Abstract
Background
Colibactin is a genotoxin that induces DNA double-strand breaks that may lead to carcinogenesis and is produced by Escherichia coli strains harboring the pks island. Human and animal studies have shown that colibactin-producing gut bacteria promote carcinogenesis and enhance the progression of colorectal cancer through cellular senescence and chromosomal abnormalities. In this study, we investigated the impact of prebiotics on the genotoxicity of colibactin-producing E. coli strains Nissle 1917 and NC101.
Methods
Bacteria were grown in medium supplemented with 20, 30 and 40 mg/mL of prebiotics inulin or galacto-oligosaccharide, and with or without 5 μM, 25 μM and 125 μM of ferrous sulfate. Colibactin expression was assessed by luciferase reporter assay for the clbA gene, essential for colibactin production, in E. coli Nissle 1917 and by RT-PCR in E. coli NC101. The human epithelial colorectal adenocarcinoma cell line, Caco-2, was used to assess colibactin-induced megalocytosis by methylene blue binding assay and genotoxicity by γ-H2AX immunofluorescence analysis.
Results
Inulin and galacto-oligosaccharide enhanced the expression of clbA in pks+ E. coli. However, the addition of 125 μM of ferrous sulfate inhibited the expression of clbA triggered by oligosaccharides. In the presence of either oligosaccharide, E. coli NC101 increased dysplasia and DNA double-strand breaks in Caco-2 cells compared to untreated cells.
Conclusion
Our results suggest that, in vitro, prebiotic oligosaccharides exacerbate DNA damage induced by colibactin-producing bacteria. Further studies are necessary to establish whether oligosaccharide supplementation may lead to increased colorectal tumorigenesis in animal models colonized with pks+ E. coli.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-021-07876-8.
Keywords: E. coli, Colorectal cancer, Colibactin, Genotoxin, Inulin, Galacto-oligosaccharides, Iron
Background
Colorectal cancer (CRC), the 3rd most prevalent cancer worldwide, is caused by various factors such as genetics, diet, environment, lifestyle and the gut microbiome [1]. CRC and colitis-associated CRC patients display an unbalanced gut microbiome, which leads to significant differences in species richness and diversity compared to healthy individuals [2]. For instance, the proportion of beneficial bacteria such as Bifidobacterium, Clostridiales and Faecalibacterium are decreased while the relative abundance of potentially harmful bacteria belonging to the Enterobacteriaceae family, such as some Escherichia coli strains, is higher [3].
E. coli that harbor the polyketide synthase (pks) island can be part of the microbial pool colonizing the gut of patients with inflammatory bowel disease [4], patients with familial adenomatous polyposis [5] or CRC, as well as healthy individuals [6]. This genomic island encodes the components of a polyketide/non-ribosomal peptide hybrid biosynthesis pathway that is responsible for the expression of the genotoxin colibactin [7]. Colibactin causes DNA double-strand breaks (DSBs) in mammalian cells and leads to cell cycle arrest, senescence and chromosomal abnormalities [8, 9]. More recently, a distinct mutational profile has been identified in CRC, suggesting a direct mutational process resulting from past exposure to colibactin-producing bacteria [10]. Furthermore, mono-colonization of pks+ E. coli in murine models showed a direct link between colibactin production and colon carcinogenesis [4, 5]. Importantly, about 20–22% of healthy individuals are colonized by pks+ E. coli [5, 6], and these individuals may be at higher risk of developing CRC.
Since complete eradication of pks+ E. coli from the gut microbiome is not feasible to reduce CRC risk [11–13], we aimed at regulating the genotoxin by using prebiotics, a major regulator of the gut microbiota metabolism [14]. Prebiotics are fermentable fibers, which include oligosaccharides, that have beneficial effects on intestinal health through the maintenance of mucosal integrity, and most importantly, through the promotion of beneficial bacteria feeding on prebiotics to generate short chain fatty acids [15, 16]. For example, inulin used in combination with a probiotic decreased the viability and growth of E. coli [17, 18], whereas galacto-oligosaccharides (GOS) was shown to reduce the adhesion of enteropathogenic E. coli to cultured cells [19]. However, little is known about the direct effect of prebiotics supplementation on genotoxin expression from pks+ E. coli present in the gut microbiota.
In this study, we investigated the effects of inulin and GOS, two oligosaccharides known to regulate bacterial metabolism, on colibactin using two pks+ E. coli strains. The effect of supplementation with iron, a known colibactin regulator [20, 21], was additionally assessed. Finally, the effects of inulin and GOS on colibactin-related genotoxicity were evaluated using the adenocarcinoma cell line Caco-2.
Methods
Reagents
Inulin was purchased from Sigma Aldrich (Missouri, USA) and GOS from Carbosynth (Compton, UK), and were prepared as stock solutions of 80 mg/mL. Ferrous sulfate (FeSO4) was purchased from Sigma Aldrich and 100 mM stock solutions were prepared.
Bacterial strains and growth conditions
E. coli strains used in this study: control strain pks- E. coli K-12, which is colibactin-negative (ER2738, New England BioLabs, New York, United States); the murine pks+ E. coli NC101 strain (a gift from Dr. Christian Jobin, Cancer Microbiota & Host Response, UF Health Cancer Center, University of Florida); and the engineered E. coli Nissle 1917 (EcN) strains carrying a chromosomal translational fusion consisting of the promoterless luxABCDE construct and the promoter of one of the four genes clbA, clbB, clbQ or clbR [7]. Frozen bacterial glycerol stocks were grown in lysogeny broth (LB) (Wisent Inc., Québec, Canada). For experiments, bacteria were grown at 37 °C, shaking at 150 rpm in standard minimal medium (M9). For infection of Caco-2 cells, bacteria were grown in Eagle’s Minimum Essential Medium (EMEM) (Wisent Inc) at 37 °C at 150 rpm.
Cell culture and in vitro infection
The human colonic adenocarcinoma cell line Caco-2 (ATCC® HTB-37™) was a gift from Dr. Petronela Ancuta, (Department of Microbiology, Infectiology and Immunology, Université de Montréal). Short Tandem Repeat (STR) analysis for Human Cell Line Authentication was performed using the GenePrint® 10 system (Promega, WI, USA) at Genome Québec, Canada. Cells were monitored for mycoplasma contamination using the ABC PCR mycoplasma detection kit (Applied Biological Materials Inc., BC, Canada). Cells were grown in EMEM supplemented with 20% fetal bovine serum (FBS) (Thermo Fisher). Cells were maintained in 75 cm2 culture flasks at 37 °C in a 5% CO2 (v/v) incubator in a humidified atmosphere.
