Abstract
Backgroud
Under the circumstance of school closures caused by the coronavirus outbreak, medical schools in China began implementing online teaching, including histology and embryology (HE) beginning in the middle of February 2020. The changes in HE education in responding to the pandemic in China needs to be determined, for further adaption of online teaching delivery or blended learning.
Methods
A nationwide survey of the major medical colleges was conducted via WeChat.
Results
In total, 83 medical schools (one respondent per school) were invited to survey, 78 medical schools responded which represented most medical schools across all the provinces in mainland China, as well as Hong Kong and Macao. The results revealed that 77% (n = 60) and 58% (n = 45) of the responding schools had conducted HE theoretical and practical online teaching, respectively, prior to the pandemic; however, 27% (n = 21) of the medical schools had temporally suspended practical sessions at the time the survey was completed. During the pandemic, 73% (n = 57) and 29% (n = 23) of the medical schools delivered HE theoretical and practical sessions by synchronous live broadcasting, respectively; 65% (n = 51) of the medical schools increased virtual microscopy using during practical sessions. During the pandemic, 54% (n = 42) of the medical schools implemented teaching activities promoting active learning; meanwhile, online assessment was implemented in 84% (n = 66) of the responding medical schools. With regard to the satisfaction with the effectiveness of online teaching during the pandemic, 64% (n = 50) of the medical schools gave positive answers and considered that it was a good opportunity to develop novel and diversified teaching methods. Despite various difficulties such as work overload and unstable online teaching environments, most medical schools are willing to continue or increase theoretical online teaching after the pandemic.
Conclusions
Medical institutes in China were the earliest of closing campuses and having complete online teaching experience during the pandemic. This paper presents overall HE teaching situation extracted from the survey, to assist other medical schools optimizing the transitions to quality online teaching within a short time, and to serve as reference for schools that demand essential knowledge in online teaching methods, infrastructure construction, and platform integrations.
Keywords: Histology education, Embryology education, Medical education, Virtual sessions, Covid-19 pandemic, Online teaching
1. Introduction
An unexpected coronavirus pandemic erupted suddenly in early 2020 and quickly spread throughout the world. Millions of people have been infected worldwide, and some patients with serious complications still face the threat of death, since there have not yet been specific treatments developed for Covid-19 [[1], [2], [3]]. The first report received by the World Health Organization (WHO) that a small cluster of pneumonia cases with unknown etiology in Wuhan, Hubei Province, China, was made on December 31, 2019 [4]. The virus had subsequently confirmed in several other countries in southern and eastern Asia by the middle of January. To control the outbreak of the virus, the Chinese government imposed a modern form of quarantine: shutting down all transportation in and out of Wuhan on January 23, 2020. The lockdown soon expanded to twelve other cities in Hubei Province [5]. On March 11, 2020, the WHO officially declared the outbreak a pandemic. Consequently, almost every country has put forward various restrictive measures of population shifts and social interactions against the spread of Covid-19 [6].
People's normal lives fell into complete stagnation because of the influence of the Covid-19 pandemic [7], which unreservedly spread to global schools and universities, including medical schools [8]. More than one hundred countries had closed their schools by the middle of March 2020, which affected the normal studies of nearly half of the global student population [9]. Traditional face-to-face education and academic activities in universities all over the world were suspended temporally and moved to online learning [10,11]. As part of the first country to perform quarantine during the pandemic, medical schools in China have been offering online education to medical students ever since the middle of February, which is usually the time of the back-to-school season for the spring term at most Chinese universities.
Histology, also called microanatomy is a prerequisite discipline for studying other medical courses [12,13]. Embryology is the basic science that describes the development of an organism within the maternal uterus. These two basic medical sciences are combined into one course in mainland China, histology and embryology (HE), which is usually separated from gross anatomy. A nationwide survey on HE education in China was carried out by our team two years ago to give educators an overall introduction to HE teaching [14]. Traditionally, the HE theoretical knowledge is taught in a lecture-based classroom, followed by practical sessions in a histology laboratory. During the Covid-19 pandemic, how did Chinese HE teachers adjust themselves to adapt to the abrupt change in situation, and how did they transform their traditional face-to-face classes into an entire online courses in such a rapid time?
As we know, the achievement of online teaching is heavily reliant on various technologies, including the appreciation of broadband and teaching platforms [15]. In recent years, techniques based on the internet have progressed greatly in China, producing a profound effect on education. Online teaching and learning activities are becoming popular among teaching academics and learners. Some live broadcasting platforms and teaching management platforms have rapidly developed in China. Commonly used synchronous live broadcasting teaching platforms include Tencent classrooms/meetings (Tencent Holdings Ltd., Shenzhen, China), which are similar to those available by Zoom (Zoom Video Communications Inc., San Jose, CA), which is popular in other parts of the world. Teaching management platforms such as Rain Classroom (Tsinghua University, Beijing, China), Xuexitong (Tsinghua University, Beijing, China) and Blackboard (Blackboard Corp., Washington, DC) are the most popular choices for Chinese teachers to upload and issue their teaching materials, including videos, presentations, exercises, etc. A few teaching management platforms, for example, Rain Classroom and Xuexitong, have upgraded their functions to support live broadcasting teaching. The massive open online courses (MOOCs), such as the Chinese University MOOC (Chinese University MOOC, Beijing, China), Xuetang Online (Tsinghua University, Beijing, China), Zhihuishu (Able-Elec Co. Ltd., Shanghai, China), and PMPH MOOC (People's Medical Publishing House, Beijing, China), are well recognized on different course platforms as content providers for medical courses in China. Screen capture and postproduction software, including Corel Video Studio (C&J Marketing Software Co., Ltd., Suzhou, China) and QQ Yingyin (Tencent Holdings Ltd., Shenzhen, China), which function as Camtasia (TechSmith Corp., Okemos, MI), and are extensively used worldwide. In addition, some social media apps, for example, WeChat (Tencent Holdings Ltd., Shenzhen, China) and QQ Yingyin (Tencent Holdings Ltd., Shenzhen, China), also provide live broadcasting in China. Till May 2020, there had already been 43 MOOCs related to human histology and/or embryology on different teaching platforms in China, providing free courses for social learners.
