To the Editor
The infection caused by novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is called coronavirus disease 2019 (COVID-19), has spread rapidly worldwide since December 2019.1 Although there is conflicting evidence on whether patients with chronic respiratory diseases are more susceptible to COVID-19, these patients exhibit a more severe presentation and higher mortality compared with those without chronic respiratory diseases.2–4 A meta-analysis revealed that approximately 2% of patients with COVID-19 have concomitant pulmonary disease, which is associated with worse outcomes.5 In agreement with this analysis, several follow-up studies revealed that patients with asthma, chronic obstructive pulmonary disease (COPD), and other chronic respiratory diseases harboured severe clinical manifestations with higher mortality compared with those without chronic respiratory diseases.6,7 However, previous research has not addressed these issues in patients with bronchiectasis. In this study, we performed a nested case–control study using nationally representative data from the COVID-19 cohort and matched cohort in South Korea to evaluate whether the prevalence of bronchiectasis is higher in the COVID-19 cohort than in the matched cohort. We also compared clinical course and mortality of COVID-19 in patients with bronchiectasis and those without bronchiectasis.
The Korean National Health Insurance Service (NHIS) provided researchers with an anonymised national cohort for the evaluation of COVID-19, which comprised the COVID-19 cohort (8070 patients with a confirmed diagnosis of COVID-19 after January 2020) and the matched cohort (121,050 age-, sex-, and residence-matched patients not infected with COVID-19). The data in this cohort were combined with claims-based data from the NHIS between January 2015 and May 2020. Hence, the datasets analysed in this study included personal data as well as inpatient and outpatient records from the past 5 years.8 The institutional review board of our institution approved this study (application No. HYUH 2020-06-029). Since the NHIS database was constructed after anonymisation, the need for informed consent from the participants was waived.
Laboratory confirmation of SARS-CoV-2 infection was defined as a positive result on real-time reverse-transcriptase polymerase chain reaction assay of nasal or pharyngeal swabs, in accordance with the guidelines for laboratory diagnosis of COVID-19 in Korea.9 Bronchiectasis was defined as ⩾2 claims under the International Classification of Diseases 10th revision (ICD-10) diagnosis code J47 during the study period (from January 2015 to May 2020). Additionally, other comorbidities were also defined as ⩾2 claims under ICD-10 codes as major diagnosis codes during the study period. The ICD-10 codes for definition can be found in our previously published study, except for lung cancer (ICD-10 diagnosis code C34).10 Severe COVID-19 was defined as (1) patients who required supplemental oxygen therapy, mechanical ventilator (MV) treatment, extracorporeal membrane oxygenation (ECMO), or intensive care unit (ICU) admission, or (2) patients who died after a confirmed COVID-19 diagnosis.
The rate of bronchiectasis was 1.6% in the COVID-19 cohort (n = 132/8070) and 1.4% in the matched cohort (n = 1630/121,050) (p = 0.030) with a 1.22-fold increased odds ratio (95% confidence interval = 1.01–1.45) of the prevalence of bronchiectasis in the COVID-19 cohort relative to the matched cohort. Of the 8070 patients with COVID-19, 132 (1.6%) had bronchiectasis and 7938 (98.4%) did not have bronchiectasis. COVID-19 patients with bronchiectasis were significantly older (p < 0.001) and more frequently exhibited pulmonary comorbidities, including asthma (62.1% versus 30.4%) and COPD (57.6% versus 17.8%), than those without bronchiectasis. Additionally, COVID-19 patients with bronchiectasis also had more frequent extra-pulmonary comorbidities, including hypertension (52.3% versus 27.0%), diabetes mellitus (61.4% versus 31.0%), and heart failure (27.3% versus 10.1%), than those without bronchiectasis (p < 0.001 for all).