Growth curves and luciferase measurements
E. coli strains from glycerol stocks were grown in LB at 37 °C at 150 rpm overnight and then sub-cultured at 1/100 dilution in M9 medium. For growth experiments, 1 × 107/100 μl of bacterial cells were inoculated in a transparent 96 well plate (Sarstedt, Nümbrecht, Germany) and were grown with shaking at 37 °C. Bacterial growth (OD600nm) was assessed at every hour. For luminescence measurements, 1 × 107/100 μl of bacterial cells were inoculated in a white 96 well plate (Greiner Bio-One, Kremsmünster, Austria) and were grown with shaking at 37 °C. Light emission (luminescence (count/s) expressed as relative light units (RLU)) was recorded every hour in parallel with OD in a Spark® multimode microplate reader (TECAN, Québec, Canada).
RNA extraction and reverse transcription polymerase chain reaction (PCR)
Total RNA from E. coli NC101 grown in LB for 7 h was isolated, and contaminating DNA was removed using DNase I (Biobasic, Ontario, Canada) for 30 min at 37 °C, followed by RNA extraction using the Total RNA Mini-Preps Kit (Biobasic). Reverse transcription PCR was performed on cDNA reverse transcribed from 50 ng RNA using the High Capacity cDNA Reverse Transcription Kit (Thermo Fisher). Real time PCR was performed using the enzyme PowerUp™ SYBR™ Green Master Mix (Thermo Fisher) using the RG 3000A R (Qiagen, Québec, Canada). Primers used are presented in Additional Table 1. Relative quantitation was performed using standard curves constructed from serial dilutions of PCR products [22]. mRNA expression for each gene was determined by direct comparison with the standard curve of the specific target generated in each PCR run. Expression levels of clbA, clbB, clbQ and clbR were normalized to 16S rRNA.
Megalocytosis assay
Quantification of the colibactin-associated genotoxic effect by megalocytosis assay was performed as previously described [23]. Briefly, E. coli NC101 and K-12 strains from glycerol stocks were grown in LB at 37 °C, shaking overnight. Strains were sub-cultured in EMEM for 4 h. Caco-2 cells were dispensed (1 × 105 cells/well) in a 24 well tissue culture plate (Falcon) at 37 °C in a 5% CO2 atmosphere. After 24 h, Caco-2 cells were infected at a multiplicity of infection (MOI) of 50 with indicated E. coli strains. After 4 h of infection, the cells were washed at least three times with phosphate buffer saline (PBS) (Wisent Inc) and incubated for 72 h in cell culture medium supplemented with 200 μg/ml gentamicin (VWR). Cells were fixed with 4% paraformaldehyde (Thermo Fisher) for 15 min, washed and stained with 1 mM methylene blue (Sigma Aldrich). Pictures were taken under a Nikon Eclipse TE300 microscope (Nikon Healthcare, Québec, Canada) and images were acquired using the NIS-Elements BR4.00.03 software (200X magnification). Methylene blue extraction solution was used to quantify cell damage and megalocytosis at 660 nm absorbance (Spark® multimode microplate reader).
Cell viability assay
Viability of Caco-2 cells was examined using a 3-(4,5-DimethylthiaZA-2-yl)-2,5-diphenyltetrazolium bromide (MTT) (Sigma Aldrich) as previously described [24]. Briefly, after infection the cells were washed with PBS and incubated for 72 h in cell culture medium supplemented with 200 μg/ml gentamicin. Cells were incubated with 10 µL of MTT for 3 h at 37 °C in a 5% CO2 atmosphere. After the incubation period, 100 μL of acid-isopropanol (0.04 N HCi in isopropanol) were added and mixed thoroughly to dissolve the formazan crystals. Cell viability was quantified at 540 nm absorbance using the Spark® multimode microplate reader.
Fluorescent immunostaining of γ-H2AX by In Cell Western assay
Quantification of DNA DSBs was performed using the In Cell Western assay as described [25]. Caco-2 cells were dispensed (1 × 105 cells/well) in a black 96 well plate (Greiner Bio-One) and incubated at 37 °C in 5% CO2 atmosphere. After 24 h, Caco-2 cells were infected at MOI 50 with E. coli strains. After 4 h of infection, the cells were washed three times with PBS and incubated for 3 h in cell culture medium supplemented with 200 μg/ml gentamicin. Cells were fixed (4% paraformaldehyde), permeabilized, blocked and then incubated overnight with rabbit monoclonal anti-γ-H2AX (BioLabs) at 1/200 dilution. Secondary antibody IRDye™800CW goat anti-rabbit (Biotium, Wisconsin, United States) was applied simultaneously with 1/500 dilution of RedDot™2 (Biotium) for DNA labeling. The DNA and γ-H2AX were visualized using Odyssey® infrared imaging scanner (LI-COR model 9120, Québec, Canada) with red denoting RedDot™2 and green for IRDye™800CW goat anti-rabbit. Images were processed using Image Studio Ver3.1 software.
Statistics
Experiments were performed at least three separate times and with each condition in triplicate. Results are presented as mean ± SEM. Graphs were drawn using GraphPad Prism (Version 5.0) software, and ANOVA with post-hoc Tukey’s test was used to determine statistically significant results.
Results
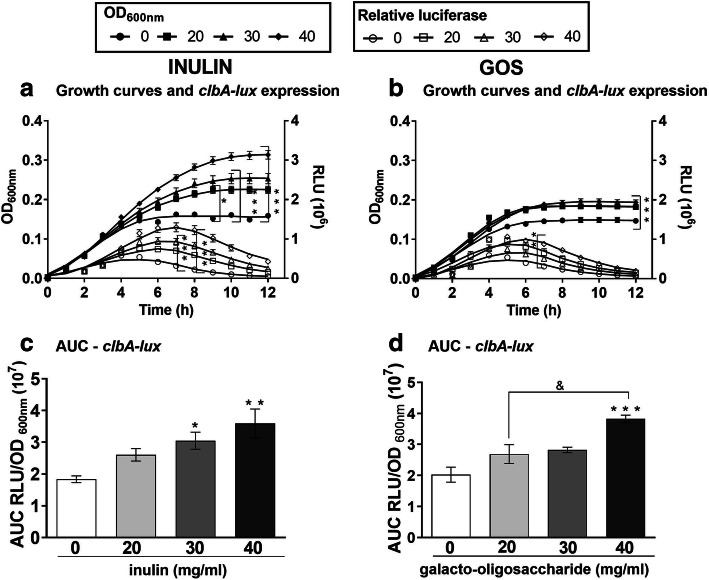
Inulin and GOS enhance clbA expression in EcN
To study the impact of oligosaccharides on the growth of EcN and colibactin expression, we cultured the bacteria in the presence of inulin or GOS. As shown in Fig. 1 a and Supplementary Fig. 1A-C the addition of inulin from 20 mg/mL to 40 mg/mL to minimal media significantly increased bacterial growth (OD600). Similarly, GOS supplementation stimulated the growth of EcN, albeit to a lesser extent than inulin (OD600, Fig. 1b and Additional Fig. 1D-F).
Fig. 1.
