This cross-sectional study examines the use of work relative value unit to calculate dermatologist productivity and compensation according to the demographic characteristics of patients.
Key Points
Question
Are patient race, sex, and age associated with the work relative value units (wRVUs) generated per outpatient dermatology encounter?
Findings
In this cross-sectional study of 66 463 outpatient dermatology encounters among 30 036 patients, visits with patients who were White, older, and male generated more wRVUs than visits with other demographic groups. Destruction of premalignant lesions and biopsies accounted for the preponderance of the observed differences by race, sex, and age.
Meaning
Results of this study suggest that race, sex, and age differences in wRVUs for outpatient dermatology encounters may incentivize dermatologists to care for patients who are most likely to develop skin cancers and thereby perpetuate disparities in access to dermatologic care.
Abstract
Importance
Clinical productivity measures may be factors in financial incentives for providing care to specific patient populations and thus may perpetuate inequitable health care.
Objective
To identify the association of patient race, age, and sex with work relative value units (wRVUs) generated by outpatient dermatology encounters.
Design, Setting, and Participants
This cross-sectional study obtained demographic and billing data for outpatient dermatology encounters (ie, an encounter performed within a department of dermatology) from September 1, 2016, to March 31, 2020, at the Emory Clinic, an academic dermatologic practice in Atlanta, Georgia. Participants included adults aged 18 years or older with available age, race, and sex data in the electronic health record system.
Main Outcomes and Measures
The primary outcome was wRVUs generated per encounter.
Results
A total of 66 463 encounters among 30 036 unique patients were included. Patients had a mean (SD) age of 55.9 (18.5) years and were predominantly White (46 575 [70.1%]) and female (39 598 [59.6%]) individuals. In the general dermatologic practice, the mean (SD) wRVUs per encounter was 1.40 (0.71). In adjusted analysis, Black, Asian, and other races (eg, American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races); female sex; and younger age were associated with fewer wRVUs per outpatient dermatology encounter. Compared with general dermatologic visits with White patients, visits with Black patients generated 0.27 (95% CI, 0.25-0.28) fewer wRVUs per encounter, visits with Asian patients generated 0.22 (95% CI, 0.20-0.25) fewer wRVUs per encounter, and visits with patients of other race generated 0.19 (95% CI, 0.14-0.24) fewer wRVUs per encounter. Female sex was also associated with 0.11 (95% CI, 0.10-0.12) fewer wRVUs per encounter, and wRVUs per encounter increased by 0.006 (95% CI, 0.006-0.006) with each 1-year increase in age. In the general dermatologic practice excluding Mohs surgeons, destruction of premalignant lesions and biopsies were mediators for the observed differences in race (56.2% [95% CI, 53.1%-59.3%] for Black race, 53.2% [95% CI, 45.6%-63.8%] for Asian race, and 53.6% [95% CI, 40.4%-77.4%] for other races), age (65.6%; 95% CI, 60.5%-71.4%), and sex (82.3%; 95% CI, 72.7%-93.1%). In a data set including encounters with Mohs surgeons, the race, age, and sex differences in wRVUs per encounter were greater than in the general dermatologic data set. Mohs surgery for basal cell and squamous cell carcinomas was a mediator for the observed differences in race (46.0% [95% CI, 42.6%-49.4%] for Black race, 41.9% [95% CI, 35.5%-49.2%] for Asian race, and 34.6% [95% CI, 13.8%-51.5%] for other races), age (49.2%; 95% CI, 44.9%-53.7%), and sex (47.9%; 95% CI, 42.0%-54.6%).
Conclusions and Relevance
This cross-sectional study found that dermatology encounters with racial minority groups, women, and younger patients generated fewer wRVUs than encounters with older White male patients. This finding suggests that physician compensation based on wRVUs may encourage the provision of services that exacerbate disparities in access to dermatologic care.
Introduction
The American health care system is burdened with inequities that have a role in increased health care costs, decreased quality of life, and poor outcomes among economically disadvantaged groups and racial minority groups.1,2 In dermatology, racial minority groups have unequal access to care, and clinicians receive less training in diagnosis and management of dermatologic disorders that primarily affect these patient populations.3,4 In the largest dermatologic registry of patients in the United States, racial minority groups appear to be underrepresented, with Black patients composing less than 5% of the database population.5 Race is also a factor in treatment selection: Black patients with acne are less likely to receive systemic therapies than White patients.6 The Institute of Medicine’s landmark report on disparities in health care access specifically noted the need to “limit provider incentives that may promote disparities.”2(p17) To mitigate such disparities, numerous policy changes have been proposed, but few of these policies have considered structural inequities in reimbursement.7,8
The modern American medical payment system began with the Omnibus Budget Reconciliation Act of 1989, which established the national Medicare physician fee schedule. This national fee schedule was a departure from locally and regionally determined Medicare fees and established a new method based on survey research.9 The American Medical Association formed the Specialty Society Relative Value Scale Update Committee (RUC), which advises the Centers for Medicare & Medicaid Services (CMS) on the relative weights used to calculate physician payments, measured in relative value units (RVUs). Each RVU represents physician time and effort or work for each service. Each service is identified using a Current Procedural Terminology (CPT) code.