Except for theoretical session, microstructural observation under a microscope in a practical laboratory is also an important part of HE teaching. The progress of techniques has brought about the extensive application of virtual microscopy in histology education [16,17]. With the help of slide scanners, a large number of high-resolution images of existing histological slides have been digitalized so that medical students do not have to rely on light microscopes in histological laboratory [18,19]. The national survey for HE teaching completed in 2018 demonstrated that 40% of medical schools in mainland China had already been partly or completely equipped with virtual microscopy in teaching [14]. The combination of virtual microscopy platform with the application of light microscopy is the most preferred approach at most of medical schools in China. Virtual microscopy platform is constructed and maintained by each individual medical school, while most of them are open to off-campus users if authorized by government as national or provincial experimental centers (i.e., supported by national or provincial government). The shift from light microscopy to virtual microscopy over the years has undoubtedly provided infrastructure for online histology courses during the current pandemic period. Nevertheless, are these appreciative techniques sufficient enough to meet the basic needs of histology online education when we have few other choices in the matters during the pandemic outbreak and related school closures?
In this context, we conducted a nationwide survey among Chinese professional HE teachers at April 2020 - after two months of complete online HE teaching, to assess the general situation of HE education online during the pandemic in China, and to provide HE teachers with some facts regarding effectively teaching online. Based on information from the Chinese Ministry of Education (MOE) website, there are currently 128 medical colleges/schools in mainland China, 2 in Hong Kong, and 1 in Macao, which are either independent medical universities or medical schools within a comprehensive university. Students in clinical medicine programs are the predominant group found in medical schools, and they are trained with a standard teaching syllabus formulated by the MOE; therefore, the items in the questionnaires focus on clinical medicine programs.
2. Materials and methods
2.1. The survey implementation
The survey instrument was designed to collect information about HE online teaching during the Covid-19 pandemic, which ranged from mid-February 2020 until mid-April 2020 in China, including such aspects of HE online teaching as theoretical sessions (lectures), practical sessions, active learning activities, online assessment, and thinking about the experience. The questionnaire items of the survey instrument were developed in Chinese (see Supplementary Material 1 for the translated, English version). The survey was piloted with the faculty members of the first author to ensure the clarity of the questionnaire and was subsequently revised based on the feedback.
A convenience sampling of the HE departments was used. The directors of the HE departments of most of the medical schools in China were part of a messaging group in the WeChat application, which is a popular social media mobile application [20]. An invitation to participate by completing the survey instrument on an online survey platform, SoJump (Ranxing, Changsha, China), was sent to the group members individually [21,22]. The survey participation was voluntary. Only one completed survey was included from each school. The following medical schools were excluded: traditional Chinese medical schools and specialist technology colleges. Some completed surveys were followed up with phone calls to confirm the accuracy of the information, to clarify obscure answers and to help the respondents complete omitted items if they were willing to do so. The survey was performed with the collaboration of the Chinese Society for Histology and Embryology, a section of the Chinese Society for Anatomy Sciences (CSAS), which is the national organization of anatomical educators.
2.2. Data analysis
All statistical and graphical analyses were performed using the SPSS statistical package, version 17.0 (IBM Corp., Armonk, NY). The data obtained from the questionnaires were analyzed using Cronbach's alpha test to determine the internal consistency of the responses. Kendall's tau b test was used to assess the correlations of the items in the questionnaires with different types of medical schools. Results of the statistical analyses were presented as mean ± standard deviation (SD), and considered statistically significant when P < 0.05.
3. Results
In this survey, we invited 83 medical schools in mainland China, Hong Kong and Macau via WeChat or email to complete the questionnaires. Only one teacher in each school was invited to complete the questionnaire. Eventually, 78 respondents answered the questions in the questionnaire, which were proven to be effective. Thus, the response ratio was 94%. The distribution of the completed surveys covered the 23 provinces, 5 autonomous regions and 4 municipalities in mainland China, as well as the two special administrative regions of Hong Kong and Macao.
The 337 main cities in mainland China are classified into six-level city tier system, which are the first, new first, second, third, fourth and fifth-tier cities, according to the degree of commercial resources aggregation, city junctions, citizen's activities, diversities of livings, and future plasticity (http://www.199it.com/archives/1057872.html). Hong Kong and Macao are also categorized into first tier cities because of their international status. Based on the locations, 33 surveyed medical schools are situated in first-tier and new first-tier cities. There is only one medical school in the fifth-tier city. Therefore, the medical schools in the fourth (n = 13) and fifth-tier cities (n = 1) are combined as one group for further correlation statistics. “Double first-class” - the newest government assessment criteria to categorize universities in mainland China, means “world-class universities” and “first-class disciplines”. There are 42 world-class universities and 95 universities having first-class disciplines [23]. Based on this criterion, 21 of the 78 medical universities/schools in this survey are qualified as “double first-class”.
The value for Cronbach's alpha for the 15 single-answer items in the questionnaire was 0.376. The results of Kendall's tau b test showed the correlation coefficient amongst cities classification and the items in the questionnaire (Table 1 ).
Table 1.
The correlation coefficient among the items and various types of medical schools.