Inulin and GOS increase the clbA promoter activity. a-b Growth curves and luminescence measurement of EcN carrying the translational clbA-luciferase reporter fusion. The effect of 0, 20, 30 and 40 mg/mL of inulin (a) and GOS (b) on growth (OD600; filled symbols) and on clbA-lux relative luminescence (RLU 106; open symbols). c-d Area under the curve (AUC) of RLU/OD600 for inulin (c) and GOS (d). *P < 0.05, **P < 0.01, ***P < 0.001 compared to control (0 mg/mL oligosaccharides) and &P < 0.05; ANOVA
To determine colibactin expression, the transcript levels of the genes clbA, clbB, clbQ, and clbR fused to a promoterless luciferase reporter construct (lux) were quantified by relative luminescence (RLU, Fig. 1a-b and Additional Fig. 1a-f). As previously reported [7], the clbA gene had the highest expression, followed by clbB, clbR and clbQ. For clbA, we found an increase in RLU over time, peaking around 7 h. When bacteria were supplemented with 40 mg/mL of oligosaccharides, a significant increase in RLU was seen when compared to control conditions of bacteria grown in the absence of prebiotics (Fig. 1a-b and Additional Fig. 1 A-F).
The area under the curve (AUC), calculated by dividing the RLU by OD600, revealed that inulin supplementation increased the expression of clbA (Fig. 1c), as well as clbB, clbQ and clbR (Additional Fig. 1G-I), in a dose-dependent manner. In turn, GOS enhanced the expression of clbA only at the highest concentration, i.e. 40 mg/mL (Fig. 1d), without affecting the levels of clbB, clbQ and clbR (Additional Fig. 1 J-L).
These results indicate that inulin stimulates the expression of several clb genes in EcN, while GOS affects clbA expression only.
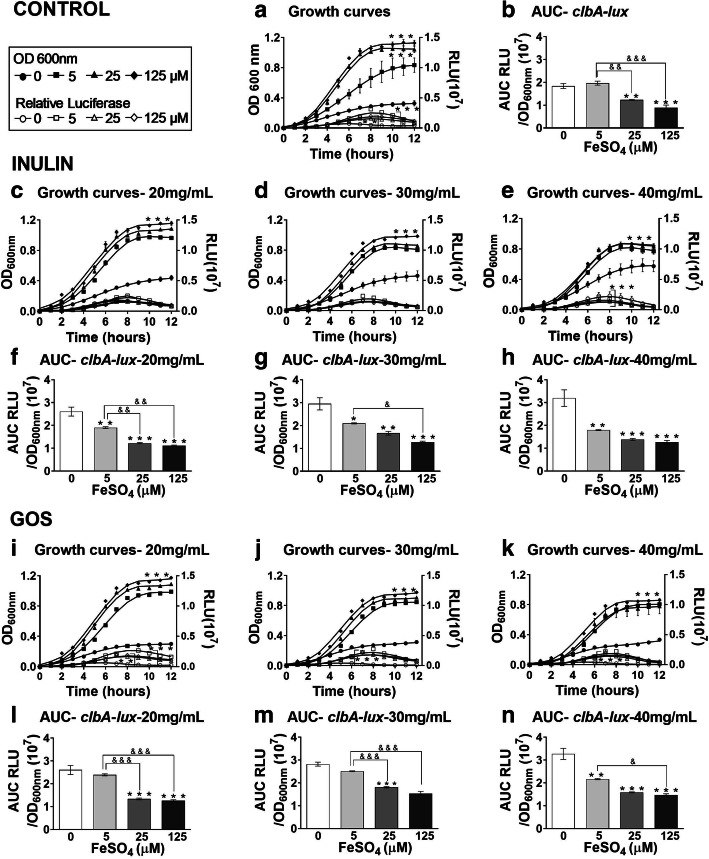
Iron decreases the clbA expression of EcN stimulated by oligosaccharides
In addition to colibactin synthesis, the clbA gene from the pks island is also involved in the synthesis of siderophores, such as enterobactin and yersiniabactin, which are small molecules synthesized by bacteria that scavenge and solubilize ferric iron (Fe3+) [26]. Iron was previously shown to downregulate the expression of the colibactin gene cluster including the clbA gene [21, 26, 27]. Hence, we tested, using the clbA reporter construct, whether the addition of iron abrogated the increased expression of the colibactin gene cluster induced by oligosaccharides supplementation. The addition of ferrous sulfate to the minimal medium resulted in significantly increased growth of EcN (Fig. 2a), whereas clbA transcript levels were reduced in a concentration-dependent-manner (Fig. 2b), as expected [21, 27]. Addition of inulin increased the growth of EcN as confirmed by our previous experiments (Fig. 2c-e; line with circles). However, when comparing the growth curves of bacteria exposed to increasing inulin concentrations in medium containing ferrous sulfate at 125 μM, the inulin-induced growth was visibly inhibited, as shown in Fig. 2c-e (line with diamonds).
Fig. 2.
Iron decreases the transcription of clbA promoter activity promoted by oligosaccharides. a Growth curves and luminescence measurement of EcN the translational clbA luciferase reporter fusion and b area under the curve (AUC) of RLU/OD600, in media containing 5 μM, 25 μM and 125 μM ferrous sulfate without inulin and with c 20, d 30, e 40 mg/mL inulin and f-h corresponding area under the curve (AUC) of RLU/OD600. Growth curves and luminescence measurement of EcN in media containing 5 μM, 25 μM and 125 μM ferrous sulfate supplemented with i 20, j 30, k 40 mg/mL GOS and l-n corresponding area under the curve (AUC) of RLU/OD600. *P < 0.05, **P < 0.01, ***P < 0.001 compared to control (0 mg/mL oligosaccharides); &P < 0.05, &&P < 0.01, and &&&P < 0.001; ANOVA
We then calculated the individual luciferase activity levels (AUC of RLU/OD600) when the bacteria were grown in medium supplemented with inulin and iron. The addition of 5 to 125 μM of ferrous sulfate to the medium with inulin led to a decrease in clbA expression in a concentration-dependent manner (Fig. 2f-h). Similar results using GOS supplementation were obtained regarding bacterial growth (Fig. 2i-k) and clbA expression (Fig. 2l-n).
These results indicate that iron supplementation inhibits the effects of oligosaccharides on bacterial growth and clbA induction as an indicator for the expression of the colibactin gene cluster.