The CMS accepts most recommendations made by the RUC. The impact of the RUC and CMS extends well beyond Medicare. The relative weights used by Medicare may alter private insurer fee schedules.10 Furthermore, RVUs are used by hospitals as indicators of productivity, to compare the revenue generated by physicians.11 Thus, the RUC has indirect implications for the financial incentives provided for specific medical services across the health care sector. Higher RVUs for CPT codes that are associated with differential health care use by race and sex could inadvertently incentivize, or at least reinforce, structural inequities.
Other research has shown how patient characteristics may affect the determination of work values. Mean total RVUs for female-only services were substantially lower than male-only urologic services (139.5 vs 207.1).12 It remains unknown whether patient race, sex, and age are associated with RVUs or net payments in outpatient dermatologic visits. The primary objective of the present study was to identify the association of patient race, age, and sex with work RVUs (wRVUs) generated in outpatient dermatology encounters (ie, encounter performed within a department of dermatology).
Methods
The Emory University Institutional Review Board approved this study. Participant consent was waived by the Emory University Institutional Review Board because the research involved no more than minimal risk, the research could not be practicably carried out without the requested waiver, and the waiver would not adversely affect the rights and welfare of the participants. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.13
Study Population and Design
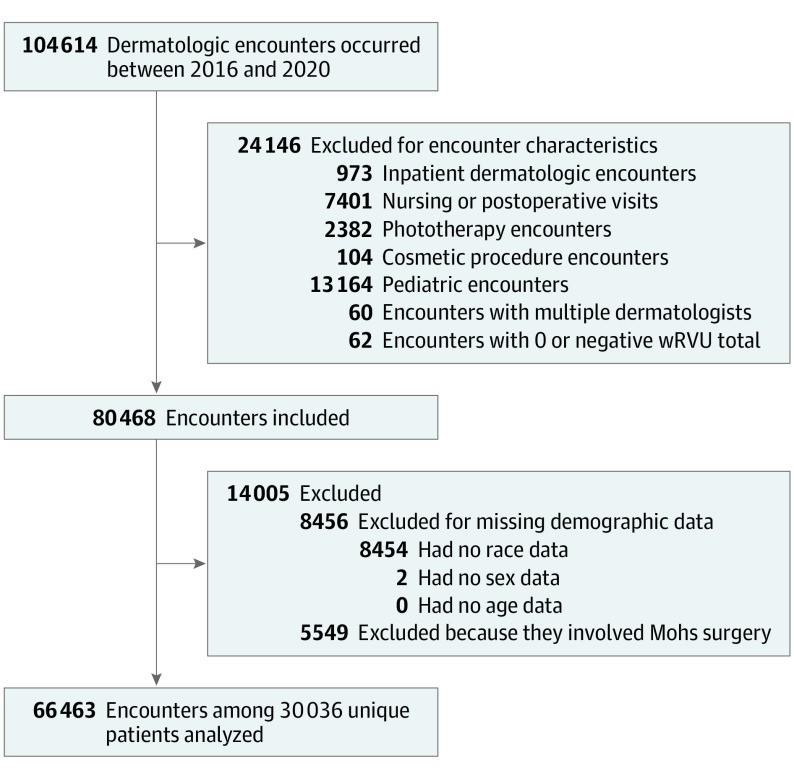
In this retrospective cross-sectional study, we used an electronic health record system to examine demographic and billing data for all adult outpatient dermatology encounters from September 1, 2016, to March 31, 2020, at the Emory Clinic, an academic dermatologic practice in Atlanta, Georgia. Exclusion criteria were inpatient visits; nursing or postoperative encounters; phototherapy visits; cosmetic procedures; patients younger than 18 years; encounters with multiple clinicians; a 0 or negative wRVU total; and missing age, race, or sex data. To study the incentives for general dermatologists without an affiliated Mohs practice, we excluded encounters with Mohs surgeons from the primary data set. To gain insight into the incentives for dermatologic clinics with an embedded Mohs practice, we analyzed a data set that included Mohs surgeon encounters.
The primary outcome was wRVUs generated per encounter. Race was categorized as White, Black, Asian, or other (eg, American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races). Insurance type was categorized as Medicaid, Medicare, commercial, self-pay, or other. Diagnoses of skin cancers were identified according to the International Statistical Classification of Diseases, Tenth Revision, Clinical Modification codes, and procedures were identified with CPT codes.
Statistical Analysis
Crude association of encounter wRVUs with race, age, sex, and insurance type was assessed using bivariable normal linear regression. Multivariable normal linear regression was used to ascertain the adjusted associations between wRVUs and exposures, including age, sex, race, and insurance type. Mediation analysis by the difference method was applied to identify the association of skin cancer diagnoses and dermatologic surgical procedures with the observed age, race, and sex disparities in wRVUs. We performed bootstrapping for 200 cycles with replacement to estimate 95% CIs.14 Because the research question pertains to the financial incentives for the way dermatologists allocated time to care for different patient groups, we conducted the primary analyses at the encounter level (fixed effects) rather than the patient level.