| City tier system | Double first class |
2 | 3 | 6 | 7 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 17 | 18 | 20 | 21 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Double - first class | .298** | – | |||||||||||||||
| 2. How to implement online theoretical sessions before the pandemic | 0.063 | 0.075 | – | ||||||||||||||
| 3. The format of online theoretical sessions during the pandemic | −0.107 | −0.078 | −0.051 | – | |||||||||||||
| 6. Time used for student-teacher interaction for synchronous live broadcasting of theoretical sessions | 0.086 | 0.000 | 0.014 | −0.142 | – | ||||||||||||
| 7. How to record the theoretical sessions for asynchronous recorded broadcasting | −0.070 | −0.122 | 0.172 | .307* | −0.206 | – | |||||||||||
| 9. The change in content materials for online theoretical sessions | −0.120 | −0.078 | 0.039 | 0.103 | 0.132 | 0.063 | – | ||||||||||
| 10. How to conduct online practical sessions before the pandemic | 0.035 | 0.132 | .344** | 0.101 | 0.102 | 0.069 | 0.134 | – | |||||||||
| 11. The increase use of VM in the practical sessions during the pandemic | 0.188 | 0.205 | −0.062 | −0.088 | -.245* | −0.097 | -.278** | −0.060 | – | ||||||||
| 12. The format of the online practical sessions during the pandemic | 0.023 | -.217* | 0.011 | .320** | 0.139 | 0.058 | −0.028 | 0.058 | -.267** | – | |||||||
| 13. The platforms/tools employed for practical sessions during the pandemic | −0.104 | -.251* | −0.164 | −0.053 | 0.056 | −0.186 | 0.124 | −0.118 | −0.129 | 0.207 | – | ||||||
| 14. Time used for teacher-student interaction during the online practical sessions | −0.004 | -.276* | 0.045 | −0.122 | .367** | −0.002 | 0.030 | −0.009 | -.266* | 0.061 | 0.010 | – | |||||
| 15. Active learning implementation before and during the pandemic | 0.139 | −0.046 | 0.135 | 0.126 | 0.158 | .317** | 0.040 | .282** | −0.072 | 0.144 | −0.115 | 0.139 | – | ||||
| 17. The tools employed to implement active learning during the pandemic | 0.026 | 0.085 | 0.154 | 0.049 | −0.078 | 0.031 | 0.081 | 0.074 | 0.024 | −0.085 | 0.025 | −0.181 | −0.118 | – | |||
| 18. Online assessment implementation before and during the pandemic | 0.019 | −0.210 | 0.050 | 0.018 | 0.165 | 0.184 | −0.029 | −0.004 | −0.180 | 0.176 | −0.105 | .341** | .323** | 0.017 | – | ||
| 20. Evaluating the effectiveness of online learning performed during the pandemic | −0.188 | 0.074 | 0.020 | −0.181 | -.355** | 0.036 | −0.174 | −0.102 | 0.125 | −0.138 | 0.052 | -.302* | −0.186 | −0.028 | −0.043 | – | |
| 21. Satisfying with the effectiveness of online learning during the pandemic | .206* | 0.068 | 0.089 | 0.052 | .344** | −0.041 | 0.159 | .234* | −0.162 | 0.139 | −0.075 | .346** | 0.199 | 0.105 | 0.052 | -.643** | – |
| 24. Continuingonline teaching after the pandemic | 0.038 | −0.040 | −0.033 | −0.066 | 0.137 | 0.163 | .206* | 0.109 | 0.035 | 0.036 | 0.066 | 0.038 | .211* | 0.066 | 0.041 | −0.124 | 0.121 |
**P < 0.01; *P < 0.05.
3.1. Theoretical sessions (lectures)
Synchronous live broadcasting is the most popular format of HE online teaching. The survey showed that 77% (n = 60) of the medical schools had already implemented various forms of online HE theoretical lectures before the pandemic, including developing MOOCs (18%, n = 14), flipped classrooms (21%, n = 16), and mixed online and face-to-face teaching formats (38%, n = 30). During the pandemic, the major delivery methods for HE theoretical sessions were live broadcasting (40%, n = 31), recorded broadcasting (13%, n = 10), and blended live and recorded broadcasting (33%, n = 26). Several teachers chose live or recorded broadcasting by audio instead of video (4%, n = 3). Among the schools where live broadcasting was chosen for their online theoretical sessions, 63% (n = 36) of them utilized synchronous live broadcasting platforms, e.g., Tencent classrooms/meetings, 36% (n = 21) of them used teaching management platforms with live broadcasting capability, e.g., Rain Classroom, Xuexitong, and 31% (n = 18) of them used social software, e.g., QQ and WeChat. During synchronous live broadcasted theoretical sessions, the vast majority of the surveyed medical schools (83%, n = 47) used less than half of the class time to interact with their students, and real-time interactive communication via voice (91%, n = 52) or text (89%, n = 51) was the most commonly used means of interaction. Other interaction forms, such as real-time on-screen comments (Danmu) and online voting (44%, n = 25), real-time online answering questions based on PowerPoint plug-ins during the synchronous live broadcasting class (51%, n = 29), and organizing online discussions among student group members (39%, n = 22), were also adopted by some schools.
Regarding asynchronous theoretical sessions, Powerpoint presentation screen capturing is most commonly used for HE online teaching. However, 61% (n = 22) of the schools adopted without teachers appearing in recorded videos, 27% (n = 10) of the schools did postproduction processing, which may have included teachers’ talking-head videos. After recording HE theoretical sessions, 44% (n = 16) of the schools chose teaching management platforms, e.g., Xuexitong, Rain Classroom, and Blackboard, to release the videos, while 24% (n = 9) of the schools used online courses platforms, e.g., Chinese University MOOC, PMPH MOOC, and Zhihuishu, and 19% (n = 7) of the schools used social software, e.g., QQ and WeChat. In regard to the contents of HE theoretical sessions, 38% (n = 30) of the responding schools completely redesigned their teaching materials for online delivery, while 36% (n = 28) of the schools only slightly modified their content, and 18% (n = 14) of the schools did modify their teaching materials at all.
3.2. Practical sessions
The HE online practical sessions were implemented at a much lower rate if compared with the theoretical sessions. The survey showed that 58% (n = 45) of the responding schools had experience with implementing online HE practical sessions using the MOOC (9%, n = 7), flipped classroom (15%, n = 12), or blended method (33%, n = 26). During the pandemic, HE practical sessions were temporally suspended in 21 responding schools (27%) at the time the survey was performed. For the schools that still conducted online HE practical sessions, 40% of the schools used synchronous live broadcasting (n = 23), 12% of the schools used asynchronous recorded broadcasting (n = 7), and 30% of the schools used both live and recorded broadcasting (n = 17). Fifty percent of the responding schools (n = 39) showed an increased use of virtual microscopy in online HE practical sessions by more than 50%, 15% of the schools (n = 12) showed an increase of less than 50%, and 35% of the schools (n = 27) reported no change in their use of virtual microscopy in online HE practical sessions. Among these schools, 49% (n = 28) used virtual simulation platforms built by their own institutions, while 36% (n = 21) and 15% (n = 8) of the schools used national or provincial virtual simulation platforms, respectively, which are virtual resource-sharing platforms recognized by central or local governments. It was found that 65% (n = 35) of the responding schools used less than 50% of the class time for interacting with students, and 30% (n = 16) of the medical schools used more than 50% of the class time as practical time.