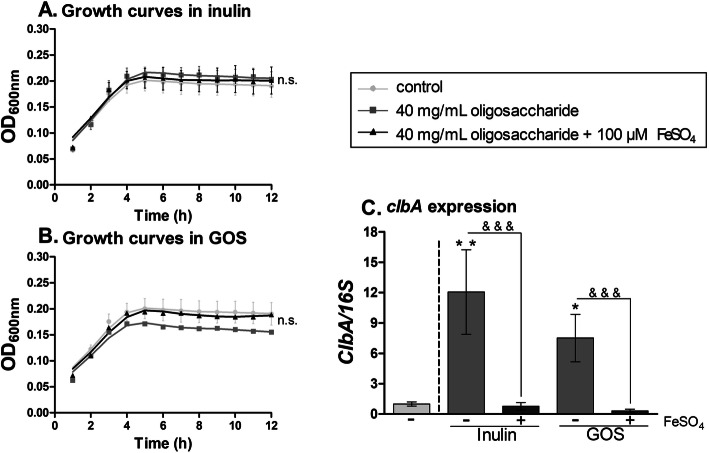
Inulin and GOS enhance clbA expression in tumor-promoting E. coli strain NC101
We tested the effects of inulin and GOS on tumor- and inflammation-promoting E. coli strain NC101, which also harbors the pks genomic island [4, 28]. We incubated E. coli NC101 in the presence of the highest concentrations of both oligosaccharides (40 mg/ml) and 100 μM of iron sulfate. As shown in Fig. 3a-b, inulin and GOS supplementation did not influence the growth of E. coli NC101. However, oligosaccharide supplementation increased the transcript levels of clbA compared to control (Fig. 3c). Similar to our luciferase results with EcN, when iron was added to the medium with oligosaccharides, the expression of the clbA gene was reduced. As shown in Additional Fig. 2a-c, inulin supplementation, but not GOS, substantially enhanced the transcript levels of clbB, clbQ, and clbR genes, an effect that was completely inhibited by the addition of iron to the medium.
Fig. 3.
Inulin and GOS increase the expression of clbA in E. coli strain NC101. a-b Growth curves of E. coli NC101 grown in 100 μM of iron sulfate and 40 mg/mL of inulin (a) or 40 mg/mL of GOS (b). c Fold change of clbA/16S rRNA expression in minimal medium supplemented with inulin or GOS, with or without 100 μM iron sulfate. *P < 0.05, **P < 0.01, n.s. non-significant compared to control (0 mg/mL oligosaccharides) and &&&P < 0.001; ANOVA
These results indicate that inulin and GOS consistently increase the expression of the clbA gene in the E. coli strain NC101 and that this increase can be inhibited by iron supplementation.
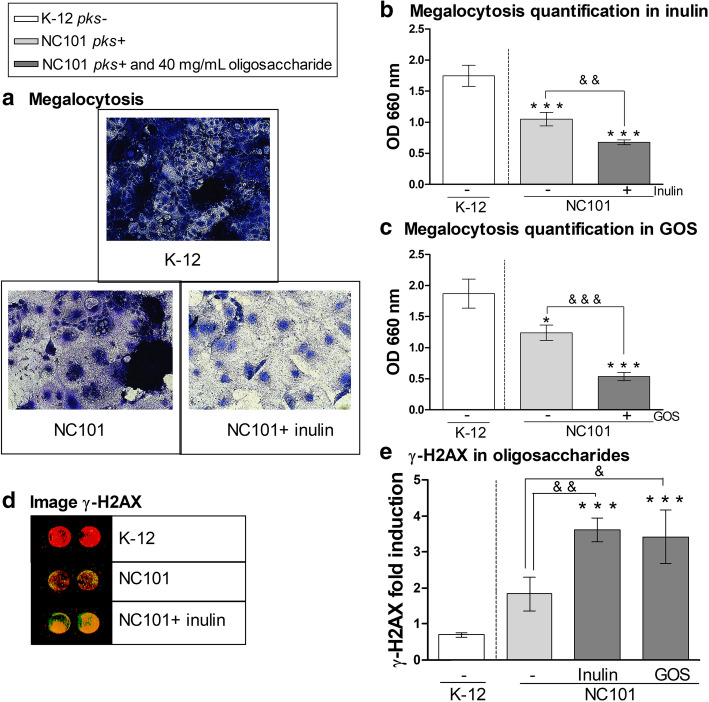
Oligosaccharides increase colibactin-induced cytotoxicity and DNA double-strand breaks in Caco-2 cells
Our results indicate that inulin and GOS upregulate clbA expression and thus expression of the colibactin operon. We investigated whether this increased expression of the colibactin gene cluster at the transcriptional level could also result in greater genotoxicity. We used the E. coli K-12 strain, which is psk-, and the pks+ strain NC101 to infect the adenocarcinoma cell line Caco-2 and assessed cytotoxicity through cell viability and the megalocytosis assay. As reported by others [24, 29], Caco-2 cell viability was reduced when infected with E. coli NC101 compared to E. coli K-12 control strain. However, a similar cell viability loss was seen in cells infected with E. coli NC101 in the absence of oligosaccharides and those supplemented with inulin or GOS (Additional Fig. 3a). As expected [29], Fig. 4a shows that cells infected with E. coli NC101 displayed enhanced megalocytosis compared to cells infected with the control E. coli K-12 strain. The addition of 40 mg/mL of oligosaccharides to the medium resulted in a significant increase in abnormal cell enlargement (Fig. 4a) as determined by the lower absorbance (660 nm), as shown in Fig. 4b (inulin, 1.6-fold decrease) and 4C (GOS, 2.3-fold decrease compared to cells infected with E. coli NC101 in the absence of oligosaccharides). Hence, most surviving cells in the inulin or GOS treated wells were megalocytic compared to untreated wells.
Fig. 4.
Inulin and GOS enhance DNA damage in Caco-2 cells infected with pks+ E. coli strain NC101. a Representative images of methylene blue staining for quantification of megalocytosis of Caco-2 cells 4 h post-infection (multiplicity of infection = 50 bacteria/cell; magnification 200x). E. coli K-12 was used as a pks- control strain. b-c Quantification of megalocytosis of Caco-2 cells with addition of inulin (b) and GOS (c) in medium. d Scan of In Cell Western image showing DNA DSBs with merged detection of total DNA (red, 680 nm) and γ-H2AX (green, 800 nm). e γ-H2AX fold induction in inulin and GOS (analysis were done on single colored picture). *P < 0.05, ***P < 0.001, compared to the control, pks- E. coli K-12 and &P < 0.05, &&P < 0.01, &&&P < 0.001; ANOVA
Taking into account the well-described effects of colibactin causing DNA DSBs [9] we used an in-cell Western assay to quantify DNA DSBs in Caco-2 cells infected with E. coli strains K-12 and NC101. DSBs in Caco-2 cells infected with E. coli NC101 were evident compared to the K-12 strain (Fig. 4d). Most importantly, the addition of 40 mg/mL of inulin led to an increase of the DSBs in Caco-2 cells as indicated by levels of γ-H2AX, a marker of DNA damage (Fig. 4e, 2-fold increase). Similar results were obtained when using GOS treatment (Fig. 4e, 1.9-fold increase).
Taken together, these data show that oligosaccharides not only increase the expression of colibactin genes, but also lead to an increase in cytotoxicity and DNA DSBs in Caco-2 cells.