The P values for continuous variables were calculated using 1-way analysis of variance, and P values for categorical variables were calculated by χ2 test of independence or Fisher exact test. P ≤ .05 was considered statistically significant. All analyses were performed using SAS, version 9.4 (SAS Institute Inc), and Python, version 3.6.8 (Python Software Foundation).
Results
General Dermatologic Practice
In the general outpatient dermatologic practice (excluding encounters with Mohs surgeons), 66 463 encounters among 30 036 unique patients were included (Figure). Patients had a mean (SD) age of 55.9 (18.5) years and were predominantly White (46 575 [70.1%]) and female (39 598 [59.6%]) individuals (Table 1). Age, insurance type, skin cancer diagnosis, and procedures varied significantly by race.
Figure. Patient Eligibility Flowsheet.
wRVU indicates work relative value unit.
Table 1. Patient and Visit Characteristics for Outpatient Encounters in a General Dermatologic Practice, Excluding Mohs Surgeonsa.
| Characteristic | No. (%) | P valuec | ||||
|---|---|---|---|---|---|---|
| Total | White | Black | Asian | Other racesb | ||
| Encounters | ||||||
| All | 66 463 (100) | 46 575 (70.1) | 16 273 (24.5) | 2831 (4.3) | 784 (1.2) | NA |
| Female patients | 39 598 (59.6) | 25 843 (65.3) | 11 642 (29.4) | 1635 (4.1) | 478 (1.2) | <.001 |
| Male patients | 26 865 (40.4) | 20 732 (77.2) | 4631 (17.2) | 1196 (4.5) | 306 (1.1) | <.001 |
| Age, mean (SD), y | 55.9 (18.5) | 58.0 (18.4) | 52.5 (17.6) | 44.4 (18.2) | 44.1 (16.9) | <.001 |
| Per encounter, mean (SD) | ||||||
| wRVUs | 1.40 (0.71) | 1.50 (0.74) | 1.18 (0.55) | 1.19 (0.60) | 1.22 (0.53) | <.001 |
| Net payments, $ | 133.39 (112.74) | 145.57 (119.81) | 103.02 (86.53) | 111.46 (92.78) | 119.24 (92.11) | <.001 |
| Insurance typed | ||||||
| Commercial | 51 490 (77.5) | 37 595 (80.7) | 10 745 (66.0) | 2479 (87.6) | 671 (85.6) | <.001 |
| Medicare | 22 942 (34.5) | 16 702 (35.9) | 5751 (35.3) | 391 (13.8) | 98 (12.5) | <.001 |
| Medicaid | 1494 (2.3) | 528 (1.1) | 887 (5.5) | 44 (1.6) | 35 (1.2) | <.001 |
| Self-pay | 697 (1.1) | 442 (1.0) | 196 (1.2) | 40 (1.4) | 19 (2.4) | <.001 |
| Othere | 1210 (1.8) | 826 (1.8) | 328 (2.0) | 46 (1.6) | 10 (1.3) | .11 |
| Encounter diagnoses | ||||||
| AK | 10 169 (15.3) | 10 102 (21.7) | 29 (0.2) | 8 (0.3) | 30 (3.8) | <.001 |
| Neoplasm of uncertain behavior | 10 638 (16.0) | 9460 (20.3) | 907 (5.6) | 207 (7.3) | 64 (8.2) | <.001 |
| BCC | 413 (0.6) | 403 (0.9) | 8 (0.1) | 1 (0.0) | 1 (0.1) | <.001 |
| SCC | 243 (0.4) | 230 (0.5) | 12 (0.1) | 1 (0.0) | 0 | <.001 |
| SCC in situ | 111 (0.2) | 101 (0.2) | 9 (0.1) | 1 (0.0) | 0) | <.001 |
| Melanoma | 210 (0.3) | 194 (0.4) | 10 (0.1) | 6 (0.2) | 0 | <.001 |
| Other malignant neoplasm | 51 (0.1) | 33 (0.1) | 18 (0.1) | 0 | 0 | .14 |
| Any skin cancerf | 902 (1.4) | 845 (1.8) | 48 (0.3) | 8 (0.3) | 1 (0.1) | <.001 |
| Procedures rendered | ||||||
| Premalignant lesion destruction | 8092 (12.2) | 8044 (17.3) | 23 (0.1) | 7 (0.3) | 18 (2.3) | <.001 |
| Biopsy | 10 935 (16.5) | 9335 (20.0) | 1267 (7.8) | 260 (9.2) | 73 (9.3) | <.001 |
| Malignant lesion destruction | 243 (0.4) | 238 (0.5) | 4 (0.0) | 1 (0.0) | 0 | <.001 |
| Malignant excision | 228 (0.3) | 223 (0.5) | 4 (0.0) | 0 | 1 (0.1) | <.001 |
| Benign excision | 279 (0.4) | 189 (0.4) | 82 (0.5) | 8 (0.3) | 0 | .06 |
Abbreviations: AK, actinic keratosis; BCC, basal cell carcinoma; NA, not applicable; wRVUs, work relative value units; SCC, squamous cell carcinoma.