3.3. Active learning sessions and online assessment
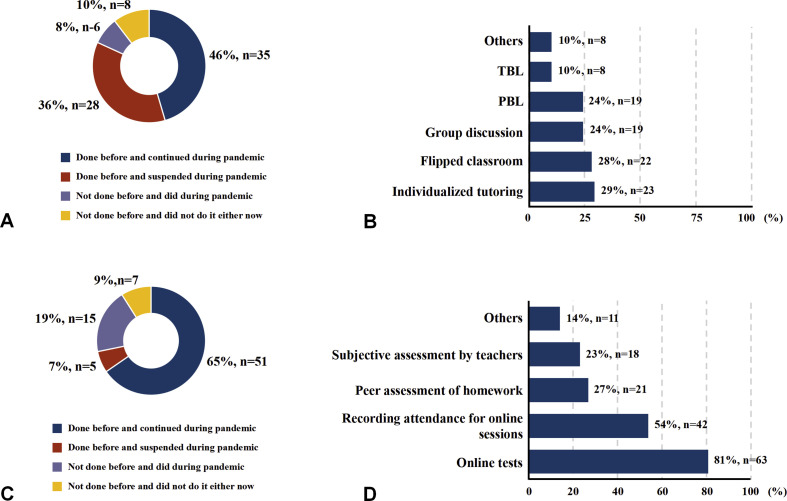
The students-centered teaching strategies were also employed during HE online teaching, but a sizable reduction could be observed. Before the pandemic, 82% (n = 64), of the responding schools had active learning sessions (e.g., flipped classroom, small group discussion, problem-based learning (PBL), and team-based learning (TBL), individualized tutoring). Among them, 46% (n = 36) continued these sessions during the pandemic, while 36% (n = 28) of the schools suspended them. Interestingly, 8% (n = 6) of the responding schools initiated active learning during the pandemic although they had never done so before (Fig. 1 A). The active learning sessions included individualized tutoring, flipped classroom, small group discussion, PBL, TBL, etc. (Fig. 1B). The platforms for running these sessions were mainly teaching management platforms such as Rain Classroom, Xuexitong, and Blackboard (86%, n = 36), although 52% (n = 22) of the responding schools utilized social media, e.g., QQ and WeChat. Other platforms including “Panopto (Panopto, Seattle, WA)”, “Zoom” and “Duifene (Duifene, Shanghai, China)” were also used by some teachers (others, 10%, n = 4).
Fig. 1.
Survey of various aspects regarding online HE active learning and assessment at medical schools in China during the pandemic.
A: Pie chart showing the implementation of active learning (e.g., partly flipped classroom, group discussion, PBL, TBL, and individualized tutoring) before and during the COVID-19 pandemic (n = 78). B: Bar chart showing the types of active learning implemented for HE during the COVID-19 pandemic (n = 42). C: Pie chart showing the implementation of online assessment before and during the pandemic (n = 78). D: Bar chart showing the main formats of online assessment employed for HE teaching during the pandemic (n = 71). Abbreviations: PBL, problem-based learning; TBL, team-based learning; HE, histology and embryology.
One particular challenge for educators switching to the online format from traditional teaching is how to implement assessment. Before the pandemic, 72% (n = 56) of the responding schools had experience with using online assessments. Among them, 65% (n = 51) of the schools continued their use during the pandemic, while 7% (n = 5) of the schools suspended their online assessments during the study period. The remaining 28% (n = 22) of the responding schools did not have experience with online assessments before the pandemic. Among them, 19% (n = 15) of these schools initiated online assessments during the pandemic (Fig. 1C). Among the responding schools that carried out online assessments, the vast majority of the medical schools adopted online tests, while the others utilized peer assessments for homework, attendance for online sessions, and subjective assessments by teachers (Fig. 1D). Some other applications (APPs) e.g. “Mentimeter quiz (Mentimeter AB, Alströmergatan, Sweden)”, “Sojump”, were employed for online assessment, mentioned at “others” option.
3.4. Teacher experience
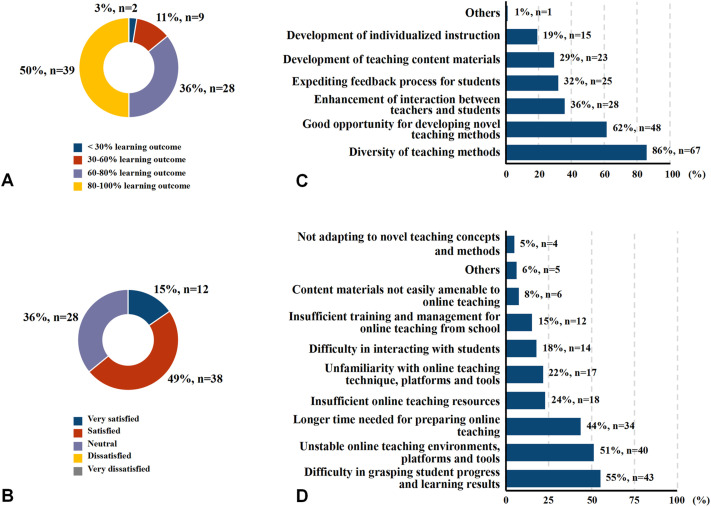
Teachers were also aware of the importance of their perceptions on this high-impact online teaching experience. Only approximately 50% (n = 39) of the responding teachers estimated that their online sessions during the pandemic helped students achieve 80–100% of the intended learning outcomes, while 36% (n = 28) claimed a 60–80% achievement rate, 11% (n = 9) claimed a 30–60% achievement rate, and 3% (n = 2) claimed a <30% achievement rate (Fig. 2 A). In addition, 15% (n = 12) and 49% (n = 38) of the responding schools reported that they were “very satisfied” and “satisfied”, respectively, with the effectiveness of their online teaching during the pandemic (Fig. 2B). The average values of Likert scale for satisfaction was 3.79 ± 0.69, if 1–5 rating scale from “very dissatisfied” to “very satisfied”. They reported that the top two gains from online learning were the “diversity of teaching methods” and “good opportunities for developing novel teaching methods” (Fig. 2C). The top two difficulties for the responding teachers were reported as “difficulty grasping students' progress and learning outcomes” and “unstable online teaching environments, platforms and tools” (Fig. 2D). Some teachers said the first week of online teaching was much difficult to adapt, and the students’ firsthand experience was irreplaceable for medical practical science. When asked whether they were willing to continue their online teaching after the pandemic, 58% (n = 45) of the responding teachers said they were willing to continue to implement theoretical sessions online, but only 1 medical school would continue to implement practical sessions online, while 17% (n = 13) of the respondents said that they would like to switch back to face-to-face teaching.
Fig. 2.
Survey of various aspects regarding personal perception for online HE teaching at medical schools in China during the pandemic (n = 78).
A: Pie chart showing the percentage of teaching objectives achieved by HE online teaching. B: Pie chart showing the satisfaction of HE online teaching during the pandemic. C: Bar chart showing the largest gain from online teaching during the pandemic. D: Bar chart showing the greatest difficulties encountered in implementing online teaching during the pandemic. Abbreviations: HE, histology and embryology.