Discussion
The aim of this study was to investigate whether prebiotics, inulin and GOS, could modulate the expression and toxicity of the genotoxin colibactin, which has been linked to CRC development. Given the well-established link between diet [30], gut microbiota [31], and CRC a better understanding of how colibactin expression is regulated by different nutrients and supplements is of paramount importance due to the increasing presence of pks+ E. coli in healthy individuals in Western countries [5, 32] and, more recently, among Malaysian [33], Indian [34], and Japanese populations [35].
We show that fermentable fibers, such as inulin and GOS, promote the growth of colibactin-producing E. coli strains and elevate the expression of colibactin-related genes, as exemplified by clbA transcription. The clbA gene located in the pks island encodes a 4′-phosphopantetheinyl transferase and is required for colibactin synthesis [9]. Accordingly, previous studies have demonstrated that clbA inactivation prevents DNA damage and chromosomal abnormalities [36, 37]. Most importantly, clbA has been shown to contribute to the production of siderophores, which are small iron chelating compounds produced by bacteria [26]. Addition of ferric chloride to the medium inhibited the expression of colibactin related-genes [20, 27]. We further showed that addition of iron abolished the increased transcription of clbA induced by inulin and GOS, counteracting the effect of these fermentable fibers. This may be of interest in the context of CRC, as many patients develop anemia and are prescribed oral iron supplementation, mostly ferrous sulphate tablets [38]. Interestingly, elevated iron levels in the colon seem to be required for the probiotic activity of EcN in mice with dextran sodium sulfate (DSS)-induced colitis [39], which would have the added benefit of inhibiting colibactin expression and reducing potential EcN genotoxicity.
Consistent with increased bacterial growth and transcription of colibactin genes, inulin and GOS exacerbated the DNA damage that was induced in the pks+ E. coli NC101 strain. An increased number of DSBs caused by colibactin would result in the accumulation of mutations in colonic cells [40], which appear in early adenomas and accumulate in late carcinoma stages [41]. Hence, increased incidence of DSBs may accelerate the development and aggressiveness of the tumors. In fact, pks+ E. coli isolated from CRC patients were found to establish persistent colonization, exacerbate inflammation, and trigger carcinogenesis in mice [42].
Our findings add to the efforts in identifying environmental factors that may influence colibactin expression. For example, cinnamon and cinnamaldehyde have been shown to inhibit the expression of the clbB gene among several E. coli isolates from CRC patients [43]. More recently, a new study identified compounds of tannin and quercetin from medicinal plant extracts of Terminalia catappa, Psidium guajava and Sandoricum koetjape that inhibited the growth and transcription of colibactin genes of colibactin-producing E. coli [44].
Colibactin-related genes can also be upregulated by environmental factors, which was shown with natural food contaminants such as mycotoxins [45]. Deoxynivalenol, produced by Fusarium graminearum and F. culmorum, has been shown to exacerbate the intestinal DNA damage induced by colibactin-producing E. coli strains [46].
Our results are somehow unexpected, because prebiotics have been shown to have beneficial properties towards the gut microbial community. Bacterial cultures from stool samples supplemented with inulin showed a decrease in the Enterobacteriaceae family while promoting the growth of beneficial bacteria such as Lactobacillus and Bifidobacteria [47], and GOS was found to diminish the adhesion capacity of pathogenic E. coli [19]. However, those studies did not assess the potential presence and/or expression levels of colibactin genes. Furthermore, several studies in CRC rodents models showed inconsistent effects of dietary oligosaccharide supplementation on tumor growth [48]. Indeed, supplementation with 10% inulin in ApcMin/+ mice induced an increase of polyps and tumors size in the small intestine [49, 50]. However, supplementation with 15% of inulin in syngeneic wild type mice transplanted with tumors cells subcutaneously presented a slower tumor growth rate [51], and supplementation with 10% GOS in rats receiving azoxymethane and DSS to induce CRC inhibited tumor growth in the colon [52]. These studies did not assess the possible presence of pks+ E. coli strains, which may modify responses to oligosaccharides in the tested CRC models. In addition, standard rodent diets may contain varying amounts of iron between studies and, at the present, it is not clear whether dietary iron content may influence colibactin expression in the gut and affect outcomes. In any case, it should be understood that the mere presence of pks+ harboring strains in the gut is not sufficient to induce CRC and that there are other contributing factors [53].
Conclusion
In conclusion we showed that, in vitro, the expression of colibactin genes and genotoxicity of E. coli strains harboring the pks island is increased by inulin and GOS supplementation. In view of the increasing usage of prebiotics and their availability as over-the-counter medicines and natural products, further experiments are needed to investigate how these prebiotics may modulate tumor development and progression in animal models and in humans in the presence of pks+ E. coli colonization. In addition to unveiling valuable information on the impact of oligosaccharides on colorectal tumors, further studies on specific conditions where oligosaccharides supplementation may have procarcinogenic effects could lead to personalized dietary recommendations to individuals harboring pks+. E. coli.
Supplementary Information
Additional file 1: Table S1. Primers. Figure S1. Inulin and GOS increase the transcription of clbB-, clbQ- and clbR-lux. Growth curves of E. coli Nissle 1917 incubated with 0, 20, 30 and 40 mg/mL of inulin (A-C) or GOS (D-F) (OD600; filled symbols), and relative luminescence (RLU 106; opened symbols) of clbB-lux (A and D), clbQ-lux (B and E), and clbR-lux (C and F). Area under the curve (AUC) of RLU/OD600 for inulin (G-I) and GOS (J-L). *P < 0.05, **P < 0.01, ***P < 0.001 compared to control (0 mg/mL, oligosaccharides); ANOVA. Figure S2. Inulin increases the transcription of clbB, clbQ and clbR in E. coli NC101. Fold change of mRNA (A) clbB (B) clbQ and (C) clbR normalized on 16S rRNA expression in E. coli NC101 grown in minimal medium supplemented with inulin or GOS, in the absence (−) or presence (+) of 100 μM ferrous sulfate. n.s. non-significant, *P < 0.05 compared to control (0 mg/mL oligosaccharides); ANOVA. Figure S3. Caco-2 cell viability decreases when infected with pks+ E. coli strain NC101. (A) Quantification of Caco-2 cells viability with addition of 40 mg/mL inulin and GOS in medium. E. coli K-12 was used as a pks- control strain. *P < 0.05, ***P < 0.001 compared to the control, pks- E. coli K-12; n.s. non-significant.; ANOVA.
Acknowledgements
We thank Jacqueline Chung for help in editing the manuscript.