All characteristics in this table were analyzed at the encounter level and not at the patient level.
Other races included American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races.
P values for continuous variables were calculated by 1-way analysis of variance. P values for categorical variables were calculated by χ2 test of independence or Fisher exact test.
Totals for insurance type exceeded the total number of encounters in the cohort because more than 1 insurance type was billed in some encounters.
Other insurance types were predominantly government-sponsored insurance programs.
Any skin cancer included BCC, SCC, melanoma, and other malignant neoplasms of the skin.
The mean (SD) wRVUs per encounter was 1.40 (0.71) for this general dermatologic practice. In adjusted analysis, increasing age, male sex, and White race were independently associated with higher wRVUs (Table 2). Dermatology encounters with Black patients were associated with 0.27 (95% CI, 0.25-0.28) fewer wRVUs per encounter; encounters with Asian patients were associated with 0.22 (95% CI, 0.20-0.25) fewer wRVUs; and encounters with patients of other races were associated with 0.19 (95% CI, 0.14-0.24) fewer wRVUs. Encounters with female patients were associated with 0.11 (95% CI, 0.10-0.12) fewer wRVUs per encounter compared with male patients. For every 1-year increase in age, encounters generated 0.006 more wRVUs (95% CI, 0.006-0.006) (Table 2). Race, sex, and age differences were also observed in adjusted models with the outcome of net payments. The mean (SD) net payment was $133.39 ($112.74). Encounters with Black patients had a payment of $28.25 less (95% CI, $26.26-$30.24) compared with encounters with White patients, and encounters with women had a payment of $9.76 less (95% CI, $8.07-$11.45) compared with encounters with men (eTable 1 in the Supplement).
Table 2. Factors Associated With Work Relative Value Units of Outpatient Encounters in a General Dermatologic Practice, Excluding Mohs Surgeons.
| Variable | wRVUs per encounter, mean (SD) | β (95% CI)a | |
|---|---|---|---|
| Crude | Adjusted | ||
| Overall | 1.40 (0.71) | NA | NA |
| Age per y | NA | 0.008 (0.008 to 0.008) | 0.006 (0.006 to 0.006) |
| Sex | |||
| Male | 1.51 (0.79) | 1 [Reference] | 1 [Reference] |
| Female | 1.33 (0.64) | −0.17 (−0.16 to −0.18) | −0.11 (−0.10 to −0.12) |
| Race | |||
| White | 1.50 (0.74) | 1 [Reference] | 1 [Reference] |
| Black | 1.18 (0.55) | −0.32 (−0.31 to −0.34) | −0.27 (−0.25 to −0.28) |
| Asian | 1.19 (0.60) | −0.31 (−0.29 to −0.34) | −0.22 (−0.20 to −0.25) |
| Otherb | 1.22 (0.53) | −0.28 (−0.24 to −0.33) | −0.19 (−0.14 to −0.24) |
| Insurance typec | |||
| Commercial | 1.40 (0.69) | −0.04 (−0.03 to −0.05) | 0.08 (0.06 to 0.09) |
| Medicare | 1.53 (0.78) | 0.20 (0.19 to 0.21) | 0.06 (0.05 to 0.08) |
| Medicaid | 1.37 (0.76) | −0.03 (−0.07 to 0.01) | 0.17 (0.14 to 0.21) |
| Self-pay | 1.44 (1.20) | 0.04 (−0.01 to 0.09) | 0.17 (0.11 to 0.22) |
| Otherd | 1.33 (0.62) | −0.07 (−0.03 to −0.11) | 0.02 (−0.02 to 0.06) |
Abbreviations: NA, not applicable; wRVUs, work relative value units.
β estimates were the change in wRVUs billed per encounter by patient characteristic.
Other races included American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races.
Individual patients may have multiple insurance coverage. Therefore, each insurance type was analyzed as its own dichotomous variable (ie, present or absent). For example, in the crude analysis, the encounters associated with commercial insurance had 0.038 (95% CI, 0.025-0.051) fewer wRVUs than the encounters without commercial insurance.
Other insurance types were predominantly government-sponsored insurance programs.
In mediation analysis of the general dermatologic practice, destruction of premalignant lesions and biopsies accounted for 82.3% (95% CI, 72.7%-93.1%) of sex differences in wRVUs; 65.6% (95% CI, 60.5%-71.4%) of age differences; and more than 50% of racial differences (56.2% [95% CI, 53.1%-59.3%] for Black race, 53.2% [95% CI, 45.6%-63.8%] for Asian race, and 53.6% [95% CI, 40.4%-77.4%] for other race) (eTable 2 in the Supplement).