3.5. Correlation analysis
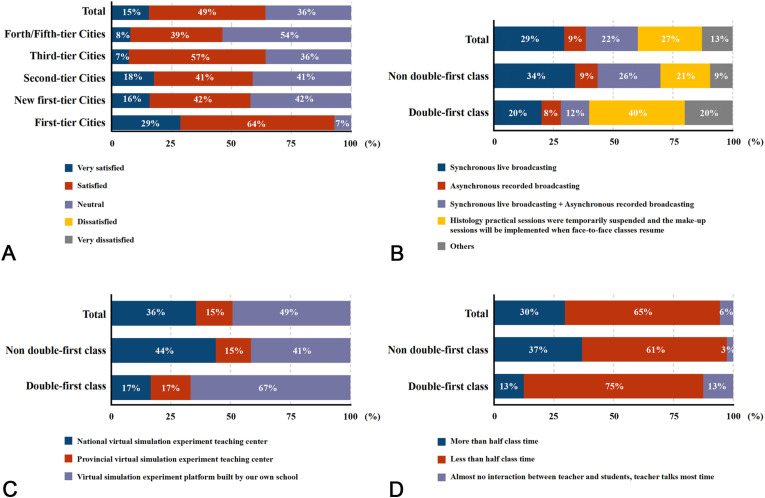
The correlation analyses were carried out between the items in the questionnaire and various classifications of medical schools (Table 1). It showed that the satisfaction of online teaching effectiveness was correlated with the city tier system (r = 0.206, P = 0.034, n = 78), with significantly higher satisfaction of the first-tier cities than others (Fig. 3 A). If classified by “Double First-Class” universities, there are positive correlations on the formats of the online HE practical sessions (r = 0.217, P = 0.035, n = 78, Fig. 3B), the platforms employed for HE practical sessions during the pandemic (r = 0.251, P = 0.045, n = 57, Fig. 3C), and the time used for teacher-student interaction during the online practical sessions (r = 0.276, P = 0.040, n = 54, Fig. 3D).
Fig. 3.
Survey of various aspects with statistical significant correlations if classified the responding medical schools into different categories.
A: Bar chart showing the percentage of satisfaction of online teaching effectiveness when classified by city tier system (n = 78). B–D: If classified by “Double First-Class” universities, B: Bar chart showing the percentage of the online HE practical sessions formats (n = 78); C: Bar chart showing the percentage of the platforms employed for HE practical sessions (n = 57); D: Bar chart showing the percentage of the time used for teacher-student interaction during the online practical sessions (n = 54). Abbreviations: HE, histology and embryology.
Meanwhile, the teachers' evaluation of the effectiveness of online learning was closed related to the extent of teachers' satisfaction with online teaching (r = −0.643, P = 0.000, n = 78). Furthermore, both aspects were closely associated with the amount of their interactive time with students (about evaluation of online learning effectiveness, for theoretical sessions, r = -0.355, P = 0.002, n = 70; for practical sessions, r = -0.302, P = 0.019, n = 54; about extent of teachers’ satisfaction with online learning, for theoretical sessions, r = 0.344, P = 0.002, n = 70; for practical sessions, r = 0.346, P = 0.007, n = 54). The interactive time with students on theoretical sessions was also positively related to the counterpart on practical sessions (r = 0.367, P = 0.007, n = 54). In regard to their intention to continue online teaching after the pandemic, the answer was associated with both changes on HE theoretical content materials (r = 0.206, P = 0.038, n = 78) and active learning implementation before and during the pandemic (r = 0.211, P = 0.037, n = 70).
3.6. Suggestions of sustainable development about HE online teaching
The open-end questions contained the suggestions for the sustainable development about HE online teaching (Table 2 ). The medical schools responded to the survey actually put forward many valuable suggestions for future HE online teaching. The responses mainly focused on four aspects, i.e., attitudes about online teaching (20%, n = 10), demands of sharing online teaching resources (37%, n = 19), online teaching strategies (29%, n = 15), and requirements of improving online teaching environments (10%, n = 5). Several medical schools advocated that CSAS should set up HE online course standards and develop a concise online HE curriculum that optimizes the basic knowledge points and redesign the course contents. Many respondents appealed for the sharing of premium online teaching resources among the medical schools nationwide, especially for the practical sessions, and sharing of virtual slides with typical microstructures as well. Some other medical schools provided very detailed suggestions on how to improve the interactions and online assessments using current virtual microscopy platforms.
Table 2.
Teachers’ comment analysis and the representative quotes (n = 51).
| Categories | Subcategories | Comments n (%) | Representative quotations |
|---|---|---|---|
| Attitudes on online teaching | Positive | 6 (12%) |
|
| |||
| Neutral | 4 (8%) |
|
|
| |||
| Strong desire to share premium online resources among medical schools | Curriculum standards | 3 (6%) |
|
| |||
| Online teaching resources | 16 (31%) |
|
|
| |||
| Suggestions and problems of online teaching | For teachers themselves | 4 (8%) |
|
| |||
| Online teaching strategies | 8 (16%) |
|
|
| |||
| Problems | 3 (6%) |
|
|
| |||
| An appeal for the improvement of online teaching environments | 5 (10%) |
|
|
| |||
| Others | 2 (4%) |
|
4. Discussion
As an effective measure to restrain the Covid-19 outbreak, the stay-at-home policy, which is a double-edged sword, also sent medical students away from their campuses. From the start of the 2020 spring semester, all the medical schools in mainland China moved their teaching activities online for their students at home [24]. The abrupt switch from “face-to-face” or blended learning to complete online teaching was unpredictable. Therefore, it basically reflected the real circumstance of online medical education in China. The information in this survey was obtained from 78 effective responses representing the major medical schools in China, therefore, the survey could be recognized as representative of HE online teaching during the Covid-19 pandemic in China.
4.1. Theoretical and practical sessions
We need to admit that the fast accomplishment of HE online education due to the Covid-19 pandemic benefited from the infrastructure construction of histology education resources, which could be reflected from the relatively high proportion of HE online teaching experience prior to the pandemic; 60 and 45 of the 78 responding medical schools, respectively, had different formats of online theoretical and practical HE teaching. In recent years, web-based HE learning has also been widely applied at medical schools in China in conjunction with the rapid development of web-based histology worldwide [25,26]. Regardless of the method used to deliver HE content online, such as live videos, recorded videos or blended videos, each of the methods needs technical support, which cannot be fulfilled within a few days/weeks without any foundation. As a novel educational mode, e-learning first appeared in mainland China in 2001 [27]. Since then, the e-learning industry in mainland China has emerged as an explosive developmental process, and it has dramatically facilitated Chinese higher education's online learning by means of providing various educational platforms and tools. It is hard to argue against the fact that the prevailing development paradigms of these software programs dramatically promote the implementation of online teaching in China, or that the effective technical measures also generate a large number of courseware, as in other countries [28].