Abbreviations
- ANOVA
analysis of variance
- AUC
area under the curve
- CRC
colorectal cancer
- EcN
E. coli Nissle 1917
- EMEM
Eagle′s Minimal Essential Medium
- DSBs
double-strand breaks
- DSS
dextran sodium sulfate
- FBS
fetal bovine serum
- GOS
galacto-oligosaccharides
- LB
lysogeny broth
- M9
minimal medium
- MOI
multiplicity of infection
- MTT
3-(4,5-DimethylthiaZA-2-yl)-2,5-diphenyltetrazolium bromide
- OD
optical density
- PBS
phosphate-buffered saline
- PCR
polymerase chain reaction
- pks
polyketide synthetase
- RLU
relative light units
- rpm
revolution per minute
Authors’ contributions
MO contributed to the investigation. MO, AC, GF, and UD contributed to methodology. MO, TC, RH, and MMS contributed to conceptualization. MO and MMS contributed to validation, formal analysis, data visualization, and wrote and reviewed the original draft. MMS additionally contributed to supervision, resources and funding acquisition of the study. All authors have read and approved the version to be published.
Funding
This work was supported by grants from the Canadian Institutes of Health Research [CIHR, grant FRN-159775] and the Natural Sciences and Engineering Research Council of Canada [NSERC, grant RGPIN-2018-06442] to MMS. MO and TC are the recipients of the Canderel scholarship from the Institut du cancer de Montréal; TC is the recipient of the Rougier-Armandie scholarship from the Université de Montréal, and RH received a scholarship from the Fonds de recherche du Québec – Santé [FRQ-S]/ Ministère de la Santé et des Services sociaux [MSSS; Resident Physician Health Research Career Training Program]. The work of UD was supported by the Interdisciplinary Center for Clinical Research of the Medical Faculty Münster [Dob2/013/12].
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Ethics approval and consent to participate
Ethical approval was not required for the experiments detailed in this manuscript.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Manon Oliero, Email: Manon.oliero@umontreal.ca.
Annie Calvé, Email: anniecalve@gmail.com.
Gabriela Fragoso, Email: gabriela.fragoso.chum@ssss.gouv.qc.ca.
Thibault Cuisiniere, Email: Thibault.cuisiniere@umontreal.ca.
Roy Hajjar, Email: Roy.hajjar@umontreal.ca.
Ulrich Dobrindt, Email: dobrindt@uni-muenster.de.
Manuela M. Santos, Email: manuela.santos@umontreal.ca
References
- 1.Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol. 2019;14(2):89–103. doi: 10.5114/pg.2018.81072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu W, Zhang R, Shu R, Yu J, Li H, Long H, Jin S, Li S, Hu Q, Yao F, et al. Study of the relationship between microbiome and colorectal Cancer susceptibility using 16SrRNA sequencing. Biomed Res Int. 2020;2020:7828392. doi: 10.1155/2020/7828392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zou S, Fang L, Lee MH. Dysbiosis of gut microbiota in promoting the development of colorectal cancer. Gastroenterol Rep (Oxf) 2018;6(1):1–12. doi: 10.1093/gastro/gox031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arthur JC, Perez-Chanona E, Muhlbauer M, Tomkovich S, Uronis JM, Fan TJ, Campbell BJ, Abujamel T, Dogan B, Rogers AB, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012;338(6103):120–123. doi: 10.1126/science.1224820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dejea CM, Fathi P, Craig JM, Boleij A, Taddese R, Geis AL, Wu X, DeStefano Shields CE, Hechenbleikner EM, Huso DL, et al. Patients with familial adenomatous polyposis harbor colonic biofilms containing tumorigenic bacteria. Science. 2018;359:552–597. doi: 10.1126/science.aah3648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buc E, Dubois D, Sauvanet P, Raisch J, Delmas J, Darfeuille-Michaud A, Pezet D, Bonnet R. High Prevalence of Mucosa-Associated E. coli Producing Cyclomodulin and Genotoxin in Colon Cancer. PLOS ONE. 2013;8(2):e56964. doi: 10.1371/journal.pone.0056964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Homburg S, Oswald E, Hacker J, Dobrindt U. Expression analysis of the colibactin gene cluster coding for a novel polyketide in Escherichia coli. FEMS Microbiol Lett. 2007;275(2):255–262. doi: 10.1111/j.1574-6968.2007.00889.x. [DOI] [PubMed] [Google Scholar]
- 8.Secher T, Samba-Louaka A, Oswald E, Nougayrède J-P. Escherichia coli producing colibactin triggers premature and transmissible senescence in mammalian cells. PLoS One. 2013;8(10):e77157. doi: 10.1371/journal.pone.0077157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nougayrede JP, Homburg S, Taieb F, Boury M, Brzuszkiewicz E, Gottschalk G, Buchrieser C, Hacker J, Dobrindt U, Oswald E. Escherichia coli induces DNA double-strand breaks in eukaryotic cells. Science. 2006;313(5788):848–851. doi: 10.1126/science.1127059. [DOI] [PubMed] [Google Scholar]
- 10.Pleguezuelos-Manzano C, Puschhof J, Rosendahl Huber A, van Hoeck A, Wood HM, Nomburg J, Gurjao C, Manders F, Dalmasso G, Stege PB, et al. Mutational signature in colorectal cancer caused by genotoxic pks(+) E. coli. Nature. 2020;580(7802):269–273. doi: 10.1038/s41586-020-2080-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamada N, Chen GY, Inohara N, Nunez G. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol. 2013;14(7):685–690. doi: 10.1038/ni.2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Massot M, Daubié A-S, Clermont O, Jauréguy F, Couffignal C, Dahbi G, Mora A, Blanco J, Branger C, Mentré F, et al. Phylogenetic, virulence and antibiotic resistance characteristics of commensal strain populations of Escherichia coli from community subjects in the Paris area in 2010 and evolution over 30 years. Microbiology (Reading) 2016;162(4):642–650. doi: 10.1099/mic.0.000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cole BK, Ilikj M, McCloskey CB, Chavez-Bueno S. Antibiotic resistance and molecular characterization of bacteremia Escherichia coli isolates from newborns in the United States. PLoS One. 2019;14(7):e0219352. doi: 10.1371/journal.pone.0219352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, Scott K, Stanton C, Swanson KS, Cani PD, et al. Expert consensus document: the international scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017;14(8):491–502. doi: 10.1038/nrgastro.2017.75. [DOI] [PubMed] [Google Scholar]