Sensitivity analyses that used multiple imputation for the 8036 non-Mohs surgery encounters that were missing race data were performed and did not alter the study findings (eTables 3 and 4 in the Supplement). A sensitivity analysis that used a generalized estimate equation model was also performed to examine wRVU clustering at the patient level and did not alter study findings (eTable 5 in the Supplement).
Combined Dermatologic Practice
In the combined outpatient dermatologic practice (including Mohs surgeons and general dermatologists), 72 012 encounters among 30 427 unique patients were analyzed (Table 3).
Table 3. Patient and Visit Characteristics for Outpatient Encounters in a Combined Dermatologic Practice, Including Mohs Surgeonsa.
| Characteristic | No. (%) | P valuec | ||||
|---|---|---|---|---|---|---|
| Total | White | Black | Asian | Other racesb | ||
| Encounters | ||||||
| All | 72 012 | 51 407 (71.4) | 16 867 (23.4) | 2917 (4.1) | 821 (1.1) | NA |
| Female patients | 41 965 (58.3) | 27 789 (66.2) | 11 997 (28.6) | 1684 (4.0) | 495 (1.2) | <.001 |
| Male patients | 30 047 (41.7) | 23 618 (78.6) | 4870 (16.2) | 1233 (4.1) | 326 (1.1) | <.001 |
| Age, mean (SD), y | 56.6 (18.5) | 58.9 (18.3) | 52.5 (17.6) | 44.6 (18.3) | 44.7 (17.2) | <.001 |
| Per encounter, mean (SD) | ||||||
| wRVUs | 1.89 (2.63) | 2.13 (3.00) | 1.27 (1.06) | 1.28 (1.19) | 1.41 (1.63) | <.001 |
| Net payments, $ | 182.11 (294.85) | 208.69 (331.52) | 113.79 (154.49) | 119.80 (128.88) | 142.43 (197.64) | <.001 |
| Insurance typed | ||||||
| Commercial | 55 616 (77.2) | 41 224 (80.2) | 11 139 (66.0) | 2550 (27.4) | 703 (85.6) | <.001 |
| Medicare | 25 755 (35.8) | 19 274 (37.5) | 5966 (35.4) | 409 (14.0) | 106 (12.9) | <.001 |
| Medicaid | 1673 (2.3) | 658 (1.3) | 931 (5.5) | 47 (1.6) | 37 (4.5) | <.001 |
| Self-pay | 738 (1.0) | 467 (0.9) | 210 (1.3) | 41 (1.4) | 20 (2.4) | <.001 |
| Othere | 1319 (1.8) | 911 (1.8) | 349 (2.1) | 49 (1.7) | 10 (1.2) | .04 |
| Encounter diagnoses | ||||||
| AK | 10 731 (14.9) | 10 658 (20.7) | 30 (0.2) | 9 (0.3) | 34 (4.1) | <.001 |
| Neoplasm of uncertain behavior | 11 605 (16.1) | 10 228 (19.9) | 1076 (6.4) | 225 (7.7) | 76 (9.3) | <.001 |
| BCC | 2276 (3.2) | 2233 (4.3) | 28 (0.2) | 7 (0.2) | 8 (1.0) | <.001 |
| SCC | 1475 (2.1) | 1427 (2.8) | 37 (0.2) | 4 (0.1) | 7 (0.9) | <.001 |
| SCC in situ | 424 (0.6) | 403 (0.8) | 16 (0.1) | 4 (0.1) | 1 (0.1) | <.001 |
| Melanoma | 336 (0.5) | 317 (0.6) | 11 (0.1) | 7 (0.2) | 1 (0.1) | <.001 |
| Other malignant neoplasm | 105 (0.2) | 72 (0.1) | 31 (0.2) | 2 (0.1) | 0 | .24 |
| Any skin cancerf | 4050 (5.6) | 3908 (7.6) | 107 (0.6) | 20 (0.7) | 15 (1.8) | <.001 |
| Procedures rendered | ||||||
| Premalignant lesion destruction | 8366 (11.6) | 8317 (16.2) | 23 (0.1) | 7 (0.2) | 19 (2.3) | <.001 |
| Biopsy | 11 513 (16.0) | 9832 (19.1) | 1332 (7.9) | 266 (9.1) | 83 (10.1) | <.001 |
| Malignant lesion destruction | 506 (0.70) | 497 (1.0) | 6 (0.0) | 2 (0.1) | 1 (0.1) | <.001 |
| Malignant excision | 1031 (1.4) | 1012 (2.0) | 12 (0.1) | 2 (0.1) | 5 (0.6) | <.001 |
| Benign excision | 1292 (1.8) | 873 (1.7) | 369 (2.2) | 44 (1.5) | 6 (0.7) | <.001 |
| Mohs surgery | 2365 (3.3) | 2296 (4.5) | 48 (0.3) | 12 (0.4) | 9 (1.1) | <.001 |
Abbreviations: AK, actinic keratosis; BCC, basal cell carcinoma; NA, not applicable; SCC, squamous cell carcinoma; wRVUs, work relative value units.
