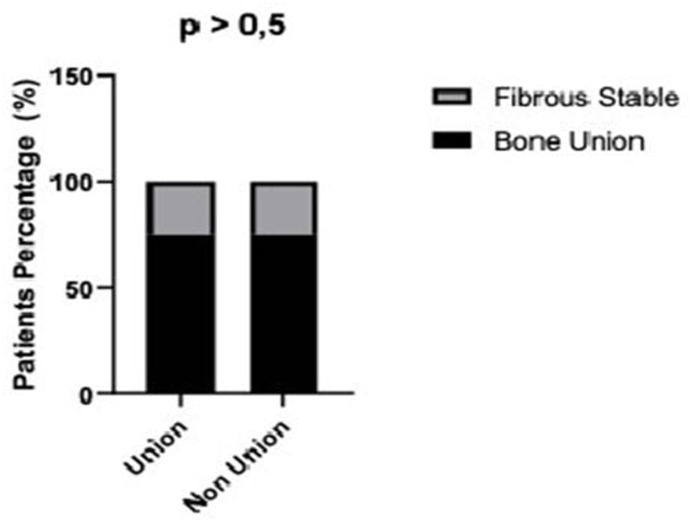
Regarding integration of femoral stems, we observed 39 (75%) bone unions and 13 (25%) stable fibrous unions at the time of the last follow-up visit. ETO union/non-union did not seem to play a significant role, since we found no significant differences (p = 0,999) between these groups, which had a similar rate of stable fibrous union (15.38%) [Fig. 4].
Fig. 4.
Comparative analysis showing not significant differences between the type of fixation and ETO union or non-union.
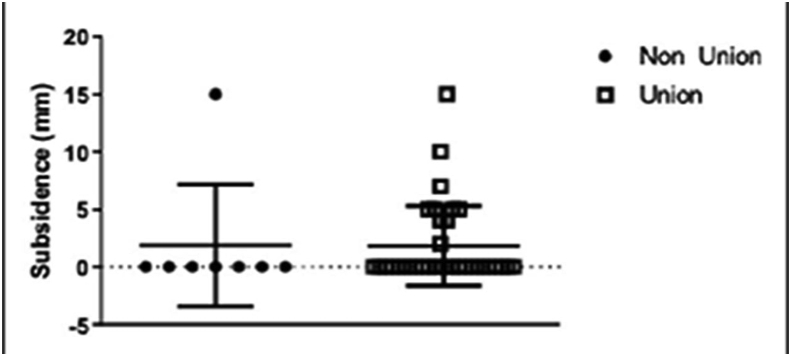
Nine (17.30%) stems subsided within a range of 2–15 mm (average: 7 mm). Four (7.69%) subsided >5 mm, 2 of them (3.84%) >10 mm and were regarded as radiological failure. All these stems stabilized during the first 6 months of the postoperative period and no revision procedures were performed because patients were asymptomatic.
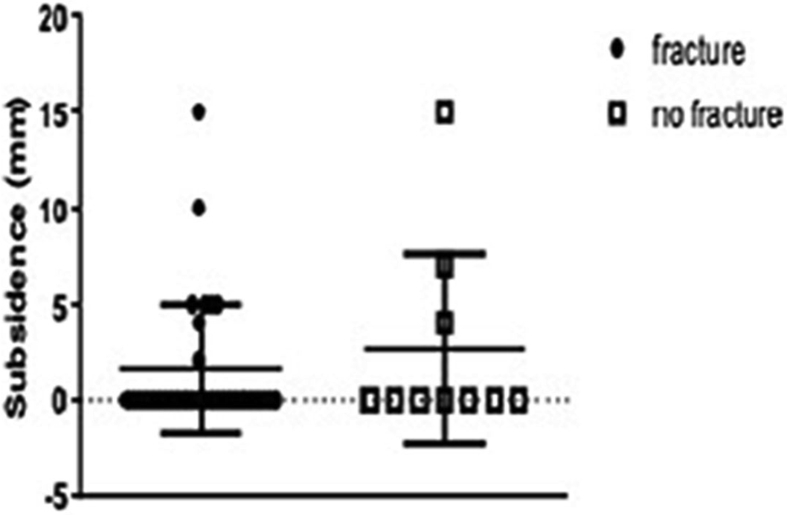
Stem subsidence was not significantly different between the union/non-union groups and the groups with and without fracture of the osteotomy: p = 0.54 and p = 0.69, respectively. [Fig. 5, Fig. 6].