- 15.Pham VT, Seifert N, Richard N, Raederstorff D, Steinert RE, Prudence K, Mohajeri MH. The effects of fermentation products of prebiotic fibres on gut barrier and immune functions in vitro. PeerJ. 2018;6:e5288. doi: 10.7717/peerj.5288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poeker SA, Geirnaert A, Berchtold L, Greppi A, Krych L, Steinert RE, de Wouters T, Lacroix C. Understanding the prebiotic potential of different dietary fibers using an in vitro continuous adult fermentation model (PolyFermS) Sci Rep. 2018;8(1):4318. doi: 10.1038/s41598-018-22438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Önal Darilmaz D, Sönmez Ş, Beyatli Y. The effects of inulin as a prebiotic supplement and the synbiotic interactions of probiotics to improve oxalate degrading activity. Int J Food Sci Technology. 2019;54(1):121–131. doi: 10.1111/ijfs.13912. [DOI] [Google Scholar]
- 18.Fooks LJ, Gibson GR. In vitro investigations of the effect of probiotics and prebiotics on selected human intestinal pathogens. FEMS Microbiol Ecol. 2002;39:67–75. doi: 10.1111/j.1574-6941.2002.tb00907.x. [DOI] [PubMed] [Google Scholar]
- 19.Shoaf K, Mulvey GL, Armstrong GD, Hutkins RW. Prebiotic galactooligosaccharides reduce adherence of enteropathogenic Escherichia coli to tissue culture cells. Infect Immun. 2006;74(12):6920–6928. doi: 10.1128/IAI.01030-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tronnet S, Garcie C, Brachmann AO, Piel J, Oswald E, Martin P: High iron supply inhibits the synthesis of the genotoxin colibactin by pathogenic Escherichia coli through a non-canonical Fur/RyhB-mediated pathway. Pathogens Disease 2017, 75(5). 10.1093/femspd/ftx066. [DOI] [PubMed]
- 21.Tronnet S, Garcie C, Rehm N, Dobrindt U, Oswald E, Martin P. Iron homeostasis regulates the Genotoxicity of Escherichia coli that produces Colibactin. Infect Immun. 2016;84(12):3358–3368. doi: 10.1128/IAI.00659-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makui H, Soares RJ, Jiang W, Constante M, Santos MM. Contribution of Hfe expression in macrophages to the regulation of hepatic hepcidin levels and iron loading. Blood. 2005;106(6):2189–95. 10.1182/blood-2005-02-0629. [DOI] [PMC free article] [PubMed]
- 23.Bossuet-Greif N, Belloy M, Boury M, Oswald E, Nougayrede J-P: Protocol for HeLa Cells Infection with Escherichia coli Strains Producing Colibactin and Quantification of the Induced DNA-damage. Bio-Protocol 2017, 7(16). 10.21769/BioProtoc.2520. [DOI] [PMC free article] [PubMed]
- 24.Bruballa AC, Shiromizu CM, Bernal AM, Pineda GE, Sabbione F, Trevani AS, Bentancor LV, Ramos MV, Fernandez-Brando RJ, Munoz MJ et al: Role of Shiga Toxins in Cytotoxicity and Immunomodulatory Effects of Escherichia coli O157:H7 during Host-Bacterial Interactions in vitro. Toxins (Basel) 2020, 12(1). 10.3390/toxins12010048. [DOI] [PMC free article] [PubMed]
- 25.Tronnet S, Oswald E: Quantification of Colibactin-associated Genotoxicity in HeLa Cells by In Cell Western (ICW) Using γ-H2AX as a Marker. Bio-Protocol 2018, 8(6). 10.21769/BioProtoc.2771. [DOI] [PMC free article] [PubMed]
- 26.Martin P, Marcq I, Magistro G, Penary M, Garcie C, Payros D, Boury M, Olier M, Nougayrede JP, Audebert M, et al. Interplay between siderophores and colibactin genotoxin biosynthetic pathways in Escherichia coli. PLoS Pathog. 2013;9(7):e1003437. doi: 10.1371/journal.ppat.1003437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wallenstein A, Rehm N, Brinkmann M, Selle M, Bossuet-Greif N, Sauer D, Bunk B, Spröer C, Wami HT, Homburg S et al: ClbR Is the Key Transcriptional Activator of Colibactin Gene Expression in Escherichia coli. 2020, 5(4):e00591–00520. 10.1128/mSphere.00591-20%J mSphere. [DOI] [PMC free article] [PubMed]
- 28.Kim SC, Tonkonogy SL, Albright CA, Tsang J, Balish EJ, Braun J, Huycke MM, Sartor RB. Variable phenotypes of enterocolitis in interleukin 10-deficient mice monoassociated with two different commensal bacteria. Gastroenterology. 2005;128(4):891–906. doi: 10.1053/j.gastro.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Bakthavatchalu V, Wert KJ, Feng Y, Mannion A, Ge Z, Garcia A, Scott KE, Caron TJ, Madden CM, Jacobsen JT, et al. Cytotoxic Escherichia coli strains encoding colibactin isolated from immunocompromised mice with urosepsis and meningitis. PLoS One. 2018;13(3):e0194443. doi: 10.1371/journal.pone.0194443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song M, Chan AT, Sun J. Influence of the gut microbiome, diet, and environment on risk of colorectal Cancer. Gastroenterology. 2020;158(2):322–340. doi: 10.1053/j.gastro.2019.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wirbel J, Pyl PT, Kartal E, Zych K, Kashani A, Milanese A, Fleck JS, Voigt AY, Palleja A, Ponnudurai R, et al. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat Med. 2019;25(4):679–689. doi: 10.1038/s41591-019-0406-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raimondi S, Righini L, Candeliere F, Musmeci E, Bonvicini F, Gentilomi G, Starcic Erjavec M, Amaretti A, Rossi M: Antibiotic Resistance, Virulence Factors, Phenotyping, and Genotyping of E. coli Isolated from the Feces of Healthy Subjects. Microorganisms 2019, 7(8). 10.3390/microorganisms7080251. [DOI] [PMC free article] [PubMed]
- 33.Iyadorai T, Mariappan V, Vellasamy KM, Wanyiri JW, Roslani AC, Lee GK, Sears C, Vadivelu J. Prevalence and association of pks+ Escherichia coli with colorectal cancer in patients at the university Malaya medical Centre, Malaysia. PLoS One. 2020;15(1):e0228217. doi: 10.1371/journal.pone.0228217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suresh A, Ranjan A, Jadhav S, Hussain A, Shaik S, Alam M, Baddam R, Wieler LH, Ahmed N. Molecular genetic and functional analysis of pks-harboring, Extra-Intestinal Pathogenic Escherichia coli From India. Front Microbiol. 2018;9:2631. doi: 10.3389/fmicb.2018.02631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoshikawa Y, Tsunematsu Y, Matsuzaki N, Hirayama Y, Higashiguchi F, Sato M, Iwashita Y, Miyoshi N, Mutoh M, Ishikawa H, et al. Characterization of colibactin-producing Escherichia coli isolated from Japanese patients with colorectal cancer. Jpn J Infect Dis. 2020. 10.7883/yoken.JJID.2020.066. [DOI] [PubMed]