However, the current results adequately suggest that medical schools in first-tier and new first-tier cities adapted better in response to the pandemic, migrating to online environment in terms of better equipment of digital resources and IT support. For example, the medical schools in first-tier or new first-tier cities completed 50% of HE MOOCs, with the medical schools in the first-tier cities ranking first at “accomplishing 80–100% of the teaching objectives” (71%) and being “satisfied with their online HE teaching” (64%).
A challenge for improving distance education is the issue of how to manipulate the interaction between teaching academics and students [[29], [30], [31]]. The implemented social distance measures in response to the pandemic have forced the shift of human social interaction from offline dominance to online dominance [32], which obviously involves the field of communication. Students claim that one of the important reasons for them to feel that they struggle with distance learning is the lack of motivation because they cannot have adequate direct interactions with their teachers as they do in a traditional classroom [33]. Students also think that there is more effective communication in didactic lectures and practical sessions than online, although there technically is no barrier to asking questions via online media [9]. This survey demonstrated that the majority of the responding schools reported a certain amount of communication with their students, which was positively related to the satisfaction with online teaching.
Compared to lectures online, the bigger challenge is how to implement HE practice online well, which is actually an issue that is prevalent in almost all disciplines of life sciences [[33], [34], [35]], although such online practice has been gradually accepted by teaching academics and students after several years of practical experience [36]. Beyond all doubt, virtual microscopy was found the most effective alternatives of performing practice when the coronavirus outbreak hit, approximately 35% of the responding medical schools still remained unchanged on their use of virtue microscopy in HE practice. This finding may mean that other approaches (e.g., watching photos which are static) were employed, that HE practice was suspended temporally, or that virtual microscopy was fully implemented at some institutes before the pandemic. Although various virtual microscopy platforms can be utilized to implement practices, we noticed that 21 responding schools reported having postponed their practices at the time the survey was performed. Some medical schools moved all the theoretical sessions ahead of practice, instead of normally one practice following one theoretical session in traditional HE class. That was their initial solution to the interrupted teaching by the unprecedented pandemic, a few schools adopted the “watch and wait” strategy at beginning. Nevertheless, most educators have responded to this teaching format enthusiastically and creatively. Some schools adjusted their strategy rapidly with the spread of the pandemic, which could mainly be dependent on the existing resources and previous experiences with online teaching. In uncertain time, different kinds of resourcefulness have been reported in ensuring the students to utilize learning resources available to study remotely, and educating the clinical trainees [37].
4.2. Active learning sessions, assessment, and teacher experience
A growing number of active learning activities, such as integrated, PBL, and TBL pilot curricula, have appeared in medical schools in China, and the HE course can be incorporated as a basic section by these teaching approaches [38,39]. Regarding whether active learning had been implemented before the pandemic, 82% of the medical schools answered yes. This number is higher than the number of respondents that we noted regarding PBL implementation in HE teaching two years ago [14], which is probably because of the quick development of active learning at medical schools in China during the past two years. Another possibility is that this approach benefits from the maturity of various platforms for online learning, which could be reflected in the fact that 86% of the medical schools which reported carrying out active learning were by means of platforms for online learning. It is worth noting that there is a significant reduction in PBL implementation during the pandemic compared to that prior to the pandemic [14], indicating the dysfunction or difficulty of PBL implementation online when compared with traditional face-to-face PBL settings. With regard to this issue, Dennis et al. considered that there was no significant difference between the synchronous online group and the traditional PBL tutorial group [40].
One important way to constantly improve active learning online is to set up an effective online assessment system in a real-world context, which is one of the difficult aspects of implementing online learning well [11,41]. Surprisingly, there is quite a high percentage (84%) of the responding medical schools that have implemented online assessments during the pandemic, in which some timely feedback might be included. Similar to the aforementioned findings regarding “the biggest difficulties encountered during implementing HE online teaching”, 55% of the respondents said it was “hard to grasp students' progress and learning outcomes”. Therefore, it is understandable that the number of online assessments increased during the pandemic since the teachers desired to learn about the students’ perceptions about online teaching from time to time.
Online learning has been somehow controversial topic among teaching academics in higher education under normal conditions [31,42], although there is no doubt that it is a growing trend. In the context of the pandemic outbreak and school closures, both teaching academics and students had little choice but to embrace this format. The first step of online education during the pandemic was how to shift to online teaching successfully for most educators. And the evaluation about whether the switch was gained on less tangible effects could be lagged. Learning outcome is a crucial indicator for judging the success or failure of online teaching. This survey showed that approximately 50% of the responding teachers estimated that their online sessions during the pandemic helped students achieve less than 80% of the intended learning outcomes. The reason for this outcome is probably related to the limitation of hardware, because 51% of the respondents mentioned that “the biggest difficulties encountered during implementing HE online teaching” was “unstable online teaching environments, platforms and tools”. Some medical schools introduced corresponding measures for implementing online teaching at the very beginning of the online teaching period (e.g., providing assistance for effectively delivering online instruction designs, engineering adequate support to students provided by teaching academics, establishing a contingency plan for unexpected incidents of online education platforms, etc.) [43]. However, this approach might not be good enough for coping with the situation in which millions of students nationwide are using online courses simultaneously.
Unexpectedly, 64% of the responding schools were either satisfied or very satisfied with the learning outcomes of online teaching during the pandemic. It was found that only 64 (82%) of the surveyed schools redesigned or adjusted the teaching content after shifting from “face-to-face” to fully online teaching. This ratio was fairly higher than that of gross anatomy, 51 (68%) of the responding schools, although the two disciplines reported the similar data on medical schools using synchronous live broadcasting (for gross anatomy, 35 surveyed schools; for HE, 31 surveyed schools; the data of gross anatomy comes from our another parallel survey). It can partly interpret the higher satisfaction with learning outcomes of HE when compared with the one in gross anatomy, except for the advantage of relatively perfect digital-resources of HE than gross anatomy. Synchronous live broadcasting ranked the most popular of online teaching, which implies that most of the online teaching might simply follow the “face-to-face” teaching strategies. This phenomena can be understood as strategies coping with emergency, but the teaching strategies and methods should be changed when switched to online teaching. We must re-consider and focus on post-pandemic online teaching from now on. Moreover, both the evaluation of teaching effectiveness and the satisfaction with learning outcomes in this survey were from internal evaluation since they were assessed by teaching academics themselves, so that the extrinsic evaluation indisputably is required.