All characteristics in this table were analyzed at the encounter level and not at the patient level.
Other races included American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races.
P values for continuous variables were calculated by 1-way analysis of variance. P values for categorical variables were calculated by χ2 test of independence or Fisher exact test.
Totals for insurance type exceeded the total number of encounters in the cohort because more than 1 insurance type was billed in some encounters.
Other insurance types were predominantly government-sponsored insurance programs.
Any skin cancer included BCC, SCC, melanoma, and other malignant neoplasms of the skin.
The mean (SD) wRVUs per encounter was 1.89 (2.63). In adjusted analysis, increasing age, male sex, and White race were independently associated with higher wRVUs. The magnitudes of the age, sex, and race differences in wRVUs per encounter were greater than in the data set that excluded the Mohs practice (Table 4). In mediation analysis for the combined practice data set, Mohs surgery for basal cell carcinomas and squamous cell carcinomas accounted for 47.9% (95% CI, 42.0%-54.6%) of sex differences, 49.2% (95% CI, 44.9%-53.7%) of age differences, and similar proportions of racial differences (46.0% [95% CI, 42.6%-49.4%] for Black race, 41.9% [95% CI, 35.5%-49.2%] for Asian race, and 34.6% [95% CI, 13.8%-51.5%] for other races).
Table 4. Factors Associated With Work Relative Value Units of Outpatient Encounters in a Combined Dermatologic Practice, Including Mohs Surgeons .
| Variable | wRVUs per encounter, mean (SD) | β (95% CI)a | |
|---|---|---|---|
| Crude | Adjusted | ||
| Overall | 1.89 (2.63) | NA | NA |
| Age per y | NA | 0.027 (0.026 to 0.028) | 0.019 (0.017 to 0.020) |
| Sex | |||
| Male | 2.25 (3.29) | 1 [Reference] | 1 [Reference] |
| Female | 1.63 (1.99) | −0.63 (−0.59 to −0.66) | −0.43 (−0.39 to −0.47) |
| Race | |||
| White | 2.13 (3.00) | 1 [Reference] | 1 [Reference] |
| Black | 1.27 (1.06) | −0.86 (−0.82 to −0.91) | −0.65 (−0.61 to −0.70) |
| Asian | 1.28 (1.19) | −0.85 (−0.75 to −0.95) | −0.51 (−0.41 to −0.61) |
| Otherb | 1.41 (1.63) | −0.73 (−0.55 to −0.91) | −0.39 (−0.22 to −0.57) |
| Insurance typec | |||
| Commercial | 1.85 (2.50) | −0.19 (−0.15 to −0.24) | 0.32 (0.26 to 0.38) |
| Medicare | 2.37 (3.52) | 0.75 (0.71 to 0.79) | 0.37 (0.30 to 0.43) |
| Medicaid | 2.10 (3.16) | 0.22 (0.09 to 0.35) | 0.81 (0.68 to 0.94) |
| Self-pay | 1.72 (2.45) | −0.18 (−0.37 to 0.02) | 0.33 (0.14 to 0.53) |
| Otherd | 1.75 (2.20) | −0.14 (−0.00 to −0.29) | 0.22 (0.07 to 0.36) |
Abbreviations: NA, not applicable; wRVUs, work relative value units.
β estimates were the change in wRVUs billed per encounter by patient characteristic.
Other races included American Indian or Native American, Native Hawaiian or Other Pacific Islander, and multiple races.
Individual patients may have multiple insurance coverage. Therefore, each insurance type was analyzed as its own dichotomous variable (ie, present or absent). For example, in the crude analysis, the encounters associated with commercial insurance had 0.038 (95% CI, 0.025-0.051) fewer wRVUs than the encounters without commercial insurance.
Other insurance types were predominantly government-sponsored insurance programs.
Discussion
This single-institution cross-sectional study demonstrated that outpatient dermatologic visits with patients who were younger, female, and from racial minority groups generated significantly fewer wRVUs compared with visits with older White men. In the analysis of a general dermatologic practice that excluded encounters with Mohs surgeons, these wRVU differences were traced to the destruction of premalignant lesions and biopsies. The observed wRVU differences highlight the relative undervaluation of care for inflammatory skin diseases that impact the quality of life and are disproportionately prevalent among underserved populations.15,16
The magnitude of the differences in wRVUs generated by patient race, sex, and age was even greater in the combined practice that included general dermatologists and Mohs surgeons. After including the embedded Mohs practice, we found that Mohs surgery for basal cell carcinomas and squamous cell carcinomas mediated the race, sex, and age potential disparities.