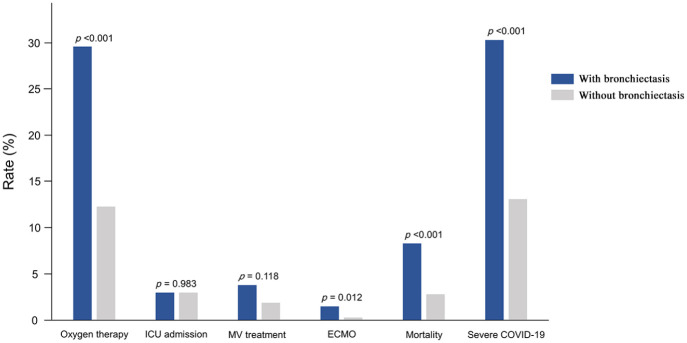
Figure 1 compares the most severe clinical course between the COVID-19 patients with bronchiectasis and those without bronchiectasis. The proportion of patients with severe COVID-19 was significantly higher in patients with bronchiectasis than in those without bronchiectasis [30.3% (40/132) versus 13.1% (1039/7938), p < 0.001]. COVID-19 patients with bronchiectasis required significantly more oxygen (cases receiving MV or ECMO and mortality cases were not included) (29.6% versus 12.3%, p < 0.001) and ECMO (mortality cases were not included) (1.5% versus 0.3%, p = 0.012), and had significantly higher mortality (8.3% versus 2.8%, p < 0.001) than those without bronchiectasis. The rates of ICU admission (3.0% versus 3.0%, p = 0.983) and MV treatment (cases receiving ECMO and mortality cases were not included) (3.8% versus 1.9%, p = 0.118) were not significantly different between the two groups.
Figure 1.
Comparison of the most severe clinical course between the COVID-19 patients with bronchiectasis and those without bronchiectasis. Patients receiving oxygen therapy did not include cases receiving MV treatment or ECMO and mortality cases; those receiving MV treatment did not include cases receiving ECMO and mortality cases; those receiving ECMO did not include mortality cases.
COVID-19, coronavirus disease 2019; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; MV, mechanical ventilation.
The first notable finding of this study is that the rate of COVID-19 was relatively higher in patients with bronchiectasis than those without bronchiectasis. Considering that age-, sex-, and residence-matching was done before comparison, this study provides evidence suggesting that bronchiectasis patients may be more vulnerable to COVID-19. Accordingly, our study findings indicate that bronchiectasis patients should be more cautious about social activities or travel in areas where COVID-19 is prevalent.11
Another notable finding is that COVID-19 patients with bronchiectasis suffered from more severe infection than those without bronchiectasis. In this study, COVID-19 patients with bronchiectasis exhibited a much higher rate of supplemental oxygen, ECMO, and higher mortality than those without bronchiectasis. Considering similar ICU admission rates, COVID-19 patients with bronchiectasis revealed worse clinical course finally than those without bronchiectasis although both groups had similar severity when admitted to ICU initially. Impaired mucociliary clearance and chronic inflammation in the airway of patients with bronchiectasis is likely to increase their susceptibility to and severity of COVID-19. Additionally, COVID-19 could exacerbate bronchiectasis. Interestingly, COVID-19 patients with bronchiectasis showed a significantly higher prevalence of COPD (57.6% versus 19.3%) and asthma (62.1% versus 17.2%) than the overall population with bronchiectasis in South Korea.10 Although asthmatics were suggested to be protected from COVID-19,12 this study showed significantly higher asthma rate in COVID-19 patients with bronchiectasis than those without bronchiectasis. Bronchiectasis may serve as a leverage to more severe COVID-19 in asthmatics; however, future research is necessary to clarify the mechanistic link. Previous research revealed that patients with COPD or asthma showed more severe clinical course and worse outcome if they have comorbid bronchiectasis.13 In line with the study, comorbid airway disease may play a major role in poorer clinical outcomes in bronchiectasis patients with COVID-19.
The major strength of this study is that it is the first real-world report on the impact of bronchiectasis on the susceptibility to and severity of COVID-19. Nonetheless, there are also several limitations to this study. First, since the NHIS database for COVID-19 did not provide data on smoking history, pulmonary function tests, laboratory findings, medications, and the duration of hospital stay, we could not include this information in our study results. Second, for the same reason above-mentioned, this study could not provide information about bronchiectasis in detail: aetiology of bronchiectasis, exacerbation history, and Pseudomonas colonisation in sputum. Accordingly, reports from international bronchiectasis registries are warranted shortly. Third, as the number of COVID-19 patients with bronchiectasis was small (1.3% of all study population), we could not establish a well-fitted regression analysis model accounting whether increased prevalence and more severe clinical course of COVID-19 did not result from comorbidities in bronchiectasis patients. Fourth, COVID-19 patients with bronchiectasis were older and had more comorbidities than those without bronchiectasis. Although it was a natural phenomenon that patients with bronchiectasis were older and had more comorbidities, this may have affected the more severe clinical presentations and poor clinical outcomes.