This survey was carried out to principally grasp HE online teaching in China in response to the pandemic. These changes are conducive to collect useful experience regarding moving medical education from traditional face-to-face format to inevitable online learning format in response to the pandemic [35]. Teaching academics could compare the merits and demerits between online teaching and traditional face-to-face lectures in a classroom. These data could be of great importance in guiding HE online teaching even after the pandemic, including updating or improving teaching outcomes, working as the index of infrastructure construction, communicating with other teaching staff or teaching administrators among higher education educators, and helping other countries understand how the medical schools in China adapted their HE course in response to the Covid-19 outbreak. Much room is left for us to further consider about the development of online education in the future.
4.3. Limitations of this study
There are strengths but also several limitations of our study. The first limitation is whether there are any changes in HE teaching hours or the ratio between theoretical and practical sessions during the pandemics that were not covered in this questionnaire. Secondly, the conclusions from the survey might not be completely suitable for specific situations in some medical colleges since uneven economic development in China has certainly influenced the establishment of higher education in each province. For example, there are relatively better infrastructures for online learning in the medical schools located in coastal provinces compared with those in inland provinces, which probably indirectly affect students’ online learning outcomes to some extent. Thirdly, this report might exhibit some temporal or periodical characteristics in teaching online since the switch was really completed in such an abrupt and passive manner, furthermore because the survey was performed at the early to middle stage of the pandemic. Thus, the snapshot of the respondents might not well reflect the longitudinal educational scene.
5. Conclusion
Whether the country was ready or not, the unexpected Covid-19 pandemic pushed HE education to online courses including theoretical and practical sessions at medical schools in China, as in many other parts of the world. This survey was designed to understand the overall situation of the stopgap of virtual HE education nationwide over the first two months of online teaching. Mingling fears and hope are shown in the results of the nationwide survey on online HE education. A positive finding is that the majority of the medical schools in China had already gained a good infrastructure for online teaching and thus fostered a surge of teaching academics with experience in implementing online courses. As a consequence, when the pandemic emerged, these HE academics could deal with the unforeseen alterations to the existing teaching model rather than being caught off guard. A negative finding is that there are still many teaching academics who lack online teaching experience. Thus, there was an increased workload due to suddenly moving traditional didactic lectures to online courses, as well as the presence of insufficient infrastructures prior to the pandemic; therefore, some medical schools suspended their practical sessions during the pandemic temporally. Hopefully, both teaching academics and students, as well as administrators of higher education, can learn lessons from the global disease outbreak so that our higher education can ultimately make considerable progress when the outbreak is over.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank all of the survey respondents who helped to complete this survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tria.2021.100115.
Funding
This work is funded by “The Pedagogical Reform of High Education at Guangdong Province” (2019–60), “The research projects of pedagogical reform at Jinan University” (JG2019091) and the grant of China Association of Higher Education (2020JXYB08). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CRediT author statement
Xin Cheng: Conceptualization, methodology, writing.
Lap Ki Chan: Conceptualization, editing and reviewing.
Hongmei Cai: Software, statistical investigation.
Deshan Zhou: Supervision, validation.
Xuesong Yang: Conceptualization, original draft preparation, reviewing.
Ethical approval
The study was conducted with ethics approval from the Research Ethics Committee of Jinan University (No. MJNER202004001). The names of the responding medical schools were deidentified when analyzing the data.
Informed consent
Informed consent for publication was obtained for the images contained in the website screenshot.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Chowell G., Mizumoto K. The COVID-19 pandemic in the USA: what might we expect? Lancet. 2020;395:1093–1094. doi: 10.1016/S0140-6736(20)30743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saglietto A., D'Ascenzo F., Zoccai G.B., et al. COVID-19 in Europe: the Italian lesson. Lancet. 2020;395:1110–1111. doi: 10.1016/S0140-6736(20)30690-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu N., Zhang D., Wang W., et al. China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 6.Bedford J., Enria D., Giesecke J., et al. WHO strategic and technical advisory group for infectious hazards. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw S.C. Hopelessness, helplessness and resilience: the importance of safeguarding our trainees' mental wellbeing during the COVID-19 pandemic. Nurse Educ. Pract. 2020;44:102780. doi: 10.1016/j.nepr.2020.102780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stokes D.C. Senior medical students in the COVID‐19 response: an opportunity to be proactive. Acad. Emerg. Med. 2020;27:343–345. doi: 10.1111/acem.13972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viner R.M., Russell S.J., Croker H., et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc. Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ebrahim S.H., Ahmed Q.A., Gozzer E., et al. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- 11.Evans D.J., Bay B.H., Wilson T.D., et al. Going virtual to support anatomy education: a STOPGAP in the Midst of the Covid‐19 pandemic. Anat. Sci. Educ. 2020;13:279–283. doi: 10.1002/ase.1963. [DOI] [PubMed] [Google Scholar]
- 12.Seliger W.G. Improved teaching of microanatomy. J. Dent. Educ. 1971;35:254–255. [PubMed] [Google Scholar]
- 13.Seliger W.G., Hillman J.R. An efficient technique for teaching microanatomy. J. Dent. Educ. 1975;39:683–686. 1971. [PubMed] [Google Scholar]