Fig. 5.
Analysis of stem subsidence comparing ETO union and non-union groups: no statistically significant differences were observed.
Fig. 6.
Analysis of stem subsidence comparing ETO fracture and no fracture: no statistically significant differences were observed.
3.1. Complications
One patient (1.92%) suffered 2 dislocations during the first 6 months of the postoperative period and, in both cases, required a closed reduction. After the last event, this patient had no additional dislocations. Two patients (3.84%) presented fracture of the greater trochanter, with a 6- and a 9 mm migration, respectively, but no clinical consequences. One (1.92%) patient suffered an acute infection that was successfully treated with irrigation and debridement and antibiotic therapy.
By the end of the follow-up period, the postoperative HHS showed a significant improvement as compared to the preoperative score (38.41 ± 3.54 vs 85.29 ± 3.36; p < 0,01).
The average follow-up was 55 (18–100) months.
By the end of the study, no patient required a revision procedure for any prosthetic component.
4. Discussion
In this series, the combined use of ETO and modular fluted and tapered distal fixation stems in rTHA achieved a significant improvement in medium-term clinical results, though it was associated with a significant number of complications. The rate of osteotomy non-union and fractures evidences the technical complexity of the procedure.
In our series, this procedure facilitated both the removal of failed components (due to mechanical loosening or septic failure) and surgical cleaning in case of infection, as described by Sambadam et al., ’s 2016 literature review on the most frequent ETO indications.4 In addition, the procedure eased the progressive preparation of the femur for the correct placement of distal fixation stems.4 This is reflected by the rate of bone fixation observed in 50–75% of treated cases, in consistency with other authors’ findings.14,15
With regard to our hypothesis, after analyzing the cases of non-union and/or fracture of the osteotomy, we questioned ourselves about the actual importance of ETO union or integrity, since, at least in this series, the survival of the reconstruction was not negatively affected by non-union or fracture, as reported by Ladurner et al.16
We believe that, in our series, the incidence of ETO non-union and fracture derives from a technical problem. The recommendations for this technique state that before opening the osteotomy with the osteotome, surgeons must make sure the entire length of the osteotomy is complete and try to open it gradually without exerting too much stress and avoiding abrupt movements. If the opening maneuver seems difficult, it is necessary to evaluate which segment has not yet been completed to prevent a fracture. These steps must be carefully followed especially in the case of severe bone stock deficiency.
On the other hand, in 30 cases of our series, the osteotomy was closed after placing the definitive femoral component, without preparing the proximal femur with trial components. This resulted in an inadequate content-container relationship between the proximal stem and the osteotomy blades: when tightening the wires, the osteotomy fractured or failed to achieve full closure. Filling this space with a bone graft could have reduced the incidence of this complication as described by Mardones et al.2 or Younger et al.7 This non-closure of the osteotomy did not occur when, according to the description of the technique, the distal component of the stem was placed, the osteotomy was closed, the proximal trial components were placed and the proximal femur was reamed for the placement of final components.
In this report, the incidence of osteotomy non-union and fracture was higher than in other series. In a recent literature review, Wronka et al.1 reported a non-union rate of up to 20%. Berry's group reported 75 osteotomies with ETO rates of non-union and fracture of 1.33% and 4%, respectively.2 Lim et al.18 reported the cases of 50 ETO patients with a non-union rate of 12%.
Unlike other reports, where the average length of the osteotomy was 12–14 cm,3,4,7,17,18 it was slightly longer in our series. Greater length did not affect the behavior of stems.
During preoperative planning, it is necessary to make sure the length of the diaphyseal segment distal to the ETO is at least 4 cm. Otherwise, the mechanical stability of the revision stem might be compromised. According to a biomechanical study conducted by Russell et al.,19 a diaphyseal segment of 1.5–2.5 cm is enough to achieve stable fixation.