- 36.Olier M, Marcq I, Salvador-Cartier C, Secher T, Dobrindt U, Boury M, Bacquie V, Penary M, Gaultier E, Nougayrede JP, et al. Genotoxicity of Escherichia coli Nissle 1917 strain cannot be dissociated from its probiotic activity. Gut Microbes. 2012;3(6):501–509. doi: 10.4161/gmic.21737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bossuet-Greif N, Vignard J, Taieb F, Mirey G, Dubois D, Petit C, Oswald E, Nougayrede JP: The Colibactin Genotoxin Generates DNA Interstrand Cross-Links in Infected Cells. mBio 2018, 9(2). 10.1128/mBio.02393-17. [DOI] [PMC free article] [PubMed]
- 38.Busti F, Marchi G, Ugolini S, Castagna A, Girelli D: Anemia and Iron Deficiency in Cancer Patients: Role of Iron Replacement Therapy. Pharmaceuticals (Basel) 2018, 11(4). 10.3390/ph11040094. [DOI] [PMC free article] [PubMed]
- 39.Constante M, Fragoso G, Lupien-Meilleur J, Calve A, Santos MM. Iron supplements modulate Colon microbiota composition and potentiate the protective effects of probiotics in dextran sodium sulfate-induced colitis. Inflamm Bowel Dis. 2017;23(5):753–766. doi: 10.1097/MIB.0000000000001089. [DOI] [PubMed] [Google Scholar]
- 40.Dziubanska-Kusibab PJ, Berger H, Battistini F, Bouwman BAM, Iftekhar A, Katainen R, Cajuso T, Crosetto N, Orozco M, Aaltonen LA, et al. Colibactin DNA-damage signature indicates mutational impact in colorectal cancer. Nat Med. 2020;26(7):1063–1069. doi: 10.1038/s41591-020-0908-2. [DOI] [PubMed] [Google Scholar]
- 41.Wolff RK, Hoffman MD, Wolff EC, Herrick JS, Sakoda LC, Samowitz WS, Slattery ML. Mutation analysis of adenomas and carcinomas of the colon: early and late drivers. Genes Chromosom Cancer. 2018;57(7):366–376. doi: 10.1002/gcc.22539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raisch J, Buc E, Bonnet M, Sauvanet P, Vazeille E, de Vallee A, Dechelotte P, Darcha C, Pezet D, Bonnet R, et al. Colon cancer-associated B2 Escherichia coli colonize gut mucosa and promote cell proliferation. World J Gastroenterol. 2014;20(21):6560–6572. doi: 10.3748/wjg.v20.i21.6560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kosari F, Taheri M, Moradi A, Hakimi Alni R, Alikhani MY. Evaluation of cinnamon extract effects on clbB gene expression and biofilm formation in Escherichia coli strains isolated from colon cancer patients. BMC Cancer. 2020;20(1):267. doi: 10.1186/s12885-020-06736-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaewkod T, Tobe R, Tragoolpua Y, Mihara H. Medicinal plant extracts protect epithelial cells from infection and DNA damage caused by colibactin-producing Escherichia coli, and inhibit the growth of bacteria. J Appl Microbiol. 2020. 10.1111/jam.14817. [DOI] [PubMed]
- 45.Wu F, Groopman JD, Pestka JJ. Public health impacts of foodborne Mycotoxins. Annu Rev Food Sci Technol. 2014;5(1):351–372. doi: 10.1146/annurev-food-030713-092431. [DOI] [PubMed] [Google Scholar]
- 46.Payros D, Dobrindt U, Martin P, Secher T, Bracarense AP, Boury M, Laffitte J, Pinton P, Oswald E, Oswald IP: The Food Contaminant Deoxynivalenol Exacerbates the Genotoxicity of Gut Microbiota. mBio 2017, 8(2). 10.1128/mBio.00007-17. [DOI] [PMC free article] [PubMed]
- 47.Jung TH, Jeon WM, Han KS. In vitro effects of dietary inulin on human fecal microbiota and butyrate production. J Microbiol Biotechnol. 2015;25(9):1555–1558. doi: 10.4014/jmb.1505.05078. [DOI] [PubMed] [Google Scholar]
- 48.Singh V, Vijay-Kumar M. Beneficial and detrimental effects of processed dietary fibers on intestinal and liver health: health benefits of refined dietary fibers need to be redefined! Gastroenterol Rep (Oxf) 2020;8(2):85–89. doi: 10.1093/gastro/goz072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pajari AM, Rajakangas J, Paivarinta E, Kosma VM, Rafter J, Mutanen M. Promotion of intestinal tumor formation by inulin is associated with an accumulation of cytosolic beta-catenin in min mice. Int J Cancer. 2003;106(5):653–660. doi: 10.1002/ijc.11270. [DOI] [PubMed] [Google Scholar]
- 50.Misikangas M, Tanayama H, Rajakangas J, Linden J, Pajari AM, Mutanen M. Inulin results in increased levels of beta-catenin and cyclin D1 as the adenomas increase in size from small to large in the min/+ mouse. Br J Nutr. 2008;99(5):963–970. doi: 10.1017/S0007114507853414. [DOI] [PubMed] [Google Scholar]
- 51.Li Y, Elmen L, Segota I, Xian Y, Tinoco R, Feng Y, Fujita Y, Segura Munoz RR, Schmaltz R, Bradley LM, et al. Prebiotic-induced anti-tumor immunity attenuates tumor growth. Cell Rep. 2020;30(6):1753–1766. doi: 10.1016/j.celrep.2020.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fernandez J, Moreno FJ, Olano A, Clemente A, Villar CJ, Lombo F. A Galacto-oligosaccharides preparation derived from lactulose protects against colorectal Cancer development in an animal model. Front Microbiol. 2018;9:2004. doi: 10.3389/fmicb.2018.02004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Murphy N, Moreno V, Hughes DJ, Vodicka L, Vodicka P, Aglago EK, Gunter MJ, Jenab M. Lifestyle and dietary environmental factors in colorectal cancer susceptibility. Mol Asp Med. 2019;69:2–9. doi: 10.1016/j.mam.2019.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Primers. Figure S1. Inulin and GOS increase the transcription of clbB-, clbQ- and clbR-lux. Growth curves of E. coli Nissle 1917 incubated with 0, 20, 30 and 40 mg/mL of inulin (A-C) or GOS (D-F) (OD600; filled symbols), and relative luminescence (RLU 106; opened symbols) of clbB-lux (A and D), clbQ-lux (B and E), and clbR-lux (C and F). Area under the curve (AUC) of RLU/OD600 for inulin (G-I) and GOS (J-L). *P < 0.05, **P < 0.01, ***P < 0.001 compared to control (0 mg/mL, oligosaccharides); ANOVA. Figure S2. Inulin increases the transcription of clbB, clbQ and clbR in E. coli NC101. Fold change of mRNA (A) clbB (B) clbQ and (C) clbR normalized on 16S rRNA expression in E. coli NC101 grown in minimal medium supplemented with inulin or GOS, in the absence (−) or presence (+) of 100 μM ferrous sulfate. n.s. non-significant, *P < 0.05 compared to control (0 mg/mL oligosaccharides); ANOVA. Figure S3. Caco-2 cell viability decreases when infected with pks+ E. coli strain NC101. (A) Quantification of Caco-2 cells viability with addition of 40 mg/mL inulin and GOS in medium. E. coli K-12 was used as a pks- control strain. *P < 0.05, ***P < 0.001 compared to the control, pks- E. coli K-12; n.s. non-significant.; ANOVA.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.