- 14.Cheng X., Chan L.K., Li H., et al. Histology and embryology education in China: the current situation and changes over the past 20 years. Anat. Sci. Educ. 2020;13(6):759–768. doi: 10.1002/ase.1956. [DOI] [PubMed] [Google Scholar]
- 15.Krenacs T., Zsakovics I., Micsik T., Fonyad L., Varga S.V., Ficsor L., Kiszler G., Molnar B. In: first ed. Méndez -Vilas A., Díaz J., editors. Vol. 2. Formatex; Badajoz, Spain: 2010. Digital microscopy – the upcoming revolution in histopathology teaching, diagnostics, research and quality assurance; pp. 965–977. (Microscopy: Science, Technology, Applications and Education). [Google Scholar]
- 16.Campbell G., Demetriou L.A., Arnett T.R. Virtual histology in the classroom and beyond. Med. Educ. 2010;44:1124–1125. doi: 10.1111/j.1365-2923.2010.03828.x. [DOI] [PubMed] [Google Scholar]
- 17.MacMillan F.M. Virtual versus light microscopy for teaching histology. J. Vet. Med. Educ. 2017;44:207. doi: 10.3138/jvme.1116-169. [DOI] [PubMed] [Google Scholar]
- 18.Paulsen F.P., Eichhorn M., Bräuer L. Virtual microscopy—the future of teaching histology in the medical curriculum? Ann. Anat. 2010;192:378–382. doi: 10.1016/j.aanat.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 19.Lee B., Hsieh S., Chang Y., et al. Web-based virtual microscopy platform for improving academic performance in histology and pathology laboratory courses: a pilot study. Anat. Sci. Educ. 2020;13(6):743–758. doi: 10.1002/ase.1940. [DOI] [PubMed] [Google Scholar]
- 20.Gan C., Wang W. Uses and gratifications of social media: a comparison of microblog and WeChat. J. Syst. Inf. Technol. 2015;17:351–363. doi: 10.1108/JSIT-06-2015-0052. [DOI] [Google Scholar]
- 21.Wang Z., Yu Q. Privacy trust crisis of personal data in China in the era of big data: the survey and countermeasures. Comput. Law Secur. Rep. 2015;31:782–792. [Google Scholar]
- 22.Sojump. Sojump.Com. Online Questionnaire, Examinations and Voting Platform. Shanghai Information Technology Co.; Shanghai, China: 2019. https://www.wjx.cn/jq/76388431.aspx URL: accessed. [Google Scholar]
- 23.Ministry M.O.E. Double First-Class Universities. Ministry of Education of the People’s Republic of China; Beijing, China. 2019: 2019. Of Education of the People's Republic of China. URL: http://www.moe.gov.cn/s78/A22/A22_ztzl/ztzl_tjsylpt/sylpt_jsdt/201903/t20190329_376024.html. accessed. [Google Scholar]
- 24.Moszkowicz D., Duboc H., Dubertret C., et al. Daily medical education for confined students during COVID‐19 pandemic: a simple videoconference solution. Clin. Anat. 2020;33(6):927–928. doi: 10.1002/ca.23601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bloodgood R.A., Ogilvie R.W. Trends in histology laboratory teaching in United States medical schools. Anat. Rec. 2006;289B:169–175. doi: 10.1002/ar.b.20111. [DOI] [PubMed] [Google Scholar]
- 26.Brisbourne M.A., Chin S.S., Melnyk E., et al. Using web-based animations to teach histology. Anat. Rec. 2002;269:11–19. doi: 10.1002/ar.10054. [DOI] [PubMed] [Google Scholar]
- 27.Szeto E. Examining issues of e-learning practices in Chinese higher education: a comparative study of Mainland China, Hong Kong and Taiwan. Int. J. E-Learn. 2013;12:383–402. [Google Scholar]
- 28.Carpenter R., Theeke L., Smothers A. Enhancing course grades and evaluations using distance education technologies. Nurse Educat. 2013;38:114–117. doi: 10.1097/NNE.0b013e31828dc2d7. [DOI] [PubMed] [Google Scholar]
- 29.Wallace R.M. Online learning in higher education: a review of research on interactions among teachers and students. Educ. Commun. Inf. 2003;3:241–280. doi: 10.1080/14636310303143. [DOI] [Google Scholar]
- 30.Dixson M.D. Creating effective student engagement in online courses: what do students find engaging? J. Scholarsh. Teach. Learn. 2010;10:1–13. [Google Scholar]
- 31.Attardi S.M., Choi S., Barnett J., et al. Mixed methods student evaluation of an online systemic human anatomy course with laboratory. Anat. Sci. Educ. 2016;9:272–285. doi: 10.1002/ase.1584. [DOI] [PubMed] [Google Scholar]
- 32.Zheng Y. Unprecedented pandemic, unprecedented shift, and unprecedented opportunity. Hum. Behav. Emerg. Tech. 2020;2:110–112. doi: 10.1002/hbe2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pather N., Blyth P., Chapman J.A., et al. Forced disruption of anatomy education in Australia and New Zealand: an acute response to the Covid‐19 pandemic. Anat. Sci. Educ. 2020;13:284–300. doi: 10.1002/ase.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doubleday E.G., O'Loughlin V.D., Doubleday A.F. The virtual anatomy laboratory: usability testing to improve an online learning resource for anatomy education. Anat. Sci. Educ. 2011;4:318–326. doi: 10.1002/ase.252. [DOI] [PubMed] [Google Scholar]
- 35.Longhurst G.J., Stone D.M., Dulohery K., et al. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in Response to the COIVD‐19 pandemic. Anat. Sci. Educ. 2020;13:301–311. doi: 10.1002/ase.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Scoville S.A., Buskirk T.D. Traditional and virtual microscopy compared experimentally in a classroom setting. Clin. Anat. 2007;20:565–570. doi: 10.1002/ca.20440. [DOI] [PubMed] [Google Scholar]
- 37.Kim R.H., Brinster N.K., Meehan S.A. Dermatopathology education during the COVID-19 pandemic: virtual simulation of the multi-headed microscope. J. Am. Acad. Dermatol. 2020;83(3):e243–e244. doi: 10.1016/j.jaad.2020.05.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Y., Zhou L., Liu X., et al. The effectiveness of the problem-based learning teaching model for use in introductory Chinese undergraduate medical courses: a systematic review and meta-analysis. PloS One. 2015;10(3) doi: 10.1371/journal.pone.0120884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu X., Cheng X., Li K., et al. Integration of histology lectures and practical teaching integration of histology lectures and practical teaching in China. Int. J. High. Educ. 2016;5(4):157–164. doi: 10.5430/ijhe.v5n4p157. [DOI] [Google Scholar]
- 40.Dennis J.K. Problem-based learning in online vs. face-to-face environments. Educ. Health. 2003;16(2):198–209. doi: 10.1080/1357628031000116907. [DOI] [PubMed] [Google Scholar]
- 41.Cohen J., Kupferschmidt K. Strategies shift as coronavirus pandemic looms. Science. 2020;367:962–963. doi: 10.1126/science.367.6481.962. [DOI] [PubMed] [Google Scholar]
- 42.Samarawickrema G., Stacey E. Adopting web‐based learning and teaching: a case study in higher education. Dist. Educ. 2007;28:313–333. doi: 10.1080/01587910701611344. [DOI] [Google Scholar]
- 43.Bao W. COVID-19 and online teaching in higher education: a case study of Peking University. Hum. Behav. Emerg. Technol. 2020;2:113–115. doi: 10.1002/hbe2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.