In our series, stem subsidence occurrence was similar to that of reported by other authors in femoral defects up to 3B.15,17, 18, 19, 20, 21 Malahias et al.17 reported a >5 mm-stem-subsidence rate of 7.1% in their aseptic revision procedures using ETO. Bhatia et al.20 analyzed 120 hip revision surgeries and reported 26 (21.66%) cases of initial subsidence, which later stabilized with a 97% survival rate after 5 years. However, in their series, the incidence of peri-prosthetic fractures was 15%.
In our series, there were no intraoperative fractures of the area distal to the osteotomy and no femoral perforations. We believe this was due to the adequate visualization of the distal femur in the osteotomy and the use of prophylactic cerclage wires, especially in cases with less responsive cortical bone.
The incidence of dislocations (1.9%) and infections (1.9%) in our series was similar to the ones reported by Ting et al.,22 Drexler et al.23 and Lakstein et al.24
The limitations of this study are inherent to retrospective studies with few patients. In addition, the follow up that does not allow for a long-term analysis of these reconstructions.
Study strengths include the fact that procedures were conducted in the same center by the same surgical team with an identical postoperative assessment and the use of uncemented modular fluted and tapered distal fixation stems, which are currently common in this type of revision procedures.
5. Conclusions
The combined used of ETO and modular fluted and tapered distal fixation stems has proved to facilitate complex procedures such as cemented stem revisions, although it is associated with several complications. In this series, prosthetic survival was not affected by non-union or fracture of the osteotomy segment. We will continue to follow up this series to determine long-term survival.
Author contributions
Germán Garabano: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing-original draft – review & edition.
Alan Maximiliano Gessara: Data curation, Investigation, Methodology.
Cesar Angel Pesciallo: Validation, Writing - review & editing.
Leonel Perez Alamino: Formal analysis, Software, Validation.
Hernán del Sel: Supervition, Writing - review & editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval
All procedures performed in this retrospective study, which involved the use of data from human participants, were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. The study was approved by de Bioethics Committee of British Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of competing interest
None.
Acknowledgements
None.
References
- 1.Wronka K.S., Gerard-Wilson M., Peel E., Rolfson O., Cnudde P.H.J. Extended Trochanteric Osteotomy: improving the access and reducing the risk in revision THA. EFORT Open Rev. 2020;5(2):104–112. doi: 10.1302/2058-5241.5.190005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mardones R., Gonzalez C., Cabanela M.E., Trousdale R.T., Berry D.J. Extended femoral osteotomy for revision of hip arthroplasty. Results and complications. J Arthroplasty. 2005;20(1):79–83. doi: 10.1016/j.arth.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Paprosky W.G., Martin E.L. Removal of well-fixed femoral and acetabular components. Am J Orthoped. 2002;31(8):476–478. [PubMed] [Google Scholar]
- 4.Sambandam S.N., Duraiswamy G., Chandrasekharan J., Mounasamy V. Extended trochanteric osteotomy: current concepts review. Eur J Orthop Surg Traumatol. 2016;26(3):231–245. doi: 10.1007/s00590-016-1749-z. [DOI] [PubMed] [Google Scholar]
- 5.Charity J., Tsiridis E., Gusmao D. Extended trochanteric osteotomy followed by cemented impaction allografting in revision hip arthroplasty. J Arthroplasty. 2013;28(1):154–160. doi: 10.1016/j.arth.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Pemmaraju G.M., Killampalli V.V. Extended proximal femoral osteotomy: technical tip. Eur J Orthop Surg Traumatol. 2015;25(6):1111–1113. doi: 10.1007/s00590-015-1634-1. [DOI] [PubMed] [Google Scholar]
- 7.Younger T.I., Bradford M.S., Magnus R.E., Paprosky W.G. Extended proximal femoral osteotomy. A new technique for femoral revision arthroplasty. J Arthroplasty. 1995;10(3):329–338. doi: 10.1016/s0883-5403(05)80182-2. [DOI] [PubMed] [Google Scholar]
