Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has infected 38 million individuals and claimed at least 1 million lives across the globe since it originated in Wuhan, China, in December 2019 (1). While SARS-CoV-2 is highly contagious and lethal, with a case fatality rate of 2.8% based on confirmed cases and deaths to date, different countries have reported varying degree of mortality. We investigated whether such difference in mortality may be explained by obesity, a quiet pandemic that has been striking the globe in the last few decades.
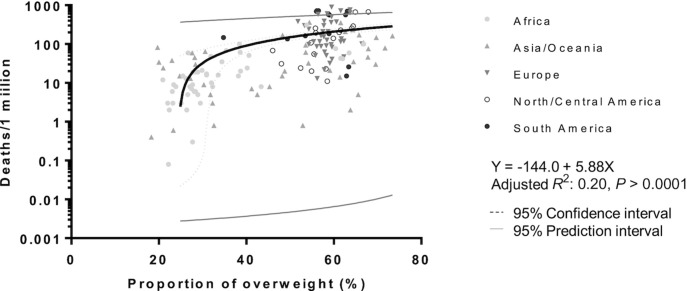
Early studies have identified that obese patients were more likely to test positive for COVID-19 (2). Furthermore, obese patients had a 3.4-fold odds of developing severe COVID-19 compared with normal-weight patients (3). Elderly individuals are most susceptible to COVID-19, but increased risk of intensive care unit admission has been reported in younger patients who are obese (4). Here, by integrating BMI data from the WHO 2016 report (5) and COVID-19 data from worldometers.info (1), we show that the prevalence of overweight [BMI (kg/m2) ≥25] population per country is significantly associated with the number of deaths per million population on a global scale (adjusted R2: 0.20; P < 0.0001), in which countries with a larger proportion of overweight individuals have a greater number of deaths from COVID-19 ( Figure 1). When the association was analyzed by continent, it was statistically significant in North/Central America and Asia/Oceania and showed a trend in other continents.
Figure 1.
Proportion of overweight population and risk of death due to COVID-19 among 176 countries. COVID-19 data from worldometers.info (1) was obtained on 16 October 2020 and BMI data were obtained from the WHO 2016 report (5) for 176 countries. The proportion of overweight [BMI (kg/m2) ≥25] population among countries strongly correlated with the number of deaths per 1 million population (adjusted R2: 0.20; P < 0.0001). COVID-19, coronavirus disease 2019.
Differences in health care infrastructures, population densities, practice of social distancing, and mask-wearing may explain a significant portion of mortality differences across countries; however, our data suggest that overweight, which is a modifiable host factor, may contribute to COVID-19 mortality at a global level. For example, Japan, in which 27.2% of its population has a BMI ≥25, only reports 13 deaths/1 million despite its high population density and highest proportion of elderly individuals. In contrast, the United Kingdom, with 63.4% being overweight, saw a death rate of 639/1 million. It is noteworthy that the youngest patient who died due to COVID-19 in Japan was a sumo wrestler who was 28 years old.
The presence of extra adipose tissue is known to increase the production of proinflammatory cytokines, such as IL-6, in which its pharmacological blockade has demonstrated promising results in treating severe cases of COVID-19 (6). Obesity also increases the risk of developing type 2 diabetes and hypertension, which, in turn, upregulate the expression of angiotensin-converting enzyme 2 (ACE-2) protein that SARS-CoV-2 uses as a binding protein for cellular entry (7). SARS-CoV-2 may gain entry to the pancreas and metabolic organs such as adipose tissue, liver, and small intestine via the ACE-2 receptor, which may lead to the observed marked insulin resistance in COVID-19 (8). Furthermore, obesity diminishes forced vital capacity, increases the risk of thromboembolism, and is associated with the development of pulmonary hypertension (9). All may increase an individual's susceptibility of developing severe viral pneumonia and death from COVID-19. The mechanism of overweight/obesity leading to increased mortality is likely multifactorial and does not account for all the difference in the large variation in deaths seen worldwide, in which differences in social distancing and mask wearing also contribute significantly. The lockdown to mitigate the spread of COVID-19 is known to already have led to quarantine weight gain during the first wave of the COVID-19 pandemic (10), so it is expected that we will see worsening of the obesity pandemic in the near future, which might even have a negative impact during the second and third waves of the COVID-19 pandemic.
The COVID-19 pandemic will eventually pass, but urgent actions to mitigate the spread of the global obesity epidemic are warranted. Countries and policy makers should come up with strategies to combat obesity, promote a healthy diet, and increase physical activity, as these interventions may reduce the tragedy of not only the next viral pandemic but also of the subsequent waves of the present pandemic.
Acknowledgments
The authors’ responsibilities were as follows—JW: methodology (equal contribution) and writing of the original draft; TS: conceptualization (equal contribution) and editing and approval of the final draft; AS: conceptualization, methodology, writing, review, and editing; and all authors: read and approved the final manuscript.
Footnotes
No financial support was received for this article.
Author disclosures: The authors report no conflicts of interest.
References
- 1.Worldometer. COVID-19 coronavirus pandemic. [Internet]. [Accessed 2020 Oct 15]. Available from: https://www.worldometers.info/coronavirus/
- 2.Razieh C, Zaccardi F, Davies MJ, Khunti K, Yates T. Body mass index and the risk of COVID‐19 across ethnic groups: analysis of UK Biobank. Diabetes Obes Metab. Jun 29, 2020. doi: 10.1111/dom.14125. [DOI] [PMC free article] [PubMed]
- 3.Cai Q, Chen F, Wang T, Luo F, Liu X, Wu Q, He Q, Wang Z, Liu Y, Liu L et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care. 2020:dc200576. [DOI] [PubMed]
- 4.Kass DA, Duggal P, Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet North Am Ed. 2020;395:1544–1545. doi: 10.1016/S0140-6736(20)31024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Global Health Observatory (GHO) data, overweight and obesity. [Internet]. [Accessed 2020 Oct 15]. Available from: https://www.who.int/gho/ncd/risk_factors/overweight/en/.
- 6.Xu X, Han M, Li T, Sun W, Wang D, Fu B, Zhou Y, Zheng X, Yang Y, Li X, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vas P, Hopkins D, Feher M, Rubino F, Whyte M. Diabetes, obesity and COVID ‐19: a complex interplay. Diabetes Obes Metab. 2020. [DOI] [PMC free article] [PubMed]
- 9.Sattar N, McInnes IB, McMurray JJV. Obesity a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020;142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 10.Zachary Z, Brianna F, Brianna L, Garrett P, Jade W, Alyssa D, Mikayla K. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obesity Res Clin Pract. 2020;14:210–216. doi: 10.1016/j.orcp.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]