Relative value units were initially developed for a specific purpose within Medicare and later were adopted by private insurers. Today, fee-for-service practices, the US Department of Veterans Affairs health care system, and many academic institutions use RVUs internally as benchmarks when assessing an individual clinician’s productivity and establishing compensation. Such financial incentives may have implications for physician behavior and for health care access and outcomes.17 For example, when an academic practice transitioned to RVU-based compensation, 90% of faculty increased their clinical productivity.18
From the perspective of a general dermatologic practice, a system with large differences in wRVUs and net payments according to patient race, sex, and age creates financial incentives to cater to patients who are most likely to develop nonmelanoma skin cancer (NMSC). Physicians may gravitate toward providing those services with higher RVUs. Otherwise, dermatologists will need to see many more patients to appear similarly productive. In a clinic with an embedded Mohs surgery practice, the financial incentive for providing services to those who are most likely to develop NMSC is even higher. Financial incentives for providing services for dermatologic conditions that primarily affect older White men may inadvertently change the dermatologist’s choice of community in which to practice, reducing access to care for some groups and perpetuating structural racism.19
Limitations
This study has some limitations. First, from the perspective of a general dermatologist with a set number of daily appointments, this study demonstrated a financial incentive to care for populations at highest risk for developing NMSC. This financial incentive may play a role in dermatologists’ selection of practice location and decrease access to care for individuals at lower risk of developing skin cancers. Ascertaining whether these RVU differences are justified is beyond the scope of this study and ultimately must be decided by the specialty. Justifying these structural incentives to care for patients at highest risk of NMSCs seems to rely on 1 of 2 arguments: (1) treating NMSCs has higher intrinsic value, or (2) screening for NMSC requires more effort and expertise than managing inflammatory skin diseases. Additional analyses of the differences in the number of wRVUs generated per unit time by patient race, sex, and age would produce the evidence for the differential effort required to provide dermatologic care for these patient populations. Other aspects of health care delivery outside of wRVU assignments may also perpetuate structural racism and disparities in access to dermatologic care. More work is needed to elucidate these additional components and to examine interventions to improve racial equity in dermatology.
Second, these study findings may not be representative of other practices. However, RVUs are assigned on a national level, likely leading to similar disparities in other settings. Furthermore, wRVUs are not a direct measure of financial compensation, which varies by payer. Nonetheless, we selected wRVUs as the primary outcome over direct collections because (1) collections may be confounded by non–patient-related factors, such as local collection practices and negotiated rates with the health system, which may not generalize as well to other centers, and (2) revising wRVU valuations could be an actionable strategy to mitigate structural disparities. This study is also limited by its observational design, which cannot account for unmeasured confounders. The electronic health record we used lacked patient ethnicity data.
Third, this study used hypothesis-driven methods to identify CPT codes that explain the differences in wRVUs by race, sex, and age. Future studies could use data-driven methods, such as regularization and variable selection techniques,20 to empirically identify the minimum set of procedural and diagnostic codes that explain the observed wRVU differences by race, sex, and age.
In addition, CMS is expected to begin implementing major changes to the coding system in 2021. Because the new codes place relatively higher value on medical decision-making, we anticipate that they will mitigate some of the observed race, sex, and age differences in wRVUs and net payments. Additional work is needed to identify the true impact of the new coding system.
Conclusions
This study found that, in an academic outpatient dermatologic clinic, visits with older White male patients generated significantly more wRVUs than visits with patients who were younger, female, and from racial minority groups. Further research is needed to examine the role that such differences may have in perpetuating disparate access to dermatologic care, to elucidate the role of the RUC and RVUs in dermatologic health care disparities, and to confirm whether these findings can be replicated across multiple institutions.
eTable 1. Factors Associated With Net Payments Received for Outpatient Dermatology Encounters in a General Dermatology Practice, Excluding Mohs Surgeons (2016-2020)
eTable 2. Proportion of wRVU Differences Explained by Procedures in a General Dermatology Practice, Excluding Mohs Surgeons (2016-2020)
eTable 3. Factors Associated With wRVUs Generated by Outpatient Dermatology Encounters, Excluding Mohs Surgeons: Sensitivity Analysis Using Multiple Imputation to Include Non-Mohs Participants With Missing Race
eTable 4. Sensitivity Analysis for wRVU Differences Explained by Procedures, Using Multiple Imputation to Include 8,036 Non-Mohs Encounters Missing Race