- 8.Abdel M.P., Cottino U., Larson D.R., Hanssen A.D., Lewallen D.G., Berry D.J. Modular fluted tapered stems in aseptic revision total hip arthroplasty. J Bone Joint Surg Am. 2017;99(10):873–881. doi: 10.2106/JBJS.16.00423. [DOI] [PubMed] [Google Scholar]
- 9.Miner T.M., Momberger N.G., Chong D., Paprosky W.L. The extended trochanteric osteotomy in revision hip arthroplasty. A critical review of 166 cases at mean 3-year, 9 months follow-up. J Arthroplasty. 2001;16(8):188–194. doi: 10.1054/arth.2001.29385. [DOI] [PubMed] [Google Scholar]
- 10.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–755. [PubMed] [Google Scholar]
- 11.Della Valle C.J., Paprosky W.G. The femur in revision total hip arthroplasty evaluation and classification. Clin Orthop Relat Res. 2004;420:55–62. doi: 10.1097/00003086-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Engh Ch, Massin P., Suther K. Roentgenographic assessment of biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 13.Loudon J.R., Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem. J Bone Joint Surg Br. 1980;62-B(4):450–453. doi: 10.1302/0301-620X.62B4.7430222. [DOI] [PubMed] [Google Scholar]
- 14.Ladurner A., Zdravkovic V., Grob K. Femoral bone restoration patterns in revision Total Hip Arthroplasty using distally fixed modular tapered titanium stems and extended trochanteric osteotomy approach. J Arthroplasty. 2018;33(7):2210–2217. doi: 10.1016/j.arth.2018.02.065. [DOI] [PubMed] [Google Scholar]
- 15.Amanatullah D.F., Howard J.L., Siman H., Trousdale R.T., Mabry T.M., Berry D.J. Revision total hip arthroplasty in patients with extensive proximal femoral bone loss using a fluted tapered modular femoral component. Bone Joint Lett J. 2015;97-B(3):312–317. doi: 10.1302/0301-620X.97B3.34684. [DOI] [PubMed] [Google Scholar]
- 16.Ladurner A., Zurmuhle P., Zdravkovic V., Grob K. Modified extended trochanteric osteotomy for the treatment of Vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty. 2017;32(8):2487–2495. doi: 10.1016/j.arth.2017.02.079. [DOI] [PubMed] [Google Scholar]
- 17.Malahias M.A., Gkiatas I., Selemon N. Outcomes and risk factors of extended trochanteric osteotomy in aseptic revision total hip arthroplasty: a systematic review. J Arthroplasty. 2020;S0883–5403(20):30791–30799. doi: 10.1016/j.arth.2020.07.034. [DOI] [PubMed] [Google Scholar]
- 18.Lim C.T., Amanatullah D.F., Huddleston J.I., Hwang K.L., Maloney W.J., Goodman S.B. Use of cortical strut allograft after extended trochanteric osteotomy in revision total hip arthroplasty. J Arthroplasty. 2017;32(5):1599–1605. doi: 10.1016/j.arth.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 19.Russell R.D., Pierce W., Huo M.H. Tapered vs cylindrical stem fixation in a model of femoral bone deficiency in revision total hip arthroplasty. J Arthroplasty. 2016;31(6):1352–1355. doi: 10.1016/j.arth.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Bhatia P.K., Barnett S.L., Lovell T.P., Hozack W.J., Malkani A.L. Femoral component revision using a 2nd generation modular femoral implant. J Arthroplasty. 2015;30(8):1397–1402. doi: 10.1016/j.arth.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 21.Jibodh S.R., Schwarzkopf R., Anthony S.G., Malchau H., Dempsey K.E., Estok D.M. Revision hip arthroplasty with a modular cementless stem: mid-term follow up. J Arthroplasty. 2013;28(7):1167–1172. doi: 10.1016/j.arth.2012.07.031. [DOI] [PubMed] [Google Scholar]
- 22.Ting N.T., Wera G.D., Levine B.R., Della Valle C.J. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin Orthop Relat Res. 2010;468(9):2382–2386. doi: 10.1007/s11999-010-1284-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drexler M., Dwyer T., Chakravertty R., Backstein D., Gross A.E., Safir O. The outcome of modified extended trochanteric osteotomy in revision THA for Vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty. 2014;29(8):1598–1604. doi: 10.1016/j.arth.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Lakstein D., Kosashvili Y., Backstein D., Safir O., Lee P., Gross A.E. The long modified extended sliding trochanteric osteotomy. Int Orthop. 2011;35(1):13–17. doi: 10.1007/s00264-009-0890-2. [DOI] [PMC free article] [PubMed] [Google Scholar]