In conclusion, patients with bronchiectasis may be more prone to COVID-19 infection than those without bronchiectasis. Additionally, COVID-19 patients with bronchiectasis showed more severe clinical manifestations and poorer outcomes than those without bronchiectasis.
Supplemental Material
Supplemental material, sj-pdf-1-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-2-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-3-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Footnotes
Author contributions: HC, HL, and SHK were responsible for the conception and design of the study. HC, HL, SKL, BY, SJC, YY, and SHK undertook the analysis and interpretation of the data. HC, HL, SKL, TSP, DWP, JYM, THK, JWS, and SHK drafted the manuscript. HC, HL, HJY, and SHK made a critical revision of the manuscript. All authors read and approved the final manuscript.
Availability of data and material: All data extracted in this study are included in this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0218) and the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2019M3E5D1A01069363).
Ethical approval and consent to participate: The institutional review board of our institution approved this study (application No. HYUH 2020-06-029). Since the NHIS database was constructed after anonymisation, the need for informed consent from the participants was waived.
ORCID iDs: Hayoung Choi  https://orcid.org/0000-0003-4812-0653
https://orcid.org/0000-0003-4812-0653
Sang-Heon Kim  https://orcid.org/0000-0001-8398-4444
https://orcid.org/0000-0001-8398-4444
Supplemental material: The reviews of this paper are available via the supplemental material section.
Contributor Information
Hayoung Choi, Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
Hyun Lee, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Sun-Kyung Lee, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea; Department of Mathematics, College of Natural Sciences, Hanyang University, Seoul, Korea.
Bumhee Yang, Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Chungcheongbuk-do, Korea.
Sung Jun Chung, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Yoomi Yeo, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Tai Sun Park, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Dong Won Park, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Ji-Yong Moon, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Tae-Hyung Kim, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Jang Won Sohn, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Ho Joo Yoon, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
Sang-Heon Kim, Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, 222-1, Wangsimni-ro, Seongdong-gu, Seoul, 04763, Korea.
References
- 1. Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Leung JM, Niikura M, Yang CWT, et al. COVID-19 and COPD. Eur Respir J 2020; 56: 2002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. García-Pachón E, Zamora-Molina L, Soler-Sempere MJ, et al. Asthma and COPD in hospitalized COVID-19 patients. Arch Bronconeumol 2020; 56: 604–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang JM, Koh HY, Moon SY, et al. Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol 2020; 146: 790–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020; 94: 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alqahtani JS, Oyelade T, Aldhahir AM, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS One 2020; 15: e0233147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584: 430–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang B, Choi H, Lee S-K, et al. Risk of coronavirus disease incidence, severe presentation, and mortality in patients with lung cancer. J Korean Cancer Assoc. Epub ahead of print 28 December 2020. DOI: 10.4143/crt.2020.1242. [DOI] [Google Scholar]
- 9. Hong KH, Lee SW, Kim TS, et al. Guidelines for laboratory diagnosis of coronavirus disease 2019 (COVID-19) in Korea. Ann Lab Med 2020; 40: 351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Choi H, Yang B, Nam H, et al. Population-based prevalence of bronchiectasis and associated comorbidities in South Korea. Eur Respir J 2019; 54: 1900194. [DOI] [PubMed] [Google Scholar]
- 11. Shteinberg M, Crossley B, Lavie T, et al. Recommendations for travelling with bronchiectasis: a joint ELF/EMBARC/ERN-lung collaboration. ERJ Open Res 2019; 5: 00113–02019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Assaf SM, Tarasevych SP, Diamant Z, et al. Asthma and severe acute respiratory syndrome coronavirus 2019: current evidence and knowledge gaps. Curr Opin Pulm Med 2021; 27: 45–53. [DOI] [PubMed] [Google Scholar]
- 13. Choi H, Lee H, Ryu J, et al. Bronchiectasis and increased mortality in patients with corticosteroid-dependent severe asthma: a nationwide population study. Ther Adv Respir Dis 2020; 14: 1753466620963030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-2-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-3-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_1753466621995043 for Impact of bronchiectasis on susceptibility to and severity of COVID-19: a nationwide cohort study by Hayoung Choi, Hyun Lee, Sun-Kyung Lee, Bumhee Yang, Sung Jun Chung, Yoomi Yeo, Tai Sun Park, Dong Won Park, Ji-Yong Moon, Tae-Hyung Kim, Jang Won Sohn, Ho Joo Yoon and Sang-Heon Kim in Therapeutic Advances in Respiratory Disease