eTable 5. Factors Associated With wRVUs Generated by General Outpatient Dermatology Encounters, Excluding Mohs Surgeons: Sensitivity Analysis Using a Generalized Estimating Equation Model to Account for RVU Clustering at the Patient Level
References
- 1.Blendon RJ, Schoen C, DesRoches CM, Osborn R, Scoles KL, Zapert K. Inequities in health care: a five-country survey. Health Aff (Millwood). 2002;21(3):182-191. doi: 10.1377/hlthaff.21.3.182 [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. The National Academies Press; 2003. [PubMed] [Google Scholar]
- 3.Ebede T, Papier A. Disparities in dermatology educational resources. J Am Acad Dermatol. 2006;55(4):687-690. doi: 10.1016/j.jaad.2005.10.068 [DOI] [PubMed] [Google Scholar]
- 4.Tripathi R, Knusel KD, Ezaldein HH, Scott JF, Bordeaux JS. Association of demographic and socioeconomic characteristics with differences in use of outpatient dermatology services in the United States. JAMA Dermatol. 2018;154(11):1286-1291. doi: 10.1001/jamadermatol.2018.3114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanBeek M, Swerlick TA, Mathes B, et al. 2020 annual report of DataDerm™: the database of the American Academy of Dermatology (AAD). J Am Acad Dermatol. 2020;S0190-9622(20)33165-0. doi: 10.1016/j.jaad.2020.11.068 [DOI] [PubMed] [Google Scholar]
- 6.Barbieri JS, Shin DB, Wang S, Margolis DJ, Takeshita J. Association of race/ethnicity and sex with differences in health care use and treatment for acne. JAMA Dermatol. 2020;156(3):312-319. doi: 10.1001/jamadermatol.2019.4818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeMeester RH, Xu LJ, Nocon RS, Cook SC, Ducas AM, Chin MH. Solving disparities through payment and delivery system reform: a program to achieve health equity. Health Aff (Millwood). 2017;36(6):1133-1139. doi: 10.1377/hlthaff.2016.0979 [DOI] [PubMed] [Google Scholar]
- 8.Chin MH. Creating the business case for achieving health equity. J Gen Intern Med. 2016;31(7):792-796. doi: 10.1007/s11606-016-3604-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schroeder SA, Sandy LG. Specialty distribution of U.S. physicians—the invisible driver of health care costs. N Engl J Med. 1993;328(13):961-963. doi: 10.1056/NEJM199304013281312 [DOI] [PubMed] [Google Scholar]
- 10.Laugesen MJ, Wada R, Chen EM. In setting doctors’ Medicare fees, CMS almost always accepts the relative value update panel’s advice on work values. Health Aff (Millwood). 2012;31(5):965-972. doi: 10.1377/hlthaff.2011.0557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nurok M, Gewertz B. Relative value units and the measurement of physician performance. JAMA. 2019;322(12):1139-1140. doi: 10.1001/jama.2019.11163 [DOI] [PubMed] [Google Scholar]
- 12.Cherouny P, Nadolski C. Underreimbursement of obstetric and gynecologic invasive services by the resource-based relative value scale. Obstet Gynecol. 1996;87(3):328-331. doi: 10.1016/0029-7844(95)00442-4 [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453-1457. doi: 10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- 14.VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annu Rev Public Health. 2016;37:17-32. doi: 10.1146/annurev-publhealth-032315-021402 [DOI] [PubMed] [Google Scholar]
- 15.Garg A, Kirby JS, Lavian J, Lin G, Strunk A. Sex- and age-adjusted population analysis of prevalence estimates for hidradenitis suppurativa in the United States. JAMA Dermatol. 2017;153(8):760-764. doi: 10.1001/jamadermatol.2017.0201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaufman BP, Guttman-Yassky E, Alexis AF. Atopic dermatitis in diverse racial and ethnic groups-variations in epidemiology, genetics, clinical presentation and treatment. Exp Dermatol. 2018;27(4):340-357. doi: 10.1111/exd.13514 [DOI] [PubMed] [Google Scholar]
- 17.Armour BS, Pitts MM, Maclean R, et al. The effect of explicit financial incentives on physician behavior. Arch Intern Med. 2001;161(10):1261-1266. doi: 10.1001/archinte.161.10.1261 [DOI] [PubMed] [Google Scholar]
- 18.Andreae MC, Freed GL. Using a productivity-based physician compensation program at an academic health center: a case study. Acad Med. 2002;77(9):894-899. doi: 10.1097/00001888-200209000-00019 [DOI] [PubMed] [Google Scholar]
- 19.Wang LL, Adelekun A, Taylor SC, Lipoff JB. Fee-for-service and structural forces may drive racial disparities in US dermatology. Br J Dermatol. 2020;183(4):750-751. doi: 10.1111/bjd.19217 [DOI] [PubMed] [Google Scholar]
- 20.Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc Series B Stat Methodol. 2005;67:301-320. doi: 10.1111/j.1467-9868.2005.00503.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Factors Associated With Net Payments Received for Outpatient Dermatology Encounters in a General Dermatology Practice, Excluding Mohs Surgeons (2016-2020)
eTable 2. Proportion of wRVU Differences Explained by Procedures in a General Dermatology Practice, Excluding Mohs Surgeons (2016-2020)
eTable 3. Factors Associated With wRVUs Generated by Outpatient Dermatology Encounters, Excluding Mohs Surgeons: Sensitivity Analysis Using Multiple Imputation to Include Non-Mohs Participants With Missing Race
eTable 4. Sensitivity Analysis for wRVU Differences Explained by Procedures, Using Multiple Imputation to Include 8,036 Non-Mohs Encounters Missing Race
eTable 5. Factors Associated With wRVUs Generated by General Outpatient Dermatology Encounters, Excluding Mohs Surgeons: Sensitivity Analysis Using a Generalized Estimating Equation Model to Account for RVU Clustering at the Patient Level